Abstract
Background
Violent crime has recently increased in many major metropolitan cities in the United States. Prior studies suggest an association between neighborhood crime levels and cardiovascular disease, but many have been limited by cross‐sectional designs. We investigated whether longitudinal changes in violent crime rates are associated with changes in cardiovascular mortality rates at the community level in one large US city‐Chicago, IL.
Methods and Results
Chicago is composed of 77 community areas. Age‐adjusted mortality rates by community area for cardiovascular disease, stroke, and coronary artery disease from 2000 to 2014, aggregated at 5‐year intervals, were obtained from the Illinois Department of Public Health Division of Vital Records. Mean total and violent crime rates by community area were obtained from the City of Chicago Police Data Portal. Using a 2‐way fixed effects estimator, we assessed the association between longitudinal changes in violent crime and cardiovascular mortality rates after accounting for changes in demographic and economic variables and secular time trends at the community area level from 2000 to 2014. Between 2000 and 2014, the median violent crime rate in Chicago decreased from 3620 per 100 000 (interquartile range [IQR], 2256, 7777) in the 2000 to 2004 period to 2390 (IQR 1507, 5745) in the 2010 to 2014 period (P=0.005 for trend). In the fixed effects model a 1% decrease in community area violent crime rate was associated with a 0.21% (95% CI, 0.09–0.33) decrease in cardiovascular mortality rates (P=<0.001) and a 0.19% (95% CI, 0.04–0.33) decrease in coronary artery disease mortality rates (P=0.01). There was no statistically significant association between change in violent crime and stroke mortality rates (−0.17% [95% CI, −0.42 to 0.08; P=0.18]).
Conclusions
From 2000 to 2014, a greater decrease in violent crime at the community area level was associated with a greater decrease in cardiovascular and coronary artery disease mortality rates in Chicago. These findings add to the growing evidence of the impact of the built environment on health and implicate violent crime exposure as a potential social determinant of cardiovascular health. Targeted investment in communities to decrease violent crime may improve community cardiovascular health.
Keywords: built environment, cardiovascular disease, crime, mortality, social determinants of health, structural racism
Subject Categories: Cardiovascular Disease, Social Determinants of Health, Health Services, Risk Factors
Clinical Perspective.
What Is New?
Community areas in Chicago with the greatest decrease in violent crime rates experienced the greatest decline in age‐adjusted cardiovascular mortality rates, after accounting for changes in sociodemographic and economic factors.
Exposure to violent crime may be an important social determinant of cardiovascular health situated in the broader context of the ways in which structural racism harms health.
What Are the Clinical Implications?
Community investment and non‐police interventions to decrease rates of violent crime may help improve community cardiovascular health.
After many years of decline, violent crime has been noted to be increasing in cities across the United States more recently. 1 In 2020, the per‐capita homicide rate increased by 30% in the largest 34 cities in the United States, and violent crime rates are projected to continue to climb. 2 Violent crime is largely concentrated in Black urban neighborhoods as a result of historic and ongoing racist policies leading to racial segregation, community disinvestment, and concentrated poverty. 3 , 4 , 5 Residents in these neighborhoods also have a high preexisting burden of chronic diseases, especially cardiovascular disease. 1 , 6 There is increasing evidence that neighborhood environment contributes to cardiovascular disease risk, 7 , 8 , 9 , 10 and exposure to violent crime may be an important social determinant of cardiovascular health, especially among racially and ethnically minoritized groups. 11
Exposure to violent crime leads to activation of physiologic pathways and chronic psychosocial stress, which in turn influences biology and behavior in ways that contribute to development of cardiovascular disease. 12 Living in a high crime area has been associated with delays in obtaining needed care, 13 as well as lower rates of physical activity 14 , 15 and unhealthy eating. 16 Biological effects, through activation of stress response pathways, lead to impaired glucose metabolism, chronic inflammation, increased vascular reactivity, and oxidative damage, which play a key role in cardiovascular disease development. 12 , 17 , 18 , 19 Recurrent exposure to high rates of violent crime has been shown to be independently associated with obesity and elevated blood pressure. 20 Neighborhoods with the highest rates of violent crime have a higher risk of coronary heart disease. 21 Spikes in violent crime are associated with acute increases in hospital visits and death due to acute myocardial infarction. 22 However, as many of the prior studies have been cross‐sectional in design or have focused on certain subsets of violent crimes, it is unknown whether trends in overall violent crime rates, at the community or neighborhood level, are associated with changes in cardiovascular mortality.
Racial disparities in cardiovascular disease burden and outcomes are pervasive. 23 New community‐level interventions are needed to address these disparities. 24 It is unclear whether community‐based non‐police interventions that decrease violent crime, such as improvements in neighborhood infrastructure, 25 can improve cardiovascular health outcomes, particularly among racially and ethnically minoritized communities. Understanding the relationship between trends in violent crime and cardiovascular health may therefore help inform strategies to improve community cardiovascular health and identify areas particularly vulnerable to worsening cardiovascular health outcomes. The aim of this study was to investigate whether longitudinal changes in violent crime rates were associated with cardiovascular mortality at the community level in one large US city, Chicago, Illinois, from 2000 to 2014.
