Abstract
Myeloid-derived suppressor cells (MDSCs) comprise heterogeneous myeloid cell populations with immunosuppressive capacity that contribute to immune regulation and tolerance induction. We previously reported impaired MDSC function in patients with primary Sjögren’s syndrome (pSS) and mice with experimental SS (ESS). However, the molecular mechanisms underlying MDSC dysfunction remain largely unclear. In this study, we first found that aryl hydrocarbon receptor (AhR) was highly expressed by human and murine polymorphonuclear MDSCs (PMN-MDSCs). Indole-3-propionic acid (IPA), a natural AhR ligand produced from dietary tryptophan, significantly promoted PMN-MDSC differentiation and suppressive function on CD4+ T cells. In contrast, feeding a tryptophan-free diet resulted in a decreased PMN-MDSC response, a phenotype that could be reversed by IPA supplementation. The functional importance of PMN-MDSCs was demonstrated in ESS mice by using a cell-depletion approach. Notably, AhR expression was reduced in PMN-MDSCs during ESS development, while AhR antagonism resulted in exacerbated ESS pathology and dysregulated T effector cells, which could be phenocopied by a tryptophan-free diet. Interferon regulatory factor 4 (IRF4), a repressive transcription factor, was upregulated in PMN-MDSCs during ESS progression. Chromatin immunoprecipitation analysis revealed that IRF4 could bind to the promoter region of AhR, while IRF4 deficiency markedly enhanced AhR-mediated PMN-MDSC responses. Furthermore, dietary supplementation with IPA markedly ameliorated salivary glandular pathology in ESS mice with restored MDSC immunosuppressive function. Together, our results identify a novel function of AhR in modulating the PMN-MDSC response and demonstrate the therapeutic potential of targeting AhR for the treatment of pSS.
Keywords: myeloid-derived suppressor cell, Sjogren’s syndrome, Aryl hydrocarbon receptor
Subject terms: Autoimmunity, Cell death and immune response
Introduction
Myeloid-derived suppressor cells (MDSCs) comprise heterogeneous immature myeloid cell populations with immunosuppressive ability exerted by producing reactive oxygen species (ROS), arginase 1 (ARG1), and NO, which can elicit inhibitory functions on various immune cell subsets, particularly effector T cells [1, 2]. Notably, cross-species studies suggested the evolutionary conservation of MDSCs between humans and mice, showing functional similarities in their effector molecules [3]. Murine MDSCs are characterized by the coexpression of CD11b and Gr-1 and can be subdivided into CD11b+Ly6G+Ly6Clow polymorphonuclear (PMN-MDSCs) and CD11b+Ly6G-Ly6Chigh monocytic (M-MDSCs) subsets. As the major cellular source of ROS, PMN-MDSCs can induce oxidative stress in the antigen-specific T-cell response upon TCR engagement [4]. Early studies indicated that PMN-MDSCs could promote cancer development by inhibiting T-cell-mediated antitumor immunity [5]. Recently, mounting evidence has also suggested a close involvement of MDSCs in autoimmune diseases, including multiple sclerosis, systemic lupus erythematosus, and primary Sjögren’s syndrome (pSS) [6].
pSS is a progressive autoimmune disease characterized by multiple organ dysfunction and tissue destruction, particularly affecting the lacrimal and salivary glands (SG), leading to severe dry-eye and dry-mouth symptoms. Although histopathological evidence indicates massive lymphocytic infiltration of CD4+ T cells and B cells in the SGs of pSS patients, the immunopathogenesis of pSS has not been fully elucidated. Emerging studies, including our recent findings, have demonstrated the pivotal roles of effector T-cell subsets, such as Th1, Th17, and T follicular helper (Tfh) cells, in humoral autoimmunity and disease development [7–11], accompanied by defects in the functions of immune regulatory subsets [12]. Using a well-established mouse model with experimental SS [13], we also reported impaired MDSC functions during disease progression in both ESS mice and pSS patients [14], among which M-MDSCs exhibited reduced ARG1 levels. However, the molecular mechanisms underlying PMN-MDSC dysfunction in ESS pathogenesis are poorly understood.
Aryl hydrocarbon receptor (AhR) is a cytoplasmic receptor that can respond to multiple exogenous and endogenous compounds from the gut flora, host metabolism, and environment [8, 15–18]. Recent studies have suggested a critical role of AhR in maintaining homeostasis in the intestinal mucosa, as several indole-containing AhR ligands can suppress intestinal inflammation [19]. In contrast, high binding affinity-mediated persistent AhR activation by halogenated aromatic hydrocarbons, such as 2,3,7,8-tetrachlorodibenzo-p-dioxin, induced toxicity and exacerbated inflammation [20]. Notably, indole-3-propionic acid (IPA), a natural AhR ligand derived from microbiota-mediated tryptophan metabolism, could reduce neuroinflammation in a mouse model of multiple sclerosis [21]. Thus, accumulating evidence suggests that “tonic” AhR signaling may be closely involved in immune tolerance induction. Indeed, oral supplementation with IPA promoted the remission of inflammatory bowel disease in both humans and mice [22]. Although previous studies by Goudot et al. demonstrated AhR as a molecular switch that controls monocyte fate determination to become macrophages or dendritic cells [19], the role of AhR in regulating the MDSC response is unclear.
In this study, we first found that AhR was highly expressed by both human and murine PMN-MDSCs but not M-MDSCs. IPA treatment significantly promoted the differentiation and function of PMN-MDSCs in culture, and this effect was abolished by the selective AhR antagonist CH223191. Notably, impaired PMN-MDSC development was observed in mice fed a tryptophan-free diet, and this could be overcome by IPA supplementation. Anti-Ly6G antibody-mediated PMN-MDSC depletion resulted in exacerbated ESS development and effector T-cell dysregulation in mice, suggesting a pivotal role of PMN-MDSCs in ESS pathogenesis. Interestingly, similar findings were also observed in ESS mice treated with CH223191 or fed a tryptophan-free diet. In addition, we identified that the repressive transcription factor interferon regulatory factor 4 (IRF4) could bind to the promoter region of AhR and negatively regulate AhR signaling. Consistent with this, IPA-mediated PMN-MDSC proliferation and ROS production were found to be significantly enhanced in IRF4−/− PMN-MDSCs compared with wild-type (WT) controls. Moreover, oral treatment with IPA effectively ameliorated the disease pathology of ESS mice, improving MDSC counts and function. Together, these results suggest that AhR may serve as a promising therapeutic target in treating human pSS, while a tryptophan-enriched diet may also be beneficial in alleviating pSS pathogenesis.
Materials and methods
Mice
Female C57BL/6 (CD45.2) and B6. SJL-Ptprca Pepcb/BoyJ (CD45.1) mice at 6–8 weeks of age were purchased from Jackson Laboratory. IRF4−/− mice in a C57BL/6 background were kindly provided by Professor Tak Wah Mak (University of Toronto). Mice were maintained in a specific pathogen-free animal facility at The University of Hong Kong. Mice were fed a normal diet as a control or a tryptophan-free diet (Research Diet, A12083001i) for 2 weeks. All the experiments in this study were approved by the Committee on the Use of Live Animals in Teaching and Research at The University of Hong Kong.
Induction of ESS mouse model
ESS induction was performed as previously reported [11]. Briefly, salivary glands were isolated from female C57BL/6 mice and homogenized in phosphate-buffered saline (PBS). The supernatant was collected after centrifugation to prepare SG proteins. Naïve female C57BL/6 mice were immunized with 400 μg SG protein emulsified in Freund’s complete adjuvant (Difco) on Day 0. On Day 14, a booster injection with 400 μg SG protein emulsified in Freund’s incomplete adjuvant (Difco) was performed. Mice immunized with adjuvant alone served as controls.
IPA treatment
IPA (Sigma‒Aldrich) was dissolved in DMSO at 1 M/L and diluted in PBS before use. ESS mice were i.p. administered IPA twice a week for 8 weeks at a dosage of 400 μg/20 g body weight. The mice in the control group were administered an equal volume of vehicle (DMSO diluted in PBS). In some experiments, IPA was administered for 8 weeks beginning at 20 weeks post-ESS induction to assess the histopathological changes in the salivary glands.
Detection of saliva flow rate
The saliva flow rate was measured as previously reported [11]. Briefly, mice were anesthetized and i.p. injected with pilocarpine (Sigma‒Aldrich) at a dose of 5 mg/kg body weight. Saliva was then collected from the oral cavity for 15 min using a 20 μl pipet tip.
