Abstract
Aims
Depression and anxiety have a detrimental effect on the health outcomes of patients with heart disease. Digital health interventions (DHIs) could offer a solution to treat depression and anxiety in patients with heart disease, but evidence of its efficacy remains scarce. This review summarizes the latest data about the impact of DHIs on depression/anxiety in patients with cardiac disease.
Methods and results
Articles from 2000 to 2021 in English were searched through electronic databases (PubMed, Cochrane Library, and Embase). Articles were included if they incorporated a randomized controlled trial design for patients with cardiac disease and used DHIs in which depression or anxiety was set as outcomes. A systematic review and meta-analysis were performed. A total of 1675 articles were included and the screening identified a total of 17 articles. Results indicated that telemonitoring systems have a beneficial effect on depression [standardized mean difference for depression questionnaire score −0.78 (P = 0.07), −0.55 (P < 0.001), for with and without involving a psychological intervention, respectively]. Results on PC or cell phone–based psychosocial education and training have also a beneficial influence on depression [standardized mean difference for depression questionnaire score −0.49 (P = 0.009)].
Conclusion
Telemonitoring systems for heart failure and PC/cell phone–based psychosocial education and training for patients with heart failure or coronary heart disease had a beneficial effect especially on depression. Regarding telemonitoring for heart failure, this effect was reached even without incorporating a specific psychological intervention. These results illustrate the future potential of DHIs for mental health in cardiology.
Keywords: Depression, Anxiety, Digital cardiology, Preventive cardiology, Telemonitoring, Virtual reality, Cardiac disease
Graphical Abstract
Graphical Abstract.
Introduction
Accumulating evidence on the relations between mental health and health outcomes in cardiac disease has put mental health on the agenda in cardiac care. Several review articles describe each type of heart disease and mental health. The European Society of Cardiology (ESC) working group on coronary pathophysiology and microcirculation stated a bidirectional relationship between depression and coronary heart disease (CHD).1 A previous article has demonstrated that depression and anxiety disorders in patients with heart failure (HF) are associated with adverse outcomes.2 Additionally, another review described depression and/or anxiety for implantable cardioverter defibrillator (ICD) recipients with HF.3 Although mental health in several types of heart disease draws attention recently, cardiologists, who deal with all aspects of heart disease in the daily practice, may think the priority of mental health is low.
Relaxation techniques, cognitive challenge or behavioural change intervention, are used as treatment components to support mental health in the treatment of heart disease.4 In addition, previous reports on cognitive behavioural therapy (CBT) in cardiac patients have shown that structured telephone support is effective.5 Collaborative care is one of the recent topics in this field. This intervention, established in the primary care field,6 is characterized in part by a multidisciplinary approach to mental health (e.g. collaboration between nurses and healthcare professionals for psychosocial care). However, a recent review reported that patients who received face-to-face interventions experienced a significant improvement regarding psychosocial factors compared with telephone-only interventions.7
Nowadays, the setup and implementation for digital health interventions (DHIs) have been accelerated in cardiology field.8 Digital health interventions have a multifaceted impact on healthcare,9 and various ways of using DHIs, such as a smartphone, PC- or mobile-based, and virtual reality (VR), intervene in depression and/or anxiety. It has the potential to overcome traditional barriers to telemonitoring, in terms of real-time monitoring of lifelog data, virtual face-to-face intervention, and group communication. Although DHIs have already shown promising results10–12 and have such a large potential, the evidence for the efficacy of DHIs for depression and/or anxiety in patients with entire cardiac disease is not fully clear.
Therefore, we hypothesized that DHIs, through its multidisciplinary function, would have a positive impact on the mental status of patients with cardiac disease. To achieve this objective, a systematic review of the most recent available data on the efficacy of DHIs in improving depression and/or anxiety in patients with cardiac disease was compiled.
Methods
Data sources and search
The search was conducted in adherence to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) reporting guideline.13 PubMed, Cochrane Library, and Embase databases were searched for studies published between 2000 and March 2021. The search was performed iteratively for synonyms of ‘cardiac disease’, ‘DHIs’, and ‘depression or anxiety’ by controlled vocabulary (such as MeSH or Emtree) and free text words (see Supplementary material online 1). Only randomized controlled trials (RCTs) with an adult study population were included. The reference lists and referred articles of the identified relevant papers were cross-checked for additional references.
