Abstract
A diaphragmatic hernia is a protrusion of the abdominal contents into the negative pressure thoracic cavity through a congenital or acquired diaphragmatic defect. Generally, acquired diaphragmatic hernia is a rare, life-threatening condition that usually follows blunt/penetrating trauma or an iatrogenic cause, resulting in the diaphragmatic rupture, accompanied by the herniation of abdominal visceral organs. We report a 47-year-old male construction worker who sustained a fall from a height of about 30 feet height. He presented with hypoxia initially and, after a primary survey, was found to have a traumatic rupture of the diaphragm with herniation of the stomach and abdominal contents, causing signs of obstructive shock. After adequate resuscitation in the Emergency Department, he was rushed to operating room. There, he suffered two very short pulseless electrical activity cardiac arrests. Therefore, an emergency anterolateral thoracotomy was done, and it was extended into laparotomy to reduce the abdominal contents through the diaphragmatic tear of 12 cm, which restored the spontaneous circulation. He recovered eventually, despite chest infections and pulmonary atelectasis, and was discharged on the 28th day and remained in good condition during the outpatient visit. Tension gastrothorax or viscerothorax is rare, but an under-recognized cause of cardiac arrest in the trauma setting necessitates a vigilant evaluation and early suspicion to prevent a catastrophic outcome. This case report emphasizes the inclusion of tension viscero or abdominal thorax as one of the recognizable causes of a pulseless electrical activity cardiac arrest.
Keywords: Diaphragmatic hernia, tension abdominal thorax, pulseless electrical activity
Introduction
The diaphragm is the C-shaped thin musculo-tendinous arched anatomical structure that separates the negative pressure thorax or chest from the positive pressure abdominal cavity. The prime muscle for respiration is the diaphragm. In addition, the diaphragm aids the few non-respiratory physiological functions to clear the end waste substances from the body by raising the intra-abdominal pressure via emesis, micturition, and defecation. Also, the diaphragm muscle encompasses the lower esophageal sphincter anatomically and prevents gastroesophageal reflux to the thoracic cavity.1 Diaphragm rupture is a rare condition that may happen due to blunt or penetrating trauma and iatrogenic causes. Such injury may have a higher incidence of acquired diaphragmatic hernia (DH), leading to incarceration and even strangulation of herniated bowel, with a fatal outcome. The severity of acquired DH varies according to the mechanism of trauma. However, diaphragmatic rupture from thoracoabdominal trauma is 0.8%–3.6%, with the incidence of herniation following diaphragmatic rupture being relatively low.2,3 Tension abdominal thorax (TAT), following a fall from height occurring secondarily due to a traumatic DH in adults, is a rare phenomenon, limited to case reports in the literature. The first reported traumatic tension gastrothorax was in 1984 by Ordog et al.4 The incidence of post-traumatic blunt acquired DH is 0.16%–5%, and the occurrence of acquired DH in patients undergoing surgery is 3%–8%.
Nevertheless, the mortality rate after acute DH varies from 5.5% to 51%.5,6 A recent study stated that 7%–66% of cases of diaphragmatic ruptures are unnoticed, the mortality after a diagnosis of diaphragmatic rupture is 17%–21%, and maximum mortality is due to cardio-respiratory compromise, which is a life-threatening complication of diaphragmatic rupture due to the visceral herniation into the diaphragm.7,8 Furthermore, penetrating abdominal injuries usually need emergency surgical intervention, and they have higher incidences of diaphragm rupture (10–19%); as such, the diagnosis of DH is frequently confirmed intraoperatively. However, the diagnosis may also be missed or delayed in patients with diaphragmatic rupture due to blunt trauma, leading to poor outcomes.9 Herein, we report the successful management of tension gastrothorax, which led to a progressive mediastinal shift that led to lung collapse, respiratory failure, obstructive shock, and cardiac arrest and much like the exact pathophysiological mechanism of tension pneumothorax. The primary purpose of this report is to emphasize that TAT can be a recognizable cause in a victim of a fall from a height. Furthermore, it may end in cardiac arrest with pulseless electrical activity (PEA) associated with mimics tension pneumothorax. Also, TAT should be added in the ACLS (Advanced Cardiac Life Support) and ATLS (Advanced Trauma Life Support) manuals and algorithm(s) as one of the causes of the PEA arrest.