Human blood samples and cell purification
Blood samples from healthy donors were obtained from the Hong Kong Red Cross Blood Transfusion Service with institutional approval (UW 20–579). Blood samples were diluted in PBS with 2% human AB serum (Sigma‒Aldrich) and carefully layered on prepared Lymphoprep (Lonza) medium, followed by centrifugation at 800 × g for 20 min at room temperature with the brake off. Peripheral blood mononuclear cells (PBMCs) were then collected for flow cytometric analysis.
MDSC isolation
Single-cell suspensions were prepared from the spleens of female C57BL/6 mice and blocked with Fc Block (BD Biosciences) at 4 °C for 10 min. Biotin anti-mouse CD4, CD8, and anti-biotin microbeads were used to remove T cells. Then, total MDSCs (CD11b+GR1+) or PMN-MDSCs (CD11b+Ly6G+Ly6Clow) were further purified by using a FACSFusion (Becton Dickinson) cell sorter.
In vitro MDSC generation and proliferation assays
Bone marrow-derived cells (BMCs) were isolated from female C57BL/6 mice, as previously reported, with minor modifications [23]. BMCs were cultured at 5 × 1012 per ml in RPMI 1640/10% FBS in the presence of the cytokines GM-CSF and IL-6 (both at a final concentration of 20 ng/ml) for MDSC polarization. After 3 days of culture, the BM-MDSCs were harvested and further purified by using a FACSFusion (Becton, Dickinson and Company) cell sorter. For the MDSC proliferation assay, murine bone marrow cells were isolated from WT or IRF4−/− mice and cultured under MDSC polarization conditions in the presence or absence of various agonists or antagonists. Flow cytometry was performed to analyze the proliferation of MDSCs. Cells with low SNARF (Thermo Fisher) or CFSE (Invitrogen) fluorescence intensity were defined as proliferating cells.
For human MDSC cultures, PBMCs were isolated by differential density gradient separation and cultured with recombinant human GM-CSF (20 ng/ml), IL-6 (20 ng/ml), and 10% fetal bovine serum (FBS) in RPMI 1640 medium for 6 days; a half volume of fresh medium was added on Day 3. Cells in the experimental groups were treated with 20 μM or 100 μM IPA alone or together with 0.5 μM cyclosporin A (Target Mol). On Day 6, cells in each group were harvested for flow cytometric analysis.
T-cell suppression assay
Murine CD4+ T cells were isolated from female C57BL/6 mice using anti-CD4 MicroBeads (Miltenyi Biotec). CD4+ T cells were labeled with carboxyfluorescein succinimidyl ester (CFSE, 5 mM; Invitrogen) and cocultured with MDSCs in 96-well U-bottom plates (Costar) in the presence of anti-CD3/CD28 microbeads (BD Biosciences) for 3 days. The fluorescence intensity of CFSE was analyzed to evaluate the proliferation of CD4+ T cells by flow cytometry. The inhibition rate was calculated as [1 - (cocultured CD4+ T-cell number/T-cell culture alone number)] × 100%.
ROS detection
ROS detection was performed as described in a previous report with minor modifications [24]. The oxidation-sensitive dye 2,7-dichlorofluorescein diacetate (DCFH-DA, MedChemExpress) was used to measure ROS production by PMN-MDSCs. Cells were cultured with DCFH-DA (5 μM) and 30 ng/mL PMA in PBS for 30 min. Cells were then labeled with anti-CD11b, anti-Ly6G, and anti-Ly6C mAbs and analyzed by flow cytometry.
Flow cytometric analysis
Murine spleens and cervical lymph nodes were isolated to prepare single-cell suspensions in a culture medium (RPMI 1640 medium with 10% FCS). The cell suspensions were initially blocked with Fc Block (BD Biosciences) at 4 °C for 10 min before incubation with antibodies to identify surface markers and intracellular molecules (Supplementary Table 1). The following antibodies were used (clone numbers): anti-mouse IRF4, CD3, CD19, CD44, CD138, CXCR5, Bcl-6, GL-7, Fas, CD138, CD23, CD21, Foxp3, IL-6, IFN-γ, IL17A, CD11b, Ly6G, Ly6C, and isotype-matched control antibodies (all obtained from BioLegend). Rabbit anti-mouse/human AhR was purchased from Abcam. Anti-human CD11b, CD33, CD66b, CD19, CD3, CD56, CD8, and CD4 antibodies were purchased from BioLegend. Human PMN-MDSCs were defined as CD3−CD11b+CD33hiCD66b+ populations, while M-MDSCs were defined as CD3-CD11b+CD33loCD66b- populations [25].
For intracellular staining, cells were stimulated with phorbol myristate acetate (50 ng/ml; Sigma‒Aldrich), ionomycin (500 ng/ml; Sigma‒Aldrich), and monensin (2 μM; BioLegend) for 5 h. Cells were then stained with cell viability dye (ZombieAquaTM, BioLegend), followed by antibodies against surface markers. Fixed and permeabilized cells were stained for intracellular cytokines by using the Cytofix/Cytoperm kit (BD Biosciences). Intranuclear AhR and Foxp3 were stained in fixed cells and permeabilized by using a Foxp3/Transcription Factor Staining Buffer Set (eBioscience). For AhR staining, a secondary antibody, DyLight donkey anti-rabbit IgG (BioLegend), was used.
RNA extraction and quantitative real-time PCR (qRT‒PCR)
Total RNA was extracted from MDSCs using the ReliaPrep™ RNA Cell Miniprep System (Promega). qRT‒PCR analysis was performed using the One-Step SYBR PrimeScriptTM RT‒PCR Kit II (TaKaRa) on a LightCycler 96 System (Roche). The sequences for the primers used were as follows: murine AhR, forward-5′-CGCGGGCACCATGAGCAG-3′ and reverse-5′-GAGACTCAGCTCCTGGATGG-3′ [26]. Murine IRF4, forward-5′- CTACCCCATGACAGCACCTT-3′ and reverse-5′- CCAAACGTCACAGGACATTG-3′ [27]. The 18 S gene was used as an internal control.
Enzyme-linked immunosorbent assay (ELISA)
Serum levels of autoantibodies against Sjögren’s syndrome-related antigen A (SSA, AVALREYRKKMDIPA) and M3 muscarinic receptor (M3R, VLVNTFCDSCIPKTYWNLGY) were examined by ELISA. Briefly, 96-well plates were coated with antigen peptides (5 μg/ml). The peptides were synthesized chemically and purified by high-performance liquid chromatography (SBS Genetec Co., Ltd.). Serum samples were incubated in plates for 2 h and incubated with biotin-conjugated anti-mouse IgG (BioLegend) for 1 h at room temperature. After washing, HRP streptavidin (BioLegend) was added and incubated in the plate for 30 min. TMB substrate (BioLegend) was freshly prepared and added to the plate. After incubation, stop solution (3 M H2SO4) was added, and the absorbance (at 450 nm) was measured with a Sunrise microplate reader (Tecan).
Chromatin immunoprecipitation (ChIP) assay
ChIP was performed by following the protocol of the ChIP Assay Kit (Beyotime, #P2078). Briefly, each 10 cm dish of MDSCs (1 × 107) was treated with IPA, CH223191, or vehicle for 72 h. Then, the cells were cross-linked with 1% formaldehyde and washed with cold PBS. The harvested cells were subjected to cellular and nuclear lysis. The whole nuclear lysate was sheared by a sonicator under optimal conditions (10 s pulse on, 20 s pulse off, 20 cycles, 40% amplitude) to yield 200–800 bp DNA. Twenty microliters of sheared lysate was aliquoted as input. The remaining 2 mL of the sheared lysate was subjected to immunoprecipitation by overnight incubation with either an anti-IRF4 antibody (BioLegend, #646402) or IgG control. The immunoprecipitated DNA and input DNA were purified and amplified by qPCR with the primers listed in Supplementary Table 2.
Statistical analysis
GraphPad Prism 6 was used for the overall statistical analysis in this study. Statistical comparisons were performed using the Mann‒Whitney U-test for comparisons between two groups, while multiple comparisons were evaluated by one-way ANOVA. Two-way ANOVA was used for multiple variables. The results are expressed as the mean ± SD. P < 0.05 was considered to be statistically significant.