Study selection
This review included full-length research papers published in peer-reviewed journals. The efficacy of DHIs on depression and anxiety is defined as improvement in psychological questionnaire scores. Inclusion criteria for studies were as follows: (i) RCTs written in English; (ii) patients were diagnosed with cardiac disease (patients with only vascular disease were excluded); (iii) comparing the group using DHIs, which was defined as healthcare improvement through digital health technologies that take advantage of recent information and communication technologies, such as mobile health, wearable devices, Internet of Things, and VR, which does not include only telephone, universal serial bus, compact disk, nor existing ICD/cardiac resynchronization therapy telemonitoring systems, with the group not using DHIs; and (iv) having depression and/or anxiety as outcome compared the questionnaire scores before and after the intervention. Two investigators (T.K. and M.S.) checked all identified articles on their titles and abstracts. If eligibility was doubtful, articles were read in full. A third investigator (V.I.G.) resolved differences in decision-making. The selection procedure was conducted according to the PRISMA guidelines.13
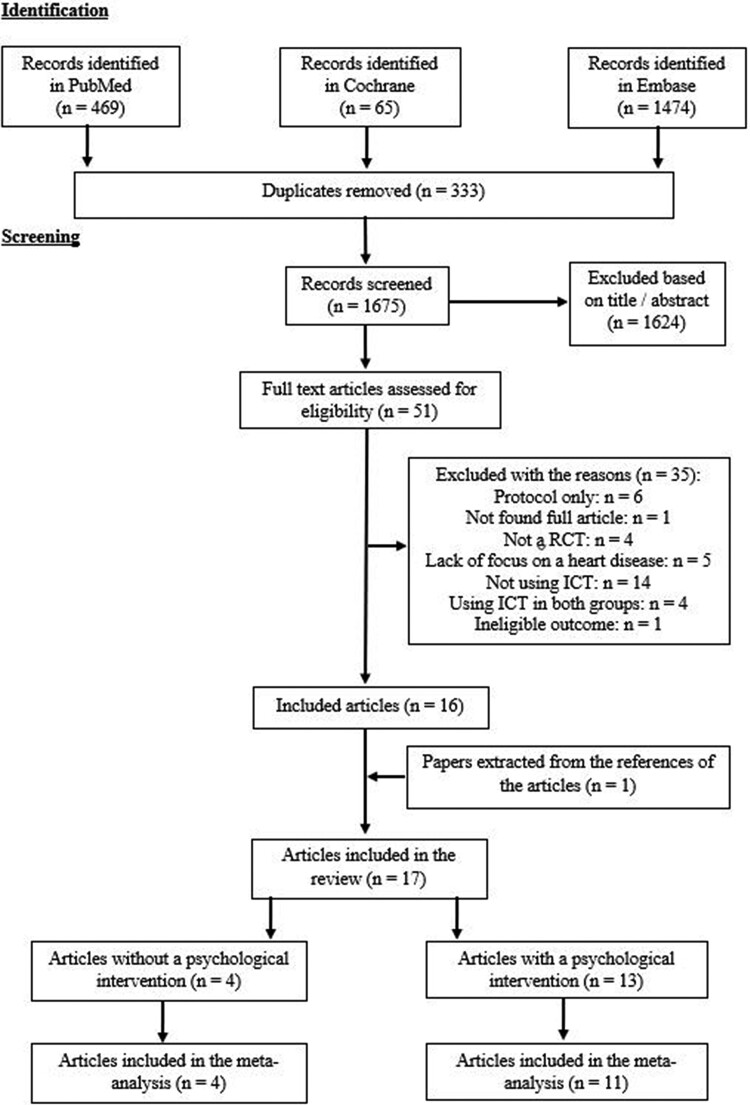
Data extraction
For each selected RCT, the first physician (T.K.) completed the data extraction. It included authors, year of publication, country of trial, patients’ diagnosis, number of patients including their characteristics, their achievement rate of an RCT, and details of drop out. Moreover, the kind of digital health, study periods, and the type of the intervention were extracted. The way of measuring depression and/or anxiety was also described. The corresponding authors of selected papers were contacted for completion of missing information. Five authors gave additional information. The selection process is shown in Figure 1.
Figure 1.
Preferred reporting items for systematic reviews and meta-analyses: diagram of the study selection strategy.
Study quality
Two investigators (T.K. and M.S.) separately assessed the risk of bias of the included articles according to the Cochrane Handbook for Systematic Reviews of Interventions,14 and a third investigator (V.I.G.) compared the results. Each parameter is scored as high, low, or unclear risk of bias. Studies were considered to be at high risk of bias if random sequence generation or allocation concealment showed a high risk. Quality assessment was performed using the RevMan 5.4 statistical software package (The Cochrane Collaboration, Oxford, UK).
Data synthesis
RevMan 5.4 was used to carry out a meta-analysis. Standardized mean differences were calculated for depression and anxiety questionnaire scores with 95% confidence interval (CI) as effect sizes and were compared between pre- and post-changes for two comparative groups (with vs. without DHI). Random effects modelling was carried out because of the variability of duration, delivery, and assessment across studies. Heterogeneity was evaluated by Q statistics with I2 > 75% being consistent with a high level of heterogeneity.15 All tests were performed at a 5% significance level. For questionnaire scores, mean changes and standard deviations (SDs) from baseline were used if available. For the studies which did not report the SD of the change in the outcomes, values were inputted by a validated strategy.16 These values were determined by specific pre- and post-intervention SD with the formula: and a conservative estimation of within-patient correlation (R) = 0.7 was assumed followed by Rosenthal’s recommendation.17 If SD was not described in studies,18 the mean SD of all remaining ones was used.19 Because selected articles included two types, which are DHIs with and without psychological intervention, they were divided into two groups and the effects of interventions on patients’ psychological factors were separately summarized. Funnel plots were used to detect publication biases.
Results
Effects of digital health without psychological intervention on depression/anxiety
Study characteristics
As shown in Figure 1 and Table 1, four full-text articles20–23 out of 17 included studies of DHIs that were not targeted at psychological aspects. All of them were suitable for meta-analysis. A total of 817 patients were entered in the four RCTs. All four studies were from Europe (Germany,20 Poland,22 Portugal,21 and Italy23). The average age range was 57–67 years, with a male predominance. Two of the four studies involved patients with HF and two involved patients with CHD, and gender differences in these diseases are reflected in male predominance. Although male participation rate was 100% for one study,23 exclusion criteria did not imply gender. Two studies20,22 reported the significant age difference between the intervention and control groups, which was a reason for lower quality and was noted below. Regarding other parameters, one study showed20 higher prevalence of New York Heart Association (NYHA) Class 3 (74.7 vs. 55.8%, P = 0.013) and higher serum creatinine levels (117.0 ± 47.3 vs. 103.0 ± 34.6 μmol/L, P = 0.037) in the intervention group. The details of patient parameters are shown in Table 1.
Table 1.
