Abstract
Physical activity has been known as an essential element to promote human health for centuries. Thus, exercise intervention is encouraged to battle against sedentary lifestyle. Recent rapid advances in molecular biotechnology have demonstrated that both endurance and resistance exercise training, two traditional types of exercise, trigger a series of physiological responses, unraveling the mechanisms of exercise regulating on the human body. Therefore, exercise has been expected as a candidate approach of alleviating a wide range of diseases, such as metabolic diseases, neurodegenerative disorders, tumors, and cardiovascular diseases. In particular, the capacity of exercise to promote tissue regeneration has attracted the attention of many researchers in recent decades. Since most adult human organs have a weak regenerative capacity, it is currently a key challenge in regenerative medicine to improve the efficiency of tissue regeneration. As research progresses, exercise-induced tissue regeneration seems to provide a novel approach for fighting against injury or senescence, establishing strong theoretical basis for more and more “exercise mimetics.” These drugs are acting as the pharmaceutical alternatives of those individuals who cannot experience the benefits of exercise. Here, we comprehensively provide a description of the benefits of exercise on tissue regeneration in diverse organs, mainly focusing on musculoskeletal system, cardiovascular system, and nervous system. We also discuss the underlying molecular mechanisms associated with the regenerative effects of exercise and emerging therapeutic exercise mimetics for regeneration, as well as the associated opportunities and challenges. We aim to describe an integrated perspective on the current advances of distinct physiological mechanisms associated with exercise-induced tissue regeneration on various organs and facilitate the development of drugs that mimics the benefits of exercise.
Subject terms: Medical research, Molecular biology
Introduction
Physical activity mainly refers to any bodily movement produced by skeletal muscles and results in energy expenditure, broadly encompassing exercise and sports, which have been done as part of daily living, occupation, leisure, and active transportation.1,2 Over the last few decades, physical activity has been convinced by clinical and experimental studies as an essential element of daily life and crucial to promote health and longevity.3–5 Importantly, it is reported that physical inactivity has become the fourth leading cause of death worldwide nowadays.6 According to 2020 World Health Organization (WHO) guidelines, it is stated that 150–300 min of moderate intensity, or 75–150 min of vigorous-intensity physical activity, or some equivalent combination of moderate intensity and vigorous-intensity aerobic physical activity should be undertaken per week.7 However, about one-third of adults worldwide do not meet the minimal intensity or time of physical activity recommended by WHO.8 Substantial evidence has shown that physical inactivity mostly has a negative impact on non-communicable diseases such as coronary heart disease,9 diabetes mellitus,10,11 cancer,12,13 and even mental health,14–16 dramatically aggravating the global health burden and shortening the life expectancy of people. Therefore, promotion of physical activity is one of the important methods to improve the quality of human lifespan.
Exercise is theoretically defined as a kind of planned, structured, and repetitive physical activity.1 As a kind of physical education activity and social cultural activity, regular exercise is accepted by more and more people. Basically, there are two types of exercise including endurance (aerobic) training and resistance (anaerobic) training (Fig. 1).17–20 Physiologically, endurance exercise training refers to the exercise in which glucose metabolism depends on oxygen under aerobic conditions, while resistance exercise training refers to the exercise in which weight or overload is carried out in anaerobic condition and it is a short period of high-intensity or maximal intensity activity.21–23 The former usually induces the adaptation of cardiovascular and respiratory systems, while the latter is more likely to result in muscle hypertrophy through increasing myofibrillar volume predominantly in type II fibers and it is accompanied by changes in central nervous system.24–27 According to the exercise testing and prescription guidelines of the American Academy of Sports Medicine,28 endurance exercise is a wide range of physical activities, such as walking, jogging, dancing, swimming and cycling, its intensity is lower than the maximum intensity and can last for several minutes to several hours.29 Endurance exercise training is based on the FITT (frequency, intensity, time, type)–VP (volume, progression) principle of exercise prescription, while the intensity of exercise can be described in terms of heart rate, oxygen consumption (VO2) and metabolic equivalent.2 Common resistance exercise training includes barbell bench press, barbell overhead squat, dumbbell bicep curl and other strength exercises. The optimal training load for strength training is still being explored.30 It is suggested that performing a single set of 6–12 repetitions with loads ranging from approximately 70–85% one repetition maximum 2–3 times per week may produce sufficient training effect.31 Indeed, the complexity of physical activities makes no such clear boundary between the two types of exercise, as endurance exercise may become anaerobic if the intensity of aerobic exercise exceeds the anaerobic threshold. With a better understanding of the physiological responses triggered by different types of exercise, a variety of exercise strategies have emerged, including high-intensity interval training (HIIT) and moderate-intensity continuous exercise training (MICT). Notably, HIIT is getting more popular among the fitness enthusiasts and athletes because it has demonstrated superiority in cardiorespiratory fitness,32–34 weight loss,35,36 and improvement of chronic diseases.37 Overall, the diversity of exercise triggers different physiological adaptations, allowing for the targeted utilization of exercise training to make improvements of the various physical states.
Fig. 1.
Benefits of exercise-induced tissue regeneration. a Exercise induces physiological hypertrophy of left ventricle and reduction of myocardial infarction area by promoting the proliferation of cardiomyocytes. b Exercise induces muscle hypertrophy by promoting the proliferation of the satellite cells in both physiological and pathological conditions. Angiogenesis and mitochondrial biosynthesis are helpful in delaying muscle fatigue. c Exercise enhances hippocampal neurogenesis, myelin regeneration, axon regeneration, and cerebral angiogenesis to improve the motor, sensory, and cognitive functions. Exercise can also improve the sensory and motor functions after spinal cord injury and promote survival and differentiation of transplanted stem cells. d Exercise increases the branches of nerve fibers in the proximal skin, and promotes axon cross-sectional area (CSA), myelin sheath thickness, Schwann cell’s nucleus area and neurogenesis, so as to relieve the pain, improving sensation and motor function of patients with peripheral neuropathy. e Exercise can change the bone marrow microenvironment, promote the proliferation of hematopoietic stem and progenitor cells and the production of leukocytes. f Exercise regulates skeletal stem cell to differentiate into osteoblasts and chondrocytes, as well as bone angiogenesis, increasing bone mineral density (BMD). Besides, exercise induces the regeneration of post-traumatic cartilage lesions. Exercise is also considered as an effective adjuvant to stem cell-based therapy and the application of biomaterials or devices for cartilage regeneration. g Exercise promotes the regeneration ability of fatty liver, improving its tolerance to ischemia. Besides, exercise can restore liver function by promoting hepatocyte proliferation and mitochondrial biosynthesis in patients with partial hepatectomy. Created with BioRender
Over the past centuries, exercise training has been regarded as an effective approach to enhance tissue function under normal physiological condition and restore function under diverse pathological conditions, including cardiovascular diseases,38–40 chronic metabolic syndromes,41,42 neurological and psychiatric disorders,43–45 and cancer,19,46–48 which are mainly treated by chemical drugs. However, many diseases with loss of functional cells rely on cell supplement for tissue or organ regeneration. Nowadays, the definition of regeneration has been getting more precise and clearer, known as embryonic regulation, homeostatic regeneration, and restorative regeneration, respectively.49,50 As restorative regeneration stands for the ultimate goal that implantation of regenerated tissue constructs into the body to repair injuries or replace the physiological function, it makes great sense to find out how homeostatic tissues initiate the regeneration program by triggering a coherent immune response, appropriate cell plasticity, as well as stem and stromal cell responses following injury.51 As is well known, the basic process of tissue or organ regeneration should involve various forms of cellular plasticity first, which means that regeneration of tissues damaged by various injury modify tissue architecture through coordinated cell proliferation, differentiation, and apoptosis.52 Regeneration physiologically contributes to homeostasis against cell apoptosis, but it shows so limited ability to repair ischemic or impaired tissue for fully functional recovery in several vital organs, for instance cardiovascular and nervous system.53–56 Therefore, many approaches are currently applied to tissue regeneration therapy, including activation of endogenous stem cells and supplement with exogenous stem cells.57–60 Importantly, it has been suggested in recent decades that exercise is also able to contribute to promoting the restoration of damaged tissues, which provides a novel theoretical basis for tissue regeneration.
Since research on restorative regeneration has attracted more and more attention, exercise-induced tissue regeneration provides new therapeutic strategies. Recently it has been reported that only high-intensity training can stimulate changes in markers of mitochondrial respiratory function in skeletal muscle and enhance oxidative phosphorylation levels,61 which proves that there is a dose-dependent response to exercise duration and/or intensity again.3 However, not all individuals are able to achieve the level of exercise needed to experience the wide range of health benefits that exercise provides. Thus, it has been one of the most fascinating topics how exercise affects various organs and promotes injury repair, which drives researchers to mimic these effects with pharmaceuticals. To develop effective therapeutic approaches, it is crucial to understand the underlying mechanisms of the regenerative effects triggered by exercise, at the level of molecules, cells, and systems. This review will summarize recent advances in the benefits of exercise on different vital organs, thereby revealing the underlying molecular mechanisms and the potential mimetics from the perspective of exercise-induced tissue regeneration for further research and clinical applications.
Benefits of exercise on tissue regeneration
Exercise-induced muscle regeneration
The musculoskeletal system is an integral component of mobility and strength in the human body. Skeletal muscles, as the most important component of the musculoskeletal system, are characterized by myofibers and connective tissue, making up more than 35% of the adult body and containing 50–75% of all body proteins.62 The mechanical injury, ischemia injury, inflammatory injury and even congenital or acquired atrophy are described as those that involve disrupted connective tissues, leading to loss of skeletal muscle mass, reduced motor unit discharge rate, and impaired function.63 It has been uncovered that moderate exercise training enhances muscle regeneration after injury, as skeletal muscle mass recovery after extensive injury can be improved by contractile activity. In general, it has been widely convinced that the local adaptations of endurance exercise in skeletal muscle mostly focus on increased mitochondrial biogenesis and capillary density, which aids in the body’s ability to transport and use oxygen to generate energy and therefore delay the onset of muscle fatigue during prolonged aerobic performance.64 However, it has been also shown that endurance exercise training promotes maintenance of muscle mass and recovery after injury.65,66 While in rat models of notexin-induced soleus muscle degeneration, running exercise ensured the full recovery of muscle mass and muscle cross-sectional area during muscle regeneration, and made muscle recovery much faster than sedentary group.67,68 In contrast, resistance exercise training is more conducive to an increase in muscle strength and power as a result of neuromuscular adaptations, increases in muscle cross-sectional area (CSA), and alterations in connective tissue stiffness.69 Strength training significantly improved protracted quadriceps muscle atrophy in anterior cruciate ligament reconstruction patients via increasing muscle fibers CSA and type I fibers.70 Of note, it has been reported that HIIT, the novel combination exercise training strategy, promotes muscle regeneration, innervation, and vascularization in regenerated areas of volumetric muscle loss injury, even enhancing the healing effect of stem cell transplantation with an amniotic membrane scaffold.71 As mentioned about muscle regeneration induced by various exercise training, further studies should seek to assess different loads/modes (uphill vs. flat) with the same volume to confirm whether this affects muscle regeneration following training and provide compound exercise patterns to improve the efficiency of muscle regeneration.
Myogenesis follows after early inflammation and revascularization, and later fibrosis and re-innervation, resulting restoration of muscle mass and function.72 The bona fide tissue-specific stem cell, considered as a key component in myogenesis, in human adult skeletal muscle is the satellite cell.73,74 It has been convinced that the satellite cells are activated, proliferating, and differentiating after muscle fibers get injured, whose mitotic activity can be enhanced by exercise in the forms of endurance or resistance exercise training.75,76 In addition, skeletal muscle regeneration by the modulation of satellite cells is affected by the balance between pro- and anti-inflammatory macrophages.77 Exercise has been confirmed to cause the transition from the M1 to M2 macrophage phenotype, regulating the satellite cells proliferation and differentiation in the injury sites.78–80 Moreover, fibro-adipogenic progenitors (FAPs) has also been confirmed to get activated in response to muscle injury and establish functional interactions with the inflammatory cells and the satellite cells to promote muscle repair.81–83 More recently, it has been demonstrated that exercise increases and activates satellite cells by promoting FAPs senescence in the mouse models of acute muscle injury and chronic inflammatory myopathy, which provides a new therapeutic strategy for exercise-induced muscle regeneration (Fig. 1b).84
Exercise-induced bone and cartilage regeneration
Briefly, the primary features of an ageing skeleton are loss of bone, degraded articular cartilage, and degenerate, narrowed intervertebral discs, contributing to pain and loss of mobility. Physical activity has long been recognized as an essential factor in the maintenance of skeletal health. An abundance of studies has shown that both endurance and resistance exercise physiologically promote bone growth of teenagers and increase peak bone mass, which contributes to prevention of osteoporosis in adult stages.85,86 Thus, it is convinced that the common decline in bone mass during ageing attenuates, by following specific exercise programs, especially in postmenopausal women.87 Although endurance exercise is important in maintaining overall health, the resistance training may be more applicable to the basic rules of bone adaptation and site-specific effects of exercise.88 Recently an 8-week of exercise protocol of resistance exercise or endurance exercise experiment confirmed resistance exercise, but not endurance exercise, is likely to be effective in increasing bone strength.89 Indeed, it has been confirmed that bone responds more positively to mechanical loads that induce high-magnitude strains at high rates or frequencies, such as quick jumping, which causes the weakness of exercise’s ability to evoke osteogenesis in traditional training patterns.90 Thus, Davison et al.91 established a novel exercise equipment and exercise training patterns to improve the efficiency of osteogenesis, giving hope to those afflicted with bone loss (osteoporosis, or osteopenia) conditions. In addition, bone regeneration also relies on vascularization of the ossifying tissue, called angiogenesis-osteogenesis coupling.92 Yao et al.93 found that treadmill running could physiologically increase vessel number in the proximal metaphysis of rats, and significant changes of bone mineral density (BMD) in response to exercise. Subsequently, a set of researches have clarified that exercise stimulates angiogenesis during bone defect healing, accelerating bone regeneration as well.94,95
Chondral injury is a pathology with high prevalence, reaching as much as 63% of general population and 36% among athletes.96,97 Despite inappropriate or excessive exercise primarily aggravates joint damage, moderate exercise is recognized to exert a beneficial effect on the healing of osteoarthritis. It has been widely reported that both traditional training, such as running and swimming, and non-traditional training, such as pilates and yoga, are effective in the management of knee and hip osteoarthritis, mainly regarding pain and strength improvement.98–100 Notably, rodent models have shown that moderate exercise prevents the progression of post-traumatic cartilage lesions.101,102 Additionally, it is suggested that there is a dose–response relationship between loading and intervertebral disc regenerative processes, implying that the loading pattern typically used in the lumbar extension resistance exercise interventions (high load, low volume, and low frequency) may impart the regeneration of the intervertebral discs.103 Actually, cartilage tissue presents limited cellularity and lacks a vascular system, leading to restrained healing capability, which brings more attention to the implantation on promoting regeneration, including stem cell transplantation and the application of biomaterials or devices.104–106 Importantly, exercise is also considered as an effective adjuvant to cartilage regeneration therapy. Substantial evidence has shown that exercise enhances the potential of autologous chondrocyte implants, matrix-induced autologous chondrocyte implants, and mesenchymal stem cell (MSC) implants for the successful treatment of damaged articular cartilage and subchondral bone by downregulating osteoclastogenic cytokine production and upregulating antiosteoclastogenic cytokine production by circulating immune cells.107 More recently, Liu et al.108 demonstrated exercise promoted hyalinecartilage regeneration and completely healed cartilage in osteochondral defect rabbits with a biodegradable piezoelectric scaffold implanted, which is potentially applicable to the treatment of osteoarthritis.
As is well known, physical activities induce mechanical stress to the joints and bones, promoting stem cell proliferation and differentiation in the process of regeneration.103,109–111 It has been reported that acute exercise increases circulating stem and progenitor cells, including hematopoietic stem cells (HSCs) and MSCs.112 Interestingly, osteoblasts and chondrocytes are derived from multipotent skeletal stem cells of MSCs,113,114 while osteoclasts are derived from the macrophage lineage of HSCs.115 Bone formation is carried out by osteoblasts and resorption is carried out by osteoclasts, which means that bone regeneration relies on the balance of two types of cells. Exercise has been shown to induce skeletal stem cells to differentiate towards osteoblasts. It is found that endurance training increases the total number of bone marrow MSCs in mice, enhances the osteogenic differentiation potential of MSCs, and inhibits the adipogenic potential of MSCs.116 Of note, osteoclast recruitment to the future resorption sites is mainly controlled by osteoblasts. It has been shown that moderate exercise increases the expression of osteoprotegerin and decreases the expression of receptor activator of nuclear factor κB ligand, both of which are expressed by osteoblasts, inhibiting osteoclast differentiation and activity.117–119 Thus, the regulatory mechanisms of stem cells responding to mechanical stimuli and biochemical signaling is critical for exercise-induced bone regeneration (Fig. 1f).
Exercise-induced cardiac regeneration
The benefits of exercise on cardiovascular system have been extensively reported.38,120,121 It is widely accepted that both endurance and resistance exercise training contribute to larger left ventricle structures than sedentary controls from the imaging findings, presenting physiological cardiac hypertrophy.122 Thus, one of the most significant exercise-induced adaptations has been described as promoting cardiac growth. However, it has been discovered that the renewal of cardiomyocytes gradually decreases from 1% turning over annually at the age of 20 to 0.3% at the age of 75, implying that adult human cardiomyocytes has a limited self-renewing capacity.53 Importantly, Boström et al.123 demonstrated that adult cardiomyocytes physiologically increased in both size and proliferation rate in response to exercise in mouse models. Meanwhile, it has been identified that endurance exercise increases birth of new cardiomyocytes in adult mice (~4.6-fold) based on incorporation of 15N-thymidine by multi-isotope imaging mass spectrometry.124 Therefore, exercise training provides a new intervention for enhancing the proliferation of cardiomyocytes.
Interestingly, Bei et al.125 stated that cardiomyocyte proliferation was not necessary for exercise-induced cardiac growth but required for its protection against ischemic injury. Ischemic injury, a mismatch of oxygen and substrate supply and demand in the myocardium, is one of the most predominant causes of cardiomyocyte loss. Exercise has been found to reduce adverse ventricular remodeling and cardiac dysfunction when initiated after infarction in animal models126,127 and humans128 for decades. Furthermore, it was found that myocardial infarct size significantly decreased in ischemia injury rats at least 1 week following the cessation of 5 consecutive days HIIT training, implying the sustained capability of exercise in cardiac repair.129 Subsequently, a range of studies have found that exercise increases numerous circulating factors to promote cardiomyocyte proliferation and reverse pathological cardiac remodeling in post-infarction models.130–134 Importantly, Vujic et al.124 demonstrated that exercise induced a robust cardiomyogenic response in an extended border zone of the infarcted area, validating the endogenous cardiomyocyte generation induced by exercise in the process of myocardial injury repair. However, previous studies have been done in the acute phase of cardiomyocyte loss, the effect of exercise on the pathological state of the chronic phase deserves further investigation.
Although exercise has protected against pathological cardiac remodeling, the effect of myocardial restoration after ischemic injury appears to vary from different exercise types.135,136 Interestingly, it has been found that HIIT, the popular exercise strategy, is not superior to MICT in changing left ventricular remodeling or aerobic capacity in the heart failure patients with preserved ejection fraction137 or reduced ejection fraction.138 Additionally, recently it has been reported that moderate heart rate reduction induces cardiomyocytes proliferation under physiological conditions and promotes cardiac regenerative repair after myocardial injury by inducing G1/S transition and increasing the expression of glycolytic enzymes in cardiomyocytes, which is exactly the opposite of the exercise-induced rapid heart rate.139 Thus, the mechanism of exercise-induced myocardial regeneration is quite complex, the effects of different training patterns and training intensities in cardiac regeneration needs further exploration. It is rational to investigate exercise mimetics to balance the benefits and drawbacks of exercise. Furthermore, there are other causes of myocardial injury, such as hypertension140 and cancer,141 leading to cardiomyocyte death, whether exercise training counteracts induced-cell death by promoting cardiomyocyte proliferation also remains unknown (Fig. 1a).
Exercise-induced regeneration in central nervous system
Neural stem and progenitor cells (NSPCs) are major promoters of central nervous system (CNS) regeneration, which migrate and differentiate into highly specified networks of neurons via neurogenesis, while oligodendrocytes and astrocytes are generated via gliogenesis.142 NSPCs response to CNS injury is extraordinarily complex and dependent upon the extent and location of injury, thus the endogenous adult neurogenesis has been highly controversial. Recently, it has been confirmed that the hippocampus contains NSPCs that continue to generate new neurons, called adult hippocampal neurogenesis (AHN), which almost continues across the lifespan, though declining with aging.143,144 Age-related neurodegenerative diseases are probably associated with impaired AHN. These animal studies have shown that voluntary exercise promotes hippocampal neurogenesis and prevents age-related decline in cell-proliferation in this brain structure.145,146 Furthermore, it has also been revealed that exercise induces volumetric retention in the left hippocampus in humans, implying endurance exercise interventions are useful for preventing age-related hippocampal deterioration.147 Besides aging, trauma, ischemic injury, and inflammation often bring about irreversible damage and loss of function to the CNS. Ischemic injury remains an important risk of neuron loss in the CNS. It has been reported that both endurance and resistance exercise training enhance cognitive performance148–150 and improve functional performance, such as balance and walking speed,151–153 in post-stroke population, implying that exercise promotes the repair of central neurons. Moreover, in the ischemic stroke rodent model, it has been confirmed that early endurance exercise, for instance wheel-running and treadmill training, contributes to functional and neuronal recovery, mainly improving motor function via enhancing synaptic plasticity,154 promoting myelin regeneration154 and neuron survival,155 and facilitating cerebral angiogenesis.156 Multiple sclerosis (MS) is another kind of CNS disorders characterized by oligodendrocyte loss and axonal degeneration/demyelination.157 Recently emerging research suggests that exercise has therapeutic benefits on the outcomes in the CNS for MS patients, including oligodendrogenesis, remyelination, and axonal regeneration.158
Spinal cord injury (SCI) disrupts both axonal pathways and segmental spinal cord circuitry, resulting in permanent loss of motor, sensory, and autonomic function. Exercise has been shown to induce synaptic plasticity and restore motor/sensory function in SCI patients.159 Subsequently, endurance exercise, such as treadmill training, has been reported to enhance axonal regeneration and sprouting in SCI rodent models via multiple ways.160–162 Of note, it has been revealed that the cholinergic neurotransmission from spinal locomotor neurons activates spinal NSPCs, leading to neurogenesis in the adult zebrafish. Interference with γ-aminobutyric acid signaling promotes functional recovery after spinal cord injury, which acts in a non-synaptic fashion to maintain NSPCs quiescence.163 Though it provides a new approach for locomotor networks’ activity-dependent neurogenesis during SCI regeneration, whether similar effects can be found in mammals needs to be further investigated. Currently, the multi-faceted regeneration strategies for SCI regeneration have been met with mixed success, however, adult neurogenesis in heterogeneous NSPC populations is still creating barriers to the function recovery of SCI. Indeed, NSPCs proliferate and differentiate into reactive astrocytes in the injured spinal cord, contributing to the glial scar border, which segregates the injury and prevents additional damage.164,165 However, this scar also prevents axonal outgrowth into the site of injury and generation of new cell types within the neural lesion.166 Thus, stem cell-based transplantation, including olfactory ensheathing cells (OECs), MSCs, and NSPCs, has opened an avenue for functional recovery of SCI, which has been enhanced by exercise training as well.167 It has been reported that exercise enhances the effect of OEC grafts in super acute thoracic cord transected rats, inducing a fourfold increase in regenerating axons within the caudal stump of the transected spinal cord.168 Additionally, exercise significantly promoted NSPCs graft survival and differentiation more into neurons and oligodendrocytes, enhancing myelination, and restoration of serotonergic fiber innervation in the lumbar spinal cord via reducing stress caused by active oxygen or active nitrogen through insulin-like growth factor 1 (IGF-1) signaling, which provided more theoretical basis for exercise rehabilitation and pharmacological mimetics169 (Fig. 1c).
