Abstract
Increasing prevalence of obesity (BMI > 30) is a pressing public health issue in the Czech Republic as well as world-wide, affecting up to 2.1 billion people. Increasing trend in the prevalence of obesity in adults and children generates large social costs. The main aim of this study is to estimate both direct and indirect costs of obesity in the Czech Republic. Social costs of obesity are estimated using the cost-of-illness approach. Direct costs (healthcare utilization costs and costs of pharmacotherapy of 20 comorbidities) are estimated using the top-down approach, while indirect costs (absenteeism, presenteeism and premature mortality) are estimated using the human capital approach. In aggregate, the annual costs attributable to obesity in the Czech Republic in 2018 were 40.8 bn CZK (1.6 bn EUR, 0.8% GDP). Direct costs were 14.5 bn CZK (0.6 bn EUR) and accounted for 3.4% of Czech healthcare expenditures. The highest healthcare utilization costs were attributable to type II diabetes (20.6%), ischemic heart disease (18.8%) and osteoarthritis (16.7%). The largest indirect costs were attributable to premature mortality (10 bn CZK/0.39 bn EUR), absenteeism (9.2 bn CZK/0.36 bn EUR) and presenteeism (7.1 bn CZK/0.27 bn EUR). This article demonstrates that obesity is a serious problem with considerable costs. Several preventive interventions should be applied in order to decrease the prevalence of obesity and achieve cost savings.
Keywords: Obesity, Social costs, Cost-of-illness study, Czech Republic
Introduction
Obesity is a serious global health problem which brings substantial economic burden to society. Worldwide rates of obesity have nearly tripled since 1975 and more than 2.1 billion people (30% of global population) suffer from overweight or obesity today. Importantly, obesity is a risk factor for cardiovascular diseases, type II diabetes and some types of cancers, which brings substantial healthcare costs, but also large indirect costs through lost productivity. The global economic impact of obesity is estimated to be $2 trillion (2.8% of global GDP), which is comparable to the impact of armed conflict, smoking or terrorism [1]. In OECD countries, 8.4% of healthcare budget is dedicated to treatment of overweight-related diseases [2].
Obesity has become a pressing concern also with regard to the COVID-19 pandemic. Numerous studies have shown that overweight and obese individuals are more at risk for being COVID-19 positive and have more severe symptoms, leading to significant increase in morbidity and mortality [3]. Moreover, due to many restrictions implemented in order to prevent the spread of COVID-19 (e.g. movement restrictions, social distancing), people lack physical activity which may aggravate current trends in the prevalence of obesity and put even larger strain on the healthcare system [3].
In the Czech Republic, the rates of obesity have been increasing since the 90’s both in adults [4] and children [5]. The goal of this study is to estimate the social costs of obesity, defined as BMI > 30 kg/m2, in the Czech Republic. The cost-of-illness (COI) approach, which views the burden of specific illness as the sum of direct (medical) and indirect costs, is implemented. The resulting social costs of obesity show us how much could be saved if the disease did not exist at all [6]. This study is being novel in estimating the social costs of obesity in the Czech Republic using the COI method, demonstrating what an extreme burden this disease brings to the society.
Literature review
Direct costs
Numerous studies have found that obesity is associated with increased risk of cardiovascular diseases, type II diabetes and cancers [7, 8]. This leads to increased medical costs due to higher use of prescription drugs and outpatient care, or longer hospital stays as a result of post-treatment complications [9–12]. Current literature indicates that the direct costs of obesity are substantial. For instance, research from the USA indicates that obesity is associated with 36% increase in inpatient and outpatient spending and 77% increase in medication costs [13]. Several studies also show that medical costs increase proportionally with BMI [14–16].
Table 4 summarizes literature focusing on direct costs of obesity. The studies vary in the amount of comorbidities included, which ranges from 4 to 18. The share of direct costs of obesity on total healthcare costs ranges from 2.3% in Sweden [16] to 6.7% in Canada [17]. In the Czech Republic, the direct costs of obesity were estimated as 7.6 billion CZK (excluding the costs of pharmacotherapy) in 2013, which accounted for 3.45% of total healthcare costs [18]. Earlier estimate from 2007 was 9.5 billion CZK (5.2% of healthcare costs), out of which 2.6 billion CZK were costs of pharmacotherapy [19]. In general, the share of costs of overweight and obesity on total healthcare costs ranges between 2 and 8% [2].
Table 4.
Literature review—direct costs
| n | Country | Method | Number of comorbidities | Population | Normal weight | Overweight | Obesity | % of healthcare costs | |
|---|---|---|---|---|---|---|---|---|---|
| Arterburn et al. [12] | 16,262 | USA | Econometric approach | N/A | 18+ | $2424 | $2664 | $2984–4399 | N/A |
| Finkelstein et al. [22] | 20,329 | USA | Econometric approach | N/A | 18–64 women | 0 (base) | $495 | $1071–1549 | N/A |
| 18–64 men | $169 | $392–1591 | |||||||
| Cawley & Meyerhoefer [10] | 23,689 | USA | Econometric approach | NA | 11–64 | $1763 | $4458 | 20.6% | |
| Kleinman et al. [61] | 72,778 | USA | Econometric approach | N/A | 18+ women | $4 142 | $4583 | $6328 | N/A |
| 18+ men | $2861 | $3378 | $4309 | ||||||
| An [62] | 125,955 | USA | Econometric approach | N/A | 18+ women | 0 (base) | N/A | $1525 | N/A |
| 18+ men | $1160 | ||||||||
| Borg et al. [16] | 23,365 | Sweden | Econometric approach | N/A | 30–60 women | 0 (base) | $101 million | 2.3% | |
| (total costs) | 30–60 men | $169 million | |||||||
| Sander & Bergemann [63] | N/A | Germany | Top-down approach | 4 | 25+ | N/A | N/A | €2 billion | N/A |
| Konnopka et al. [11] | N/A | Germany | Top-down approach | 16 (W), 17 (M) | 18+ | N/A | €4 854 million | 2.1% | |
| Lehnert et al. [24] | N/A | Germany | Top-down approach | 16 (W), 17 (M) | 18+ | N/A | €8 647 million | 3.27% | |
| Schmid et al. [60] | N/A | Switzerland | Top-down approach | 18 | 15+ | N/A | CHF 1 077–1 615 million | 2.3–3.5% | |
| Kang et al. [25] | 1.9 mil | Korea | Top-down approach | 7 | 20+ | N/A | $270.5 million | $810.5 million | 3.7% |
| Dee et al. [23] | N/A | Northern Ireland | Top-down approach | 16 | N/A | N/A | €127 million | 2.8% | |
| N/A | Republic of Ireland | €437 million | 2.7% | ||||||
| Krueger et al. [17] | N/A | Canada | Top-down aproach | 16 | 12+ women | N/A | $4.3 billion | $7.6 billion | 6.7% |
| 13 | 12+ men | $4.8 billion | $6.6 billion | ||||||
| Hodycová [19] | N/A | Czech Republic | Top-down approach | 7 | 18+ | N/A | N/A | 9.5 billion CZK | 5.2% |
| Tuzarová [18] | N/A | Czech Republic | Top-down approach | 18 (W), 16 (M) | 18+ | N/A | N/A | 7.6 billion CZK | 3.45% |
| Effertz et al. [9] | 146,000 | Germany | Bottom-up approach | NA | 15+ | N/A | N/A | €29.39 billion | 7.9% |
Range for obesity class I–III. Normal weight is classified as BMI < 27, overweight: 27 BMI < 30, obesity: BMI 30. Values are converted from SEK by a rate US$1 = SEK8. In Korea, classification of obesity according to BMI is different than in Europe (Overweight: 23–24.9 kg/m; Obesity I: 25–29.9 kg/m2; Obesity II: 30 kg/m) . Cardiovascular diseases are taken as one comorbidity. 6.7 billion healthcare utilization, 2.6 billion pharmacotherapy. Percentage of healthcare costs stated in [2]
Indirect costs
Absenteeism
Absenteeism refers to absence from work due to illness. The rate of absenteeism due to illness varies across countries, but Czech Republic has one of the highest rates in Europe, reaching on average 16.3 days missed in 2018 [20].