Case history
A 47-year-old male, a known hypertensive on regular medications, arrived at our hospital as a victim of a fall from a height on the 21 July 2021 at about 7 pm. The patient was alert, conscious, unable to lie flat, and looked anxious, in the Emergency Department (ED)—resuscitation room. His chief complaints were chest tightness, difficulty breathing, epigastric pain, and left lower limb pain. His pulse was 125 beats/min, blood pressure 100/70 mm Hg, respiration rate 25 breaths/min, and temperature 37.5°C; oxygen saturation was 85% on room air. Several abrasions on the face and thorax were found on physical examination, including long bone fractures in the left lower limbs, decreased chest movement with right tracheal deviation, and mild epigastric tenderness. On auscultation, diminished breath sounds in the left hemithorax, heard heart sounds in the right sternal border of the chest, bowel sounds were audible in the left hemithorax, and no visible engorged veins. The abdomen was tender. The peripheral pulses were all present. The chest X-ray (CXR) revealed a right tracheal deviation, left lung collapse, right mediastinum shift, and significant fluid level beneath a raised left hemidiaphragm, authenticating a left hemidiaphragmatic rupture with gastric herniation (Figure 1). The CXR findings gave a picture of a tension viscerothorax. His initial laboratory results were within normal limits. FAST (Focused Assessment of Sonography in Trauma) patients were typical. Multiple trials of nasogastric tube insertion were initiated and failed.
Figure 1.

Initial chest X-ray showing a shift of trachea, mediastinum, ruptured diaphragm, left lower lobe collapse, herniated stomach, and bowel.
Therefore, the distress was not relieved, and oxygen flow increased to 12 lpm through the non-rebreathing facemask. Nevertheless, oxygen saturation remained at 86% only, with unstable vital signs. After further resuscitation, the team decided to do a computed tomography (CT) room, which revealed collapse and compression of the left lung, right mediastinal shift, right pneumomediastinum, and herniation of the stomach in left hemithorax through a diaphragmatic defect (Figure 2). Hence, written informed consent was obtained from the patient, and transferred immediately to the operating theater; while moving the patient to the operating table, the patient developed cardiac arrest twice, first for 40 s and then for one cycle, which was about 2 min, and was resuscitated successfully. During this emergency crisis, our thoracic surgical team decided to go for an emergency left anterolateral thoracotomy through the seventh intercostal space, which showed the gastric volvulus, some intestinal loops, and the part of the transverse colon herniated through the diaphragm defect. Hence, thoracotomy was extended into laparotomy. Thereby, abdominal contents and bowel loops were pulled out from the thoracic cavity into the abdomen and restored the diaphragmatic tear of 12 cm with interrupted polypropylene sutures supported with polypropylene mesh. Finally, one intercostal drainage tube was placed into the left thoracic cavity. The patient had been covered with broad-spectrum antibiotics. On the first post-operative day, we weaned the patient from the inotropic substances; the patient was extubated. The patient was transferred from the intensive care unit to the surgical ward on the second post-operative day. The post-operative recovery was eventful with recurrent chest infections, left lung atelectasis, and collapse; his hemoglobin dropped to 8 g/dL due to the fractured left femur. The patient was eventually discharged, as he managed his normal diet, mobilized relatively independently on the 28th post-operative day, and remained in good condition during an outpatient visit after 1 week.
Figure 2.
