Abstract
Aims
Technological advancements have transformed healthcare. System delays in transferring patients with ST-segment elevation myocardial infarction (STEMI) to a primary percutaneous coronary intervention (PCI) centre are associated with worse clinical outcomes. Our aim was to design and develop a secure mobile application, STEMIcathAID, streamlining communication, and coordination between the STEMI care teams to reduce ischaemia time and improve patient outcomes.
Methods and results
The app was designed for transfer of patients with STEMI to a cardiac catheterization laboratory (CCL) from an emergency department (ED) of either a PCI capable or a non-PCI capable hospital. When a suspected STEMI arrives to a non-PCI hospital ED, the ED physician uploads the electrocardiogram and relevant patient information. An instant notification is simultaneously sent to the on-call CCL attending and transfer centre. The attending reviews the information, makes a video call and decides to either accept or reject the transfer. If accepted, on-call CCL team members receive an immediate push notification and begin communicating with the ED team via a HIPAA compliant chat. The app provides live GPS tracking of the ambulance and frequent clinical status updates of the patient. In addition, it allows for screening of STEMI patients in cardiogenic shock. Prior to discharge, important data elements have to be entered to close the case.
Conclusion
We developed a novel mobile app to optimize care for STEMI patients and facilitate electronic extraction of relevant performance metrics to improve allocation of resources and reduction of costs.
Keywords: STEMI, Door-to-balloon time, First medical contact, EKG
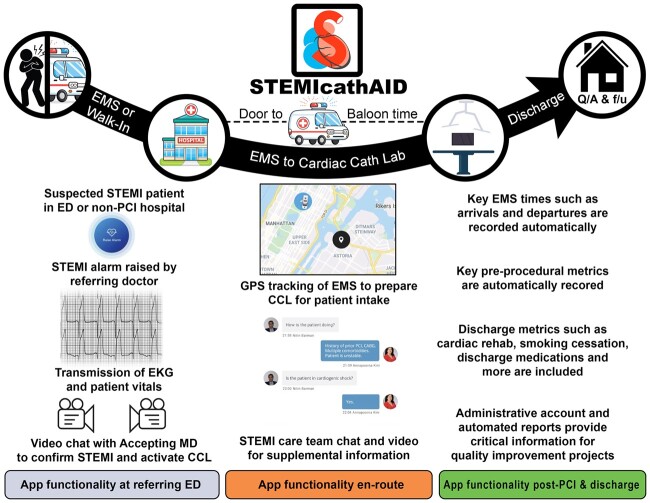
Graphical Abstract
Development of a mobile application, STEMIcathAID, to optimize care for ST-segment elevation myocardial infarction (STEMI) patients in a large healthcare system. When a patient with suspected STEMI arrives to a non-percutaneous coronary intervention hospital, the attending physician (referring MD) raises an alarm and uploads the patient’s electrocardiogram. An instant automatic notification is sent to the on-call cardiac catheterization laboratory (CCL) attending, who reviews the information, discusses the case over the phone and/or video chat with the referring MD and makes a decision to either accept or reject the STEMI request. If the request is accepted, the on-call CCL team receives an immediate automatic notification with a loud alarm sound. The app is activated and provides a communication platform for all STEMI care team members with access to video calls, chat, instantaneous updates on the patient’s clinical situation, and live GPS tracking of the ambulance. Emergency medical service and first medical contact times along with all patient-related metrics are recorded automatically and can be extracted for quality assurance purposes. Prior to discharge, a set of important data elements such as discharge medications, cardiac rehabilitation recommendations, and lifestyle modifications have to be entered to close the case.
Introduction
ST-segment elevation myocardial infarction (STEMI) is a medical emergency, in which patient survival and clinical outcomes depend on reducing the time interval from symptom onset to reperfusion, the total ischaemic time.1 System delay is an independent predictor of mortality in STEMI patients treated with primary percutaneous coronary intervention (PCI).2 The European Society of Cardiology (ESC) and American College of Cardiology Foundation/American Heart Association (ACCF/AHA) guidelines emphasize the importance of improving the time from the first medical contact (FMC) to primary PCI with an ideal FMC-to-device time goal of 90 min or less.3–6 Considerable advances in STEMI management over the recent decades have been achieved by implementing a series of important strategies targeting system delays such as obtaining a pre-hospital electrocardiogram (EKG) by emergency medical service (EMS) and activation of the cardiac catheterization laboratory (CCL).7–9 While the CCL pre-activation is a critical component of reducing reperfusion time and is associated with decreased mortality, it might result in frequent cancellations due to ‘false alarms’.10–12
Healthcare mobile applications (apps) have revolutionized the way patients receive medical treatment. Delivering the best possible care to a STEMI patient involves multiple steps and teams and requires all components of the care to work quickly and seamlessly. Over the last decade, telemedicine systems,13–15 social communication platforms,16 and mobile apps17,18 have been successfully used for optimizing STEMI care (Table 1). In this background, our goal was to develop a secure mobile app, STEMIcathAID, to streamline real-time communication, and coordination between the STEMI care teams from the onset of the emergency through hospital discharge in an effort to reduce ischaemia times and improve patients’ outcomes. In addition to pre-hospital STEMI activation of the CCL, the app automatically geenrates a shock notification, in order to notify the CCL teams, if clinical criteria for cardiogenic shock (CS) are met. The app implements the current international guidelines and performance measures3,4,8 and incorporates our own extensive experience in treating STEMI in a large healthcare system combining eight hospital campuses in New York City. This report describes the rationale and design of the mobile app with a special focus on the user roles, security, and functionality.
Table 1.
Mobile applications and telemedicine solutions for STEMI care
| Technology/equipment | Study period/centre/country | Functionality | Patient population/effect on patient outcomes | |
|---|---|---|---|---|
| 1 | Telemedicine |
2008–2011 Aarhus University Hospital Skejby, Denmark (Rasmussen et al., Heart, 201415) |
|
|
| 2 | Mobile telemedicine system |
2008–2012 National Cerebral and Cardiovascular Center Osaka, Japan (Kawakami et al., Circ J, 201614) |
|
|
| 3 | Telemedicine |
2005–2014 11 centres in Denmark, Italy, Netherland, USA, Canada (meta-analysis) (Brunetti et al., Int J Cardiol, 201713) |
|
|
| 4 |
STOP STEMI© Mobile app/phones and tablets |
2012–2013 Good Shepherd Health System Longview, TX, USA (Dickson et al., Crit Pathw Cardiol, 201418) |
|
|
| 5 | Mobile app ‘STEMI’/mobile phones |
2015–2016 Presov University Slovakia (Studencan et al., PLoS One, 201817) |
|
|
| 6 |
Push notifications for pre-hospital EKG/Vocera WiFi communication system |
2012–2013 Intermountain Medical Center Murray, UT, USA (Goebel et al., West J Emerg Med, 201932) |
|
|
| 7 |
WeChat app Group/mobile phones |
2018 The Second Affiliated Hospital of Shantou University Medical College China (Liu et al., J Telemed Telecare, 202016) |
|
|
| 8 | Tiantanzhixin app for patients with chronic diseases/mobile phones |
2019–2020 Beijing Tiantan Hospital China (Nan et al., Med Sci Monit, 202033) |
|
|
CCL, cardiac catheterization laboratory; D2B, door-to-balloon; ED, emergency department; EKG, electrocardiogram; EMS, emergency medical service; ETA, estimated time of arrival; FMC, first medical contact; STEMI, ST-segment elevation myocardial infarction.