Table 5 summarizes literature which includes the costs of absenteeism associated with obesity. Almost all studies find that the costs of absenteeism are significantly larger for obese workers compared with normal-weight workers. However, the magnitude of the difference varies across studies, which can be caused by country, data or methodology differences. Usually, absenteeism is compared between obese and normal weight individuals (e.g. [9, 21, 22]), but some studies compare BMI > 25 (thus including overweight) with normal weight (e.g. [11, 23–25]), which makes some results uncomparable. Studies which examine absenteeism across three obesity classes show that the rates of absenteeism increase with BMI [21, 22, 26].
Table 5.
Literature review—absenteeism
| n | Country | Measurement unit | Population | Normal weight | Overweight | Obesity | |
|---|---|---|---|---|---|---|---|
| Konnopka et al. [11] | N/A | Germany | Number of days/year | 15+ | 0 (base) | 5,875,022 days | |
| Total yearly costs | €646 million | ||||||
| Lehnert et al. [64] | 7990 | Germany | Yearly costs per person (days absent/year) | 18–65 women | 0 (base) | €284 (3.64 days) | €405 (5.19 days) |
| Yearly costs per person (days absent/year) | 18–65 men | N/A (N/A) | €367 (3.48 days) | ||||
| Total yearly costs | 18–65 | €2.18 billion | |||||
| Lehnert et al. [24] | N/A | Germany | Number of days/year | 15+ | 0 (base) | 11,478,208 days | |
| Total yearly costs | €1.28 billion | ||||||
| Effertz et al. [9] | 146 000 | Germany | Total yearly costs | 15+ | 0 (base) | N/A | €3.87 billion |
| Finkelstein et al. [22] | 25,427 | USA | yearly costs per person (days absent/year) | 18–64 women | $0 (base)/(3.4 days) | $93 (3.9 days) | $302–805 (5.2–8.2 days) |
| yearly costs per person (days absent/year) | 18–64 men | $0 (base)/(3 days) | $6 (3 days) | $70–436 (3.5–5 days) | |||
| Finkelstein et al. [28] | 24,140 | USA | Yearly costs per person (days absent/year) | 18+ women | 0 (base) | $147 (1.1 days) | $407–1262 (3.1–9.4 days) |
| Yearly costs per person (days absent/year) | 18+ men | $85 (0.5 days) | $277–1026 (1.6–5.9 days) | ||||
| Dall et al. [21] | 225 mil | USA | Yearly costs per person | 18+ | 0 (base) | $47 | $104–264 |
| Total yearly costs | $3.5 billion | $3.9–6.8 billion | |||||
| Andreyeva et al. [26] | 14 975 | USA | yearly cost per person (days absent/year) | 18+ | 0 (base)/(4.25 days) | N/A (4.48 days) | $216–348 (5.42–6.13 days) |
| Total yearly costs | 0 (base) | N/A | $8.65 billion | ||||
| Kleinman et al. [61] | 72,778 | USA | Yearly costs per person (days absent/year) | 18+ women | $890 (4.09 days) | $1046 (5.02 days) | $1175 (5.81 days) |
| Yearly costs per person (days absent/year) | 18+ men | $615 (2.66 days) | $640 (2.81 days) | $792 (3.7 days) | |||
| Kang et al. [25] | 1.9 mil | Korea | Total yearly costs | 20+ women | 0 (base) | $29.5 million | |
| 20+ men | $44.4 million | ||||||
| Dee et al. [23] | N/A | Northern Ireland | Total yearly costs | N/A | 0 (base) | €215 million | |
| Republic of Ireland | Total yearly costs | €136 million | |||||
| Neovius et al. [65] | 45,920 | Sweden | Lifetime productivity losses | 19–65 men | €12,500 | €15,000 | €16,100 |
| Tuzarová [18] | N/A | Czech Republic | Number of days/year | 24–60 women & | 0 (base) | N/A | 3.7 million days |
| Total yearly costs | 25–64 men | 3.2 billion CZK | |||||
€481 million without unpaid work. €1.37 billion women and €0.81 billion men. €858 million without unpaid work. Range for obesity class I–III . eNormal weight: BMI ; overweight: BMI and
Presenteeism
Presenteeism refers to reduced productivity at work due to presence of mental or physical health complications [27]. There is growing evidence that the costs of presenteeism associated with chronic conditions largely exceed the costs of absenteeism [28–30].
To the best of our knowledge, presenteeism related to obesity has not been measured in the Czech Republic thus far, therefore, our estimates are based on current literature, which is summarized in Table 6. All the studies find that obesity is positively associated with presenteeism, but the extent differs across studies. Compared with normal weight individuals, the estimates range from 1.1 to 3.8 more days lost [31–34] and reach 22.7–33 days lost for obesity class III [28, 35].
Table 6.
Literature review—presenteeism
| n | Country | Measurement unit | Gender | Normal weight | Overweight | Obesity | |||
|---|---|---|---|---|---|---|---|---|---|
| Class I | Class II | Class III | |||||||
| Boles et al. [32] | 2264 | USA | Productivity loss (%) | Both | 5.6 | 7.1 | |||
| Productivity loss (days) | 14.0 | 17.6 | |||||||
| Pelletier et al. [66] | 500 | USA | Productivity loss (%) | Both | 4.7 | 7.9 | |||
| Productivity loss (days) | 11.8 | 19.8 | |||||||
| Burton et al. [33] | 28,375 | USA | Productivity loss (%) | Both | 0 (base) | N/A | 1.5 | ||
| Productivity loss (days) | N/A | 3.8 | |||||||
| Ricci and Chee [34] | 7000 | USA | Weekly hours lost | both | 4.2 | 4.2 | 4.8 | ||
| Productivity loss (days) | 26.3 | 26.3 | 30 | ||||||
| Gates et al. [67] | 341 | USA (KY) | Productivity loss (%) | Both | 3.3 | 3.1 | 2.5 | 4.2 | |
| Productivity loss (days) | 8.1 | 7.8 | 6.1 | 10.4 | |||||
| Finkelstein et al. [28] | 10,262 | USA | Productivity loss (days) | Women | 0 (base) | 0.9 | 6.3 | 11.0 | 22.7 |
| 13 878 | Men | − 3.3 | 2.3 | 5.8 | 21.9 | ||||
| Goetzel et al. [31] | 10,026 | USA | Productivity loss ($) | Both | 1200 | 1402 | 1416 | ||
| Productivity loss (days) | 5.8 | 6.8 | 6.9 | ||||||
| Kirkham et al. [68] | 17,089 | USA | Productivity loss (days) | Both | 4.2 | N/A | N/A | 4.7 | |
| Gupta et al. [35] | 31,653 | FRA, DE, IT | Productivity loss (%) | Both | 16 | 15.6 | 17.6 | 20.4 | 29.2 |
| ESP, UK | Productivity loss (days) | 40 | 39.1 | 44.0 | 50.9 | 73.0 | |||
Productivity loss in days is annual; conversion from productivity loss in percent to productivity loss in days is done assuming 250 working days per year.
