Abstract
Introduction
The true incidence of periprosthetic femoral fracture (PFF) around cemented polished taper-slip implants remains largely unknown. Registries usually only capture PFFs that result in revision, missing those managed non-operatively or treated by open reduction and internal fixation (ORIF). This study reports the long-term rate of PFF with the original triple-tapered C-stem femoral implant.
Materials and methods
A prospective review of a consecutive series of 500 primary total hip arthroplasties (THAs) performed at a single centre between March 2000 and December 2005, with average follow-up of 15 years (12–19 years).
Results
There were 500 consecutive THAs in 455 patients. Seven PFFs (1.4%) occurred in seven patients at an average of 7.9 years (range 2–11.5) from the primary arthroplasty. Five PFFs were managed by ORIF, one Vancouver B3 fracture was revised for a loose implant and one patient was treated non-operatively. Average age at primary operation was 74 years (67–87) and BMI averaged 27.3 (22–31). There was no typical fracture pattern and no statistically significant associations with patient demographics (age, gender, BMI, diagnosis) or prosthetic details (size, offset, alignment, cement mantle, subsidence). Survivorship to the occurrence of PFF was 99% (97.3–99.6%) at 10 years and 97.8% (95.5–99.0%) at 15.
Conclusion
A PFF rate of 1.4% at an average follow-up of 15 years represents the true incidence of PFF with the use of the original triple-tapered C-Stem femoral implant, similar to that of published Exeter series (1.85%) but lower than the CPT (3.3%).
Keywords: Periprosthetic femoral fracture, Cemented, Polished, Taper-slip, Hip arthroplasty
Introduction
Periprosthetic femoral fracture (PFF) is an infrequent, yet potentially devastating complication of total hip arthroplasty (THA), which is associated with poorer functional outcomes, significant morbidity and an increased overall 12-month mortality of 11% [1]. In 2020, it was reported that patients admitted to hospital with PFF were at increased risk of developing post-operative COVID-19 infection [2].
Increased life expectancy and the longevity of physically active adults into older age [3] have led to a projected increased demand for primary THA in the UK of 134% by 2030 [4]. Coinciding with this, an estimated increased incidence of PFF of 4.6% every decade until 2045 has also been predicted [5].
The management of PFF is complex and can result in further costly re-operations, prolonged rehabilitation and persisting dysfunction [6, 7]. The true incidence of PFF remains unknown, but a prevalence of 0.1–4% has previously been estimated [3, 7–9]. National joint registries, except the Swedish Hip Arthroplasty Registry, record only those PFFs which necessitate revision, failing to capture those managed non-operatively or by ORIF [10, 11].
Uncemented implants are associated with an increased rate of PFF [12, 13] but it is less clear what impact the design specifics of cemented stems have on the incidence. The two categories of cemented stems are the taper-slip (force-closed) and the composite beam (shape-closed). Taper-slip stems provide excellent long-term results [14–16], and their use dominates the hip arthroplasty market in the United Kingdom [17].
A statistically significant increased risk of PFF for taper-slip stems compared to composite beams has been reported [18, 19], despite which there remain few published series addressing the issue and reporting the long-term results of taper-slip stems [14, 15, 20, 21] with only one previous publication on the long-term results of the original C-stem [16]. The aim of this study was to determine the true long-term incidence of PFF in a prospective cohort of 500 consecutive cemented polished triple-tapered original C-stem femoral implants.
Materials and methods
Data were collected prospectively on 500 consecutive primary THAs in 455 patients performed between March 2000 and December 2005. Ethical approval for this study was not required.
The original cemented polished triple-tapered C-stem featured a 9/10 rather than the later 12/14 trunnion and was used in all cases, having the same dimensions as the later C-stem AMT, other than the extended shoulder (both DePuy International, Leeds, UK). All operations were performed at a single centre under the care of four Orthopaedic Consultants, in laminar flow operating theatres.
A posterior surgical approach was used with a stay suture in the short external rotators to protect the sciatic nerve. A box chisel was used to access the piriform fossa, then a blunt-ended tapered reamer before sequential broaching of the canal to obtain a cement mantle of at least 2 mm. Trial reduction was performed to assess leg length and stability, before a cement restrictor of appropriate size was inserted, and the canal prepared with pulse lavage.
A third generation cementing technique was used, with vacuum-mixed Palacos-R Bone Cement (Heraeus GmbH, Hanau, Germany) containing Gentamicin inserted in retrograde fashion with a cement gun. The cement was constantly pressurised prior to the insertion of the femoral prosthesis with a hollow polymethyl-methacrylate (PMMA) tip centraliser, which was then held until the cement had set. The prosthesis was then reduced, and stability, leg length and offset are re-assessed before closure of the short external rotators and capsule as a single layer with loop PDS, but without trans-osseous sutures.