METHODS
Data Sources and Measures
The data that support the findings of this study are available from the corresponding author upon reasonable request. This study was considered exempt from review by the University of Pennsylvania Institutional Review Board as all data used are routinely collected and publicly available. Chicago consists of 77 community area with stable boundaries over time that allow for longitudinal analyses. 26 These community areas, which are smaller than ZIP codes, correspond to a neighborhood or several small neighborhoods. Using the Illinois Department of Public Health Division of Vital Records, we obtained age‐adjusted mortality rates by community area for cardiovascular disease (International Classification of Diseases, Tenth Revision [ICD‐10]) codes: I00‐I09, I11, I13, I20‐I51), stroke (ICD‐10 codes: I60‐I69), and coronary artery disease (ICD‐10 codes: I20‐I25) deaths from 2000 to 2014 (age>35 years). 27 Community area level mortality rates were available aggregated into 5‐year time periods: 2000 to 2004, 2005 to 2009, and 2010 to 2014.
Annual crime data were obtained from the City of Chicago Police Data Portal, a publicly available data set of all reported incidents of crime to the Chicago Police Department, geocoded to the city block of crime occurrence. 28 Each incident was assigned to the community area that the city block where it occurred was located in. Violent crime was defined, based on the Uniform Crime Reporting Program administered by the Federal Bureau of Investigations, as assault, battery, criminal sexual assault, robbery, and homicide based on the Chicago Police Department Crime Type Categories. 29 All other crimes, were considered nonviolent. Crime data were available for each year from 2001 to 2014. After calculating the annual, community‐level, per capita rates of violent and nonviolent crime, the mean of these rates over each of the 5‐year time period that the mortality data were available for was calculated. For the first time period (2000–2004), mean annual crime rates from 2001 to 2004 were used.
Additional demographic and economic variables at the community area level were obtained from US Census Bureau data. The following community area level variables were obtained: median household income (inflation adjusted to 2000), unemployment rate (>16 years), less than high school educational attainment rate (age>25 years), housing vacancy rate, and proportion of residents by race, and ethnicity of all residents. 30 , 31 , 32 As data were not available for each time period at the community area level, data from the 2000 US Census was assigned to the 2000 to 2004 time period, data from the 5‐year American Community survey for the years 2006 to 2010 were assigned to the 2004 to 2009 time period, and data from the 5‐year American Community survey for the years 2014 to 2018 were assigned to the 2010 to 2014 time period.
Two additional variables were used in secondary analyses: the number of residents of a community area per physician in each community area for the year 2008 obtained from the American Medical Association DoctorFinder tool (data available in quintiles of community areas as calculated by the Northwestern University Feinberg School of Medicine, Center for Healthcare Equity/Institute for Healthcare Studies) and the community area level percentage of the adult population with health insurance obtained from the 5‐year American Community survey for the years 2008 to 2012. 33 , 34
Outcomes
The primary outcome was the percent change in community area level age‐adjusted cardiovascular mortality rates from 2000 to 2014. Secondary outcomes include percent change in age‐adjusted mortality rates from coronary artery disease and stroke during the same time period.
Statistical Analysis
We first calculated population‐weighted summary measures of each variable for each of the three 3 time periods. Mean percent change, over the 3 periods, in crime and mortality rates were also calculated. Linear trends in each variable over the 3 periods were assessed using a fixed effects model with a linear period term (ie, period treated as a linear continuous variable). We compared the mean percent change for mortality rates between tertiles of community areas based on change in crime rates using Kruskal‐Wallis tests. To estimate the association between change in violent crime rates and change in cardiovascular mortality, a 2‐way fixed effects model was used. A fixed effects, or within, estimator is a longitudinal analysis technique that by examining the association between longitudinal change in the predictor and outcome variables for each subject (community area in this analysis) can control for both measured and unmeasured time‐invariant confounders. 35 A 2‐way fixed effects estimator also includes an indicator for time to account for secular time trends in the outcome. To account for other potential community area level time‐varying confounders that may influence the association between violent crime and cardiovascular mortality rates, the following time‐varying covariates were included in the model: proportion of residents who are non‐Hispanic Black, Hispanic (any race or ethnicity), other race (which included Asian, American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, or more races, or some other race), inflation‐adjusted median household income, unemployment rate, housing vacancy rate, and less than high school educational attainment rate. Mortality and violent crime rates were included as log transformed variables in the model. As all variables were aggregated at the community area level, the model was weighted by the community area population.
In secondary analyses, we explored the association between change in violent crime rates and the secondary outcomes of mortality rates from coronary artery disease and stroke, as well as the association between change in cardiovascular mortality and total crime rates. Additionally, to evaluate the role of health care access in the associations noted in the primary analysis, quintile of the number of residents per physician (including primary and specialty care physicians) and the proportion of residents with health insurance coverage, were included in 1 model. As both additional covariates were available only at a single time point, a Hausman‐Taylor estimator was used, 36 which, unlike a traditional fixed‐effects model, allows for the estimation of coefficients for time‐invariant covariates within a fixed‐effects framework. This secondary model was not weighted by the community area population.
Results are presented as means with SD or 95% CIs or medians with interquartile range (IQR) as indicated. P values <0.05 were considered statistically significant. There was no P value adjustment for multiple comparisons. Summary statistics and time trends for the primary 2‐way fixed effects model were estimated using SAS 9.4. The Hausman‐Taylor model was estimated using STATA 15. Drs Eberly and Khatana had full access to all data and are responsible for its integrity.
RESULTS
Trends in time‐varying demographic and economic characteristics for all 77 community areas, weighted by population, by time period are summarized in Table 1. The population‐weighted proportion of Black residents declined over the 3 time periods from a median of 17.0% (IQR 3, 85) in the first time period to 8.9% (3.2, 47.5) in the third time period (P<0.0001 for trend). The proportion of Hispanic residents increased over the 3 time periods from 16.5% (IQR 4.1, 46.9) to 18.4% (IQR 5.9, 47.5) (P=0.02). The unemployment rate (P=0.0001) and vacant housing rate (P<0.0001) initially increased in the second time period, but then declined in the third time period (unemployment: 8.3% to 10.6% to 7.7%; vacant housing: 6.8% to 12.1% to 10.4%).