Compares normal weight against BMI<18.5 or >24.9
Compares BMI categories with BMI<24.9 (normal weight + underweight)
The study uses average wage rate $25.67/h
Premature mortality
Excess weight is associated with substantial increases in early mortality [36]. Obesity and its related diseases are estimated to reduce life expectancy by 0.9–4.2 years [2], which leads to large productivity losses. Current literature on the costs of premature mortality related to obesity is summarized in Table 7. The estimates of number of years lost due to obesity-related premature mortality vary across studies and substantially increase with BMI [37]. In the Czech Republic, overweight-attributable reduction in life expectancy is estimated to be 3.5 years [38] and in 2013, the obesity-related costs due to premature mortality were evaluated as 1.2 billion CZK [18]. In general, the studies show that the costs are larger for men than women, typically due to higher wages, higher retirement age or higher prevalence of obesity.
Table 7.
Literature review—premature mortality
| n | Country | Measurement unit | Discount rate | Population | Normal weight | Overweight | Obesity | |
|---|---|---|---|---|---|---|---|---|
| Konnopka et al. [11] | N/A | Germany | Annual number of deaths | 5% | 15+ | 0 (base) | 36,653 | |
| Total productivity lost | €3381 million | |||||||
| Lehnert et al. [64] | N/A | Germany | Annual number of deaths | 5% | 15+ | 0 (base) | 47,964 | |
| Total productivity lost | €5669 million | |||||||
| Effertz et al. [9] | 146,000 | Germany | Annual number of deaths | 2% | 15+ | 0 (base) | N/A | 101,886 |
| Amount of lost years | 2072 million | |||||||
| Total productivity lost | €23.12 billion | |||||||
| Fontaine et al. [37] | 23 659 | USA | Years of life lost per person | N/A | 15–75 women | N/A | <1 year | 3–8 years |
| 15–75 men | <1 year | 3–13 years | ||||||
| Dall et al. [21] | 225 million | USA | Total productivity lost | 3% | 18+ | 0 (base) | $1.9 billion | $6.9–25.9 billion |
| Per capita productivity lost | $25 | $182–1006 | ||||||
| Borg et al. [16] | 23,365 | Sweden | Total productivity lost | 3% | 30–60 women | 0 (base) | $1.15 million | $64.0 million |
| 30–60 men | 3.3 million | 298.5 million | ||||||
| Neovius et al. [65] | 45,920 | Sweden | Per capita productivity losses | 3% | 18+ men | €25,100 | €31,800 | €52,100 |
| Dee et al. [23] | N/A | Northern Ireland | Total productivity lost | 4% | 18–75 | 0 (base) | €147 million | |
| Republic of Ireland | 18–75 | €593 million | ||||||
| Kang et al. [25] | 1.9 million | Korea | Total productivity lost | 6% | 20+ women | 0 (base) | $70 million | |
| 20+ men | $374 million | |||||||
| Tuzarová [18] | N/A | Czech Republic | Amount of lost years | 1.5% | 25–60 women | 0 (base) | N/A | 5440 years |
| Total productivity lost | 395 million CZK | |||||||
| Amount of lost years | 25–64 men | 2290 years | ||||||
| Total productivity lost | 800 million CZK | |||||||
Range for different BMI groups, BMI = 24 is used as reference category
Range for obesity class I–III
Estimates from the Czech Republic
Only a few studies estimated the social costs of obesity in the Czech Republic. In 2007, the direct costs of obesity were estimated as 9.5 billion CZK [19]. Another estimate which is largely based on other (foreign) studies estimated direct and indirect costs of obesity to be 20.3–42.5 billion CZK and 17.2–37.8 billion CZK, respectively [39]. In 2013, direct and indirect costs of obesity were quantified as 12.1 billion CZK and corresponded to 0.3% of GDP in 2013 [18].
Data and methodology
Data
Table 1 summarizes the data used in the baseline model. The healthcare utilization costs and costs of pharmacotherapy in 2018 are obtained from the General Health Insurance Fund (GHIF) jointly for men and women [40], which are extrapolated to the whole population.1 The data for computation of costs of absenteeism and premature mortality in 2018 are obtained from the Institute for Health Information and Statistics (IHIS), specifically from the Information System Incapacity for work [41] and the Information System Deaths [42]. For each comorbidity, they are available for 5-year age groups for men and women separately. The estimation of costs of presenteeism is based on literature review.
Table 1.
Data sources
| Measure | Data source | Year |
|---|---|---|
| Direct costs | ||
| Healthcare utilization | General Health Insurance Fund | 2018 |
| Pharmaceuticals | General Health Insurance Fund | 2018 |
| Indirect costs | ||
| Absenteeism | Information System Incapacity for Work | 2018 |
| Presenteeism | Literature review | NA |
| Premature mortality | Information System Deaths | 2018 |
| Other sources | ||
| Prevalence of obesity | NCD-RisC Database | 2016 |
| Relative risks | Guh et al. | 1994–2006 |
| Dobbins et al. | 1985–2011 | |
| Average salary | Czech Statistical Office | 2018 |
| Unpaid work | Czech Academy of Sciences | 2015 |
| Value of unpaid work | Average Earnings Information System | 2018 |
| Life expectancy | Czech Statistical Office | 2018 |
| Employed population | Eurostat | 2018 |
Prevalence of obesity in the Czech Republic is taken from the NCD Risk Factor Collaboration (NCD-RisC) study with the most recent data being from 2016. This study provides the prevalence of obesity in 200 countries based on data measured by physicians. The age-standardised prevalence of obesity in population 20 years and older is 27.3% for men and 26.5% for women [43]. Relative risks are derived from Guh et al. [7] and Dobbins et al. [8]. These studies provide a review of existing studies that identify statistically significant comorbidities of obesity, i.e. the diseases that are more likely to occur in obese population vs. normal weight population. Guh et al. (2009) conduct a review of studies coming predominantly from the USA (55%) and Europe (40%), and Dobbins et al. (2013) conduct a review of studies conducted mainly in the USA, Norway, Sweden or Japan.
Paid work is valued by the average gross salary for each gender and age group in 2018 reported by the Czech Statistical Office (CSO) [44]. The average daily amount of hours spent doing housework was estimated to be 3 h for women and 2 h for men [45]. The value of unpaid work is approximated by the average wage of cleaning services workers in 2018 (the average hourly wage is 87 CZK/h [46]). Life expectancy in 2018 is derived from the CSO [47] and the number of employed people aged 25-64 years in 2018 is obtained from Eurostat [48].
