Version Changes
Revised. Amendments from Version 1
Minor edits like MSD definition, intra-examiner reliability, additional information on the number of publications sought from databases in PRISMA flow chart, few grammatical errors were included in the manuscript as per the recommendations of the reviewers.
Abstract
Background: Work-related musculoskeletal disorders (MSD) are common in dentistry due to the prolonged static work involved during patient care, making dental health care personnel vulnerable to musculoskeletal complaints. We aimed to pool the prevalence estimates of MSD among various dental healthcare providers, including dentists, dental students, dental hygienists, and auxiliaries.
Methods: A systematic search of five databases was performed (Scopus, Embase, CINAHL, Web of Science, Dentistry & Oral Sciences Source). The studies that reported the prevalence of MSD among dental healthcare workers and those written in English were selected. Screening and data extraction were performed by two review authors independently. Discrepencies were resolved by another review author. Risk of bias assessment was done using a nine-item questionnaire developed by Hoy et al. Pooled estimates were calculated using meta-analysis of proportions (random effects model).
Results: Among the 3090 publications screened, 234 publications were included for full-text screening. Meta-analysis was performed for 89 estimates from 88 publications. Females showed significantly higher prevalence [OR = 1.42 (95% CI = 1.09–1.84); I 2 = 66.02; N = 32]. The analysis yielded a pooled estimate of 78.4% (95% CI = 74.8–82). The meta-regression showed similar prevalence over the years (Coefficient: 0.001; P-value: 0.762).
Conclusions: A high prevalence of MSD was noted among dental healthcare providers, with about seven out of ten having experienced MSD in the past. This emphasizes the need for awareness and adoption of appropriate ergonomic postures by dental healthcare providers from early in their careers to minimize work-related MSD.
Keywords: musculoskeletal disorders, workplace, dentist, dental students, dental auxiliary, systematic review
Introduction
“Musculoskeletal disorders (MSD) are injuries to the human support system of muscles, ligaments, tendons, nerves, blood vessels, bones, and joints” ( https://www.cdc.gov/). MSDs are defined as musculoskeletal system and connective tissue diseases and disorders when the event or exposure leading to the case is bodily reaction (e.g., bending, climbing, crawling, reaching, twisting), overexertion, or repetitive motion. MSDs do not include disorders caused by slips, trips, falls, or similar incidents (Bureau of Labor Statistics of the Department of Labor. NIOSH workers health chartbook 2004. NIOSH Publication No. 2004-146. Washington, D.C). Such injuries resulting due to occupation or work-related exposure are termed work-related MSD. Work-related MSD is common in dentistry due to the prolonged static work involved during patient care, making dental health care personnel vulnerable to musculoskeletal complaints. Moreover, the current lifestyle practices make the onset of such problems likely at an early stage of life. MSD includes pain, discomfort, or limitation in a range of activities in the head, neck, shoulders, arms, wrists, fingers, elbows, upper and lower back, buttocks, thighs, feet, ankle, etc.
MSD among dental healthcare personnel can potentially impact the individual and the community. Literature has shown a decrease in work efficiency, stress, poor sleep quality, multisite pain, frequent absenteeism, and/or early retirement resulting in loss of workforce. 1 , 2 The preventive strategies adopted to mitigate MSD are massage treatments, increased physical activity, adopting ergonomically designed equipment, maintaining correct postures, and using complementary and alternative medicine. 3 , 4
The studies on self-reported MSD have reported a high prevalence among dental healthcare personnel. 5 – 10 Studies have also evaluated the associated risk factors of MSD among dentists, 7 , 11 – 19 dental hygienists, 6 , 20 , 21 and dental students. 22 , 23 Increasing age, gender (female), comorbidities, prolonged working hours, increased patient load, lack of physical exercise, non-usage of loupes, stress, lack of breaks between patients, awkward postures, administrative work, vibration, and repetition were some of the reported risk factors of MSD. 4 , 24 A few literature reviews and meta-analysis on these conditions have reported a high prevalence among dental healthcare personnel. 25 – 31 However, there was no attempt to study the overall prevalence estimates of MSD burden among various dental healthcare providers, including dentists, dental students, dental assistants, and auxiliaries at a global level. Hence, we aimed to pool the estimates of the MSD burden among dental healthcare providers.
Methods
Inclusion and exclusion criteria
The studies that reported the overall prevalence of MSD among dental healthcare personnel (dentists, dental students, hygienists, or dental auxiliaries), and the studies written in English were included. Only cross-sectional studies and cohort studies, where prevalence data can be extracted or calculated were included. The studies reported as commentaries, letters, or conference abstracts were excluded. The protocol was registered with INPLASY ( DOI: 10.37766/inplasy2021.5.0100). 32
Literature search
A systematic search in five databases (Scopus (RRID:SCR_022706), Embase (RRID:SCR_001650), CINAHL (RRID:SCR_022707), Web of Science (RRID:SCR_022706), Dentistry & Oral Sciences Source (RRID:SCR_022705)) from inception to 5 August 2021 was performed. The keywords used were “dentist OR dental hygienist OR dental personnel OR dental student” AND “musculoskeletal disease OR musculoskeletal disorder OR occupational disease OR work-related musculoskeletal disorder.” Suitable filters (reports on humans, research articles) for each database were applied.
Screening
The search was imported to Rayyan, a web-based application (RRID:SCR_017584). 33 The screening and data extraction were done by two review authors independently (MK and MM). Disagreements were arbitrated by another review author (PKC). Agreement between the reviewers for title and abstract screening and full text screening showed almost perfect agreement (Kappa: 0.94 and 0.98 respectively).
Risk of bias (RoB) assessment
All studies were assessed using the 10 item Quality Assessment Checklist for Prevalence Studies questionnaire 34 by two review authors independently (HS and PKC). Disagreements were arbitrated by another review author (CD). Each question has two levels, low risk (0) and high risk (1). The total of all nine questions was used to categorize the studies as “low (0–3), moderate (4–6), or high risk (7–9)”.
Data extraction
The variables for data extraction included study details such as authors, year, country, continent, study design, sample size, type of participants (dentist or dental students, or dental auxiliaries), age distribution, sex distribution, the overall prevalence of MSD at maximum recall along with lifetime, annual, one-week prevalence, gender and site-specific estimates.
Statistical analysis
Due to variation in the reporting of the prevalence of MSD among the included studies, the prevalence estimates at the maximal follow-up were used to calculate the pooled estimates of MSD. Measures of heterogeneity (Q and I 2) were calculated. A random-effects model (restricted maximum likelihood estimation method) was used to calculate the prevalence estimates using the OpenMeta[Analyst] software for Windows 8 (Metafor Package 1.4, 1999) (RRID: SCR_022698). Time trends of MSD were evaluated using meta-regression. A sub-group analysis based on the continent, country, type of dental personnel, site of MSD, and sex was performed. A funnel plot was used to evaluate the publication bias. Complete data for the analysis can be accessed at Mendeley datasets. 35
Results
A comprehensive systematic search of five databases (Scopus (1080), Embase (592), CINAHL (728), Web of Science (514), Dentistry & Oral Sciences Source (750)) yielded a total of 3664 articles. Reviews, conference proceedings, case reports, clinical trials, studies on ergonomics, quality of life, burnout, etc. letters, magazine reports, work related hazards other than MSD, studies among health professionals other than dentists were excluded (n = 2856). A further 146 publications were excluded after screening the full-text. Meta-analysis was performed for 89 estimates ( Table 1 and Figure 1).
