Abstract
Background
Burnout is an occupational phenomenon caused by ineffectively managed work-related stress. Burnout is common among healthcare professionals and has the capacity to compromise patient care, but is not well characterised in pharmacists.
Aim
This systematic review aimed to establish the prevalence of burnout among pharmacists, and its associated risk factors.
Method
A systematic search of Embase, PubMed, CINAHL and PsychInfo was carried out.
Studies were included using the following eligibility criteria; original research investigating burnout prevalence in pharmacists in patient-facing roles in any jurisdiction, using any validated burnout measurement instrument. No language or date barriers were set. Data were extracted by the first author and accuracy checked by co-authors. A pooled prevalence was estimated, and narrative synthesis provided.
Results
Burnout prevalence data were extracted from 19 articles involving 11,306 pharmacist participants across eight countries. More than half (51%) of pharmacists were experiencing burnout. Associated risk factors included longer working hours, less professional experience, high patient and prescription volumes, excessive workload and poor work/life balance. The COVID-19 pandemic has negatively impacted pharmacist burnout and resilience. Involvement in education and training and access to burnout management resources were associated with lower rates of burnout, but burnout intervention effectiveness is unknown.
Conclusion
Burnout remains high among pharmacists and may negatively affect the quality of patient care. There is significant heterogeneity pertaining to the definition and assessment of burnout and there remains a need to identify and evaluate effective individual and organisational burnout interventions.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11096-022-01520-6.
Keywords: Burnout, Pharmacists, Professional wellbeing, Systematic review
Impact statements
Over half of pharmacists surveyed report experiencing professional burnout.
The Covid-19 pandemic has worsened reported burnout but these levels appear to have stabilised, albeit at high levels.
Organisation level changes to workload and work type are required to retain pharmacists and ensure continued patient safety.
Introduction
Burnout is a term used to describe the psychological response to work related stress, presenting as emotional exhaustion, increased levels of depersonalisation and cynicism and reduced feeling of personal accomplishment or efficacy [1]. The World Health Organisation’s definition describes it as an occupational phenomenon that occurs when chronic stress is ineffectively managed, although it is not considered a medical illness [2]. There has been an explosion of interest in researching burnout [3]. This has led to the development of multiple burnout assessment questionnaires, such as the Maslach Burnout Inventory (MBI) [4], the Copenhagen Burnout inventory (CBI) [5] and the Oldenburg Burnout Inventory (OBI) [6].
Burnout rates are high among healthcare professionals [3] and have been associated with reduction in productivity [7], increased job turnover [7] and reduced psychological and physical wellbeing [8]. The subsequent negative impact on patient care is significant, resulting in medication errors, reduced quality of care and fatalities [7, 9, 10]. The pharmacy profession is not as extensively studied as other professions such as medicine and teachers [3]. One previous systematic review reported a prevalence ranging from 10–61% of pharmacists, but this estimate range was based on just five studies, all from the United States, and based on pre-Covid-19 studies only [11]. This is of significance as the role of the pharmacist in healthcare provision has evolved at varying pace worldwide, in some cases catalysed by pandemic-related changes.
More evolved pharmacy systems now include use of pharmacist’s full scope of practice including prescribing [12] and vaccine administration [13]. With a growing ageing population worldwide, multimorbidity and polypharmacy is now commonplace and pharmacist-directed care and medicines management are becoming increasingly complex [12]. Pharmacists play a vital role in the safe and efficient use of medicines, continuity of supply amid regular medicines shortages, compounding of medicines and medicines information [14]. In addition, patient-facing pharmacists, especially those in a community setting, are a substantially utilised resource by the public, due to pharmacies’ convenience, accessibility and free services, resulting in high patient and prescription volumes, frequent clinical consultation and patient education. This increase in workload and responsibility, coupled with the additional pressure of a pandemic on health services may impact pharmacists’ physical and psychological wellbeing and rates of burnout [14].
Aim
This systematic review aimed to establish the prevalence of burnout among pharmacists, and its associated risk factors.
Method
This review was carried out in accordance with the PRISMA 2020 guidance [15]. A search for articles investigating burnout in pharmacists was conducted on the 27th February 2022 on EBSCO (which encompasses the databases PubMed, CINAHL and PsychInfo 1982-present), Embase (1982-present) and ERIC (2003-present). A bespoke search strategy was developed with keyword searches with MeSH terms applied in the database search of EMBASE, ERIC and EBSCO (See Supplementary Appendix 1). Results were not limited to English language to allow broad article inclusion. One existing systematic review investigating burnout in pharmacists [11] was found during the search and the articles in this review were additionally screened for inclusion. Citation tracking was also performed.
Inclusion criteria
Original studies investigating burnout in pharmacists in patient-facing roles in any jurisdiction, using any validated burnout measurement instrument were eligible for inclusion in this review. The most commonly used validated instruments include Maslach burnout Inventory, Oldenburg Burnout Inventory and Copenhagen Burnout Inventory. Details of the instruments used were extracted. Studies were excluded if they did not report burnout related outcomes or investigated other healthcare or pharmacy professionals for which pharmacist-specific data could not be extracted, or were qualitative in nature. Studies of pharmacists in non-patient facing roles were also excluded as these are typically heterogeneous roles, and results would be difficult to generalise with traditional pharmacist roles. Conference proceedings were excluded as they offer limited data, are generally not peer reviewed and may duplicate published work.