Methodology
Social costs of obesity are estimated using the cost-of-illness (COI) approach, which views the economic burden of disease as the sum of several categories of direct and indirect costs [49]. There are two types of approaches within the COI methodology: prevalence and incidence approach. The prevalence approach is used in our analysis as it assesses the current economic burden of illness [50]. For more details on methodology, please refer to Appendix B.
Direct costs
Direct costs refer to medical and non-medical expenditures related to obesity-related diseases and are estimated using the top-down approach. This approach uses population attributable fraction (PAF) which attributes part of healthcare costs to obesity. Due to data constraints specific to the Czech Republic, the computation of direct costs is divided into healthcare utilization costs and costs of pharmaceuticals.
Based on two studies [7, 8], 20 comorbidities of obesity and their relative risks RR (how much more likely will these diseases occur in obese individuals compared to normal weight) are identified. Using RR and prevalence (p) of obesity in the Czech Republic from the NCD RisC study, (i.e. what portion of comorbidity’s costs are due to obesity) is computed:
Healthcare costs attributable to obesity (HC) are computed as:
where is population attributable fraction for comorbidity c and are the healthcare utilization costs associated with comorbidity c.
Similar approach is taken in estimating the costs of pharmacotherapy attributable to obesity. Based on two studies [19, 23], five groups of pharmaceuticals are identified (e.g. pharmaceuticals used in the cure of diabetes mellitus, cardiovascular diseases etc.) along with the specific Anatomical Therapeutic Chemical (ATC) classification codes (see Appendix B for more details). Pharmaceutical costs attributable to obesity (PC) are computed as:
where are the pharmaceutical costs of ATC group related to a comorbidity c.
Indirect costs
Indirect costs refer to the value of lost production due to morbidity and mortality, which we estimate using the Human capital approach (HCA). We include the costs of absenteeism, presenteeism and premature mortality. The value of both paid work () and unpaid work () is included in the costs, monetized by average gross salary () and average wage of houseworker (), respectively:
where refers to age- (a) and gender- (g) specific evaluation of productivity lost. specific for age (a), comorbidity (c) and gender (g) is used to determine the obesity-attributable productivity lost, because the data are stratified by 5-year age groups and genders.
Absenteeism refers to missed days at work due to illness. The number of days absent () due to obesity related comorbidities (c) for age (a) and gender (g) is multiplied by to find the number of days absent from work due to obesity ():
The indirect costs due to obesity-related absenteeism () are computed as:
Presenteeism describes lower productivity while present at work. Due to unavailability of data on obesity-related rates of presenteeism in the Czech Republic, we estimate the costs based on literature review, assuming that on average, obese individuals miss 2 days of work due to presenteeism. In case of presenteeism, we only distinguish the costs for each gender g, disregarding their age as we do not have data for it. The indirect costs due to obesity-related presenteeism () are computed as:
where is the number of employed people in working-age population and is the number of obese people in labour force ( is gender-specific prevalence of obesity in working-age population, i.e. 25–64 years old), PL stands for productive days lost due to presenteeism and is the gender-specific valuation of paid and unpaid work.
To estimate the value lost due to premature mortality, we use the data on number of deaths due to each comorbidity of obesity stratified by gender and age. The present value of future lost earnings (NPV) is computed using a discount rate (i) which is 3% in the baseline scenario:
where FV stands for future value and t is the amount of years lost.
The indirect costs due to obesity-related premature mortality () are computed as:
where stands for age-, comorbidity- and gender-specific number of deaths. Only half of the productivity is accounted for in the first year () to correct for different occurrences of death during the year. The productive years (i.e. before retirement age ret) are monetized by the value of paid and unpaid work, while the years after retirement until life expectancy age exp are monetized by the value of unpaid work only. Only part of these costs is attributable to obesity, which is computed using the .
Sensitivity analysis
In sensitivity analysis, we test the robustness of results by varying several parameters of the model (more details are available in Sect. B.3):
PAF are recomputed using the 95% confidence interval of relative risks.
PAF are recomputed using the relative risks from the Dynamo project.
Prevalence data from the EHES/EHIS study from 2014 [51, 52] are used.
Discount rate of 1% and 5% is used for computing the costs of premature mortality.
Unpaid work is completely excluded from total costs.
Presenteeism is computed for missing 1, 3 and 4 days of work (baseline value is 2 days).
Results
Direct costs
Healthcare utilization costs
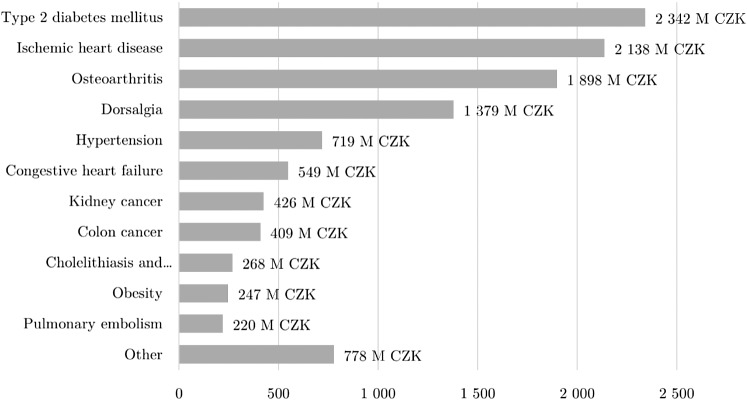
Table 9 lists the relevant comorbidities of obesity along with the ICD-10 codes and PAF computed based on the prevalence of obesity in the Czech Republic2 and relative risks [7, 8]. Total costs of healthcare utilization due to obesity are reported in Table 10 and amount to 11.4 billion CZK (see Fig. 1). The largest portion of these costs is due to type II diabetes mellitus (2.3 billion CZK), ischemic heart disease (2.1 billion CZK) and osteoarthritis (1.9 billion CZK).
Table 9.