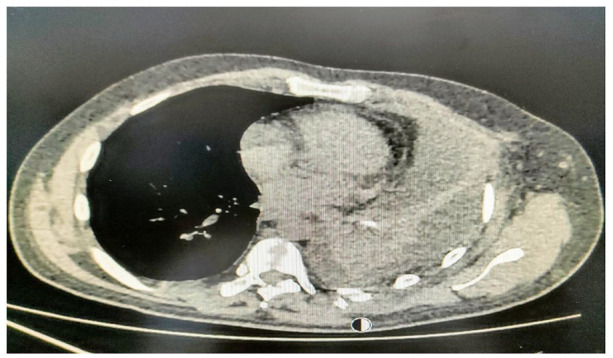
Computed tomography showing collapse and compression of the left lung, right mediastinal shift, right pneumomediastinum, and herniation of the stomach in left hemithorax through the diaphragmatic defect.
Discussion
Tension gastrothorax following blunt trauma, particularly from a fall from a height, is a rare, uncommon entity and is a life-threatening event. It can present acutely, as in our case, or present with the transient or eventual herniation or obstruction of the bowel or vital organs, from hours to days to many years (>1 h to 9 days to 10–40 and 50 years).10 Numerous studies highlighted that tension gastrothorax could be a complication of congenital DH or trauma, or it can be a complication of specific surgical procedures.11 Diaphragmatic injuries, about 8%, following blunt abdominal trauma are silent, delayed, and missed, and 12%–66% of diaphragmatic injuries are missed at the initial screening.12 Similar to our case, few studies stated that 50%–80% of diaphragmatic injuries frequently occur on the left hemithorax, possibly due to the anatomical position of the liver that cushions the diaphragm.13 The clinical presentation varies between individuals, so a vigilant orderly diagnostic approach is highly recommended.14 The literature review on diaphragmatic injury is mostly limited to case reports and case series, highlighting that a visceral organ can herniate through the diaphragmatic defect with gastrothorax resulting with or without tension component, and it is the major complication of blunt trauma involving diaphragm injury with an acute or delayed presentation.15 A fall from a height will create excessive tension in the visceral attachments and result in tears. At the same time, there is a possibility that visceral organs may herniate into the diaphragmatic defect, and our patient is not associated with any other life-threatening injuries, such as spleen, liver, renal, aortic, and cardiac injuries, which are the most common. However, the stomach, right hepatic lobe, transverse colon, spleen, small bowel, and omentum were herniated into the thorax through the diaphragmatic deficit. Similar to the statement of Shin Ahn et al., herniation of the visceral organs of our patient resulted in tension gastrothorax, mimicking pneumothorax.16 However, it is difficult to differentiate between gastrothorax and tension pneumothorax due to their clinical and debatable radiological similarities, although chest radiography has its known limitations. Both tension gastrothorax and tension pneumothorax can present simultaneously. In our case, a CXR was helpful in the early assessment; plain chest radiography is the first diagnostic tool, and its diagnostic success is about 75%.17 However, computed tomography and contrast-enhanced multi-planar computed tomography (MPCT) have become the standard of care; thus, knowledge of the CT signs plays a vital role in recognizing the injury pattern. However, transferring a potentially unstable patient into the CT suite is not good unless the resuscitation suite has a Hybrid ED setup. Immediate thoracocentesis and then thoracostomy are the definite treatment for tension pneumothorax. Whereas in tension gastrothorax, it will be harmful and may increase morbidity and lethal perforation of the viscus.18 Hence, we are very keen that any presumed pneumothorax can lead to a misdiagnosis, and subsequent chest tube insertion can lead to fatal gastric or colonic perforation consequences. The insertion of a nasogastric tube in tension gastrothorax releases the trapped air in the patient’s stomach for hemodynamic stabilization.19 In our case, nasogastric tube insertion was not accessible due to anatomical structural changes, which led the stomach to kink at the diaphragm level. The multiple nasogastric insertion attempts provoked hyperventilation and air swallowing, worsening gastric distension and hemodynamic instability. Furthermore, the diaphragm is a constantly moving organ; therefore, any ruptures or defects seldom heal without surgical repair.20 Therefore, the