Results
AhR activation promotes PMN-MDSC regulatory function
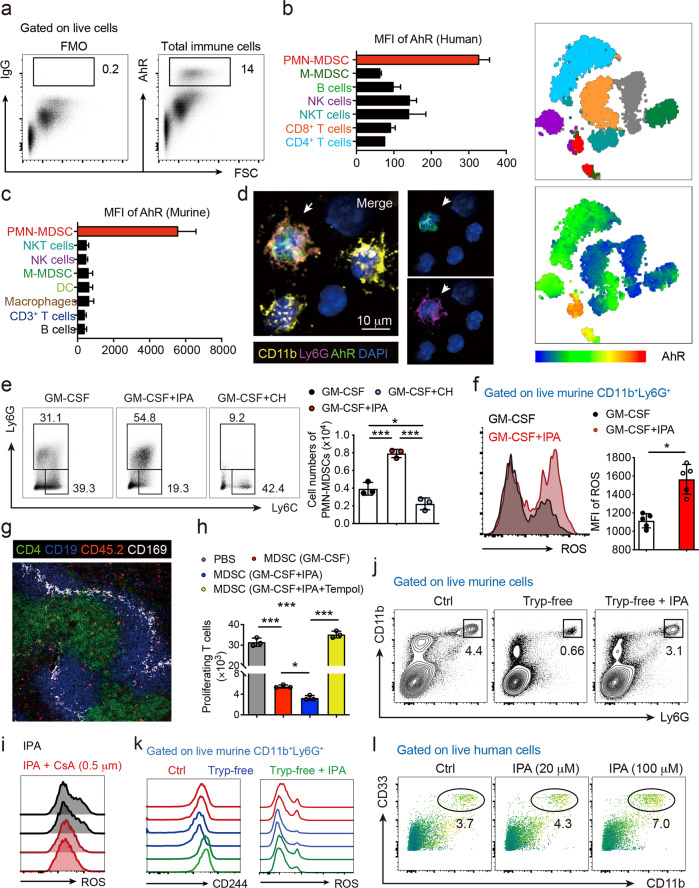
We first performed a phenotypic analysis of AhR expression. AhR was found to be expressed by a small fraction of human immune cells from healthy donors (Fig. 1a). Interestingly, t-distributed stochastic neighbor embedding (t-SNE) analysis showed that PMN-MDSCs expressed high levels of AhR compared with other immune cell lineages (Fig. 1b). Similarly, PMN-MDSCs were found to express the highest levels of AhR among various immune cell subsets in WT mice (Fig. 1c) when intracellular expression of AhR was further visualized (Fig. 1d). Thus, these results indicate that AhR may be closely involved in modulating the PMN-MDSC response.
Fig. 1.
AhR activation promotes the PMN-MDSC response. a Representative flow cytometric analysis was performed to analyze the intranuclear staining of AhR in PBMCs from healthy donors. b, c t-SNE plot and mean fluorescence intensity (MFI) of AhR expression among various immune cell subsets from both humans and mice, showing that AhR was highly and predominantly expressed in PMN-MDSCs (n = 3). d Representative images of murine PMN-MDSCs visualized by fluorescence microscopy to detect intracellular AhR staining (n = 5). e Murine bone marrow cells were isolated and cultured under MDSC polarization conditions for 3 days in the presence or absence of IPA and CH223191 (n = 3 in each group), and the frequency and number of PMN-MDSCs were analyzed. f ROS production by splenic PMN-MDSCs was measured by analyzing the fluorescence intensity of DCFH-DA (n = 5). g CD45.2+ PMN-MDSCs were adoptively transferred to congenic CD45.1+ mice. Representative image showing that within white pulp (marked by CD169, white), CD45.2+ PMN-MDSCs (red) appeared mainly in the CD4+ T-cell zones (green) and T-B borders in the spleen. h Murine bone marrow cells were isolated and cultured under MDSC polarization conditions in the presence or absence of IPA for 3 days. PMN-MDSCs were sorted, purified, and cocultured with CFSE-labeled CD4+ T cells with or without the ROS scavenger Tempol. T-cell proliferation was determined by measuring the CFSE fluorescence intensity by flow cytometry (n = 3). i IPA and NADPH oxidase inhibitor cyclosporin A (CsA) were cotreated with MDSCs upon polarization, and intracellular ROS production was detected by flow cytometry. j, k The frequencies of splenic PMN-MDSCs were analyzed by flow cytometry in mice fed a normal diet (Ctrl) and tryptophan-free diet with or without IPA supplementation for 2 weeks (j), and the MFI values of CD244 and ROS were determined (m) (n = 5). l PBMCs from healthy donors were polarized toward MDSC in the absence or presence of IPA for 6 days, and CD33+CD11b+CD66b+ PMN-MDSCs were analyzed (n = 3). Data were derived from at least three independent experiments. Data were presented as the mean ± SD. ns, not significant. *P < 0.05, **P < 0.01, and ***P < 0.001
To determine the potential effect of AhR activation in MDSCs, purified splenic PMN-MDSCs and M-MDSCs were first incubated with IPA, a natural AhR ligand. In culture, IPA treatment did not affect the survival of PMN-MDSCs, M-MDSCs or neutrophils (Supplementary Fig. 1a, b). Next, purified BMCs were cultured for MDSC differentiation in the presence of IPA. Flow cytometric analyses showed that PMN-MDSC differentiation and proliferation were significantly promoted upon AhR activation with IPA but suppressed by CH223191, a selective AhR antagonist (Fig. 1e and Supplementary Fig. 1c). Moreover, IPA treatment enhanced the production of ROS (Fig. 1f), a regulatory molecule mainly produced by PMN-MDSCs and involved in mediating antigen-specific T-cell suppression [4]. In addition, we performed the adoptive transfer of CD45.2 C57BL/6 MDSCs into congenic CD45.1 Boy/J mice. As indicated by the positions of CD169+ marginal zone metallophilic macrophages, transferred MDSCs localized to the white pulp T-cell zone and T-B borders in the spleen, potentiating their interaction with T cells in situ (Fig. 1g). To assess the function of PMN-MDSCs, we cultured differentiated PMN-MDSCs with CFSE-labeled naïve CD4+ T cells for a proliferation assay (T-cell/PMN-MDSC ratio = 2:1). As expected, IPA-treated PMN-MDSCs elicited more potent inhibitory effects on T-cell proliferation, which could be abrogated by cotreatment with the ROS scavenger Tempol (Fig. 1h). This finding was supported by previous studies showing that AhR agonists could promote the activities of NADPH oxidases [28], the major source of intracellular ROS production [29]. Consistent with these observations, IPA-mediated ROS production was abolished by the selective NADPH oxidase inhibitor cyclosporin A (Fig. 1i).
IPA is an exclusive indole metabolite converted from tryptophan that accumulates in host serum [30]. Interestingly, mice fed a tryptophan-free diet exhibited diminished splenic PMN-MDSCs with reduced ROS production and expression of CD244 (Fig. 1j, k, Supplementary Fig. 1d, e), a recently reported phenotypic marker expressed by PMN-MDSCs but not neutrophils [31]. Similar findings were also observed in PMN-MDSCs from the peripheral blood, albeit not in those from the bone marrow. Notably, the impaired PMN-MDSC response in mice given a tryptophan-free diet could be restored by IPA supplementation. In addition, IPA treatment enhanced human PMN-MDSC differentiation from PBMCs (Fig. 1l). Together, these data demonstrated a pivotal function of AhR activation in regulating the PMN-MDSC response.
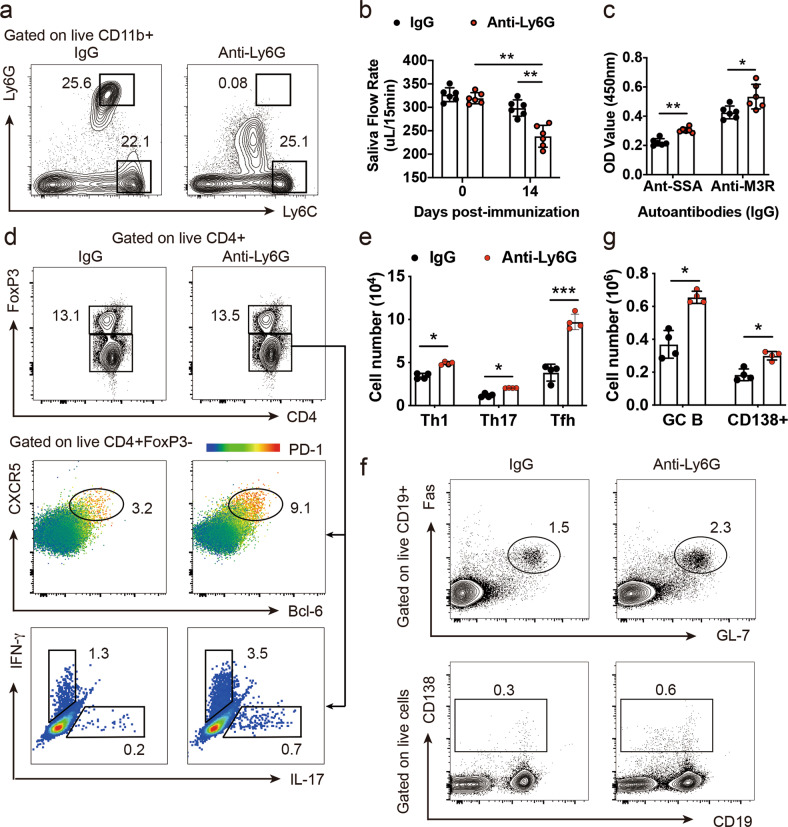
Defective PMN-MDSC function exacerbates ESS development with enhanced T-cell responses
Our previous studies suggested impaired regulatory functions of MDSCs from pSS patients and ESS mice [14]. To investigate whether defective PMN-MDSCs contribute to the dysregulation of effector CD4+ T cells, particularly Th1, Th17, and Tfh cells [7–9, 12], during ESS development, we first treated immunized mice with anti-Ly6G neutralizing antibodies upon ESS induction (Fig. 2a). In ESS mice with PMN-MDSC depletion, disease progression was markedly exacerbated, as shown by the accelerated reduction in salivary flow rate and elevated serum levels of autoantibodies (Fig. 2b, c). Moreover, phenotypic analyses revealed an enhanced splenic effector CD4+ T-cell response, including increases in the proportions of Th1, Th17, and Tfh cells, upon in vivo depletion of PMN-MDSCs, suggesting a critical involvement of PMN-MDSCs in restraining effector T cells during ESS development (Fig. 2d, e). Consequently, CD19+GL-7+Fas+ germinal center (GC) B cells, as well as CD138+ plasma cells, were also markedly increased (Fig. 2f, g), and this was associated with elevated autoantibody levels. Thus, these results identified a critical role of PMN-MDSCs in the development of ESS.