EMS used the app in cases of diagnostic uncertainty only.
App rationale and design
STEMIcathAID was designed by the Mount Sinai Hospital (MSH) STEMI care team, developed by an external technical app development team and tested in one of our non-PCI hospitals after rigorous clinical, Information Technology (IT), and security reviews. The app development process can be divided into the following phases.
Conceptualization
The development of the application started in July 2018 when the STEMI care team members reviewed the current standards of treatment for STEMI patients—overall and within the Mount Sinai Health system, and assessed the need for improvement in various components of the system of care for patients with STEMI. The response to STEMI patients consisted of pager messages, phone calls, and email notifications between physicians and nurses to perform an emergent catheterization, arrange patient’s transfer from one of our non-PCI hospitals to the CCL, and collect valuable clinical information. The system was outdated, inefficient and required a team of dedicated employees to collect performance metrics for internal process optimization and for external reporting. After multiple meetings involving physicians, fellows, nurses, technicians, and administrative personnel involved in STEMI patients care, we developed a concept for the app by addressing challenging situations arising during team members notification and communication, patients transfer, ambulance tracking, data capture, and collection. We aimed to (i) improve communication between all parties involved by eliminating multiple phone calls and text messages; (ii) facilitate transfer of information relevant to optimal care decisions; (iii) automate the workflow using a multi-level alert and notification system to replace an outdated pager system; (iv) reduce incorrect CCL activations; (v) improve time management for all teams by ‘real-time’ tracking of FMC times, ambulance times and hospital arrival times; and (vi) automate quality assurance (QA) data collection and extraction.
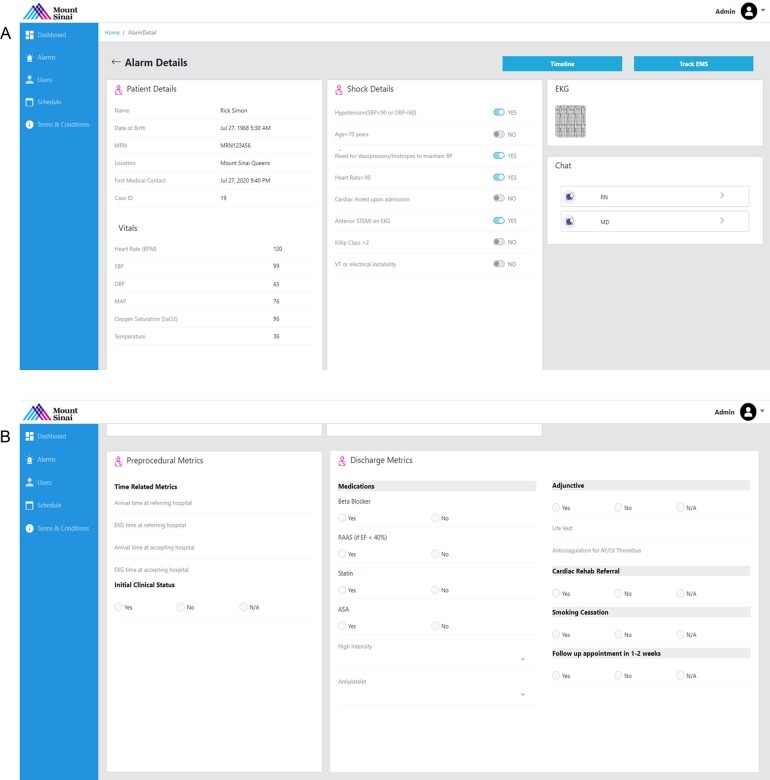
Preparation
In this phase, we collected and summarized clinical evidence and current guidelines for the management of patients with STEMI in order to implement the most recent advances in the STEMI care into the app algorithm. To enhance communication among the teams, we decided to utilize a wide variety of communication tools including phone and video calls, image transfer, and chat functionality. The tools allow every team member to collaborate and work simultaneously in taking care of the patient from presentation to discharge. Based on the app’s aims and taking into account our previous experience in creating mobile apps (OCTAID, BifurcAID, CalcificAID, TranseptAID, and TAVRcathAID),19 we named the new app STEMIcathAID and developed a logo reflecting and communicating the app’s aims and functionality (Figure 1).
Figure 1.
STEMIcathAID logo. The app’s logo reflects and communicates its aims and functionality.