The search results were exported into Zotero® software and screened to remove duplicate articles. A title and abstract screen was performed by two authors independently, and the articles selected were reviewed at full text by two authors. Authors liaised with each other if clarity was needed on an article’s eligibility for inclusion. Data were tabulated using Excel®. Results from included studies were described in a narrative synthesis. Heterogeneity of prevalence estimates was observed between burnout assessment tools. A minority of studies also used the CBI which reported prevalence by burnout type. As a result, a pooled prevalence estimate was restricted to the MBI and SMBM. The pooled estimate and CI were calculated assuming a random effects model via the Metaprop command in STATA (Stata Statistical Software: Release 16. StataCorp LLC, College Station, TX).
Quality assessment
A quality assessment of the studies was carried out applying a modified Newcastle–Ottawa quality assessment scale (See Supplementary Appendix 2) and each was ranked as good, fair or poor quality with a maximum possible score of 8. Common risks of bias were also assessed.
Results
Study characteristics
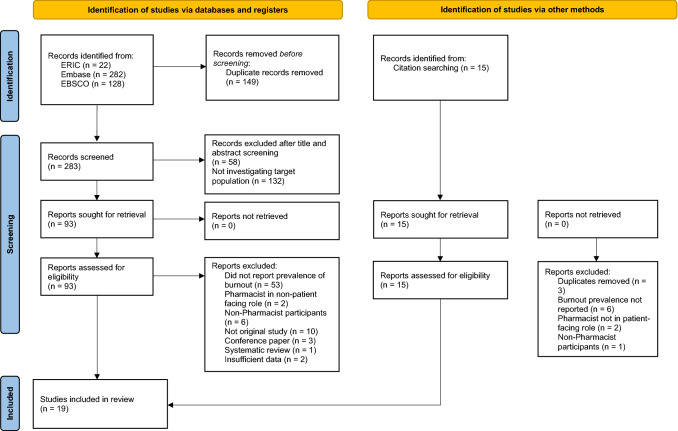
Nineteen articles [16–34] were deemed eligible for inclusion and selected for data extraction. Figure 1 details the PRISMA flow diagram. All of the studies were cross-sectional, carried out across eight different countries, the majority from the USA (n = 11/19), published from 1990 up to 2022, with a total of 11,306 pharmacist participants in patient-facing work environments. Nine studies [17–20, 23, 24, 27, 28, 34] investigated pharmacists across multiple professional settings, six studies [21, 26, 28, 31–33] measured burnout in hospital pharmacists and four studies [16, 22, 25, 29] investigated community pharmacists. The number of participants in each study ranged from 116–2231. Study characteristics are summarised in Table 1.
Fig. 1.
Preferred reporting items for systematic reviews and meta analyses (PRISMA) flow diagram
Table 1.
Characteristics of Studies included for Systematic Review
| Author | Location | Year(s) of survey | Study design | Sample Size (n =) | Professional Setting | Age (years): mean or [median] | % Female | Burnout assessment instrument | Outcome definition | Overall burnout prevalence estimate (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Alameddine et al. [16] | Lebanon | 2020–2021 | Cross-sectional | 459 | Community | NRa | 60 | CBI | CBI score > 50 | Personal burnout 56.7 work related burnout 58.2 client related burnout 57 |
| Golbach et al. [17] | USA | 2020 | Cross-sectional | 550 | Mixed | 34 | 74 | MBI-HSS | MBI-EE ≥ 27 OR MBI-DP ≥ 10 MBI-PA ≤ 33 | 61.8 |
| Santos et al. [18] | Portugal | 2020 | Cross-sectional | 1246 | Mixed | NRa | 85.5 | MBI-HSS | EE at z = M + (SD × 0.5) DP/CY at z = M + (SD × 1.25) PA at z = M + (SD × 0.10) | 7.3 |
| Jones et al. [19] | USA | 2020 | Cross-sectional | 484 | Mixed | 41.96 | 71.5 | Pro.QOL-BO, CF/STS subscales | Pro.QOL (BO + CF + STS) 23–41 = moderate (BO + CF + STS) > 42 = high | 65.3 (moderate-high score) 47 (self-reported) |
| Tan et al. [20] | Singapore | 2020 | Cross-sectional | 702 | Mixed | 33 | 73.7 | MBI-HSS | MBI-EE ≥ 27 MBI-DP ≥ 11 | 61.5 |
| Weichel et al. [21] | Canada | 2019 | Cross-sectional | 270 | Hospital | NRa | 77 | MBI-HSS (MP) | MBI-EE ≥ 27 MBI-DP ≥ 10 | 61.1 |
| Youssef et al. [22] | Lebanon | 2021 | Cross-sectional | 387 | Community | NRa | 53.7 | CBI | CBI score ≥ 50 | Personal burnout 77.8 work related burnout 76.8 client related burnout 89.7 |
| Ball et al. [23] | USA | 2018 | Cross-sectional | 193 | Mixed | 37 | 62 | MBI-HSS | MBI-EE ≥ 27 ORMBI-DP ≥ 10 ORMBI-PA ≤ 33 | 64 |