Exercise-induced regeneration in peripheral nervous system
The regenerative capacity of the nervous system varies considerably between the peripheral nervous system (PNS) and CNS. On the contrary, the adult human PNS retains the ability of axons to regenerate after injury and successfully reinnervate the intended target.170 In the PNS, injured nerves undergo successful Wallerian degeneration and subsequently the axons upstream of the injury undergo polarized growth toward their target tissues.171 Therefore, enhancing the regeneration of axons is often considered to be a therapeutic target for improving functional recovery after peripheral nerve injury. Several clinical studies have suggested exercise as a non-pharmacological approach to positively affect various aspects of peripheral neuropathy such as diabetic peripheral neuropathy (DPN),172,173 chemotherapy-induced peripheral neuropathy (CIPN),174,175 and even carpal tunnel syndrome.176 Among these studies, a 10-week composite training program of endurance and resistance exercise led to significant reductions in pain and neuropathic symptoms, and increased intraepidermal nerve fiber branching from a proximal skin biopsy in DPN patients.173 Similarly, the positive effects of exercise, including decreasing pain and improving physical function177 as well as improvement of deep sensitivity178 and static balance performance,179 have been confirmed in CIPN patients. The effect of exercise promoting peripheral nerve regeneration is also observed in animal models. Physiologically, ladder-based resistance training effectively induced similar growth in the radial and sciatic nerves (SN) of adult rats including myelinated axons CSA, unmyelinated axons CSA, myelin sheath thickness, and Schwann cells nuclei area.180 Meanwhile, the functional and histological recovery after the mouse SN crush was positively influenced by treatment with eccentric exercise.181 Moderate swimming training was found to promote nerve regeneration in SN ligation or SN transection mice as well.182,183 Additionally, treadmill training accentuated nerve regeneration, accelerated functional recovery and prevented muscle atrophy in median nerve crush injury rat models184 (Fig. 1d).
Exercise-induced regeneration of other tissues
The liver exhibits the unique regenerative capacity that ensures body homeostasis or post-injury repair.185 Experimental models that involve partial hepatectomy or chemical injury have revealed the efforts of exercise that make the liver return to equivalent size and weight to those prior to injury. It has been reported that a 4 weeks endurance exercise program markedly enhances the ischemic tolerance and the regenerative capacity of fatty liver in diet-induced steatosis mice.186 Moreover, Fard-Aghaie et al.187 confirmed that a novel physical prehabilitation of treadmill training promoted hepatocyte proliferation and enhanced mitochondrial biogenesis, restoring liver function after partial hepatectomy operation in rodent models. Although the liver is a solid organ with a high regenerative capacity, the rate of physiological cell turnover is very slow. Thus, the regenerative activities of hepatocytes and cholangiocytes induced by exercise provides new strategies for restoring liver function (Fig. 1g).
The skin, the largest organ of the human body, defends against daily assaults from the external environment. In general, scarring and regeneration are two physiologically opposite endpoints to skin injuries. Thus, scarless regeneration is the ultimate goal in repairing skin injury. Indeed, emerging evidence has shown exercise promotes skin wounds healing. For example, endurance exercise improves cutaneous wound healing rates of different etiologies in mice and humans.188–190 Interestingly, a study of mice trained on a motorized treadmill has suggested that different intensities of exercise have different impacts on healing rates.191 In addition, another study has shown that low-intensity exercise accelerates wound healing rates in diabetic mice but high-intensity exercise fails.192 However, promoting wound healing is not the same as promoting skin regeneration, as there are few studies for further cellular mechanisms. Whether exercise promotes resident skin stem cell proliferation remains unclear.
Exercise offers regenerative effects to the hematopoietic system as well. In this regard, preclinical studies of treadmill exercise training in mouse models have demonstrated endurance exercise is able to modify the bone marrow microenvironment, alter hematopoiesis, and accelerate hematopoietic regeneration.193,194 Leukocytes derive from hematopoietic stem and progenitor cells (HSPCs), acting as a major responder of exercise. Recently it has been reported that running exercise diminishes leptin production in adipose tissue to regulate HSPCs proliferation and leukocyte production in mice.195 The impact of exercise on leukocyte production and on HSPC epigenome and transcriptome persists for several weeks. Curiously, it was also showed that ultra-endurance exercise contributed to an increase in circulating leukocytes and induced an inflammatory response that resulted in a highly significant decline of circulating hematopoietic progenitor cells functionality in humans.196 This may be the result of different inflammatory effects of the organism in response to different exercise intensities and patterns. Hematopoietic stem cell transplantation (HSCT) is increasingly used for hematological malignancies or severe non-malignant hematological disorders. Since exercise is convinced to affect HSPC, HSCT combined with exercise therapy is also a topic worth being explored to improve prognosis.197 Lisio et al.198 demonstrated a survival benefit and increased total blood reconstitution in mice that were pre-conditioned with endurance exercise after bone marrow transplantation. However, as implementation varies across studies in terms of timing of exercise initiation, exercise types and duration of exercise according to potential benefits of exercise reported by previous studies, the efficacy of exercise program among HSCT patients varies.199,200 The efficacy of exercise promoting HSCT is worthy of recognition, however, further mechanistic studies are needed (Fig. 1e).
Molecular mechanisms of tissue regeneration induced by exercise
In response to exercise, the organism will have both structural and functional adaptive changes which confer the beneficial effect of exercise. However, the mechanisms by which exercise initiates cellular responses involved in tissue repair/regeneration are still inadequately understood. Generally, exercise predominantly leads to an increase in mechanical signals such as fluid flow, dynamic tension, compression, and hydrostatic pressure. Thus, mechanotransduction, the process by which the organism converts mechanical loading into cellular responses, is regarded as one kind of potent signaling pathways for adaptive responses to exercise.201 Besides mechanical signals, numerous studies have shown that a range of bioactive substances regulated by exercise (namely, exerkines) contribute to maintaining homeostasis and improving the impaired function of diverse organs.202,203 These exerkines can be secreted by a variety of cells, including satellite cells, osteoblasts, immune cells, endothelial cells, fibroblasts, macrophages, and even adipocytes, which act as autocrine, paracrine, or circulating regulators in response to exercise.204,205 Notably, it has been extensively investigated that both mechanical stress and biochemical signals are involved in promoting cell proliferation and renewal induced by exercise.206–210 Since the complicated mechanism of exercise-induced tissue regeneration advances rapidly, we will discuss in detail the substantial novel progress in the regulation of tissue regeneration from multiple aspects.
Mechanotransduction
Indeed, a variety of cell surface proteins and structures, named mechanosensors, has been proposed to convert these mechanical stimuli into electrical or biochemical signals. The Piezo family, one of the mechanically activated ion channel, has emerged as the critical mechanosensors in many cell types, responding to various forms of mechanical forces, including membrane stretch, static pressure, and fluid shear stress.211–213 Of note, Piezo1 is also highly expressed in osteocytes and can be upregulated by mechanical stretching, involved in stem cell differentiation and bone formation.214–216 In addition, Piezo1 channels, working as non-selective cationic channels in endothelial cells, had profound importance for shear stress-evoked Ca2+ signaling, sensing the exercise induced changes in blood flow.217 Focal adhesions, one type of integrin-based adhesion complex, is another important mechanosensor of transmitting mechanical signals and promoting protein biosynthesis.218–220 Unlike integrin-based adhesions that receive mechanical stimuli from the extracellular matrix, gap junctions, two juxtaposed connexons on the surfaces of adjacent cells, are bridges for mechanical signaling communication between cells. Multiple types of connexins play a role in responding to the mechanotransduction, among which connexin 43 was shown that its knockout in early osteoblasts caused impaired muscle formation in mice.221,222 Moreover, low density lipoprotein receptor-related proteins 5/6 (LRP5/6), the single-pass transmembrane protein, have been found to act as the receptor of Wnt ligands and be indispensable for Wnt/β-catenin signaling transduction, which has been shown to affect bone mass by regulating osteoblast proliferation and activity.223–225 Besides these canonical membrane structures, novel mechanosensitive proteins are regularly discovered, such as the recent discovery of plexin D1 as a mechanosensitive receptor,226 with more likely awaiting discovery. Taken together, these important membrane structures are the cornerstone of various cellular responses to external mechanical stimuli, and may be another prelude to unlocking the secrets of exercise induced regeneration.
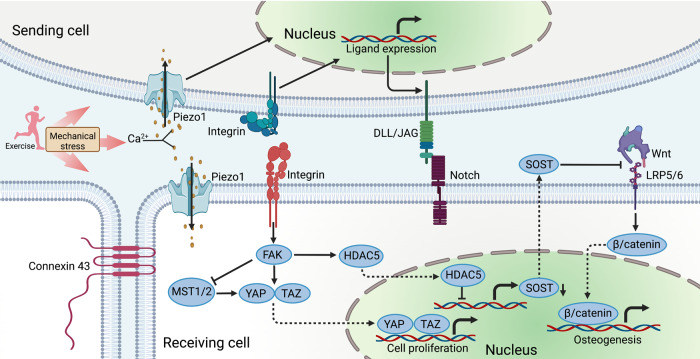
Within the help of the mechanosensors, the activation of sequential signaling cascades and expression of downstream target genes exhibit some common features, even in various cell types, including osteocytes,227 myocytes,228 neurons,229,230 liver cells,231,232 and cardiomyocytes.233,234 Basically, signal transduction can occur through the direct physical connections between the membrane, the cytoskeleton, and the nucleus, triggering gene expression and protein synthesis.235 Importantly, the transmission of information still involves facilitating biochemical signals via intracellular signaling molecules and secondary messengers. The activation of Wnt/β-catenin pathway has been proven to be a key regulator of cell growth. Recently a multi-omic analysis of stretched osteocytes has uncovered mechanically stimulated osteocytes support bone regeneration via ossification and extracellular matrix remodeling, focusing on the activation of Wnt/β-catenin pathway in both human and murine cells, showing the conservation of mechanotransduction mechanisms.236 It has been established that exercise-induced loading reduces expression of sclerostin (SOST) and Dickkopf-related protein 1 (Dkk1), the inhibitors of the Wnt pathway, in osteocytes, thus stimulating new bone formation.237 Focal adhesion kinase (FAK), an attachment protein associated integrin-based adhesion complex, has also been a key component of transmitters of mechanical signals. FAK was reported to be required for IGF-1-induced muscle hypertrophy, through tuberous sclerosis complex 2 (TSC2)/mammalian target of rapamycin (mTOR)/ribosomal S6 kinase 1 (S6K1)-dependent signaling pathway.238 Interestingly, fluid flow shear stress could trigger FAK dephosphorylation, driving class IIa histone deacetylase 5 (HDAC5) nuclear translocation, which demonstrated a role for HDAC5 in loading-induced SOST suppression.239 Another most described mediators are the transcriptional coactivators yes-associated protein (YAP) and transcriptional coactivator with PDZ-binding motif (TAZ).240 Generally, YAP and TAZ, known to be regulated by FAK through RhoA-mediated contractile force, translocate from the cytoplasm to the nucleus in cells perceiving high levels of mechanical signaling.241,242 Notably, nuclear translocation of YAP/TAZ has been also regulated by Hippo signaling pathway.243,244 Multiple mechanical stimuli mostly inhibit the Hippo pathway, promoting YAP/TAZ to enter the nucleus to activate genes involved in the cell cycle and cell proliferation.245,246 Thus, suppression of Hippo signaling play an important role in promotion of tissue regeneration as well, suggesting a new intervention mechanism for exercise-induced regeneration.247,248 Furthermore, Notch signaling has been shown to be another associated pathway of mechanotransduction as well.249 Generally, mechanical loading sensed by integrins or mechanosensitive Piezo results in the transcription of ligands of sending cell, regulating Notch signaling of receiving cell, which modulates cell proliferation and differentiation.250 It has been reported that Notch signaling is impaired in regenerating aged skeletal muscle, which can be restored by physiological stimuli of exercise.251–253 Therefore, further researches should be carried out to demonstrate the underlying mechanisms of mechanotransduction mediated tissue regeneration with different exercise types, which may provide the novel targets for clinical interventions (Fig. 2).
Fig. 2.
Mechanotransduction regulating regenerative responses. The signaling transduction of exercise-induced regeneration are generally initiated by mechanical signals. A series of membrane receptors or channels can respond to mechanical signals, thereby converting mechanical signals into chemical molecular signals. Piezo1 channels, working as non-selective cationic channels, sense the exercise-induced stress, converting into mechanical stress-evoked Ca2+ signaling. Integrin-based adhesion complex activates FAK, promoting YAP/TAZ translocation via inhibiting Hippo signaling. FAK can drive HDAC5 nuclear translocation and suppress SOST. Integrins or Piezo channels activate the transcription of ligands of Notch receptor in sending cell, triggering Notch signaling of receiving cell. Wnt/β-catenin pathway is important in osteogenesis, which can be inhibited by SOST. Connexin 43 responds to the mechanotransduction for cell-to-cell communication. Created with BioRender
PI3K/Akt signaling pathway
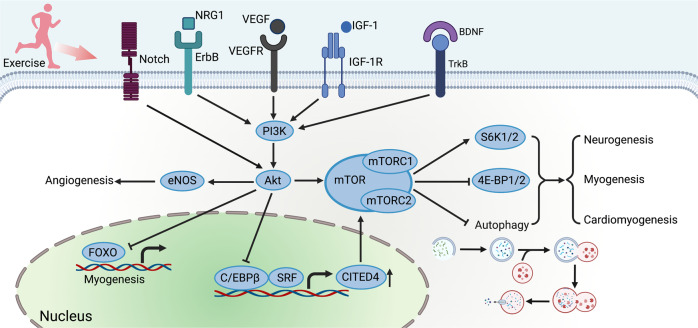
Emerging evidence has revealed the essential contribution of PI3K/Akt signaling pathway to exercise-induced regeneration.254,255 An array of growth factors has been reported to act as exerkines, such as IGF-1,256 brain-derived neurotrophic factor (BDNF),257 epidermal growth factor (EGF)258 and their associated family, triggering the cellular responses via PI3K/Akt pathway. Amongst all the growth factors induced by exercise, the most widely studied is IGF-1. Notably, circulating IGF-1 is primarily secreted by the liver, while peripheral tissues, including bone and muscle, produce IGF-1 as well, acting in a paracrine/autocrine fashion. Exercise-induced IGF-1 locally leads to the sequential activation of PI3K/Akt signaling pathways with consequent induction of myoblasts,259,260 osteocytes261,262 and cardiomyocytes263,264 proliferation and differentiation. Meanwhile, neuregulin 1 (NRG1), a member of EGF family, and its tyrosine kinase receptor ErbB family is found to promote cell growth and differentiation physiologically and pathologically by targeting PI3K/Akt pathway.265–267 Moreover, BDNF and its receptor, tropomyosin-related kinase B (TrkB) mediate PI3K/Akt pathway as well, sharing the similar effects.268,269 BDNF has been discovered to be time-dependently upregulated in rat skeletal muscle after acute endurance exercise, which is convinced to be involved in exercise-induced skeletal muscle regeneration.257 Briefly, exercise-induced BDNF expression also plays a crucial role in neuronal survival, proliferation, maturation, and outgrowth in both the brain,270–273 spinal cord,274,275 and PNS.276,277 Angiogenesis has also played a vital role in human physiology of tissue repair, since oxygen supply and nutrients constitute important primitive materials for tissue anabolic activity.278–280 The transcription of vascular endothelial growth factor (VEGF) a kind of pro-angiogenic factor, is mainly activated by exercise-induced hypoxia and mechanical stress, which plays a crucial role in endothelial cell survival and promotion of capillary sprouting via PI3K/Akt pathway.281,282 Several studies have revealed that both endurance and resistance exercise increase the expression of VEGF in the brain, heart, skeletal muscle, and bones.95,283,284 HIIT training contributed to an overall increase in the expression levels of VEGF and VEGF receptor-2 (VEGFR2) in skeletal muscle of subjects with peripheral myopathy associated with heart failure, promoting muscle capillarization,285 and differentially expressed genes of the skeletal muscle showed the PI3K/Akt signaling pathway was activated in response to HIIT.286 Of note, it has been found that the PI3K/Akt axis is not only activated by a range of exerkines mentioned above, but also in response to mechanical stress.287–289 Exercise frequently mediates crosstalk between mechanoregulation of regeneration and canonical regenerative signaling pathways. While Akt has been reported to be activated by Notch, a important role in mechanotransduction, in EPCs after endurance exercise in hypertension patients, targeting endothelial nitric oxide synthase, for restoration of impaired angiogenesis capacity of late EPCs.290
The downstream responses of PI3K/Akt pathway are also varied. One of the significant targets of Akt is mTOR, an evolutionarily conserved serine/threonine kinase. Actually, mTOR exists in two distinct complexes: mTOR complex 1 and mTOR complex 2 (mTORC1 and 2).291 The activation of mTORC1 is frequently spotted in the adaptive response to exercise.292 Importantly, the activation of mTOR-axis has been the critical process of exercise-induced regeneration in different tissues, including muscle,293,294 heart,295 brain296 and spinal cord.297 Mostly, mTORC1 phosphorylates and activates S6K1/2 and eukaryotic translation initiation factor 4E (eIF4E)-binding proteins 1 and 2 (4E-BP1/2), which contribute to stimulation of mRNA translation, thereby regulating increases or decreases in anabolic and catabolic processes.298 Additionally, the activation of mTORC1 suppresses autophagy and perhaps other lysosomal functions.299 For instance, NRG1 activated PI3K/Akt axis, targeting mTOR-pathway in hippocampal neurogenesis, which was confirmed by exercise-induced expression of autophagy-related proteins.300 Moreover, CCAAT/enhancer binding protein β (C/EBPβ)-Cbp/p300-interacting transactivator with ED-rich carboxy-terminal domain 4 (CITED4) axis has been identified as critical modulator in the cardiomyocyte proliferation in adult exercised hearts, which has also been shown to be regulated by Akt.123,301 It has been confirmed that C/EBPβ is downregulated by endurance exercise to enhance cardiomyocyte proliferation via negatively regulating CITED4 in vitro.123 C/EBPβ and CITED4 has been reported to be regulated in myocardial ischemia or transverse aortic constriction murine models after exercise training.39,302,303 Overall, CITED4 acts as downstream of C/EBPβ, thereby activating the mTOR pathway, promoting exercise-induced cardiomyocyte proliferation and protecting from adverse cardiac remodeling.303–305 Another potential downstream mediator of the cell proliferation and development induced by exercise are forkhead box class O family (FOXOs). Akt/FOXO3a signaling pathway is activated in exercise-induced autophagy, which is beneficial for remedying sarcopenia.306 Akt is also likely to mediate FOXO family inhibition in the regulation of stem cell proliferation.307 Inhibition of FOXOs activity decreases myostatin expression and increases satellite cell proliferation, and fusion, and leads to muscle hypertrophy308,309 (Fig. 3).
Fig. 3.
PI3K/Akt signaling pathway. The PI3K/Akt pathway is mainly activated by an array of growth factors, such as IGF-1, NRG1, VEGF, and BDNF. Akt can be directly activated by Notch signaling. The PI3K/Akt pathway mainly acts as the upstream of mTOR activation. The activation of mTOR promotes cardiomyogenesis, myogenesis, and neurogenesis via various signaling. Importantly, PI3K/Akt axis inhibits C/EBPβ, thus upregulating CITED4 to activate mTOR and promoting myogenesis. Additionally, the PI3K/Akt axis inhibits FOXOs, promoting myogenesis. eNOS is upregulated by the PI3K/Akt axis, promoting angiogenesis. Created with BioRender
MAPK signaling pathways
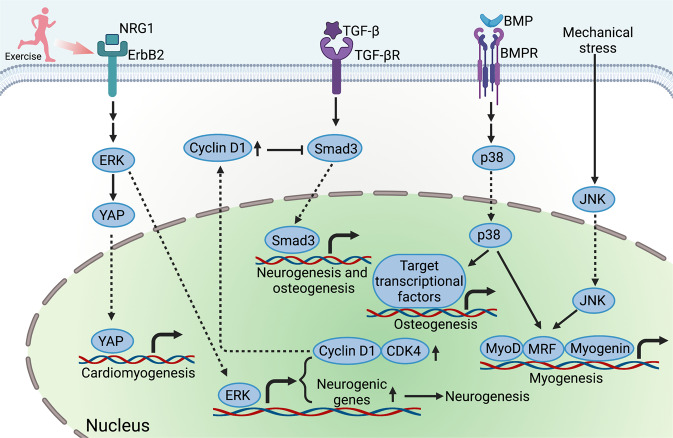
The extracellular signal-regulated kinases 1 and 2 (ERK1/2), p38 mitogen-activated protein kinase (MAPK), and c-Jun N-terminal kinase (JNK), as key members of MAPK family, are also serine/threonine protein kinases that are irreplaceable players participating in diverse biological activities.310 Similar to PI3K/Akt signaling, MAPK signaling can be activated by a range of growth factors, thus playing an important role in exercise-induced tissue regeneration. More recently, it has been investigated that NRG1/ErbB2 signaling mediates the interaction of YAP with nuclear-envelope and cytoskeletal components for cardiomyocytes regeneration via the activation of ERK.311 Besides, MAPK/ERK signaling is also targeting the regulation of the cell cycle. Postnatal cell cycle exit is often accompanied by reduced expression of cyclins and cyclin-dependent kinases.312–314 Endurance exercise up-regulated cyclin-dependent kinase 4 and Cyclin D1 by ERK signaling, inducing the proliferation and differentiation of endogenous neural stem cells, and improving neural function of rats with cerebral infarction.315 Exercise was also reported to activate MAPK/ERK signaling to promote cycling of satellite cells.294 Furthermore, running exercise accelerated muscle regeneration in aged mice, suppressing transforming growth factor-β (TGF-β)/Smad3 signaling in quiescent muscle stem cells via the restoration of Cyclin D1.316 Additionally, it has also been well-known that bone morphogenetic proteins (BMPs), members of TGF-β super family, are upregulated in bones and cartilages after exercise.317–319 Mostly, the regulation of downstream networks of BMPs signaling is specifically though canonical Smad-dependent pathways.320 Importantly, BMP signaling has played a vital role in osteoblast differentiation, which promotes osteoblastogenesis through p38 MAPK pathway as well.321–323 Furthermore, following repeated bouts of eccentric cycling, it was reported that phosphorylation of JNK and p38 MAPK were also activated in skeletal muscle, inducing the overexpression of MyoD, myogenic regulatory factors (MRFs) and Myogenin324 (Fig. 4).
Fig. 4.
MAPK signaling pathway. The MAPKs signaling can be activated by exercise-induced mechanical stress and a range of growth factors, including NRG1, TGF-β and BMP, thus playing an important role in exercise-induced tissue regeneration. MAPK/ERK signaling activates YAP translocation into nucleus, promoting cardiomyogenesis. The activation of ERK also promotes neurogenesis and cycling of satellite cells. The restoration of cyclin D1 inhibits TGF-β/Smad signaling. The p38 MAPK and JNK can activate the transcription factors that initiate the expression of osteogenetic and myogenetic genes, including Myod, MRF, and Myogenin, promoting osteogenesis and myogenesis. Created with BioRender
AMPK/SIRT1/PGC-1α signaling pathway
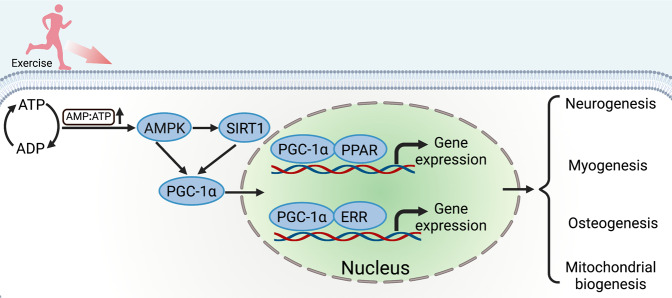
Peroxisome proliferator-activated receptor (PPAR)-γ coactivator-1α (PGC-1α) is commonly expressed in high-energy-demanding tissues such as heart, muscle, and brown adipose tissue, which is already considered as the core regulator of metabolic regulating pathways such as the adenosine monophosphate-activated protein kinase (AMPK)-sirtuin 1 (SIRT1)-PGC-1α pathway.325 Undoubtedly, exercise leads to the activation of AMPK in vivo through the modulation of the AMP-to-ATP ratio.326,327 Though PGC-1α mainly involved in mitochondrial biosynthesis and cellular respiration, has been reported to act as a vital regulator in cell proliferation and differentiation as well.67,328 Exercise strongly induces overexpression of PGC-1α in both human and rodent muscle,329,330 which may trigger a remodeling of the satellite cells niche by altering the extracellular matrix composition, including the levels of fibronectin, thus affecting the proliferative output of satellite cells.331 While in terms of osteogenesis, PGC-1α has already been shown to play an important role in skeletal homeostasis by coactivating a range of transcription factors.332 Overexpression of PGC-1α was sufficient to enhance osteocytic gene expression in IDG-SW3 cells, murine primary osteoblasts, and osteocytes, and ex vivo bone cultures.333 In addition, deletion of PGC-1α suppressed differentiation and activity of osteoblast, resulting in a significant decrease of cortical thickness and trabecular thickness.334 Recently, it has been found that running exercise increases the expression of PGC-1α in the hippocampus of depressed mice, targeting for antidepressant treatment via promoting the proliferation parvalbumin-positive interneurons.335 Mechanically, PGC-1α activates a variety of metabolic programs in different tissues through its ability to form heteromeric complexes with many nuclear hormone receptors, such as PPARs336 and estrogen-related receptors (ERRs).337 Interestingly, PGC-1α is regulated by AMPK/SIRT1 axis, promoting exercise-induced tissue regeneration, as well as involved in mitochondrial signaling,338,339 Thus PGC-1α has acted as a vital regulator in the adaptive response to exercise, which may be the key regulator of the cross-talk between mitochondrial biogenesis and exercise-induced regeneration (Fig. 5).