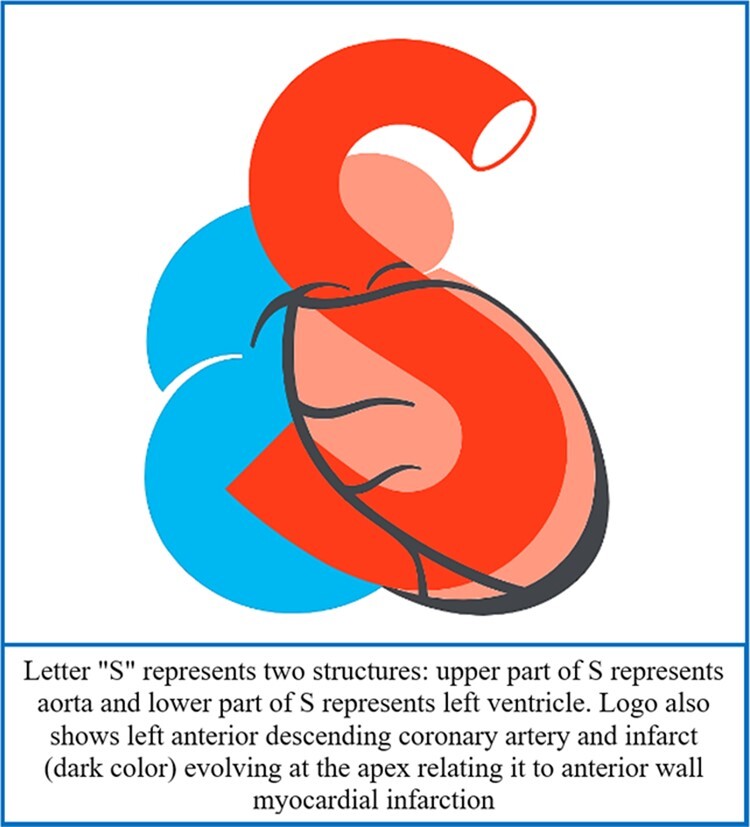
Algorithm development
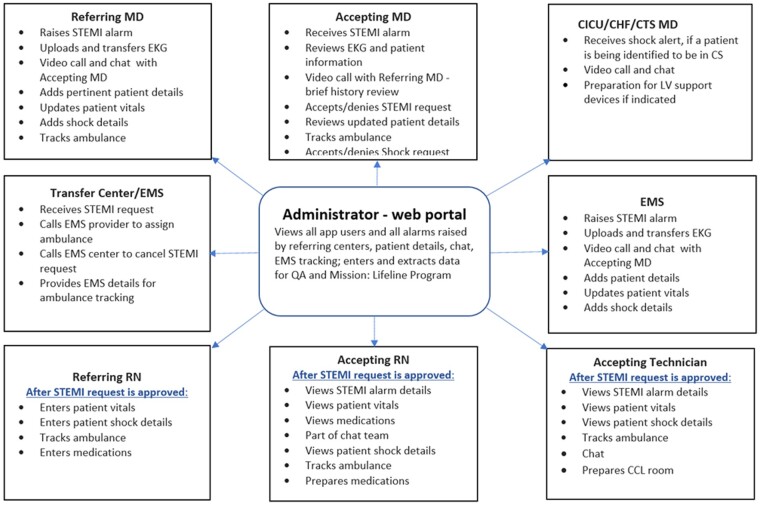
This phase included identification of the main pathways, definition of users and roles, app design, and proposal preparation. The app pathways were defined as follows: EKG upload at a referring centre, STEMI assessment and activation by interventional cardiologist on call, CCL and transfer centre activation, live ambulance tracking, and CS screening. The key members of the STEMI team were identified as medical provider from a non-PCI hospital (referring MD and RN), EMS personnel, on-call CCL doctors and nurses (accepting MD and RN), transfer centre personnel and CS team (CICU/CHF/CTS MD) as shown in (Figure 2). Multiple referring centres are allowed in the app with each centre having access to its own patients only. The administrator has access to all patients and is able to overview the activity of all centres and users through a web portal. The users will have the app installed on their mobile phones and use secure login IDs to access it. On-call CCL personnel will login into the app at the beginning of their shift and logout at the end of the shift. The referring and accepting RNs will have an additional option to access the app functionality using a web portal.
Figure 2.
STEMIcathAID users and roles. The app’s users are the key members of the STEMI care team representing a non-PCI hospital (referring MD and RN), on-call CCL doctors and nurses (accepting MD and RN), emergency medical services (EMS) personnel, transfer centre, and CS team including Cardiac Intensive Care Unit (CICU), Congestive heart failure (CHF) and Cardiothoracic Surgery (CTS). The app is design to include multiple referring centres with each centre having access to its own patients only. The administrator has access to all patients and is able to overview the activity of all centres and users through a web portal.
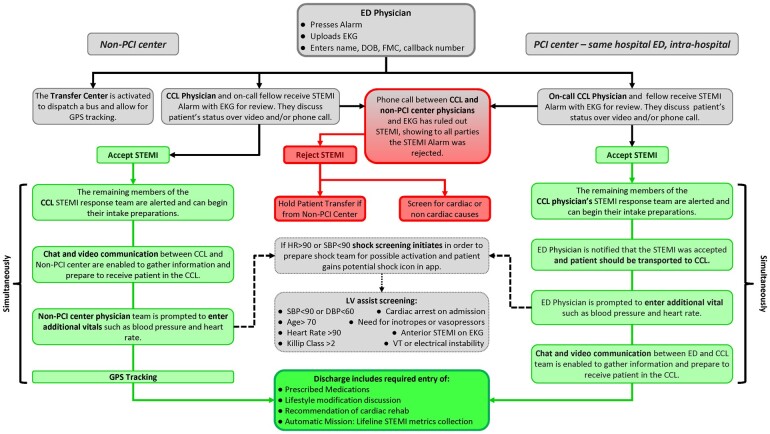
When a patient with suspected STEMI arrives to one of non-PCI hospitals emergency department (ED) (referring centre), the ED attending physician (referring MD) opens the app and raises an alarm using a single button on the app’s home page (Figure 3). Then he/she uploads the patient’s EKG by taking a photo of it through the app and enters the patient’s name, date of birth, FMC time, and a call back number. An instant simultaneous notification is sent to the on-call CCL attending (accepting MD) and to the transfer centre in case of inter-facility transfer. The CCL on-call attending reviews the information, discusses the case over the phone and/or video chat with the referring MD and makes a decision to either accept or reject the request. The patient’s vital signs including blood pressure, heart rate, oxygen saturation, and temperature are entered into the app. While the accepting MD is reviewing the EKG and other criteria to decide if appropriate to accept, the transfer centre assigns an ambulance to transfer the patient. If the STEMI request is accepted, the on-call CCL team including fellows, nurses, and technicians receive an immediate push notification with a loud alarm sound. The app is now activated and opens a communication platform for all STEMI care team members. Secure video calls and chat between the team members are used to receive instantaneous updates about the patient’s clinical situation provide further instructions and prepare the CCL room for the emergency procedure to facilitate intervention without delay. The app provides live GPS tracking of the transferring ambulance. If STEMI is ruled out and the request is rejected, all teams receive a reject notification and patient transfer is cancelled. If the patient is determined to be in, or at risk for, CS, STEMI team members will receive a shock alert and preparations for left ventricular support device will also be made. When the patient is ready for discharge, discharge medications, cardiac rehabilitation recommendations, and lifestyle modifications are discussed with the patient and entered into the app. If a STEMI patient arrives to an ED of a primary PCI capable hospital, the ED attending physician opens the app, raises an alarm and a simultaneous notification is sent to the on-call CCL physician. If the STEMI request is accepted, on-call CCL team is notified that the patient should be transported to the CCL and the ED physician is prompted to enter additional vitals and medication information. (Figure 3).
Figure 3.
STEMIcathAID design and workflow diagram. The app is design to streamline real-time communication and coordination between the STEMI care teams from the onset of the emergency through hospital discharge.