Table 1.
Population Weighted Sociodemographic and Economic Variables for All 77 Chicago Community Areas by Time Period
| Variable | Time period | P value for trend | ||
|---|---|---|---|---|
| 2000–2004 | 2005–2009 | 2010–2014 | ||
| Population, median [IQR] | 32 275.0 (18 165, 52 723) | 31 028 (18 109, 48 743) | 29 021 (19 342, 45 271) | <0.0001 |
| Proportion of residents in following subgroups: | ||||
| Non‐Hispanic Black, median [IQR] | 17.0 (3.0, 85.5) | 11.5 (4.0, 72.0) | 8.9 (3.2, 47.5) | <0.0001 |
| Hispanic (any race or ethnicity), median [IQR] | 16.5 (4.1, 46.9) | 16.6 (5.2, 50.6) | 18.4 (5.9, 47.5) | 0.02 |
| Other race‡, median [IQR] | 3.4 (1.3, 7.4) | 3.6 (1.3, 9.4) | 5.9 (1.9, 12.4) | <0.0001 |
| Unemployment rate, median [IQR] | 8.3 (6.0, 15.7) | 10.6 (7.6, 16.7) | 7.7 (4.3, 13.6) | 0.0001 |
| Vacant housing rate, median [IQR] | 6.8 (4.3, 10.1) | 12.1 (8.9, 17.7) | 10.4 (8.6, 14.5) | <0.0001 |
| Median household income, median [IQR]* | 34 639.85 (30 704.00, 42 861.15) | 41 528.22 (330 393.76, 58 985.61) | 38 397.86 (25 649.14, 55 746.42) | <0.0001 |
| Less than high school education rate, median [IQR] | 28.0 (21.2, 39.5) | 18.7 (13.2, 30.3) | 14.4 (8.0, 21.4) | <0.0001 |
| Total crime rate† | 12 662.7 (9618.2, 23 032.9) | 11299.5 (8622.7, 23 965.0) | 8276.9 (6371.0, 16 620.6) | <0.0001 |
| Violent crime rate† | 3501.1 (2164.1, 7650.4) | 2952.7 (1998.0, 6573.7) | 2159.4 (1411.9, 4975.1) | <0.0001 |
IQR indicates interquartile range.
Inflation adjusted to year 2000.
Crime rate is per 100 000.
Other race includes Asian, American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, 2 or more races, or some other race.
The population weighted median violent crime rate in Chicago decreased over the 3 time periods (P<0.001 for linear time trend). The median violent crime rate was 3501.1 per 100 000 (IQR 2164, 7650) in the 2000 to 2004 period, 2952.7 per 100 000 (IQR 1998.0, 6573.7) in the 2005 to 2009 period, and 2159.4 (IQR 1412, 4975) in the 2010 to 2014 period (P<0.001 for linear time trend) (Table 1). The mean percent change in violent crime rates across all community areas over the study period was −15.8% (SD=9.8%). Among the 77 community areas, in the tertile with the greatest decrease in violent crime rates, the mean percent change for violent crime rates over the study period ranged from −59.2% (SD=13.7) to −19.0% (SD=15.0) (Figure). In the intermediate tertile, it ranged from −18.8% (SD=11.2) to −10.5% (SD=11.7). In the tertile of community areas with the smallest decrease or increase in violent crime rates, the mean percent change ranged from −10.3% (SD=15.9) to 2.9% (SD=16.7).
Figure 1. Mean percent change for age‐adjusted cardiovascular mortality and violent crime by community area in Chicago, Illinois between 2000 and 2014*.
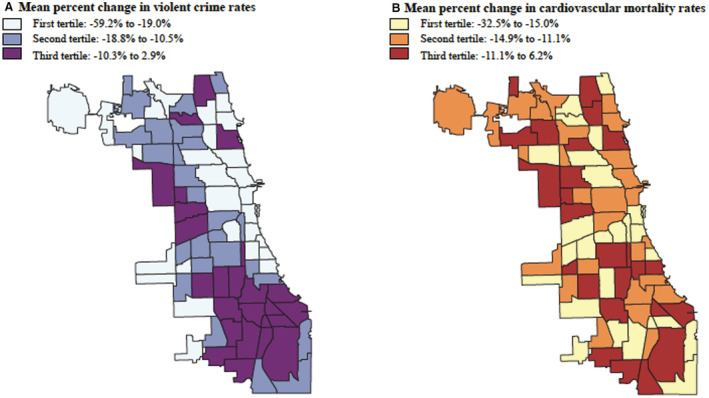
*Mean of the percent change between each period in each community area.
The median age‐adjusted cardiovascular mortality rate in Chicago was 276.8 per 100 000 (IQR 245.8, 320.5) in the 2000 to 2004 period, 230.0 per 100 000 (IQR 195.5, 267.7) in the 2005 to 2009 period, and 197.1 (IQR 178.0, 246.2) in the 2010 to 2014 period (P<0.0001 for linear time trend). The mean percent change in cardiovascular mortality rates across all community areas over the 3 periods was −13.1% (SD=4.7%). In the tertile of community areas with the greatest decrease in cardiovascular mortality rates, the mean percent change for cardiovascular mortality rates ranged from −32.5% (SD=5.5) to −15.0% (SD=4.7) (Figure). In the intermediate tertile, it ranged from −14.9% (SD=22.8) to −11.1% (SD=3.0). In the tertile of community areas with the smallest decrease or increase in cardiovascular mortality rates, the mean percent change ranged from −11.1% (SD=1.6) to 6.2% (SD=24.2).