Fig. 2.
Defective PMN-MDSC function exacerbates ESS development in mice. a Representative flow cytometric analysis showed the efficacy of PMN-MDSC depletion in the spleens of ESS mice with an anti-Ly6G neutralizing antibody. b, c ESS pathology was accelerated in anti-Ly6G-treated ESS mice with obvious salivary hypofunction (b) and elevated autoantibodies (c) at Day 14 post-immunization (n = 6). d, e Representative flow cytometric analysis showed phenotypic analysis (d) and numbers (e) of T effector cell subsets, including PD-1+CXCR5+Bcl-6+Tfh, IFN-γ+Th1, and IL-17+Th17 cells in the spleens of ESS mice with or without anti-Ly6G treatment. f, g Representative flow cytometric analysis showed phenotypic analysis (f) and numbers (g) of GL-7+Fas+ germinal center B cells and plasma cells in the spleens of ESS mice, respectively. Data were derived from at least three independent experiments. Data were presented as the mean ± SD. *P < 0.05, **P < 0.01 and ***P < 0.001
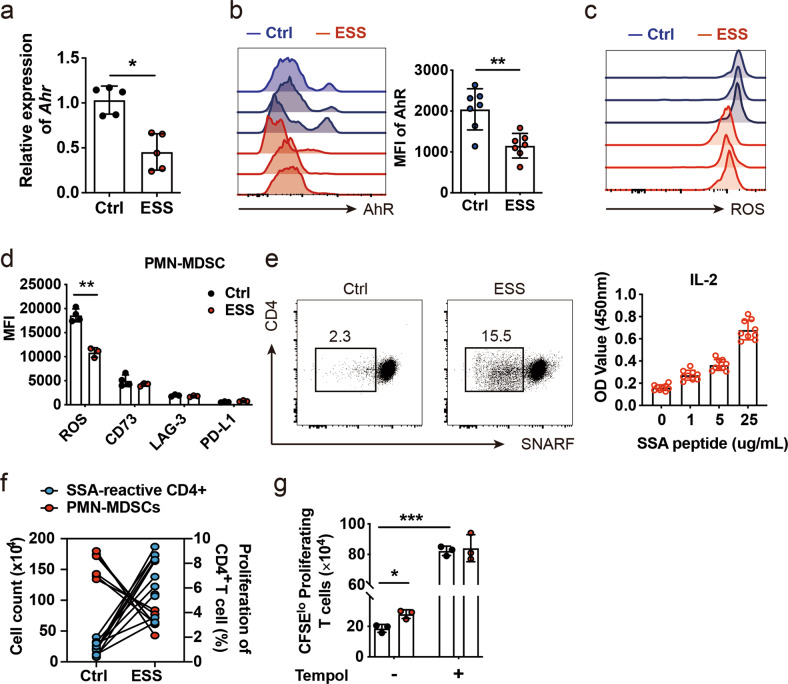
AhR modulates PMN-MDSC function during ESS development
In ESS mice, we detected significantly downregulated AhR expression at both the mRNA (Fig. 3a) and protein levels (Fig. 3b) in PMN-MDSCs; reduced ROS production during ESS progression was also detected in these cells (Fig. 3c). Similar results were also observed in NOD mice with SS-like symptoms (Supplementary Fig. 2). Interestingly, no obvious change in the expression levels of other regulatory molecules [32], such as CD73, LAG-3, and PD-L1, was detected in PMN-MDSCs from ESS mice (Fig. 3d). In contrast to the increased CD4+ T-cell responses detected in ESS mice, the cell counts of PMN-MDSCs were significantly decreased (Fig. 3e, f). We further assessed the suppressive function of PMN-MDSCs on the T-cell response. Consistently, PMN-MDSCs from ESS mice exhibited impaired regulatory function with downregulated AhR expression compared with naïve controls, an effect that could be abolished by treatment with ROS scavengers (Fig. 3g).
Fig. 3.
Reduced AhR expression is associated with a defective PMN-MDSC response in ESS development. a, b The expression of AhR was determined in splenic PMN-MDSCs from naïve and ESS mice by qPCR (a) and flow cytometric analysis (b). c, d Splenic PMN-MDSCs from naïve and ESS mice were sorting-purified for detection of regulatory molecules (d) by flow cytometry, and a representative histogram showed intracellular ROS production (c). e CD44+CD4+ T cells from naïve control (Ctrl) or ESS mice were sorting-purified and cocultured with SG protein-loaded dendritic cells for 24 h; rapid proliferation of SNARFlo autoreactive CD4+ T cells was detected by flow cytometry, and IL-2 production by CD44+CD4+ T cells from ESS mice was measured by ELISA in a dose-dependent manner. f Proliferative CD4+ T cells were stimulated with SG protein, and splenic PMN-MDSCs were enumerated in Ctrl and ESS mice. g Splenic PMN-MDSCs from naïve and ESS mice were sorting-purified and subjected to coculture with CD4+ T cells in the presence or absence of Tempol, and proliferative T cells were analyzed by flow cytometry. Data were derived from at least three independent experiments. Data were presented as the mean ± SD. *P < 0.05 and **P < 0.01
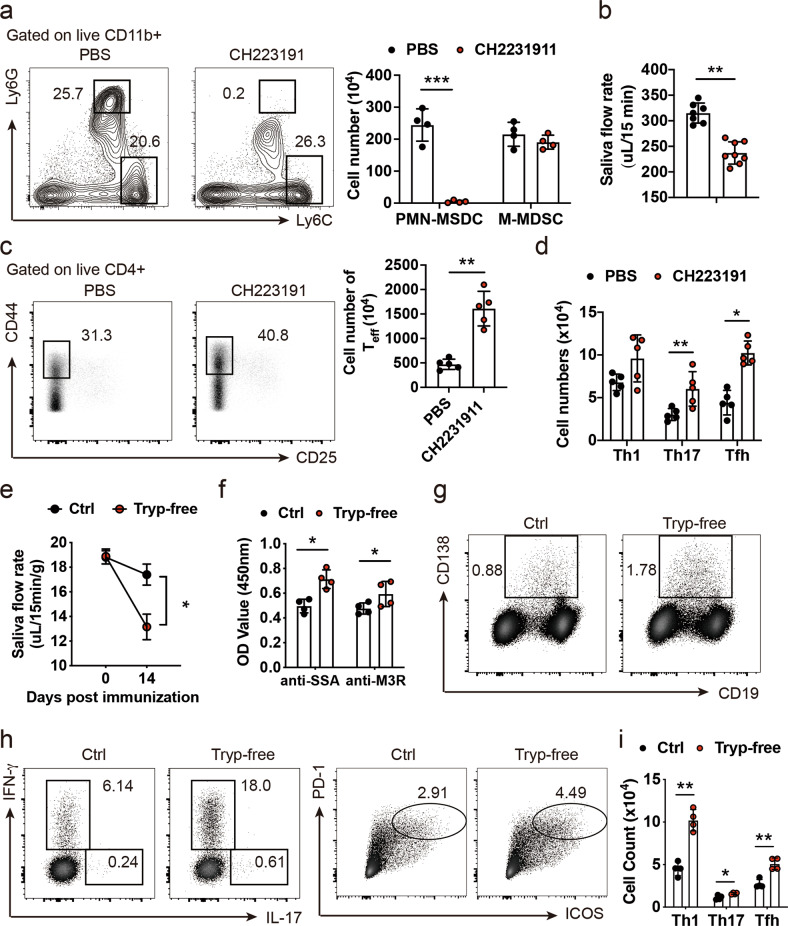
To further determine the role of AhR in modulating the functional changes of PMN-MDSCs during disease progression, the selective AhR antagonist CH223191 was used. Interestingly, CH223191 significantly decreased the viability of PMN-MDSCs, as well as neutrophils (Supplementary Fig. 3), consistent with recent findings that CH223191 treatment could induce apoptosis pathway and result in decreased cell viability [33]. Consistently, treatment with CH223191 phenocopied the effect of PMN-MDSC depletion in mice treated with anti-Ly6G neutralizing antibodies, showing that the frequencies of PMN-MDSCs were markedly diminished while those of M-MDSCs remained unaffected (Fig. 4a). Consistently, AhR antagonism resulted in exacerbated ESS pathology and dysregulated effector T-cell responses (Fig. 4b, c), including increases in Th1, Th17, and Tfh cell subsets (Fig. 4d). Moreover, we confirmed this finding in ESS mice fed a tryptophan-free diet. ESS mice with dietary tryptophan deficiency also exhibited a defective PMN-MDSC response and accelerated ESS pathology (Fig. 4e, g), with significantly enhanced Th1, Th17, and Tfh cell responses detected by flow cytometric analysis (Fig. 4h, i). Together, these results demonstrated that the downregulation of AhR in PMN-MDSCs contributed to their impaired regulatory function during ESS development.
