Abstract
Patients with congenital heart disease (CHD) are a vulnerable subgroup of cardiac patients. These patients have a high morbidity and high mortality rate. As the number of patients with CHD keeps growing, while also getting older, new tools for the care and follow-up of these vulnerable patients are warranted. eHealth has an enormous potential to revolutionize health care, and particularly for CHD patients, by expanding care beyond hospital walls and even moving some of the provided care to the comfort of home. As new eHealth tools continue to grow in number, such as invasive eHealth tools, health care delivered through eHealth continues to evolve. This teaching series summarizes current insights and discusses challenges yet to be overcome. Importantly, none of them are insurmountable. This all lays ground for a promising future for eHealth in the care of patients with CHD.
Keywords: Telemedicine, Heart disease, eHealth, Congenital heart disease, ACHD
Graphical Abstract
Introduction
eHealth is rapidly developing and innovative technical applications and solutions continue to grow in number. Some highly anticipated technologies, such as remote monitoring of patients with acquired heart failure or arrhythmias, have initially shown disappointing results in large randomized controlled trials in terms of reducing mortality and hospitalizations.1 However, recently a large randomized controlled trial on telemonitoring in patients with acquired heart failure demonstrated a reduction of mortality in highly selected patients.2 These patients were being monitored at home 24 h a day, 7 days a week, resulting in an intensive and costly telemonitoring programme. Nonetheless, these positive results indicate that eHealth is gradually evolving and learning from its past mistakes.
Patients with congenital heart disease (CHD) are a vulnerable subgroup of cardiac patients. These patients have a high morbidity and high mortality rate. As the number of patients with CHD keeps growing, while also getting older, new tools for the care and follow-up of these vulnerable patients are warranted.
Until recently, limited data were available on the effects of eHealth on clinical outcomes in CHD patients. This Teaching is a brief update on current applications and future perspectives of eHealth in the care of adult patients with CHD. We describe advantages and challenges of eHealth in CHD patients and identified patients with a high risk for clinical deterioration, who might benefit most from using eHealth. The relatively young adult CHD population only rarely uses mHealth, but the majority demonstrated in questionnaires to be motivated to start using eHealth, see Figure 1.3 Particularly the adult CHD population is a highly attractive patient group in which to initiate mHealth initiatives due to their relatively young age, affinity with mobile devices, chronic condition necessitating lifelong surveillance, and the general need to reduce the burden of disease.3 In a questionnaire study with a median age of 40 (range 18–78) years, 92 % owned a smartphone.3 In a similar study by Lopez et al.4 among adolescents (between 16 and 20 years of age) and adults (21–40 years of age) with moderate or complex CHD, all had access to the Internet via a mobile phone, and 55% had searched online for information on CHD.
Figure 1.
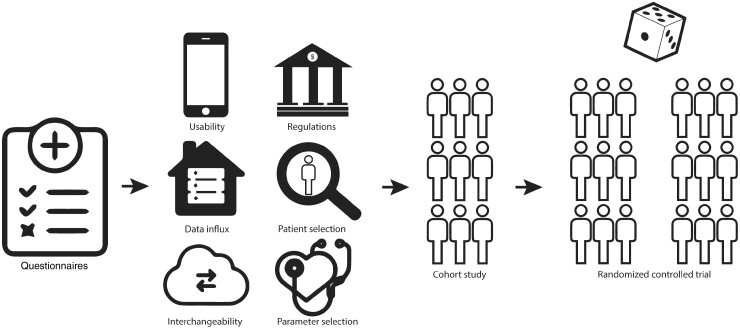
Graphical abstract on how to initiate eHealth in congenital heart disease patients?
Current insights
Kauw et al.5 reviewed the medical literature and showed that only limited data were available on the use of eHealth applications in CHD patients. Most studies focused on paediatric patients. The most frequently used application of eHealth in CHD patients was home-monitoring of body weight and oxygen saturation in infants in between corrective surgery, which showed positive results in reducing mortality rate, complications, and improving nutritional status. These results demonstrated that using eHealth applications in CHD patients seems promising and should be further explored.