Outpatient review began at six weeks, then continued annually for five years and every second year thereafter. Plain radiographs were performed prior to discharge, then at twelve months and each clinical review thereafter.
Antero-posterior radiographs of the pelvis were taken using a standardised technique, with the X-ray centred over the symphysis pubis and the patellae pointing upwards. Femoral component alignment was measured with respect to the long axis of the femur (neutral being within five degrees), and the cement mantle was graded using the Barrack system [22]. Subsidence was measured using the Fowler technique [23] and PFF was categorised using the Vancouver Classification [24, 25].
Statistical analysis
Descriptive statistics were presented for relevant variables at THA level by fracture outcome (PFF or not). For continuous variables, statistics such as mean, median, standard deviation (SD), first and third quantiles (Q1, Q3), and number of observations were calculated. For categorical variables, count and percentage of each category were presented. To test the difference in the variables between the fracture and non-fracture groups, t tests were performed for continuous variables and Fisher’s exact test for categorical variables. Survival analysis was performed with the end point as time to PFF or to the latest follow-up (if no PFF), and Kaplan–Meier survival estimates were plotted for the entire cohort. In addition, a series of Cox regression model was used to explore variables associated with PFF. All statistical analyses were conducted using Stata (StataCorp LLC, Texas, USA).
Results
There were 500 consecutive primary THAs in 455 patients, with 282 females (62%) and 173 males (38%). Average age at surgery was 68.8 years (range 23–92), and average BMI was 29 (range 18–42). The most common indication for surgery was primary osteoarthritis (80.6%, Table 1).
Table 1.
Pre-operative diagnosis
| Pre-operative diagnosis | Number | % |
|---|---|---|
| Osteoarthritis | 403 | 80.60 |
| AVN | 51 | 10.20 |
| Rheumatoid Arthritis | 19 | 3.80 |
| NOF | 7 | 1.40 |
| Paget's Disease | 4 | 0.80 |
| DDH | 3 | 0.60 |
| Other | 13 | 2.60 |
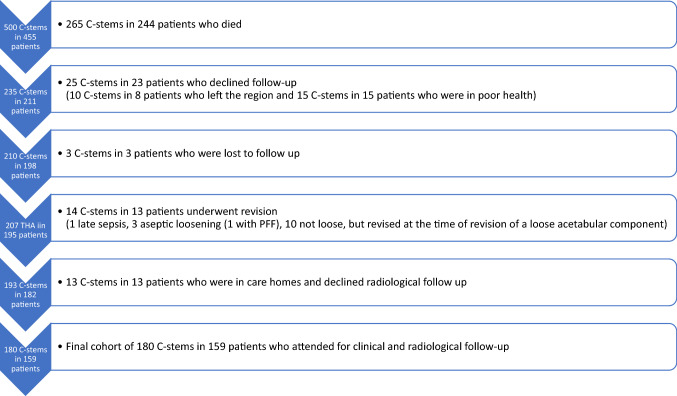
During follow-up, 244 (54%) patients died (265 THA, 53%), 23 patients (5%) with 25 THA (5%) declined further follow-up [8 moved out of region (10 THA), 15 due to poor health (15 THA)], with only three further patients (0.7%) with three THA (0.6%) being lost to follow-up. Fourteen femoral implants (2.8%) in thirteen patients (2.9%) were revised [one late sepsis, three aseptic loosening (one with a PFF), 10 during revision of a loose acetabular component]. Of the remaining 172 patients (37.8%) with 193 THA (38.6%), 13 (2.9%; 13 THA, 2.6%) residing in care homes declined radiological follow-up. These patients underwent a telephone consultation to confirm that they remained satisfied, had not suffered any complications and consented to a review of their medical records and radiological images, none of which subsequently demonstrated any PFF. This left a total of 180 THA (36%) in 159 patients (34.9%) with complete clinical and radiological follow-up (Fig. 1).
Fig. 1.
Flow chart diagram of patients detailing follow-up
High offset femoral stems were used in 288 cases (58%), with the average combined femoral offset (stem plus head) for the entire series being 44.1 mm (range 35–54 mm, Table 2).
Table 2.