| Kang et al. [24] | USA | 2018 | Cross-sectional | 357 | Mixed | NRa | 70 | MBI-HSS (MP) | MBI-EE ≥ 27 ORMBI-DP ≥ 10 | 55.5 |
| Patel et al. [25] | USA | NR | Cross-sectional | 411 | Community | 45.3 | 70.3 | MBI-HSS | MBI-EE ≥ 27 ORMBI-DP ≥ 10 OR^MBI-PA ≤ 33 | 74.9 |
| Rozycki et al. [26] | USA | 2018–2019 | Cross-sectional | 116 | Hospital | 32.6 | 66.4 | MBI-HSS (MP) | MBI-EE ≥ 27 ORMBI-DP ≥ 10 ORMBI-PA ≤ 33 | 69.8 |
| Skrupky et al. [27] | USA | 2019 | Cross-sectional | 2231 | Mixed | NRa | 71.3 | WBI (2 questions from MBI) | High score (not specified) onMBI-EE ORMBI-DP | 59.1 |
| Smith et al. [28] | USA | 2020 | Cross-sectional | 221 | Hospital | NR | NR | MBI-HSS (MP) | MBI-EE ≥ 27 ORMBI-DP ≥ 10 | 60 |
| Protano et al. [29] | Italy | NR | Cross-sectional | 469 | Community | 42.6 | 74.2 | SMBM | SMBM ≥ 4.40 | 10.5 |
| Durham et al. [30] | USA | 2016 | Cross-sectional | 329 | Mixed | NRa | 66.9 | MBI-HSS | MBI-EE ≥ 27 ORMBI-DP ≥ 10 ORMBI-PA ≤ 33 | 53.2 |
| Jones et al. [31] | USA | 2016 | Cross-sectional | 974 | Hospital | 35 | 69.5 | MBI (NS) | MBI-EE ≥ 27 ORMBI-DP ≥ 10 | 61.2 |
| Higuchi et al. [32] | Japan | NR | Cross-sectional | 380 | Hospital | 37.3 | 60.4 | Pro.QOL-BO, CF/STS subscales | Pro.QOL-BO > 26Pro.QOL-CF/STS > 16 | 49.2 |
| Muir & Bortoletto, [33] | Australia | 2005 | Cross-sectional | 266 | Hospital | 42.6 | 73 | MBI (NS) | NR | 5 |
| Lahoz & Mason, [34] | USA | NR | Cross-sectional | 1261 | Mixed | 41.3 | 29.2 | MBI (NS) | NR | 51.9 |
BO, Burnout; CF, Compassion fatigue; CBI, Copenhagen Burnout Inventory; DP, Depersonalisation; EE, Emotional exhaustion; MBI, Maslach Burnout Inventory; MBI-HSS, MBI-Human Services Survey; MBI-HSS (MP), MBI-HSS Medical Professionals; NR, Not reported; NS, Not specified; PA, Personal accomplishment; Pro. QOL, Professional Quality of Life Scale; STS, Secondary traumatic stress; SMBM, Shirom-Melamed Burnout Measure; WBI, Wellbeing Index
aReported age ranges
Assessment of burnout
Fourteen of the studies [17, 18, 20, 21, 23, 24, 26–31, 33, 34] (73.7%) measured burnout using a version of the MBI. Two studies [16, 22] used the CBI and one study [29] used the Shirom-Melamed Burnout Measure (SMBM). The remaining two studies [19, 32] used the Professional Quality of Life Scale. The MBI and SMBM measure burnout across three similar domains; the CBI domains are personal burnout, work-related burnout and client-related burnout. The Professional Quality of Life subscales are burnout, secondary traumatic stress, compassion fatigue and compassion satisfaction [19]. The Wellbeing Index is a simple questionnaire without subscales, with higher scores indicating higher likelihood of burnout, among other measured parameters such as fatigue and anxiety [27].
Prevalence of burnout
Burnout prevalence estimates ranged from 5 to 75%. Three studies [18, 29, 33] reported burnout rates of 10% or lower, while the remainder of the studies reported estimates of 49% or higher. Pooled prevalence was calculated from 17 studies [17–21, 23–34] giving an overall prevalence estimate of 51% (95% CI 38–65%), shown in Fig. 2. The remaining two studies [16, 22] utilised the CBI and reported that 56.7% and 77.8% of community pharmacist participants had personal burnout, 58.2% and 76.8% had work-related burnout and 57% and 89.7% had client-related burnout, respectively, with neither study reporting an overall burnout prevalence estimate. Burnout prevalence estimates among hospital pharmacists ranged from 5 to 70%. Overtime, burnout prevalence has increased and stabilised at a high level since 2020, when Covid-19 was declared a pandemic, with ten studies [17–21, 23–28] in this time period reporting burnout rates of 55% or higher. High rates of burnout were consistent across studies, geographies and professional setting.