Comorbidities of obesity
| Diagnosis | ICD-10 code | PAF (%) and 95% CI | |
|---|---|---|---|
| Women | Men | ||
| Asthma | J45 | 18.0 (9.2, 27) | 10.6 (3.7, 17.9) |
| Dorsalgia | M54 | 33.7 (26.3, 41) | 33.4 (26.0, 40.7) |
| Type 2 diabetes mellitus | E11, E13, E14 | 76.2 (69.3, 81.8) | 61.4 (55.7, 66.5) |
| Ischemic heart disease | I20–I25 | 37.1 (33.7, 40.5) | 16.6 (12.4, 33.4) |
| Leukemia | C91–C95 | 8.2 (2.2, 14.4) | – |
| Malignant melanoma | C43, D03 | – | 6.7 (1.9, 11.7) |
| Stroke | I69.4, I64 | 12.1 (7.0, 17.2) | 12.4 (8.4, 16.6) |
| Obesity | E66.0, E66.2, E66.8, E66.9, E65 | 100 | 100 |
| Cholelithiasis and cholecystitis | K81, K80 | 27.0 (4.6, 50.0) | 10.6 (1.1, 21.0) |
| Osteoarthritis | M15–M19 | 21.2 (19.8, 22.6) | 46.9 (32.7, 59.9) |
| Pulmonary embolism | I26 | 41.3 (31.1, 51.1) | 41.0 (30.8, 50.8) |
| Endometrial cancer | C54.1, C55, D07.0, D39.0 | 38.4 (34.9, 41.8) | – |
| Kidney cancer | C64, C65, C66, D30.0 - D30.2 | 31.5 (28.1, 34.8) | 18.5 (14.4, 22.5) |
| Breast cancer | D05, D24, D48.6, C50 | 3.5 (1.4, 5.8) | – |
| Pancreatic cancer | C25, D01.7, D13.6, D13.7 | 14.4 (4.6, 25.2) | 26.3 (15.2, 37.7) |
| Colon cancer | C18, D12.0–D12.6 | 15.6 (12.7, 18.5) | 20.8 (14.0, 27.8) |
| Ovarian cancer | C56, D27, D39.1 | 7.3 (5.3, 9.2) | – |
| Gallbladder cancer | C23, C24, D13.5 | 18.7 (8.2, 29.6) | 11.5 (4.5, 19.0) |
| Congestive heart failure | I50 | 18.0 (1.9, 35.4) | 17.9 (6.2, 30.5) |
| Hypertension | I10–I15 | 28.5 (14.2, 42.8) | 18.9 (12.4, 25.5) |
Table 10.
Healthcare utilization costs
| Diagnosis | Costs (95% CI) | % of total costs |
|---|---|---|
| Type 2 diabetes mellitus | 2342.4 (2128.3, 2526.7) | 20.60% |
| Ischemic heart disease | 2137.8 (1833.5, 2942.9) | 18.80% |
| Osteoarthritis | 1898.0 (1462.8, 2297.7) | 16.69% |
| Dorsalgia | 1378.8 (1074.9, 1680.6) | 12.12% |
| Hypertension | 718.6 (403.2, 1037.7) | 6.32% |
| Congestive heart failure | 548.9 (124.7, 1008.0) | 4.83% |
| Kidney cancer | 426.2 (362.2, 488.3) | 3.75% |
| Colon cancer | 408.7 (300.2, 519.3) | 3.59% |
| Cholelithiasis and cholecystitis | 268.3 (40.2, 506.1) | 2.36% |
| Obesity | 246.9 (246.9, 246.9) | 2.17% |
| Pulmonary embolism | 220.1 (165.6, 272.6) | 1.94% |
| Asthma | 191.4 (86.4, 301.0) | 1.68% |
| Breast cancer | 138.9 (54.6, 229.4) | 1.22% |
| Stroke | 130 (81.9, 179.7) | 1.14% |
| Pancreatic cancer | 89.0 (43.3, 137.6) | 0.78% |
| Endometrial cancer | 83.1 (75.6, 90.5) | 0.73% |
| Leukemia | 64.9 (17.3, 113.5) | 0.57% |
| Ovarian cancer | 43.5 (31.7, 54.7) | 0.38% |
| Gallbladder cancer | 20.4 (8.6, 32.9) | 0.18% |
| Malignant melanoma | 17.1 (4.9, 29.9) | 0.15% |
| Total | 11,373.0 (8546.9, 14,696.2) | 100% |
Values are in millions CZK
Fig. 1.
Healthcare utilization costs
Source: author’s computations
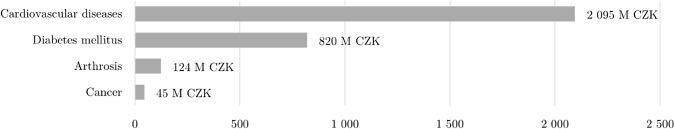
Costs of pharmacotherapy
Figure 2 summarizes the costs of pharmacotherapy. Table 11 shows the ATC groups included in the study and the costs attributable to obesity [19, 23]. Drugs used in diabetes make up the largest part of pharmacotherapy costs (820 million CZK), followed by antithrombotic agents (595 million CZK) used for the cure of cardiovascular diseases and agents acting on the renin-angiotensin system (573 million CZK) used for the cure of cancer. Total pharmacotherapy costs attributable to obesity are 3.1 billion CZK.
Fig. 2.
Costs of pharmacotherapy
Source: author’s computations
Table 11.
Costs of pharmacotherapy
| ATC classification | ATC code | Costs (95% CI) |
|---|---|---|
| For the cure of obesity | ||
| Antiobesity preparations, excluding diet products | A08 | 0 (0, 0) |
| For the cure of diabetes mellitus | ||
| Drugs used in diabetes | A10 | 819.8 (744.9, 884.3) |
| For the cure of cardiovascular diseases | ||
| Antithrombotic agents | B01 | 595.2 (363.3, 906.2) |
| Cardiac therapy | C01 | 83.7 (51.1, 127.4) |
| Antihypertensives | C02 | 95.9 (53.8, 138.4) |
| Diuretics | C03 | 101.4 (56.9, 146.4) |
| Beta blocking agents | C07 | 128.4 (72.1, 185.4) |
| Calcium channel blockers | C08 | 86.5 (48.5, 124.9) |
| Agents acting on the renin-angiotensin system | C09 | 573.3 (321.7, 827.8) |
| Lipid modifying agents | C10 | 430.4 (262.7, 655.3) |
| For the cure of cancer | ||
| Antineoplastic agents | L01 | 45.4 (32, 59.2) |
| For the cure of arthrosis | ||
| Anti-inflammatory and antirheumatic products | M01 | 123.6 (96.3, 150.6) |
| Total | 3083.2 (2103.1, 4206.9) |
Indirect costs
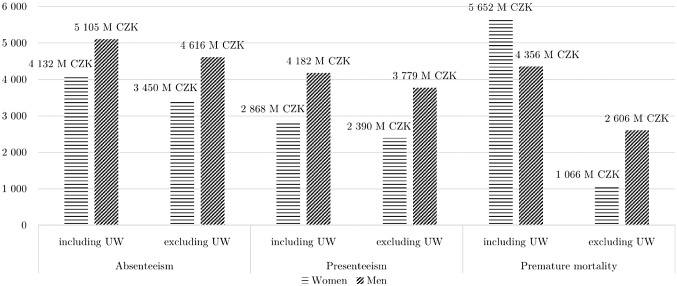
The indirect costs are visually summarized in Fig. 3.
Fig. 3.
Summary of indirect costs
Source: author’s computations; UW unpaid work
Absenteeism
2.8 million days were lost due to obesity in men and 2.6 million days in women in 2018. Total costs of absenteeism are 9.2 billion CZK (4.1 billion CZK for women and 5.1 billion CZK for men) and 8.1 billion CZK (3.5 billion CZK for women and 4.6 billion CZK for men) after excluding the value of unpaid work. The results are summarized in Table 12.
Table 12.
Results—absenteeism
| Days lost | Including unpaid work | Excluding unpaid work | |
|---|---|---|---|
| Women (25–64) | 2,616,984 | 4131 | 3450 |
| Men (25–64) | 2,818,935 | 5105 | 4616 |
| Total | 5,435,919 | 9237 | 8067 |
Values are in millions CZK
Presenteeism
The baseline value for days lost in our model is 2 days of work lost, which is associated with costs of 7.1 billion and 6.2 billion after excluding the value of unpaid work. The costs of presenteeism for 1, 3 and 4 days lost amount to 3.5, 10.6 and 14.1 billion CZK respectively (3.1, 9.3 and 12.3 billion CZK, respectively, after excluding the value of unpaid work). The costs of presenteeism are summarized in Table 13.