Fig. 5.
AMPK/SIRT1/PGC-1α signaling pathway. Exercise changes the energy status, consuming a large amount of ATP, which elevates AMP-to-ATP ratio. Consequently, AMPK/SIRT1/PGC-1α signaling pathway is activated. PGC-1α is very important in the anabolic process of exercise-induced response. PGC-1α and PPAR/ERR form co-transcriptional complexes that initiate the overexpression of target genes, thereby promoting tissue regeneration and repair, including neurogenesis, myogenesis, and osteogenesis. Created with BioRender
Noncoding RNAs and their regulated signaling pathways
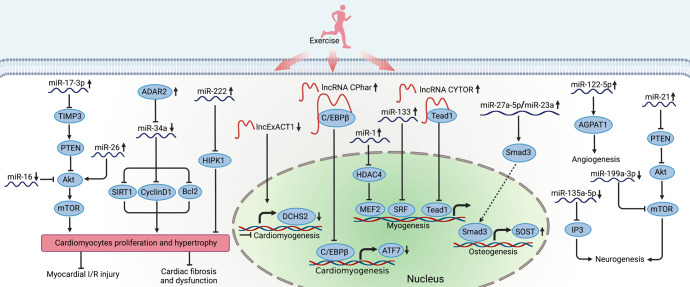
Recently emerging evidences support the critical role of noncoding RNAs, another important cluster of exerkines, in the regulation of exercise-induced tissue regeneration. Among them, microRNAs (miRNAs) have shown significant changes in the musculoskeletal system after exercise training.340 It was reported that in healthy untrained males, miR-1, miR-133, and miR-181a were increased in skeletal muscle samples collected 3 h following 60 min of cycling at 70% of VO2 peak.341 Similarly, the former two were shown to decrease in skeletal muscle miRNA profiles of muscle atrophy mice.342,343 Indeed, miR-1 promotes myoblast differentiation, whereas miR-133 stimulates myoblast proliferation. Mechanically, miR-1 modulated myocyte enhancer factor 2 (MEF2) via suppressing HDAC4 and miR-133 inhibited serum response factor (SRF), promoting myogenesis in different stages.344 Of note, miR-1 also positively promoted the protein synthesis and myogenesis by targeting IGF-1/Akt/FOXO3 signaling pathway.345,346 More recently, liver-derived extracellular vesicle miR-122-5p after treadmill training was reported to promote angiogenesis through shifting substrate preference to fatty acids in endothelial cells by targeting 1-acyl-sn-glycerol-3-phosphate acyltransferase (AGPAT1), increasing capillary density in the quadriceps, and accelerating wound healing in mice.347 In addition, treadmill exercise training has been also reported to influence the miRNA profiles of bone tissue, such as miR-190a-5p, miR-203-5p, miR-27a-5p, and miR-5118.348 Importantly, miR-27a-5p is confirmed as a member of miR-23a cluster. The components of the miR-23a cluster regulated osteoblast differentiation by targeting the modulation of SOST via TGF-β signaling pathway, which may explain the regulation of exercise-induced osteogenesis by miRNAs.349 Moreover, more miRNAs have been identified to involve in the different process of fracture healing, thus, whether these miRNAs are regulated by exercise still deserves further exploration.350
Likewise, a wide range of miRNAs have been found to increase in exercised heart as well, acting as vital regulators of exercise-induced cardiomyocyte proliferation and involving in myocardial injury repair. Expression of the protein kinase HIPK1 was identified as a direct target of miR-222 with anti-proliferative effects in cardiomyocytes, contributing to exercise-induced cardiomyogenesis.124,131 MiR-17-3p positively regulated cardiomyocytes proliferation and hypertrophy by targeting tissue inhibitor metallopeptidase 3 (TIMP3) and acting upstream of the phosphatase and tensin homolog deleted on chromosome 10 (PTEN)/Akt signaling pathway, protecting against myocardial ischemia–reperfusion injury.133 Additionally, aerobic exercise training increased miR-26 and decreased miR-16, significantly promoting cardiomyocyte hypertrophy and proliferation via Akt/mTOR signaling pathway.351 Furthermore, miR-34a, regulated by adenosine deaminases acting on RNA 2 (ADAR2), contributed to exercise-induced cardiomyocyte proliferation, targeting SIRT1, Cyclin D1 and Bcl2.352
While in terms of exercise-induced adult neurogenesis, it was reported that running exercise downregulated miR-135a-5p, targeting inositol 1,4,5-trisphosphate (IP3) signaling, thus increasing proliferation of neural precursor cells of the mouse dentate gyrus.353 It was also shown that miR-199a-3p increased in spinal cord after SCI and miR-21 increased in SCI animals that had undergone exercise.354 It was confirmed that miR-21 promoted and miR-199a-3p attenuated neurite growth in sciatic nerve injury rats via targeting PTEN in the regulation of Akt/mTOR pathway.297
Similarly, long noncoding RNAs (lncRNAs) have been shown to respond to exercise as well, promoting cell proliferation and differentiation during tissue regeneration.355 A set of lncRNAs have been reported to play key roles in myogenesis and adult skeletal muscle regeneration.356 Amongst them, the overexpression of lncRNA CYTOR, responding to exercise in both human and rodents, in mouse myogenic progenitor cells enhanced myogenic differentiation by sequestering the transcription factor Tead1, which was a regulatory mechanism of fast-twitch myogenesis in aging.357 Meanwhile, lncRNA CPhar358 and lncExACT1359 have been found to be regulated in exercised heart. Notably, lncRNA CPhar, characterized to be increased with exercise, triggered exercise-induced cardiac physiological hypertrophy via sequestering C/EBPβ and downregulating activating transcription factor 7 (ATF7), thus preventing myocardial ischemic injury-induced cardiac remodeling and dysfunction.358 Whereas lncExACT1 increased in heart failure but decreased in exercised hearts, inhibition of which induced cardiomyogenesis and protected against cardiac fibrosis and dysfunction as well.359 Dachsous cadherin-related 2 (DCHS2) had a role in the heart as a downstream effector of lncExACT1, mainly targeting Hippo/YAP signaling.359 Although evidence is still lacking to support the comprehensive functionality of most lncRNAs, the high tissue-specificity and regulation of specific facets of cellular networks have suggested that lncRNAs are superior to proteins in terms of potential, undesired toxic effects associated with their targeting360 (Fig. 6).
Fig. 6.
Noncoding RNA regulating the exercise-induced regeneration. Exercise induces many noncoding RNAs in the regulation of physiological response. MiR-17-3p acts as the upstream of PTEN by inhibiting TIMP3, promoting cardiomyocyte proliferation and hypertrophy through Akt/mTOR pathway. Another two miRNAs, miR-26, and miR-16, also involve in the Akt/mTOR pathway. ADAR2 inhibits miR-34a, targeting SIRT1, CyclinD1, and Bcl2 and leading to cardiomyocyte proliferation. Exercise-induced miR-222 decreases the expression of HIPK1, promoting cardiomyogenesis. Furthermore, miR-1 and miR-133 promote myogenesis via inhibiting HDAC4 and SRF, respectively. MiR-122-5p can promote angiogenesis through AGPAT1 pathway. Additionally, miR-27a-5p upregulates the expression of SOST to achieve osteogenesis. Of note, miR-21 and miR-199a-3p are also regulated by exercise, which is involved in PTEN/Akt signaling pathway. While miR-135a-5p promotes neurogenesis via inhibiting IP3 pathway. Exercise also modulates the effect of lncRNA on tissue regeneration. LncRNA CYTOR can achieve myogenesis through sequestering Tead1. LncExACT1 induces pathological myocardial hypertrophy, which is downregulated by exercise. While lncRNA CPhar promotes cardiomyogenesis through decreasing ATF7 by sequestering C/EBPβ. Created with BioRender
Potential exercise mimetics contributing to tissue regeneration
As is mentioned that exercise induces a set of physiological responses that benefit regeneration on various organs, it has gained great potential for use in patients having low exercise compliance or in those for whom regular exercise is not feasible. Consequently, exercise mimetics may have therapeutic applications across a variety of diseases. The following part reviews candidate exercise mimetics with emerging therapeutic targets and strategies for the development of exercise mimetics.
Pharmaceuticals
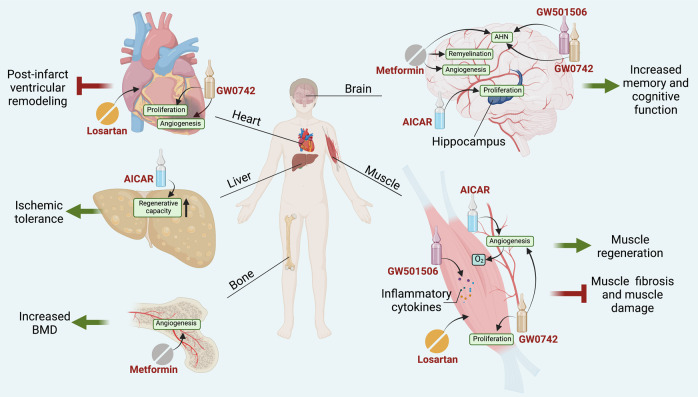
Indeed, AMPK/SIRT1/PGC-1α pathway acts as an important role of exercise-induced physiological responses. Given it, AMPK agonists are proposed as the promising exercise mimetics.361–363 However, it is widely recognized that AMPK activation induces a switch of cellular metabolism from anabolic to catabolic, promoting ATP conservation by inhibiting cell growth and proliferation, which makes AMPK agonists specialize in anti-tumor therapy rather than regeneration.364–367 Nevertheless, 5-aminoimidazole-4-carboxamide ribonucleotide (AICAR), one of the AMPK agonists, promotes angiogenesis in muscle by activating AMPK signaling in endothelial cells, mimicking the effects of exercise.368,369 Interestingly, though the majority of the effects of AICAR on skeletal muscles are AMPK-dependent, it may have indirect effect of AMPK activation in other organs. For example, AICAR has been suggested to increase hippocampus neuron number via activating the overexpression of BDNF, improving spatial memory; however, it cannot maintain a sustained positive effect as well as running due to the poor permeability through the blood–brain barrier.370–372 In addition, AICAR acts as an exercise mimetic in settings of fatty liver disease, enhancing the ischemic tolerance and the regenerative capacity of fatty liver.186 Likewise, another AMPK agonist exhibiting impressive exercise mimicking capability is metformin, which is extensively used as a first-line antiglycemic drug.373 Metformin showed positive cognitive effects or increased memory function via promoting angiogenesis, AHN, and remyelination in aged or stroke rodent models.374–376 Besides neurogenesis, metformin also has exhibited capability of osteogenesis, inducing the similar effects on femoral BMD gains compared to plyometric exercise in ovariectomized rats.377
PPARs are proposed to interact with PGC-1α, promoting a series of exercise-induce responses. Deficiency of PPARδ has been reported to result in a reduction of satellite cell number and the regenerative capacity.378 PPARδ increased the proliferation and differentiation of myoblasts through FOXO1, whereas GW501516, a kind of synthetic PPARδ agonist, promoted the processes of myogenesis.379,380 More recently, GW501516 was also reported to limit muscle tissue damage and restores muscle tetanic contraction in mice via mimicking localized exercise-induced inflammation by upregulating Forkhead box A2.381 Notably, GW0742, another synthetic PPARδ agonist, promoted angiogenesis and cell proliferation in muscle382 and heart383 via activation of calcineurin. Similar to AICAR and metformin, GW501516 and GW0742 increased memory performance and enhanced hippocampal neurogenesis as well.370,384 Thus, a phase IIa clinical study was carried out to test T3D-959, a newly synthetic PPARδ agonist, in subjects with mild to moderate Alzheimer’s disease, which suggests that PPARδ agonists are also moving towards clinical translation.385
Angiotensin II receptor blockade, an anti-hypertensive agent, is also an impressive replacement of exercise-induced regeneration. Losartan, a classical angiotensin-receptor blockade, was reported to limit post-infarct ventricular remodeling in rats, predominantly mimicking the protective effect of exercise on the heart.386 More recently, losartan reversed allodynia, reduced muscle fibrosis, and improved muscle regeneration in a murine model of orthopedic trauma combining tibia fracture and pin fixation with muscle damage, recapitulating the exercise-induced regeneration on post-injury recovery387 (Fig. 7).
Fig. 7.
Emerging pharmaceuticals mimicking exercise-induced tissue regeneration. AMPK/SIRT1/PGC-1α/PPARδ pathway has been selected as an important intervention of exercise-induced physiological responses. AICAR, metformin, GW501516, and GW0742, used to mimic exercise-induced physiological responses, demonstrate the ability to promote damaged tissue repair. Additionally, losartan is used to promote muscle regeneration. Created with BioRender
Natural molecular mediators
As mentioned above, the organism will release various natural molecular mediators involved in signaling pathways that promote regeneration during exercise. The regulatory mechanisms of these biomolecules are being understood by a wide range of researchers, which allows biosynthetic agents or genetic drugs to mimic the effects of exercise as well.
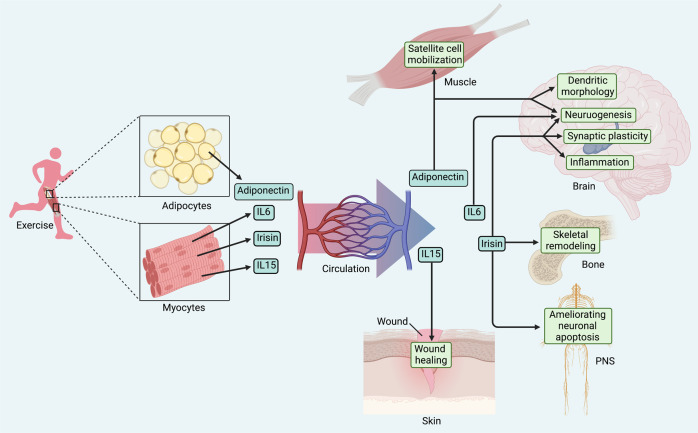
Irisin, a novel myokine, cleaved from membrane precursor fibronectin type III domain-containing 5 (FNDC5) in response to exercise, and acts as a linkage between muscles and other tissues.388 Besides inducing browning of white adipose tissue, irisin was discovered to promote proliferation and differentiation of osteoblasts through activating the p38 and ERK signaling.389,390 In the meantime, recombinant irisin positively regulated osteoblast differentiation under simulated microgravity via the overexpression of β-catenin, successfully providing a prevention strategy for bone loss and muscle atrophy induced by microgravity.391 Interestingly, irisin was also reported to bind to the proteins of the αV class of integrins, increasing production of SOST involved in bone resorption by increasing osteoclasts activity, which implied the two-sided effects of irisin on the therapeutic potential of skeletal remodeling.392 In terms of neuroprotection, circulating irisin crossed the blood-brain barrier and elevated BDNF level in the hippocampus, thereby promoting neurogenesis, enhancing synaptic plasticity, and modulating inflammation, which was demonstrated in models of neurodegenerative disease and cerebral ischemia.393–395 Furthermore, a recent study showed that recombinant adenovirus containing the irisin sequence improved burn-related neuropathy by ameliorating neuroinflammation-induced neuronal apoptosis, which demonstrated the protective effect of irisin on the PNS as well.396 Therefore, the therapeutic mechanism of irisin is not fully understood but has strong potential.
Adiponectin, one of the emerging adipokines, is also modulated by exercise, thus exerting a regenerative effect. Chronic exercise training imposed to rodents increased circulating adiponectin levels and AdipoR1 (adiponectin specific muscle receptor) expression.397,398 Thus, adiponectin was found to be responsible for the exercise-induced restoration of satellite cell mobilization, regenerative capacity in aged mice via the AMPK/SIRT1/PGC-1α axis.399 Moreover, adiponectin is capable of crossing the blood-brain barrier and affecting the CNS. Adiponectin mimicked exercise-induced effects in stress-elicited depression mice by retaining the normal proliferation of neural progenitors and dendritic morphology of neurons in the hippocampal dentate gyrus.400 In addition, AdipoRon (adiponectin receptor agonist), which mimicked the effects of running, rescued impaired cognitive function by improving hippocampal neurogenesis via adiponectin-Notch pathway.401 Similarly, AdipoRon treatment confirmed the exercise-induced hippocampal neuroplasticity in diabetic mice as well, which provides another promising candidate exercise mimetics.402,403
There are a set of immunomodulatory cytokines secreted into the circulation during exercise, such as interleukin-6 (IL-6) and IL-15, which are also integrated into the list of candidate exercise mimetics. IL-6 has been found to be synthesized and secreted into circulating by skeletal muscle during exercise, activating PI3K/Akt signaling, MAPK signaling and AMPK signaling in targeting cells.404–406 IL-6 was shown to promote proliferation of post-natal murine neural stem cell numbers.407 Thus, administration of recombinant IL-6 in a low-dose pulsatile strategy might directly modulate Schwann and nerve cells as a regenerative response to exercise in diabetic peripheral neuropathy.408 Notably, tocilizumab, one of the IL-6 receptor antibodies, has been used to treat some forms of arthritis.409 The side effect, such as blocking of exercise-mediated loss of visceral adipose tissue mass, has been confirmed recently.410,411 Whether the application of IL-6 receptor antibodies will block exercise-induced regenerative capacity is also a topic worthy of further investigation. While IL-15 is also a myokine of the IL-2 family responding to exercise.412 IL-15 has been reported to have local effects on skeletal muscles, such as promoting myoblast differentiation.413,414 Furthermore, exercise-mediated improvements in the healing of aged skin depend upon circulating IL-15. Exercise-mimicking recombinant IL-15 directly enhanced the growth of the aged mouse fibroblasts and keratinocytes, promoting impaired wound healing via activation of signal transducer and activator of transcription 3 signaling pathway, even though it was barely scarless regeneration415 (Fig. 8).
Fig. 8.
Natural molecular mediators. A set of exerkines are considered as candidate exercise mimetics, including irisin, adiponectin and interleukin, which can be used as gene therapy. These emerging target molecules provide new insights into the mechanisms of injured tissue regeneration and facilitate the efficiency of clinical translation. Created with BioRender
Discussion and perspective
Application of exercise intervention under aging condition
With the progress of society, the average human life expectancy has increased significantly. In parallel with longer lifespan, aging-specific health problem have emerged, which makes a growing global burden. Although it is brought to light that aging can not to be abolished, it is still expected to be able to attenuate the process and greatly ameliorate its effects, which implies the ultimate goal is not only longer lifespan, but also a better quality of life.416 Indeed, besides trauma and inflammation, aging is a vital process in the lifespan, whose essence is replicative cellular senescence.417 Senescent cells accumulate at sites of age-related pathologies and have an impact on the normal physiology of the tissues, causing a progressive functional deterioration.418 Exercise training is considered as a promising regenerative intervention for aged tissues, contributing to prevention and management of the challenging chronic diseases faced by elderly population.
Dementia is characterized by impairment of cognitive abilities and memory. Alzheimer’s disease (AD), a main and common type of dementia, is probably identified as age-related impairment of AHN.143 It has been reported that exercise not only reduces the risk of developing AD in aged population, but also improves the cognitive function of individuals with mild cognitive impairment and AD.419 Increasing evidence suggests that a variety of bioactive substances induced by exercise exert neuroprotective effects in mouse models via restoration of AHN and regulation of synaptic plasticity as well.420,421 In addition, numerous studies have shown that exercise can improve the poor prognosis of other age-related neurodegeneration via promoting neuronal survival and plasticity, or neurogenesis.422 Interestingly, endurance exercise has been reported to enhance the secretion of an enzyme, called glycosylphosphatidylinositol-specific phospholipase D1, derived from liver, ameliorating impaired neurogenesis and cognition in the aged hippocampus of mice.423 It is a new approach to explore the influence of other organs on the aged brain, providing new targets for the treatment of neurodegenerative diseases.
The level of bone loss increases with age, leading to osteoporosis in the elderly, particularly postmenopausal woman, which increases risk of fractures. Exercise training is considered as an effective method to stimulate bone osteogenesis in osteoporotic patients. As is mentioned, bone is a force-receptive organ, which needs to achieve sufficient mechanical intensity to effectively trigger the response of osteogenesis. As a result, not all types of exercise have the same positive effect on BMD. High intensity aerobic or resistance exercises are confirmed to be more effective in promoting the increase of BMD.424,425 In addition, several meta-analyses have shown that exercise appears extremely site-specific, increasing BMD only in the stimulated body regions.426,427 Thus, more composite exercises of diverse patterns and intensities need to be explored in order to more effective bone regeneration in whole body of aging adults.
Sarcopenia, the loss of skeletal muscle mass and strength, is an inevitable event during the aging process, which reduces physical capacity and enhances the problems associated with disabilities.428 Capelli et al.429 indicated that decay of maximal aerobic power and anaerobic capacity occurred with aging in cycling athletes, confirming age-related loss of muscle mass. Accumulating evidence supports that exercise training represents an effective intervention strategy to reduce or even reverse age-related loss of muscle mass as well.430 A meta-analysis, including 1,328 adults, demonstrated that resistance exercise training was effective in eliciting gains in lean body mass among the older people, particularly if they performed higher volume programs.431 Thus, as an effect of the independent exercise regimes on muscle mass, resistance exercise programs seem to be mostly effective in increasing muscle strength in sarcopenic frail elderly people.432,433 In regard of the cellular level, both resistance and endurance exercise training have shown to increase the number of satellite cells for regeneration in old animals and humans.434–437 The key role for muscle regeneration may be the intensity and frequency of exercise stimulation, however, the specific mechanisms responsible for re-trigger of growth capacity by exercise are not of comprehensive recognition yet.
Limitation and prospects of exercise intervention
Although remarkable progress has been made in the treatment of exercise interventions over the past few decades (Table 1), the side effects of over exercise are also being recognized. It is common to visualize that excessive-exercise or inappropriate exercise leads to sport-related injuries, ranging from the ankle and the knee, to the face and even the brain, which has ruined the careers of most athletes.438–441 Notably, chronic excessive exercise might adversely impact cardiovascular health. The increased incidence of atrial fibrillation seen in endurance athletes is one of the best documented cardiac maladaptations, which is related to exercise-induced changes in autonomic tone alongside the development of an arrhythmogenic atrial substrate.442 Myocardial fibrosis and coronary artery calcification have also been detected in ultra-endurance races.443,444 In addition, the marked suppression of growth factors and hormones, including testosterone, IGF-1, and leptin, after ultra-endurance exercise has also reported, which is strongly associated with the magnitude of the energy deficit.445 It has been realized that excessive exercise leads to immune imbalance and decrease in reactive oxygen species scavenging capacity, which has deleterious effects on health as well.446 Fortunately, with a better understanding of the adaptive responses of the organism to exercise gained, it has been found that we all carry our own “endogenous medicine box”. We have the opportunity to take the most applicable pills from the box to target a variety of different diseases. Thus, how to explore and make good use of the body’s own endogenous health resources, especially how to develop personalized rehabilitation exercise prescriptions for different diseases and different patients, has attracted more and more researchers to explore this field.