Fig. 2.
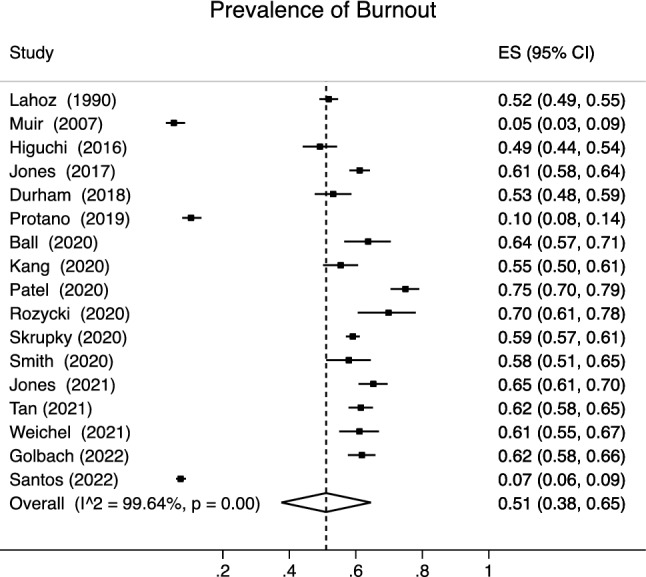
Pooled prevalence estimate of Burnout in Pharmacists. ES = estimate of prevalence (per study) with associated confidence interval and is calculated using STATA® metaprop command. The hatched line represents the pooled mean estimate to allow for comparison with individual contributing studies
Two [18, 33] of the three studies reporting the lowest rates of burnout among pharmacists had strict defining criteria by scoring high across all domains of the MBI, in comparison to all other studies using the MBI which generally classified a participant as experiencing or at risk of burnout if they scored high in one domain. The remaining study [29] with a low burnout rate used the SMBM and defined 10.5% of participants as having “clinically relevant” levels of burnout based on overall SMBM index scores across all domains, so this prevalence may be lower for the same reason.
Risk factors
Risk factors that increased the likelihood of burnout were varied, some being transient, cultural or jurisdictional, such as difficult economic circumstances [16], health care reform [31] or the impact of the COVID-19 pandemic [17, 22]. Two of the studies identified female gender as a risk factor [24, 34], however, the majority of the collective participants were female, and male pharmacists are likely to be under-represented. The most frequently mentioned risk factors are listed in Table 2. Those that were experiencing burnout were more likely to have made a medication-related error [17, 27] or were more likely to leave their current employment [16, 17, 20, 26, 27]. Factors associated with a lower rate or protective effect against burnout were involvement in patient and peer education and training [28], time away from work, social interactions and hobbies [21], having burnout management resources and being a tutor to a pharmacy student [21, 24], although having too many students was identified as a possible risk factor in one study [30]. One study reported that those who were aware of or had accessed wellness programs or burnout resources provided by their employer had lower rates of burnout [24].
Table 2.
Most common risk factors associated with Burnout
| • Working full time/longer hours worked per week [16, 19, 21, 23, 24, 28] |
| • Younger age/less professional experience [17, 21, 24, 25, 32, 33] |
| • High prescription/patient volumes [24, 25, 27, 29] |
| • Increased workload [15, 17, 18, 20] |
| • Poor work/life balance [18, 20, 19] |
| • Too many non-clinical/administrative duties [16, 26, 30] |
| • Inadequate administrative/teaching time [26, 30] |
| • Additional professional/leadership role [24, 27] |
| • Lack of burnout management resources or unaware of resources available [16, 24] |
| • Lack of appreciation by colleagues for professional contributions [20, 30] |
Quality assessment results
Results of application of the quality assessment tool are shown in Table 3. Studies that were ranked as fair or poor quality was primarily due to incomplete or unreported statistical tests, followed by low response rates. There was a high risk of selection, performance and detection bias for all studies as there was no random sampling or blinding of outcome assessors. Both response and non-response bias was also present in all studies as none can definitively deduce that those who did not respond did not have burnout symptoms, coupled with low response rates in most studies. It could be argued that those with burnout are more likely to participate in such studies and conversely, less likely to participate due to burnout itself. This possibly represents an underestimation of burnout in the literature.
Table 3.