Femoral stem sizes
| Femoral stem size | Number | % |
|---|---|---|
| 1 | 26 | 5.20 |
| 2 | 67 | 13.40 |
| HO2 | 80 | 16.00 |
| 3 | 65 | 13.00 |
| HO3 | 102 | 20.40 |
| 4 | 39 | 7.80 |
| HO4 | 80 | 16.00 |
| 5 | 4 | 0.80 |
| HO5 | 26 | 5.20 |
| 6 | 7 | 1.40 |
| 7 | 4 | 0.80 |
HO high offset stem
Seven PFFs occurred in seven patients (1.4%, Table 3), with a mean time from operation of 7.9 years (2–11.5). There was one Vancouver Type A fracture, three Type B1, two Type B2 and one Type B3 fracture. None were distal to the tip of the implant (Vancouver C).
Table 3.
Fracture type and management, patient, prosthesis and radiological findings
| Patient | Vancouver | Mx | Time | Age | Gender | BMI | Side | Dx | Stem | Offset | Align | Barrack | Subs-12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | A | ORIF | 133 | 68 | M | 25 | R | OA | HO3 | 47 | VAR | B | 0.5 |
| 2 | B1 | CON | 24 | 79 | M | 31 | L | OA | 2 | 41 | N | A | 0.5 |
| 3 | B1 | ORIF | 84 | 78 | F | 29 | R | OA | 4 | 42 | N | A | 1 |
| 4 | B1 | ORIF | 64 | 87 | F | 23 | R | OA | HO2 | 45 | N | A | 1 |
| 5 | B2 | ORIF | 138 | 67 | M | 30 | R | OA | HO4 | 52 | N | B | 0.5 |
| 6 | B2 | ORIF | 88 | 71 | F | 31 | L | OA | HO2 | 42 | N | B | 2 |
| 7 | B3 | REV | 137 | 68 | F | 22 | L | OA | 4 | 45 | VAL | A | 1 |
Mx how the fracture was managed. ORIF is open reduction and internal fixation, Con is conservative management, Rev is revision, Dx pre-operative diagnosis, OA is osteoarthritis, Time number of months until fracture, Align is alignment of the stem, Var is varus, N is neutral, Val is valgus, Barrack is the grading of the cement mantle, Offset is the combined offset of the stem plus the head, Subs-12 is subsidence at 12 months
The mean age at time of surgery was 74 years (67–87) in the PFF group compared to 68.6 years (23–92) in the non-fracture group, which was not statistically significant (p = 0.187). There were four fractures in female patients and three in males, with four being right sided and three left. The average BMI was 27.3 (22–31) in the PFF group compared to 28.6 (18–42), and the pre-operative diagnosis in all PFF cases was osteoarthritis (Table 3).
Femoral prosthesis alignment was neutral in five cases, varus in one and valgus in one, with cement mantle quality being Barrack Grade A in three cases and Grade B in four. Prosthetic offset (stem plus head) averaged 45.1 (41–52) in the fracture group compared to 44.1 (35–54), with subsidence of the femoral component at 12 months averaging 0.9 mm in both groups. Distal femoral cortical hypertrophy (DFCH) occurred in six cases (0.12%), none of whom suffered a PFF.
Five PFFs were managed by ORIF, one B2 fracture was treated non-operatively as the patient was unfit for surgery and the B3 fracture underwent revision for aseptic loosening of the stem (Table 3). There were no subsequent re-operations in any of these patients, four of whom died at an average of 16.5 months (range 3 to 36) from the date of fracture.
Statistical analysis of age, gender, pre-operative diagnosis, operated side, BMI, implant size, prosthetic offset (stem plus head), Barrack classification and femoral alignment demonstrated no statistical significance between the fracture and non-fracture groups (Table 4). A series of Cox regression models was performed with variables in Table 4 as covariates. Because the sample size was small (only seven PFF), the model was restricted to include a single continuous or dummy variable. It was found that none of the variables had a statistically significant association with PFF.
Table 4.