Study and participant characteristics
| Articles (year), country | Patients’ diagnosis | No. of randomized patients (IG/CG) | Male (%) | Mean age (years) | Patients who complete the study (%) |
|---|---|---|---|---|---|
| 1. Articles of digital health WITHOUT a psychological intervention | |||||
| Koehler et al. (2021), Germany | HF with low EF (NYHA 2 or 3) | 674 (339/335) | 81.3 | 67 | 60.1 (405/674) |
| Vieira et al. (2018), Portugal | CHD | 46 (15/15/16)a | unknown | 58 | 71.7 (33/46) |
| Smolis-Bąk et al. (2015), Poland | HF with low EF (NYHA 3), planned CRTD implantation, and metabolic disorders | 52 (26/26) | 90.4 | 63 | 88.5 (46/52) |
| Giallauria et al. (2006), Italy | Recent MI (<8 days) | 45 (15/15/15)b | 100 | 57 | 95.6 (43/45) |
| 2. Articles of digital health WITH a psychological intervention | |||||
| Schulz et al. (2020), Germany | ICD implantation with mildly increased psychosocial distress | 118 (59/59) | 78 | 59 | 83.9 (99/118) |
| Hessabi et al. (2020), Iran | Admission to CCU | 60 (30/30) | 50 | 51 | Unknown |
| Maciołek et al. (2020), Poland | CHD or HF | 65 (32/33) | 67.7 | 60 | 93.8 (61/65) |
| Islam et al. (2019), Australia | CHD | 710 (352/358) | 82.1 | 58 | 96.2 (683/710) |
| Norlund et al. (2018), Sweden | Recent MI (< 3 months) with symptoms of depression or anxiety | 239 (117/122) | 66.5 | 60 | 88.3 (211/239) |
| Kalter-Leibovici et al. (2017), Israel | HF (NYHA 2 to 4) | 1360 (682/678) | 72.5 | 71 | 61.8 (840/1360) |
| Habibović et al. (2017), The Netherlands | ICD implantation | 289 (146/143) | 81.3 | 59 | 75.1 (217/289) |
| Piotrowicz et al. (2016), Poland | HF with low EF (NYHA 2 or 3) | 111 (77/34) | 88.4 | 56 | 62.1 (69/111) |
| Bekelman et al. (2015), USA | HF | 392 (193/199) | 96.6 | 68 | 98.0 (384/392) |
| Dale et al. (2015), New Zealand | CHD | 123 (61/62) | 81.3 | 59 | 94.3 (116/123) |
| Villani et al. (2014), Italy | HF with low EF (NYHA 3 or 4) | 80 (40/40) | 72.8 | 72 | 81.3 (65/80) |
| Davidson et al. (2013), USA | ACS with persistent depressive symptoms | 150 (73/77) | 58 | 60 | 92.0 (138/150) |
| Ramaekers et al. (2009), The Netherlands | HF | 101 (56/45) | 61.4 | 72 | Unknown |
IG, intervention group; CG, control group; HF, heart failure; EF, ejection fraction; NYHA, New York Heart Association; CHD, coronary heart disease; CRTD, cardiac resynchronization therapy defibrillator; MI, myocardial infarction; ICD, implantable cardioverter defibrillator; CCU, cardiac care unit; ACS, acute coronary syndrome.
IG was divided into Kinect intervention (n = 15) and a paper booklet intervention (n = 15).
IG was divided into cardiac rehabilitation intervention with tele ECG (n = 15) and without tele ECG (n = 15).
Types of digital health and characteristics of intervention
Included studies did not use DHI for the purpose of reducing depression and/or anxiety. The type of DHIs was divided into ‘telemonitoring’20,22,23 and ‘VR’21 (see Supplementary material online 2). A telemonitoring system was used for data capturing of parameters such as blood pressure (BP), body weight (BW), electrocardiogram (ECG), etc.20,22,23 One study included a VR intervention that was performed in patients with CHD.21
Reasons for drop out
The study periods ranged from 2 to 24 months. The mean completion rates among the included trials were 64.5% (range 60.1–95.6%). This rate was >30% in the study of telemonitoring for patients with HF (NYHA Class 2 or 3).20 Common causes for drop out included personal or family reasons21 and medical reasons.20–22 One article did not report precise reasons for drop out.23
Study quality
The risk of bias was assessed in each study. Almost all the studies demonstrated a low risk of bias for attrition bias, reporting bias, and selection bias. Several studies20,22 showed differences in age between the intervention and control group in baseline patient characteristics. Although there were no significant differences regarding other parameters including psychological measures, age is related to digital literacy in general. Considering this point and incompleteness of some information, one study (25%) had a low risk of bias and the risk of others (75%) showed unknown for selection bias. Blinding of participants and personnel was not possible due to the nature of the intervention. Blinding of outcome assessment was not demonstrated in most studies. Overall, all six studies were thought to be of high quality (see Supplementary material online 3). Funnel plots of the depression outcomes were shown in Supplementary material online 4. Since the funnel plots were nearly symmetrical, no evidence of strong publication bias was found.
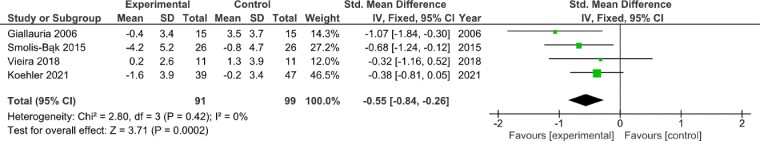
Outcome (depression)
All four studies reported depression outcomes. Most of studies about telemonitoring for HF reported a positive result. Figure 2 shows the results of the meta-analysis and forest plot between the two groups. Depression questionnaire scores were significantly lower (better) in the intervention group than in the control group (standardized mean difference −0.55; 95% CI −0.84 to −0.26; P < 0.001), with low heterogeneity (I2 = 0%, P = 0.42). Supplementary material online 5 showed the subgroup analysis focusing on telemonitoring as DHI type. The intervention group reported a significant lower (better) depression questionnaire scores on telemonitoring compared with the control group (standardized mean difference −0.61; 95% CI −0.96 to −0.25; P < 0.001) with low heterogeneity found (I2 = 19%, P = 0.29).
Figure 2.
Effect of digital health intervention without psychological intervention on depression outcomes.
Outcome (anxiety)
Two studies described anxiety outcomes. Meta-analysis showed no significant effect of DHI on anxiety (standardized mean difference −0.00; 95% CI −0.55 to 0.54; P = 1.00; see Supplementary material online 6) with low heterogeneity found (I2 = 0%, P = 0.59).