Quality assessment of included studies using modified Newcastle–Ottawa Quality Assessment Scale
| Study | Representativeness of the Sample | Sample size | Non-respondents | Ascertainment of the exposure | Assessment of outcome | Statistical Test | Total score (max. 8) | Quality rank |
|---|---|---|---|---|---|---|---|---|
| Alameddine et al. [16] | * | * | 0 | ** | * | * | 6 | Good |
| Golbach et al. [17] | * | 0 | 0 | ** | * | * | 5 | Good |
| Santos et al. [18] | * | * | 0 | ** | * | * | 6 | Good |
| Jones et al. [19] | * | 0 | 0 | ** | * | 0 | 4 | Fair |
| Tan et al. [20] | * | * | 0 | ** | * | * | 6 | Good |
| Weichel et al. [21] | * | 0 | 0 | ** | * | * | 5 | Good |
| Youssef et al. [22] | * | * | 0 | ** | * | * | 6 | Good |
| Ball et al. [23] | * | 0 | 0 | ** | * | * | 5 | Good |
| Kang et al. [24] | * | 0 | 0 | ** | * | * | 5 | Good |
| Patel et al. [25] | * | 0 | 0 | ** | * | 0 | 4 | Fair |
| Rozycki et al. [26] | * | * | 0 | ** | * | 0 | 5 | Good |
| Skrupky et al. [27] | * | * | 0 | ** | * | * | 6 | Good |
| Smith et al. [28] | * | 0 | 0 | ** | * | * | 5 | Good |
| Protano et al. [29] | * | 0 | 0 | ** | * | * | 5 | Good |
| Durham et al. [30] | * | 0 | 0 | ** | * | 0 | 4 | Fair |
| Jones et al. [19] | * | 0 | 0 | ** | * | * | 5 | Good |
| Higuchi et al. [32] | * | * | 0 | ** | * | * | 6 | Good |
| Muir & Bortoletto, [33] | * | 0 | 0 | ** | * | 0 | 4 | Fair |
| Lahoz & Mason, [34] | * | 0 | 0 | ** | * | 0 | 4 | Fair |
0 No point awarded, *1 point awarded, **2 points awarded
Discussion
Statement of key findings
More than half of pharmacists surveyed were defined as experiencing burnout, with prevalence estimates ranging from 5 to 75%, and in the last three years this has increased and plateaued at almost 60%. While prevalence estimates are limited by assessment instrument and study design challenges, these results give a picture of a significant workforce wellbeing problem within the pharmacy profession. With more than half of pooled respondents reporting feelings of burnout across published studies, organisational factors, occupational stressors and personal resilience must all be examined. Most of the risk factors associated with burnout were modifiable and workload related. Burnout was also associated with higher risk of dispensing errors and leaving the pharmacy profession [16, 17, 20, 26, 27], which could significantly impact current and future quality of patient care. The COVID-19 pandemic was also identified in some studies as a contributing factor to developing burnout [16–19, 22]. There was a significant heterogeneity in the data. Varying levels of burnout could be due to practice setting differences, as well as jurisdictional differences in professional roles. Differences in burnout prevalence also reflect individual factors, such as participants’ perception of burnout and subjective experiences. Jones [31] reported a burnout prevalence based on Pro.QOL scores of 65.3%, yet participants’ self-reported burnout was 47%. These findings suggest a lack of awareness of what burnout is, but could also reflect a work culture where stress is considered a normal part of professional life. Both could possibly contribute to burnout over time, whereby pharmacists continue to work in stressful environments without protest.
Strengths and weaknesses
To the investigators’ knowledge, this is the second systematic review examining burnout in pharmacists. However, this review is an up to date insight into pharmacist burnout as the previous review [11] was undertaken before the COVID-19 pandemic. There are several limitations to this systematic review. Only observational studies were included, which are at high risk of bias and do not identify causation. The data presented stems from only eight countries, a disproportionate amount representing the USA (n = 11/19 studies). There is also a disproportionate amount of studies published in the last three years (13/19 studies) making it difficult to assess prevalence over time.
Interpretation
The primary reason for variance in prevalence among the studies reviewed is inconsistency in both the definition and measurement of burnout. The three studies [18, 29, 33] with the lowest prevalence estimates defined burnout as scoring high across all subscales of the burnout assessment tools used. The authors of the MBI no longer recommend using previously published cut-off scores, which were removed in 2016 from the most recent edition of the MBI manual [35] as they lack validity and now recommend using burnout profiles to establish burnout patterns. The benefits of burnout profiles are that they acknowledge the varied and subjective nature of burnout among individuals, giving a more holistic view. However, only one study [18] utilised this approach. It found that the most affected domain of the MBI was personal accomplishment at 50.1%, which is inconsistent with the rest of the studies using the traditional cut-off score method, which most found this domain being the least affected, with several studies excluding it completely. In a recent systematic review investigating the validity of five different burnout measures [36], the CBI and OBI had the most robust validity and reliability for measuring burnout. However, all of these questionnaires have their own strengths and limitations and the development of a diagnostic standard is needed [36].
The impact of burnout
The most concerning consequence of burnout is that those experiencing burnout are more likely to leave the profession completely [3, 8]. This has a subsequent negative impact in multiple ways; on healthcare teams, as pharmacists leave taking valuable skills and experience with them and on patients, potentially compromising quality of care and influencing the frequency of medication errors [17, 37]. This is possibly cyclical, as it could also be argued that quality of care provided by those with burnout is compromised, potentially causing errors. Staff shortages and lack of resources are a frequent concern and increased staff turnover can also potentially impact patient care. Burnout can negatively affect mental health and wellbeing and is associated with conditions such as depression and anxiety [1, 37]. There is a financial impact to burnout as there are costs involved in absence, staff turnover, recruitment and potentially individual costs, such as loss of income due to absence or treatment of associated co-morbidities. Chronic heavy workload and poor organisational structure and work culture are often cited as important drivers of burnout [8, 37, 38] and in order to reduce the impact of burnout, these factors need to be addressed by pharmacy owners and policymakers to retain pharmacists and foster a work environment conducive to pharmacists’ wellbeing.