Between 2000 and 2014, the mean percent change for age‐adjusted cardiovascular mortality rates was −14.8% (SD=3.4) in the tertile of community areas with the greatest decrease in violent crime rates, −13.1% (SD=5.2) in the intermediate tertile, and −11.5% (SD=4.8) in the tertile with smallest decrease or increase in violent crime rates (P=0.48 for comparison between first and intermediate tertile and P=0.02 for comparison between first and third tertile) (Table 2).
Table 2.
Changes in Age‐Adjusted Cardiovascular Mortality by Community Area Tertiles of Change in Violent Crime Rates
| Community area tertiles based on change in violent crime rate* | Mean percent change for age‐adjusted cardiovascular morality rate (SD)† | P value for difference compared with first tertile† |
|---|---|---|
| First tertile (smallest change) | 11.5 (4.8) | … |
| Second tertile | −13.1 (5.2) | 0.48 |
| Third tertile (largest change) | −14.8 (3.4) | 0.02 |
Tertiles of change in violent crime rate based on mean percent change in violent crime rates between each period in each community area. first tertile: −59.2% to −19.0%, second tertile: −18.8% to −10.5%, third tertile: −10.3% to 2.9%.
Mean of the percent change in age‐adjusted cardiovascular mortality rates between each period in each community area.
In the 2‐way fixed effects model, after accounting for changes in demographic and economic variables and secular time trends, a 1% decrease in community area violent crime rates was associated with a 0.21% (95% CI, 0.09–0.33) decrease in cardiovascular mortality rates (P<0.001) (Table 3).
Table 3.
Association of Changes in Community‐Area Violent Crime with Change in Cardiovascular Outcomes
| Outcome* | Cardiovascular mortality rates | Coronary artery disease mortality rates | Stroke mortality rates | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | 95% CI | P value | Estimate | 95% CI | P value | Estimate | 95% CI | P value |
| Violent crime rate* | 0.21† | 0.09 to 0.33 | 0.0006 | 0.19† | 0.042 to 0.33 | 0.01 | 0.17† | −0.077 to 0.422 | 0.18 |
| Proportion of residents non‐Hispanic Black | −0.005 | −0.008 to −0.001 | 0.01 | −0.003 | −0.008 to 0.001 | 0.15 | 0.0003 | −0.008 to 0.008 | 0.95 |
| Proportion of residents Hispanic (any race or ethnicity) | 0.003 | 0.001 to 0.005 | 0.007 | 0.003 | 0.0007 to 0.006 | 0.01 | 0.005 | 0.001 to 0.010 | 0.03 |
| Proportion of residents other race‡ | −0.008 | −0.014 to −0.001 | 0.02 | −0.010 | −0.018 to −0.002 | 0.02 | 0.01 | −0.004 to 0.024 | 0.15 |
| Unemployment rate | 0.004 | −0.0004 to 0.008 | 0.08 | 0.004 | −0.001 to 0.009 | 0.13 | −0.007 | −0.015 to 0.002 | 0.14 |
| Vacant housing rate | 4.26×10−6 | 1.77×10−6 to 6.75×10−6 | 0.001 | 5.45×10−6 | 2.37×10−6 to 8.53×10−6 | 0.0007 | 3.27×10−6 | −2.00×10−6 to 8.54×10−6 | 0.23 |
| Median household income | 0.001 | −0.003 to 0.006 | 0.52 | 0.002 | −0.004 to 0.007 | 0.52 | 0.01 | 0.001 to 0.019 | 0.04 |
| Less than high school education attainment rate | −0.002 | −0.005 to 0.001 | 0.19 | −0.005 | −0.009 to −0.001 | 0.02 | 0.001 | −0.006 to 0.008 | 0.74 |
| Period 2000–2004 | Reference | ||||||||
| Period 2005–2009 | −0.24 | −0.29 to −0.19 | <0.0001 | −0.36 | −0.43 to −0.30 | <0.0001 | −0.28 | −0.39 to −0.16 | <0.0001 |
| Period 2010–2014 | −0.27 | −0.35 to −0.20 | <0.0001 | −0.51 | −0.60 to 0.41 | <0.0001 | −0.35 | −0.50 to −0.19 | <0.0001 |
Included in model as a log transformed variable. Rate is per 100 000 residents.
A 1% change in the independent variable associated with a percent change in the outcome equal to the estimate value.
Other race includes Asian, American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, 2 or more races, or some other race.
Secondary Analyses
The median age‐adjusted coronary artery disease mortality rate in Chicago was 203.0 per 100 000 (IQR 184.9, 217.4) in the 2000 to 2004 period, 156.8 per 100 000 (IQR 136.5, 171.1) in the 2005 to 2009 period, and 126.6 (IQR 108.8, 136.8) in the 2010 to 2014 period (P<0.0001 for linear time trend). The mean percent change in coronary artery disease mortality rates across all community areas over the 3 periods was −20.8% (SD=5.1%). The median age‐adjusted stroke mortality rate in Chicago was 49.8 per 100 000 (IQR 45.5, 63.0) in the 2000 to 2004 period, 41.6 per 100 000 (IQR 34.7, 41.6) in the 2005 to 2009 period, and 35.8 (IQR 30.0, 44.2) in the 2010 to 2014 period (P<0.0001 for linear time trend). The mean percent change in stroke mortality rates across all community areas was −13.6% (SD=8.3). In the 2‐way fixed effects model, a 1% decrease violent crime rates was also associated with a 0.19% (95% CI, 0.04–0.33) decrease in age‐adjusted coronary artery disease mortality rates (P=0.01) (Table 3). There was no significant association between change in violent crime rates and stroke mortality rates (−0.17% [95% CI, −0.42 to 0.08; P=0.18]) (Table 3).