Fig. 4.
AhR antagonism suppresses PMN-MDSCs and aggravates ESS development. a Representative flow cytometric analysis and numbers of MDSCs in the spleens of ESS mice treated with PBS or CH2231911. b Salivary function was assessed in ESS mice treated with PBS or CH2231911 14 days post-immunization (n = 8). c, d Splenic CD4+CD44+ T effector cells, including Th1, Th17, and Tfh subsets, were examined and enumerated (n = 5). e, f Upon ESS induction, immunized mice were fed a normal diet (Ctrl) or tryptophan-free diet for 14 days, and the salivary function and serum levels of autoantibodies were assessed (n = 4). g Representative flow cytometric analysis of plasma cells in the spleen of ESS mice fed a control or tryptophan-free diet. h, i Representative flow cytometric analysis of Th1, Th17, and Tfh cells (h) in the spleen of ESS mice fed a control or tryptophan-free diet, which were further enumerated (i). Data were derived from at least three independent experiments. Data were presented as the mean ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001
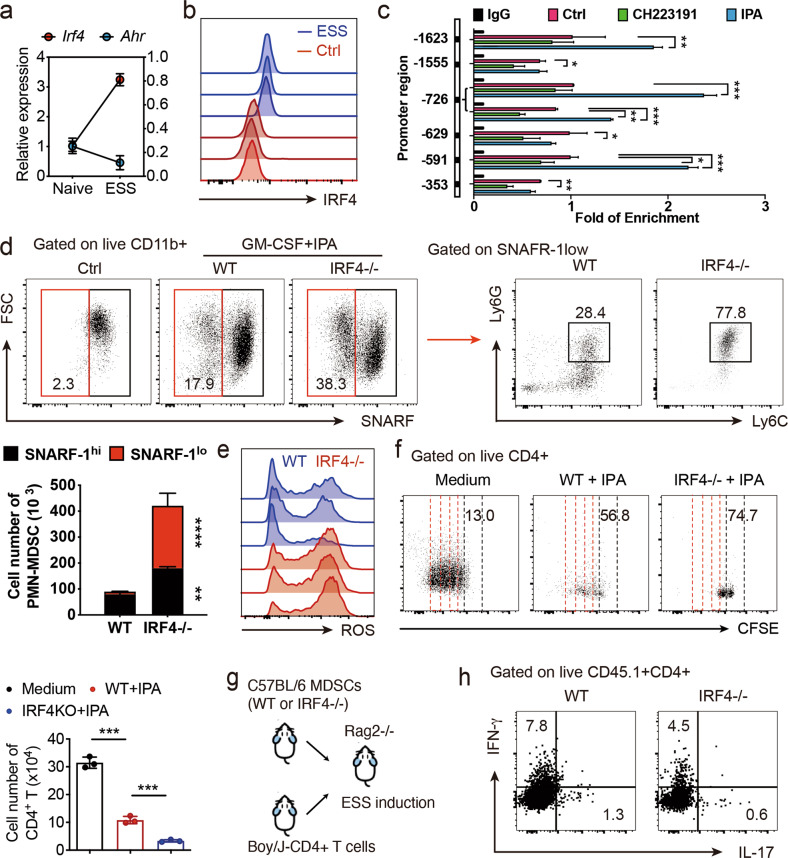
IRF4 negatively regulates the AhR-mediated PMN-MDSC response
To investigate the mechanisms underlying defective AhR signaling during ESS development, we performed transcriptome analysis and determined the possible impacts of the differences in gene expression on free radical production [34, 35]. We predicted that IRF4 could potentially bind to the promoter region of AhR but not cytosolic regulatory subunits (jaspar.genereg.net/). During ESS development, IRF4 expression was markedly increased in PMN-MDSCs and inversely correlated with AhR expression (Fig. 5a, b). This observation coincided with previous findings that IRF4 served as a transcriptional repressor in MDSC differentiation [18]. Thus, anti-IRF4 ChIP-PCR analysis was performed in differentiated PMN-MDSCs, showing the binding sites of IRF4 in the AhR promoter (Fig. 5c). Notably, given that AhR was mainly expressed by PMN-MDSCs, with equal amounts of input, AhR immunoprecipitation by IRF4 was increased by IPA-mediated PMN-MDSC expansion and decreased by CH223191 treatment. We next purified BMCs from IRF4−/− mice and cultured them under MDSC polarization conditions in the presence of IPA. IRF4−/− MDSC proliferation and PMN-MDSC differentiation were markedly enhanced compared with those of the wild-type controls. As shown in Fig. 5d, IPA-mediated IRF4−/− PMN-MDSCs were significantly expanded, by 30-fold. Consistent with this observation, treatment with simvastatin, an IRF4 inhibitor, also promoted IPA-mediated PMN-MDSC differentiation (Supplementary Fig. 4). Although IRF4−/− PMN-MDSCs exhibited ROS production comparable to that of WT controls at steady state (data not shown), markedly enhanced ROS generation was detected in IRF4−/− PMN-MDSCs upon AhR activation with IPA (Fig. 5e). Consequently, IRF4 deficiency further boosted the IPA-induced suppressive function of PMN-MDSCs in cocultures (Fig. 5f). Furthermore, IPA-differentiated WT or IRF4−/− CD45.2+PMN-MDSCs were adoptively cotransferred with CD45.1+CD4+ T cells into Rag2−/− mice, followed by ESS induction (Fig. 5g). As expected, IRF4−/− PMN-MDSCs elicited more potent suppressive effects on Th1 and Th17 responses in vivo (Fig. 5h). Together, these results demonstrate that IRF4 is a negative regulator of AhR signaling.
Fig. 5.