Table 1. Characteristics of the included studies in the meta-analysis.
| Author and year | Continent | Sample size | Population | ROB | Prevalence |
|---|---|---|---|---|---|
| Osborn et al. 1990 | NA | 385 | Dentists | Low | 68.31 |
| Rundcrantz et al. (a) 1990 | Eu | 311 | DA | Low | 83.28 |
| Rundcrantz et al. (b) 1991 | Eu | 311 | Dentists | Low | 84.24 |
| Marshall et al. 1997 | Au | 355 | Dentists | Low | 81.97 |
| Akesson et al. 1999 | Eu | 74 | ALL | Low | 91.89 |
| Kerosuo et al. 2000 | Eu | 228 | Dentists | Low | 70.61 |
| Lalumandier et al. 2001 | NA | 5119 | ALL | Low | 47.14 |
| Anton et al. 2002 | NA | 95 | DA | Low | 92.63 |
| Szymanska 2002 | Eu | 268 | Dentists | Low | 91.42 |
| Tezel et al. 2005 | Asia | 221 | DS | Low | 85.97 |
| Leggat et al. 2006 | Au | 285 | Dentists | Low | 87.37 |
| Polat et al. 2007 | Asia | 120 | Dentists | Low | 94.17 |
| Puriene et al. 2008 | Eu | 1670 | Dentists | Low | 86.53 |
| de Carvalho et al. 2009 | SA | 227 | DS | Low | 70.93 |
| Akar et al. 2009 | Asia | 185 | DA | Low | 23.78 |
| Ayers et al. 2009 | Au | 560 | Dentists | Low | 59.82 |
| Dajpratham et al. 2010 | Asia | 163 | ALL | Low | 96.93 |
| Kierklo et al. 2011 | Eu | 220 | Dentists | Low | 90.00 |
| Ellapen et al 2011 | Africa | 94 | Dentists | Low | 54.26 |
| Moradia and Prakash 2011 | Asia | 77 | ALL | Low | 63.64 |
| Sankar et al. 2012 | Asia | 259 | Dentists | Low | 41.70 |
| Tzu et al. 2012 | Asia | 197 | Dentists | Low | 92.39 |
| Muralidharan et al. 2013 | Asia | 73 | Dentists | Low | 78.08 |
| Kumar et al. 2013 | Asia | 536 | Dentists | Low | 100.00 |
| Vuletic et al. 2013 | Eu | 89 | Dentists | Low | 69.66 |
| Kazancioglu et al. 2013 | Asia | 608 | Dentists | Low | 87.01 |
| Rafeemanesh et al. 2013 | Asia | 58 | Dentists | Low | 82.76 |
| Zoidaki et al. 2013 | Eu | 80 | Dentists | Low | 82.50 |
| Movahhed et al. 2013 | Asia | 177 | DS | Low | 83.62 |
| Sustova et al. 2013 | Eu | 182 | DS | Low | 39.01 |
| Vora et al. 2014 | Asia | 86 | Dentists | Low | 62.79 |
| Zarra and Lambrianidis 2014 | Eu | 120 | Dentists | Low | 60.83 |
| Mendegeri et al. 2014 | Asia | 60 | Dentists | Low | 88.33 |
| Shadmehr et al. 2014 | Asia | 446 | Dentists | Low | 80.94 |
| Kursun et al. 2014 | Asia | 264 | DS | Low | 48.48 |
| Tirgar et al. 2015 | Asia | 60 | Dentists | Low | 93.33 |
| Gupta et al. (a) 2015 | Asia | 877 | Dentists | Low | 71.04 |
| Humann et al. 2015 | NA | 488 | DA | Low | 98.36 |
| Sakzewski et al. 2015 | Au | 466 | Dentists | Low | 86.05 |
| Kanaparthy et al. 2015 | Asia | 134 | DS | Moderate | 53.73 |
| Aljanakh et al. 2015 | Asia | 68 | Dentists | Low | 77.94 |
| Alghadir et al. 2015 | Asia | 146 | Dentists | Low | 84.93 |
| Hodacova et al. 2015 | Eu | 575 | Dentists | Low | 97.91 |
| Bhagwat et al. 2015 | Asia | 200 | Dentists | Low | 57.50 |
| Gupta et al. (b) 2015 | Asia | 2879 | Dentists | Low | 100.00 |
| Sahu et al. 2015 | Asia | 206 | Dentists | Low | 81.07 |
| Tamo et al. 2015 | Asia | 156 | Dentists | Low | 70.51 |
| Batham and Yasobant 2016 | Asia | 93 | Dentists | Low | 92.47 |
| Rehman et al. 2016 | Asia | 120 | DS | Low | 70.00 |
| Kriangkrai et al. 2016 | Asia | 68 | DS | Low | 100.00 |
| Rayyan et al. 2016 | Asia | 191 | DS | Low | 83.77 |
| Cho et al. 2016 | Asia | 401 | Dentists | Low | 86.78 |
| Phedy et al. 2016 | Asia | 241 | Dentists | Low | 63.49 |
| Freire et al. 2016 | SA | 94 | Dentists | Low | 90.43 |
| Al-Rawi et al. 2016 | Asia | 101 | Dentists | Low | 67.33 |
| Barry et al. 2017 | NA | 337 | DA | Low | 80.42 |
| Garbin et al. 2017 | SA | 204 | Dentists | Low | 81.37 |
| Taib et al. 2017 | Asia | 82 | Dentists | Low | 100.00 |
| Al-Hourani et al. 2017 | Asia | 81 | DA | Low | 100.00 |
| Revankar et al. 2017 | Asia | 150 | Dentists | Moderate | 81.33 |
| Hegde et al. 2018 | Asia | 200 | Dentists | Low | 97.00 |
| Hosseini et al. 2019 | Asia | 136 | Dentists | Low | 91.91 |
| Scepanovic et al. 2019 | Eu | 87 | ALL | Low | 79.31 |
| El Naji et al. 2019 | Asia | 134 | Dentists | Low | 19.40 |
| Benlidayi et al. 2019 | Asia | 99 | DS | Low | 85.86 |
| Zafar et al. 2019 | Asia | 142 | DS | Low | 58.45 |
| dos Santos et al. 2019 | SA | 241 | DS | Low | 82.57 |
| Meisha et al. 2019 | Asia | 234 | Dentists | Low | 70.09 |
| Gandham et al. 2019 | Asia | 150 | Dentists | Low | 58.67 |
| Khandan et al. 2020 | Asia | 51 | Dentists | Low | 84.31 |
| Netanely et al. 2020 | Asia | 102 | DA | Low | 89.22 |
| Harris et al. 2020 | NA | 647 | DA | Low | 82.53 |
| Pope-Ford et al. 2020 | NA | 14 | Dentists | Moderate | 92.86 |
| Senosy et al. 2020 | Asia | 66 | Dentists | Low | 89.39 |
| Shekhawat et al. 2020 | Asia | 72 | Dentists | Low | 100.00 |
| Rahman et al. 2020 | Asia | 82 | DA | Low | 81.71 |
| Uppada et al. (b) 2020 | Asia | 624 | Dentists | Low | 69.07 |
| Aboalshamat 2020 | Asia | 332 | ALL | Low | 81.33 |
| Ohlendorf et al. (b) 2020 | Eu | 450 | ALL | Low | 95.78 |
| Ohlendorf et al. (a) 2020 | Eu | 406 | DA | Low | 98.52 |
| Uppada et al. (a) 2020 | Asia | 156 | Dentists | Low | 84.62 |
| Kumar M et al. 2020 | Asia | 151 | ALL | Low | 58.28 |
| Berdouses et al. 2020 | Eu | 1500 | Dentists | Low | 54.07 |
| Ahmad et al. 2020 | Asia | 244 | Dentists | Low | 86.48 |
| Hashim et al. 2021 | Asia | 202 | DS | Moderate | 68.32 |
| Alnaser et al. 2021 | Asia | 186 | Dentists | Low | 47.85 |
| Gandolfi et al. 2021 | Eu | 284 | ALL | Low | 84.86 |
| Felemban et al. 2021 | Asia | 377 | DS | Low | 91.25 |
| Bhuvaneshwari et al. 2021 | Asia | 545 | Dentists | Low | 88.07 |
Eu: Europe; NA: North America; SA: South America; Au: Australia; DA: Dental auxillaries; DS: Dental students; ALL: All types of dental health care personnel; ROB: Risk of Bias.