Technical development
The app proposal had been discussed with several software development companies and Daffodil Software Pvt. Ltd. (Gurgaon, India) was selected for the project based on the level of expertise in development of HIPAA compliant apps, previous projects, 24/7 technical support, client reviews, and financial considerations. The technical app development team started building the app after project details were clarified, mockups, and wireframes were discussed and approved by the STEMI care team. Weekly meetings were conducted to sustain communication between the technical and clinical teams, monitor progress and provide instant feedback on the product at each stage of the development. Close collaboration between clinicians and the technical team was crucial for the development of the secure sophisticated mobile app with multiple roles and access levels to meet the tasks of multiple providers. One of the important issues was selection of third party vendors for text chat and video integration into the application. We reviewed several vendors who offer text chat and video platforms to review critical considerations such as HIPAA compliancy, data storage and compatibility, execution of a Business Associate Agreement (BAA), and app maintenance. Since no single vendor was able to provide a HIPAA compliant text chat and video platform, two different vendors, Vonage and PubNub, were selected for these specific features.
Application security
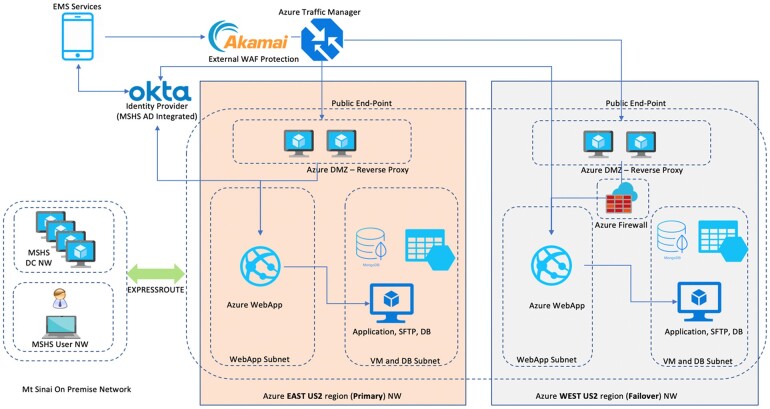
STEMIcathAID architecture diagram demonstrates multiple layers of security implemented into the app to keep patient data protected and ensure HIPAA compliance. Application level security: the administrator creates profiles for authorized users, who will have access to the app after downloading it to a password protected encrypted mobile phones and setting up their accounts. Passwords are stored as salted hash, and user data are stored separately. Notification is shown to a user when the user tries to log in from multiple devices, there is an option to sign out from all other devices in case of suspicious activity. EKG image is captured within application and uploaded directly to the backend along with patient information (name, date of birth, FMC, vitals, and shock details); it is not stored on the device. All the data are encrypted in transit with SSL/TLS protocol. The backend decrypts the data and uploads the image on the object storage bucket. This transaction is also secured with SSL/TLS and the bucket itself has encryption at rest. The data are encrypted with KMS and stored into the DB. Alarm notification is sent to only certain users based on the role and schedule and contains the case ID; there is no patient-related data. The raised alarm first needs to be approved by an on call CCL physician, only then the details are shared with the other users. If the alarm is not approved, the referring MD will be notified and the alarm will be removed from the app after 24 h; however, the details are still stored in the database. Only the relevant information is visible to each user based on role. The request is removed 24 h after its closure for all roles except for the accepting MD. Infrastructure level security: the backend server lies within a VPC and is inaccessible from outside that VPC except for via the application endpoint that is the load balancer from the cloud provider. The load balancer itself sits behind a firewall. The storage volume for database is also encrypted with KMS. A risk assessment review of the app was completed by the MSH IT Security Department and included information protection, network perimeter and mobile devices security, intrusion detection, connections to any external platforms associated with third party services or apps, compliance with government regulations, vulnerability management and security incident monitoring, reporting and response among other aspects of IT security control.
The web and mobile backend of the application is hosted on MSH’s Microsoft Azure server to take advantage of the pre-vetted, secure, internal solution recommended by MSH security team (Figure 4). This addressed compliance issues and ensured that protected health information (PHI) elements would be safely stored within the hospital digital network. Azure virtual machine (VM) scale sets let one create and manage a group of identical, load balanced VMs. The number of VM instances can automatically increase or decrease in response to demand or a defined schedule providing high availability to the app. Data stored in Azure VM disks is encrypted using keys stored in Azure Key Vault. Azure Site Recovery offers a real-time disaster recovery solution for quick recovery of PHI in the event of a natural calamity or disaster.
Figure 4.
App architecture diagram. The web and mobile backend of the application is hosted on MSH’s Microsoft Azure server; protected health information (PHI) elements are stored within the Mount Sinai digital network. The number of Azure virtual machine (VM) instances is automatically adjust to the app’s demand. The stored data is encrypted using keys stored in Azure Key Vault. Azure Site Recovery offers a real-time disaster recovery solution in the event of a natural calamity or disaster.
Data capture and reporting
One of the important features of the application is the ability to automatically capture key times to reperfusion and pre-procedural/discharge metrics for each patient including the AHA Mission: Lifeline STEMI recognition program’s performance measures.8 Almost 80 parameters including key times to reperfusion (FMC, arrival at the referring hospital, raising the alarm, EKG transmission, ROSC time, moving to CCL) and related to the patient arrival at a non-PCI hospital (EKG, vitals, medication, and CS), transfer to CCL (EMS pick up and arrival time), and discharge (date/time, medication and counselling) are collected for each patient (Supplementary material online, Table S1). The data can be extracted and exported as an Excel or .csv file weekly or/and monthly for routine performance metrics assessment to ensure optimization and continuous improving of STEMI care.
Testing and training
The app was extensively tested on different versions of both iOS and Android operating systems installed on a variety of mobile phones. User manuals were developed for each team, and in-person and/or online training sessions were conducted before the app launch.