Effects of digital health with psychological intervention on depression/anxiety
Study characteristics
As demonstrated in Figure 1 and Table 1, out of the total of 17 included articles, 13 pertained to DHIs with a psychological focus.18,24–35 Because no mean differences for outcomes were stated, the two studies27,31 were excluded from the meta-analysis. A total of 3798 patients participated in 13 RCTs. Seven studies were from Europe (Germany,24 Poland,26,34 Sweden,28 The Netherland,30,33 and Italy35), two were from USA18,31, two were from Asia (Iran25 and Israel29), and two were from Oceania (Australia27 and New Zealand32). The average age range was 51–72 years, with a male predominance. Especially, in 8 of the 13 studies, the male participation rate exceeded 70%. These studies were conducted in patients with HF,29,31,34,35 CHD,27,32 and ICD implantation.24,30 Gender differences in these diseases are reflected in male predominance. Two studies29,34 reported the significant age difference between the intervention and control groups, which was a reason for lower quality and was described below. In terms of other factors, one study24 reported higher rates of coronary revascularization (58 vs. 17%, P = 0.01) and amiodarone prescription (5.2 vs. 19%, P = 0.05) in the intervention group. Another study29 showed higher rates of NYHA Class 4 (7.5 vs. 4.3%, P = 0.005) and shorter distance of 6-min walking test (165 vs. 200 m, P = 0.002) at baseline in the intervention group. Another study30 demonstrated lower rates of having undergone a percutaneous coronary intervention (20.5 vs. 36.4%, P = 0.003) and angiotensin-converting enzyme-inhibitors prescription (56.2 vs. 68.5%, P = 0.03) in the intervention group. The details of patient parameters are shown in Table 1.
Types of digital health and characteristics of intervention
Included studies used DHIs to provide or support psychological intervention during the study period. The type of digital health was divided into ‘telemonitoring with a psychological intervention’,29,31,33–35‘PC/cellular phone–based psychosocial education and training’,18,24,27,28,30,32 and ‘VR’.25,26 In terms of ‘telemonitoring with a psychological intervention’, telemonitoring is indeed DHI, but one of the psychological interventions did not use DHI (counselling during each follow-up visit35). The target population of all five studies using a telemonitoring intervention was HF. Regarding the PC-based psychosocial education and training, CBT was provided. As for VR intervention, relaxing images and/or music were provided in cardiac care unit (CCU)25 or in cardiac rehabilitation (CR)26 with the relaxation training sessions.
Reasons for drop out
The study periods ranged from 3 days to 12 months. The mean completion rates among the included trials were 79.3% (ranged from 61.8 to 98.0%) excluding two studies25,33 because no information was obtained. This rate was >30% in the study of telemonitoring for patients with HF (NYHA Classes 2–4).29 Common causes for drop out included personal or family reasons,24,28,32 medical reasons,24,27,29,30,32 and technical problems about the devices.24 Some articles did not report precise reasons for drop out.31,33,35
Study quality
The risk of bias was assessed in every study. Almost all the studies demonstrated a low risk of bias for attrition bias and reporting bias. As for selection bias, two studies29,34 showed differences in age between the intervention and control group in baseline characteristics. Taking into account this point and incompleteness of some information, six studies (46%) had a low risk of bias and seven studies (54%) showed unknown because of incomplete information. Blinding of participants and personnel was not possible due to the nature of the intervention. Blinding of outcome assessment was not demonstrated in most studies. Overall, all of 13 studies were thought to be of high quality (see Supplementary material online 3). Funnel plots of the depression and anxiety outcomes are shown in Supplementary material online 7. Since the funnel plots were nearly symmetrical, no evidence of strong publication bias was found.
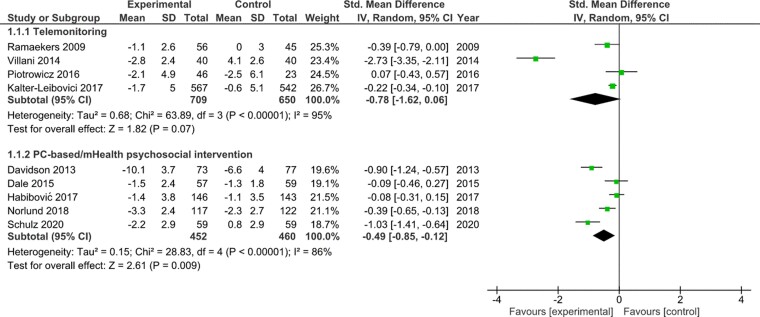
Outcomes (depression)
Nine of 11 studies included in the meta-analysis reported depression as an outcome. Supplementary material online 8 indicated the results of the meta-analysis and forest plot between the two groups. Depression questionnaire scores were significantly lower (better) in the intervention group than in the control group (standardized mean difference −0.34; 95% CI −0.42 to −0.26; P < 0.001) with considerable heterogeneity (I2 = 92%, P < 0.001). Figure 3 shows the result of subgroup analysis classified by DHI type. The intervention group tended to have lower (better) depression questionnaire scores on telemonitoring than the control group (standardized mean difference −0.78; 95% CI −1.62 to 0.06; P = 0.07) with considerable heterogeneity found (I2 = 95%, P < 0.001). The intervention group also showed a significant lower (better) depression questionnaire scores on PC/mobile health–based psychosocial education and training compared with the control group (standardized mean difference −0.49; 95% CI −0.85 to −0.12; P = 0.009) with considerable heterogeneity found (I2 = 86%, P < 0.001).
Figure 3.
Subgroup analysis focusing on telemonitoring as digital health intervention type with psychological intervention for depression outcomes.