Figure 1. PRISMA flow chart.
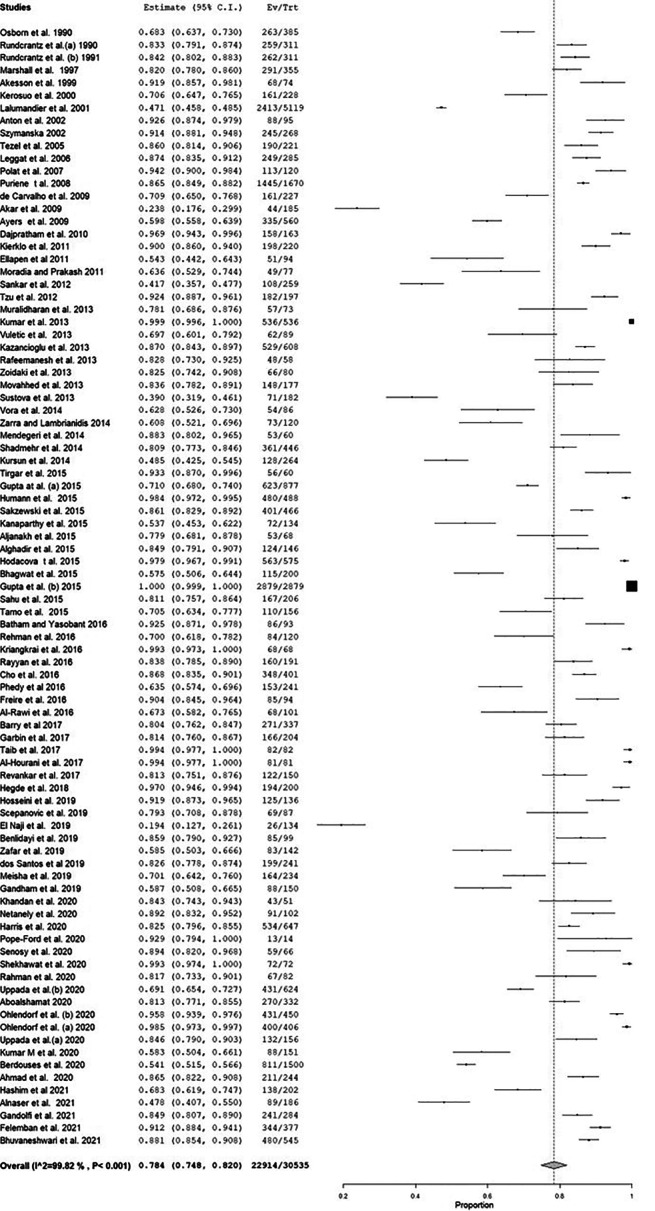
Prevalence
The prevalence of MSD ranged from 19.4 to 100%. Only seven publications showed less than 50% of MSD. 17 , 36 – 41 More than one-quarter (n = 24) of the included publications reported more than 90% prevalence. 5 – 12 , 16 , 18 , 23 , 42 – 54 One fourth of the studies (n = 21) reported a lifetime prevalence, 3 , 37 , 39 , 44 , 45 , 49 , 51 , 53 – 66 while only eight studies reported a one-week prevalence. 8 , 18 , 19 , 22 , 42 , 53 , 54 , 67 Most of the included studies reported a one-year prevalence (n = 65) ( Table 1).
Age
Most of the studies reported the age distribution of the participants (n = 61), while 14 studies reported only the age range of the participants. Prevalence estimates could not be calculated as there was substantial variation in age grouping.
Gender
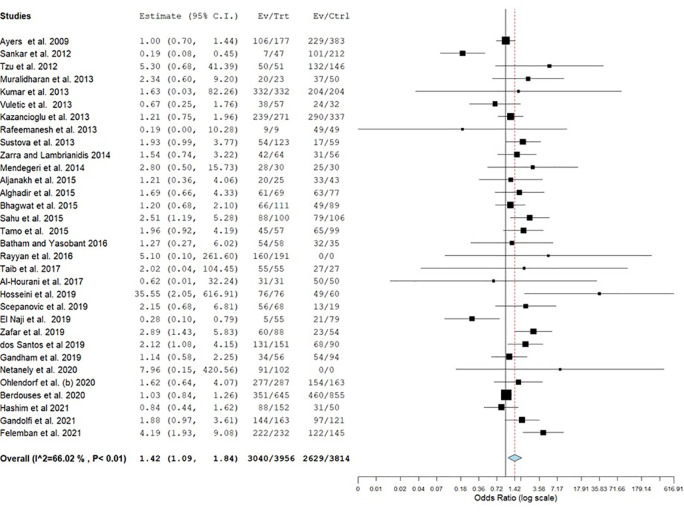
Most of the studies reported the gender distribution of the participants (n = 80). Only one-third of the studies (n = 32) reported gender-specific estimates. The pooled prevalence of MSD among males and females was 72.4% (95% CI = 65.2–79.6) and 77.4% (95% CI = 69.4–85.4) respectively 6 , 7 , 10 , 12 , 13 , 16 , 18 , 22 , 23 , 38 , 39 , 41 , 53 , 56 , 58 , 59 , 62 , 67 – 80 ( Table 2). Females had significantly higher estimates of MSD than males (OR = 1.42) ( Figure 2).
Table 2. Sub-group analysis of the pooled estimates of overall musculoskeletal disorders.
| Characteristic | Estimate (95% CI) | Q | I 2 | N |
|---|---|---|---|---|
| Recall interval | ||||
| Overall | 0.78 (0.75–0.82) | 13941.24 | 99.82 | 89 |
| Lifetime | 0.78 (0.7–0.85) | 4752.99 | 99.4 | 21 |
| One year | 0.82 (0.78–0.85) | 4922.35 | 99.79 | 65 |
| One week | 0.66 (0.52–0.79) | 330.09 | 97.67 | 8 |
| Sex | ||||
| Male | 0.73 (0.65–0.8) | 1914.47 | 98.69 | 30 |
| Female | 0.77 (0.69–0.85) | 2047.83 | 99.41 | 32 |
| Dental personnel | ||||
| Dentists | 0.79 (0.75–0.83) | 5788.91 | 99.85 | 56 |
| Dental auxiliaries | 0.83 (0.69–0.97) | 768.63 | 99.7 | 10 |
| Dental students | 0.73 (0.64–0.82) | 671.93 | 98.09 | 14 |
| Mixed | 0.78 (0.66–0.89) | 2346.13 | 99.16 | 9 |
| Continent | ||||
| North America | 0.8 (0.67–0.93) | 3272.59 | 99.5 | 7 |
| Europe | 0.8 (0.72–0.88) | 1530.95 | 99.29 | 17 |
| Australia | 0.79 (0.66–0.91) | 124.04 | 97.79 | 4 |
| Asia | 0.78 (0.73–0.83) | 4693.83 | 99.88 | 56 |
| South America | 0.81 (0.74–0.89) | 21.15 | 87.39 | 4 |
| Country | ||||
| US | 0.8 (0.64–0.95) | 3263.61 | 99.59 | 6 |
| Sweden | 0.86 (0.81–0.91) | 5.485 | 67.53 | 3 |
| Australia | 0.85 (0.82–0.88) | 3.984 | 49.84 | 3 |
| Turkey | 0.71 (0.48–0.94) | 506.76 | 99.3 | 6 |
| Brazil | 0.81 (0.74–0.89) | 21.15 | 87.39 | 4 |
| India | 0.77 (0.7–0.85) | 1744.26 | 99.94 | 20 |
| Iran | 0.86 (0.82–0.91) | 20.21 | 71.87 | 6 |
| Greece | 0.66 (0.49–0.82) | 41.93 | 95.13 | 3 |
| Saudi | 0.76 (0.66–0.85) | 133.73 | 95.64 | 8 |
| Malaysia | 0.9 (0.79–1) | 43.86 | 94.73 | 3 |
| Risk of bias | ||||
| Low | 0.79 (0.75–0.82) | 13700.42 | 99.83 | 85 |
| Moderate | 0.74 (0.58–0.9) | 37.04 | 93.86 | 4 |
Figure 2. Forest plot of gender difference in the prevalence of musculoskeletal disorders (MSD).