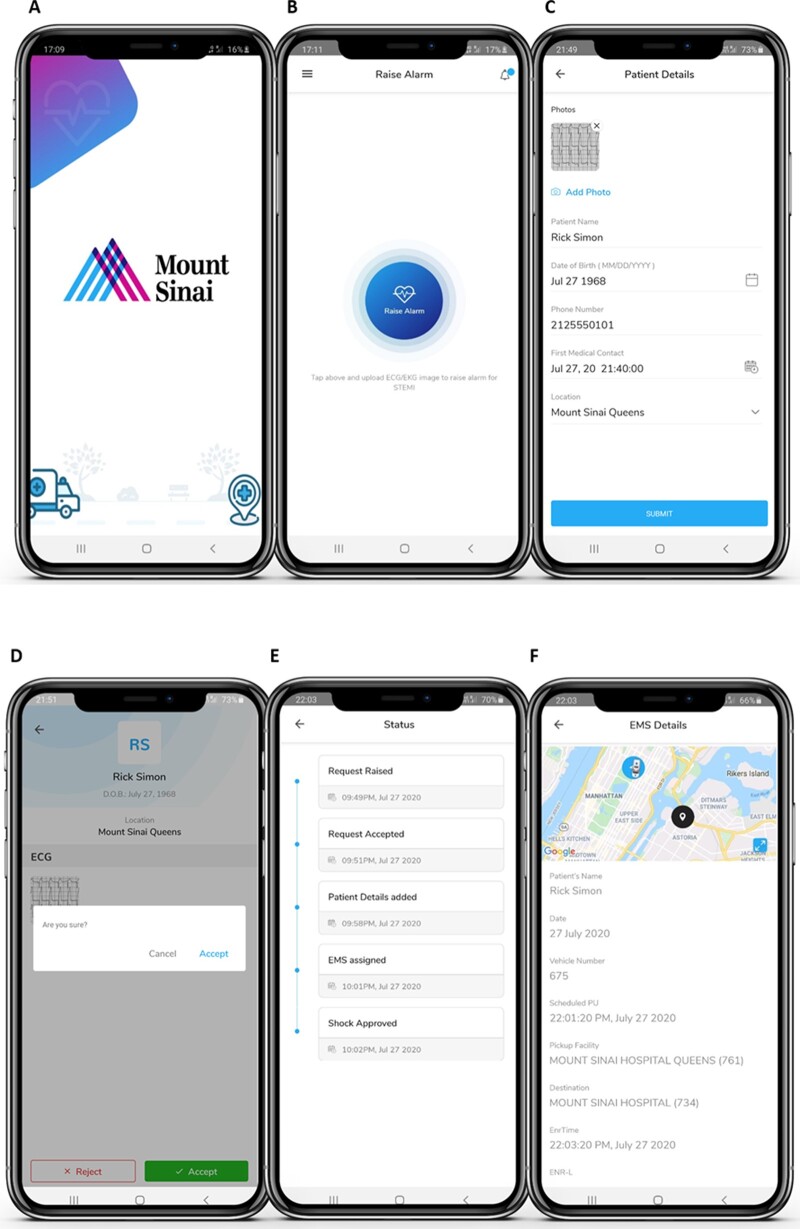
App launch
STEMIcathAID was launched as a pilot programme between Mount Sinai Queens (MSQ) hospital and the MSH CCL. MSQ does not have a CCL and nearly 150 STEMI patients are transferred every year from MSQ emergency room to the MSH CCL in Manhattan for PCI. The distance between the two hospitals is about 6 miles, but in typically heavy New York City traffic, transfers are often delayed creating challenges for our STEMI patients and the STEMI care team. The app was distributed between the STEMI care teams in the MSH CCL, MSQ ED, and transfer centre. The main steps of the test case included raising a STEMI alarm and entering the patient’s information by the ED attending in MSQ (Figure 5A–C), reviewing the information and confirming the request by the CCL attending (Figure 5D), assigning EMS by the transfer centre and ambulance tracking by all teams (Figure 5E and F), communication between the teams using HIPAA compliant chat (Figure 5G) and generating a shock notification (Figure 5H and J, red triangle next to the timer). The test case was continuously monitored through the web portal (Figure 6), which was also used for the patent’s discharge after PCI. All of the app’s functionalities were validated; mostly positive feedback was provided by participating parties with some suggestions for further improvements. As a result of the feedback, a dedicated and fully functional web portal role was created for the RN role, video chat was enabled before accepting a STEMI alert, and EMS tracking was enabled for all roles.
Figure 5.
STEMIcathAID launch. The app was launched as a pilot programme between Mount Sinai Queens (MSQ) hospital and the Mount Sinai Hospital CCL.
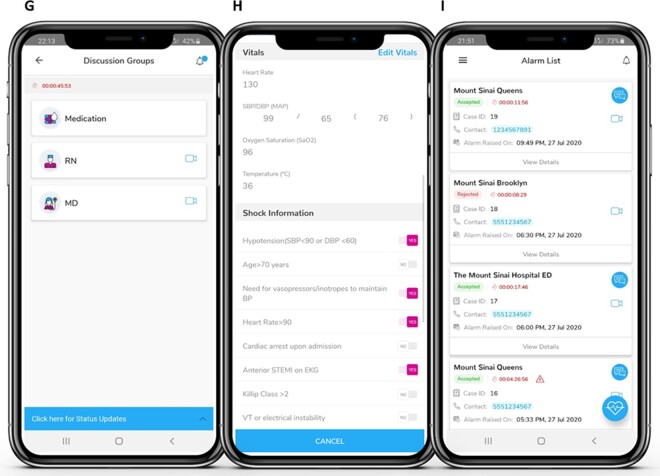
Figure 6.
The administrative portal of STEMIcathAID. Every STEMI case can be continuously monitored through the web portal (A), which is also used for the patent’s discharge after PCI (B).
Discussion
The study describes the rationale and design of a novel mobile application solution, STEMIcathAID, to optimize clinical workflows in the care of patients presenting with STEMI and CS (Graphical abstract). STEMIcathAID’s algorithmic approach helps improve coordination and communication essential to the rapid assessment and transfer of STEMI patients from the ED of a non-PCI facility to the CCL. The app includes EKG transmission and interpretation, CCL and transfer centre activation, multi-level alarm and notification system, secure video calls and chat between the team members, instantaneous updates on patient’s clinical status, and GPS coordinates of the ambulance. A running clock tracking the minutes and seconds from the FMC time is displayed next to the patient’s name to promote the sense of urgency in transferring the patient and meeting critical STEMI performance metrics. All patient data and key time points are captured automatically with robust HIPAA compliant safeguards by the app and can be extracted for internal QA reviews and for external reporting. In addition to CCL activation, the app automatically generates a shock notification, if clinical criteria for CS are met in order to facilitate the early recognition of CS in patients with STEMI, a group with especially high mortality. CS complicates STEMI in 5–10% of the cases20,21 and remains the major cause of death for patients hospitalized with acute myocardial infarction (MI).22 CS treatment requires a coordinated approach with multidisciplinary care in designated centres and substantial use of hospital resources.23 CS notification would allow for earlier case planning with regards to potential MCS to unload the ventricle prior to performing PCI on the culprit vessel. Reducing door to unload times and streamlining the use of left ventricular assist devices to help reverse the downward spiral of the neurohormonal shock cascade to improve patient outcomes, is a benefit of our app, which cannot be overstated.