Summary of statistical analysis
| Variables | Non-fracture (N = 493) |
Fracture (N = 7) |
p value |
|---|---|---|---|
| Age | 0.187 | ||
| Mean (SD) | 68.61 (10.73) | 74.00 (7.53) | |
| Median (Q1, Q3) | 70.0 (64.0, 75.0) | 71.0 (68.0, 79.0) | |
| N (% Non-missing) | 493 (100.0%) | 7 (100.0%) | |
| BMI | 0.468 | ||
| Mean (SD) | 28.61 (4.78) | 27.29 (3.86) | |
| Median (Q1, Q3) | 29.0 (25.0, 32.0) | 29.0 (23.0, 31.0) | |
| N (% Non-missing) | 380 (77.1%) | 7 (100.0%) | |
| Offset | 0.537 | ||
| Mean (SD) | 44.13 (4.31) | 45.14 (3.89) | |
| Median (Q1, Q3) | 44.0 (41.0, 48.0) | 45.0 (42.0, 47.0) | |
| N (% Non-missing) | 493 (100.0%) | 7 (100.0%) | |
| Side | 1.000 | ||
| Right | 273 (55.4%) | 4 (57.1%) | |
| Left | 220 (44.6%) | 3 (42.9%) | |
| Gender | 0.704 | ||
| Female | 318 (64.5%) | 4 (57.1%) | |
| Male | 175 (35.5%) | 3 (42.9%) | |
| Femoral Stem Size | 0.685 | ||
| 1 | 26 (5.3%) | 0 (0.0%) | |
| 2 | 66 (13.4%) | 1 (14.3%) | |
| HO2 | 78 (15.8%) | 2 (28.6%) | |
| 3 | 65 (13.2%) | 0 (0.0%) | |
| HO3 | 101 (20.5%) | 1 (14.3%) | |
| 4 | 37 (7.5%) | 2 (28.6%) | |
| HO4 | 79 (16.0%) | 1 (14.3%) | |
| 5 | 4 (0.8%) | 0 (0.0%) | |
| HO5 | 26 (5.3%) | 0 (0.0%) | |
| 6 | 7 (1.4%) | 0 (0.0%) | |
| 7 | 4 (0.8%) | 0 (0.0%) | |
| Barack classification | 0.340 | ||
| A | 326 (66.1%) | 3 (42.9%) | |
| B | 149 (30.2%) | 4 (57.1%) | |
| D | 12 (2.4%) | 0 (0.0%) | |
| Unknown* | 6 (1.2%) | 0 (0.0%) | 0.686 |
| Alignment | |||
| Neutral | 335 (68.0%) | 5 (71.4%) | |
| Right | 106 (21.5%) | 1 (14.3%) | |
| Left | 46 (9.3%) | 1 (14.3%) | |
| Unknown* | 6 (1.2%) | 0 (0.0%) |
T tests used for continuous variables and Fisher’s exact test used for categorical variables
HO high offset stem
*Unknown: six patients died before 12-month follow-up radiographs were obtained
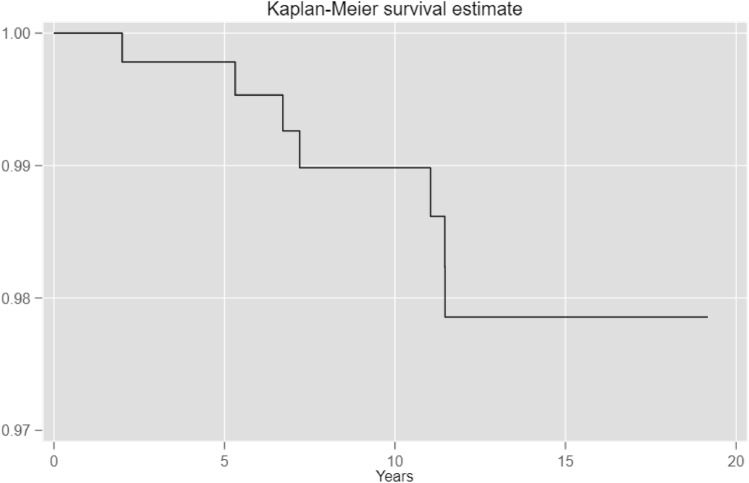
Kaplan–Meier survivorship, with PFF as the end point, was 99.0% (292 THA at risk, 97.3–99.6%) at 10 years and 97.8% (114 THA at risk, 95.5–99.0%) at 15 years (Fig. 2).
Fig. 2.
Kaplan–Meier survival curve for entire cohort
Discussion
The PFF rate was 1.4% in a consecutive cohort of 500 cemented polished triple-tapered C-stem femoral implants, using third generation cementing and Palacos-R + G bone cement, with long-term follow-up averaging 15 years. There was no typical fracture pattern or statistically significant associations with patient demographic or prosthetic details.
The Exeter (Stryker, New Jersey, USA) and CPT stems (Zimmer, Warsaw, Indiana, USA) are double-tapered femoral implants and comprise in excess of 75% of the UK market share [17]. The C-stem has a third taper, running from lateral to medial, for proximal loading of the calcar to reduce negative bone remodelling in the long term [16] and only six cases (0.12%) in the current series developed DFCH confirming that this was being achieved.