Table 1.
Clinical trials related to exercise intervention in diverse diseases
| Organ | Disease | Participants | Intervention | Course | Effect | Registration number | Reference |
|---|---|---|---|---|---|---|---|
| Muscle | Sarcopenia | Adult women aged over 65 years with sarcopenia | Body weight-based and elastic band resistance exercise | 60 min/session, 3 times/week, for 16 weeks | Grip strength↑, gait speed↑, isometric muscle strength↑ | The Institutional Review Board (KHSIRB-18-021) | Seo et al.447 |
| Older men with osteoporosis and sarcopenia | Low-volume/high-intensity-dynamic resistance exercise | Twice/week, for 12 months | Integral lumbar spine BMD↑, SMI↑, maximum hip/leg extensor strength↑ | NCT03453463 | Kemmler et al.448 | ||
| Adults with liver cirrhosis | Progressive resistance exercise training | 60 min/session, 3 times/week, for 12 weeks | Peak torque in isokinetic knee extension↑, CSA of the quadriceps muscle↑ | NCT02343653 | Aamann et al.449 | ||
| Older men with osteosarcope | High-intensity resistance exercise training | Twice/week, for 28 weeks | Sarcopenia Z-score↑, SMI↑, handgrip strength↑ | NCT03453463 | Lichtenberg et al.450 | ||
| Bone | Osteoporosis | Postmenopausal women with osteoporosis | Exercise program consisting of resistance exercise, balance exercise and aerobic exercise | Aerobic exercise: rapid walking, 60 min/day, 5 days/week, for 12 weeks resistance exercise and balance exercise: 70 min/day, 3 times/week, for 12 weeks | Muscle strength↑, walking performance↑, static balance↑ | NCT03816449 | Filipović et al.451 |
| Postmenopausal women with osteoporosis | High-intensity resistance and impact training, home-based exercise | 30 min/day, twice/week, for 8 months | Inclinometer-determined standing tall thoracic kyphosis↑, indices of bone strength↑, functional performance↑ | ACTRN12616000475448 | Watson et al.424,452 | ||
| Adult men aged over 45 years with osteoporosis | High-intensity resistance and impact training, supervised machine-based isometric axial compression | 30 min/day, twice/week, for 8 months | Femoral neck BMD↑, area and bone strength index↑, and trabecular BMC↑and bone strength index↑ | ANZCTR12616000344493 | Harding et al.453 | ||
| Postmenopausal women with osteoporosis | Exercise program contains low intensity strength and balance exercise | 60 min/day, 3 times/week, for 6 months | Static balance↑, dynamic balance↑, strength of the upper and lower limbs↑ | Landako Health Center in the Basque Country (Northern Spain) | Otero et al.454 | ||
| Heart | Heart failure | Frail adults with HFrEF | Supervised aerobic exercise training: cycle or walk-based exercise | >30 min/day, 3 times/week, for 3 months | Risk of all-cause hospitalization↓ | NCT00047437 | Pandey et al.455 |
| Middle-aged adults with LVH | Combination of yoga, balance, and strength training | 3 times/week, for 12 months | VO2 max↑, LV myocardial stiffness↓ | NCT03476785 | Hieda et al.456 | ||
| Brain | SIVCI | Adults with mild SIVCI | Progressive aerobic training | 3 times/week, for 6 months | General cognitive function (ADAS-Cog performance)↑, 6-minute walk distance↑ | NCT01027858 | Liu-Ambrose et al.457 |
| Stroke | Stroke adults with vascular cognitive impairment | Combination of endurance, strength, and balance exercise | 50 min/day, 3 times/week, for 3 months | Cognitive performances↑ | ISRCTN 16009172 | Wang et al.458 | |
| Adults with subacute stroke | Aerobic, body weight supported, treadmill based physical fitness training | 25 min/day, 5 times/week, for 4 weeks | Maximal walking Speed→, Barthel index score→, adverse events↑ | NCT01953549. | Nave et al.459 | ||
| Alzheimer’s disease | Adults with mild–moderate Alzheimer’s disease | Moderate-to-high-intensity aerobic exercise | 60 min/day, 3 times/week, for 16 weeks | Basic mobility↑, usual gait speed↑, fast gait speed↑ | NCT01681602 | Sobol et al.460 | |
| Adults with subjective memory impairment | Moderate-plus activities included moderate, hard, and very hard intensity activities (e.g., brisk walking, ballroom dancing, gym circuit, or swimming) | 50 min/day, 3 times/week, for 18 weeks | General cognitive function (ADAS-Cog performance)↑ | ACTRN12605000136606 | Lautenschlager et al.461 | ||
| Dementia | Adults with mild-to-moderate dementia | Moderate to high intensity aerobic and strength exercise training | 60–90 min/day, 3 times/week, for 16 weeks | Physical fitness (6 min walk test)↑, general cognitive function (ADAS-Cog performance)→ | ISRCTN10416500 | Lamb et al.462 |
BMD bone mineral density, SMI skeletal muscle mass index, CSA cross-sectional area, BMC bone mineral content, HFrEF heart failure with reduced ejection fraction, LVH left ventricular hypertrophy, VO2 maximal oxygen uptake, SIVCI subcortical ischemic vascular cognitive impairment, ADAS-Cog Alzheimer’s Disease Assessment Scale–Cognitive subscale
As a matter of fact, the knowledge of the adaptive responses to exercise is still only the tip of the iceberg. There are still three major points in the current researches on exercise for regeneration requiring further exploration. Firstly, the organism responds differently to diverse exercise patterns and intensities with great individual variability, resulting in instability and poor reproducibility of the exercise test. Therefore, the design of a rational exercise intervention is helpful to investigate the mechanisms of exercise regeneration, which is more effectively applied in clinical treatment further. Secondly, although the role of exercise for tissue regeneration undoubtedly brings new ideas and strategies, exercise mimetics need in-depth exploration. Notably, exercise mimetics may have utility across a wide range of human disorders, which is a gift for patients who are subjectively or objectively unable to achieve exercise benefits. However, as individual variability in exercise, exercise mimetics are not going to work as a universal panacea for divergent disorders but are more likely to be most effective for specific disorders, or even subtypes of such disorders. Thus, exploration of multi-target exercise mimetics is a key step in broadening the range of applications and improving the value of clinical translation. Thirdly, regeneration is indeed an anti-aging remedy, but it also often goes hand in hand with tumors. Whether exercise mimetics have a carcinogenic risk while promoting cell proliferation deserves more research to prove, which means a higher demand on the administration and dose of the drugs.
Beyond any doubt, exercise-induced regenerative medicine is an emerging and promising discipline. Currently, a variety of signaling pathways and related novel biomolecules have been identified in exercise adaptive regeneration, exhibiting more potential perspectives for disease prevention and treatment.
Acknowledgements
This work is supported by National Natural Science Foundation of China (92068101, 31871498), Project from Shanghai Municipal Health Commission (2022XD050), Shanghai Municipal Education Commission-Gaofeng Clinical Medicine Grant Support (828313), Project from National Research Center for Translational Medicine at Shanghai (TMSK-2021–106), Shanghai Collaborative Innovation Program on Regenerative Medicine and Stem Cell Research (2019CXJQ01), and Innovative Research Team of High-level Local Universities in Shanghai.
Author contributions
L.C. and Y.F. conceived and revised the paper. J.C. and R.Z. wrote the paper and organized the figures. All authors have read and approved the article.
Competing interests
The authors declare no competing interests.
Footnotes
These authors contributed equally: Jibao Chen, Ren Zhou
Contributor Information
Ye Feng, Email: fengye0509@163.com.
Lin Cheng, Email: lincheng@shsmu.edu.cn.
References
- 1.Caspersen CJ, Christenson PGM. Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep. 1985;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 2.Garber CE, et al. American college of sports medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 3.Arem H, et al. Leisure time physical activity and mortality. JAMA Intern. Med. 2015;175:959–967. doi: 10.1001/jamainternmed.2015.0533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bauman AE, et al. An evidence-based assessment of the impact of the Olympic Games on population levels of physical activity. Lancet. 2021;398:456–464. doi: 10.1016/S0140-6736(21)01165-X. [DOI] [PubMed] [Google Scholar]
- 5.Lieberman DE, Kistner TM, Richard D, Lee I, Baggish AL. The active grandparent hypothesis: physical activity and the evolution of extended human healthspans and lifespans. Proc. Natl Acad. Sci. USA. 2021;118:e2107621118. doi: 10.1073/pnas.2107621118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kohl HW, et al. The pandemic of physical inactivity: global action for public health. Lancet. 2012;380:294–305. doi: 10.1016/S0140-6736(12)60898-8. [DOI] [PubMed] [Google Scholar]
- 7.Bull FC, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020;54:1451–1462. doi: 10.1136/bjsports-2020-102955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hallal PC, et al. Global physical activity levels: surveillance progress, pitfalls, and prospects. Lancet. 2012;380:247–257. doi: 10.1016/S0140-6736(12)60646-1. [DOI] [PubMed] [Google Scholar]
- 9.Lavie CJ, Ozemek C, Carbone S, Katzmarzyk PT, Blair SN. Sedentary behavior, exercise, and cardiovascular health. Circ. Res. 2019;124:799–815. doi: 10.1161/CIRCRESAHA.118.312669. [DOI] [PubMed] [Google Scholar]
- 10.Lee C, Han K, Yoo J, Kwak M. Synergistic harmful interaction between sustained physical inactivity and hypertension/diabetes mellitus on the risk of all-cause mortality: a retrospective observational cohort study. J. Hypertens. 2021;39:2058–2066. doi: 10.1097/HJH.0000000000002905. [DOI] [PubMed] [Google Scholar]
- 11.Medina C, et al. Cardiovascular and diabetes burden attributable to physical inactivity in Mexico. Cardiovasc. Diabetol. 2020;19:99. doi: 10.1186/s12933-020-01050-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patterson R, et al. Sedentary behaviour and risk of all-cause, cardiovascular and cancer mortality, and incident type 2 diabetes: a systematic review and dose response meta-analysis. Eur. J. Epidemiol. 2018;33:811–829. doi: 10.1007/s10654-018-0380-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee I, et al. Effect of physical inactivity on major non-communicable diseases worldwide: an analysis of burden of disease and life expectancy. Lancet. 2012;380:219–229. doi: 10.1016/S0140-6736(12)61031-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rodriguez-Ayllon M, et al. Role of physical activity and sedentary behavior in the mental health of preschoolers, children and adolescents: a systematic review and meta-analysis. Sports Med. 2019;49:1383–1410. doi: 10.1007/s40279-019-01099-5. [DOI] [PubMed] [Google Scholar]
- 15.Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: towards understanding the antidepressant mechanisms of physical activity. Neurosci. Biobehav. Rev. 2019;107:525–539. doi: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- 16.Nooijen C, Blom V, Ekblom O, Ekblom MM, Kallings LV. Improving office workers’ mental health and cognition: a 3-arm cluster randomized controlled trial targeting physical activity and sedentary behavior in multi-component interventions. BMC Public Health. 2019;19:266. doi: 10.1186/s12889-019-6589-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Erguson BF. ACSM’s guidelines for exercise testing and prescription 9th Ed. 2014. J. Can. Chiropr. Assoc. 2014;58:328. [Google Scholar]
- 18.Lamberti N, et al. Effects of low-intensity endurance and resistance training on mobility in chronic stroke survivors: a pilot randomized controlled study. Eur. J. Phys. Rehab. Med. 2017;53:228–239. doi: 10.23736/S1973-9087.16.04322-7. [DOI] [PubMed] [Google Scholar]
- 19.Wehrle A, Kneis S, Dickhuth H, Gollhofer A, Bertz H. Endurance and resistance training in patients with acute leukemia undergoing induction chemotherapy—a randomized pilot study. Support. Care Cancer. 2019;27:1071–1079. doi: 10.1007/s00520-018-4396-6. [DOI] [PubMed] [Google Scholar]
- 20.Garcia-Pinillos F, Laredo-Aguilera JA, Munoz-Jimenez M, Latorre-Roman PA. Effects of 12-week concurrent high-intensity interval strength and endurance training program on physical performance in healthy older people. J. Strength Cond. Res. 2019;33:1445–1452. doi: 10.1519/JSC.0000000000001895. [DOI] [PubMed] [Google Scholar]
- 21.Gibala MJ, Little JP, MacDonald MJ, Hawley JA. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J. Physiol. 2012;590:1077–1084. doi: 10.1113/jphysiol.2011.224725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Knuiman P, Hopman MTE, Mensink M. Glycogen availability and skeletal muscle adaptations with endurance and resistance exercise. Nutr. Metab. 2015;12:59. doi: 10.1186/s12986-015-0055-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gabriele, et al. Muscle stem cell and physical activity: what point is the debate at? Open Med. 2017;12:144–156. doi: 10.1515/med-2017-0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Folland JP, Williams AG. The adaptations to strength training: morphological and neurological contributions to increased strength. Sports Med. 2007;37:145–168. doi: 10.2165/00007256-200737020-00004. [DOI] [PubMed] [Google Scholar]
- 25.Hoppeler H, Baum O, Lurman G, Mueller M. Molecular mechanisms of muscle plasticity with exercise. Compr. Physiol. 2011;1:1383–1412. doi: 10.1002/cphy.c100042. [DOI] [PubMed] [Google Scholar]
- 26.Farup J, Sørensen H, Kjølhede T. Similar changes in muscle fiber phenotype with differentiated consequences for rate of force development: endurance versus resistance training. Hum. Mov. Sci. 2014;34:109–119. doi: 10.1016/j.humov.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 27.McGee SL, Hargreaves M. Exercise adaptations: molecular mechanisms and potential targets for therapeutic benefit. Nat. Rev. Endocrinol. 2020;16:495–505. doi: 10.1038/s41574-020-0377-1. [DOI] [PubMed] [Google Scholar]
- 28.Garber CE, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults. Med. Sci. Sports Exerc. 2011;43:1334–1359. doi: 10.1249/MSS.0b013e318213fefb. [DOI] [PubMed] [Google Scholar]
- 29.Wilder RP, et al. Physical fitness assessment: an update. J. Long. Term. Eff. Med. Implants. 2006;16:193–204. doi: 10.1615/JLongTermEffMedImplants.v16.i2.90. [DOI] [PubMed] [Google Scholar]
- 30.Swift DL, Johannsen NM, Lavie CJ, Earnest CP, Church TS. The role of exercise and physical activity in weight loss and maintenance. Prog. Cardiovasc. Dis. 2014;56:441–447. doi: 10.1016/j.pcad.2013.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Androulakis-Korakakis P, Fisher JP, Steele J. The minimum effective training dose required to increase 1RM strength in resistance-trained men: a systematic review and meta-analysis. Sports Med. 2020;50:751–765. doi: 10.1007/s40279-019-01236-0. [DOI] [PubMed] [Google Scholar]
- 32.Martin-Smith R, et al. High intensity interval training (HIIT) improves cardiorespiratory fitness (CRF) in healthy, overweight and obese adolescents: a systematic review and meta-analysis of controlled studies. Int. J. Environ. Res. Public Health. 2020;17:2955. doi: 10.3390/ijerph17082955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.CHIN EC, et al. Low-frequency HIIT improves body composition and aerobic capacity in overweight men. Med. Sci. Sports Exerc. 2020;52:56–66. doi: 10.1249/MSS.0000000000002097. [DOI] [PubMed] [Google Scholar]
- 34.Grace F, et al. High intensity interval training (HIIT) improves resting blood pressure, metabolic (MET) capacity and heart rate reserve without compromising cardiac function in sedentary aging men. Exp. Gerontol. 2018;109:75–81. doi: 10.1016/j.exger.2017.05.010. [DOI] [PubMed] [Google Scholar]
- 35.Su L, et al. Effects of HIIT and MICT on cardiovascular risk factors in adults with overweight and/or obesity: a meta-analysis. PLoS ONE. 2019;14:e210644. doi: 10.1371/journal.pone.0210644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wewege M, van den Berg R, Ward RE, Keech A. The effects of high-intensity interval training vs. moderate-intensity continuous training on body composition in overweight and obese adults: a systematic review and meta-analysis. Obes. Rev. 2017;18:635–646. doi: 10.1111/obr.12532. [DOI] [PubMed] [Google Scholar]
- 37.Ross LM, Porter RR, Durstine JL. High-intensity interval training (HIIT) for patients with chronic diseases. J. Sport Health Sci. 2016;5:139–144. doi: 10.1016/j.jshs.2016.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fiuza-Luces C, et al. Exercise benefits in cardiovascular disease: beyond attenuation of traditional risk factors. Nat. Rev. Cardiol. 2018;15:731–743. doi: 10.1038/s41569-018-0065-1. [DOI] [PubMed] [Google Scholar]
- 39.Nasim, et al. High-intensity interval training increase GATA4, CITED4 and c-Kit and decreases C/EBPβ in rats after myocardial infarction. Life Sci. 2019;221:319–326. doi: 10.1016/j.lfs.2019.02.045. [DOI] [PubMed] [Google Scholar]
- 40.Eskandari A, Soori R, Choobineh S, Tirani ZM. Exercise promotes heart regeneration in aged rats by increasing regenerative factors in myocardial tissue. Physiol. Int. 2020;107:166–176. doi: 10.1556/2060.2020.00008. [DOI] [PubMed] [Google Scholar]
- 41.Gulsin GS, et al. Cardiovascular determinants of aerobic exercise capacity in adults with type 2 diabetes. Diabetes Care. 2020;43:2248–2256. doi: 10.2337/dc20-0706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang H, et al. Pre-operative exercise therapy triggers anti-inflammatory trained immunity of Kupffer cells through metabolic reprogramming. Nat. Metab. 2021;3:843–858. doi: 10.1038/s42255-021-00402-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.De Miguel Z, et al. Exercise plasma boosts memory and dampens brain inflammation via clusterin. Nature. 2021;600:494–499. doi: 10.1038/s41586-021-04183-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Wilson RJ, et al. Voluntary running protects against neuromuscular dysfunction following hindlimb ischemia-reperfusion in mice. J. Appl. Physiol. 2019;126:193–201. doi: 10.1152/japplphysiol.00358.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Li C, et al. Early wheel-running promotes functional recovery by improving mitochondria metabolism in olfactory ensheathing cells after ischemic stroke in rats. Behav. Brain Res. 2019;361:32–38. doi: 10.1016/j.bbr.2018.12.038. [DOI] [PubMed] [Google Scholar]
- 46.Kehm RD, et al. Recreational physical activity is associated with reduced breast cancer risk in adult women at high risk for breast cancer: a cohort study of women selected for familial and genetic risk. Cancer Res. 2020;80:116–125. doi: 10.1158/0008-5472.CAN-19-1847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Padr O AI, et al. Exercise training protects against cancer-induced cardiac remodeling in an animal model of urothelial carcinoma. Arch. Biochem. Biophys. 2018;645:12–18. doi: 10.1016/j.abb.2018.03.013. [DOI] [PubMed] [Google Scholar]
- 48.Hagar A, et al. Endurance training slows breast tumor growth in mice by suppressing Treg cells recruitment to tumors. BMC Cancer. 2019;19:536. doi: 10.1186/s12885-019-5745-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vervoort M. Regeneration and development in animals. Biol. Theory. 2011;6:25–35. doi: 10.1007/s13752-011-0005-3. [DOI] [Google Scholar]
- 50.Poss KD. Advances in understanding tissue regenerative capacity and mechanisms in animals. Nat. Rev. Genet. 2010;11:710–722. doi: 10.1038/nrg2879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Galliot B, Crescenzi M, Jacinto A, Tajbakhsh S. Trends in tissue repair and regeneration. Development. 2017;144:357–364. doi: 10.1242/dev.144279. [DOI] [PubMed] [Google Scholar]
- 52.Fu X. Repair cell first, then regenerate the tissues and organs. Mil. Med. Res. 2021;8:2. doi: 10.1186/s40779-021-00297-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bergmann O, et al. Evidence for cardiomyocyte renewal in humans. Science. 2009;324:98–102. doi: 10.1126/science.1164680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.He L, Zhou B. Cardiomyocyte proliferation: remove brakes and push accelerators. Cell Res. 2017;27:959–960. doi: 10.1038/cr.2017.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Nakada D, Levi BP, Morrison SJ. Integrating physiological regulation with stem cell and tissue homeostasis. Neuron. 2011;70:703–718. doi: 10.1016/j.neuron.2011.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Armada-da-Silva PA, Pereira C, Amado S, Veloso AP. Role of physical exercise for improving posttraumatic nerve regeneration. Int. Rev. Neurobiol. 2013;109:125–149. doi: 10.1016/B978-0-12-420045-6.00006-7. [DOI] [PubMed] [Google Scholar]
- 57.Zarei-Kheirabadi M, et al. Human embryonic stem cell-derived neural stem cells encapsulated in hyaluronic acid promotes regeneration in a contusion spinal cord injured rat. Int. J. Biol. Macromol. 2020;148:1118–1129. doi: 10.1016/j.ijbiomac.2020.01.219. [DOI] [PubMed] [Google Scholar]
- 58.Kim SG. A cell-based approach to dental pulp regeneration using mesenchymal stem cells: a scoping review. Int. J. Mol. Sci. 2021;22:4357. doi: 10.3390/ijms22094357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Čamernik K, et al. Mesenchymal stem cells in the musculoskeletal system: from animal models to human tissue regeneration? Stem Cell Rev. Rep. 2018;14:346–369. doi: 10.1007/s12015-018-9800-6. [DOI] [PubMed] [Google Scholar]
- 60.Spitzhorn L, et al. Transplanted human pluripotent stem cell-derived mesenchymal stem cells support liver regeneration in Gunn rats. Stem Cells Dev. 2018;27:1702–1714. doi: 10.1089/scd.2018.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Granata C, et al. High-intensity training induces non-stoichiometric changes in the mitochondrial proteome of human skeletal muscle without reorganisation of respiratory chain content. Nat. Commun. 2021;12:7056. doi: 10.1038/s41467-021-27153-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Janssen I, Heymsfield SB, Wang Z, Ross R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 2000;89:81–88. doi: 10.1152/jappl.2000.89.1.81. [DOI] [PubMed] [Google Scholar]
- 63.Jarvinen TA, et al. Muscle injuries: optimising recovery. Best. Pract. Res. Clin. Rheumatol. 2007;21:317–331. doi: 10.1016/j.berh.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 64.Joyner MJ, Coyle EF. Endurance exercise performance: the physiology of champions. J. Physiol. 2008;586:35–44. doi: 10.1113/jphysiol.2007.143834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Qaisar R, Bhaskaran S, Van Remmen H. Muscle fiber type diversification during exercise and regeneration. Free Radic. Biol. Med. 2016;98:56–67. doi: 10.1016/j.freeradbiomed.2016.03.025. [DOI] [PubMed] [Google Scholar]
- 66.Konopka AR, Harber MP. Skeletal muscle hypertrophy after aerobic exercise training. Exerc. Sport Sci. Rev. 2014;42:53–61. doi: 10.1249/JES.0000000000000007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Koulmann N, et al. Physical exercise during muscle regeneration improves recovery of the slow/oxidative phenotype. Muscle Nerve. 2016;55:91–100. doi: 10.1002/mus.25151. [DOI] [PubMed] [Google Scholar]