Geographic distribution
Only a few studies were reported from North America (n = 7), 37 , 43 , 49 , 52 , 63 , 81 , 82 South America (n = 4), 19 , 50 , 77 , 83 and Australia (n = 4), 14 , 68 , 84 , 85 while only one study was reported from Africa. 86 Most of the studies were from Asia 3 , 5 – 10 , 12 , 15 – 18 , 22 , 23 , 36 , 38 , 40 , 41 , 45 , 46 , 48 , 51 , 55 – 62 , 64 – 66 , 69 – 71 , 73 – 76 , 78 , 79 , 87 – 100 and Europe 11 , 13 , 39 , 42 , 44 , 47 , 53 , 54 , 67 , 72 , 80 , 101 – 105 ( Table 2). Countries with more than three studies were included for the sub-group analysis. The highest pooled prevalence was seen in Malaysia, and the lowest pooled prevalence was seen in Greece.
Risk of bias (RoB)
Out of the 88 studies included, only four studies had a moderate RoB. 22 , 52 , 57 , 60 The pooled estimates for studies with low and moderate RoB were 79% and 74% ( Table 2).
Site distribution
The commonly reported sites were the neck, back, lower back, shoulder, upper back, and wrists. The least affected sites were thighs, legs, arms, feet, and ankles ( Table 3).
Table 3. Site-specific pooled estimates of overall musculoskeletal disorders.
| Site | Estimate (95% CI) | Q | I 2 | N |
|---|---|---|---|---|
| Neck | 0.51 (0.46–0.56) | 11158.95 | 98.86 | 78 |
| Shoulder | 0.41 (0.36–0.47) | 8921.3 | 99.09 | 71 |
| Wrist | 0.31 (0.27–0.35) | 4668.92 | 98.39 | 65 |
| Arm | 0.11 (0.07–0.15) | 269.08 | 96.9 | 14 |
| Elbow | 0.16 (0.11–0.2) | 1666.43 | 98.82 | 50 |
| Fingers | 0.18 (0.06–0.3) | 260.81 | 98.23 | 6 |
| Hip | 0.16 (0.13–0.2) | 1697.04 | 97.31 | 49 |
| Thighs | 0.1 (0.06–0.14) | 92.07 | 89.32 | 10 |
| Knee | 0.18 (0.15–0.21) | 1483.36 | 95.92 | 49 |
| Leg | 0.11 (0.06–0.17) | 604.18 | 99.34 | 19 |
| Ankle | 0.14 (0.11–0.17) | 1023.76 | 97.12 | 41 |
| Feet | 0.13 (0.06–0.2) | 302.74 | 97.02 | 10 |
| Back | 0.5 (0.39–0.6) | 8971.27 | 99.45 | 17 |
| Lower back | 0.46 (0.42–0.5) | 3142.31 | 97.49 | 66 |
| Upper back | 0.35 (0.3–0.4) | 3480.2 | 97.99 | 58 |
Meta-analysis
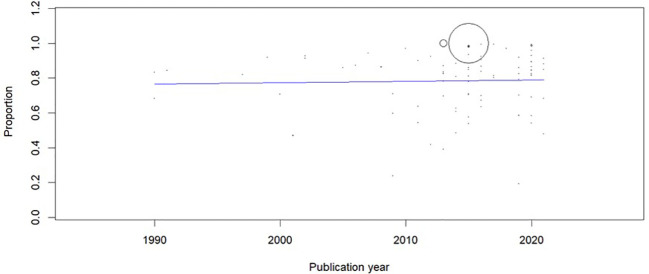
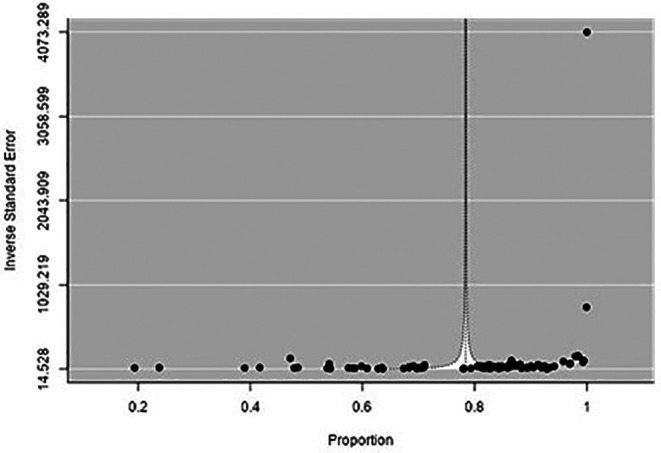
There was high heterogeneity among the included studies, as evidenced by Q and I 2 statistics. The model yielded a pooled estimate of 78.4% ( Figure 3), and sensitivity analysis did not show any change in the overall estimate. The meta-regression showed no change in the trend of MSD (Coefficient: 0.001; 95% CI: -0.004 to 0.006) ( Figure 4). Asymmetry was noted in the funnel plot (p < 0.001) ( Figure 5).
Figure 3. Forest plot of the prevalence of musculoskeletal disorders (MSD).
Figure 4. Meta-regression to evaluate the trends in the prevalence of musculoskeletal disorders (MSD).
Figure 5. Funnel plot to evaluate the publication bias.
Discussion
MSD’s result in pain, discomfort, or limitation in the range of movement. They are preventable conditions often due to poor ergonomic postures adopted by dental health care providers. We aimed to pool the estimates of MSD among dental healthcare providers. Eighty-eight publications recorded a comprehensive assessment of all body areas and reported the overall prevalence of MSD. The estimates needed to be evaluated carefully due to the high heterogeneity. The overall estimate was 78%, which was much higher than Greek and Czech surveys. 37 , 80 However, extensive surveys of dentists from India and Lithuania have reported similar or higher prevalence estimates. 3 , 9 , 101 Therefore, it is clear that dental professionals have quite a higher prevalence of MSD. Age-specific prevalence estimates could not be estimated due to a lack of standardized age groups or specific prevalence estimates. It was found that females showed higher prevalence estimates than males. Although the number of studies that reported gender distribution was high, only one-third of these studies reported gender-specific estimates of MSD.
The prevalence estimates were similar across the continents. The highest number of studies were reported from the Asian continent. The highest number of studies were from India, 3 , 5 , 9 , 10 , 18 , 38 , 51 , 55 , 56 , 59 , 60 , 64 , 65 , 69 , 74 , 75 , 78 , 88 , 97 , 99 followed by the US, 37 , 43 , 49 , 52 , 81 , 82 Iran, 15 , 16 , 48 , 66 , 71 , 89 and Turkey. 36 , 40 , 45 , 61 , 70 , 87 Studies from Malaysia 7 , 95 , 98 reported the highest prevalence estimates among various countries, followed by Iran, 15 , 16 , 48 , 66 , 71 , 89 Sweden, 42 , 102 Australia, 14 , 84 , 85 Brazil, 19 , 50 , 77 , 83 and the US. 37 , 43 , 49 , 52 , 81 , 82 There was not much variation in the prevalence estimates among the dentists, dental auxiliaries, and dental students. These observations suggest that all types of dental healthcare providers globally suffer from MSDs due to prolonged static postures. Over three decades, there was no significant change in the trend of MSD, indicating a consistently higher prevalence, highlighting the need to incorporate ergonomics into the dental curriculum.