Force-closed femoral implants achieve stability by means of controlled subsidence within the cement mantle, acting as a wedge and generating hoop stresses in the cement-bone construct [10]. The polished implant surface allows micromotion at the implant–cement interface without abrasion, facilitating controlled subsidence due to the visco-elastic property of bone cement called creep, which is non-recoverable deformation under load. PFF in taper-slip implants is typically caused by a low-velocity rotational injury with forced axial loading [10], and it has been postulated that the wedge shape of the prosthesis, which is not fixed within the cement mantle, will transmit momentarily increased hoop stresses at the cement–bone interface leading to an increased risk of PFF compared to composite beam stems, which are fixed within the cement mantle [19].
The Vancouver classification system guides optimum management of PFF for both cemented and uncemented prostheses [24, 25] and has been integrated into the unified classification system, to characterise periprosthetic fractures around any joint [26]. Due to the complexity relating specifically to polished taper-slip implants, Maggs et al. recently advocated a sub-classification of B2 fractures distinguishing between those in which the cement–bone interface is well fixed and those in which it is loose, as this determines the definitive management [10].
National joint registries now provide the majority of arthroplasty outcome data, but with the exception of the Swedish Hip Arthroplasty Registry, capture only those patients in whom a complication has necessitated revision surgery [10, 11]. In the case of PFF, this will not include fractures treated by ORIF or non-operatively due to patient frailty, and in a recent study of 539 PFFs, 23% (122 PFFs) were managed non-operatively, 31% (169 PFFs) by ORIF alone and 46% (246 PFFs) by ‘revision and/or fixation’ [27].
Registries therefore underestimate the incidence of PFF [1, 8, 10] but inconsistencies can also occur with the revision data itself [28]. A recent study assessing risk factors for PFF compared the German Arthroplasty Registry data to insurance record ICD codes, discovering a 13.7% discrepancy with regards to PFF being the actual cause of revision [29].
In the current study, only the single patient with the Vancouver B3 PFF, which underwent revision, would have been captured by the National Joint Registry (NJR). An inaccurate PFF incidence of 0.2% would therefore have been estimated, as opposed to the actual rate of 1.4%, with an average follow-up of 15 years.
Where registry data are lacking, well-conducted single, or multi-centre, case series can give insight into the true rates and management of PFF. Due to their proportion of market share, the Exeter and CPT stems constitute the majority of the reported series assessing the risk and rates of PFF with taper-slip designs.
Mahon et al. reviewed 829 Exeter V40 stems reporting a PFF rate resulting in revision of 0.36%, with a mean follow-up of 12.4 years [21] and Petheram et al. reported a PFF rate resulting in revision of 0.78% in a series of 382 Exeter Universal stems with an average follow-up of 22.4 years [14]. Westerman et al. reviewed the first 540 Exeter V40 stems performed at their centre in the two years following its introduction, reporting a PFF rate of 1.85% at a mean follow-up of 12.4 years [20].
The CPT stem is similar in design to the Exeter, but has a wider shoulder. One study of 191 CPT stems with a mean follow-up of 15.9 years reported only one PFF (0.52%) leading to revision, which occurred at five years [15, 30], however, another reported a PFF rate of 3.34% in a series of 1403 hips, with a mean follow-up of only 4 years [7]. In an observational cohort study, Mohammed et al. compared PFF rates at a single centre during the transition from the standard use of a CPT stem to the Lubinus SP2 composite beam. At two years, the CPT group had sustained 18 PFFs (3.31%) and the Lubinus group only two (0.37%) [6]. The latter two studies had a limited duration of follow-up, and in the current series, the fractures occurred at an average of 7.9 years, with only one during the first four years, consistent with the 7.6 years reported in a large study in 2022 [31].
In a registry-based study, Palan et al. reported incidences of PFF, based only on revision, of 0.12% for the Exeter V40 stem, 0.14% for the C-stem and 0.46% for the CPT, which, as expected, were markedly lower than in the cohort studies [19]. This study also postulated that the CPT’s higher PFF rate may be down to having a larger, broader shoulder than both the Exeter and the C-Stem [19].
In a biomechanical study, Erdhart et al. compared the periprosthetic fracture patterns around the CPT and the C-Stem. Ten double-tapered CPT stems and 10 triple-tapered C-stems were cemented into synthetic femurs and subjected to axial compression. There were seven Vancouver B fractures in the CPT constructs and three Vancouver C. In all ten C-stem constructs, the fractures occurred at the tip of the implant with the cement mantle remaining intact, suggesting there is less harmful strain produced to the cement mantle in torsion than in other designs [32]. There was, however, no typical fracture pattern in the PFF cohort in the current study (Table 3).