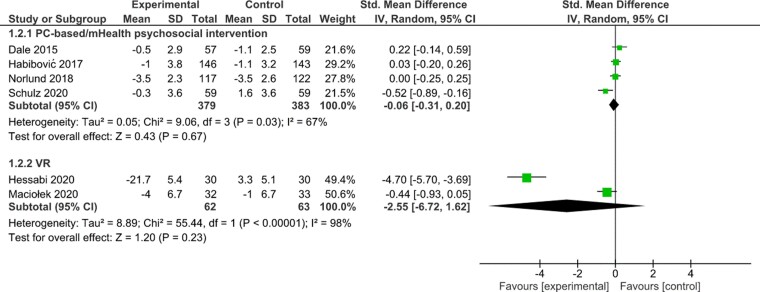
Outcome (anxiety)
Seven studies out of 10 studies included in the meta-analysis reported anxiety outcomes. Supplementary material online 9 indicated the results of the meta-analysis and forest plot between the two groups. Anxiety questionnaire scores were significantly lower (better) in the intervention group than in the control group (standardized mean difference −0.23; 95% CI −0.37 to −0.10; P < 0.001) with considerable heterogeneity (I2 = 95%, P < 0.001). Figure 4 illustrates the result of subgroup analysis classified by DHI type. The intervention group showed no significant effect of psychosocial education and training using PC/mobile health on anxiety (standardized mean difference −0.06; 95% CI −0.31 to 0.20; P = 0.67) with substantial heterogeneity found (I2 = 67%, P = 0.03). It reported VR also had no significant effect on anxiety (standardized mean difference −2.55; 95% CI −6.72 to 1.62; P = 0.23), with considerable heterogeneity (I2 = 98%, P < 0.001).
Figure 4.
Subgroup analysis focusing on telemonitoring as digital health intervention type with psychological intervention for anxiety outcomes.
Discussion
Main findings
This systematic review and meta-analysis were conducted to elucidate the effects of DHIs on depression/anxiety of patients with heart disease. The results of the study are summarized as the following main findings. (i) Digital health interventions (especially telemonitoring) for HF or CHD patients are found to have a significant or trending positive effects on reducing depression levels even when the intervention is not aimed at improving mental health. (ii) The effects of PC- or mobile-based psychosocial interventions for patients with CHD or PC-based interventions for patients with ICD have significantly positive effects for reducing depression level.
Articles of digital health interventions without psychological intervention
This category included three studies of telemonitoring for patients with HF or myocardial infarction,20,22,23 and they had a significant positive impact on depression outcomes. In these studies, telemonitoring was used mostly measuring lifelog data without a psychological intervention. One of the included papers20 reported patients randomized to telemedicine show better quality of life (QoL) compared with patients in the control group and many systematic reviews mention that telemonitoring improves QoL, especially in HF patients.36 Telemonitoring of lifelog data includes physiological monitoring of cardiac patients (BP, BW, etc.), which is itself basic information for routine patient care. The previous review37 reported that telehealth is effective in reinforcing self-care behaviours and improving QoL for patients with HF, such as daily weighing and salt restriction. It is also well known that QoL is closely related to depression; improvement QoL through lifelog data telemonitoring of patients using digital health can be expected to reduce depressive mood.
Meanwhile, telemonitoring and being supervised by health providers include a content of ‘collaborative care management,’ which has been reported to reduce depressive symptoms.7,38 ‘Collaborative care’ is based on the multifaceted approach for depression in primary care, and includes (tele)monitoring or supervision by physicians while being in their primary care management.39 Especially in Giallauria’s study,23 telemonitoring was used in home-based CR, which consists of several factors of collaborative care. Although there was no specific psychological intervention intended in the included studies, telemonitoring of lifelog data by digital health contains such characteristics, which can result in improvement of psychological distress.
Articles of digital health interventions with psychological intervention
Telemonitoring for HF patients with psychosocial interventions tended to have a positive effect on depression. The ESC guidelines reported that multidisciplinary involvement has been recognized as a key point of non-pharmaceutical interventions to support HF patients.40 Thus, multidisciplinary collaborative care using a telemonitoring system is not only unique, but also effective because it facilitates patients to gain access to a psychologist, a nurse, and other healthcare professionals. The studies included video counselling or cardiac telerehabilitation as interventions. A recent review reports that such ‘online’ services are as good as in-person services,41 which supports this result. Together with the results of the DHI papers, which did not involve psychological intervention, telemonitoring of lifelog data is one of the best methods for managing depression.
The results of PC/cellular phone–based intervention for ICD and CHD patients had a significant effect for reducing depression in the review. A previous systematic review has shown that web-based and computer-delivered interventions are effective in improving depression and anxiety in healthy individual.42 A recent review in the COVID era has shown that PC-based consultations or CBT for chronic ill status improves psychological parameters, i.e. depression and anxiety.43 Schulz et al.24 discussed that how patients rated the availability of a trained psychologist and participation in discussions in the web as helpful in this intervention. The usefulness of DHIs in CBT is well demonstrated. On the other hand, the effect size for improvement in anxiety was very small and no benefit was demonstrated in this review. The results for depression and anxiety showed the same trend, with the exception of one paper,18 making it difficult to assess exactly why this difference occurred. For example, remote monitoring for ICD patients may cause anxiety by the confrontation with patients’ mental condition,44 and patients may respond differently to DHIs for depression and anxiety. In addition, the review includes articles that are essentially about patients with heart disease, not about patients diagnosed with anxiety disorder, indicating a lack of focus on the patients’ unique mental condition. The previous review45 also mentioned the need for more personalization in this field, and it is possible that these barriers are one of the reasons for ‘illogical’ results.
Lastly, the two papers about VR focused on anxiety for patients with CCU or CR. Although subgroup analysis of VR technology did not yield significant result for improvement in anxiety, within-group analysis showed a favourable effect of VR. A previous article mentioned that the visual and auditory nature is one of the reasons of the positive effect.46 As for intensive care unit (ICU), a recent paper demonstrated that a VR intervention reduced levels of anxiety and depression.47 Virtual reality techniques may be effective for stressed patients in ICU, which can apply to CCU. However, it is one of the newer topics in the fields of DHI, and more solid evidence is needed to show efficacy.