There was substantial inconsistency in the assessment of prevalence estimates among the studies. The Nordic/standardized Nordic questionnaire was the most commonly used tool to assess MSDs. A few studies used generic questionnaires and single-item questions without adequate validity and reliability. Moreover, the studies used various time recall periods (lifetime, one year, six months, one month, and one week) to assess the prevalence estimates. The studies that used lifetime or extended recall periods might have included pre-existing MSDs that may not be work-related, which could have diluted the estimates of MSD.
MSD can arise from various reasons, and there was a lack of clarity in most of the studies. Only one study explicitly recorded the estimates before and after joining the dental profession. 58 There was a general lack of clarity on the estimates reported for various body parts (shoulders, hands, elbow, wrists, legs, ankles, hips, fingers, toes). The studies reported right, left, and bilateral prevalence estimates of MSD without detailing the prevalence for each site. MSD in such areas could have been reported as unilateral and bilateral rather than right, left, and bilateral estimates. Furthermore, there was no uniformity in the evaluation of site-specific assessments among the studies included (e.g. lack of clarity on the terms hand and arms).
The strength of this review is the inclusion of studies that reported the overall estimates of MSD, including many databases, all types of dental healthcare personnel, overall, lifetime and annual estimates, sub-group analysis, gender, and site-specific prevalence estimates. A few limitations were observed in our study. They are the exclusion of studies published in other languages, lack of age-specific prevalence estimates, lack of differentiation between work-related and pre-existing MSDs, causes of MSDs due to inadequate reporting in primary studies, use of self-reported measures of MSD rather than objective measures, and exclusion of studies with no comprehensive assessment or overall estimates of MSD.
The additional confounding factors related to lifestyle (sedentary lifestyle, lack of regular physical exercise, and other extra-curricular activities) could significantly influence the onset and duration of MSD. Furthermore, the number of clinical working days/week, working hours/day, type and duration of procedures, specialization, number of patients/days, remedial measures, and history of MSD in the past could also substantially impact the estimates of MSD. These inconsistencies in the included studies could have influenced the overall prevalence of MSD.
Conclusions
MSD among dental healthcare personnel is widespread and mostly chronic. Seven out of ten dental healthcare providers could have experienced MSD in the past. However, the severity and self-limiting nature of MSD cannot be underestimated. Awareness, adoption, and maintenance of appropriate ergonomic postures should be encouraged at dental schools and early in the career. Future studies should use the “Strengthening the Reporting of Observational Studies in Epidemiology ( STROBE)” guidelines and use validated questionnaires for reporting MSD.
Data availability
Underlying data
Mendeley Data: Underlying data for ‘Musculoskeletal disorders among dental health care professionals’. https://www.doi.org/10.17632/2ttwfmzm9n.2 35
Reporting guidelines
Mendeley Data: PRISMA checklist for ‘Musculoskeletal disorders among dental health care professionals’. https://www.doi.org/10.17632/2ttwfmzm9n.2 35
Data are available under the terms of the Creative Commons Attribution 4.0 International license (CC-BY 4.0)
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 2; peer review: 2 approved]
References
- 1. Marklund S, Mienna CS, Wahlström J, et al. : Work ability and productivity among dentists: associations with musculoskeletal pain, stress, and sleep. Int. Arch. Occup. Environ. Health. 2020;93(2):271–278. 10.1007/s00420-019-01478-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lindegård A, Larsman P, Hadzibajramovic E, et al. : The influence of perceived stress and musculoskeletal pain on work performance and work ability in Swedish health care workers. Int. Arch. Occup. Environ. Health. 2014;87(4):373–379. 10.1007/s00420-013-0875-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gupta D, Devaki M, Dommaraju N, et al. : Musculoskeletal pain management among dentists: An alternative approach. Holist. Nurs. Pract. 2015;29(6):385–390. 10.1097/HNP.0000000000000074 [DOI] [PubMed] [Google Scholar]
- 4. Pejčić N, Petrović V, Marković D, et al. : Assessment of risk factors and preventive measures and their relations to work-related musculoskeletal pain among dentists. Work. 2017;57(4):573–593. 10.3233/WOR-172588 [DOI] [PubMed] [Google Scholar]
- 5. Shekhawat K, Chauhan A, Sakthidevi S, et al. : Work-related musculoskeletal pain and its self-reported impact among practicing dentists in Puducherry, India. Indian J. Dent. Res. 2020;31(3):354–357. 10.4103/ijdr.IJDR_352_18 [DOI] [PubMed] [Google Scholar]
- 6. Al-Hourani Z, Nazzal M, Khader Y, et al. : Work-related musculoskeletal disorders among Jordanian dental technicians: Prevalence and associated factors. Work. 2017;56(4):617–623. 10.3233/WOR-172524 [DOI] [PubMed] [Google Scholar]
- 7. Taib MFM, Bahn S, Yun MH, et al. : The effects of physical and psychosocial factors and ergonomic conditions on the prevalence of musculoskeletal disorders among dentists in Malaysia. Work. 2017;57(2):297–308. 10.3233/WOR-172559 [DOI] [PubMed] [Google Scholar]
- 8. Kriangkrai R, Sirimala N, Nathamtong S, et al. : Self-reported prevalence and risk factors of musculoskeletal pain in Thai dental students. Int. Dent. J. Students Res. 2016;4(3):116–122. [Google Scholar]
- 9. Gupta D, Mathur A, Patil G, et al. : Prevalence of musculoskeletal disorder and alternative medicine therapies among dentists of North India: A descriptive study. Pharmacognosy Res. 2015;7(4):350–354. 10.4103/0974-8490.157810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Kumar VK, Kumar SP, Baliga MR: Prevalence of work-related musculoskeletal complaints among dentists in India: A national cross-sectional survey. Indian J. Dent. Res. 2013;24(4):428–438. 10.4103/0970-9290.118387 [DOI] [PubMed] [Google Scholar]
- 11. Hodacova L, Sustova Z, Cermakova E, et al. : Self-reported risk factors related to the most frequent musculoskeletal complaints among Czech dentists. Ind. Health. 2015;53(1):48–55. 10.2486/indhealth.2013-0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lin TH, Liu YC, Hsieh TY, et al. : Prevalence of and risk factors for musculoskeletal complaints among Taiwanese dentists. J. Dent. Sci. 2012;7(1):65–71. 10.1016/J.JDS.2012.01.009 [DOI] [Google Scholar]
- 13. Vuletic J, Potran M, Kalem D, et al. : Prevalence and risk factors for musculoskeletal disorders in dentists. Stomatol. Glas. Srb. 2013;60(1):24–31. 10.2298/sgs1301024v [DOI] [Google Scholar]