- 68.Richard-Bulteau H, Serrurier B, Crassous B, Banzet S, Koulmann N. Recovery of skeletal muscle mass after extensive injury: positive effects of increased contractile activity. Am. J. Physiol. Cell Physiol. 2008;294:C467–C476. doi: 10.1152/ajpcell.00355.2007. [DOI] [PubMed] [Google Scholar]
- 69.Hughes DC, Ellefsen S, Baar K. Adaptations to endurance and strength training. Cold Spring Harb. Perspect. Med. 2018;8:a29769. doi: 10.1101/cshperspect.a029769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Friedmann-Bette, et al. Strength training effects on muscular regeneration after ACL reconstruction. Med. Sci. Sports Exerc. 2018;50:1152–1161. doi: 10.1249/MSS.0000000000001564. [DOI] [PubMed] [Google Scholar]
- 71.Izadi MR, Habibi A, Khodabandeh Z, Nikbakht M. Synergistic effect of high-intensity interval training and stem cell transplantation with amniotic membrane scaffold on repair and rehabilitation after volumetric muscle loss injury. Cell Tissue Res. 2021;383:765–779. doi: 10.1007/s00441-020-03304-8. [DOI] [PubMed] [Google Scholar]
- 72.Grounds MD. The need to more precisely define aspects of skeletal muscle regeneration. Int. J. Biochem. Cell Biol. 2014;56:56–65. doi: 10.1016/j.biocel.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 73.Kaczmarek A, et al. The role of satellite cells in skeletal muscle regeneration—the effect of exercise and age. Biology. 2021;10:1056. doi: 10.3390/biology10101056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Yin H, Price F, Rudnicki MA. Satellite cells and the muscle stem cell niche. Physiol. Rev. 2013;93:23–67. doi: 10.1152/physrev.00043.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Fukada S, Nakamura A. Exercise/resistance training and muscle stem cells. Endocrinol. Metab. 2021;36:737–744. doi: 10.3803/EnM.2021.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Murach KA, Fry CS, Dupont Versteegden EE, McCarthy JJ, Peterson CA. Fusion and beyond: satellite cell contributions to loading‐induced skeletal muscle adaptation. FASEB J. 2021;35:e21893. doi: 10.1096/fj.202101096R. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Perandini LA, Chimin P, Lutkemeyer DDS, Câmara NOS. Chronic inflammation in skeletal muscle impairs satellite cells function during regeneration: can physical exercise restore the satellite cell niche? FASEB J. 2018;285:1973–1984. doi: 10.1111/febs.14417. [DOI] [PubMed] [Google Scholar]
- 78.Wang H, et al. Altered macrophage phenotype transition impairs skeletal muscle regeneration. Am. J. Pathol. 2014;184:1167–1184. doi: 10.1016/j.ajpath.2013.12.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Walton RG, et al. Human skeletal muscle macrophages increase following cycle training and are associated with adaptations that may facilitate growth. Sci. Rep. 2019;9:969. doi: 10.1038/s41598-018-37187-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Minari ALA, Oyama LM, Dos Santos RVT. Downhill exercise-induced changes in gene expression related with macrophage polarization and myogenic cells in the triceps long head of rats. Inflammation. 2015;38:209–217. doi: 10.1007/s10753-014-0024-x. [DOI] [PubMed] [Google Scholar]
- 81.Madaro L, et al. Denervation-activated STAT3–IL-6 signalling in fibro-adipogenic progenitors promotes myofibres atrophy and fibrosis. Nat. Cell Biol. 2018;20:917–927. doi: 10.1038/s41556-018-0151-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Farup J, Madaro L, Puri PL, Mikkelsen UR. Interactions between muscle stem cells, mesenchymal-derived cells and immune cells in muscle homeostasis, regeneration and disease. Cell Death Dis. 2015;6:e1830. doi: 10.1038/cddis.2015.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Joe AWB, et al. Muscle injury activates resident fibro/adipogenic progenitors that facilitate myogenesis. Nat. Cell Biol. 2010;12:153–163. doi: 10.1038/ncb2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Saito Y, Chikenji TS, Matsumura T, Nakano M, Fujimiya M. Exercise enhances skeletal muscle regeneration by promoting senescence in fibro-adipogenic progenitors. Nat. Commun. 2020;11:889. doi: 10.1038/s41467-020-14734-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Specker B, Minett M. Can physical activity improve peak bone mass? Curr. Osteoporos. Rep. 2013;11:229–236. doi: 10.1007/s11914-013-0152-5. [DOI] [PubMed] [Google Scholar]
- 86.Kemmler W, Bebenek M, von Stengel S, Bauer J. Peak-bone-mass development in young adults: effects of study program related levels of occupational and leisure time physical activity and exercise. A prospective 5-year study. Osteoporos. Int. 2015;26:653–662. doi: 10.1007/s00198-014-2918-8. [DOI] [PubMed] [Google Scholar]
- 87.Gomez-Cabello A, Ara I, Gonzalez-Aguero A, Casajus JA, Vicente-Rodriguez G. Effects of training on bone mass in older adults: a systematic review. Sports Med. 2012;42:301–325. doi: 10.2165/11597670-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 88.Suominen H. Muscle training for bone strength. Aging Clin. Exp. Res. 2006;18:85–93. doi: 10.1007/BF03327422. [DOI] [PubMed] [Google Scholar]
- 89.Shahabi S, et al. The effects of 8-week resistance and endurance trainings on bone strength compared to irisin injection protocol in mice. Adv. Biomed. Res. 2021;10:40. doi: 10.4103/abr.abr_220_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Turner CH. Three rules for bone adaptation to mechanical stimuli. Bone. 1998;23:399–407. doi: 10.1016/S8756-3282(98)00118-5. [DOI] [PubMed] [Google Scholar]
- 91.Davison S, et al. Exercise-based correlates to calcaneal osteogenesis produced by a chronic training intervention. Bone. 2019;128:115049. doi: 10.1016/j.bone.2019.115049. [DOI] [PubMed] [Google Scholar]
- 92.Maes C. Role and regulation of vascularization processes in endochondral bones. Calcif. Tissue Int. 2013;92:307–323. doi: 10.1007/s00223-012-9689-z. [DOI] [PubMed] [Google Scholar]
- 93.Yao Z, et al. Increase of both angiogenesis and bone mass in response to exercise depends on VEGF. J. Bone Miner. Res. 2004;19:1471–1480. doi: 10.1359/JBMR.040517. [DOI] [PubMed] [Google Scholar]
- 94.Holstein JH, et al. Exercise enhances angiogenesis during bone defect healing in mice. J. Orthop. Res. 2011;29:1086–1092. doi: 10.1002/jor.21352. [DOI] [PubMed] [Google Scholar]
- 95.Wazzani R, et al. Physical activity and bone vascularization: a way to explore in bone repair context? Life. 2021;11:783. doi: 10.3390/life11080783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH. Prevalence of chondral defects in athletes’ knees: a systematic review. Med. Sci. Sports Exerc. 2010;42:1795–1801. doi: 10.1249/MSS.0b013e3181d9eea0. [DOI] [PubMed] [Google Scholar]
- 97.Perera JR, Gikas PD, Bentley G. The present state of treatments for articular cartilage defects in the knee. Ann. R. Coll. Surg. Engl. 2012;94:381–387. doi: 10.1308/003588412X13171221592573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Wellsandt E, Golightly Y. Exercise in the management of knee and hip osteoarthritis. Curr. Opin. Rheumatol. 2018;30:151–159. doi: 10.1097/BOR.0000000000000478. [DOI] [PubMed] [Google Scholar]
- 99.Raposo F, Ramos M, Lúcia Cruz A. Effects of exercise on knee osteoarthritis: a systematic review. Musculoskelet. Care. 2021;19:399–435. doi: 10.1002/msc.1538. [DOI] [PubMed] [Google Scholar]
- 100.Vincent KR, Vasilopoulos T, Montero C, Vincent HK. Eccentric and concentric resistance exercise comparison for knee osteoarthritis. Med. Sci. Sports Exerc. 2019;51:1977–1986. doi: 10.1249/MSS.0000000000002010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Iijima H, et al. Exercise intervention increases expression of bone morphogenetic proteins and prevents the progression of cartilage-subchondral bone lesions in a post-traumatic rat knee model. Osteoarthr. Cartil. 2016;24:1092–1102. doi: 10.1016/j.joca.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 102.Assis L, et al. Aerobic exercise training and low-level laser therapy modulate inflammatory response and degenerative process in an experimental model of knee osteoarthritis in rats. Osteoarthr. Cartil. 2016;24:169–177. doi: 10.1016/j.joca.2015.07.020. [DOI] [PubMed] [Google Scholar]
- 103.Steele J, Bruce-Low S, Smith D, Osborne N, Thorkeldsen A. Can specific loading through exercise impart healing or regeneration of the intervertebral disc? Spine J. 2015;15:2117–2121. doi: 10.1016/j.spinee.2014.08.446. [DOI] [PubMed] [Google Scholar]
- 104.Fernandes TL, et al. Macrophage: a potential target on cartilage regeneration. Front. Immunol. 2020;11:111. doi: 10.3389/fimmu.2020.00111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Kubosch EJ, et al. The potential for synovium-derived stem cells in cartilage repair. Curr. Stem Cell Res. Ther. 2018;13:174–184. doi: 10.2174/1574888X12666171002111026. [DOI] [PubMed] [Google Scholar]
- 106.Benmassaoud MM, Gultian KA, DiCerbo M, Vega SL. Hydrogel screening approaches for bone and cartilage tissue regeneration. Ann. NY Acad. Sci. 2019;1460:25–42. doi: 10.1111/nyas.14247. [DOI] [PubMed] [Google Scholar]
- 107.Smith JK. Exercise as an adjuvant to cartilage regeneration therapy. Int. J. Mol. Sci. 2020;21:9471. doi: 10.3390/ijms21249471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Liu Y, et al. Exercise-induced piezoelectric stimulation for cartilage regeneration in rabbits. Sci. Transl. Med. 2022;14:eabi7282. doi: 10.1126/scitranslmed.abi7282. [DOI] [PubMed] [Google Scholar]
- 109.Yokota H, Leong DJ, Sun HB. Mechanical loading: bone remodeling and cartilage maintenance. Curr. Osteoporos. Rep. 2011;9:237–242. doi: 10.1007/s11914-011-0067-y. [DOI] [PubMed] [Google Scholar]
- 110.Tong X, et al. The effect of exercise on the prevention of osteoporosis and bone angiogenesis. Biomed. Res. Int. 2019;2019:8171897. doi: 10.1155/2019/8171897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Qi MC, Zou SJ, Han LC, Zhou HX, Hu J. Expression of bone‐related genes in bone marrow MSCs after cyclic mechanical strain: implications for distraction osteogenesis. Int. J. Oral Sci. 2009;1:143–150. doi: 10.4248/IJOS.09021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Schmid M, Kröpfl JM, Spengler CM. Changes in circulating stem and progenitor cell numbers following acute exercise in healthy human subjects: a systematic review and meta-analysis. Stem Cell Rev. Rep. 2021;17:1091–1120. doi: 10.1007/s12015-020-10105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chan CKF, et al. Identification of the human skeletal stem cell. Cell. 2018;175:43–56. doi: 10.1016/j.cell.2018.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ortinau LC, et al. Identification of functionally distinct Mx1+αSMA+ periosteal skeletal stem cells. Cell Stem Cell. 2019;25:784–796. doi: 10.1016/j.stem.2019.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kylmaoja E, Nakamura M, Tuukkanen J. Osteoclasts and remodeling based bone formation. Curr. Stem Cell Res. Ther. 2016;11:626–633. doi: 10.2174/1574888X10666151019115724. [DOI] [PubMed] [Google Scholar]
- 116.Marędziak M, Śmieszek A, Chrząstek K, Basinska K, Marycz K. Physical activity increases the total number of bone-marrow-derived mesenchymal stem cells, enhances their osteogenic potential, and inhibits their adipogenic properties. Stem Cells Int. 2015;2015:379093. doi: 10.1155/2015/379093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Kreja L, Liedert A, Hasni S, Claes L, Ignatius A. Mechanical regulation of osteoclastic genes in human osteoblasts. Biochem. Biophys. Res. Commun. 2008;368:582–587. doi: 10.1016/j.bbrc.2008.01.106. [DOI] [PubMed] [Google Scholar]
- 118.Kish K, Mezil Y, Ward WE, Klentrou P, Falk B. Effects of plyometric exercise session on markers of bone turnover in boys and young men. Eur. J. Appl. Physiol. 2015;115:2115–2124. doi: 10.1007/s00421-015-3191-z. [DOI] [PubMed] [Google Scholar]
- 119.Udagawa N, et al. Osteoclast differentiation by RANKL and OPG signaling pathways. J. Bone Miner. Metab. 2021;39:19–26. doi: 10.1007/s00774-020-01162-6. [DOI] [PubMed] [Google Scholar]
- 120.Sanchis-Gomar F, Fiuza-Luces C, Lucia A. Exercise as the master polypill of the 21st century for the prevention of cardiovascular disease. Int. J. Cardiol. 2015;181:360–361. doi: 10.1016/j.ijcard.2014.12.048. [DOI] [PubMed] [Google Scholar]
- 121.Lavie CJ, et al. Exercise and the cardiovascular system. Circ. Res. 2015;117:207–219. doi: 10.1161/CIRCRESAHA.117.305205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Utomi V, et al. Systematic review and meta-analysis of training mode, imaging modality and body size influences on the morphology and function of the male athlete’s heart. Heart. 2013;99:1727–1733. doi: 10.1136/heartjnl-2012-303465. [DOI] [PubMed] [Google Scholar]
- 123.Boström P, et al. C/EBPβ controls exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell. 2010;143:1072–1083. doi: 10.1016/j.cell.2010.11.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Vujic A, et al. Exercise induces new cardiomyocyte generation in the adult mammalian heart. Nat. Commun. 2018;9:1659. doi: 10.1038/s41467-018-04083-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Bei Y, et al. Cardiac cell proliferation is not necessary for exercise-induced cardiac growth but required for its protection against ischaemia/reperfusion injury. J. Cell. Mol. Med. 2017;21:1648–1655. doi: 10.1111/jcmm.13078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bansal A, et al. Proteomic analysis reveals late exercise effects on cardiac remodeling following myocardial infarction. J. Proteomics. 2010;73:2041–2049. doi: 10.1016/j.jprot.2010.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Yengo CM, Zimmerman SD, McCormick RJ, Thomas DP. Exercise training post-MI favorably modifies heart extracellular matrix in the rat. Med. Sci. Sports Exerc. 2012;44:1005–1012. doi: 10.1249/MSS.0b013e318244bc8a. [DOI] [PubMed] [Google Scholar]
- 128.Haykowsky M, et al. A meta-analysis of the effects of exercise training on left ventricular remodeling following myocardial infarction: start early and go longer for greatest exercise benefits on remodeling. Trials. 2011;12:92. doi: 10.1186/1745-6215-12-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Rahimi M, et al. The effect of high intensity interval training on cardioprotection against ischemia-reperfusion injury in wistar rats. EXCLI J. 2015;14:237–246. doi: 10.17179/excli2014-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Jia D, Hou L, Lv Y, Xi L, Tian Z. Postinfarction exercise training alleviates cardiac dysfunction and adverse remodeling via mitochondrial biogenesis and SIRT1/PGC‐1α/PI3K/Akt signaling. J. Cell. Physiol. 2019;234:23705–23718. doi: 10.1002/jcp.28939. [DOI] [PubMed] [Google Scholar]
- 131.Liu X, et al. miR-222 is necessary for exercise-induced cardiac growth and protects against pathological cardiac remodeling. Cell Metab. 2015;21:584–595. doi: 10.1016/j.cmet.2015.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Otaka N, et al. Myonectin is an exercise-induced myokine that protects the heart from ischemia-reperfusion injury. Circ. Res. 2018;123:1326–1338. doi: 10.1161/CIRCRESAHA.118.313777. [DOI] [PubMed] [Google Scholar]
- 133.Shi J, et al. miR-17-3p contributes to exercise-induced cardiac growth and protects against myocardial ischemia-reperfusion injury. Theranostics. 2017;7:664–676. doi: 10.7150/thno.15162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Bei Y, et al. Exercise-induced circulating extracellular vesicles protect against cardiac ischemia–reperfusion injury. Basic Res. Cardiol. 2017;112:38. doi: 10.1007/s00395-017-0628-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Garza MA. Cardiac remodeling and physical training post myocardial infarction. World J. Cardiol. 2015;7:52–64. doi: 10.4330/wjc.v7.i2.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Garza MA, Wason EA, Cruger JR, Chung E, Zhang JQ. Strength training attenuates post-infarct cardiac dysfunction and remodeling. J. Physiol. Sci. 2019;69:523–530. doi: 10.1007/s12576-019-00672-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Mueller S, et al. Effect of high-intensity interval training, moderate continuous training, or guideline-based physical activity advice on peak oxygen consumption in patients with heart failure with preserved ejection fraction. JAMA. 2021;325:542–551. doi: 10.1001/jama.2020.26812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Ellingsen Ø, et al. High-intensity interval training in patients with heart failure with reduced ejection fraction. Circulation. 2017;135:839–849. doi: 10.1161/CIRCULATIONAHA.116.022924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Tan J, et al. Moderate heart rate reduction promotes cardiac regeneration through stimulation of the metabolic pattern switch. Cell Rep. 2022;38:110468. doi: 10.1016/j.celrep.2022.110468. [DOI] [PubMed] [Google Scholar]
- 140.Sharman JE, La Gerche A, Coombes JS. Exercise and cardiovascular risk in patients with hypertension. Am. J. Hypertens. 2015;28:147–158. doi: 10.1093/ajh/hpu191. [DOI] [PubMed] [Google Scholar]
- 141.Antunes JMM, Ferreira RMP, Moreira-Gonçalves D. Exercise training as therapy for cancer-induced cardiac cachexia. Trends Mol. Med. 2018;24:709–727. doi: 10.1016/j.molmed.2018.06.002. [DOI] [PubMed] [Google Scholar]
- 142.Bond AM, et al. Differential timing and coordination of neurogenesis and astrogenesis in developing mouse hippocampal subregions. Brain Sci. 2020;10:909. doi: 10.3390/brainsci10120909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Moreno-Jiménez EP, et al. Adult hippocampal neurogenesis is abundant in neurologically healthy subjects and drops sharply in patients with Alzheimer’s disease. Nat. Med. 2019;25:554–560. doi: 10.1038/s41591-019-0375-9. [DOI] [PubMed] [Google Scholar]
- 144.Boldrini M, et al. Human hippocampal neurogenesis persists throughout aging. Cell Stem Cell. 2018;22:589–599. doi: 10.1016/j.stem.2018.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.van Praag H. Neurogenesis and exercise: past and future directions. Neuromol. Med. 2008;10:128–140. doi: 10.1007/s12017-008-8028-z. [DOI] [PubMed] [Google Scholar]
- 146.Nam SM, et al. Effects of treadmill exercise on neural stem cells, cell proliferation, and neuroblast differentiation in the subgranular zone of the dentate gyrus in cyclooxygenase-2 knockout mice. Neurochem. Res. 2013;38:2559–2569. doi: 10.1007/s11064-013-1169-y. [DOI] [PubMed] [Google Scholar]
- 147.Firth J, et al. Effect of aerobic exercise on hippocampal volume in humans: a systematic review and meta-analysis. Neuroimage. 2018;166:230–238. doi: 10.1016/j.neuroimage.2017.11.007. [DOI] [PubMed] [Google Scholar]
- 148.Batcho C, Stoquart G, Thonnard J. Brisk walking can promote functional recovery in chronic stroke patients. J. Rehabil. Med. 2013;45:854–859. doi: 10.2340/16501977-1211. [DOI] [PubMed] [Google Scholar]
- 149.Cumming TB, Tyedin K, Churilov L, Morris ME, Bernhardt J. The effect of physical activity on cognitive function after stroke: a systematic review. Int. Psychogeriatr. 2012;24:557–567. doi: 10.1017/S1041610211001980. [DOI] [PubMed] [Google Scholar]
- 150.Marzolini S, Oh P, McIlroy W, Brooks D. The effects of an aerobic and resistance exercise training program on cognition following stroke. Neurorehab. Neural Repair. 2013;27:392–402. doi: 10.1177/1545968312465192. [DOI] [PubMed] [Google Scholar]
- 151.Pang MYC, Charlesworth SA, Lau RWK, Chung RCK. Using aerobic exercise to improve health outcomes and quality of life in stroke: evidence-based exercise prescription recommendations. Cerebrovasc. Dis. 2013;35:7–22. doi: 10.1159/000346075. [DOI] [PubMed] [Google Scholar]
- 152.Vahlberg B, Cederholm T, Lindmark B, Zetterberg L, Hellström K. Short-term and long-term effects of a progressive resistance and balance exercise program in individuals with chronic stroke: a randomized controlled trial. Disabil. Rehabil. 2016;39:1615–1622. doi: 10.1080/09638288.2016.1206631. [DOI] [PubMed] [Google Scholar]
- 153.Mehta S, et al. Resistance training for gait speed and total distance walked during the chronic stage of stroke: a meta-analysis. Top. Stroke Rehabil. 2014;19:471–478. doi: 10.1310/tsr1906-471. [DOI] [PubMed] [Google Scholar]
- 154.Hu J, et al. Constraint-induced movement therapy enhances AMPA receptor-dependent synaptic plasticity in the ipsilateral hemisphere following ischemic stroke. Neural Regen. Res. 2021;16:319. doi: 10.4103/1673-5374.290900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Shabanzadeh AP, et al. Modifying PTEN recruitment promotes neuron survival, regeneration, and functional recovery after CNS injury. Cell Death Dis. 2019;10:567. doi: 10.1038/s41419-019-1802-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Tang Y, et al. Effects of treadmill exercise on cerebral angiogenesis and MT1-MMP expression after cerebral ischemia in rats. Brain Behav. 2018;8:e1079. doi: 10.1002/brb3.1079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Chang A, et al. Neurogenesis in the chronic lesions of multiple sclerosis. Brain. 2008;131:2366–2375. doi: 10.1093/brain/awn157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Guo LY, Lozinski B, Yong VW. Exercise in multiple sclerosis and its models: focus on the central nervous system outcomes. J. Neurosci. Res. 2020;98:509–523. doi: 10.1002/jnr.24524. [DOI] [PubMed] [Google Scholar]
- 159.Sandrow-Feinberg HR, Houlé JD. Exercise after spinal cord injury as an agent for neuroprotection, regeneration and rehabilitation. Brain Res. 2015;1619:12–21. doi: 10.1016/j.brainres.2015.03.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Chew C, Sengelaub D. Exercise promotes recovery after motoneuron injury via hormonal mechanisms. Neural Regen. Res. 2020;15:1373. doi: 10.4103/1673-5374.274323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Davaa G, et al. Exercise ameliorates spinal cord injury by changing DNA methylation. Cells. 2021;10:143. doi: 10.3390/cells10010143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Jung S, Seo T, Kim D. Treadmill exercise facilitates recovery of locomotor function through axonal regeneration following spinal cord injury in rats. J. Exerc. Rehabil. 2016;12:284–292. doi: 10.12965/jer.1632698.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Chang W, et al. Locomotion dependent neuron-glia interactions control neurogenesis and regeneration in the adult zebrafish spinal cord. Nat. Commun. 2021;12:4857. doi: 10.1038/s41467-021-25052-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hesp ZC, et al. Proliferating NG2-cell-dependent angiogenesis and scar formation alter axon growth and functional recovery after spinal cord injury in mice. J. Neurosci. 2018;38:1366–1382. doi: 10.1523/JNEUROSCI.3953-16.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Stenudd M, Sabelström H, Frisén J. Role of endogenous neural stem cells in spinal cord injury and repair. JAMA Neurol. 2015;72:235–237. doi: 10.1001/jamaneurol.2014.2927. [DOI] [PubMed] [Google Scholar]