The only previously published long-term series with the original C-stem included 621 arthroplasties performed using trochanteric osteotomy. At a mean follow-up of 13 years, there were no instances of PFF, but fractures of the femoral prosthesis occurred in two cases [16]. There were no cases of femoral prosthesis fracture in the current study.
The strength of the current study is that data were collected prospectively, with only three patients (0.66%) being lost to follow-up, two of them after 10 years, allowing an accurate determination of the outcome of almost every THA. One limitation germane to all longitudinal studies is the number of patients who will inevitably die during the follow-up period, which, in the current study, was 244 patients (54%) with 265 THA (53%) at an average follow-up of 15 years (Table 5).
Table 5.
Summary of studies
| Author | Implant name | Manufacturer | Average follow-up (yrs) | PFFs, hips (n) | PFF % | Time to PFF (yrs) | Average age (yrs) | Comments |
|---|---|---|---|---|---|---|---|---|
| Westerman et al. [20] | Exeter V40 | Stryker | 12.4 | 10 of 540 | 1.85 | 10.9 | 67.7 | Six PPFs were cause for stem revision (1.11%) |
| Mahon et al. [21] | Exeter V40 | Stryker | 12.3 | 3 of 829 | 0.36 | 6.9 | 67.8 | Only details PFF as cause of revision |
| Petheram et al. [14] | Exeter Universal | Stryker | 22.4 | 3 of 382 | 0.78 | – | 66.3 | Only details PFF as cause of revision |
| Yates et al. [30], Burston et al. [15] | CPT | Zimmer | 10 then 15 | 1 of 191 | 0.52 | 5 | 64.9 | Both papers report on same cohort at 10 and 15 years, respectively |
| Palan et al. [19] | Exeter V40 | Stryker | 3.8 | 182 of 146,409 | 0.12 | – | 72 | Registry Data—Only details PFF as caused of revision |
| Registry data based on revision | CPT | Zimmer | " | 111 of 24,300 | 0.46 | – | 73 | " |
| Charnley | DePuy | " | 15 of 20,182 | 0.07 | – | 73 | " | |
| C-Stem | DePuy | " | 21 of 15,113 | 0.14 | – | 71 | " | |
| Broden et al. [7] | CPT | Zimmer | 4.0 | 47 of 1403 | 3.35 | 7 months | 82 | Elderly cohort—mean age 82 years |
| Mohammed et al. [6] | CPT | Zimmer | 2.0 | 18 of 543 | 3.31 | 2 months | 82 | Follow-up only to two years |
| Lubinus SP2 | Waldermar Link | 2.0 | 2 of 534 | 0.37 | " | " | " |
Conclusion
The incidence of PFF in this prospective cohort of 500 THAs using the original cemented polished triple-tapered C-stem femoral implant was 1.4% after 15 years of follow-up. This is similar to the PFF rates reported for the polished double-tapered Exeter V40 but lower than for the CPT.
With an increased incidence of PFF predicted over the next three decades, a more detailed knowledge of the risk profile for specific implant designs is required. This could be achieved either by expanding the minimum data set for National Joint Registries to include all PFFs managed by any means or alternatively, by widening the scope of National Hip Fracture Databases to include PFFs in a similar way that femoral shaft and distal femoral fractures have recently been included in the Best Practice Tariff in the United Kingdom. Large long-term single-, or multi-centre, studies of individual prostheses would remain of great value, as they include more detailed demographic and radiological analysis, in order to augment the currently limited body of knowledge on this subject.
Acknowledgements
The senior author (DHS) would like to thank previous consultant colleagues, research fellows and registrars at North Manchester General Hospital, where this study was performed, for their contributions, as well as Mrs. M. Austin and Miss D. Hudson who maintained the high rates of follow-up throughout the study period.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.
Declarations
Conflict of interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Ethical approval
Ethical approval for this study was not required.
Informed consent
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Kwaku Baryeh, Email: Kwaku.baryeh1@nhs.net.
Chao Wang, Email: c.wang@sgul.kingston.ac.uk.