A 1% decrease in total crime rates over the study period was associated with a 0.16% (95% CI, 0.04–0.29) decrease in cardiovascular disease mortality rates (P=0.009) (Table 4). There was no significant association between change in total crime rates and mortality rates for coronary artery disease (−0.11% [95% CI, −0.26 to 0.04; P=0.15]) or stroke (−0.19% [95% CI, −0.44 to 0.07; P=0.15]) (Table 3). In the Hausman‐Taylor model incorporating time‐invariant quintile of the number of community area residents per physician and health insurance coverage, changes in violent crime remained significantly associated with changes in cardiovascular mortality, and there was no significant association noted between change in cardiovascular mortality rates and either of the 2 health care related variables (Table S1).
Table 4.
Association of Changes in Community‐Area Total Crime and Cardiovascular Outcomes
| Outcome* | Cardiovascular mortality rates | Coronary artery disease mortality rates | Stroke mortality rates | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Estimate | 95% CI | P value | Estimate | 95% CI | P value | Estimate | 95% CI | P value |
| Total crime* | 0.16† | 0.04 to 0.29 | 0.009 | 0.11† | −0.04 to 0.26 | 0.15 | 0.19† | −0.07 to 0.44 | 0.15 |
| Black race | −0.004 | −0.007 to −4.20×10−6 | 0.05 | −0.003 | −0.007 to 0.002 | 0.30 | 0.001 | −0.007 to 0.009 | 0.81 |
| Hispanic ethnicity | 0.003 | 0.001 to 0.006 | 0.004 | 0.004 | 0.0007 to 0.006 | 0.01 | 0.006 | 0.0009 to 0.01 | 0.02 |
| Other race‡ | −0.008 | −0.015 to −0.0011 | 0.02 | −0.01 | −0.02 to −0.002 | 0.01 | 0.01 | −0.003 to 0.02 | 0.14 |
| Unemployment | 0.003 | −0.0008 to 0.008 | 0.12 | 0.004 | −0.001 to 0.009 | 0.15 | −0.007 | −0.02 to 0.002 | 0.12 |
| Vacant housing | 3.55×10−6 | 1.08×10−6 to 6.02×10−6 | 0.006 | 4.46×10−6 | 1.41×10−6 to 7.52×10−6 | 0.005 | 3.20×10−6 | −1.95×10−6 to 8.36×10−6 | 0.22 |
| Median Household Income | 0.001 | −0.003 to 0.006 | 0.61 | 0.002 | −0.004 to 0.008 | 0.49 | 0.009 | −0.0004 to 0.018 | 0.06 |
| Less than high school education | −0.002 | −0.005 to 0.001 | 0.21 | −0.005 | −0.009 to −0.001 | 0.02 | 0.002 | −0.005 to 0.008 | 0.66 |
| Year 2000–2004 | Reference | ||||||||
| Year 2005–2009 | −0.24 | −0.30 to −0.19 | <0.0001 | −0.37 | −0.44 to −0.30 | <0.0001 | −0.28 | −0.40 to −0.16 | <0.0001 |
| Year 2010–2014 | −0.29 | −0.37 to −0.21 | <0.0001 | −0.53 | −0.63 to −0.44 | <0.0001 | −0.34 | −0.50 to −0.18 | <0.0001 |
Included in model as a log transformed variable. Rate is per 100 000 residents.
A 1% change in the independent variable is associated with a percent change in the outcome equal to the estimate value.
Other race includes Asian, American Indian or Alaska Native, Native Hawaiian and Other Pacific Islander, 2 or more races, or some other race.
DISCUSSION
From 2000 to 2014, Chicago community areas experiencing the greatest decrease in violent crime rates had the greatest decline in age‐adjusted cardiovascular mortality rates whereas community areas with the smallest decrease in crime had a significantly smaller decline in mortality rates. After controlling for time‐invariant differences between communities, secular trends in mortality, and changes in important time‐varying sociodemographic and economic factors, a decrease in community area level violent crime rates in Chicago was significantly associated with a decrease in mortality rates from cardiovascular and coronary artery disease.
The pathophysiologic mechanisms that may explain the association between violent crime and adverse cardiovascular outcomes are likely multifactorial. The psychosocial stress triggered by exposure to violent crime is associated with lower consumption of healthy foods and higher rates of substance use. 16 Safety concerns preclude opportunities for healthy physical activity. 14 , 37 Chronic psychologic stress, triggered by crime exposure, is associated with chronic activation of physiologic stress pathways, which induce insulin resistance, atherosclerosis, and vascular reactivity. 17 , 19 , 38 , 39 Recurrent exposure to high rates of violent crime is associated with higher body mass index, elevated blood pressure, and other cardiovascular disease risk factors. 20 , 21 , 40 , 41 Exposure to violent crime is also associated with delays in prescription fills, missing outpatient appointments, and increases in cardiovascular disease‐related hospital admissions. 13 , 41
In our analysis, although crime rates fell, on average, in nearly all community areas, there were significant differences in the rate of this decline. Community areas that experienced the smallest decline in crime also experienced the smallest improvements in cardiovascular mortality, thus exacerbating preexisting disparities between neighborhoods in the city. With the recent rise in crime rates in the United States, 2 our results suggest that these disparities may become even more pronounced over time.