Table 13.
Results—presenteeism
| Including unpaid work | Excluding unpaid work | |||||||
|---|---|---|---|---|---|---|---|---|
| Days lost | 1 day | 2 days | 3 days | 4 days | 1 day | 2 days | 3 days | 4 days |
| Women | 1434 | 2868 | 4302 | 5736 | 1195 | 2390 | 3585 | 4780 |
| Men | 2091 | 4182 | 6273 | 8364 | 1889 | 3779 | 5668 | 7558 |
| Total | 3525 | 7050 | 10,575 | 14,100 | 3084 | 6169 | 9253 | 12,338 |
Values are in millions CZK
Premature mortality
In 2018 women lost 72, 670 years due to obesity, from which 2947 years were productive years. Men lost in total 89, 850 years due to obesity, from which 8737 years were productive years. The reason why the productive years make such a small part of total years lost due to obesity is that most people die due to obesity-related diseases after retirement. Using the discount rate of 3%, the costs of premature mortality due to obesity are 10 billion CZK, including unpaid work. The costs are higher for women even though the amount of productive years lost is lower compared to men because women lose more unproductive years than men. After excluding the unpaid work, the costs are 3.7 billion CZK. Table 14 shows the results for different discount rates.
Table 14.
Results—premature mortality
| Including unpaid work | Excluding unpaid work | |||||
|---|---|---|---|---|---|---|
| Discount rate | 1% | 3% | 5% | 1% | 3% | 5% |
| Women | 6288 | 5652 | 5149 | 1215 | 1066 | 949 |
| Men | 4951 | 4356 | 3892 | 2948 | 2606 | 2335 |
| Total | 11,239 | 10008 | 9041 | 4163 | 3672 | 3285 |
Values are in millions CZK
Summary of results
Total costs of obesity in the Czech Republic for the year 2018 are summarized in Table 2. In total, they amount to 40.8 billion CZK, which corresponds to 0.8% of GDP in 2018 [53]. The indirect costs account for majority of the costs: 26.3 billion CZK (65%), whereas the direct costs are 14.5 billion CZK (35%), which accounts for 3.4% of total healthcare costs in 2018.3
Table 2.
Summary of results
| CZK | % of total costs | |
|---|---|---|
| Direct costs | 14,456.2 | 35.5 |
| Healthcare utilization | 11,373.0 | 27.9 |
| Pharmacotherapy | 3083.2 | 7.6 |
| Indirect costs | 26,295.5 | 64.5 |
| Absenteeism | 9237.0 | 22.7 |
| Presenteeism | 7050.1 | 17.3 |
| Premature mortality | 10,008.4 | 24.6 |
| Total | 40,751.7 | 100.0 |
Values are in millions CZK
Sensitivity analysis
Table 3 shows the change in costs attributable to obesity as the key parameters are varied. Total costs range between 32.3 billion CZK (− 20.8% from baseline values) and 51.1 billion CZK (+25.5% from baseline values). The largest changes result from using the low and high relative risks values (95% CI). The overall costs decrease by 8.4% when the 2014 data on prevalence of obesity are used.
Table 3.
Sensitivity analysis
| Direct costs | % change | Indirect costs | % change | Total costs | % change | |
|---|---|---|---|---|---|---|
| Baseline | 14,456.2 | – | 26,295.5 | – | 40,751.7 | – |
| Relative risks low values | 10,650.0 | − 26.3% | 21,610.8 | − 17.8% | 32,260.8 | − 20.8% |
| Relative risks high values | 18,902.1 | 30.8% | 32,231.2 | 22.6% | 51,133.2 | 25.5% |
| Relative risks Dynamo project | 12,975.7 | − 0.2% | 24,103.2 | − 8.3% | 37,078.9 | − 9.0% |
| EHIS/EHES prevalence (2014) | 13,088.1 | − 9.5% | 24,260.7 | − 7.7% | 37,348.8 | − 8.4% |
| Discount rate 1% | 14,456.2 | 0% | 27,526.2 | 4.7% | 41,982.4 | 3.0% |
| Discount rate 5% | 14,456.2 | 0% | 25,327.9 | − 3.7% | 39,784.1 | − 2.4% |
| Excluding unpaid work | 14,456.2 | 0% | 17,907.6 | − 31.9% | 32,363.8 | − 20.6% |
| Presenteeism 1 day | 14,456.2 | 0% | 22,770.5 | − 13.4% | 37,226.7 | − 8.7% |
| Presenteeism 3 days | 14,456.2 | 0% | 29,820.6 | 13.4% | 44,276.8 | 8.7% |
| Presenteeism 4 days | 14,456.2 | 0% | 33,345.6 | 26.8% | 47,801.8 | 17.3% |
Values are in millions CZK
Discussion
The goal of this study was to estimate the social costs of obesity in the Czech Republic in 2018. The resulting costs are equal to 40.8 billion CZK, which corresponds to 0.8% of GDP. This result should be taken as a lower-bound estimate of the costs of obesity as the prevalence data come from 2016, we use a very conservative estimate for the costs of presenteeism, we exclude intangible costs and use the top-down approach. The comparison of results across studies is complicated due to differences in methodological approach. A study from Germany, which is socio-economically similar to the Czech Republic, estimated the costs of overweight (BMI > 25) in 2008 using a similar approach as 0.5% of GDP [24]. This estimate is lower than ours mainly because it uses older data: both the prevalence of obesity and healthcare costs have increased largely since 2008.
A new OECD study estimates the burden of overweight and obesity (BMI > 25) in 52 different countries to be 1.6–5.3% of GDP [2]. The specific estimate for the Czech Republic is 4% of GDP, which is much higher than our estimate. This may have several reasons. Our study focuses purely on obesity (BMI > 30), whereas the OECD study also includes overweight (i.e. BMI > 25). The prevalence of overweight is much higher than of obesity in the Czech Republic: 70% for men and 55% for women. Furthermore, the OECD study uses different methodological approach (a microsimulation model vs. a country-level COI study) and data sources (often derived from other countries or studies), so the results are not directly comparable (see Appendix C for more details).
The direct costs of obesity are 14.5 billion CZK, corresponding to 3.4% of healthcare expenditures. International studies estimate the impact of overweight and obesity on health expenditures in the range of 2–7.9% [2]. The estimate from Germany from 2008, which has the same healthcare financing scheme, is 3.27% of healthcare expenditures [24]. The indirect costs are 26.3 billion CZK, which exceeds previous estimates from the Czech Republic due to inclusion of presenteeism, unpaid work, use of gross salaries and rising prevalence of obesity.
Cost-of-illness methodology is the most common measurement approach to estimate the burden of disease, but it has certain drawbacks. A variety of approaches within the COI methodology can be taken, which limits the comparability of results across studies. Additionally, it measures the value of individual’s life only in terms of the production evaluated by average wage, ignoring other dimensions of illness and death, such as pain and lower quality of life [50]. However, when performed with a clear explanation, COI studies represent an important analytic tool in public health policy [55].