David H. Sochart, Email: David.sochart@nhs.net
References
- 1.Carli AV, Negus JJ, Haddad FS. Periprosthetic femoral fractures and trying to avoid them. Bone Joint J. 2017;99-B:50–59. doi: 10.1302/0301-620X.99B1.BJJ-2016-0220.R1. [DOI] [PubMed] [Google Scholar]
- 2.Clement ND, Hall AJ, Makaram NS, Robinson PG, Patton RFL, Moran M, et al. IMPACT-Restart: the influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Joint J. 2020;102-B:1774–1781. doi: 10.1302/0301-620X.102B12.BJJ-2020-1395.R2. [DOI] [PubMed] [Google Scholar]
- 3.Cook RE, Jenkins PJ, Walmsley PJ, Patton JT, Robinson CM. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res. 2008;466:1652–1656. doi: 10.1007/s11999-008-0289-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel A, Pavlou G, Mújica-Mota RE, Toms AD. The epidemiology of revision total knee and hip arthroplasty in England and Wales. Bone Joint J. 2015;97-B:1076–1081. doi: 10.1302/0301-620X.97B8.35170. [DOI] [PubMed] [Google Scholar]
- 5.Pivec R, Issa K, Kapadia BV, Cherian JJ, Maheshwari AV, Bonutti PM, et al. Incidence and future projections of periprosthetic femoral fracture following primary total hip arthroplasty: an analysis of international registry data. J Long Term Eff Med Implants. 2015 doi: 10.1615/JLongTermEffMedImplants.2015012625. [DOI] [PubMed] [Google Scholar]
- 6.Mohammed J, Mukka S, Hedbeck CJ, Chammout G, Gordon M, Sköldenberg O. Reduced periprosthetic fracture rate when changing from a tapered polished stem to an anatomical stem for cemented hip arthroplasty: an observational prospective cohort study with a follow-up of 2 years. Acta Orthop. 2019;90:427–432. doi: 10.1080/17453674.2019.1624339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brodén C, Mukka S, Muren O, Eisler T, Boden H, Stark A, et al. High risk of early periprosthetic fractures after primary hip arthroplasty in elderly patients using a cemented, tapered, polished stem: An observational, prospective cohort study on 1,403 hips with 47 fractures after mean follow-up time of 4 years. Acta Orthop. 2015;86:169–174. doi: 10.3109/17453674.2014.971388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Baryeh K, Sochart DH. Post-operative peri-prosthetic fracture rates following the use of cemented polished taper-slip stems for primary total hip arthroplasty: a systematic review. Arch Orthop Trauma Surg. 2022 doi: 10.1007/s00402-021-04302-3. [DOI] [PubMed] [Google Scholar]
- 9.Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures: classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty. 2005;20:857–865. doi: 10.1016/j.arth.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Maggs JL, Swanton E, Whitehouse SL, Howell JR, Timperley AJ, Hubble MJW, et al. B2 or not B2? That is the question: a review of periprosthetic fractures around cemented taper-slip femoral components. Bone Joint J. 2020;103-B:71–78. doi: 10.1302/0301-620X.103B1.BJJ-2020-0163.R1. [DOI] [PubMed] [Google Scholar]
- 11.Chatziagorou G, Lindahl H, Kärrholm J. Surgical treatment of Vancouver type B periprosthetic femoral fractures. Bone Joint J. 2019;101-B:1447–1458. doi: 10.1302/0301-620X.101B11.BJJ-2019-0480.R2. [DOI] [PubMed] [Google Scholar]
- 12.Abdel MP, Watts CD, Houdek MT, Lewallen DG, Berry DJ. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Jt J. 2016;98B:461–467. doi: 10.1302/0301-620X.98B4.37201. [DOI] [PubMed] [Google Scholar]
- 13.Springer BD, Etkin CD, Shores PB, Gioe TJ, Lewallen DG, Bozic KJ. Perioperative periprosthetic femur fractures are strongly correlated with fixation method: an analysis from the American Joint Replacement Registry. J Arthroplasty. 2019;34:S352–S354. doi: 10.1016/j.arth.2019.02.004. [DOI] [PubMed] [Google Scholar]
- 14.Petheram TG, Whitehouse SL, Kazi HA, Hubble MJW, Timperley AJ, Wilson MJ, et al. The Exeter Universal cemented femoral stem at 20 to 25 years. Bone Joint J. 2016;98-B:1441–1449. doi: 10.1302/0301-620X.98B11.37668. [DOI] [PubMed] [Google Scholar]
- 15.Burston BJ, Barnett AJ, Amirfeyz R, Yates PJ, Bannister GC. Clinical and radiological results of the collarless polished tapered stem at 15 years follow-up. J Bone Joint Surg Br. 2012;94:889–894. doi: 10.1302/0301-620X.94B7.28799. [DOI] [PubMed] [Google Scholar]