Future task
A previous systematic review mentioned the barriers to user engagement with DHIs for mental health.48 Because patients with heart disease represent a different population than relatively young psychiatric patients, it is important to understand the specific characteristics and personal preferences of the target population,49 among several limitations for DHIs. There is a research-to-practice gap for digital mental health implementation.50 As patients’ knowledge and experience with DHIs varies, healthcare providers need to respect patients’ shared decision-making and customize it to the patients’ clinical needs. This review indicates that telemonitoring systems, either directly or indirectly, and PC/mobile-based cognitive behavioural approaches has the potential to ameliorate depression levels in patients with heart disease at this moment. An RCT (NCT03373110) with three DHI arms (online mindfulness-based cognitive therapy and exercise telemonitoring, online CBT and exercise telemonitoring, and exercise telemonitoring alone) is ongoing in the USA. This trial certainly combines DHIs with and without psychological intervention, and the outcomes include both daily steps and mental health, reflecting the multifaceted nature of digital cardiology. Given the number of patients with heart disease increasing rapidly in the current aging society, mental health for elderly is an important issue. Although research in this field is still insufficient, implementation and progression of DHIs for psychological factors into our society must be encouraged.
Limitations
This review has some limitations. Firstly, only articles written in English were included and no attempt was made to include the grey literature. Secondly, the included studies had various types of cardiac disease, DHI, and outcome, and there was a high degree of heterogeneity even when subgroup analyses were performed. However, standard mean difference and random effects model were selected in this meta-analysis to account for the variability observed in the included studies. Risk of bias for each study was also systematically checked. Thirdly, even though the estimating equation was used, some RCTs had missing data, which may have introduced bias in the results. Fourthly, the conclusion is biased towards DHIs for HF and CHD because existing electronic devices (e.g. pacemaker, ICD) were excluded from DHIs. As evidence from RCTs on arrhythmia management using wearable devices (e.g. smartwatches) accumulates, DHI will provide more balanced coverage of cardiac disease in systematic reviews. Lastly, some included articles showed significant improvement in DHI in between-group analysis while the within-group analysis mentioned the improvement of outcomes also in the control group alone. It may indicate the difference between statistical and clinical significance.
Conclusion
This systematic review demonstrated that the use of information and communication technology has a beneficial impact on depression in patients with heart disease. Especially, telemonitoring systems for HF can be effective for psychological parameters even if they do not include psychological interventions.
Supplementary material
Supplementary material is available at European Heart Journal – Digital Health online.
Supplementary Material
Acknowledgement
The authors thank all the staff members of the laboratories and the statistician at the Jessa Hospital for their effort and understanding in this review.
Contributor Information
Toshiki Kaihara, Department of Cardiology, Heart Centre Hasselt, Jessa Hospital, Hasselt, Belgium; UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium; Division of Cardiology, Department of Internal Medicine, St Marianna University School of Medicine, Kawasaki, Japan.
Martijn Scherrenberg, Department of Cardiology, Heart Centre Hasselt, Jessa Hospital, Hasselt, Belgium; UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium; Faculty of Medicine and Health Sciences, UAntwerp, Antwerp, Belgium.
Valent Intan-Goey, Faculty of Medicine, Antwerp University Hospital, Edegem, Belgium.
Maarten Falter, Department of Cardiology, Heart Centre Hasselt, Jessa Hospital, Hasselt, Belgium; UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium; Faculty of Medicine, KULeuven, Leuven, Belgium.
Hanne Kindermans, UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium.
Ines Frederix, Department of Cardiology, Heart Centre Hasselt, Jessa Hospital, Hasselt, Belgium; UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium; Faculty of Medicine and Health Sciences, UAntwerp, Antwerp, Belgium; Faculty of Medicine, Antwerp University Hospital, Edegem, Belgium.
Paul Dendale, Department of Cardiology, Heart Centre Hasselt, Jessa Hospital, Hasselt, Belgium; UHasselt, Faculty of Medicine and Life Sciences/Human-Computer Interaction and eHealth, Diepenbeek, Belgium.
Authors’ contributions
T.K. had full access to all the study data and takes responsibility for the integrity of the data and the accuracy of the data analysis. T.K., M.S., M.F., H.K., and P.D. contributed to the study conception or design of the work. T.K., M.S., and V.I.G. contributed the acquisition of data for the work. T.K. contributed the analysis and interpretation of data for the work. T.K. drafted the manuscript. All authors critically revised the manuscript, and gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Funding
None declared.
Data Availability
All dataset analysed are included in this manuscript and supplementary materials.
References
- 1. Vaccarino V, Badimon L, Bremner JD, Cenko E, Cubedo J, Dorobantu M, Duncker DJ, Koller A, Manfrini O, Milicic D, Padro T, Pries AR, Quyyumi AA, Tousoulis D, Trifunovic D, Vasiljevic Z, De Wit C, Bugiardini R, Lancellotti P, Carneiro AV. Depression and coronary heart disease: 2018 position paper of the ESC working group on coronary pathophysiology and microcirculation. Eur Heart J 2020;41:1687–1696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Celano CM, Villegas AC, Albanese AM, Gaggin HK, Huffman JC. Depression and anxiety in heart failure: a review. Harv Rev Psychiatry 2018;26:175–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Freedenberg V, Thomas SA, Friedmann E. Anxiety and depression in implanted cardioverter-defibrillator recipients and heart failure: a review. Heart Fail Clin 2011;7:59–68. [DOI] [PubMed] [Google Scholar]
- 4. Richards SH, Anderson L, Jenkinson CE, Whalley B, Rees K, Davies P, Bennett P, Liu Z, West R, Thompson DR, Taylor RS. Psychological interventions for coronary heart disease: cochrane systematic review and meta-analysis. Eur J Prev Cardiol 2018;25:247–259. [DOI] [PubMed] [Google Scholar]
- 5. Oneil A, Taylor B, Hare DL, Sanderson K, Cyril S, Venugopal K, Chan B, Atherton JJ, Hawkes A, Walters DL, Oldenburg B. Long-term efficacy of a tele-health intervention for acute coronary syndrome patients with depression: 12-month results of the MoodCare randomized controlled trial. Eur J Prev Cardiol 2015;22:1111–1120. [DOI] [PubMed] [Google Scholar]
- 6. Hegel MT, Imming J, Cyr-provost M, Hitchcock NP, Arean PA, Unutzer J. Role of behavioral health professionals in a collaborative stepped care treatment model for depression in primary care: project IMPACT. Fam Syst Heal 2002;20:265–277. [Google Scholar]
- 7. Cui X, Dong W, Zheng H, Li H. Collaborative care intervention for patients with chronic heart failure: a systematic review and meta-analysis. Medicine (Baltimore) 2019;98:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Scherrenberg M, Wilhelm M, Hansen D, Völler H, Cornelissen V, Frederix I, Kemps H, Dendale P. The future is now: a call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European association of preventive cardiology. Eur J Prev Cardiol 2020:2047487320939671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Whitelaw S, Pellegrini DM, Mamas MA, Cowie M, Van Spall HGC. Barriers and facilitators of the uptake of digital health technology in cardiovascular care: a systematic scoping review. Eur Hear J Digit Heal 2021;2:62–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Firth J, Torous J, Nicholas J, Carney R, Pratap A, Rosenbaum S, Sarris J. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry 2017;16:287–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ebert DD, Daele Van T, Nordgreen T, Karekla M, Compare A, Zarbo C, Brugnera A, Øverland S, Trebbi G, Jensen KL, Kaehlke F, Baumeister H. Internet- and mobile-based psychological interventions: applications, efficacy, and potential for improving mental health: a report of the EFPA E-health taskforce. Eur Psychol 2018;23:167–187. [Google Scholar]
- 12. Freeman D, Reeve S, Robinson A, Ehlers A, Clark D, Spanlang B, Slater M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol Med 2017;47:2393–2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Page MJ, Moher D. Evaluations of the uptake and impact of the preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and extensions: a scoping review. Syst Rev Syst Rev 2017;6:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, 2011. Available fromwww.handbook.cochrane.org.