In this study, HCA is used to estimate the indirect costs of obesity. This method has been mainly criticised for assuming full employment in the economy, which relates mainly to the costs of absenteeism where every day the worker misses is regarded as lost production. However, the approach disregards the fact that the work can be made up by the worker after his/her return, or it can be done by his/her colleagues [50]. The friction cost approach (FCA) solves this drawback and counts the productivity losses only for the time it takes to replace the absent worker. The HCA is further criticised for evaluating the costs based on age- and gender-specific wages, implying that people earning lower wages are less valuable for the society. Willingness-to-pay approach mitigates this problem, however, it is not often employed as it requires extensive surveys of preferences and the results highly depend on the individuals’ subjective responses to hypothetical questions [55].
There are several limitations in our study, mainly related to availability of relevant data. Firstly, we use the data on prevalence of obesity from 2016, even though we estimate the costs of obesity in 2018 as no more recent data stratified by gender and age groups are available. The results of the EHES 20194 survey suggest increasing trends of obesity, which would imply even larger social costs [56]. Secondly, the relative risks used in computations of population attributable fractions (PAF) and the rate of presenteeism are based on foreign literature. This is the reason why we also perform a thorough sensitivity analysis and vary some of the key parameters of the model. It is evident that foreign data have limited relevance in the Czech Republic. For further improvement of the analysis, it will be necessary to conduct a survey in the Czech Republic.
Our study demonstrates that the costs of obesity are considerable in the Czech Republic and comparable to the costs of smoking and alcohol consumption, which are estimated as 14.5 billion CZK (0.8% of GDP) in 1999 [57] and 59.5 billion CZK (1.2% of GDP) in 2016 [58], respectively. However, smoking and alcohol consumption have received more consistent attention in clinical practice and public health policy [13]. Similarly as alcohol consumption and smoking, early onset of obesity or overweight significantly increases the probability of being obese in adulthood [59]. This implies that obesity is a serious disease which should no longer be regarded as a lifestyle issue but needs to be recognised as a serious medical condition [60].
Conclusion
The rising prevalence of obesity has been putting an increasing pressure on the health care system and society, which will be further aggravated due to the COVID-19 pandemic. The goal of this study was to quantify the extent of this burden in the Czech Republic using data from 2018. The social costs of obesity are estimated using the cost-of-illness approach. Total costs of obesity are estimated to be 40.8 billion CZK, which corresponds to 0.8% of GDP in 2018. Out of this, 14.5 billion CZK (35%) are attributable to direct costs and 26.3 billion (65%) are attributable to indirect costs. The direct costs account for 3.4% of total healthcare costs in 2018. Within indirect costs, the largest part is attributable to premature mortality (10 billion CZK), absenteeism (9.2 billion CZK) and presenteeism (7.1 billion CZK).
This is a unique country-level COI study which focuses on the costs of obesity in the Czech Republic and accounts for several groups of direct and indirect costs. These costs are substantial which is supported by the fact that they are comparable to the costs of smoking or alcohol consumption in the Czech Republic. Moreover, with rising prevalence of overweight and obesity in children and adults, these costs are likely to increase. A comprehensive, systemic program of multiple interventions should be implemented to increase awareness, reverse the trend of growing rates of obesity and save money in the long-term horizon.
Appendix A: Literature review
Appendix B: Methods appendix
This study uses the cost-of-illness (COI) approach to estimate the social costs of obesity. Two approaches exist within the COI approach: (i) the prevalence approach, which estimates the costs of all new and pre-existing cases in one year, including years lost due to premature death discounted to present value, and (ii) the incidence approach, which estimates lifetime costs of all new cases/deaths in given year. Prevalence approach is used in the analysis as the aim is to assess the current economic burden of obesity.
B.1 Direct costs
Direct costs of illness include all resources related to its prevention, treatment and rehabilitation [50]. The top-down approach, which measures the proportion of a disease that is due to exposure to risk factor, is used. This approach uses aggregated data, along with PAF (population attributable fraction), which is used to determine the attributable costs. For example, it attributes part of costs of diabetes to obesity [55].
The computation of direct costs of obesity is divided into two parts due to data constraints specific to the Czech Republic. The reason is that the healthcare utilization costs are documented with International Classification of Diseases (ICD) codes, whereas pharmaceutical costs are documented with ATC (Anatomical Therapeutic Chemical) classification codes.
B.1.1 Healthcare utilization costs
Healthcare utilization costs are computed in the following way:
Identify the comorbidities of obesity, i.e. the diseases that are more likely to occur if a person suffers from obesity.
Find the relative risk () for each comorbidity c. That is, how much more likely is a disease to occur in population with obesity as opposed to population with normal weight. , where is is the probability of disease at obese population and is the probability of disease at normal weight population.
Find prevalence (p) of obesity in the Czech Republic, i.e. the proportion of population whose BMI exceeds 30 kg/m2.
- Compute (population attributable fraction for comorbidity c), which tells us what fraction of disease’s costs is attributable to obesity:
The does not take into account ages nor genders as the data on healthcare utilization costs are provided for each diagnosis without the distinction of age groups or gender. For instance, for stroke is equal to 11%, meaning that 11% of healthcare costs of stroke are caused by obesity. - Compute the healthcare utilization costs attributable to obesity (HC):
where are the healthcare utilization costs associated with comorbidity c. The healthcare utilization costs are obtained from the General Health Insurance Fund and contain all the costs of patients that had a comorbidity of obesity (e.g. Diabetes II mellitus with ICD codes E11, E13 or E14) as the main diagnosis, i.e. it was the main cause of receiving a treatment.
B.1.2 Costs of pharmacotherapy
Since healthcare utilization costs do not contain the costs of pharmacotherapy,5 we include these separately by identifying the ATC groups which are related to comorbidities of obesity. We include five groups of pharmaceuticals based on Hodycova (2009) and Dee (2015) [19, 23]:
for the cure of obesity
for the cure of diabetes mellitus
for the cure of cardiovascular diseases
for the cure of cancer
for the cure of arthrosis
Specific ATC groups are available in Table 11. The costs of pharmaceuticals provided by the General Health Insurance Fund contain only the costs used in the treatment of the comorbidity (e.g. if we take the example of diabetes mellitus, these costs are not the costs of pharmaceuticals incurred by all diabetic patients, but they are the costs of pharmaceuticals used in the treatment of diabetes). Pharmaceutical costs PC are computed as:
where are the pharmaceutical costs of ATC group which is related to a comorbidity of obesity c. PAF are used to compute the part of pharmaceutical costs that are directly attributable to obesity.
B.2 Indirect costs
Indirect costs of illness are the value of lost production due to morbidity or mortality. This lost time is multiplied by age- and gender-specific average gross wage rates to calculate the indirect costs [50]. The Human capital approach (HCA) is used to estimate the indirect costs. It takes the patient’s perspective and counts any hour not worked as an hour lost. The value of housework is also incorporated into the lost production and it is valued as the opportunity cost of hiring a replacement from the labor market [9].