Given the relationship we found between violent crime and cardiovascular outcomes, it is important to consider the root causes of violence. Structural racism—both in historical government policies such as redlining and ongoing discriminatory practices within the real estate and banking industries—has resulted in many Black neighborhoods that have dealt with sustained and intentional disinvestment, including concentrated poverty, failing schools, and lack of economic opportunities. 3 , 4 , 5 , 42 , 43 , 44 One salient result are neighborhood conditions marked by deterioration—crumbling housing stock, blighted vacant land, and a lack of greenspace. These neighborhood conditions have been associated with both violent crime and poor cardiovascular outcomes. 7 , 8 , 21 , 45 , 46 Given the demonstrated association between violent crime and cardiovascular outcomes, independent of other economic factors, our results implicate violent crime as a potential social determinant of cardiovascular health situated in the broader context of the ways in which structural racism harms health.
These findings add to the growing evidence of the impact of the built environment on health and have important public health considerations. Economic prosperity has been previously demonstrated to be associated with cardiovascular mortality. 47 Communities with high crime rates receive less economic investment, thus perpetuating a cycle of poverty that has long‐lasting impacts on health. 48 Targeted and sustained investment to break the link between long‐standing community disinvestment and subsequent poor health outcomes is needed, particularly in Black neighborhoods. 49 How evidence‐based non‐police neighborhood interventions associated with crime reduction, such as housing and blight remediation, provision of subsidized affordable housing units, greening vacant land, and structural housing repairs, 24 , 25 , 49 , 50 , 51 , 52 affect cardiovascular health warrants further attention. In addition, we must acknowledge the legacy of racist policies and practices that have led to concentrated disadvantage and crime in Black and other racially and ethnically minoritized neighborhoods. Policies must be implemented to address the health consequences of structural racism and racial segregation. Community partnerships are essential to further expand our knowledge of the impact of violent crime on cardiovascular health and the impact of community‐driven interventions on violence‐related cardiovascular outcomes. 24
Our study has several limitations. Because of the observational nature of this study, causal inferences cannot be made. As this is an ecological study at the community area level, individual level inferences from the findings cannot be made. 53 Although the 2‐way fixed effects model accounts for measured or unmeasured time‐invariant confounders as well as secular time trends in the outcome, residual time‐varying confounding as well as reverse causality are still possible. However, we accounted for several important economic and demographic time‐varying confounders that have previously been shown to be associated with cardiovascular health. Although not all of the time‐varying covariates used in the model were from the exact period for which the mortality rates were available, they do allow us to adjust for trends in these potential important time‐varying confounders. Regarding reverse causality, it is theoretically plausible that changes in cardiovascular mortality rates may influence changes in violent crime rates in an area rather than vice versa. Our study has the benefit of granularity at the community area level (rather than census or ZIP code level). However, to account for the statistical instability of small‐area estimates, data were aggregated over multiyear periods and we were unable to evaluate changes on a smaller time scale (such as annually). Cardiovascular health outcomes were tied to a community area of residence and corresponding exposure to violent crime in that area were determined. Some of the reported crime incidents in a community area may be for nonresidents. Data were available only through 2014 and thus do not capture more recent years including recent rises in crime. These results represent 1 large urban US city and may not be generalizable to other cities.
CONCLUSIONS
From 2000 to 2014, decreases in violent crime rates were significantly associated with improvements in cardiovascular mortality in community areas in Chicago. The disparity in cardiovascular mortality rates between community areas was exacerbated as communities with the smallest improvements in violent crime rates experienced the smallest improvements in cardiovascular mortality. Given recently reported increases in violent crime in US cities, further widening of the gap in cardiovascular health between communities is likely. Therefore, investigating whether non‐police community‐based strategies to decrease violent crime may play a role in community cardiovascular health is crucial.
Sources of Funding
Dr Khatana receives grants from the National Heart, Lung, and Blood Institute (5K23HL153772–02) and the American Heart Association (20CDA35320251).
Disclosures
None.
Supporting information
Table S1
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.122.025168
For Sources of Funding and Disclosures, see page 8.
References
- 1. Friedman M, Grawert A, Cullen J. Crime in 2016. New York, NY: Brennan Center for Justice; 2016:7. [Google Scholar]
- 2. Rosenfeld R, Abt T, Lopez E. Pandemic, Social Unrest, and Crime in U.S. Cities: 2020 Year‐End Update. Washington, D.C.: Council on Criminal Justice; 2021. [Google Scholar]
- 3. Sampson RJ, Wilson WJ, Katz H. Reassessing “toward a theory of race, crime, and urban inequality”: enduring and new challenges in 21st century America. Du Bois Rev. 2018;15:13–34. doi: 10.1017/S1742058X18000140 [DOI] [Google Scholar]
- 4. Hipp JR. Spreading the wealth: the effect of the distribution of income and race/ethnicity across households and neighborhoods on city crime trajectories. Criminology. 2011;49:631–665. doi: 10.1111/j.1745-9125.2011.00238.x [DOI] [Google Scholar]