Pre-activation of the CCL is one of the critical component of reducing treatment delays.24,25 CCL activation >10 min prior to hospital arrival was associated with a greater likelihood of achieving FMC ≤90 min and lower in-hospital mortality, but occurred in fewer than a half of emergency STEMI patients enrolled in the US REGISTRY study.26 While being an effective tool in minimizing time to reperfusion, CCL pre-hospital activation can lead to a greater frequency of false-positive activations. A retrospective evaluation of CCL activations for suspected STEMI found that only 71.6% of these patients received a final diagnosis of STEMI.10 Almost two-thirds (65.5%) of all activations occurred outside of normal working hours, during the night or on a weekend. A higher incidence of incorrect activation might lead to fatigue and ‘burn out’ among CCL physicians and staff and have a significant economic impact on the hospital.8 Our app can potentially reduce the incidence of incorrect CCL activations, since patients are screened by an interventional cardiologist as opposed to the ED staff.
Pre-hospital EKG acquisition and interpretation can reduce the incidence of inappropriate activations by to improving the accuracy of diagnosis and decision-making for CCL activation.8 Wireless EKG transmission to a cardiologist’s hand-held device significantly decreased ED door-to-reperfusion time compared to an EKG hand delivered with patient to the ED.27 Over the last decade, the use of telemedicine platforms for pre-hospital EKG transmission led to advancements in STEMI care (Table 1).13–15 The rate of inappropriate CCL activations was reduced to 4% in a study of 991patients with suspected STEMI pre-hospital diagnosed with telemedicine in a large centre in Denmark.15 In a meta-analysis of 7552 STEMI patients from five countries, pre-hospital EKG triage with telemedicine resulted in 40% reduction of time to treatment.13 The advantages of telemedicine in solving unique challenges of STEMI care in developing countries have been demonstrated by the Latin America Telemedicine Infarct Network (LATIN) and Rajasthan Heart Attack Treatment (RAHAT) programmes. Implementation of the programmes based on a hub and spoke model resulted in an increased accuracy of EKG interpretation from 40% to 95% and improved access to STEMI care and PCI for millions of patients in Latin America and India.28
A widely available communication platform, the WeChat app, was used for pre-hospital EKG transfer in a large urban PCI centre in China.16 A single STEMI group created within the app connected 158 doctors, nurses and technicians taking care of STEMI patients from seven non-PCI centres and CCL, which resulted in a high number of not relevant notifications for many participants around the clock. No patient information was shared in the app and all information regarding a case was deleted within two hours of the PCI. Despite the limitations, implementation of the technology into clinical practice resulted in a significant reduction of FMC-to-wire and door-to-wire time. First mobile application for STEMI management, STOP STEMI©, incorporated EKG transmission to all STEMI care team members, updates on the CCL readiness status and a universal clock comparing the current case against national standards.18 After implementing the app in a large healthcare system in the USA for patients presenting with STEMI to the ED, the hospital achieved a 22% reduction in the mean door-to-balloon time with an average difference of 20 min. Another mobile app, ‘STEMI’ (STEMI Global Ltd.), allowed voice consultation with a cardiologist in addition to an instantaneous EKG transmission by the EMS team.17 In case of confirmed STEMI, the patient was transported directly to the CCL and the app provides an automatic estimated time of arrival. The cardiologist’s phone can monitor the EMS vehicle position. The app was not been used for all STEMI patients, but rather in cases of diagnostic uncertainty, and the decision to use the app for remote EKG consultation was left to the EMS teams. Implementation of the ‘STEMI’ in a large area in Eastern Slovakia with a single PCI centre led to a significant reduction in the total ischaemic interval and decrease in unnecessary transportations to local non-PCI hospitals due to a limited ability of the EMS crew to interpret EKG. We believe that advanced functionalities of STEMIcathAID that allow to streamline the communication and coordination between all members of STEMI care team will result in significant reduction of system delays and improvement in patient outcomes. We intend to test the hypothesis in a study comparing patient outcomes, key times to reperfusion and other performance measures before and after implementation of the app in our clinical practice.
Since 2010, the AHA’s Mission: Lifeline programme has recognized hospitals for their outstanding performance in high-quality systems care performance by meeting or exceeding guideline therapy recommendations in treating patients presenting with STEMI. Recognition measures for STEMI receiving centres include the percentage of patients with aspirin on arrival, ‘arrival to PCI time’ and ‘FMC to PCI time’ under 90 min, percent of patients with aspirin, beta blocker statin, angiotensin-converting enzyme inhibitor/angiotensin II receptor blocker, smoking cessation counselling, and cardiac rehab referral on discharge among other performance metrics. STEMIcathAID not only automatically captures the critical time sensitive data before patient arrival to the CCL, but also allows tracking of important data elements, which will be entered to close the case prior to discharge (Supplementary material online, Table S1). With STEMIcathAID, each case provides instantaneous feedback and continuous education, and an opportunity to improve STEMI systems of care and outcomes for the multidisciplinary team caring for a vulnerable patient population. The aggregation of data in a single platform will allow us in the future to use a machine learning model to anticipate what factors lead to the best performance outcomes. A machine learning algorithm was recently used to estimate the probability of MI in patients with suspected MI in order to identify high-risk patients who may benefit from earlier clinical decisions.29 The novel risk assessment model performed better than the current ESC pathway and demonstrated for the first time the potential benefits of machine learning-based approaches to clinical decision-making for patients with suspected acute coronary syndrome. Patients presenting with STEMI were not included in the study and there has not been a previous attempt to use machine learning or artificial intelligence to further improve patients’ outcomes and resource allocation in STEMI care.
The validity of standardized STEMI performance metrics for inter-hospital transfer patients has been questioned in several studies. Many STEMI patients around the world continue to present to a non-PCI hospital first and require inter-hospital transfer even in areas with well-organized systems for direct triage to a PCI centre. While inter-hospital transfer for primary PCI inadvertently increases time to reperfusion, transfer patients have demonstrated significant differences in their clinical presentation compared to the direct access to CCL group.30,31 The inter-hospital transfer patients treated in a single centre in London had less severe symptoms and borderline EKGs.31 The group had longer symptom-call times (104 vs. 46 min, P < 0.0001), lower EKG ST-elevation scores (3.0 vs. 5.0, P < 0.0001), and a four-fold increase in protocol negative EKGs at presentation (31.6 vs. 9.4%, P < 0.0001). The findings suggest that Reperfusion delays due to inter-hospital transfer are not always ‘system failures’, but rather delays caused by the diagnostic uncertainty. STEMIcathAID can potentially reduce the delays in the cases requiring additional diagnostic testing by providing communication platform for STEMI care teams essential to the rapid assessment of inter-hospital transfer patients.