- 15. Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Follmann D, Elliott P, Suh I, Cutler J. Variance imputation for overviews of clinical trials with continuous response. J Clin Epidemiol 1992;45:769–773. [DOI] [PubMed] [Google Scholar]
- 17. Rosenthal R. Meta-analytic Procedures for Social Research. Newbury Park, CA: Sage Publ; 1993. [Google Scholar]
- 18. Davidson KW, Bigger JT, Burg MM, Carney RM, Chaplin WF, Czajkowski S, Dornelas E, Duer-Hefele J, Frasure-Smith N, Freedland KE, Haas DC, Jaffe AS, Ladapo JA, Lespérance F, Medina V, Newman JD, Osorio GA, Parsons F, Schwartz JE, Shaffer JA, Shapiro PA, Sheps DS, Vaccarino V, Whang W, Ye S. Centralized, stepped, patient preference-based treatment for patients with post-acute coronary syndrome depression: CODIACS vanguard randomized controlled trial. JAMA Intern Med 2013;173:997–1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. Br Med J 2004;329:145–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Koehler J, Stengel A, Hofmann T, Wegscheider K, Koehler K, Sehner S, Rose M, Deckwart O, Anker SD, Koehler F, Laufs U. Telemonitoring in patients with chronic heart failure and moderate depressed symptoms: results of the telemedical interventional monitoring in heart failure (TIM-HF) study. Eur J Heart Fail 2021;23:186–194. [DOI] [PubMed] [Google Scholar]
- 21. Vieira Á, Melo C, Machado J, Gabriel J. Virtual reality exercise on a home-based phase III cardiac rehabilitation program, effect on executive function, quality of life and depression, anxiety and stress: a randomized controlled trial. Disabil Rehabil Assist Technol Informa 2018;13:112–123. [DOI] [PubMed] [Google Scholar]
- 22. Smolis-Bąk E, Dąbrowski R, Piotrowicz E, Chwyczko T, Dobraszkiewicz-Wasilewska B, Kowalik I, Kazimierska B, Jędrzejczyk B, Smolis R, Gepner K, MacIąg A, Sterliński M, Szwed H. Hospital-based and telemonitoring guided home-based training programs: effects on exercise tolerance and quality of life in patients with heart failure (NYHA class III) and cardiac resynchronization therapy. A randomized, prospective observation. Int J Cardiol 2015;199:442–447. [DOI] [PubMed] [Google Scholar]
- 23. Giallauria F, Lucci R, Pilerci F, De LA, Manakos A, Psaroudaki M, D’Agostino M, Vitelli A, Maresca L, Del FD, Vigorito C. Efficacy of telecardiology in improving the results of cardiac rehabilitation after acute myocardial infarction. Monaldi Arch Chest Dis Card Ser 2006;66:8–12. [DOI] [PubMed] [Google Scholar]
- 24. Schulz SM, Ritter O, Zniva R, Nordbeck P, Wacker C, Jack M, Groschup G, Deneke T, Puppe F, Ertl G, Angermann C, Störk S, Pauli P. Efficacy of a web-based intervention for improving psychosocial well-being in patients with implantable cardioverter-defibrillators: the randomized controlled ICD-FORUM trial. Eur Heart J 2020;41:1203–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hessabi M, Sajjadi M, Shareinia H, Rouhani M. The effect of virtual reality on anxiety and quality of sleep in patients in cardiac care unit. Int J Pharm Phytopharm Res 2020;10:37–42. [Google Scholar]
- 26. Maciołek J, Wąsek W, Kamiński B, Piotrowicz K, Krzesiński P. The impact of mobile virtual reality–enhanced relaxation training on anxiety levels in patients undergoing cardiac rehabilitation. Kardiol Pol 2021;78:1032–1034. [DOI] [PubMed] [Google Scholar]
- 27. Islam SMS, Chow CK, Redfern J, Kok C, Rådholm K, Stepien S, Rodgers A, Hackett ML. Effect of text messaging on depression in patients with coronary heart disease: a substudy analysis from the TEXT ME randomised controlled trial. BMJ Open 2019;9:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Norlund F, Wallin E, Olsson EMG, Wallert J, Burell G, von Essen L, Held C. Internet-based cognitive behavioral therapy for symptoms of depression and anxiety among patients with a recent myocardial infarction: the u-care heart randomized controlled trial. J Med Internet Res 2018;20:e88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kalter-Leibovici O, Freimark D, Freedman LS, Kaufman G, Ziv A, Murad H, Benderly M, Silverman BG, Friedman N, Cukierman-Yaffe T, Asher E, Grupper A, Goldman D, Amitai M, Matetzky S, Shani M, Silber H, Israel Heart Failure Disease Management Study (IHF-DMS) investigators . Disease management in the treatment of patients with chronic heart failure who have universal access to health care: a randomized controlled trial. BMC Med 2017;15:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Habibović M, Denollet J, Cuijpers P, van der Voort PH, Herrman JP, Bouwels L, Valk SDA, Alings M, Theuns DAMJ, Pedersen SS. Web-based distress management for implantable cardioverter defibrillator patients: a randomized controlled trial. Heal Psychol 2017;36:392–401. [DOI] [PubMed] [Google Scholar]
- 31. Bekelman DB, Plomondon ME, Carey EP, Sullivan MD, Nelson KM, Hattler B, McBryde CF, Lehmann KG, Gianola K, Heidenreich PA, Rumsfeld JS. Primary results of the patient-centered disease management (PCDM) for heart failure study a randomized clinical trial. JAMA Intern Med 2015;175:725–732. [DOI] [PubMed] [Google Scholar]