- 16.Purbach B, Kay PR, Siney PD, Fleming PA, Wroblewski BM. The C-stem in clinical practice: fifteen-year follow-up of a triple tapered polished cemented stem. J Arthroplasty. 2013;28:1367–1371. doi: 10.1016/j.arth.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 17.National Joint Registry for England Wales Northern Ireland and the Isle of Man. NJR 18th Annual Report 2021. Natl Jt Regist 2021
- 18.Kazi HA, Whitehouse SL, Howell JR, Timperley AJ. Not all cemented hips are the same: a register-based (NJR) comparison of taper-slip and composite beam femoral stems. Acta Orthop. 2019;90:214–219. doi: 10.1080/17453674.2019.1582680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Palan J, Smith MC, Gregg P, Mellon S, Kulkarni A, Tucker K, et al. The influence of cemented femoral stem choice on the incidence of revision for periprosthetic fracture after primary total hip arthroplasty: an analysis of national joint registry data. Bone Jt J. 2016;98-B:1347–1354. doi: 10.1302/0301-620X.98B10.36534. [DOI] [PubMed] [Google Scholar]
- 20.Westerman RW, Whitehouse SL, Hubble MJW, Timperley AJ, Howell JR, Wilson MJ. The Exeter V40 cemented femoral component at a minimum 10-year follow-up. Bone Jt J. 2018;100B:1002–1009. doi: 10.1302/0301-620X.100B8.BJJ-2017-1535.R1. [DOI] [PubMed] [Google Scholar]
- 21.Mahon J, McCarthy CJ, Sheridan GA, Cashman JP, O’Byrne JM, Kenny P. Outcomes of the Exeter V40 cemented femoral stem at a minimum of ten years in a non-designer centre. Bone Jt Open. 2020;1:743–748. doi: 10.1302/2633-1462.112.BJO-2020-0163.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barrack RL, Mulroy RD, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74-B:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 23.Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am. 1988;19:477–489. [PubMed] [Google Scholar]
- 24.Duncan CP, Masri BA. Fractures of the femur after hip replacement. Instr Course Lect. 1995;44:293–304. [PubMed] [Google Scholar]
- 25.Masri BA, Meek RMD, Duncan CP. Periprosthetic fractures evaluation and treatment. Clin Orthop Relat Res. 2004 doi: 10.1097/00003086-200403000-00012. [DOI] [PubMed] [Google Scholar]
- 26.Duncan CP, Haddad FS. The Unified Classification System (UCS): improving our understanding of periprosthetic fractures. Bone Jt J. 2014 doi: 10.1302/0301-620X.96B6.34040. [DOI] [PubMed] [Google Scholar]
- 27.The COMPOSE Study Team Management and outcomes of femoral periprosthetic fractures at the hip. Bone Joint J. 2022;104-B:997–1008. doi: 10.1302/0301-620X.104B8.BJJ-2021-1682.R1. [DOI] [PubMed] [Google Scholar]
- 28.Afzal I, Radha S, Smoljanović T, Stafford GH, Twyman R, Field RE. Validation of revision data for total hip and knee replacements undertaken at a high volume orthopaedic centre against data held on the National Joint Registry. J Orthop Surg Res. 2019;14:318. doi: 10.1186/s13018-019-1304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Konow T, Baetz J, Melsheimer O, Grimberg A, Morlock M. Factors influencing periprosthetic femoral fracture risk. Bone Joint J. 2021;103-B:650–658. doi: 10.1302/0301-620X.103B4.BJJ-2020-1046.R2. [DOI] [PubMed] [Google Scholar]
- 30.Yates PJ, Burston BJ, Whitley E, Bannister GC. Collarless polished tapered stem: Clinical and radiological results at a minimum of ten years’ follow-up. J Bone Jt Surg Ser B. 2008;90:16–22. doi: 10.1302/0301-620X.90B1.19546. [DOI] [PubMed] [Google Scholar]
- 31.The COMPOSE Study Team Epidemiology and characteristics of femoral periprosthetic fractures. Bone Joint J. 2022;104-B:987–996. doi: 10.1302/0301-620X.104B8.BJJ-2021-1681.R1. [DOI] [PubMed] [Google Scholar]
- 32.Erhardt JB, Khoo PP, Stoffel KK, Yates PJ. Periprosthetic fractures around polished collarless cemented stems: the effect of stem design on fracture pattern. HIP Int. 2013;23:459–464. doi: 10.5301/hipint.5000052. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors confirm that the data supporting the findings of this study are available within the article [and/or] its supplementary materials.