One of the first steps to develop and implement a new technique such as eHealth is a stakeholder analysis, see Figure 1. In the Netherlands, a dedicated stakeholder analysis was performed to evaluate experiences of users of eHealth telemonitoring programmes to identify the challenges that have to be overcome to improve success rates of future eHealth programmes in adult CHD patients.6 Semi-structured interviews were conducted with cardiologists, nurses, patients, health care managers, and Information Communication Technology (ICT)-developers in order to identify the main hurdles of these programmes. Interestingly, different challenges were experienced in the various subgroups, indicating that collaboration between all involved parties is essential for a successful integration of an eHealth programme.
The next logical step in the evaluation of eHealth care in adults with CHD is an observational cohort study, see Figure 1. We performed a clinical cohort study in which adult CHD patients were enrolled in an eHealth programme.7 Adult CHD patients were eligible for inclusion if they met the inclusion criteria: Palpitations within the last 3 years (with or without arrhythmia diagnosis) or heart failure (HF) New York Heart Association (NYHA) class≥II, and possession of a mobile device. Symptomatic patients were included, as the most benefit could be expected within this patient group. It is unclear what the effects of screening are in asymptomatic patients. This programme included weekly monitoring body weight, blood pressure, and heart rhythm. In this study, we demonstrated several clinical advantages of the eHealth programme, as we established new diagnoses of arrhythmias and hypertension, and medication adjustments were required in between outpatient clinic visits. Importantly, adherence was >70% in 77% of the patients that started weekly measurements (70/91). Patients that were female, older of age, and experienced palpitations at inclusion were more likely to acquire an adherence of >70%. These results are much better than adherence reported by Klausen et al.8 Of 81 patients in an eHealth intervention group (mean age 14.6 years), only 8 (10%) were active users during the last week of the intervention. The Dutch programme did not find any differences in clinical outcomes with respect to hospital admissions, emergency hospital visits, and telephone contacts. As this cohort study used historical data, these results have to be interpreted with caution. Therefore, randomized controlled trials are required to further elucidate the effect of eHealth programmes on clinical outcomes in CHD patients, see Figure 1.
Discussion
For eHealth to be effective in the care of CHD patients, a few challenges still remain, such as usability of an eHealth tool, analysis of patient-generated data, interchangeability of data between different electronic medical records (EMR), adaptation of legal and financial regulations, identification of patients that will benefit most, and identification of parameters that are most indicative for the detection of clinical deterioration.
Firstly, using an eHealth device or application has to be straightforward for patients, as well as health care professionals. This challenge emerged from our stakeholder analysis, but is also demonstrated by other studies, especially in older patients.9,10 A possible solution to this problem could be the automated collection of patient data (e.g. heart rate frequency monitoring by a smartwatch), which never misses a measurement if set-up correctly and happens unnoticed by the patient. This way challenges such as usability, but also patient adherence and medicalization of the patient can be overcome. Potentially, reminders or serious gaming affects adherence.11 Examples of devices that automatically and unnoticed gather patient data are wearables or implantable devices, such as smartwatches or an implantable pulmonary artery pressure monitor device.12
Secondly, for health care professionals, the huge influx of patient-generated data is feared because this is thought to generate more workload, as all patient-generated data has to be analysed by physicians or nurses to prevent missing clinically significant information.13 To automate the analysis of patient-generated data, machine learning techniques are currently being studied. These techniques are not yet used on a large scale in clinical practice, but it can be expected that these new techniques will provide accurate analysis of data and will reliably take over more and more of the workload of health care professionals.14
Thirdly, an important challenge for health care professionals, but also for ICT-developers, is the interchangeability of (patient-generated) data between different EMR systems.15 Currently, in many countries, it is not yet possible to exchange data of the same patient between different EMR systems. In daily clinical practice, this is experienced as a major limitation. Therefore, for eHealth to be a success, adequate implementation in all different EMR systems and interchangeability of data between these systems is essential.
Fourthly, adapting financial and legal regulations to the use of eHealth in daily practice remains a challenge. Reimbursement of these new-developed forms of care, delivered through remote monitoring, was a pressing issue when the first eHealth programmes started and reimbursement by health care insurances only gradually took shape in the Netherlands. This hindered innovative eHealth programmes initially, however, health insurance companies and governmental regulations are now quickly adapting. Another issue in adapting regulations to eHealth is the legal side of this new concept of healthcare. For example, privacy of patient-generated data has to be guaranteed and liability in case of adverse events has to be regulated by law. Adequate legal and reimbursement regulations have to be continuously updated to keep up with recent technical innovations and to prevent a delay between innovation of healthcare and actually using it in daily clinical practice.