Our current goal is to begin transferring STEMI patients from all Mount Sinai Healthcare System hospitals to test the capabilities of STEMIcathAID platform to improve STEMI care. The application will later be rolled out to test other transfer pathways including EMS and 30-day patient outcomes data collection. We are also contemplating including additional metrics and strategies, such as ED Bypass, that would contribute to reducing FMC-to-device time. We believe that integration of STEMIcathAID into clinical practice will provide a unique opportunity to improve STEMI systems of care and improve patient outcomes.
Limitations
The current version of STEMIcathAID does not provide EMS integration, which will be implemented in the future and would require extensive training of a large number of personnel. There is also no integration with electronic medical record systems, a desirable future expansion of the app. The app is HIPAA compliant, but will need to ensure General Data Protection Regulation (GDPR) compliance in case of adoption in European Union. Brief training of staff will be required in each hospital in order to fully understand the features and functionalities of the application. The expected cost savings from reducing false CCL activations, better data management and improvements in patient outcomes will not be achieved immediately, but rather over time.
Supplementary material
Supplementary material is available at European Heart Journal – Digital Health online.
Conflict of interest: N.B. reports speaker/consultant fees from Boston Scientific, Cardiovascular Systems, Inc., and Terumo Medical. U.B. has received speaker honoraria from AstraZeneca, Amgen, and Boston Scientific. G.D. has received consulting fees or honoraria from AstraZeneca, Biosensors, Boston Scientific, and Medtronic; is on the Advisory Board of Abbott Laboratories and Boston Scientific; has received research grants to the institution from Biotronik and Abbott Laboratories; and has equity (entirely divested) in Medtronic. S.K.S. reports honoraria from Abbot Vascular, Boston Scientific, and Cardiovascular Systems, Inc. for Speaker’s Bureau. All other authors have declared no conflict of interest.
Data availability
The data underlying this article are available in the article and in its online supplementary material.
Supplementary Material
References
- 1. Denktas AE, Anderson HV, McCarthy J, Smalling RW.. Total ischemic time: the correct focus of attention for optimal ST-segment elevation myocardial infarction care. JACC Cardiovasc Interv 2011;4:599–604. [DOI] [PubMed] [Google Scholar]
- 2. Terkelsen CJ, Sorensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, Vach W, Johnsen SP, Thuesen L, Lassen JF.. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA 2010;304:763–771. [DOI] [PubMed] [Google Scholar]
- 3. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimsky P.. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Rev Esp Cardiol (Engl Ed) 2017;70:1082. [DOI] [PubMed] [Google Scholar]
- 4. Jneid H, Addison D, Bhatt DL, Fonarow GC, Gokak S, Grady KL, Green LA, Heidenreich PA, Ho PM, Jurgens CY, King ML, Kumbhani DJ, Pancholy S.. 2017 AHA/ACC Clinical performance and quality measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. Circ Cardiovasc Qual Outcomes 2017;10:e000032. [DOI] [PubMed] [Google Scholar]
- 5. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX.. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2013;61:e78–e140. [DOI] [PubMed] [Google Scholar]
- 6.Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC)Steg PG, James SK, Atar D, Badano LP, Blomstrom-Lundqvist C, Borger MA, Di Mario C, Dickstein K, Ducrocq G, Fernandez-Aviles F, Gershlick AH, Giannuzzi P, Halvorsen S, Huber K, Juni P, Kastrati A, Knuuti J, Lenzen MJ, Mahaffey KW, Valgimigli M, van 't Hof A, Widimsky P, Zahger D.. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J 2012;33:2569–2619. [DOI] [PubMed] [Google Scholar]
- 7. Jacobs AK, Antman EM, Faxon DP, Gregory T, Solis P.. Development of systems of care for ST-elevation myocardial infarction patients: executive summary. Circulation 2007;116:217–230. [DOI] [PubMed] [Google Scholar]
- 8. Kontos MC, Gunderson MR, Zegre-Hemsey JK, Lange DC, French WJ, Henry TD, McCarthy JJ, Corbett C, Jacobs AK, Jollis JG, Manoukian SV, Suter RE, Travis DT, Garvey JL.. Prehospital activation of hospital resources (PreAct) ST-segment-elevation myocardial infarction (STEMI): a standardized approach to prehospital activation and direct to the catheterization laboratory for STEMI recommendations from the American Heart Association's Mission: Lifeline Program. J Am Heart Assoc 2020;9:e011963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. O'Gara PT, Kushner FG, Ascheim DD, Casey DE Jr, Chung MK, de Lemos JA, Ettinger SM, Fang JC, Fesmire FM, Franklin BA, Granger CB, Krumholz HM, Linderbaum JA, Morrow DA, Newby LK, Ornato JP, Ou N, Radford MJ, Tamis-Holland JE, Tommaso CL, Tracy CM, Woo YJ, Zhao DX, Anderson JL, Jacobs AK, Halperin JL, Albert NM, Brindis RG, Creager MA, DeMets D, Guyton RA, Hochman JS, Kovacs RJ, Kushner FG, Ohman EM, Stevenson WG, Yancy CW; American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation 2013;127:e362–e425. [DOI] [PubMed] [Google Scholar]
- 10. Mixon TA, Suhr E, Caldwell G, Greenberg RD, Colato F, Blackwell J, Jo CH, Dehmer GJ.. Retrospective description and analysis of consecutive catheterization laboratory ST-segment elevation myocardial infarction activations with proposal, rationale, and use of a new classification scheme. Circ Cardiovasc Qual Outcomes 2012;5:62–69. [DOI] [PubMed] [Google Scholar]
- 11. McCabe JM, Armstrong EJ, Kulkarni A, Hoffmayer KS, Bhave PD, Garg S, Patel A, MacGregor JS, Hsue P, Stein JC, Kinlay S, Ganz P.. Prevalence and factors associated with false-positive ST-segment elevation myocardial infarction diagnoses at primary percutaneous coronary intervention-capable centers: a report from the Activate-SF registry. Arch Intern Med 2012;172:864–871. [DOI] [PubMed] [Google Scholar]
- 12. Degheim G, Berry A, Zughaib M.. False activation of the cardiac catheterization laboratory: The price to pay for shorter treatment delay. JRSM Cardiovasc Dis 2019;8:2048004019836365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Brunetti ND, De Gennaro L, Correale M, Santoro F, Caldarola P, Gaglione A, Di Biase M.. Pre-hospital electrocardiogram triage with telemedicine near halves time to treatment in STEMI: a meta-analysis and meta-regression analysis of non-randomized studies. Int J Cardiol 2017;232:5–11. [DOI] [PubMed] [Google Scholar]