Impact of COVID-19 pandemic
Several studies were published during the COVID-19 pandemic and cited concerns of pharmacists that included lack of confidence providing care to those with COVID-19, become infected or passing infection to family members [18, 22]. It was reported that the pandemic had increased pharmacist workload [16], increased work hours or that self-reported burnout was specifically related to or impacted by the pandemic [17, 19]. Overall, the perceived threat of COVID-19 was associated with higher levels of burnout. Conversely, accepting COVID-19 risks altruistically and education and training on COVID-19 were associated with lower levels of burnout [18, 22]. Pharmacists are often the first point of contact for patients and the pandemic has impacted issues such as personal protective equipment provision, medication shortages, increased patient volumes and providing the public with evidence-based COVID-related information, all contributing further to workload burden and negatively affecting pharmacists’ mental health and wellbeing [14, 39]. This impact introduces the concept of “syndemics” [40], whereby the epidemic of burnout and its existing stressors has been exacerbated by the pandemic, creating additional workload and new stressors, such as vaccine rollout, virtual consultations and medication delivery services amidst regular staff shortages [41], reflecting the need to provide additional support to healthcare professionals in public health emergencies [42]. One study found that personal resiliency requires workplace support, but changes like improved scheduling and mandatory breaks, confidence using technology, specialised staff and task focused environments were positively associated with resiliency and pharmacists’ ability to adapt to novel situations [43].
Further research
Burnout is high among pharmacists and strategies to overcome and manage burnout are essential. The nature of the pharmacist role has a large amount of responsibility and heavy workload reflected in the risk factors listed in Table 2. Lack of resources is a consistent issue, whether it be understaffing, contributing to higher workload and increased working hours, or administrative work and additional roles draining pharmacist resources, or a lack of burnout management resources. It may be prudent for healthcare organisations to examine their organisational structure and how this contributes to burnout among employees and implement changes to address shortcomings. Newly qualified pharmacists need to be protected by additional systems-level support to retain them in the profession, as younger age and less professional experience are risk factors themselves. Therefore, the concept of resilience and managing potential burnout needs to start during pharmacy education, but this is not commonplace. Weichel [21] investigated burnout education in pharmacy schools in Canada and found that 90% of them did not have burnout prevention addressed in their curricula. Of the studies that considered the availability of burnout management resources [17, 23–25, 30], a large proportion of participants claimed they had either no access to or were unaware of any burnout support provided. It would appear that healthcare organisations that have support in place need to create awareness of their availability and encourage pharmacists in distress to utilise such supports.
Another issue is identifying the most effective burnout interventions. There have been several systematic reviews investigating intervetnions in physicians [44–46] with mixed results. Most of the published research is individual focused, with mindfulness techniques, cognitive behavioural therapy and self-care causing short term or small reductions in burnout [44, 45]. Organisational changes, such as reductions in workload, changes to working hours and improved organisation communication may have more meaningful reductions in burnout, or may boost the effect of individual interventions [46, 47], but much of the existing evidence base is of low quality, lacks long term follow up and there is a dearth of investigation in pharmacists. Pharmacy leadership bodies have online resources for managing resilience and wellbeing but their effectiveness and how often they are utilised by pharmacists is understudied.
Conclusion
Approximately half of pharmacists are experiencing burnout globally which has the potential to negatively impact patient care. There is a clear increase in the amount of research investigating burnout among pharmacists in the last five years. There is a need for longitudinal studies to account for any transient contributors, like COVID-19. Burnout awareness and management techniques should be addressed within healthcare organisations should provide wellness programmes and support to those at risk of and/or experiencing symptoms of burnout, as well as continuously evaluate their effectiveness and how its organisational structure and work culture affects burnout.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
No specific funding was received.
Conflicts of interest
The authors have no conflicts of interest to declare.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Bianchi R, Schonfeld IS, Laurent E. Is it time to consider the “burnout syndrome” a distinct illness? Front Public Health. 2015;8(3):158. doi: 10.3389/fpubh.2015.00158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. ICD-11 for mortality and morbidity statistics (2018). Available from: https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/129180281 Accessed 01 Nov 2022.
- 3.Haase KK. Addressing burnout in clinical pharmacy: What can we learn from other health care disciplines? Pharmacother. 2020;3(3):645–654. [Google Scholar]
- 4.Maslach C, Schaufeli W. Historical and conceptual development of burnout. Professional burnout: Recent developments in theory and research. USA; 1993 p. 1–6. Report No.: 12.