- 32. Dale LP, Whittaker R, Jiang Y, Stewart R, Rolleston A, Maddison R. Text message and internet support for coronary heart disease self-management: results from the text4heart randomized controlled trial. J Med Internet Res 2015;17:e237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Ramaekers BLT, Janssen-Boyne JJ, Gorgels APM, Vrijhoef HJM. Adherence among telemonitored patients with heart failure to pharmacological and nonpharmacological recommendations. Telemed e-Health 2009;15:517–524. [DOI] [PubMed] [Google Scholar]
- 34. Piotrowicz E, Piotrowski W, Piotrowicz R. Positive effects of the reversion of depression on the sympathovagal balance after telerehabilitation in heart failure patients. Ann Noninvasive Electrocardiol 2016;21:358–368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Villani A, Malfatto G, Compare A, Rosa FD, Bellardita L, Branzi G, Molinari E, Parati G. Clinical and psychological telemonitoring and telecare of high risk heart failure patients. J Telemed Telecare 2014;20:468–475. [DOI] [PubMed] [Google Scholar]
- 36. Bashi N, Karunanithi M, Fatehi F, Ding H, Walters D. Remote monitoring of patients with heart failure: an overview of systematic reviews. J Med Internet Res 2017;19:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Radhakrishnan K, Jacelon C. Impact of telehealth on patient self-management of heart failure. A review of literature. J Cardiovasc Nurs 2012;27:33–43. [DOI] [PubMed] [Google Scholar]
- 38. Janine A, Peter B, Simon G, Karina L, David R, Linda G, Chris D, Peter C. Collaborative care for depression and anxiety problems. Cochrane Database Syst Rev 2012;10:CD006525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Bower P, Gilbody S, Richards D, Fletcher J, Sutton A. Collaborative care for depression in primary care. Making sense of a complex intervention: systematic review and meta-regression. Br J Psychiatry 2006;189:484–493. [DOI] [PubMed] [Google Scholar]
- 40. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJ V, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK, ESC Scientific Document Group . 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–3726. [DOI] [PubMed] [Google Scholar]
- 41. Batastini AB, Paprzycki P, Jones ACT, MacLean N. Are videoconferenced mental and behavioral health services just as good as in-person? A meta-analysis of a fast-growing practice. Clin Psychol Rev 2021;83:101944. [DOI] [PubMed] [Google Scholar]
- 42. Davies EB, Morriss R, Glazebrook C. Computer-delivered and web-based interventions to improve depression, anxiety, and psychological well-being of university students: a systematic review and meta-analysis. J Med Internet Res 2014;16:1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Sasseville M, Leblanc A, Boucher M, Dugas M, Mbemba G, Tchuente J, Chouinard MC, Beaulieu M, Beaudet N, Skidmore B, Cholette P, Aspiros C, Larouche A, Chabot G, Gagnon MP. Digital health interventions for the management of mental health in people with chronic diseases: a rapid review. BMJ Open 2021;11:e044437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vinck I, Stroobandt S, Gerkens S, De Laet C. Remote Monitoring for Patients with Implanted Defibrillators. Technology Evaluation and Broader Regulatory Framework. Health Technology Assessment (HTA) and Health Services Research (HSR). Brussels: Belgian Health Care Knowledge Centre (KCE). 2010. KCE Reports 136C. D/2010/10.273/55. [Google Scholar]
- 45. Chow CK, Ariyarathna N, Islam SMS, Thiagalingam A, Redfern J. mHealth in cardiovascular health care. Hear Lung Circ 2016;25:802–807. [DOI] [PubMed] [Google Scholar]
- 46. Aliakbari M, Alipor A, Ebrahimimoghadam H, Fekraty M. The effect of virtual reality (VR) on psychological disorders in cancer cases. Mil Caring Sci 2017;4:49–57. [Google Scholar]
- 47. Ong TL, Ruppert MM, Akbar M, Rashidi P, Ozrazgat-Baslanti T, Bihorac A, Suvajdzic M. Improving the intensive care patient experience with virtual reality—A feasibility study. Crit Care Explor 2020;2:e0122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Borghouts J, Eikey E, Mark G, De LC, Schueller SM, Schneider M, Stadnick N, Zheng K, Mukamel D, Sorkin DH. Barriers to and facilitators of user engagement with digital mental health interventions: systematic review. J Med Internet Res 2021;23:e24387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Titov N, Hadjistavropoulos HD, Nielssen O, Mohr DC, Andersson G, Dear BF. From research to practice: ten lessons in delivering digital mental health services. J Clin Med 2019;8:1239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Graham AK, Lattie EG, Powell BJ, Lyon AR, Smith JD, Schueller SM, Stadnick NA, Brown CH, Mohr DC. Implementation strategies for digital mental health interventions in health care settings. Am Psychol 2020;75:1080–1092. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All dataset analysed are included in this manuscript and supplementary materials.