IRF4 negatively regulates the AhR-mediated PMN-MDSC response. a, b IRF4 expression in splenic PMN-MDSCs from naïve and ESS mice was determined by qPCR (a) and flow cytometric (b) analyses (n = 3). c MDSCs were polarized with various treatments for 3 days, and anti-IRF4 ChIP-PCR was performed to reveal the binding sites in the AhR promoter. d Wild-type (WT) or IRF4−/− BMCs were cultured for MDSC polarization in the presence or absence of IPA treatment, and PMN-MDSC differentiation and proliferation were assessed by flow cytometry. The proliferative SNARFlo PMN-MDSCs were further enumerated. e Representative flow cytometric analysis showed ROS production by IPA-induced WT or IRF4−/− PMN-MDSCs. f WT or IRF4−/− PMN-MDSCs induced by IPA were sorted, purified, and cocultured with CD4+ T cells under anti-CD3/28 mAb activation conditions for 3 days. Representative flow cytometric analysis showed T-cell proliferation (T-cell/PMN-MDSC ratio 2:1, n = 3). g, h IPA-induced WT or IRF4−/− MDSCs from CD45.2 C57BL/6 mice were adoptively cotransferred with CD45.1+CD4+ T cells from congenic Boy/J mice into immunodeficient Rag2−/− mice, followed by ESS induction. Representative flow cytometric analysis showed splenic Th1 and Th17-cell subsets in the recipient mice. Data were derived from at least three independent experiments. Data were presented as the mean ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001
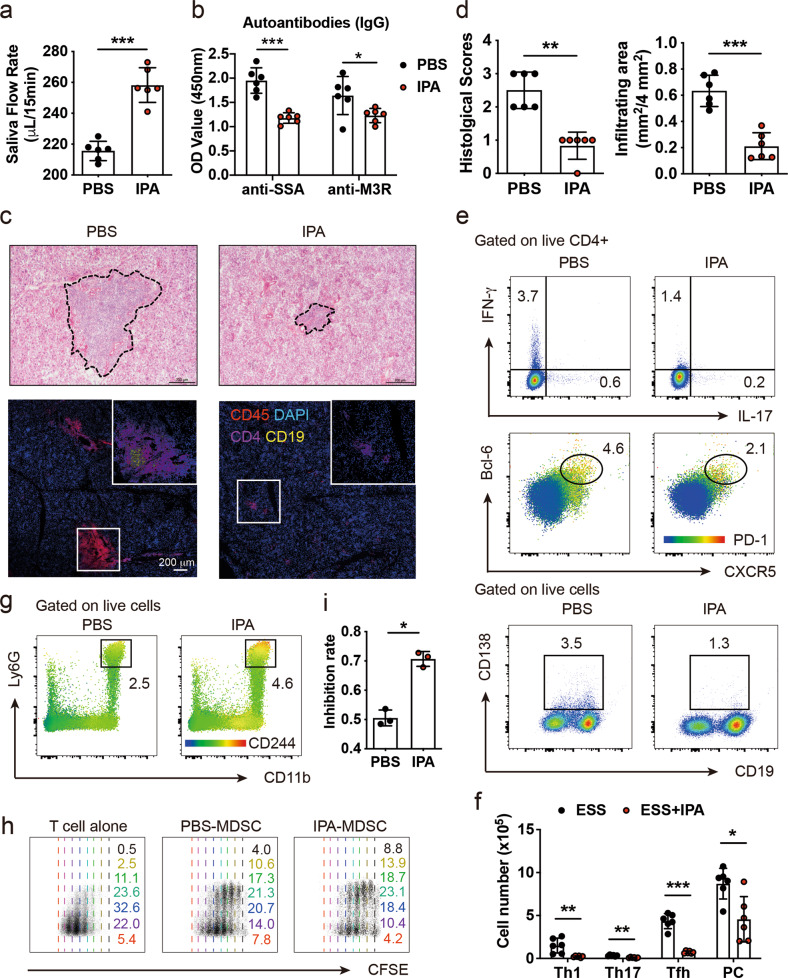
IPA treatment ameliorates disease development in ESS mice
Given the dietary importance of tryptophan metabolites in controlling the homeostasis of PMN-MDSCs, we next sought to explore whether IPA supplementation could restore their regulatory function and elicit therapeutic effects in treating ESS. Upon disease onset, ESS mice were treated with IPA or PBS vehicle twice a week for 8 weeks. Improved salivary function and decreased levels of serum autoantibodies were observed in IPA-treated ESS mice (Fig. 6a, b). To assess the therapeutic effects of IPA on histopathological changes, ESS mice were treated with IPA for 8 weeks beginning at 20 weeks post-immunization. Massive lymphocytic infiltrations, predominantly of CD4+ T cells and B cells, were detected surrounding acinar and ductal lobules in the SG of ESS mice treated with PBS vehicle, while IPA treatment significantly ameliorated SG pathology, showing only mild infiltrations (Fig. 6c, d). Phenotypic analysis revealed markedly reduced effector T-cell subsets, including Th1, Th17, and Tfh cell responses, in IPA-treated ESS mice (Fig. 6e, f), but the frequencies of regulatory T cells were not affected (data not shown). Consistent with the observed lower serum levels of autoantibodies, the levels of plasma cells were also found to be decreased upon IPA treatment. We further confirmed the enhanced PMN-MDSC response in IPA-treated ESS mice compared with those treated with vehicle (Fig. 6g). Notably, MDSCs purified from IPA-treated ESS mice showed a stronger inhibitory function on T-cell proliferation in cocultures (Fig. 6h, i). Moreover, ESS mice fed tryptophan supplements showed ameliorated disease severity with reduced T effector cells (Supplementary Fig. 5). Together, these results demonstrated the therapeutic effect of targeting AhR in suppressing ESS development by enhancing the PMN-MDSC response.
Fig. 6.
IPA treatment enhances the suppressive function of MDSCs and attenuates disease severity in ESS mice. a, b Immunized ESS mice were treated with PBS vehicle or IPA for 8 weeks, and the disease pathology, including salivary function (a) and autoantibodies against M3R and SSA (b), was assessed (n = 6). c, d ESS mice 20 weeks post-immunization were treated with PBS vehicle or IPA for 8 weeks. The histopathological changes in SGs, including tissue damage and infiltrating CD4+ T cells and B cells, were visualized, and the histological scores and infiltrated areas were evaluated. e, f Representative phenotypic analyses of Th1, Th17, Tfh, and plasma cells in the spleens are shown, and the numbers are summarized (n = 6). g Representative flow cytometric analysis of splenic PMN-MDSCs from ESS mice treated with PBS or IPA. h, i Splenic MDSCs from ESS mice were sorting-purified and cocultured with CFSE-labeled CD4+ T cells (T-cell/MDSC ratio of 2:1) for 3 days, and T-cell proliferation was assessed by flow cytometry (h). The inhibition rate was deduced (i). Data were derived from at least three independent experiments. Data were presented as the mean ± SD. *P < 0.05, **P < 0.01, and ***P < 0.001
Discussion
The defective function of regulatory immune cells during pSS development has been reported recently, but the underlying mechanisms remain largely unclear [8, 12, 14, 36]. Here, we identified that AhR was highly expressed in PMN-MDSCs but decreased during ESS progression, along with reduced ROS production and impaired regulatory function. Furthermore, we revealed that AhR engagement strictly controlled the proliferation, differentiation, and regulatory function of PMN-MDSCs, as AhR antagonism or a tryptophan-free diet significantly aggravated ESS severity, and that IRF4 served as a negative regulator upon AhR activation. Importantly, IPA supplementation enhanced the PMN-MDSC response and ameliorated ESS development in mice.
Several lines of evidence indicate that AhR is critically involved in various biological processes, including malignant transformation, hematopoietic cell development, and fate determination of immune cell lineages [37]. Extensive studies have suggested that AhR activation promotes immune tolerance in the intestine by inducing regulatory T cells directly or indirectly [38–41]. In addition, the endogenous AhR ligand 2-(1′H-indole-3′-carbonyl)-thiazole-4-carboxylic acid methyl ester (ITE) could induce tolerogenic dendritic cells, further supporting regulatory T-cell differentiation [40]. In mice with experimental colitis, indole-3-pyruvic acid-mediated AhR activation could induce the differentiation of type 1 regulatory T cells, while IPA promoted an increase in the number of CD103+CD11b− dendritic cells [42]. Recent studies also suggested an important role of AhR in both murine and human macrophages in the pathogenesis of SLE [43]. Therefore, accumulating evidence indicates that AhR is a promising target for the treatment of autoimmune disorders [44, 45]. Indeed, oral administration of the AhR agonist laquinimod or ITE has been shown to attenuate disease severity in mice with experimental autoimmune encephalomyelitis [40, 46]. In the present study, we further demonstrated that AhR was also critically involved in regulating the PMN-MDSC response during ESS pathogenesis, suggesting that AhR signaling might serve as a novel drug target in treating patients with pSS.
Previous studies have reported the preclinical application of cell therapy with PMN-MDSCs, including mouse models of multiple sclerosis [47] and rheumatoid arthritis [48], by suppressing effector T-cell subsets. We have recently shown that olfactory ecto-mesenchymal stem cell-derived exosomes can significantly enhance the suppressive function of MDSCs by upregulating arginase expression with increased ROS and NO levels as well as suppressing the development of ESS in mice [36]. In contrast, M-MDSC transfer resulted in increased disease severity and incidence as well as elevation of Th17 cells [49]. Emerging studies have reported that transcription factors, such as CEBPB [50] and STAT3 [15], are involved in MDSC development or function. IRF4, a member of the interferon regulatory family of transcription factors, was found to be essential for maintaining the differentiation and homeostasis of various immune cell subsets, including dendritic cells and macrophages [16, 17]. However, aberrant levels of IRF4 are highly associated with autoimmune disorders [51]. Recently, Nam S. et al. showed that IRF4 expression decreased in MDSCs during tumor development, while MDSCs with lower IRF4 levels exhibited greater suppression of T-cell proliferation [18]. This finding coincided with our findings that IRF4 was negatively associated with PMN-MDSC count and regulatory function. Although various stimuli could contribute to IRF4 regulation [51], the mechanism underlying enhanced IRF4 expression in pSS pathogenesis remains elusive. Interestingly, we found that IRF4 deficiency or antagonism markedly promoted the IPA-mediated PMN-MDSC response, as IRF4−/− PMN-MDSCs exhibited enhanced ROS production and more potent inhibitory function in cultures, which may potentiate the possible synergism of AhR activation and IRF4 antagonism for therapeutic approaches.