- 14. Sakzewski L, Naser-Ud-Din S: Work-related musculoskeletal disorders in Australian dentists and orthodontists: Risk assessment and prevention. Work. 2015;52(3):559–579. 10.3233/WOR-152122 [DOI] [PubMed] [Google Scholar]
- 15. Khandan M, Koohpaei A, Shahbazi M, et al. : Assessment of Individual and Occupational Risk Factors of Musculoskeletal Disorders Using BPAI among Dentists in Qom, Iran. Arch. Hyg. Sci. 2020;9(3):234–245. 10.29252/archhygsci.9.3.234 [DOI] [Google Scholar]
- 16. Hosseini A, Choobineh A, Razeghi M, et al. : Ergonomic Assessment of Exposure to Musculoskeletal Disorders Risk Factors among Dentists of Shiraz, Iran. J. Dent. Shiraz. Univ. Med. Sci. 2019;20(1):53–60. 10.30476/dentjods.2019.44564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Alnaser MZ, Almaqsied AM, Alshatti SA: Risk factors for work-related musculoskeletal disorders of dentists in Kuwait and the impact on health and economic status. Work. 2021;68(1):213–221. 10.3233/WOR-203369 [DOI] [PubMed] [Google Scholar]
- 18. Batham C, Yasobant S: A risk assessment study on work-related musculoskeletal disorders among dentists in Bhopal, India. Indian J. Dent. Res. 2016;27(3):236–241. 10.4103/0970-9290.186243 [DOI] [PubMed] [Google Scholar]
- 19. Garbin AJÍ, Soares GB, Arcieri RM, et al. : Musculoskeletal disorders and perception of working conditions: A survey of brazilian dentists in São Paulo. Int. J. Occup. Med. Environ. Health. 2017;30(3):367–377. 10.13075/ijomeh.1896.00724 [DOI] [PubMed] [Google Scholar]
- 20. Ylipää V, Arnetz BB, Preber H: Predictors of good general health, well-being, and musculoskeletal disorders in Swedish dental hygienists. Acta Odontol. Scand. 1999;57(5):277–282. 10.1080/000163599428706 [DOI] [PubMed] [Google Scholar]
- 21. Warren N: Causes of musculoskeletal disorders in dental hygienists and dental hygiene students: A study of combined biomechanical and psychosocial risk factors. Work. 2010;35(4):441–454. 10.3233/WOR-2010-0981 [DOI] [PubMed] [Google Scholar]
- 22. Hashim R, Salah A, Mayahi F, et al. : Prevalence of postural musculoskeletal symptoms among dental students in United Arab Emirates. BMC Musculoskelet. Disord. 2021;22(1):30. 10.1186/s12891-020-03887-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Felemban RA, Sofi RA, Alhebshi SA, et al. : Prevalence and predictors of musculoskeletal pain among undergraduate students at a dental school in Saudi Arabia. Clin. Cosmet. Investig. Dent. 2021;13:39–46. 10.2147/CCIDE.S292970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Alshouibi EN, Almansour LA, Alqurashi AM, et al. : The effect of number of patients treated, dental loupes usage, stress, and exercise on musculoskeletal pain among dentists in Jeddah. J. Int. Soc. Prev. Community Dent. 2020;10(3):336–340. 10.4103/jispcd.JISPCD_2_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Chikte UM, Khondowe O, Louw Q, et al. : A meta analysis of the prevalence of spinal pain among dentists. SADJ. 2011;66(5):214–218. [PubMed] [Google Scholar]
- 26. ZakerJafari HR, YektaKooshali MH: Work-Related Musculoskeletal Disorders in Iranian Dentists: A Systematic Review and Meta-analysis. Saf. Health Work. 2018;9(1):1–9. 10.1016/j.shaw.2017.06.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hayes MJ, Cockrell D, Smith DR: A systematic review of musculoskeletal disorders among dental professionals. Int. J. Dent. Hyg. 2009;7(3):159–165. 10.1111/j.1601-5037.2009.00395.x [DOI] [PubMed] [Google Scholar]
- 28. Shams-Hosseini NS, Vahdati T, Mohammadzadeh Z, et al. : Prevalence of Musculoskeletal Disorders among Dentists in Iran: A Systematic Review. Mater Sociomed. 2017;29(4):257–262. 10.5455/MSM.2017.29.257-262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Puriene A, Janulyte V, Musteikyte M, et al. : General health of dentists. Literature review. Stomatologija. 2007;9(1):10–20. [PubMed] [Google Scholar]
- 30. Leggat PA, Kedjarune U, Smith DR: Occupational health problems in modern dentistry: A review. Ind. Health. 2007;45(5):611–621. 10.2486/indhealth.45.611 [DOI] [PubMed] [Google Scholar]
- 31. Lietz J, Kozak A, Nienhaus A: Prevalence and occupational risk factors of musculoskeletal diseases and pain among dental professionals in Western countries: A systematic literature review and meta-analysis. PLoS One. 2018;13(12):e0208628. 10.1371/journal.pone.0208628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Pentapati K, Chenna D, Kumar M, et al. : Prevalence of Musculoskeletal Disorders (MSD) among Dental Health Care Workers. 2021. 10.37766/inplasy2021.5.0100 [DOI]
- 33. Ouzzani M, Hammady H, Fedorowicz Z, et al. : Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016;5(1):210. 10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hoy D, Brooks P, Woolf A, et al. : Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J. Clin. Epidemiol. 2012;65(9):934–939. 10.1016/j.jclinepi.2011.11.014 [DOI] [PubMed] [Google Scholar]
- 35. Pentapati K, Deepika C: Musculoskeletal disorders among dental health care professionals. 2022;1. 10.17632/2TTWFMZM9N.1 [DOI]
- 36. Akar GC, Aksoy G, Özmutaf NM, et al. : An assessment of awareness and self-report about occupation-related health problems among dental laboratory technicians in Turkey. Nobel Med. 2009;5(3):27–32. [Google Scholar]
- 37. Lalumandier JA, McPhee SD, Parrott CB, et al. : Musculoskeletal pain: prevalence, prevention, and differences among dental office personnel. Gen. Dent. 2001;49(2):160–166. [PubMed] [Google Scholar]
- 38. Gowri Sankar S, Reddy PV, Reddy BR, et al. : The Prevalence of Work-related Musculoskeletal Disorders among Indian Orthodontists. J. Indian Orthod. Soc. 2012;46(4):264–268. 10.5005/jp-journals-10021-1102 [DOI] [Google Scholar]
- 39. Sustová Z, Hodacová L, Kapitán M: The prevalence of musculoskeletal disorders among dentists in the Czech Republic. Acta Med. (Hradec Kralove). 2013;56(4):150–156. 10.14712/18059694.2014.10 [DOI] [PubMed] [Google Scholar]
- 40. Kurşun Ş, Evirgen S, Akbulut N, et al. : Work characteristics and musculoskeletal disorders among postgraduate dental students: A pilot study. J. Musculoskelet. Pain. 2014;22(1):62–67. 10.3109/10582452.2014.883010 [DOI] [Google Scholar]
- 41. El-Naji W, Al Warawreh AM, Al-Saraireh SA, et al. : Occupational hazards among Jordanian dentists. Pakistan Oral Dent J. 2019;39(2):129. [Google Scholar]
- 42. Åkesson I, Johnsson B, Rylander L, et al. : Musculoskeletal disorders among female dental personnel - Clinical examination and a 5-year follow-up study of symptoms. Int. Arch. Occup. Environ. Health. 1999;72(6):395–403. 10.1007/s004200050391 [DOI] [PubMed] [Google Scholar]
- 43. Anton D, Rosecrance J, Merlino L, et al. : Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am. J. Ind. Med. 2002;42(3):248–257. 10.1002/ajim.10110 [DOI] [PubMed] [Google Scholar]
- 44. Szymańska J: Disorders of the musculoskeletal system among dentists from the aspect of ergonomics and prophylaxis. Ann. Agric. Environ. Med. 2002;9(2):169–173. [PubMed] [Google Scholar]