Fifthly, and probably one of the most important issues, is that the appropriate and most eligible patient groups have to be identified for the use of specific eHealth applications. Just applying eHealth to the whole CHD patient population is expected to not be effective, as severity of diagnosis and clinical status can differ greatly between patients. This has also been demonstrated in patients with acquired heart disease in patients with HF. Adequate patient selection is required to significantly improve the effectiveness and success of eHealth applications. We opted for symptomatic patients, because this is where the most benefits could be expected. However, this is subject of debate. A substantial number of CHD are associated with other features, including mental retardation.16 Most studies excluded patients with mental retardation, because the effect of eHealth is uncertain in this group.
Finally, similar to eligible patient identification, identifying the most adequate and effective parameters to monitor in patients and detect early signs of deterioration is of great importance for the success of eHealth. Multiple studies have, for example, studied monitoring weight in acquired HF patients in order to detect deterioration, but with limited rates of success.2,17
Future expectations
New ways of monitoring patients with HF at home have emerged, such as invasive monitoring of the pulmonary artery pressure through an implemented device in the pulmonary artery.18 Also home testing of B-type natriuretic peptide has been studied to predict HF decompensation.19 These new parameters seem promising as they are believed to be more accurate in predicting HF decompensation than weight gain, however, large randomized trials still need to confirm this. As technical innovation increases the number of possible parameters to monitor, evaluation of these parameters should continue, not only for HF, but also for other (cardiac) diseases.
Conclusion
eHealth has an enormous potential to revolutionize health care, and particularly for CHD patients, by expanding care beyond hospital walls and even moving some of the provided care to the comfort of home. As new eHealth tools continue to grow in number, such as invasive eHealth tools, health care delivered through eHealth continues to evolve. Some of the discussed challenges have yet to be overcome, however, none of them are insurmountable. This all lays ground for a promising future for eHealth in the care of patients with CHD.
Funding
This work was supported by the Dutch Heart Foundation [grant number 2017 T2] and Dutch Federation of University Medical Centers (NFU).
Conflict of interest: The authors declare that there is no conflict of interest.
Data Availability
No new data were generated or analysed in support of this research
References
- 1. Hindricks G, Taborsky M, Glikson M, Heinrich U, Schumacher B, Katz A, Brachmann J, Lewalter T, Goette A, Block M, Kautzner J, Sack S, Husser D, Piorkowski C, Søgaard P, IN-TIME Study Group. Implant-based multiparameter telemonitoring of patients with heart failure (IN-TIME): a randomised controlled trial. Lancet Lond Engl 2014;384:583–590. [DOI] [PubMed] [Google Scholar]
- 2. Koehler F, Koehler K, Deckwart O, Prescher S, Wegscheider K, Kirwan B-A, Winkler S, Vettorazzi E, Bruch L, Oeff M, Zugck C, Doerr G, Naegele H, Störk S, Butter C, Sechtem U, Angermann C, Gola G, Prondzinsky R, Edelmann F, Spethmann S, Schellong SM, Schulze PC, Bauersachs J, Wellge B, Schoebel C, Tajsic M, Dreger H, Anker SD, Stangl K.. Efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet Lond Engl 2018;392:1047–1057. [DOI] [PubMed] [Google Scholar]
- 3. Schuuring MJ, Backx AP, Zwart R, Veelenturf AH, Robbers-Visser D, Groenink M, Abu-Hanna A, Bruining N, Schijven MP, Mulder BJ, Bouma BJ.. Mobile health in adults with congenital heart disease: current use and future needs. Neth Heart J Mon J Neth Soc Cardiol Neth Heart Found 2016;24:647–652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Lopez KN, Karlsten M, Bonaduce De Nigris F, King J, Salciccioli K, Jiang A, Marelli A, Kovacs AH, Fordis M, Thompson D.. Understanding age-based transition needs: perspectives from adolescents and adults with congenital heart disease. Congenit Heart Dis 2015;10:561–571. [DOI] [PubMed] [Google Scholar]