- 5.Kristensen TS, Borritz M, Villadsen E, et al. The copenhagen burnout inventory: a new tool for the assessment of burnout. Work Stress. 2005;19:192–207. doi: 10.1080/02678370500297720. [DOI] [Google Scholar]
- 6.Halbesleben JR, Demerouti E. The construct validity of an alternative measure of burnout: Investigating the english translation of the oldenburg burnout inventory. Work Stress. 2005;19(3):208–220. doi: 10.1080/02678370500340728. [DOI] [Google Scholar]
- 7.Hagemann TM, Reed BN, Bradley BA, et al. Burnout among clinical pharmacists: Causes, interventions, and a call to action. Pharmacother. 2020;3(4):832–842. [Google Scholar]
- 8.Royal Pharmaceutical Society, Workforce Wellbeing. Available from: https://www.rpharms.com/recognition/all-our-campaigns/workforce-wellbeing Accessed 01 Nov 2022.
- 9.Shanafelt TD, Balch CM, Bechamps G, et al. burnout and medical errors among american surgeons. Ann Surg. 2010;251:995–1000. doi: 10.1097/SLA.0b013e3181bfdab3. [DOI] [PubMed] [Google Scholar]
- 10.Hall LH, Johnson J, Watt I, et al. healthcare staff wellbeing, burnout, and patient safety: a systematic review. PLoS ONE. 2016;11(7):e0159015. doi: 10.1371/journal.pone.0159015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.McQuade BM, Reed BN, DiDomenico RJ, et al. Feeling the burn? A systematic review of burnout in pharmacists. Pharmacother. 2020;3(3):663–675. [Google Scholar]
- 12.Bourne RS, Baqir W, Onatade R. Pharmacist independent prescribing in secondary care: opportunities and challenges. Int J Clin Pharm. 2016;38(1):1–6. doi: 10.1007/s11096-015-0226-9. [DOI] [PubMed] [Google Scholar]
- 13.Poudel A, Lau ETL, Deldot M, et al. Pharmacist role in vaccination: Evidence and challenges. Vaccine. 2019;37:5939–5945. doi: 10.1016/j.vaccine.2019.08.060. [DOI] [PubMed] [Google Scholar]
- 14.Hayden JC, Parkin R. The challenges of COVID-19 for community pharmacists and opportunities for the future. Ir J Psychol Med. 2020;37(3):198–203. doi: 10.1017/ipm.2020.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;29(372):n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alameddine M, Bou-Karroum K, Hijazi MA. A national study on the resilience of community pharmacists in Lebanon: a cross-sectional survey. J Pharm Policy Pract. 2022;15(1):1. doi: 10.1186/s40545-022-00406-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Golbach AP, McCullough KB, Soefje SA et al. Evaluation of burnout in a national sample of hematology-oncology pharmacists. JCO Oncol Pract. 2021;OP2100471 [DOI] [PubMed]
- 18.Santos PMD, Silva CRD, Costa D et al. Burnout in the pharmaceutical activity: the impact of COVID-19. Front Psychiatry. 2022:2389. [DOI] [PMC free article] [PubMed]
- 19.Jones AM, Clark JS, Mohammad RA. Burnout and secondary traumatic stress in health-system pharmacists during the COVID-19 pandemic. Am J Health Syst Pharm. 2021;78(9):818–824. doi: 10.1093/ajhp/zxab051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tan YZ, Chong JJ, Chew LST, et al. Burnout and resilience among pharmacists: A Singapore study. Pharmacother. 2022;5(1):75–84. doi: 10.1016/j.japh.2021.09.013. [DOI] [PubMed] [Google Scholar]
- 21.Weichel C, Lee JS, Lee JY. Burnout among hospital pharmacists: prevalence, self-awareness, and preventive programs in pharmacy school curricula. Can J Hosp Pharm. 2021;74(4):309–316. doi: 10.4212/cjhp.v74i4.3192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Youssef D, Youssef J, Hassan H, et al. Prevalence and risk factors of burnout among Lebanese community pharmacists in the era of COVID-19 pandemic: results from the first national cross-sectional survey. J Pharm Policy Pract. 2021;14:1–12. doi: 10.1186/s40545-021-00393-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ball AM, Schultheis J, Lee HJ, et al. Evidence of burnout in critical care pharmacists. Am J Health Syst Pharm. 2020;77:790–796. doi: 10.1093/ajhp/zxaa043. [DOI] [PubMed] [Google Scholar]
- 24.Kang K, Absher R, Granko RP. Evaluation of burnout among hospital and health-system pharmacists in North Carolina. Am J Health Syst Pharm. 2020;77:441–448. doi: 10.1093/ajhp/zxz339. [DOI] [PubMed] [Google Scholar]
- 25.Patel SK, Kelm MJ, Bush PW, et al. Prevalence and risk factors of burnout in community pharmacists. J Am Pharm Assoc. 2021;61:145–150. doi: 10.1016/j.japh.2020.09.022. [DOI] [PubMed] [Google Scholar]
- 26.Rozycki E, Bilhimer M, Bridgeman P, et al. Evaluation of burnout among emergency medicine pharmacists. Pharmacother. 2020;3(8):1423–1433. [Google Scholar]
- 27.Skrupky LP, West CP, Shanafelt T, et al. Ability of the Well-Being Index to identify pharmacists in distress. J Am Pharm Assoc. 2020;60:906–914.e2. doi: 10.1016/j.japh.2020.06.015. [DOI] [PubMed] [Google Scholar]