- 45. Polat Z, Başkan S, Altun S, et al. : Musculoskeletal symptoms of dentists from south-east turkey. Biotechnol. Biotechnol. Equip. 2007;21(1):86–90. 10.1080/13102818.2007.10817421 [DOI] [Google Scholar]
- 46. Dajpratham P, Ploypetch T, Kiattavorncharoen S, et al. : Prevalence and associated factors of musculoskeletal pain among the dental personnel in a dental school. J. Med. Assoc. Thail. 2010;93(6):714–721. [PubMed] [Google Scholar]
- 47. Kierklo A, Kobus A, Jaworska M, et al. : Work-related musculoskeletal disorders among dentists - A questionnaire survey. Ann. Agric. Environ. Med. 2011;18(1):79–84. [PubMed] [Google Scholar]
- 48. Tirgar A, Javanshir K, Talebian A, et al. : Musculoskeletal disorders among a group of Iranian general dental practitioners. J. Back Musculoskelet. Rehabil. 2015;28(4):755–759. 10.3233/BMR-140579 [DOI] [PubMed] [Google Scholar]
- 49. Humann P, Rowe DJ: Relationship of Musculoskeletal Disorder Pain to Patterns of Clinical Care in California Dental Hygienists. J. Dent. Hyg. JDH. 2015;89(5):305–312. [PubMed] [Google Scholar]
- 50. Freire AC d GF, Soares GB, Rovida TAS, et al. : Musculoskeletal disorders among dentists in northwest area of the state of São Paulo, Brazil. Brazilian J. Oral Sci. 2016;15(3):190–195. 10.20396/bjos.v15i3.8649979 [DOI] [Google Scholar]
- 51. Hegde S, Donly A, Shankar K: Prevalence of Musculoskeletal Disorders among Dental Professionals-A Questionnaire Study. Indian J. Public Heal. Res. Dev. 2018;9(3):33–37. 10.5958/0976-5506.2018.00178.X [DOI] [Google Scholar]
- 52. Pope-Ford R, Pope-Ozimba J: Musculoskeletal disorders and emergent themes of psychosocial factors and their impact on health in dentistry. Work. 2020;65(3):563–571. 10.3233/WOR-203110 [DOI] [PubMed] [Google Scholar]
- 53. Ohlendorf D, Naser A, Haas Y, et al. : Prevalence of musculoskeletal disorders among dentists and dental students in germany. Int. J. Environ. Res. Public Health. 2020;17(23):1–19. 10.3390/ijerph17238740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Ohlendorf D, Haas Y, Naser A, et al. : Prevalence of Muscular Skeletal Disorders among Qualified Dental Assistants. Int. J. Environ. Res. Public Health. 2020;17(10):3490. 10.3390/ijerph17103490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Alpa V, Ramdev N, Parekh V, et al. : A survey on prevalence of work related musculoskeletal disorder among the dentists in Vadodara city - a questionnaire based study. J. Pearldent. 2014;5(1):31–36. [Google Scholar]
- 56. Mendegeri V, Ramdurg PK, Kambale S, et al. : Prevalence Of Musculoskeletal Disorders Among Dentists: A Pilot Study. Indian J. Dent. Sci. 2014;6(5):16–20. [Google Scholar]
- 57. Kanaparthy A, Kanaparthy R, Boreak N: Postural awareness among dental students in Jizan, Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2015;5(Suppl 2):S107–S111. 10.4103/2231-0762.172950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Alghadir A, Zafar H, Iqbal ZA: Work-related musculoskeletal disorders among dental professionals in Saudi Arabia. J. Phys. Ther. Sci. 2015;27(4):1107–1112. 10.1589/jpts.27.1107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Bhagwat S, Hegde S, Mandke L: Prevalence of musculoskeletal disorders among Indian dentists: A pilot survey with assessment by rapid entire body assessment. World J. Dent. 2015;6(1):39–44. 10.5005/jp-journals-10015-1310 [DOI] [Google Scholar]
- 60. Revankar V, Chakravarthy Y, Naveen S, et al. : Musculoskeletal disorders and mental health-related issues as occupational hazards among dental practitioners in Salem city: A cross-sectional study. J. Pharm. Bioallied Sci. 2017;9(5):S228–S230. 10.4103/jpbs.JPBS_145_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Coskun Benlidayi I, Al-Bayati Z, Guzel R, et al. : Neither got a good bill of musculoskeletal health: a comparative study among medical and dental students. Acta Clin. Belgica Int. J. Clin. Lab. Med. 2019;74(2):110–114. 10.1080/17843286.2018.1483564 [DOI] [PubMed] [Google Scholar]
- 62. Zafar H, Almosa N: Prevalence of work-related musculoskeletal disorders among dental students of King Saud University, Riyadh, Kingdom of Saudi Arabia. J. Contemp. Dent. Pract. 2019;20(4):449–453. 10.5005/jp-journals-10024-2537 [DOI] [PubMed] [Google Scholar]
- 63. Harris ML, Sentner SM, Doucette HJ, et al. : Musculoskeletal disorders among dental hygienists in Canada. Can. J. Dent. Hyg. 2020;54(2):61–67. [PMC free article] [PubMed] [Google Scholar]
- 64. Uppada UK, Susmitha M, Ullah Hussaini S, et al. : Ergonomics among dentists in the states of Telangana and Andhra Pradesh. Natl. J. Maxillofac. Surg. 2020;11(2):253–257. 10.4103/njms.NJMS_33_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Uppada UK, Sinha R, Madishetti S, et al. : Ergonomics among oral and maxillofacial surgeons in the Indian States of Telangana and Andhra Pradesh - An evaluative study. Ann. Maxillofac. Surg. 2020;10(2):325–329. 10.4103/ams.ams_39_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Movahhed T, Ajami B, Soltani M, et al. : Musculoskeletal pain reports among Mashhad dental students, Iran. Pak. J. Biol. Sci. 2013;16(2):80–85. 10.3923/pjbs.2013.80.85 [DOI] [PubMed] [Google Scholar]
- 67. Gandolfi MG, Zamparini F, Spinelli A, et al. : Musculoskeletal disorders among italian dentists and dental hygienists. Int. J. Environ. Res. Public Health. 2021;18(5):1–20. 10.3390/ijerph18052705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Ayers KMS, Thomson WM, Newton JT, et al. : Self-reported occupational health of general dental practitioners. Occup. Med. (Chic Ill). 2009;59(3):142–148. 10.1093/occmed/kqp004 [DOI] [PubMed] [Google Scholar]
- 69. Muralidharan D, Fareed N, Shanthi M: Musculoskeletal Disorders among Dental Practitioners: Does It Affect Practice? Epidemiol. Res. Int. 2013;2013:1–6. 10.1155/2013/716897 [DOI] [Google Scholar]
- 70. Kazancioglu HO, Bereket MC, Ezirganli S, et al. : Musculoskeletal complaints among oral and maxillofacial surgeons and dentists: A questionnaire study. Acta Odontol. Scand. 2013;71(3-4):469–474. 10.3109/00016357.2012.696688 [DOI] [PubMed] [Google Scholar]
- 71. Rafeemanesh E, Jafari Z, Kashani FO, et al. : A study on job postures and musculoskeletal illnesses in dentists. Int. J. Occup. Med. Environ. Health. 2013;26(4):615–620. 10.2478/s13382-013-0133-z [DOI] [PubMed] [Google Scholar]
- 72. Zarra T, Lambrianidis T: Musculoskeletal disorders amongst Greek endodontists: A national questionnaire survey. Int. Endod. J. 2014;47(8):791–801. 10.1111/iej.12219 [DOI] [PubMed] [Google Scholar]
- 73. Aljanakh M, Shaikh S, Siddiqui AA, et al. : Prevalence of musculoskeletal disorders among dentists in the Ha’il Region of Saudi Arabia. Ann. Saudi Med. 2015;35(6):456–461. 10.5144/0256-4947.2015.456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Tamo T, Kalita C, Bhuyan A: Evaluation of occupational musculoskeletal disorders and related risk factors among dentists working in North East India. Dent. Med. Res. 2015;3(2):43. 10.4103/2348-1471.159182 [DOI] [Google Scholar]