- 14. Kawakami S, Tahara Y, Noguchi T, Yagi N, Kataoka Y, Asaumi Y, Nakanishi M, Goto Y, Yokoyama H, Nonogi H, Ogawa H, Yasuda S.. Time to reperfusion in ST-segment elevation myocardial infarction patients with vs. without pre-hospital mobile telemedicine 12-lead electrocardiogram transmission. Circ J 2016;80:1624–1633. [DOI] [PubMed] [Google Scholar]
- 15. Rasmussen MB, Frost L, Stengaard C, Brorholt-Petersen JU, Dodt KK, Sondergaard HM, Terkelsen CJ.. Diagnostic performance and system delay using telemedicine for prehospital diagnosis in triaging and treatment of STEMI. Heart 2014;100:711–715. [DOI] [PubMed] [Google Scholar]
- 16. Liu H, Wang W, Chen H, Li Z, Feng S, Yuan Y.. Can WeChat group-based intervention reduce reperfusion time in patients with ST-segment myocardial infarction? A controlled before and after study. J Telemed Telecare 2020;26:627–637. [DOI] [PubMed] [Google Scholar]
- 17. Studencan M, Alusik D, Plachy L, Bajerovska L, Ilavsky M, Karas J, Kilianova A, Sykora J, Hosa V, Kmec J, Slanina M, Boguska D.. Significant benefits of new communication technology for time delay management in STEMI patients. PLoS One 2018;13:e0205832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Dickson R, Nedelcut A, Seupaul R, Hamzeh M.. STOP STEMI©—a novel medical application to improve the coordination of STEMI care: a brief report on door-to-balloon times after initiating the application. Crit Pathw Cardiol 2014;13:85–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bhatheja S, Fuster V, Chamaria S,, Kakkar S, Zlatopolsky R, Rogers J, Otobo E, Atreja A,, Sharma SK, Kini AS.. Developing a mobile application for global cardiovascular education. J Am Coll Cardiol 2018;72:2518–2527. [DOI] [PubMed] [Google Scholar]
- 20. Goldberg RJ, Samad NA, Yarzebski J, Gurwitz J, Bigelow C, Gore JM.. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N Engl J Med 1999;340:1162–1168. [DOI] [PubMed] [Google Scholar]
- 21. Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, Jain D, Gotsis W, Ahmed A, Frishman WH, Fonarow GC.. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc 2014;3:e000590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hochman JS, Sleeper LA, Webb JG, Dzavik V, Buller CE, Aylward P, Col J, White HD, Investigators S. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA 2006;295:2511–2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. van Diepen S, Katz JN, Albert NM, Henry TD, Jacobs AK, Kapur NK, Kilic A, Menon V, Ohman EM, Sweitzer NK, Thiele H, Washam JB, Cohen MG; American Heart Association Council on Clinical Cardiology; Council on Cardiovascular and Stroke Nursing; Council on Quality of Care and Outcomes Research; and Mission: Lifeline. Contemporary management of cardiogenic shock: a scientific statement from the American Heart Association. Circulation 2017;136:e232–e268. [DOI] [PubMed] [Google Scholar]
- 24. Fordyce CB, Al-Khalidi HR, Jollis JG, Roettig ML, Gu J, Bagai A, Berger PB, Corbett CC, Dauerman HL, Fox K, Garvey JL, Henry TD, Rokos IC, Sherwood MW, Wilson BH, Granger CB; STEMI Systems Accelerator Project. Association of rapid care process implementation on reperfusion times across multiple ST-segment-elevation myocardial infarction networks. Circ Cardiovasc Interv 2017;10:e004061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Squire BT, Tamayo-Sarver JH, Rashi P, Koenig W, Niemann JT.. Effect of prehospital cardiac catheterization lab activation on door-to-balloon time, mortality, and false-positive activation. Prehosp Emerg Care 2014;18:1–8. [DOI] [PubMed] [Google Scholar]
- 26. Shavadia JS, Roe MT, Chen AY, Lucas J, Fanaroff AC, Kochar A, Fordyce CB, Jollis JG, Tamis-Holland J, Henry TD, Bagai A, Kontos MC, Granger CB, Wang TY.. Association between cardiac catheterization laboratory pre-activation and reperfusion timing metrics and outcomes in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention: a report from the ACTION Registry. JACC Cardiovasc Interv 2018;11:1837–1847. [DOI] [PubMed] [Google Scholar]
- 27. Adams GL, Campbell PT, Adams JM, Strauss DG, Wall K, Patterson J, Shuping KB, Maynard C, Young D, Corey C, Thompson A, Lee BA, Wagner GS.. Effectiveness of prehospital wireless transmission of electrocardiograms to a cardiologist via hand-held device for patients with acute myocardial infarction (from the Timely Intervention in Myocardial Emergency, NorthEast Experience [TIME-NE]). Am J Cardiol 2006;98:1160–1164. [DOI] [PubMed] [Google Scholar]
- 28. Mehta S, Botelho R, Cade J, Perin M, Bojanini F, Coral J, Parra D, Ferre A, Castillo M, Yepez P.. Global challenges and solutions: role of telemedicine in ST-elevation myocardial infarction interventions. Interv Cardiol Clin 2016;5:569–581. [DOI] [PubMed] [Google Scholar]
- 29. Than MP, Pickering JW, Sandoval Y, Shah ASV, Tsanas A, Apple FS, Blankenberg S, Cullen L, Mueller C, Neumann JT, Twerenbold R, Westermann D, Beshiri A, Mills NL; MI3 collaborative. Machine learning to predict the likelihood of acute myocardial infarction. Circulation 2019;140:899–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Miedema MD, Newell MC, Duval S, Garberich RF, Handran CB, Larson DM, Mulder S, Wang YL, Lips DL, Henry TD.. Causes of delay and associated mortality in patients transferred with ST-segment-elevation myocardial infarction. Circulation 2011;124:1636–1644. [DOI] [PubMed] [Google Scholar]
- 31. Tarkin J, Malhotra A, Apps A, Smith R, Di Mario C, Rogers P, Lane R, Kabir T, Mason M, Ilsley C, Whitbread M, Dalby M.. Inter-hospital transfer for primary angioplasty: delays are often due to diagnostic uncertainty rather than systems failure and universal time metrics may not be appropriate. EuroIntervention 2015;11:511–517. [DOI] [PubMed] [Google Scholar]
- 32. Goebel M, Bledsoe J.. Push notifications reduce emergency department response times to prehospital ST-segment elevation myocardial infarction. West J Emerg Med 2019;20:212–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Nan J, Meng S, Hu H, Jia R, Chen W, Li Q, Zhang T, Song K, Wang Y, Jin Z.. Comparison of clinical outcomes in patients with ST elevation myocardial infarction with percutaneous coronary intervention and the use of a telemedicine app before and after the COVID-19 Pandemic at a Center in Beijing, China, from August 2019 to March 2020. Med Sci Monit 2020;26:e927061. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article are available in the article and in its online supplementary material.