- 28.Smith SE, Slaughter AA, Butler SA, et al. Examination of critical care pharmacist work activities and burnout. Pharmacother. 2021;4(5):554–569. [Google Scholar]
- 29.Protano C, De Sio S, Cammalleri V, et al. A Cross-Sectional Study on Prevalence and Predictors of Burnout among a Sample of Pharmacists Employed in Pharmacies in Central Italy. Biomed Res Int. 2019;24(2019):8590430. doi: 10.1155/2019/8590430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Durham ME, Bush PW, Ball AM. Evidence of burnout in health-system pharmacists. Am J Health Syst Pharm. 2018;75:S93–100. doi: 10.2146/ajhp170818. [DOI] [PubMed] [Google Scholar]
- 31.Jones GM, Roe NA, Louden L, et al. Factors associated with burnout among US hospital clinical pharmacy practitioners: results of a nationwide pilot survey. Hosp Pharm. 2017;52:742–751. doi: 10.1177/0018578717732339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Higuchi Y, Inagaki M, Koyama T, et al. A cross-sectional study of psychological distress, burnout, and the associated risk factors in hospital pharmacists in Japan. BMC Public Health. 2016;8(16):534. doi: 10.1186/s12889-016-3208-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Muir PR, Bortoletto DA. Burnout among Australian hospital pharmacists. J Pharm Pract Res. 2007;37(3):187–189. doi: 10.1002/j.2055-2335.2007.tb00740.x. [DOI] [Google Scholar]
- 34.Lahoz MR, Mason HL. Burnout among pharmacists. Am Pharm. 1990; NS30(8):28–32 [DOI] [PubMed]
- 35.Maslach Burnout Toolkit for Medical Personnel - Mind Garden [Internet]. [cited 2022 Jun 19]. Available from: https://www.mindgarden.com/329-maslach-burnout-toolkit-for-medical-personnel#horizontalTab3 Accessed 01 Nov 2022.
- 36.Shoman Y, Marca SC, Bianchi R, et al. Psychometric properties of burnout measures: a systematic review. Epidemiol Psychiatr Sci. 2021;30:e8. doi: 10.1017/S2045796020001134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.House of Commons 2021 Workforce burnout and resilience in the NHS and social care. Available at: https://committees.parliament.uk/work/494/workforce-burnout-and-resilience-in-the-nhs-and-social-care/ Accessed 01 Nov 2022.
- 38.Chui MA, Look KA, Mott DA. The association of subjective workload dimensions on quality of care and pharmacist quality of work life. Res Social Adm Pharm. 2014;10(2):328–340. doi: 10.1016/j.sapharm.2013.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Elbeddini A, Wen CX, Tayefehchamani Y et al. Mental health issues impacting pharmacists during COVID-19. J Pharm Policy Pract [Internet]. 2020;13(1). [DOI] [PMC free article] [PubMed]
- 40.Lemke MK, Apostolopoulos Y, Sönmez S. Syndemic frameworks to understand the effects of COVID-19 on commercial driver stress, health, and safety. J Transp Health. 2020;1(18):100877. doi: 10.1016/j.jth.2020.100877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Connelly D. Work-related stress: the hidden pandemic in pharmacy [Internet]. The Pharmaceutical Journal. Available from: https://pharmaceutical-journal.com/article/feature/work-related-stress-the-hidden-pandemic-in-pharmacy Accessed 01 Nov 2022.
- 42.Missouridou E, Mangoulia P, Pavlou V et al. Wounded healers during the COVID-19 syndemic: compassion fatigue and compassion satisfaction among nursing care providers in Greece. Perspect Psychiatr Care. 2021. 10.1111/ppc.12946 [DOI] [PMC free article] [PubMed]
- 43.Austin Z, Gregory P. Resilience in the time of pandemic: the experience of community pharmacists during COVID-19. Res Social Adm Pharm. 2021;17(1):1867–1875. doi: 10.1016/j.sapharm.2020.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Murray M, Murray L, Donnelly M. Systematic review of interventions to improve the psychological well-being of general practitioners. BMC Prim Care. 2016;17(1):36. doi: 10.1186/s12875-016-0431-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Regehr C, Glancy D, Pitts A, et al. Interventions to reduce the consequences of stress in physicians: a review and meta-analysis. J Nerv Ment Dis. 2014;202:353–359. doi: 10.1097/NMD.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 46.West CP, Dyrbye LN, Erwin PJ, et al. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet. 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 47.Panagioti M, Panagopoulou E, Bower P, et al. Controlled Interventions to Reduce Burnout in Physicians: A Systematic Review and Meta-analysis. JAMA Intern Med. 2017;177:195–205. doi: 10.1001/jamainternmed.2016.7674. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.