standard treatment of choice in tension viscerothorax is surgical repair. Most authors recommend that immediate surgical intervention is the best choice for reducing viscera in the abdominal cavity. In our case, the tension viscerothorax event occurred less than an hour after the fall from height, and multiple attempts of gastric decompression failure worsened the patient’s condition. Hence, the patient was transferred to the operating theater/room (OR) and on the operating table; the patient deteriorated into cardiac arrest but was successfully resuscitated and stabilized after nasogastric tube decompression. Based on the associated injuries and trauma-related syndromes, our choice of surgical approach is resuscitative thoracotomy and extended into laparotomy,21 and it is easier to reduce the gastric, bowel, and visceral contents in the abdominal cavity and prevent deterioration resulting from cardiac arrest.22 Although the obstructive shock, caused by tension pneumothorax and tension gastrothorax, is the same, the diagnosis and management are different. A bedside CXR in the resuscitation room will aid in diagnosing tension gastrothorax. In contrast, tension pneumothorax must be diagnosed clinically or with point-of-care ultrasound (POCUS) and treated swiftly before the X-ray.23 A simple nasogastric tube decompression or orogastric tube and immediate operative repair will save the patient. As per the ATLS adage, do no more harm. Hence, we do not recommend needle thoracentesis or chest tube to decompress the herniated stomach, bowel, or other viscera. If the expertise and facility are available, decompression endoscopy in the resuscitation room or OR is more favorable.
Conclusion
Tension gastrothorax or viscerothorax is a rare but under-recognized cause of cardiac arrest in the setting of trauma which necessitates a vigilant observation and early suspicion to prevent a catastrophic outcome.
Acknowledgments
The authors thank surgeons Dr Ayman and Dr Abdullah and critical care staffs of Aseer Central Hospital, Saudi Arabia.
Footnotes
Author contributions: Dr S.J.P. originated and conceived the idea, managed the patient initially, wrote discussion, and revised the draft thoroughly, before the submission. Dr S.P. organized the literature review and compiled the references comprehensively, and revised the draft thoroughly, before the submission. A.A.B. originated and conceived the idea, managed the patient in critical care, and wrote the discussion and revised the draft thoroughly, before the submission. M.J.E.O. communicated with the surgical team and medical records. Mr N.M.A. organized the literature review and compiled the references comprehensively and revised the draft thoroughly, before the submission. Mr N.S. organized the literature review and compiled the references comprehensively and revised the draft thoroughly, before the submission. Dr O.P. conceived the idea,, wrote introduction, case report, and discussion, and revised the draft thoroughly, before the submission.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Our institution does not require ethical approval for reporting individual cases or case series. However, we got the permission to write this rare case report for possible publication.
Informed consent: Written informed consent was obtained from the patient(s) for their anonymized information to be published in this article.
ORCID iDs: Ali Al Bshabshe  https://orcid.org/0000-0003-0974-7226
https://orcid.org/0000-0003-0974-7226
Omprakash Palanivel  https://orcid.org/0000-0002-8718-4302
https://orcid.org/0000-0002-8718-4302
References
- 1. Rosen RD. Physiology, lower esophageal sphincter, https://www.ncbi.nlm.nih.gov/books/NBK557452/ (5 April 2022, accessed May–October 2022). [PubMed]
- 2. Pancholi CK, Hombalkar NN, Dalvi SB, et al. Left-sided hydro-pneumothorax in a operated case of left diaphragmatic hernia repair: a diagnostic dilemma. J Clin Diagn Res 2015; 9(4): PD03–PD04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kozak O, Mentes O, Harlak A, et al. Late presentation of blunt right diaphragmatic rupture (hepatic hernia). Am J Emerg Med 2008; 26(5): 638.e3–638.e5. [DOI] [PubMed] [Google Scholar]