In conclusion, our results first revealed that AhR plays a critical role in regulating the PMN-MDSC response and that defective AhR activation contributes to the impaired regulatory function of PMN-MDSCs during autoimmune progression. Moreover, IPA, as a dietary tryptophan metabolite, can effectively ameliorate ESS development with restored MDSC function. Together, our findings indicate that targeting AhR may serve as a novel therapeutic approach for treating human pSS.
Supplementary information
Acknowledgements
This work was supported by the Chongqing International Institute for Immunology (2020YJC10), the National Natural Science Foundation of China (NSFC) (82071817, 81971542, and 82171771), the Hong Kong Research Grants Council General Research Fund (17113319 and 27111820) and Theme-Based Research Scheme (T12-703/19 R), the Shenzhen Science and Technology Program (YCYJ20210324114602008) and the Centre for Oncology and Immunology under the Health@InnoHK Initiative of the Innovation and Technology Commission, Hong Kong, China.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Yanxia Wei, Na Peng.
Contributor Information
Ke Rui, Email: ruike@ujs.edu.cn.
Xiang Lin, Email: linxiang@hku.hk.
Liwei Lu, Email: liweilu@hku.hk.
Supplementary information
The online version contains supplementary material available at 10.1038/s41423-022-00943-5.
References
- 1.Nagaraj S, Youn JI, Gabrilovich DI. Reciprocal relationship between myeloid-derived suppressor cells and T cells. J Immunol. 2013;191:17–23. doi: 10.4049/jimmunol.1300654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Knier B, Hiltensperger M, Sie C, Aly L, Lepennetier G, Engleitner T, et al. Myeloid-derived suppressor cells control B cell accumulation in the central nervous system during autoimmunity. Nat Immunol. 2018;19:1341–51. doi: 10.1038/s41590-018-0237-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alshetaiwi H, Pervolarakis N, McIntyre LL, Ma D, Nguyen Q, Rath JA, et al. Defining the emergence of myeloid-derived suppressor cells in breast cancer using single-cell transcriptomics. Sci Immunol. 2020;5:5341. doi: 10.1126/sciimmunol.aay6017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Otsuji M, Kimura Y, Aoe T, Okamoto Y, Saito T. Oxidative stress by tumor-derived macrophages suppresses the expression of CD3 zeta chain of T-cell receptor complex and antigen-specific T-cell responses. Proc Natl Acad Sci USA. 1996;93:13119–24. doi: 10.1073/pnas.93.23.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Flores-Toro JA, Luo D, Gopinath A, Sarkisian MR, Campbell JJ, Charo IF, et al. CCR2 inhibition reduces tumor myeloid cells and unmasks a checkpoint inhibitor effect to slow progression of resistant murine gliomas. Proc Natl Acad Sci USA. 2020;117:1129–38. doi: 10.1073/pnas.1910856117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Park MJ, Lee SH, Kim EK, Lee EJ, Park SH, Kwok SK, et al. Myeloid-derived suppressor cells induce the expansion of regulatory B cells and ameliorate autoimmunity in the sanroque mouse model of systemic lupus erythematosus. Arthritis Rheumatol. 2016;68:2717–27. doi: 10.1002/art.39767. [DOI] [PubMed] [Google Scholar]
- 7.Nocturne G, Mariette X. Advances in understanding the pathogenesis of primary Sjogren’s syndrome. Nat Rev Rheumatol. 2013;9:544–56. doi: 10.1038/nrrheum.2013.110. [DOI] [PubMed] [Google Scholar]
- 8.Fu W, Liu X, Lin X, Feng H, Sun L, Li S, et al. Deficiency in T follicular regulatory cells promotes autoimmunity. J Exp Med. 2018;215:815–25. doi: 10.1084/jem.20170901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin X, Rui K, Deng J, Tian J, Wang X, Wang S, et al. Th17 cells play a critical role in the development of experimental Sjogren’s syndrome. Ann Rheum Dis. 2015;74:1302–10. doi: 10.1136/annrheumdis-2013-204584. [DOI] [PubMed] [Google Scholar]
- 10.Psianou K, Panagoulias I, Papanastasiou AD, de Lastic AL, Rodi M, Spantidea PI, et al. Clinical and immunological parameters of Sjogren’s syndrome. Autoimmun Rev. 2018;17:1053–64. doi: 10.1016/j.autrev.2018.05.005. [DOI] [PubMed] [Google Scholar]
- 11.Xiao F, Lin X, Tian J, Wang X, Chen Q, Rui K, et al. Proteasome inhibition suppresses Th17 cell generation and ameliorates autoimmune development in experimental Sjogren’s syndrome. Cell Mol Immunol. 2017;14:924–34. doi: 10.1038/cmi.2017.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lin X, Wang X, Xiao F, Ma K, Liu L, Wang X, et al. IL-10-producing regulatory B cells restrain the T follicular helper cell response in primary Sjogren’s syndrome. Cell Mol Immunol. 2019;16:921–31. doi: 10.1038/s41423-019-0227-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guggino G, Lin X, Rizzo A, Xiao F, Saieva L, Raimondo S, et al. Interleukin-25 axis is involved in the pathogenesis of human primary and experimental murine Sjogren’s syndrome. Arthritis Rheumatol. 2018;70:1265–75. doi: 10.1002/art.40500. [DOI] [PubMed] [Google Scholar]
- 14.Tian J, Rui K, Hong Y, Wang X, Xiao F, Lin X, et al. Increased GITRL impairs the function of myeloid-derived suppressor cells and exacerbates primary Sjogren syndrome. J Immunol. 2019;202:1693–703. doi: 10.4049/jimmunol.1801051. [DOI] [PubMed] [Google Scholar]
- 15.Kumar V, Cheng P, Condamine T, Mony S, Languino LR, McCaffrey JC, et al. CD45 phosphatase inhibits STAT3 transcription factor activity in myeloid cells and promotes tumor-associated macrophage differentiation. Immunity. 2016;44:303–15. doi: 10.1016/j.immuni.2016.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ainsua-Enrich E, Hatipoglu I, Kadel S, Turner S, Paul J, Singh S, et al. IRF4-dependent dendritic cells regulate CD8(+) T-cell differentiation and memory responses in influenza infection. Mucosal Immunol. 2019;12:1025–37. doi: 10.1038/s41385-019-0173-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chistiakov DA, Myasoedova VA, Revin VV, Orekhov AN, Bobryshev YV. The impact of interferon-regulatory factors to macrophage differentiation and polarization into M1 and M2. Immunobiology. 2018;223:101–11. doi: 10.1016/j.imbio.2017.10.005. [DOI] [PubMed] [Google Scholar]
- 18.Nam S, Kang K, Cha JS, Kim JW, Lee HG, Kim Y, et al. Interferon regulatory factor 4 (IRF4) controls myeloid-derived suppressor cell (MDSC) differentiation and function. J Leukoc Biol. 2016;100:1273–84. doi: 10.1189/jlb.1A0215-068RR. [DOI] [PubMed] [Google Scholar]
- 19.Goudot C, Coillard A, Villani AC, Gueguen P, Cros A, Sarkizova S, et al. Aryl hydrocarbon receptor controls monocyte differentiation into dendritic cells versus macrophages. Immunity. 2017;47:582–96.e586. doi: 10.1016/j.immuni.2017.08.016. [DOI] [PubMed] [Google Scholar]
- 20.Giani Tagliabue S, Faber SC, Motta S, Denison MS, Bonati L. Modeling the binding of diverse ligands within the Ah receptor ligand binding domain. Sci Rep. 2019;9:10693. doi: 10.1038/s41598-019-47138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rothhammer V, Mascanfroni ID, Bunse L, Takenaka MC, Kenison JE, Mayo L, et al. Type I interferons and microbial metabolites of tryptophan modulate astrocyte activity and central nervous system inflammation via the aryl hydrocarbon receptor. Nat Med. 2016;22:586–97. doi: 10.1038/nm.4106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hyland NP, Cavanaugh CR, Hornby PJ. Emerging effects of tryptophan pathway metabolites and intestinal microbiota on metabolism and intestinal function. Amino Acids. 2022;54:57–70. doi: 10.1007/s00726-022-03123-x. [DOI] [PubMed] [Google Scholar]
- 23.Coligan JE, Bierer BE, Margulies DH, Shevach EM, Strober W, Solito S, et al. Methods to measure MDSC immune suppressive activity in vitro and in vivo. Curr Protoc Immunol. 2019;124:e61. doi: 10.1002/cpim.61. [DOI] [PubMed] [Google Scholar]