- 166.Hackett AR, et al. Injury type-dependent differentiation of NG2 glia into heterogeneous astrocytes. Exp. Neurol. 2018;308:72–79. doi: 10.1016/j.expneurol.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Tashiro S, et al. Current progress of rehabilitative strategies in stem cell therapy for spinal cord injury: a review. NPJ Regen. Med. 2021;6:81. doi: 10.1038/s41536-021-00191-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Takeoka A, et al. Axon regeneration can facilitate or suppress hindlimb function after olfactory ensheathing glia transplantation. J. Neurosci. 2011;31:4298–4310. doi: 10.1523/JNEUROSCI.4967-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Hwang DH, et al. Survival of neural stem cell grafts in the lesioned spinal cord is enhanced by a combination of treadmill locomotor training via insulin-like growth factor-1 signaling. J. Neurosci. 2014;34:12788–12800. doi: 10.1523/JNEUROSCI.5359-13.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Benowitz LI, Popovich PG. Inflammation and axon regeneration. Curr. Opin. Neurol. 2011;24:577–583. doi: 10.1097/WCO.0b013e32834c208d. [DOI] [PubMed] [Google Scholar]
- 171.Conforti L, Gilley J, Coleman MP. Wallerian degeneration: an emerging axon death pathway linking injury and disease. Nat. Rev. Neurosci. 2014;15:394–409. doi: 10.1038/nrn3680. [DOI] [PubMed] [Google Scholar]
- 172.Kluding PM, et al. The effect of exercise on neuropathic symptoms, nerve function, and cutaneous innervation in people with diabetic peripheral neuropathy. J. Diabetes Complicat. 2012;26:424–429. doi: 10.1016/j.jdiacomp.2012.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Allet L, et al. The gait and balance of patients with diabetes can be improved: a randomised controlled trial. Diabetologia. 2010;53:458–466. doi: 10.1007/s00125-009-1592-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Zimmer P, et al. Eight-week, multimodal exercise counteracts a progress of chemotherapy-induced peripheral neuropathy and improves balance and strength in metastasized colorectal cancer patients: a randomized controlled trial. Support. Care Cancer. 2018;26:615–624. doi: 10.1007/s00520-017-3875-5. [DOI] [PubMed] [Google Scholar]
- 175.Dhawan S, Andrews R, Kumar L, Wadhwa S, Shukla G. A randomized controlled trial to assess the effectiveness of muscle strengthening and balancing exercises on chemotherapy-induced peripheral neuropathic pain and quality of life among cancer patients. Cancer Nurs. 2020;43:269–280. doi: 10.1097/NCC.0000000000000693. [DOI] [PubMed] [Google Scholar]
- 176.Ballestero-Pérez R, et al. Effectiveness of nerve gliding exercises on carpal tunnel syndrome: a systematic review. J. Manip. Physiol. Ther. 2017;40:50–59. doi: 10.1016/j.jmpt.2016.10.004. [DOI] [PubMed] [Google Scholar]
- 177.Streckmann F, et al. Exercise program improves therapy-related side-effects and quality of life in lymphoma patients undergoing therapy. Ann. Oncol. 2014;25:493–499. doi: 10.1093/annonc/mdt568. [DOI] [PubMed] [Google Scholar]
- 178.Kleckner IR, et al. Effects of exercise during chemotherapy on chemotherapy-induced peripheral neuropathy: a multicenter, randomized controlled trial. Support. Care Cancer. 2018;26:1019–1028. doi: 10.1007/s00520-017-4013-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Bland KA, et al. Effect of exercise on taxane chemotherapy–induced peripheral neuropathy in women with breast cancer: a randomized controlled trial. Clin. Breast Cancer. 2019;19:411–422. doi: 10.1016/j.clbc.2019.05.013. [DOI] [PubMed] [Google Scholar]
- 180.Neto WK, et al. Ladder-based resistance training elicited similar ultrastructural adjustments in forelimb and hindlimb peripheral nerves of young adult Wistar rats. Exp. Brain Res. 2021;239:2583–2592. doi: 10.1007/s00221-021-06156-y. [DOI] [PubMed] [Google Scholar]
- 181.Martins DF, et al. Long-term regular eccentric exercise decreases neuropathic pain-like behavior and improves motor functional recovery in an axonotmesis mouse model: the role of insulin-like growth factor-1. Mol. Neurobiol. 2018;55:6155–6168. doi: 10.1007/s12035-017-0829-3. [DOI] [PubMed] [Google Scholar]
- 182.de Moraes AA, de Almeida CAS, Lucas G, Thomazini JA, DeMaman AS. Effect of swimming training on nerve morphological recovery after compressive injury. Neurol. Res. 2018;40:955–962. doi: 10.1080/01616412.2018.1504180. [DOI] [PubMed] [Google Scholar]
- 183.Liao C, et al. Effects of swimming exercise on nerve regeneration in a rat sciatic nerve transection model. Biomedicine. 2017;7:3. doi: 10.1051/bmdcn/2017070103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Coelho Ferreira M, et al. Effects of two intensities of treadmill exercise on neuromuscular recovery after median nerve crush injury in Wistar rats. J. Exerc. Rehabil. 2019;15:392–400. doi: 10.12965/jer.19.328126.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Michalopoulos GK, Bhushan B. Liver regeneration: biological and pathological mechanisms and implications. Nat. Rev. Gastroenterol. Hepatol. 2021;18:40–55. doi: 10.1038/s41575-020-0342-4. [DOI] [PubMed] [Google Scholar]
- 186.Linecker M, et al. Exercise improves outcomes of surgery on fatty liver in mice. Ann. Surg. 2020;271:347–355. doi: 10.1097/SLA.0000000000002904. [DOI] [PubMed] [Google Scholar]
- 187.Fard Aghaie MH, et al. The effects of physical prehabilitation: Improved liver regeneration and mitochondrial function after ALPPS operation in a rodent model. J. Hepatobiliary Pancreat. Sci. 2021;28:692–702. doi: 10.1002/jhbp.945. [DOI] [PubMed] [Google Scholar]
- 188.Emery CF, Kiecolt-Glaser JK, Glaser R, Malarkey WB, Frid DJ. Exercise accelerates wound healing among healthy older adults: a preliminary investigation. J. Gerontol. A Biol. Sci. Med. Sci. 2005;60:1432–1436. doi: 10.1093/gerona/60.11.1432. [DOI] [PubMed] [Google Scholar]
- 189.Keylock KT, et al. Exercise accelerates cutaneous wound healing and decreases wound inflammation in aged mice. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2008;294:R179–R184. doi: 10.1152/ajpregu.00177.2007. [DOI] [PubMed] [Google Scholar]
- 190.Mutlak O, Aslam M, Standfield N. The influence of exercise on ulcer healing in patients with chronic venous insufficiency. Int. Angiol. 2018;37:160–168. doi: 10.23736/S0392-9590.18.03950-0. [DOI] [PubMed] [Google Scholar]
- 191.Zogaib FG, Monte-Alto-Costa A. Moderate intensity physical training accelerates healing of full-thickness wounds in mice. Braz. J. Med. Biol. Res. 2011;44:1025–1035. doi: 10.1590/S0100-879X2011007500115. [DOI] [PubMed] [Google Scholar]
- 192.Keylock T, Meserve L, Wolfe A. Low-intensity exercise accelerates wound healing in diabetic mice. Wounds. 2018;30:68–71. [PubMed] [Google Scholar]
- 193.Emmons R, Niemiro GM, Owolabi O, De Lisio M. Acute exercise mobilizes hematopoietic stem and progenitor cells and alters the mesenchymal stromal cell secretome. J. Appl. Physiol. 2016;120:624–632. doi: 10.1152/japplphysiol.00925.2015. [DOI] [PubMed] [Google Scholar]
- 194.Emmons R, Ngu M, Xu G, Hernández-Saavedra D, Lisio MD. Effects of obesity and exercise on bone marrow progenitor cells following radiation. Med. Sci. Sports Exerc. 2019;51:1126–1136. doi: 10.1249/MSS.0000000000001894. [DOI] [PubMed] [Google Scholar]
- 195.Frodermann V, et al. Exercise reduces inflammatory cell production and cardiovascular inflammation via instruction of hematopoietic progenitor cells. Nat. Med. 2019;25:1761–1771. doi: 10.1038/s41591-019-0633-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Stelzer I, et al. Ultra-endurance exercise induces stress and inflammation and affects circulating hematopoietic progenitor cell function. Scand. J. Med. Sci. Sports. 2015;25:e442–e450. doi: 10.1111/sms.12347. [DOI] [PubMed] [Google Scholar]
- 197.Appelbaum FR. Hematopoietic-cell transplantation at 50. N. Engl. J. Med. 2007;357:1472–1475. doi: 10.1056/NEJMp078166. [DOI] [PubMed] [Google Scholar]
- 198.De Lisio M, Baker JM, Parise G. Exercise promotes bone marrow cell survival and recipient reconstitution post-bone marrow transplantation, which is associated with increased survival. Exp. Hematol. 2013;41:143–154. doi: 10.1016/j.exphem.2012.10.003. [DOI] [PubMed] [Google Scholar]
- 199.Wiskemann J, Huber G. Physical exercise as adjuvant therapy for patients undergoing hematopoietic stem cell transplantation. Bone Marrow Transplant. 2008;41:321–329. doi: 10.1038/sj.bmt.1705917. [DOI] [PubMed] [Google Scholar]
- 200.Baumann FT, et al. Physical activity for patients undergoing an allogeneic hematopoietic stem cell transplantation: benefits of a moderate exercise intervention. Eur. J. Haematol. 2011;87:148–156. doi: 10.1111/j.1600-0609.2011.01640.x. [DOI] [PubMed] [Google Scholar]
- 201.Khan KM, Scott A. Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. Br. J. Sports Med. 2009;43:247–252. doi: 10.1136/bjsm.2008.054239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Magliulo L, Bondi D, Pini N, Marramiero L, Di Filippo ES. The wonder exerkines—novel insights: a critical state-of-the-art review. Mol. Cell. Biochem. 2022;477:105–113. doi: 10.1007/s11010-021-04264-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Safdar A, Saleem A, Tarnopolsky MA. The potential of endurance exercise-derived exosomes to treat metabolic diseases. Nat. Rev. Endocrinol. 2016;12:504–517. doi: 10.1038/nrendo.2016.76. [DOI] [PubMed] [Google Scholar]
- 204.Hoffmann C, Weigert C. Skeletal muscle as an endocrine organ: the role of myokines in exercise adaptations. Csh. Perspect. Med. 2017;7:a29793. doi: 10.1101/cshperspect.a029793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Han Y, You X, Xing W, Zhang Z, Zou W. Paracrine and endocrine actions of bone—the functions of secretory proteins from osteoblasts, osteocytes, and osteoclasts. Bone Res. 2018;6:16. doi: 10.1038/s41413-018-0019-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Henriksen T, Green C, Pedersen BK. Myokines in myogenesis and health. Recent Pat. Biotechnol. 2012;6:167–171. doi: 10.2174/1872208311206030167. [DOI] [PubMed] [Google Scholar]
- 207.Herrmann M, et al. Interactions between muscle and bone—where physics meets biology. Biomolecules. 2020;10:432. doi: 10.3390/biom10030432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Monemian EA, et al. Tissue regeneration from mechanical stretching of cell-cell adhesion. Tissue Eng. C Methods. 2019;25:631–640. doi: 10.1089/ten.tec.2019.0098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Castillo AB, Leucht P. Bone homeostasis and repair: forced into shape. Curr. Rheumatol. Rep. 2015;17:58. doi: 10.1007/s11926-015-0537-9. [DOI] [PubMed] [Google Scholar]
- 210.Dolan CP, et al. Digit specific denervation does not inhibit mouse digit tip regeneration. Dev. Biol. 2022;486:71–80. doi: 10.1016/j.ydbio.2022.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Murthy SE, Dubin AE, Patapoutian A. Piezos thrive under pressure: mechanically activated ion channels in health and disease. Nat. Rev. Mol. Cell Biol. 2017;18:771–783. doi: 10.1038/nrm.2017.92. [DOI] [PubMed] [Google Scholar]
- 212.Gudipaty SA, et al. Mechanical stretch triggers rapid epithelial cell division through Piezo1. Nature. 2017;543:118–121. doi: 10.1038/nature21407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Kefauver JM, Ward AB, Patapoutian A. Discoveries in structure and physiology of mechanically activated ion channels. Nature. 2020;587:567–576. doi: 10.1038/s41586-020-2933-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.He L, Si G, Huang J, Samuel ADT, Perrimon N. Mechanical regulation of stem-cell differentiation by the stretch-activated Piezo channel. Nature. 2018;555:103–106. doi: 10.1038/nature25744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Sun W, et al. The mechanosensitive Piezo1 channel is required for bone formation. ELife. 2019;8:e47454. doi: 10.7554/eLife.47454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Li X, et al. Stimulation of Piezo1 by mechanical signals promotes bone anabolism. ELife. 2019;8:e49631. doi: 10.7554/eLife.49631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Beech DJ. Endothelial Piezo1 channels as sensors of exercise. J. Physiol. 2018;596:979–984. doi: 10.1113/JP274396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Rozo M, Li L, Fan C. Targeting β1-integrin signaling enhances regeneration in aged and dystrophic muscle in mice. Nat. Med. 2016;22:889–896. doi: 10.1038/nm.4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Boppart MD, Mahmassani ZS. Integrin signaling: linking mechanical stimulation to skeletal muscle hypertrophy. Am. J. Physiol. Cell Physiol. 2019;317:C629–C641. doi: 10.1152/ajpcell.00009.2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Geiger B, Spatz JP, Bershadsky AD. Environmental sensing through focal adhesions. Nat. Rev. Mol. Cell Biol. 2009;10:21–33. doi: 10.1038/nrm2593. [DOI] [PubMed] [Google Scholar]
- 221.Plotkin LI, Davis HM, Cisterna BA, Sáez JC. Connexins and pannexins in bone and skeletal muscle. Curr. Osteoporos. Rep. 2017;15:326–334. doi: 10.1007/s11914-017-0374-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Shen H, Grimston S, Civitelli R, Thomopoulos S. Deletion of Connexin43 in osteoblasts/osteocytes leads to impaired muscle formation in mice. J. Bone Miner. Res. 2015;30:596–605. doi: 10.1002/jbmr.2389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Ren Q, Chen J, Liu Y. LRP5 and LRP6 in Wnt signaling: similarity and divergence. Front. Cell Dev. Biol. 2021;9:670960. doi: 10.3389/fcell.2021.670960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Williams BO. LRP5: from bedside to bench to bone. Bone. 2017;102:26–30. doi: 10.1016/j.bone.2017.03.044. [DOI] [PubMed] [Google Scholar]
- 225.Zhao L, Shim JW, Dodge TR, Robling AG, Yokota H. Inactivation of Lrp5 in osteocytes reduces Young’s modulus and responsiveness to the mechanical loading. Bone. 2013;54:35–43. doi: 10.1016/j.bone.2013.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Mehta V, et al. The guidance receptor plexin D1 is a mechanosensor in endothelial cells. Nature. 2020;578:290–295. doi: 10.1038/s41586-020-1979-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 227.Li X, Kordsmeier J, Xiong J. New advances in osteocyte mechanotransduction. Curr. Osteoporos. Rep. 2021;19:101–106. doi: 10.1007/s11914-020-00650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 228.Wackerhage H, Schoenfeld BJ, Hamilton DL, Lehti M, Hulmi JJ. Stimuli and sensors that initiate skeletal muscle hypertrophy following resistance exercise. J. Appl. Physiol. 2019;126:30–43. doi: 10.1152/japplphysiol.00685.2018. [DOI] [PubMed] [Google Scholar]
- 229.Song Y, et al. The mechanosensitive ion channel Piezo inhibits axon regeneration. Neuron. 2019;102:373–389. doi: 10.1016/j.neuron.2019.01.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Li F, et al. The Atr-Chek1 pathway inhibits axon regeneration in response to Piezo-dependent mechanosensation. Nat. Commun. 2021;12:3845. doi: 10.1038/s41467-021-24131-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Song Z, et al. Mechanosensing in liver regeneration. Semin. Cell Dev. Biol. 2017;71:153–167. doi: 10.1016/j.semcdb.2017.07.041. [DOI] [PubMed] [Google Scholar]
- 232.Lorenz L, et al. Mechanosensing by β1 integrin induces angiocrine signals for liver growth and survival. Nature. 2018;562:128–132. doi: 10.1038/s41586-018-0522-3. [DOI] [PubMed] [Google Scholar]
- 233.Lyon RC, Zanella F, Omens JH, Sheikh F. Mechanotransduction in cardiac hypertrophy and failure. Circ. Res. 2015;116:1462–1476. doi: 10.1161/CIRCRESAHA.116.304937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 234.Jiang F, et al. The mechanosensitive Piezo1 channel mediates heart mechano-chemo transduction. Nat. Commun. 2021;12:869. doi: 10.1038/s41467-021-21178-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Tsata V, Beis D. In full force. Mechanotransduction and morphogenesis during homeostasis and tissue regeneration. J. Cardiovasc. Dev. Dis. 2020;7:40. doi: 10.3390/jcdd7040040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Santos L, Ugun-Klusek A, Coveney C, Boocock DJ. Multiomic analysis of stretched osteocytes reveals processes and signalling linked to bone regeneration and cancer. NPJ Regen. Med. 2021;6:32. doi: 10.1038/s41536-021-00141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 237.Tanaka S, Matsumoto T. Sclerostin: from bench to bedside. J. Bone Miner. Metab. 2021;39:332–340. doi: 10.1007/s00774-020-01176-0. [DOI] [PubMed] [Google Scholar]
- 238.Crossland H, et al. Focal adhesion kinase is required for IGF-1-mediated growth of skeletal muscle cells via a TSC2/mTOR/S6K1-associated pathway. Am. J. Physiol. Endocrinol. Metab. 2013;305:E183–E193. doi: 10.1152/ajpendo.00541.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 239.Sato T, et al. A FAK/HDAC5 signaling axis controls osteocyte mechanotransduction. Nat. Commun. 2020;11:3282. doi: 10.1038/s41467-020-17099-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 240.Dupont S, et al. Role of YAP/TAZ in mechanotransduction. Nature. 2011;474:179–183. doi: 10.1038/nature10137. [DOI] [PubMed] [Google Scholar]
- 241.Aragona M, et al. A mechanical checkpoint controls multicellular growth through YAP/TAZ regulation by actin-processing factors. Cell. 2013;154:1047–1059. doi: 10.1016/j.cell.2013.07.042. [DOI] [PubMed] [Google Scholar]
- 242.Wang L, et al. Integrin-YAP/TAZ-JNK cascade mediates atheroprotective effect of unidirectional shear flow. Nature. 2016;540:579–582. doi: 10.1038/nature20602. [DOI] [PubMed] [Google Scholar]
- 243.Zheng Y, Pan D. The Hippo signaling pathway in development and disease. Dev. Cell. 2019;50:264–282. doi: 10.1016/j.devcel.2019.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.Piccolo S, Dupont S, Cordenonsi M. The biology of YAP/TAZ: Hippo signaling and beyond. Physiol. Rev. 2014;94:1287–1312. doi: 10.1152/physrev.00005.2014. [DOI] [PubMed] [Google Scholar]
- 245.Ma S, Meng Z, Chen R, Guan K. The Hippo pathway: biology and pathophysiology. Annu. Rev. Biochem. 2019;88:577–604. doi: 10.1146/annurev-biochem-013118-111829. [DOI] [PubMed] [Google Scholar]
- 246.Chang Y, Wu J, Wang C, Jang ACC. Hippo signaling-mediated mechanotransduction in cell movement and cancer metastasis. Front. Mol. Biosci. 2020;6:157. doi: 10.3389/fmolb.2019.00157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Liu Q, et al. Suppressing Hippo signaling in the stem cell niche promotes skeletal muscle regeneration. Stem Cells. 2021;39:737–749. doi: 10.1002/stem.3343. [DOI] [PubMed] [Google Scholar]
- 248.Gabriel BM, Hamilton DL, Tremblay AM, Wackerhage H. The Hippo signal transduction network for exercise physiologists. J. Appl. Physiol. 2016;120:1105–1117. doi: 10.1152/japplphysiol.01076.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 249.Ziouti F, et al. NOTCH signaling is activated through mechanical strain in human bone marrow-derived mesenchymal stromal cells. Stem Cells Int. 2019;2019:5150634. doi: 10.1155/2019/5150634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 250.Stassen OMJA, Ristori T, Sahlgren CM. Notch in mechanotransduction–from molecular mechanosensitivity to tissue mechanostasis. J. Cell Sci. 2020;133:jcs250738. doi: 10.1242/jcs.250738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Arthur ST, Cooley ID. The effect of physiological stimuli on sarcopenia; impact of Notch and Wnt signaling on impaired aged skeletal muscle repair. Int. J. Biol. Sci. 2012;8:731–760. doi: 10.7150/ijbs.4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Bi P, et al. Stage-specific effects of Notch activation during skeletal myogenesis. ELife. 2016;5:e17355. doi: 10.7554/eLife.17355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 253.Fujimaki S, et al. Functional overload enhances satellite cell properties in skeletal muscle. Stem Cells Int. 2016;2016:7619418. doi: 10.1155/2016/7619418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Lin J, et al. Swimming exercise stimulates IGF1/PI3K/Akt and AMPK/SIRT1/PGC1α survival signaling to suppress apoptosis and inflammation in aging hippocampus. Aging. 2020;12:6852–6864. doi: 10.18632/aging.103046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Feng L, Li B, Xi Y, Cai M, Tian Z. Aerobic exercise and resistance exercise alleviate skeletal muscle atrophy through IGF-1/IGF-1R-PI3K/Akt pathway in mice with myocardial infarction. Am. J. Physiol. Cell Physiol. 2022;322:C164–C176. doi: 10.1152/ajpcell.00344.2021. [DOI] [PubMed] [Google Scholar]
- 256.Kraemer WJ, Ratamess NA, Nindl BC. Recovery responses of testosterone, growth hormone, and IGF-1 after resistance exercise. J. Appl. Physiol. 2017;122:549–558. doi: 10.1152/japplphysiol.00599.2016. [DOI] [PubMed] [Google Scholar]
- 257.Yu T, Chang Y, Gao X, Li H, Zhao P. Dynamic expression and the role of BDNF in exercise-induced skeletal muscle regeneration. Int. J. Sports Med. 2017;38:959–966. doi: 10.1055/s-0043-118343. [DOI] [PubMed] [Google Scholar]
- 258.Li S, et al. MOTS-c and exercise restore cardiac function by activating of NRG1-ErbB signaling in diabetic rats. Front. Endocrinol. 2022;13:812032. doi: 10.3389/fendo.2022.812032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 259.Yoshida T, Delafontaine P. Mechanisms of IGF-1-mediated regulation of skeletal muscle hypertrophy and atrophy. Cells. 2020;9:1970. doi: 10.3390/cells9091970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Fink J, Schoenfeld BJ, Nakazato K. The role of hormones in muscle hypertrophy. Phys. Sportsmed. 2018;46:129–134. doi: 10.1080/00913847.2018.1406778. [DOI] [PubMed] [Google Scholar]
- 261.Guntur AR, Rosen CJ. IGF-1 regulation of key signaling pathways in bone. Bonekey Rep. 2013;2:437. doi: 10.1038/bonekey.2013.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Bikle DD, et al. Role of IGF-I signaling in muscle bone interactions. Bone. 2015;80:79–88. doi: 10.1016/j.bone.2015.04.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 263.McMullen JR, et al. Phosphoinositide 3-kinase(p110α) plays a critical role for the induction of physiological, but not pathological, cardiac hypertrophy. Proc. Natl Acad. Sci. USA. 2003;100:12355–12360. doi: 10.1073/pnas.1934654100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 264.Kim J, et al. Insulin-like growth factor i receptor signaling is required for exercise-induced cardiac hypertrophy. Mol. Endocrinol. 2008;22:2531–2543. doi: 10.1210/me.2008-0265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 265.Gumà A, Martínez-Redondo V, López-Soldado I, Cantó C, Zorzano A. Emerging role of neuregulin as a modulator of muscle metabolism. Am. J. Physiol. Endocrinol. Metab. 2010;298:E742–E750. doi: 10.1152/ajpendo.00541.2009. [DOI] [PubMed] [Google Scholar]
- 266.D Uva G, et al. ERBB2 triggers mammalian heart regeneration bypromoting cardiomyocyte dedifferentiation andproliferation. Nat. Cell Biol. 2015;17:627–638. doi: 10.1038/ncb3149. [DOI] [PubMed] [Google Scholar]
- 267.Cai MX, et al. Exercise training activates neuregulin 1/ErbB signaling and promotes cardiac repair in a rat myocardial infarction model. Life Sci. 2016;149:1–9. doi: 10.1016/j.lfs.2016.02.055. [DOI] [PubMed] [Google Scholar]
