Dear Editor,
With the coronavirus disease 2019 (COVID-19) pandemic, families of intensive care unit (ICU) patients witnessed practice changes, such as the prohibition of hospital visits and reduced opportunities to see attending physicians [1]. Such changes might affect the mental status of a patient’s family, but previous studies were limited by the lack of controls [2, 3]. Moreover, it remains unclear whether the increased mental disorders were due to the COVID-19 pandemic itself or COVID-19 pandemic-related changes in ICU care for a family. Therefore, we aimed to examine the impact of COVID-19 pandemic-related changes in ICU care for the family on the mental status of spouses of ICU patients using a controlled interrupted time series design.
We used data on married couples from a large commercially available Japanese administrative database from DeSC Healthcare Inc. Tokyo, Japan, from April 1, 2019 to February 28, 2021. The study period was split into before and during the COVID-19 pandemic on April 1, 2020. Using the risk set matched-pair sampling method, we created matched pairs (1 case:10 controls) with cases being the spouse of a patient admitted to ICU and controls being spouses (matched by birth month and year, sex, and medical insurance status) of individuals who had not experienced ICU admission on the date of ICU admission for the case before and after April 1, 2020 (before COVID-19 and during COVID-19). The main outcome was the incidence of mental disorders within 90 days of the date of ICU admission for the cases. We conducted a controlled interrupted time series analysis that involved both before and during the COVID-19 pandemic comparison and comparison between spouses of ICU patients and matched controls [4]. Details are available in Supplemental Material.
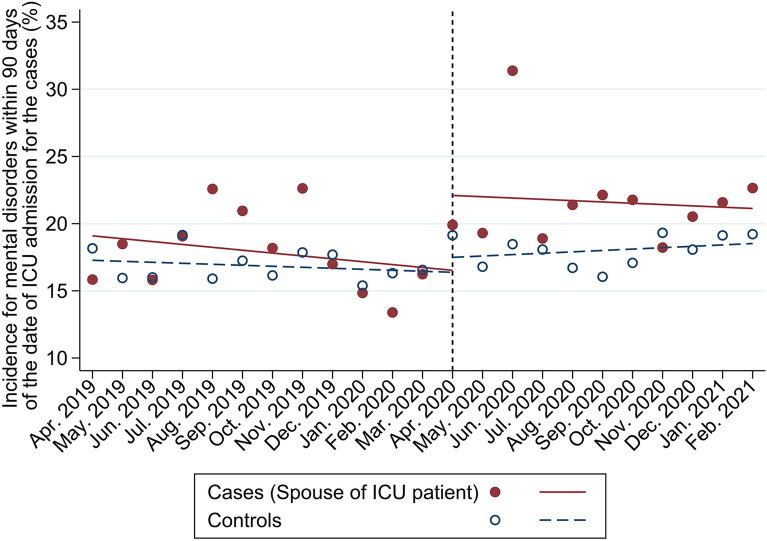
Among 483,768 eligible spouses, we identified 5524 (1.1%) patients who were admitted to the ICU, and 5190 cases matched with 51,603 controls. Incidence of mental disorders within 90 days of the date of ICU admission for the cases was observed in 17.9% and 21.5% of the cases before and during the COVID-19 pandemic, respectively, and in 17% and 17.5% of the controls, respectively. The controlled interrupted time series analysis showed an upward level change in the cases compared with the controls during the COVID-19 pandemic (+ 4.5%, 95% confidence intervals + 0.01% to + 8.98%) (Fig. 1).
Fig. 1.
Change in the incidence of mental disorders before and during the COVID-19 pandemic in spouses of ICU patients and matched controls. Points represent the mean percentage of incidence of mental disorders within 90 days of the date of ICU admission for the cases in each month. Solid and dashed lines represent the predicted outcomes using controlled interrupted time-series analysis. April 2019 through March 2020 was the period before the COVID-19 pandemic, and April 2020 through February 2021 was the period during the COVID-19 pandemic. The red points and red solid lines represent the spouses of the ICU patient group and the blue points and blue dashed lines represent the matched control group. ICU intensive care unit; COVID-19 coronavirus disease 2019
To our knowledge, this study is the first that examines the association between mental disorders in spouses of ICU patients and the COVID-19 pandemic by using a before-after design and by establishing an appropriate control. Although the present study had limitations (Supplemental Material), the controlled interrupted time series analyses results can provide strong evidence on public health events and rank second to randomized controlled designs in terms of its ability to control for bias [4]. Therefore, the observed increase in mental disorders among spouses of ICU patients calls for further studies to develop effective strategies, such as addressing barriers to care for family members of ICU patients using emerging technologies or investigating the health policy effectiveness of reopening ICU [5].
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
HO conceived the study idea. HO and TG designed the study. HO processed the corrected data. HO and HY analyzed the data. All authors interpreted the data. HO and TG wrote the initial draft of the manuscript. All authors revised the manuscript for intellectual content and approved the final version. HO was the guarantor of this study. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted.
Funding
None.
Data availability
The datasets analyzed in the current study are not publicly available because of contracts with the hospitals providing data to the database. All codes used in the current study are available from the corresponding author on reasonable request.
Declarations
Conflicts of interest
The authors report no personal conflicts of interest pertaining to this work.
Ethical approval
The Institutional Review Board of The University of Tokyo approved this study. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent to participate
Because the data were anonymized before the researchers received them, the requirement for informed consent was waived by the Institutional Review Board of The University of Tokyo.
Consent to publish
All authors approved the final version of the manuscript submitted for publication.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Aziz S, Arabi YM, Alhazzani W, et al. Managing ICU surge during the COVID-19 crisis: rapid guidelines. Intensive Care Med. 2020;46:1303–1325. doi: 10.1007/s00134-020-06092-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heesakkers H, van der Hoeven JG, Corsten S, et al. Mental health symptoms in family members of COVID-19 ICU survivors 3 and 12 months after ICU admission: a multicentre prospective cohort study. Intensive Care Med. 2022;48:322–331. doi: 10.1007/s00134-021-06615-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rose L, Cook A, Onwumere J, et al. Psychological distress and morbidity of family members experiencing virtual visiting in intensive care during COVID-19: an observational cohort study. Intensive Care Med. 2022;48:1156–1164. doi: 10.1007/s00134-022-06824-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lopez Bernal J, Cummins S, Gasparrini A. The use of controls in interrupted time series studies of public health interventions. Int J Epidemiol. 2018;47:2082–2093. doi: 10.1093/ije/dyy135. [DOI] [PubMed] [Google Scholar]
- 5.Azoulay E, Kentish-Barnes N. A 5-point strategy for improved connection with relatives of critically ill patients with COVID-19. Lancet Respir Med. 2020;8:e52. doi: 10.1016/S2213-2600(20)30223-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets analyzed in the current study are not publicly available because of contracts with the hospitals providing data to the database. All codes used in the current study are available from the corresponding author on reasonable request.