- 75. Sahu D, Tandon S, Dhingra S, et al. : Prevalence of musculoskeletal disorders among dentists: A pilot cross-sectional survey. J. Indian Assoc. Public Heal. Dent. 2015;13(3):307. 10.4103/2319-5932.165281 [DOI] [Google Scholar]
- 76. Rayyan M, Hetou S, Al Salem R, et al. : Work-related Musculoskeletal Disorders among Dental Students of Different Academic Levels. J. Int. Oral Heal. 2016;8(4):471–475. 10.2047/jioh-08-04-12 [DOI] [Google Scholar]
- 77. Santos RR, Garbin CAS, Batista JA, et al. : Prevalence of musculoskeletal pain in dental students and associated factors. Brazilian J. Oral Sci. 2019;18:e191668. 10.20396/bjos.v18i0.8657270 [DOI] [Google Scholar]
- 78. Gandham A, Boppana N, Vinnakota N, et al. : Assessment of musculoskeletal disorders and associated risk factors among dentists in Rajahmundry City: A cross-sectional study. J. Indian Assoc. Public Heal. Dent. 2019;17(2):114. 10.4103/jiaphd.jiaphd_9_19 [DOI] [Google Scholar]
- 79. Netanely S, Luria S, Langer D: Musculoskeletal disorders among dental hygienist and students of dental hygiene. Int. J. Dent. Hyg. 2020;18(2):210–216. 10.1111/idh.12428 [DOI] [PubMed] [Google Scholar]
- 80. Berdouses E, Sifakaki M, Katsantoni A, et al. : Work-Related Musculoskeletal Disorders among Greek Dentists - A Nationwide Survey. Dent. Res. Oral Heal. 2020;3(4):169–181. [Google Scholar]
- 81. Osborn JB, Newell KJ, Rudney JD, et al. : Musculoskeletal pain among Minnesota dental hygienists. J. Dent. Hyg. JDH/Am. Dent. Hyg. Assoc. 1990;64(3):132–138. [PubMed] [Google Scholar]
- 82. Barry RM, Spolarich AE, Weber M, et al. : Impact of Operator Positioning on Musculoskeletal Disorders and Work Habits Among Mississippi Dental Hygienists. J. Dent. Hyg. JDH. 2017;91(6):6–14. [PubMed] [Google Scholar]
- 83. Carvalho MVD, Soriano EP, França Caldas A, et al. : Work-Related Musculoskeletal Disorders Among Brazilian Dental Students. J. Dent. Educ. 2009;73(5):624–630. 10.1002/j.0022-0337.2009.73.5.tb04737.x [DOI] [PubMed] [Google Scholar]
- 84. Marshall ED, Duncombe LM, Robinson RQ, et al. : Musculoskeletal symptoms in New South Wales dentists. Aust. Dent. J. 1997;42(4):240–246. 10.1111/j.1834-7819.1997.tb00128.x [DOI] [PubMed] [Google Scholar]
- 85. Leggat PA, Smith DR: Musculoskeletal disorders self-reported by dentists in Queensland, Australia. Aust. Dent. J. 2006;51(4):324–327. 10.1111/j.1834-7819.2006.tb00451.x [DOI] [PubMed] [Google Scholar]
- 86. Ellapen TJ, Narsigan S, Herdeen HJ, et al. : Impact of poor dental ergonomical practice. SADJ. 2011;66(6):272, 274–272, 277. [PubMed] [Google Scholar]
- 87. Tezel A, Kavrut F, Tezel A, et al. : Musculoskeletal disorders in left- and right-handed Turkish dental students. Int. J. Neurosci. 2005;115(2):255–266. 10.1080/00207450590519517 [DOI] [PubMed] [Google Scholar]
- 88. Moradia S, Patel P: A Study on Occupational Pain among Dentists of Surat City. Natl J Community Med. 2011;2(1):116–118. [Google Scholar]
- 89. Shadmehr A, Haddad O, Azarnia S, et al. : Disorders of the musculoskeletal system among Tehran, Iranian dentists. J Musculoskelet Pain. 2014;22(3):256–259. 10.3109/10582452.2014.883022 [DOI] [Google Scholar]
- 90. Rehman B, Aslam A, Afsheen A, et al. : Ergonomic hazards to dental surgeons: A cross-sectional study. Pakistan Oral Dent J. 2016;39(2):129–132. [Google Scholar]
- 91. Phedy P, Gatam L: Prevalence and associated factors of musculoskeletal disorders among young dentists in Indonesia. Malaysian Orthop J. 2016;10(2):1–5. 10.5704/MOJ.1607.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Cho K, Young CH, Han GS: Risk factors associated with musculoskeletal symptoms in Korean dental practitioners. J. Phys. Ther. Sci. 2016;28(1):56–62. 10.1589/jpts.28.56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Al-Rawi NH, El Khatib H, Rajoub L, et al. : Work-related musculoskeletal pain among different dental specialists in United Arab Emirates. J. Contemp. Dent. Pract. 2016;17(8):639–644. 10.5005/jp-journals-10024-1904 [DOI] [PubMed] [Google Scholar]
- 94. Meisha DE, Alsharqawi NS, Samarah AA, et al. : Prevalence of work-related musculoskeletal disorders and ergonomic practice among dentists in Jeddah, Saudi Arabia. Clin. Cosmet. Investig. Dent. 2019;11:171–179. 10.2147/CCIDE.S204433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Rahman N, Adnan M, Yusoff A, et al. : Work-related musculoskeletal symptoms and coping strategies among dental auxiliaries at hospital universiti Sains Malaysia. Indian J. Dent. Res. 2020;31(1):61–66. 10.4103/ijdr.IJDR_430_18 [DOI] [PubMed] [Google Scholar]
- 96. Aboalshamat, Aboalshamat KT, Aboalshamat KT, et al. : Nordic assessment of occupational disorders among dental students and dentists in Saudi Arabia. J. Int. Soc. Prev. Community Dent. 2020;10(5):561–568. 10.4103/JISPCD.JISPCD_142_20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Kumar M, Pai KM, Vineetha R: Occupation-related musculoskeletal disorders among dental professionals. Med. Pharm. Reports. 2020;93(4):405–409. 10.15386/MPR-1581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Ahmad NS, Abdullah AAA, Thyng OK, et al. : Musculoskeletal Disorders Among Dental Students. J. Res. Med. Dent. Sci. 2020;8(3):32–38. [Google Scholar]
- 99. Bhuvaneshwari S, Shveta J, Kaur J, et al. : Assessment of Various Dental Occupational Hazards and Safety Measures among Dentists of Odisha, India. J. Contemp. Dent. Pract. 2021;21(10):1165–1169. 10.5005/JP-JOURNALS-10024-2885 [DOI] [PubMed] [Google Scholar]
- 100. Senosy SA, Anwar MM, Elareed HR: Profession-related musculoskeletal disorders among Egyptian physicians and dentists. J. Public Heal. 2020;28(1):17–22. 10.1007/s10389-019-01016-0 [DOI] [Google Scholar]
- 101. Puriene A, Aleksejuniene J, Petrauskiene J, et al. : Self-reported occupational health issues among Lithuanian dentists. Ind. Health. 2008;46(4):369–374. 10.2486/indhealth.46.369 [DOI] [PubMed] [Google Scholar]
- 102. Rundcrantz BL, Johnsson B, Moritz U: Pain and discomfort in the musculoskeletal system among dentists. A prospective study. Swed. Dent. J. 1991;15(5):219–228. [PubMed] [Google Scholar]
- 103. Kerosuo E, Kerosuo H, Kanerva L: Self-reported health complaints among general dental practitioners, orthodontists, and office employees. Acta Odontol. Scand. 2000;58(5):207–212. 10.1080/000163500750051755 [DOI] [PubMed] [Google Scholar]
- 104. Zoidaki A, Riza E, Kastania A, et al. : Musculoskeletal disorders among dentists in the Greater Athens area, Greece: risk factors and correlations. J. Public Health (Bangkok). 2013;21(21):163–173. 10.1007/S10389-012-0534-7 [DOI] [Google Scholar]
- 105. Šćepanović D, Klavs T, Verdenik I, et al. : The Prevalence of Musculoskeletal Pain of Dental Workers Employed in Slovenia. Work Heal. Saf. 2019;67(9):461–469. 10.1177/2165079919848137 [DOI] [PubMed] [Google Scholar]