- 4. Ordog GJ, Wasserberger J, Balasubramaniam S. Tension gastrothorax complicating post-traumatic rupture of the diaphragm. Am J Emerg Med 1984; 2(3): 219–221. [DOI] [PubMed] [Google Scholar]
- 5. Mihos P, Polaris K, Gakidis J, et al. Traumatic rupture of the diaphragm: experience with 65 patients. Injury 2003; 34: 169–172. [DOI] [PubMed] [Google Scholar]
- 6. Panda A, Kumar A, Gamanagatti S, et al. Traumatic diaphragmatic injury: a review of CT signs and the difference between blunt and penetrating injury. Diagn Interv Radiol 2014; 20: 121–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Desir A, Ghaye B. CT of blunt diaphragmatic rupture. RSNA, 2012, radiographics.rsna.org [DOI] [PubMed]
- 8. Fair KA, Gordon NT, Barbosa RR, et al. Traumatic diaphragmatic injury in the American College of Surgeons National Trauma Data Bank: a new examination of a rare diagnosis. Am J Surg 2015; 209(5): 864–868. [DOI] [PubMed] [Google Scholar]
- 9. Zhao L, Han Z, Liu H, et al. Delayed traumatic diaphragmatic rupture: diagnosis and surgical treatment. J Thoracic Dis 2019; 11(7): 2774–2777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rashid F, Chakrabarty M, Singh R, et al. A review on delayed presentation of diaphragmatic rupture. World J Emerg Surg 2009; 4: 32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Testini M, Girardi A, Isernia RM, et al. Emergency surgery due to diaphragmatic hernia: case series and review. World J Emerg Surg 2017; 12: 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Magu S, Agarwal S, Singla S. Computed tomography in the evaluation of diaphragmatic hernia following blunt trauma. Indian J Surg 2012; 74(4): 288–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Hariharan D, Singhal R, Kinra S, et al. Post-traumatic intrathoracic spleen presenting with upper GI bleed a case report. BMC Gastroenterol 2006; 6: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hofmann S, Kornmann M, Henne-Bruns D, et al. Traumatic diaphragmatic ruptures: clinical presentation, diagnosis and surgical approach in adults. GMS Interdiscip Plast Reconstr Surg DGPW 2012; 1: Doc02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ganie FA, Lone H, Lone GN, et al. Delayed presentation of traumatic diaphragmatic hernia: a diagnosis of suspicion with increased morbidity and mortality. Trauma Mon 2013; 18(1): 12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ahn S, Kim W, Sohn CH, et al. Tension viscerothorax after blunt abdominal trauma: a case report and review of the literature. J Emerg Med 2012; 43(6): e451–e453. [DOI] [PubMed] [Google Scholar]
- 17. Simon LV, Lopez RA, Burns B. Diaphragm rupture. StatPearls, 2022, https://www.ncbi.nlm.nih.gov/books/NBK470214 (accessed 4 February 2022). [PubMed]
- 18. McCann B, O’Gara A. Tension viscerothorax: an important differential for tension pneumothorax. Emerg Med J 2005; 22(3): 220–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Horst M, Sacher P, Molz G, et al. Tension gastrothorax. J Pediatr Surg 2005; 40(9): 1500–1504. [DOI] [PubMed] [Google Scholar]
- 20. Goh BK, Wong AS, Tay KH, et al. Delayed presentation of a patient with a ruptured diaphragm complicated by gastric incarceration and perforation after apparently minor blunt trauma. CJEM 2004; 6(4): 277–280. [DOI] [PubMed] [Google Scholar]
- 21. Saunders R, Vlahui T, Krebill E, et al. A traumatic tension viscerothorax causing a cardiac arrest: what are your treatment options? Critical Care Medicine, January 2019; 47(1): 869. [Google Scholar]
- 22. Bunya N, Sawamoto K, Uemura S, et al. How to manage tension gastrothorax: a case report of tension gastrothorax with multiple trauma due to traumatic diaphragmatic rupture. Int J Emerg Med 2017; 10(1): 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Lau YH, See KC. Point-of-care ultrasound for critically-ill patients: a mini-review of key diagnostic features and protocols. World J Crit Care Med 2022; 11(2): 70–84. [DOI] [PMC free article] [PubMed] [Google Scholar]