- 268.Gubert C, Hannan AJ. Exercise mimetics: harnessing the therapeutic effects of physical activity. Nat. Rev. Drug Discov. 2021;20:862–879. doi: 10.1038/s41573-021-00217-1. [DOI] [PubMed] [Google Scholar]
- 269.Li Y, et al. Protection against acute cerebral ischemia/reperfusion injury by Leonuri Herba Total Alkali via modulation of BDNF-TrKB-PI3K/Akt signaling pathway in rats. Biomed. Pharmacother. 2021;133:111021. doi: 10.1016/j.biopha.2020.111021. [DOI] [PubMed] [Google Scholar]
- 270.Chang M, Park C, Rhie S, Shim W, Kim D. Early treadmill exercise increases macrophage migration inhibitory factor expression after cerebral ischemia/reperfusion. Neural Regen. Res. 2019;14:1230–1236. doi: 10.4103/1673-5374.251330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Zhang Q, Deng X, Sun X, Xu J, Sun F. Exercise promotes axon regeneration of newborn striatonigral and corticonigral projection neurons in rats after ischemic stroke. PLoS ONE. 2013;8:e80139. doi: 10.1371/journal.pone.0080139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Kowiański P, et al. BDNF: A key factor with multipotent impact on brain signaling and synaptic plasticity. Cell. Mol. Neurobiol. 2018;38:579–593. doi: 10.1007/s10571-017-0510-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 273.Liu PZ, Nusslock R. Exercise-mediated neurogenesis in the hippocampus via BDNF. Front. Neurosci. 2018;12:52. doi: 10.3389/fnins.2018.00052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 274.Bilchak JN, Caron G, Cote MP. Exercise-induced plasticity in signaling pathways involved in motor recovery after spinal cord injury. Int. J. Mol. Sci. 2021;22:4858. doi: 10.3390/ijms22094858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Weishaupt N, Blesch A, Fouad K. BDNF: the career of a multifaceted neurotrophin in spinal cord injury. Exp. Neurol. 2012;238:254–264. doi: 10.1016/j.expneurol.2012.09.001. [DOI] [PubMed] [Google Scholar]
- 276.McGregor CE, English AW. The role of BDNF in peripheral nerve regeneration: activity-dependent treatments and Val66Met. Front. Cell. Neurosci. 2019;12:522. doi: 10.3389/fncel.2018.00522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 277.English AW, Wilhelm JC, Ward PJ. Exercise, neurotrophins, and axon regeneration in the PNS. Physiology. 2014;29:437–445. doi: 10.1152/physiol.00028.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 278.Reddy LVK, Murugan D, Mullick M, Begum Moghal ET, Sen D. Recent approaches for angiogenesis in search of successful tissue engineering and regeneration. Curr. Stem Cell Res. Ther. 2020;15:111–134. doi: 10.2174/1574888X14666191104151928. [DOI] [PubMed] [Google Scholar]
- 279.Hu K, Olsen BR. The roles of vascular endothelial growth factor in bone repair and regeneration. Bone. 2016;91:30–38. doi: 10.1016/j.bone.2016.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 280.Zhang J, et al. Endothelial lactate controls muscle regeneration from ischemia by inducing M2-like macrophage polarization. Cell Metab. 2020;31:1136–1153. doi: 10.1016/j.cmet.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 281.Shibuya M. Differential roles of vascular endothelial growth factor receptor-1 and receptor-2 in angiogenesis. J. Biochem. Mol. Biol. 2006;39:469–478. doi: 10.5483/bmbrep.2006.39.5.469. [DOI] [PubMed] [Google Scholar]
- 282.Melincovici CS, et al. Vascular endothelial growth factor (VEGF)-key factor in normal and pathological angiogenesis. Rom. J. Morphol. Embryol. 2018;59:455–467. [PubMed] [Google Scholar]
- 283.Tang K, Xia FC, Wagner PD, Breen EC. Exercise-induced VEGF transcriptional activation in brain, lung and skeletal muscle. Respir. Physiol. Neurobi. 2010;170:16–22. doi: 10.1016/j.resp.2009.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 284.Pourheydar B, Biabanghard A, Azari R, Khalaji N, Chodari L. Exercise improves aging-related decreased angiogenesis through modulating VEGF-A, TSP-1 and p-NF-Ƙb protein levels in myocardiocytes. J. Cardiovasc. Thorac. Res. 2020;12:129–135. doi: 10.34172/jcvtr.2020.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 285.Tryfonos A, et al. Exercise training enhances angiogenesis-related gene responses in skeletal muscle of patients with chronic heart failure. Cells. 2021;10:1915. doi: 10.3390/cells10081915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 286.Chen L, Bai J, Li Y. miR-29 mediates exercise-induced skeletal muscle angiogenesis by targeting VEGFA, COL4A1 and COL4A2 via the PI3K/Akt signaling pathway. Mol. Med. Rep. 2020;22:661–670. doi: 10.3892/mmr.2020.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 287.Da Y, et al. Mechanical stress promotes biological functions of C2C12 myoblasts by activating PI3K/AKT/mTOR signaling pathway. Mol. Med. Rep. 2019;21:470–477. doi: 10.3892/mmr.2019.10808. [DOI] [PubMed] [Google Scholar]
- 288.Song F, et al. Mechanical stress regulates osteogenesis and adipogenesis of rat mesenchymal stem cells through PI3K/Akt/GSK-3β/β-Catenin signaling pathway. Biomed. Res. Int. 2017;2017:6027402. doi: 10.1155/2017/6027402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Liu M, et al. Phosphorylated GSK-3β protects stress-induced apoptosis of myoblasts via the PI3K/Akt signaling pathway. Mol. Med. Rep. 2020;22:317–327. doi: 10.3892/mmr.2020.11105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 290.Liang J, et al. Promotion of aerobic exercise induced angiogenesis is associated with decline in blood pressure in hypertension. Hypertension. 2021;77:1141–1153. doi: 10.1161/HYPERTENSIONAHA.120.16107. [DOI] [PubMed] [Google Scholar]
- 291.Laplante M, Sabatini DM. mTOR signaling in growth control and disease. Cell. 2012;149:274–293. doi: 10.1016/j.cell.2012.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 292.Watson K, Baar K. mTOR and the health benefits of exercise. Semin. Cell Dev. Biol. 2014;36:130–139. doi: 10.1016/j.semcdb.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 293.Baraldo M, et al. Skeletal muscle mTORC1 regulates neuromuscular junction stability. J. Cachexia Sarcopenia Muscle. 2020;11:208–225. doi: 10.1002/jcsm.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 294.Chen Z, et al. Exercise protects proliferative muscle satellite cells against exhaustion via the Igfbp7-Akt-mTOR axis. Theranostics. 2020;10:6448–6466. doi: 10.7150/thno.43577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 295.Liao J, Li Y, Zeng F, Wu Y. Regulation of mTOR pathway in exercise-induced cardiac hypertrophy. Int. J. Sports Med. 2015;36:343–350. doi: 10.1055/s-0034-1395585. [DOI] [PubMed] [Google Scholar]
- 296.Chen K, et al. Exercise training improves motor skill learning via selective activation of mTOR. Sci. Adv. 2019;5:w1888. doi: 10.1126/sciadv.aaw1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 297.Kar AN, et al. MicroRNAs 21 and 199a-3p regulate axon growth potential through modulation of Pten and mTor mRNAs. eNeuro. 2021;8:121–155. doi: 10.1523/ENEURO.0155-21.2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Valvezan AJ, Manning BD. Molecular logic of mTORC1 signalling as a metabolic rheostat. Nat. Metab. 2019;1:321–333. doi: 10.1038/s42255-019-0038-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 299.Deleyto-Seldas N, Efeyan A. The mTOR-autophagy axis and the control of metabolism. Front. Cell Dev. Biol. 2021;9:655731. doi: 10.3389/fcell.2021.655731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 300.Jang Y. Endurance exercise-induced expression of autophagy-related protein coincides with anabolic expression and neurogenesis in the hippocampus of the mouse brain. Neuroreport. 2020;31:442–449. doi: 10.1097/WNR.0000000000001431. [DOI] [PubMed] [Google Scholar]
- 301.Ding S, et al. C/EBPB-CITED4 in exercised heart. Adv. Exp. Med. Biol. 2017;1000:247–259. doi: 10.1007/978-981-10-4304-8_14. [DOI] [PubMed] [Google Scholar]
- 302.Lerchenmüller C, et al. CITED4 protects against adverse remodeling in response to physiological and pathological stress. Circ. Res. 2020;127:631–646. doi: 10.1161/CIRCRESAHA.119.315881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 303.Bezzerides VJ, et al. CITED4 induces physiologic hypertrophy and promotes functional recovery after ischemic injury. JCI Insight. 2016;1:e85904. doi: 10.1172/jci.insight.85904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Bahramian A, Mirzaei B, Karimzadeh F, Ramhmaninia F, Hemmatinafar M. The effects of exercise training intensity on the expression of C/EBPβ and CITED4 in rats with myocardial infarction. Asian J. Sports Med. 2018;9:e59300. doi: 10.5812/asjsm.59300. [DOI] [Google Scholar]
- 305.Ryall KA, Bezzerides VJ, Rosenzweig A, Saucerman JJ. Phenotypic screen quantifying differential regulation of cardiac myocyte hypertrophy identifies CITED4 regulation of myocyte elongation. J. Mol. Cell. Cardiol. 2014;72:74–84. doi: 10.1016/j.yjmcc.2014.02.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 306.Zeng Z, et al. Exercise-induced autophagy suppresses sarcopenia through Akt/mTOR and Akt/FoxO3a signal pathways and AMPK-mediated mitochondrial quality control. Front. Physiol. 2020;11:583478. doi: 10.3389/fphys.2020.583478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 307.Sanchez AMJ, Candau RB, Bernardi H. FoxO transcription factors: their roles in the maintenance of skeletal muscle homeostasis. Cell. Mol. Life Sci. 2014;71:1657–1671. doi: 10.1007/s00018-013-1513-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 308.Rathbone CR, Booth FW, Lees SJ. FoxO3a preferentially induces p27Kip1 expression while impairing muscle precursor cell-cycle progression. Muscle Nerve. 2008;37:84–89. doi: 10.1002/mus.20897. [DOI] [PubMed] [Google Scholar]
- 309.Liu C, et al. Effect of RNA oligonucleotide targeting Foxo-1 on muscle growth in normal and cancer cachexia mice. Cancer Gene Ther. 2007;14:945–952. doi: 10.1038/sj.cgt.7701091. [DOI] [PubMed] [Google Scholar]
- 310.Wen X, Jiao L, Tan H. MAPK/ERK pathway as a central regulator in vertebrate organ regeneration. Int. J. Mol. Sci. 2022;23:1464. doi: 10.3390/ijms23031464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 311.Aharonov A, et al. ERBB2 drives YAP activation and EMT-like processes during cardiac regeneration. Nat. Cell Biol. 2020;22:1346–1356. doi: 10.1038/s41556-020-00588-4. [DOI] [PubMed] [Google Scholar]
- 312.Tane S, et al. CDK inhibitors, p21Cip1 and p27Kip1, participate in cell cycle exit of mammalian cardiomyocytes. Biochem. Biophys. Res. Commun. 2014;443:1105–1109. doi: 10.1016/j.bbrc.2013.12.109. [DOI] [PubMed] [Google Scholar]
- 313.Mohamed T, et al. Regulation of cell cycle to stimulate adult cardiomyocyte proliferation and cardiac regeneration. Cell. 2018;173:104–116. doi: 10.1016/j.cell.2018.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 314.Zhu L, et al. Remifentanil preconditioning promotes liver regeneration via upregulation of β-arrestin 2/ERK/cyclin D1 pathway. Biochem. Biophys. Res. Commun. 2021;557:69–76. doi: 10.1016/j.bbrc.2021.04.008. [DOI] [PubMed] [Google Scholar]
- 315.Liu W, et al. Physical exercise promotes proliferation and differentiation of endogenous neural stem cells via ERK in rats with cerebral infarction. Mol. Med. Rep. 2018;18:1455–1464. doi: 10.3892/mmr.2018.9147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 316.Brett JO, et al. Exercise rejuvenates quiescent skeletal muscle stem cells in old mice through restoration of Cyclin D1. Nat. Metab. 2020;2:307–317. doi: 10.1038/s42255-020-0190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 317.Kwon JH, Moon KM, Min KW. Exercise-induced myokines can explain the importance of physical activity in the elderly: an overview. Healthcare. 2020;8:378. doi: 10.3390/healthcare8040378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 318.Zhang L, et al. Medium-intensity treadmill exercise exerts beneficial effects on bone modeling through bone marrow mesenchymal stromal cells. Front. Cell Dev. Biol. 2020;8:600639. doi: 10.3389/fcell.2020.600639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 319.Iijima H, et al. Physiological exercise loading suppresses post-traumatic osteoarthritis progression via an increase in bone morphogenetic proteins expression in an experimental rat knee model. Osteoarthr. Cartil. 2017;25:964–975. doi: 10.1016/j.joca.2016.12.008. [DOI] [PubMed] [Google Scholar]
- 320.Zou M, et al. The Smad dependent TGF-β and BMP signaling pathway in bone remodeling and therapies. Front. Mol. Biosci. 2021;8:593310. doi: 10.3389/fmolb.2021.593310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 321.Zuo C, et al. Osteoblastogenesis regulation signals in bone remodeling. Osteoporos. Int. 2012;23:1653–1663. doi: 10.1007/s00198-012-1909-x. [DOI] [PubMed] [Google Scholar]
- 322.Wu M, Chen G, Li Y. TGF-β and BMP signaling in osteoblast, skeletal development, and bone formation, homeostasis and disease. Bone Res. 2016;4:16009. doi: 10.1038/boneres.2016.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 323.Chen G, Deng C, Li Y. TGF-β and BMP signaling in osteoblast differentiation and bone formation. Int. J. Biol. Sci. 2012;8:272–288. doi: 10.7150/ijbs.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 324.Valladares-Ide D, et al. Activation of protein synthesis, regeneration, and MAPK signaling pathways following repeated bouts of eccentric cycling. Am. J. Physiol. Endocrinol. Metab. 2019;317:E1131–E1139. doi: 10.1152/ajpendo.00216.2019. [DOI] [PubMed] [Google Scholar]
- 325.Fan W, Evans RM. Exercise mimetics: impact on health and performance. Cell Metab. 2017;25:242–247. doi: 10.1016/j.cmet.2016.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Herzig S, Shaw RJ. AMPK: guardian of metabolism and mitochondrial homeostasis. Nat. Rev. Mol. Cell Biol. 2018;19:121–135. doi: 10.1038/nrm.2017.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 327.Garcia D, Shaw RJ. AMPK: mechanisms of cellular energy sensing and restoration of metabolic balance. Mol. Cell. 2017;66:789–800. doi: 10.1016/j.molcel.2017.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 328.Chen H, Fan W, He H, Huang F. PGC-1: a key regulator in bone homeostasis. J. Bone Miner. Metab. 2022;40:1–8. doi: 10.1007/s00774-021-01263-w. [DOI] [PubMed] [Google Scholar]
- 329.Norrbom J, et al. PGC-1alpha mRNA expression is influenced by metabolic perturbation in exercising human skeletal muscle. J. Appl. Physiol. 2004;96:189–194. doi: 10.1152/japplphysiol.00765.2003. [DOI] [PubMed] [Google Scholar]
- 330.Koves TR, et al. Peroxisome proliferator-activated receptor-gamma co-activator 1alpha-mediated metabolic remodeling of skeletal myocytes mimics exercise training and reverses lipid-induced mitochondrial inefficiency. J. Biol. Chem. 2005;280:33588–33598. doi: 10.1074/jbc.M507621200. [DOI] [PubMed] [Google Scholar]
- 331.Dinulovic I, Furrer R, Beer M, Ferry A. Muscle PGC-1α modulates satellite cell number and proliferation by remodeling the stem cell niche. Skelet. Muscle. 2016;6:39. doi: 10.1186/s13395-016-0111-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 332.Handschin C. The biology of PGC-1alpha and its therapeutic potential. Trends Pharmacol. Sci. 2009;30:322–329. doi: 10.1016/j.tips.2009.03.006. [DOI] [PubMed] [Google Scholar]
- 333.Sánchez-de-Diego C, et al. Glucose restriction promotes osteocyte specification by activating a PGC-1α-dependent transcriptional program. iScience. 2019;15:79–94. doi: 10.1016/j.isci.2019.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 334.Colaianni G, et al. Deletion of the transcription factor PGC-1alpha in mice negatively regulates bone mass. Calcif. Tissue Int. 2018;103:638–652. doi: 10.1007/s00223-018-0459-4. [DOI] [PubMed] [Google Scholar]
- 335.Wang J, et al. Hippocampal PGC-1α-mediated positive effects on parvalbumin interneurons are required for the antidepressant effects of running exercise. Transl. Psychiatry. 2021;11:222. doi: 10.1038/s41398-021-01339-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 336.Wang S, Dougherty EJ, Danner RL. PPARγ signaling and emerging opportunities for improved therapeutics. Pharmacol. Res. 2016;111:76–85. doi: 10.1016/j.phrs.2016.02.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 337.McMeekin LJ, et al. Estrogen-related receptor alpha (ERRα) is required for PGC-1α-dependent gene expression in the mouse brain. Neuroscience. 2021;479:70–90. doi: 10.1016/j.neuroscience.2021.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 338.Wang L, et al. mTORC1-PGC1 axis regulates mitochondrial remodeling during reprogramming. FEBS J. 2020;287:108–121. doi: 10.1111/febs.15024. [DOI] [PubMed] [Google Scholar]
- 339.Thirupathi A, de Souza CT. Multi-regulatory network of ROS: the interconnection of ROS, PGC-1 alpha, and AMPK-SIRT1 during exercise. J. Physiol. Biochem. 2017;73:487–494. doi: 10.1007/s13105-017-0576-y. [DOI] [PubMed] [Google Scholar]
- 340.Silva FCD, et al. Effects of physical exercise on the expression of microRNAs: a systematic review. J. Strength Cond. Res. 2020;34:270–280. doi: 10.1519/JSC.0000000000003103. [DOI] [PubMed] [Google Scholar]
- 341.Russell AP, et al. Regulation of miRNAs in human skeletal muscle following acute endurance exercise and short-term endurance training. J. Physiol. 2013;591:4637–4653. doi: 10.1113/jphysiol.2013.255695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 342.Allen DL, et al. Effects of spaceflight on murine skeletal muscle gene expression. J. Appl. Physiol. 2009;106:582–595. doi: 10.1152/japplphysiol.90780.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 343.Mytidou C, et al. Age-related exosomal and endogenous expression patterns of miR-1, miR-133a, miR-133b, and miR-206 in skeletal muscles. Front. Physiol. 2021;12:708278. doi: 10.3389/fphys.2021.708278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 344.Chen J, et al. The role of microRNA-1 and microRNA-133 in skeletal muscle proliferation and differentiation. Nat. Genet. 2006;38:228–233. doi: 10.1038/ng1725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 345.Elia L, et al. Reciprocal regulation of microRNA-1 and insulin-like growth factor-1 signal transduction cascade in cardiac and skeletal muscle in physiological and pathological conditions. Circulation. 2009;120:2377–2385. doi: 10.1161/CIRCULATIONAHA.109.879429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 346.Matheny RW, et al. RNA transcript expression of IGF-I/PI3K pathway components in regenerating skeletal muscle is sensitive to initial injury intensity. Growth Horm. IGF Res. 2017;32:14–21. doi: 10.1016/j.ghir.2016.09.002. [DOI] [PubMed] [Google Scholar]
- 347.Lou J, et al. Exercise promotes angiogenesis by enhancing endothelial cell fatty acid utilization via liver-derived extracellular vesicle miR-122-5p. J. Sport Health Sci. 2022;11:495–508. doi: 10.1016/j.jshs.2021.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 348.Yang H, et al. Treadmill exercise influences the microRNA profiles in the bone tissues of mice. Exp. Ther. Med. 2021;22:1035. doi: 10.3892/etm.2021.10467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.Zeng H, et al. MicroRNA miR-23a cluster promotes osteocyte differentiation by regulating TGF-β signalling in osteoblasts. Nat. Commun. 2017;8:15000. doi: 10.1038/ncomms15000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 350.Groven RVM, van Koll J, Poeze M, Blokhuis TJ, van Griensven M. miRNAs related to different processes of fracture healing: an integrative overview. Front. Surg. 2021;8:786564. doi: 10.3389/fsurg.2021.786564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 351.Pelozin BRA, Soci UPR, Gomes JLP, Oliveira EM, Fernandes T. mTOR signaling-related microRNAs as cardiac hypertrophy modulators in high-volume endurance training. J. Appl. Physiol. 2022;132:126–139. doi: 10.1152/japplphysiol.00881.2020. [DOI] [PubMed] [Google Scholar]
- 352.Wu X, et al. ADAR2 increases in exercised heart and protects against myocardial infarction and doxorubicin-induced cardiotoxicity. Mol. Ther. 2022;30:400–414. doi: 10.1016/j.ymthe.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 353.Pons-Espinal M, et al. MiR-135a-5p is critical for exercise-induced adult neurogenesis. Stem Cell Rep. 2019;12:1298–1312. doi: 10.1016/j.stemcr.2019.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Liu G, Detloff MR, Miller KN, Santi L, Houle JD. Exercise modulates microRNAs that affect the PTEN/mTOR pathway in rats after spinal cord injury. Exp. Neurol. 2012;233:447–456. doi: 10.1016/j.expneurol.2011.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 355.Bonilauri B, Dallagiovanna B. Long non-coding RNAs are differentially expressed after different exercise training programs. Front. Physiol. 2020;11:567614. doi: 10.3389/fphys.2020.567614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 356.Li Y, Chen X, Sun H, Wang H. Long non-coding RNAs in the regulation of skeletal myogenesis and muscle diseases. Cancer Lett. 2018;417:58–64. doi: 10.1016/j.canlet.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 357.Wohlwend M, et al. The exercise-induced long noncoding RNA CYTOR promotes fast-twitch myogenesis in aging. Sci. Transl. Med. 2021;13:c7367. doi: 10.1126/scitranslmed.abc7367. [DOI] [PubMed] [Google Scholar]
- 358.Gao R, et al. Long noncoding RNA cardiac physiological hypertrophy-associated regulator induces cardiac physiological hypertrophy and promotes functional recovery after myocardial ischemia-reperfusion injury. Circulation. 2021;144:303–317. doi: 10.1161/CIRCULATIONAHA.120.050446. [DOI] [PubMed] [Google Scholar]
- 359.Li H, et al. lncExACT1 and DCHS2 regulate physiological and pathological cardiac growth. Circulation. 2022;145:1218–1233. doi: 10.1161/CIRCULATIONAHA.121.056850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.Statello L, Guo C, Chen L, Huarte M. Gene regulation by long non-coding RNAs and its biological functions. Nat. Rev. Mol. Cell Biol. 2021;22:96–118. doi: 10.1038/s41580-020-00315-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 361.Vincent EE, et al. Differential effects of AMPK agonists on cell growth and metabolism. Oncogene. 2015;34:3627–3639. doi: 10.1038/onc.2014.301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 362.Narkar VA, et al. AMPK and PPARδ agonists are exercise mimetics. Cell. 2008;134:405–415. doi: 10.1016/j.cell.2008.06.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 363.Ehrenborg E, Krook A. Regulation of skeletal muscle physiology and metabolism by peroxisome proliferator-activated receptor δ. Pharmacol. Rev. 2009;61:373–393. doi: 10.1124/pr.109.001560. [DOI] [PubMed] [Google Scholar]
- 364.Hardie DG. AMP-activated protein kinase: a cellular energy sensor with a key role in metabolic disorders and in cancer. Biochem. Soc. Trans. 2011;39:1–13. doi: 10.1042/BST0390001. [DOI] [PubMed] [Google Scholar]
- 365.Višnjić D, Lalić H, Dembitz V, Tomić B, Smoljo T. AICAr, a widely used AMPK activator with important AMPK-independent effects: a systematic review. Cells. 2021;10:1095. doi: 10.3390/cells10051095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 366.Chiang C, et al. Metformin-treated cancer cells modulate macrophage polarization through AMPK-NF-κB signaling. Oncotarget. 2017;8:20706–20718. doi: 10.18632/oncotarget.14982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 367.Mallik R, Chowdhury TA. Metformin in cancer. Diabetes Res. Clin. Pract. 2018;143:409–419. doi: 10.1016/j.diabres.2018.05.023. [DOI] [PubMed] [Google Scholar]