- 5. Kauw D, Koole MAC, van Dorth JR, Tulevski II, Somsen GA, Schijven MP, Dohmen DAJ, Bouma BJ, Mulder BJM, Schuuring MJ, Winter MM.. eHealth in patients with congenital heart disease: a review. Expert Rev Cardiovasc Ther 2018;16:627–634. [DOI] [PubMed] [Google Scholar]
- 6. Kauw D, Huisma PR, Medlock SK, Koole MAC, Wierda E, Abu-Hanna A, Schijven MP, Mulder BJM, Bouma BJ, Winter MM, Schuuring MJ.. Mobile health in cardiac patients: an overview on experiences and challenges of stakeholders involved in daily use and development. BMJ Innov; 2020;6:184–191. [Google Scholar]
- 7. Kauw D, Koole MAC, Winter MM, Dohmen DAJ, Tulevski II, Blok S, Somsen GA, Schijven MP, Vriend JWJ, Robbers-Visser D, Mulder BJM, Bouma BJ, Schuuring MJ.. Advantages of mobile health in the management of adult patients with congenital heart disease. Int J Med Inf 2019;132:104011. [DOI] [PubMed] [Google Scholar]
- 8. Klausen SH, Andersen LL, Søndergaard L, Jakobsen JC, Zoffmann V, Dideriksen K, Kruse A, Mikkelsen UR, Wetterslev J.. Effects of eHealth physical activity encouragement in adolescents with complex congenital heart disease: the PReVaiL randomized clinical trial. Int J Cardiol 2016;221:1100–1106. [DOI] [PubMed] [Google Scholar]
- 9. Lee C, Coughlin JF.. Perspective: older adults’ adoption of technology: an integrated approach to identifying determinants and barriers. J Prod Innov Manag 2015;32:747–759. [Google Scholar]
- 10. Grindrod KA, Li M, Gates A.. Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR MHealth UHealth 2014;2:e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Abraham O, LeMay S, Bittner S, Thakur T, Stafford H, Brown R.. Investigating serious games that incorporate medication use for patients: systematic literature review. JMIR Serious Games 2020;8:e16096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Perez MV, Mahaffey KW, Hedlin H, Rumsfeld JS, Garcia A, Ferris T, Balasubramanian V, Russo AM, Rajmane A, Cheung L, Hung G, Lee J, Kowey P, Talati N, Nag D, Gummidipundi SE, Beatty A, Hills MT, Desai S, Granger CB, Desai M,, Turakhia MP, Apple Heart Study Investigators. Large-scale assessment of a smartwatch to identify atrial fibrillation. N Engl J Med 2019;381:1909–1917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Granja C, Janssen W, Johansen MA.. Factors determining the success and failure of ehealth interventions: systematic review of the literature. J Med Internet Res 2018;20:e10235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Shameer K, Johnson KW, Glicksberg BS, Dudley JT, Sengupta PP.. Machine learning in cardiovascular medicine: are we there yet? Heart 2018;104:1156–1164. [DOI] [PubMed] [Google Scholar]
- 15. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M.. Evaluating barriers to adopting telemedicine worldwide: a systematic review. J Telemed Telecare 2018;24:4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kauw D, Woudstra OI, van Engelen K, Meijboom FJ, Mulder BJM, Schuuring MJ, Bouma BJ.. 22q11.2 deletion syndrome is associated with increased mortality in adults with tetralogy of Fallot and pulmonary atresia with ventricular septal defect. Int J Cardiol 2020;306:56–60. [DOI] [PubMed] [Google Scholar]
- 17. Inglis SC, Clark RA, Dierckx R, Prieto-Merino D, Cleland JGF.. Structured telephone support or non-invasive telemonitoring for patients with heart failure. Heart 2017;103:255–257. [DOI] [PubMed] [Google Scholar]
- 18. Ayyadurai P, Alkhawam H, Saad M, Al-Sadawi MA, Shah NN, Kosmas CE, Vittorio TJ.. An update on the CardioMEMS pulmonary artery pressure sensor. Ther Adv Cardiovasc Dis 2019;13:1753944719826826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Maisel A, Barnard D, Jaski B, Frivold G, Marais J, Azer M, Miyamoto MI, Lombardo D, Kelsay D, Borden K, Iqbal N, Taub PR, Kupfer K, Clopton P, Greenberg B.. Primary results of the HABIT Trial (heart failure assessment with BNP in the home). J Am Coll Cardiol 2013;61:1726–1735. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No new data were generated or analysed in support of this research