- 5. Krivo LJ, Peterson RD, Kuhl DC. Segregation, racial structure, and neighborhood violent crime. AJS. 2009;114:1765–1802. doi: 10.1086/597285 [DOI] [PubMed] [Google Scholar]
- 6. Sumner SA, Mercy JA, Dahlberg LL, Hillis SD, Klevens J, Houry D. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314:478–488. doi: 10.1001/jama.2015.8371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Diez Roux AV, Merkin SS, Arnett D, Chambless L, Massing M, Nieto FJ, Sorlie P, Szklo M, Tyroler HA, Watson RL. Neighborhood of residence and incidence of coronary heart disease. N Engl J Med. 2001;345:99–106. doi: 10.1056/NEJM200107123450205 [DOI] [PubMed] [Google Scholar]
- 8. Diez Roux AV, Kershaw K, Lisabeth L. Neighborhoods and cardiovascular risk: beyond individual‐level risk factors. Curr Cardiovasc Risk Rep. 2008;2:175–180. doi: 10.1007/s12170-008-0033-0 [DOI] [Google Scholar]
- 9. Leal C, Chaix B. The influence of geographic life environments on cardiometabolic risk factors: a systematic review, a methodological assessment and a research agenda. Obes Rev. 2011;12:217–230. doi: 10.1111/j.1467-789X.2010.00726.x [DOI] [PubMed] [Google Scholar]
- 10. Unger E, Diez‐Roux AV, Lloyd‐Jones DM, Mujahid MS, Nettleton JA, Bertoni A, Badon SE, Ning H, Allen NB. Association of neighborhood characteristics with cardiovascular health in the multi‐ethnic study of atherosclerosis. Circ Cardiovasc Qual Outcomes. 2014. Jul;7:524–531. doi: 10.1161/CIRCOUTCOMES.113.000698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Suglia SF, Sapra KJ, Koenen KC. Violence and cardiovascular health: a systematic review. Am J Prev Med. 2015;48:205–212. doi: 10.1016/j.amepre.2014.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Theall KP, Shirtcliff EA, Dismukes AR, Wallace M, Drury SS. Association between neighborhood violence and biological stress in children. JAMA Pediatr. 2017;171:53–60. doi: 10.1001/jamapediatrics.2016.2321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Billimek J, Sorkin DH. Self‐reported neighborhood safety and nonadherence to treatment regimens among patients with type 2 diabetes. J Gen Intern Med. 2012;27:292–296. doi: 10.1007/s11606-011-1882-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yu E, Lippert AM. Neighborhood crime rate, weight‐related behaviors, and obesity: a systematic review of the literature. Sociol Compass. 2016;10:187–207. doi: 10.1111/soc4.12356 [DOI] [Google Scholar]
- 15. Piro FN, Noss O, Claussen B. Physical activity among elderly people in a city population: the influence of neighbourhood level violence and self‐perceived safety. J Epidemiol Community Health. 2006;60:626–632. doi: 10.1136/jech.2005.042697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Russell SJ, Hughes K, Bellis MA. Impact of childhood experience and adult well‐being on eating preferences and behaviours. BMJ Open. 2016;6:e007770. doi: 10.1136/bmjopen-2015-007770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338:171–179. doi: 10.1056/NEJM199801153380307 [DOI] [PubMed] [Google Scholar]
- 18. South EC, Stillman K, Buckler DG, Wiebe D. Association of gun violence with emergency department visits for stress‐responsive complaints. Ann Emerg Med. 2021. May;77:469–478. doi: 10.1016/j.annemergmed.2020.10.014. Epub 2020 Dec 17. PMID: 33342597. [DOI] [PubMed] [Google Scholar]
- 19. Suglia SF, Koenen KC, Boynton‐Jarrett R, Chan PS, Clark CJ, Danese A, Faith MS, Goldstein BI, Hayman LL, Isasi CR, et al. American Heart Association Council on Epidemiology and Prevention; Council on Cardiovascular Disease in the Young; Council on Functional Genomics and Translational Biology; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research . Childhood and adolescent adversity and cardiometabolic outcomes: a scientific statement from the American Heart Association. Circulation. 2018;137:e15‐e28. doi: 10.1161/CIR.0000000000000536. Epub 2017 Dec 18. PMID: 29254928; PMCID: PMC7792566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Tung EL, Wroblewski KE, Boyd K, Makelarski JA, Peek ME, Lindau ST. Police‐recorded crime and disparities in obesity and blood pressure status in Chicago. J Am Heart Assoc. 2018. Mar 24;7:e008030. doi: 10.1161/JAHA.117.008030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Sundquist K, Theobald H, Yang M, Li X, Johansson SE, Sundquist J. Neighborhood violent crime and unemployment increase the risk of coronary heart disease: a multilevel study in an urban setting. Soc Sci Med. 2006. Apr;62:2061–71. doi: 10.1016/j.socscimed.2005.08.051. Epub 2005 Oct 3. [DOI] [PubMed] [Google Scholar]
- 22. Ahern J, Matthay EC, Goin DE, Farkas K, Rudolph KE. Acute changes in community violence and increases in hospital visits and deaths from stress‐responsive diseases. Epidemiology. 2018;29:684–691. doi: 10.1097/EDE.0000000000000879 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04 [DOI] [PubMed] [Google Scholar]
- 24. Kondo MC, Andreyeva E, South EC, MacDonald JM, Branas CC. Neighborhood interventions to reduce violence. Annu Rev Public Health. 2018. 1:253–271. doi: 10.1146/annurev-publhealth-040617-014600. Epub 2018 Jan 12. [DOI] [PubMed] [Google Scholar]
- 25. South EC, MacDonald J, Reina V. Association between structural housing repairs for low‐income homeowners and neighborhood crime. JAMA Netw Open. 2021;4:e2117067. doi: 10.1001/jamanetworkopen.2021.17067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. City of Chicago . Interactive Map of All Community Areas. https://chicago.maps.arcgis.com/apps/webappviewer/index.html?id=d56603be39824be099557dcdf9d7f7b9. Accessed April 10, 2021.
- 27. Illinois Department of Public Health, Division of Vital Records, Death Certificate Data Files . https://chicagohealthatlas.org/indicators/. Accessed May 20, 2021.
- 28. Chicago Police Department Police Data Portal . https://data.cityofchicago.org/Public‐Safety/Crimes‐2021/dwme‐t96c. Accessed May 2, 2021.
- 29. Chicago Police Department. Crime type categories: definition & description. Data Requests | Chicago Police Department. Accessed April 20, 2021.