- 368.Ouchi N, Shibata R, Walsh K. AMP-activated protein kinase signaling stimulates VEGF expression and angiogenesis in skeletal muscle. Circ. Res. 2005;96:838–846. doi: 10.1161/01.RES.0000163633.10240.3b. [DOI] [PubMed] [Google Scholar]
- 369.Zibrova D, et al. GFAT1 phosphorylation by AMPK promotes VEGF-induced angiogenesis. Biochem. J. 2017;474:983–1001. doi: 10.1042/BCJ20160980. [DOI] [PubMed] [Google Scholar]
- 370.Kobilo T, Yuan C, van Praag H. Endurance factors improve hippocampal neurogenesis and spatial memory in mice. Learn. Mem. 2011;18:103–107. doi: 10.1101/lm.2001611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 371.Guerrieri D, van Praag H. Exercise-mimetic AICAR transiently benefits brain function. Oncotarget. 2015;6:18293–18313. doi: 10.18632/oncotarget.4715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Wrann CD, et al. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 2013;18:649–659. doi: 10.1016/j.cmet.2013.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 373.Giaccari A, Solini A, Frontoni S, Del Prato S. Metformin benefits: another example for alternative energy substrate mechanism? Diabetes Care. 2021;44:647–654. doi: 10.2337/dc20-1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 374.Liu Y, Tang G, Zhang Z, Wang Y, Yang G. Metformin promotes focal angiogenesis and neurogenesis in mice following middle cerebral artery occlusion. Neurosci. Lett. 2014;579:46–51. doi: 10.1016/j.neulet.2014.07.006. [DOI] [PubMed] [Google Scholar]
- 375.Zhu X, et al. Metformin improves cognition of aged mice by promoting cerebral angiogenesis and neurogenesis. Aging. 2020;12:17845–17862. doi: 10.18632/aging.103693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 376.DiTacchio KA, Heinemann SF, Dziewczapolski G. Metformin treatment alters memory function in a mouse model of Alzheimer’s disease. J. Alzheimers Dis. 2015;44:43–48. doi: 10.3233/JAD-141332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 377.Stunes AK, et al. Skeletal effects of plyometric exercise and metformin in ovariectomized rats. Bone. 2020;132:115193. doi: 10.1016/j.bone.2019.115193. [DOI] [PubMed] [Google Scholar]
- 378.Chandrashekar P, et al. Inactivation of PPARβ/δ adversely affects satellite cells and reduces postnatal myogenesis. Am. J. Physiol. Endocrinol. Metab. 2015;309:E122–E131. doi: 10.1152/ajpendo.00586.2014. [DOI] [PubMed] [Google Scholar]
- 379.Angione AR, Jiang C, Pan D, Wang Y, Kuang S. PPARδ regulates satellite cell proliferation and skeletal muscle regeneration. Skelet. Muscle. 2011;1:33. doi: 10.1186/2044-5040-1-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 380.Nahlé Z, et al. CD36-dependent regulation of muscle FoxO1 and PDK4 in the PPARδ/β-mediated adaptation to metabolic stress. J. Biol. Chem. 2008;283:14317–14326. doi: 10.1074/jbc.M706478200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 381.Phua WWT, et al. PPARβ/δ agonism upregulates Forkhead Box A2 to reduce inflammation in C2C12 myoblasts and in skeletal muscle. Int. J. Mol. Sci. 2020;21:1747. doi: 10.3390/ijms21051747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 382.Gaudel C, Schwartz C, Giordano C, Abumrad NA, Grimaldi PA. Pharmacological activation of PPARβ promotes rapid and calcineurin-dependent fiber remodeling and angiogenesis in mouse skeletal muscle. Am. J. Physiol. Endocrinol. Metab. 2008;295:E297–E304. doi: 10.1152/ajpendo.00581.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 383.Wagner N, et al. Peroxisome proliferator-activated receptor β stimulation induces rapid cardiac growth and angiogenesis via direct activation of calcineurin. Cardiovasc. Res. 2009;83:61–71. doi: 10.1093/cvr/cvp106. [DOI] [PubMed] [Google Scholar]
- 384.Strosznajder AK, Wójtowicz S, Jeżyna MJ, Sun GY, Strosznajder JB. Recent insights on the role of PPAR-β/δ in neuroinflammation and neurodegeneration, and its potential target for therapy. Neuromol. Med. 2021;23:86–98. doi: 10.1007/s12017-020-08629-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 385.Chamberlain S, Gabriel H, Strittmatter W, Didsbury J. An exploratory phase IIa study of the PPAR delta/gamma agonist T3D-959 assessing metabolic and cognitive function in subjects with mild to moderate Alzheimer’s disease. J. Alzheimers Dis. 2020;73:1085–1103. doi: 10.3233/JAD-190864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 386.Xu X, et al. Exercise training combined with angiotensin II receptor blockade limits post-infarct ventricular remodelling in rats. Cardiovasc. Res. 2008;78:523–532. doi: 10.1093/cvr/cvn028. [DOI] [PubMed] [Google Scholar]
- 387.Tawfik VL, et al. Angiotensin receptor blockade mimics the effect of exercise on recovery after orthopaedic trauma by decreasing pain and improving muscle regeneration. J. Physiol. 2020;598:317–329. doi: 10.1113/JP278991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 388.Bostrom P, et al. A PGC1-alpha-dependent myokine that drives brown-fat-like development of white fat and thermogenesis. Nature. 2012;481:463–468. doi: 10.1038/nature10777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 389.Ma Y, et al. Irisin promotes proliferation but inhibits differentiation in osteoclast precursor cells. FASEB J. 2018;32:5813–5823. doi: 10.1096/fj.201700983RR. [DOI] [PubMed] [Google Scholar]
- 390.Qiao X, et al. Irisin promotes osteoblast proliferation and differentiation via activating the MAP kinase signaling pathways. Sci. Rep. 2016;6:18732. doi: 10.1038/srep18732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 391.Chen Z, et al. Recombinant irisin prevents the reduction of osteoblast differentiation induced by stimulated microgravity through increasing β-Catenin expression. Int. J. Mol. Sci. 2020;21:1259. doi: 10.3390/ijms21041259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 392.Kim H, et al. Irisin mediates effects on bone and fat via αV integrin receptors. Cell. 2018;175:1756–1768. doi: 10.1016/j.cell.2018.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 393.Jodeiri Farshbaf M, Alviña K. Multiple roles in neuroprotection for the exercise derived myokine irisin. Front. Aging Neurosci. 2021;13:649929. doi: 10.3389/fnagi.2021.649929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 394.Lourenco MV, et al. Exercise-linked FNDC5/irisin rescues synaptic plasticity and memory defects in Alzheimer’s models. Nat. Med. 2019;25:165–175. doi: 10.1038/s41591-018-0275-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 395.Waseem R, et al. FNDC5/irisin: physiology and pathophysiology. Molecules. 2022;27:1118. doi: 10.3390/molecules27031118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 396.Huang S, Yang S, Lo J, Wu S, Tai M. Irisin gene delivery ameliorates burn-induced sensory and motor neuropathy. Int. J. Mol. Sci. 2020;21:7798. doi: 10.3390/ijms21207798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 397.Garekani ET, Mohebbi H, Kraemer RR, Fathi R. Exercise training intensity/volume affects plasma and tissue adiponectin concentrations in the male rat. Peptides. 2011;32:1008–1012. doi: 10.1016/j.peptides.2011.01.027. [DOI] [PubMed] [Google Scholar]
- 398.Zeng Q, et al. Effects of exercise on adiponectin and adiponectin receptor levels in rats. Life Sci. 2007;80:454–459. doi: 10.1016/j.lfs.2006.09.031. [DOI] [PubMed] [Google Scholar]
- 399.Inoue A, et al. Exercise restores muscle stem cell mobilization, regenerative capacity and muscle metabolic alterations via adiponectin/AdipoR1 activation in SAMP10 mice. J. Cachexia Sarcopenia Muscle. 2017;8:370–385. doi: 10.1002/jcsm.12166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 400.Wang P, et al. Potential involvement of adiponectin signaling in regulating physical exercise-elicited hippocampal neurogenesis and dendritic morphology in stressed mice. Front. Cell. Neurosci. 2020;14:189. doi: 10.3389/fncel.2020.00189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 401.You J, et al. Role of adiponectin-Notch pathway in cognitive dysfunction associated with depression and in the therapeutic effect of physical exercise. Aging Cell. 2021;20:e13387. doi: 10.1111/acel.13387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 402.Lee TH, et al. Chronic AdipoRon treatment mimics the effects of physical exercise on restoring hippocampal neuroplasticity in diabetic mice. Mol. Neurobiol. 2021;58:4666–4681. doi: 10.1007/s12035-021-02441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 403.Li A, Yau SY, Machado S, Yuan TF, So KF. Adult neurogenic and antidepressant effects of adiponectin: a potential replacement for exercise? CNS Neurol. Disord. Drug Targets. 2015;14:1129–1144. doi: 10.2174/1871527315666151111125533. [DOI] [PubMed] [Google Scholar]
- 404.Pedersen BK, Febbraio MA. Muscles, exercise and obesity: skeletal muscle as a secretory organ. Nat. Rev. Endocrinol. 2012;8:457–465. doi: 10.1038/nrendo.2012.49. [DOI] [PubMed] [Google Scholar]
- 405.Peake JM, Della GP, Suzuki K, Nieman DC. Cytokine expression and secretion by skeletal muscle cells: regulatory mechanisms and exercise effects. Exerc. Immunol. Rev. 2015;21:8–25. [PubMed] [Google Scholar]
- 406.Reihmane D, Dela F. Interleukin-6: possible biological roles during exercise. Eur. J. Sport Sci. 2014;14:242–250. doi: 10.1080/17461391.2013.776640. [DOI] [PubMed] [Google Scholar]
- 407.Storer MA, et al. Interleukin-6 regulates adult neural stem cell numbers during normal and abnormal post-natal development. Stem Cell Rep. 2018;10:1464–1480. doi: 10.1016/j.stemcr.2018.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 408.Cox AA, et al. Low-dose pulsatile interleukin-6 as a treatment option for diabetic peripheral neuropathy. Front. Endocrinol. 2017;8:89. doi: 10.3389/fendo.2017.00089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 409.Schmitt C, Kuhn B, Zhang X, Kivitz AJ, Grange S. Disease-drug-drug interaction involving tocilizumab and simvastatin in patients with rheumatoid arthritis. Clin. Pharmacol. Ther. 2011;89:735–740. doi: 10.1038/clpt.2011.35. [DOI] [PubMed] [Google Scholar]
- 410.Wedell-Neergaard A, et al. Exercise-induced changes in visceral adipose tissue mass are regulated by IL-6 signaling: a randomized controlled trial. Cell Metab. 2019;29:844–855. doi: 10.1016/j.cmet.2018.12.007. [DOI] [PubMed] [Google Scholar]
- 411.Trinh B, et al. Blocking endogenous IL-6 impairs mobilization of free fatty acids during rest and exercise in lean and obese men. Cell Rep. Med. 2021;2:100396. doi: 10.1016/j.xcrm.2021.100396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 412.Furuichi Y, Manabe Y, Takagi M, Aoki M, Fujii NL. Evidence for acute contraction-induced myokine secretion by C2C12 myotubes. PLoS ONE. 2018;13:e206146. doi: 10.1371/journal.pone.0206146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 413.O. Leary MF, Wallace GR, Bennett AJ, Tsintzas K, Jones SW. IL-15 promotes human myogenesis and mitigates the detrimental effects of TNFα on myotube development. Sci. Rep. 2017;7:12997. doi: 10.1038/s41598-017-13479-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 414.Yoshida S, et al. Interleukin‐15 receptor subunit alpha regulates interleukin‐15 localization and protein expression in skeletal muscle cells. Exp. Physiol. 2022;107:222–232. doi: 10.1113/EP090205. [DOI] [PubMed] [Google Scholar]
- 415.Wong W, Crane ED, Kuo Y, Kim A, Crane JD. The exercise cytokine interleukin-15 rescues slow wound healing in aged mice. J. Biol. Chem. 2019;294:20024–20038. doi: 10.1074/jbc.RA119.010740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 416.Partridge L, Deelen J, Slagboom PE. Facing up to the global challenges of ageing. Nature. 2018;561:45–56. doi: 10.1038/s41586-018-0457-8. [DOI] [PubMed] [Google Scholar]
- 417.Muñoz-Espín D, Serrano M. Cellular senescence: from physiology to pathology. Nat. Rev. Mol. Cell Biol. 2014;15:482–496. doi: 10.1038/nrm3823. [DOI] [PubMed] [Google Scholar]
- 418.Calcinotto A, et al. Cellular senescence: aging, cancer, and injury. Physiol. Rev. 2019;99:1047–1078. doi: 10.1152/physrev.00020.2018. [DOI] [PubMed] [Google Scholar]
- 419.De la Rosa A, et al. Physical exercise in the prevention and treatment of Alzheimer’s disease. J. Sport Health Sci. 2020;9:394–404. doi: 10.1016/j.jshs.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 420.Liang Y, et al. All roads lead to Rome-a review of the potential mechanisms by which exerkines exhibit neuroprotective effects in Alzheimer’s disease. Neural Regen. Res. 2022;17:1210–1227. doi: 10.4103/1673-5374.325012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 421.Choi SH, et al. Combined adult neurogenesis and BDNF mimic exercise effects on cognition in an Alzheimer’s mouse model. Science. 2018;361:eaan8821. doi: 10.1126/science.aan8821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 422.Sujkowski A, Hong L, Wessells RJ, Todi SV. The protective role of exercise against age-related neurodegeneration. Ageing Res. Rev. 2022;74:101543. doi: 10.1016/j.arr.2021.101543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 423.Horowitz AM, et al. Blood factors transfer beneficial effects of exercise on neurogenesis and cognition to the aged brain. Science. 2020;369:167–173. doi: 10.1126/science.aaw2622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 424.Watson SL, et al. High-intensity resistance and impact training improves bone mineral density and physical function in postmenopausal women with osteopenia and osteoporosis: the LIFTMOR randomized controlled trial. J. Bone Miner. Res. 2018;33:211–220. doi: 10.1002/jbmr.3284. [DOI] [PubMed] [Google Scholar]
- 425.Anupama DS, Norohna JA, Acharya KK, Ravishankar, George A. Effect of exercise on bone mineral density and quality of life among postmenopausal women with osteoporosis without fracture: a systematic review. Int. J. Orthop. Trauma Nurs. 2020;39:100796. doi: 10.1016/j.ijotn.2020.100796. [DOI] [PubMed] [Google Scholar]
- 426.Martyn-St James M, Carroll S. Meta-analysis of walking for preservation of bone mineral density in postmenopausal women. Bone. 2008;43:521–531. doi: 10.1016/j.bone.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 427.Ma D, Wu L, He Z. Effects of walking on the preservation of bone mineral density in perimenopausal and postmenopausal women: a systematic review and meta-analysis. Menopause. 2013;20:1216–1226. doi: 10.1097/GME.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 428.Cruz-Jentoft AJ, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 429.Capelli C, Rittveger J, Bruseghini P, Calabria E, Tam E. Maximal aerobic power and anaerobic capacity in cycling across the age spectrum in male master athletes. Eur. J. Appl. Physiol. 2016;116:1395–1410. doi: 10.1007/s00421-016-3396-9. [DOI] [PubMed] [Google Scholar]
- 430.Landi F, Marzetti E, Martone AM, Bernabei R, Onder G. Exercise as a remedy for sarcopenia. Curr. Opin. Clin. Nutr. 2013;17:25–31. doi: 10.1097/MCO.0000000000000018. [DOI] [PubMed] [Google Scholar]
- 431.Peterson MD, Sen A, Gordon PM. Influence of resistance exercise on lean body mass in aging adults: a meta-analysis. Med. Sci. Sports Exerc. 2011;43:249–258. doi: 10.1249/MSS.0b013e3181eb6265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 432.Giallauria F, Cittadini A, Smart NA, Vigorito C. Resistance training and sarcopenia. Monaldi Arch. Chest Dis. 2016;84:51–53. doi: 10.4081/monaldi.2015.738. [DOI] [PubMed] [Google Scholar]
- 433.Papa EV, Dong X, Hassan M. Resistance training for activity limitations in older adults with skeletal muscle function deficits: a systematic review. Clin. Interv. Aging. 2017;12:955–961. doi: 10.2147/CIA.S104674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 434.Joanisse S, et al. Exercise conditioning in old mice improves skeletal muscle regeneration. FASEB J. 2016;30:3256–3268. doi: 10.1096/fj.201600143RR. [DOI] [PubMed] [Google Scholar]
- 435.Leenders M, et al. Elderly men and women benefit equally from prolonged resistance-type exercise training. J. Gerontol. A Biol. Sci. Med. Sci. 2013;68:769–779. doi: 10.1093/gerona/gls241. [DOI] [PubMed] [Google Scholar]
- 436.Cisterna B, et al. Adapted physical exercise enhances activation and differentiation potential of satellite cells in the skeletal muscle of old mice. J. Anat. 2016;228:771–783. doi: 10.1111/joa.12429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 437.Zacharewicz E, et al. Identification of MicroRNAs linked to regulators of muscle protein synthesis and regeneration in young and old skeletal muscle. PLoS ONE. 2014;9:e114009. doi: 10.1371/journal.pone.0114009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 438.Arnold MJ, Moody AL. Common running injuries: evaluation and management. Am. Fam. Physician. 2018;97:510–516. [PubMed] [Google Scholar]
- 439.Fagher K, Lexell J. Sports-related injuries in athletes with disabilities. Scand. J. Med. Sci. Sports. 2014;24:e320–e331. doi: 10.1111/sms.12175. [DOI] [PubMed] [Google Scholar]
- 440.Murphy C, O. Connell JE, Kearns G, Stassen L. Sports-related maxillofacial injuries. J. Craniofac. Surg. 2015;26:2120–2123. doi: 10.1097/SCS.0000000000002109. [DOI] [PubMed] [Google Scholar]
- 441.Pierpoint LA, Collins C. Epidemiology of sport-related concussion. Clin. Sports Med. 2021;40:1–18. doi: 10.1016/j.csm.2020.08.013. [DOI] [PubMed] [Google Scholar]
- 442.Elliott AD, Linz D, Verdicchio CV, Sanders P. Exercise and atrial fibrillation: prevention or causation? Heart Lung Circ. 2018;27:1078–1085. doi: 10.1016/j.hlc.2018.04.296. [DOI] [PubMed] [Google Scholar]
- 443.O’Keefe EL, Torres-Acosta N, O’Keefe JH, Lavie CJ. Training for longevity: the reverse J-Curve for exercise. Mo. Med. 2020;117:355–361. [PMC free article] [PubMed] [Google Scholar]
- 444.Dockerill C, Lapidaire W, Lewandowski AJ, Leeson P. Cardiac remodelling and exercise: what happens with ultra-endurance exercise? Eur. J. Prev. Cardiol. 2020;27:1464–1466. doi: 10.1177/2047487320904511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 445.Geesmann B, Gibbs JC, Mester J, Koehler K. Association between energy balance and metabolic hormone suppression during ultraendurance exercise. Int. J. Sports Physiol. Perform. 2017;12:984–989. doi: 10.1123/ijspp.2016-0061. [DOI] [PubMed] [Google Scholar]
- 446.Turner JE, Bennett SJ, Bosch JA, Griffiths HR, Aldred S. Ultra-endurance exercise: unanswered questions in redox biology and immunology. Biochem. Soc. Trans. 2014;42:989–995. doi: 10.1042/BST20140120. [DOI] [PubMed] [Google Scholar]
- 447.Seo M, et al. Effects of 16 weeks of resistance training on muscle quality and muscle growth factors in older adult women with sarcopenia: a randomized controlled trial. Int. J. Environ. Res. Public Health. 2021;18:6762. doi: 10.3390/ijerph18136762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 448.Kemmler W, et al. Effects of high‐intensity resistance training on osteopenia and sarcopenia parameters in older men with osteosarcopenia—one‐year results of the randomized controlled Franconian Osteopenia and Sarcopenia Trial (FrOST) J. Bone Miner. Res. 2020;35:1634–1644. doi: 10.1002/jbmr.4027. [DOI] [PubMed] [Google Scholar]
- 449.Aamann L, et al. Resistance training increases muscle strength and muscle size in patients with liver cirrhosis. Clin. Gastroenterol. Hepatol. 2020;18:1179–1187. doi: 10.1016/j.cgh.2019.07.058. [DOI] [PubMed] [Google Scholar]
- 450.Lichtenberg T, von Stengel S, Sieber C, Kemmler W. The favorable effects of a high-intensity resistance training on sarcopenia in older community-dwelling men with osteosarcopenia: the randomized controlled FrOST study. Clin. Interv. Aging. 2019;14:2173–2186. doi: 10.2147/CIA.S225618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 451.FilipoviC TN, et al. A 12-week exercise program improves functional status in postmenopausal osteoporotic women: randomized controlled study. Eur. J. Phys. Rehabil. Med. 2021;57:120–130. doi: 10.23736/S1973-9087.20.06149-3. [DOI] [PubMed] [Google Scholar]
- 452.Harding AT, et al. Exploring thoracic kyphosis and incident fracture from vertebral morphology with high-intensity exercise in middle-aged and older men with osteopenia and osteoporosis: a secondary analysis of the LIFTMOR-M trial. Osteoporos. Int. 2021;32:451–465. doi: 10.1007/s00198-020-05583-x. [DOI] [PubMed] [Google Scholar]
- 453.Harding AT, et al. Effects of supervised high-intensity resistance and impact training or machine-based isometric training on regional bone geometry and strength in middle-aged and older men with low bone mass: the LIFTMOR-M semi-randomised controlled trial. Bone. 2020;136:115362. doi: 10.1016/j.bone.2020.115362. [DOI] [PubMed] [Google Scholar]
- 454.Otero M, Esain I, Gonzalez-Suarez AM, Gil SM. The effectiveness of a basic exercise intervention to improve strength and balance in women with osteoporosis. Clin. Interv. Aging. 2017;12:505–513. doi: 10.2147/CIA.S127233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 455.Pandey A, et al. Frailty status modifies the efficacy of exercise training among patients with chronic heart failure and reduced ejection fraction: an analysis from the HF-ACTION trial. Circulation. 2022;146:80–90. doi: 10.1161/CIRCULATIONAHA.122.059983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 456.Hieda M, et al. One-year committed exercise training reverses abnormal left ventricular myocardial stiffness in patients with stage B heart failure with preserved ejection fraction. Circulation. 2021;144:934–946. doi: 10.1161/CIRCULATIONAHA.121.054117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 457.Liu-Ambrose T, et al. Aerobic exercise and vascular cognitive impairment. Neurology. 2016;87:2082–2090. doi: 10.1212/WNL.0000000000003332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 458.Bo W, et al. Effects of combined intervention of physical exercise and cognitive training on cognitive function in stroke survivors with vascular cognitive impairment: a randomized controlled trial. Clin. Rehabil. 2019;33:54–63. doi: 10.1177/0269215518791007. [DOI] [PubMed] [Google Scholar]
- 459.Nave AH, et al. Physical Fitness Training in Patients with Subacute Stroke (PHYS-STROKE): multicentre, randomised controlled, endpoint blinded trial. BMJ. 2019;366:l5101. doi: 10.1136/bmj.l5101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 460.Sobol NA, et al. Effect of aerobic exercise on physical performance in patients with Alzheimer’s disease. Alzheimers Dement. 2016;12:1207–1215. doi: 10.1016/j.jalz.2016.05.004. [DOI] [PubMed] [Google Scholar]
- 461.Lautenschlager NT, et al. Effect of physical activity on cognitive function in older adults at risk for Alzheimer disease. JAMA. 2008;300:1027–1037. doi: 10.1001/jama.300.9.1027. [DOI] [PubMed] [Google Scholar]
- 462.Lamb SE, et al. Dementia And Physical Activity (DAPA) trial of moderate to high intensity exercise training for people with dementia: randomised controlled trial. BMJ. 2018;361:k1675. doi: 10.1136/bmj.k1675. [DOI] [PMC free article] [PubMed] [Google Scholar]