- 24.Tian J, Ma J, Ma K, Guo H, Baidoo SE, Zhang Y, et al. beta-Glucan enhances antitumor immune responses by regulating differentiation and function of monocytic myeloid-derived suppressor cells. Eur J Immunol. 2013;43:1220–30. doi: 10.1002/eji.201242841. [DOI] [PubMed] [Google Scholar]
- 25.Veglia F, Perego M, Gabrilovich D. Myeloid-derived suppressor cells coming of age. Nat Immunol. 2018;19:108–19. doi: 10.1038/s41590-017-0022-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Krishnan S, Ding Y, Saedi N, Choi M, Sridharan GV, Sherr DH, et al. Gut microbiota-derived tryptophan metabolites modulate inflammatory response in hepatocytes and macrophages. Cell Rep. 2018;23:1099–111. doi: 10.1016/j.celrep.2018.03.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ouyang X, Zhang R, Yang J, Li Q, Qin L, Zhu C, et al. Transcription factor IRF8 directs a silencing programme for TH17 cell differentiation. Nat Commun. 2011;2:314. doi: 10.1038/ncomms1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wada T, Sunaga H, Ohkawara R, Shimba S. Aryl hydrocarbon receptor modulates NADPH oxidase activity via direct transcriptional regulation of p40phox expression. Mol Pharm. 2013;83:1133–40. doi: 10.1124/mol.112.083303. [DOI] [PubMed] [Google Scholar]
- 29.Fang S, Cheng Y, Deng F, Zhang B. RNF34 ablation promotes cerebrovascular remodeling and hypertension by increasing NADPH-derived ROS generation. Neurobiol Dis. 2021;156:105396. doi: 10.1016/j.nbd.2021.105396. [DOI] [PubMed] [Google Scholar]
- 30.Danaceau JP, Anderson GM, McMahon WM, Crouch DJ. A liquid chromatographic-tandem mass spectrometric method for the analysis of serotonin and related indoles in human whole blood. J Anal Toxicol. 2003;27:440–4. doi: 10.1093/jat/27.7.440. [DOI] [PubMed] [Google Scholar]
- 31.Youn JI, Collazo M, Shalova IN, Biswas SK, Gabrilovich DI. Characterization of the nature of granulocytic myeloid-derived suppressor cells in tumor-bearing mice. J Leukoc Biol. 2012;91:167–81. doi: 10.1189/jlb.0311177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhou J, Nefedova Y, Lei A, Gabrilovich D. Neutrophils and PMN-MDSC: their biological role and interaction with stromal cells. Semin Immunol. 2018;35:19–28. doi: 10.1016/j.smim.2017.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leja-Szpak A, Góralska M, Link-Lenczowski P, Czech U, Nawrot-Porąbka K, Bonior J, et al. The opposite effect of L-kynurenine and Ahr inhibitor Ch223191 on apoptotic protein expression in pancreatic carcinoma cells (Panc-1) Anticancer Agents Med Chem. 2019;19:2079–90. doi: 10.2174/1871520619666190415165212. [DOI] [PubMed] [Google Scholar]
- 34.Viola A, Munari F, Sánchez-Rodríguez R, Scolaro T, Castegna A. The metabolic signature of macrophage responses. Front Immunol. 2019;10:1462. doi: 10.3389/fimmu.2019.01462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Huang SCC, Smith AM, Everts B, Colonna M, Pearce EL, Schilling JD, et al. Metabolic reprogramming mediated by the mTORC2-IRF4 signaling axis is essential for macrophage alternative activation. Immunity. 2016;45:817–30. doi: 10.1016/j.immuni.2016.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rui K, Hong Y, Zhu Q, Shi X, Xiao F, Fu H, et al. Olfactory ecto-mesenchymal stem cell-derived exosomes ameliorate murine Sjogren’s syndrome by modulating the function of myeloid-derived suppressor cells. Cell Mol Immunol. 2021;18:440–51. doi: 10.1038/s41423-020-00587-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Trikha P, Lee DA. The role of AhR in transcriptional regulation of immune cell development and function. Biochim Biophys Acta Rev Cancer. 2020;1873:188335. doi: 10.1016/j.bbcan.2019.188335. [DOI] [PubMed] [Google Scholar]
- 38.Goettel JA, Gandhi R, Kenison JE, Yeste A, Murugaiyan G, Sambanthamoorthy S, et al. AHR activation is protective against colitis driven by T cells in humanized mice. Cell Rep. 2016;17:1318–29. doi: 10.1016/j.celrep.2016.09.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ye J, Qiu J, Bostick JW, Ueda A, Schjerven H, Li S, et al. The aryl hydrocarbon receptor preferentially marks and promotes gut regulatory T cells. Cell Rep. 2017;21:2277–90. doi: 10.1016/j.celrep.2017.10.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Quintana FJ, Murugaiyan G, Farez MF, Mitsdoerffer M, Tukpah AM, Burns EJ, et al. An endogenous aryl hydrocarbon receptor ligand acts on dendritic cells and T cells to suppress experimental autoimmune encephalomyelitis. Proc Natl Acad Sci USA. 2010;107:20768–73. doi: 10.1073/pnas.1009201107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hauben E, Gregori S, Draghici E, Migliavacca B, Olivieri S, Woisetschlager M, et al. Activation of the aryl hydrocarbon receptor promotes allograft-specific tolerance through direct and dendritic cell-mediated effects on regulatory T cells. Blood. 2008;112:1214–22. doi: 10.1182/blood-2007-08-109843. [DOI] [PubMed] [Google Scholar]
- 42.Aoki R, Aoki-Yoshida A, Suzuki C, Takayama Y. Indole-3-pyruvic acid, an aryl hydrocarbon receptor activator, suppresses experimental colitis in mice. J Immunol. 2018;201:3683–93. doi: 10.4049/jimmunol.1701734. [DOI] [PubMed] [Google Scholar]
- 43.Shinde R, Hezaveh K, Halaby MJ, Kloetgen A, Chakravarthy A, da Silva Medina T, et al. Apoptotic cell-induced AhR activity is required for immunological tolerance and suppression of systemic lupus erythematosus in mice and humans. Nat Immunol. 2018;19:571–82. doi: 10.1038/s41590-018-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Hickman-Brecks CL, Racz JL, Meyer DM, LaBranche TP, Allen PM. Th17 cells can provide B cell help in autoantibody induced arthritis. J Autoimmun. 2011;36:65–75. doi: 10.1016/j.jaut.2010.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wang Y, Schafer CC, Hough KP, Tousif S, Duncan SR, Kearney JF, et al. Myeloid-derived suppressor cells impair B cell responses in lung cancer through IL-7 and STAT5. J Immunol. 2018;201:278–95. doi: 10.4049/jimmunol.1701069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kaye J, Piryatinsky V, Birnberg T, Hingaly T, Raymond E, Kashi R, et al. Laquinimod arrests experimental autoimmune encephalomyelitis by activating the aryl hydrocarbon receptor. Proc Natl Acad Sci USA. 2016;113:E6145–E6152. doi: 10.1073/pnas.1607843113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ioannou M, Alissafi T, Lazaridis I, Deraos G, Matsoukas J, Gravanis A, et al. Crucial role of granulocytic myeloid-derived suppressor cells in the regulation of central nervous system autoimmune disease. J Immunol. 2012;188:1136–46. doi: 10.4049/jimmunol.1101816. [DOI] [PubMed] [Google Scholar]
- 48.Fujii W, Ashihara E, Hirai H, Nagahara H, Kajitani N, Fujioka K, et al. Myeloid-derived suppressor cells play crucial roles in the regulation of mouse collagen-induced arthritis. J Immunol. 2013;191:1073–81. doi: 10.4049/jimmunol.1203535. [DOI] [PubMed] [Google Scholar]
- 49.Guo C, Hu F, Yi H, Feng Z, Li C, Shi L, et al. Myeloid-derived suppressor cells have a proinflammatory role in the pathogenesis of autoimmune arthritis. Ann Rheum Dis. 2016;75:278–85. doi: 10.1136/annrheumdis-2014-205508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Li W, Tanikawa T, Kryczek I, Xia H, Li G, Wu K, et al. Aerobic glycolysis controls myeloid-derived suppressor cells and tumor immunity via a specific CEBPB isoform in triple-negative breast cancer. Cell Metab. 2018;28:87–103.e106. doi: 10.1016/j.cmet.2018.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Xu WD, Pan HF, Ye DQ, Xu Y. Targeting IRF4 in autoimmune diseases. Autoimmun Rev. 2012;11:918–24. doi: 10.1016/j.autrev.2012.08.011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.