- 30. U.S. Census Bureau . 2000 American community survey. 1‐year public use microdata samples. Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [Google Scholar]
- 31. U.S. Census Bureau . 2006‐2010 American community survey. 5‐year public use microdata samples. Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [Google Scholar]
- 32. U.S. Census Bureau . 2014‐2018 American community survey. 5‐year public use microdata samples. Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [Google Scholar]
- 33. Yonek, J. , Hasnain‐Wynia, R. A Profile of Health and Health Resources within Chicago's 77 Communities . Northwestern University Feinberg School of Medicine, Center for Healthcare Equity/Institute for Healthcare Studies, 2011.
- 34. U.S. Census Bureau . 2008‐2012. American community survey. 5‐year public use microdata samples. Retrieved from https://factfinder.census.gov/faces/nav/jsf/pages/searchresults.xhtml?refresh=t [Google Scholar]
- 35. Gunasekara FI, Richardson K, Carter K, Blakely T. Fixed effects analysis of repeated measures data.Int. J Epidemiol. 2014;43:264–269. doi: 10.1093/ije/dyt221 [DOI] [PubMed] [Google Scholar]
- 36. Hausman JA, Taylor WE. Panel data and unobservable individual effects. Econometrica. 1981;49:1377–1398. doi: 10.2307/1911406 [DOI] [Google Scholar]
- 37. Weinstein A, Feigley P, Pullen P, Mann L, Redman L. Neighborhood safety and the prevalence of physical inactivity: selected states, 1996. MMWR Morb Mortal Wkly Rep. 1999;48:143–146. [PubMed] [Google Scholar]
- 38. Wilson DK, Kliewer W, Teasley N, Plybon L, Sica DA. Violence exposure, catecholamine excretion, and blood pressure nondipping status in African American male versus female adolescents. Psychosom Med. 2002;64:906–915. [DOI] [PubMed] [Google Scholar]
- 39. Murali R, Chen E. Exposure to violence and cardiovascular and neuroendocrine measures in adolescents. Ann. Behav. Med. 2005;30:155–163. doi: 10.1207/s15324796abm3002_8 [DOI] [PubMed] [Google Scholar]
- 40. Sprung MR, Faulkner LMD, Evans MK, Zonderman AB, Waldstein SR. Neighborhood crime is differentially associated with cardiovascular risk factors as a function of race and sex. J Public Health Res. 2019;8:1643. doi: 10.4081/jphr.2019.1643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Tung EL, Chua RFM, Besser SA, Lindau ST, Kolak M, Anyanwu EC, Liao JK, Tabit CE. Association of rising violent crime with blood pressure and cardiovascular risk: longitudinal evidence from Chicago, 2014‐2016. Am J Hypertens. 2019;32:1192–1198. doi: 10.1093/ajh/hpz134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Massey D. American apartheid: segregation and the making of the underclass. Am J Sociol. 1990;96:329–357. doi: 10.1086/229532 [DOI] [Google Scholar]
- 43. Pager D, Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annu Rev Sociol. 2008;34:181–209. doi: 10.1146/annurev.soc.33.040406.131740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago: University of Chicago Press; 1987. [Google Scholar]
- 45. Jacoby SF, Dong B, Beard JH, Wiebe DJ, Morrison CN. The enduring impact of historical and structural racism on urban violence in Philadelphia. Soc Sci Med. 2018;199:87–95. doi: 10.1016/j.socscimed.2017.05.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Branas CC, Rubin D, Guo W. Vacant properties and violence in neighborhoods. ISRN Public Health. 2013;2012:246142. doi: 10.5402/2012/246142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Khatana SAM, Venkataramani AS, Nathan AS, Dayoub EJ, Eberly LA, Kazi DS, Yeh RW, Mitra N, Subramanian SV, Groeneveld PW. Association between county‐level change in economic prosperity and change in cardiovascular mortality among middle‐aged US adults. JAMA. 2021;325:445–453. doi: 10.1001/jama.2020.26141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Lacoe J, Bostic RW, Acolin A. Crime and private investment in urban neighborhoods. J Urban Econ. 2018;108:154–169. doi: 10.1016/j.jue.2018.11.001 [DOI] [Google Scholar]
- 49. Kondo MC, Keene D, Hohl BC, MacDonald JM, Branas CC. A difference‐in‐differences study of the effects of a new abandoned building remediation strategy on safety. PLoS One. 2015. Jul 8;10:e0129582. doi: 10.1371/journal.pone.0129582. Erratum in: PLoS One. 2015;10:e0136595. PMID: 26153687; PMCID: PMC4496053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Freedman M, Owens EG. Low‐income housing development and crime. J Urban Econ. 2011;70:115–131. doi: 10.1016/j.jue.2011.04.001 [DOI] [Google Scholar]
- 51. Woo A, Joh K. Beyond anecdotal evidence: do subsidized housing developments increase neighborhood crime? Appl Geogr. 2015;64:8–96. doi: 10.1016/j.apgeog.2015.09.004 [DOI] [Google Scholar]
- 52. Kondo M, Hohl B, Han S, Branas C. Effects of greening and community reuse of vacant lots on crime. Urban Stud. 2016;53:3279–3295. doi: 10.1177/0042098015608058. Epub 2015 Oct 20. PMID: 28529389; PMCID: PMC5436723 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Robinson WS. Ecological correlations and the behavior of individuals. Int J Epidemiol. 2009;38:337–41. doi: 10.1093/ije/dyn357. Epub 2009 Jan 28. Erratum in: Int J Epidemiol. 2011 Aug;40:1134. PMID: 19179346 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1