We include three common components of indirect costs: absenteeism, presenteeism and premature mortality. For premature mortality, the present value of future lost earnings is computed using a discount rate. The total lost productivity is the sum of paid work (measured in days per month) and unpaid work (measured in hours per month). Paid work is valued by gender- and age-specific monthly gross salary, whereas unpaid work is valued by the average hourly salary of a household worker:6
where refers to age- (a) and gender- (g) specific evaluation of productivity lost, stands for the age- and gender-specific amount of paid work, refers to age and gender-specific gross salary, stands for the gender-specific amount of unpaid work and stands for the wage of household worker.7 The productivity lost from paid work is considered until the average retirement age (63.2 years for men and 62.7 years for women [69]), whereas the productivity lost from unpaid work is considered until the average life expectancy age (76 for men and 82 for women [47]). The data on indirect costs (specifically absenteeism and premature mortality) allow for more detailistic computation of costs attributable to obesity, so which is specific for age (a), comorbidity (c) and gender (g) is used:
B.2.1 Absenteeism
Absenteeism refers to absence from work due to illness. To calculate the number of days absent from work attributable to obesity, we use the number of terminated cases of incapacity for work for obesity-related comorbidities in days from 2018 provided by the IHIS [41].
The number of days spent absent from work due to obesity for age (a), comorbidity (c) and gender (g) are computed as:
where stands for age- (a), comorbidity- (c) and gender- (g) specific days absent. Total costs due to obesity-related absenteeism () are monetarily valued as:
where is the evaluation of paid and unpaid work as specified above.
B.2.2 Presenteeism
To the best of our knowledge, no survey measuring obesity-related presenteeism has been conducted in the Czech Republic so far. Our assumption is based on literature review summarised in Table 6. The review contains studies predominantly from the USA. Only one study focuses on five European countries (France, Germany, Italy, Spain and UK) and states that obesity-related presenteeism means 4–33 more days lost compared to normal weight, depending on obesity class. Based on the literature review, we assume that the average annual rate of presenteeism for obese individuals in the Czech Republic is 2 days lost for both men and women. This assumption is rather conservative, but we prefer a conservative approach rather than overestimating the costs. In sensitivity analysis, we also estimate the costs for 1, 3 and 4 days lost due to presenteeism. Yearly lost productivity due to presenteeism is valued as:
where is the number of employed people in working-age population (distinguished by gender g), and is the number of obese people in labour force (p is prevalence of obesity in working-age population, i.e. 25–64 years old), PL stands for productive days lost due to presenteeism and is the gender-specific valuation of paid and unpaid work.8
B.2.3 Premature mortality
To calculate the costs of premature mortality due to obesity-related diseases, we use the data from the IHIS [42]. These data contain the number of deaths at each age cathegory due to comorbidities of obesity. To evaluate the lost productivity, we take into account not only the productive years lost (i.e. years before retirement age), but also the years after retirement age as not including this would imply that life of retired people has no value [50]. The productive years are valued by average monthly salary specific for 5-year age group and gender, and by the value of unpaid work (approximated by hourly salary of cleaning services employee), assuming that both men and women perform daily unpaid work according to a survey by the Czech Academy of Sciences [45]. The years after retirement age and before life expectancy are valued by the amount of unpaid work according to a survey by the Czech Academy of Sciences [11, 45].
In COI studies, costs are computed for one given year, but in case of premature mortality, the net present value of future lost earnings is included [55]. The value of productivity losses is discounted to present value using a discount rate:
where i is the discount rate, FV stands for future value and t is the amount of years lost. The discount rate usually ranges between 0 and 10% [55]. We use the discount rate of 3% as suggested by Segel et al. (2006) [55], but because the discount rate affects the results largely, we also perform sensitivity analysis with discount rates 1% and 5% [70].
The obesity-attributable costs of premature mortality are computed as:
where stands for age-, comorbidity- and gender-specific number of deaths. Only half of the productivity is accounted for in the first year () to correct for different occurences of death during the year. Until retirement (ret), the lost productivity is valued by both paid and unpaid work. From retirement age until the average life expectancy age (exp), the lost productivity is valued by the value of unpaid work. We do not take into account background death rates in future years (i.e. deaths that would have occurred separate from obesity-related causes) as it is not standard in this methodological approach.
B.3 Sensitivity analysis
The robustness of our results is tested using sensitivity analysis where we vary several essential parameters used in the evaluation of costs of obesity (Table 8):
PAF are recomputed using the 95% confidence interval of relative risks from Dobbins et al. [8] and Guh et al. [7].
PAF are recomputed using the relative risks from the Dynamo project. This project provides relative risks for selected diseases as indicated in Table 8 and is based on studies from Europe. Additionally, it provides adjustments of relative risks based on age.
Prevalence data from the European Health Examination Survey [52] and European Health Interview Survey [52] (EHES and EHIS) are used. These surveys were conducted in 2014 in the Czech Republic.9 EHES is a survey focusing on working population (aged 25–64) and the data are collected by physicians. EHIS focuses on all population aged 15+ years and the data are self-reported. We use mainly the EHES data and complete them with the EHIS data in age groups 15–24 and 65+. The prevalence of obesity in population 15+ years is 25.3% for men and 22.9% for women [51], while the prevalence in working population (25–64 years) is 29.1% for men and 24.7% for women [52].
Discount rate of 1% and 5% is used for computing the costs of premature mortality.
Unpaid work is completely excluded from total costs.
Presenteeism is computed for missing 1, 3 and 4 days of work (baseline value is 2 days).
Table 8.
Relative risks from the Dynamo project
| Women | Men | Age adjustment | |
|---|---|---|---|
| Ischemic heart disease | 2 | 2 | 0.70 age over 65 |
| Stroke | 1.55 | 1.5 | 0.75 from age 65 |
| Diabetes | 7 | 5.5 | 0.92 from age 60 |
| 0.90 from age 75 | |||
| Breast cancer | 1 | 1 | 1.25 over age 50 women |
| Colorectal cancer | 1.1 | 1.4 | 0.90 from age 45 |
| Kidney cancer | 1.8 | 1.55 | – |
| Gallbladder cancer | 1.85 | 1.25 | 1.17 from age 45 men |
| 0.80 from age 45 women | |||
| Endometrial cancer | 2.5 | – | – |
Source: The Dynamo Project [71]
Appendix C: Comparison with the OECD study
In 2019, OECD published a study estimating the burden of obesity in 52 countries, including the Czech Republic [2]. The estimate of economic burden of overweight is estimated as 4% of GDP, which is much higher than ours estimate of 0.8% of GDP. The OECD study and our research differ in many aspects. Here are the most important ones:
The OECD study does not distinguish obesity from overweight. Our paper focuses purely on obesity (BMI > 30), whereas the OECD study evaluates the costs of overweight (BMI > 25). Even though pre-obesity, or overweight (BMI 25–30), is dangerous in a way that it often leads to obesity, it is associated with significantly lower risk of developing serious complications from comorbidities, as opposed to obesity.
- The methodology of the OECD study and our study is completely different. While the OECD study uses a microsimulation model, we perform a country-level COI study using the top-down approach. As stated in the OECD study, studies using the top-down approach usually provide a lower-bound estimate. The microsimulation model creates a synthetic population based on national demographic characteristics and risk factors from which life expectancy, disease prevalence and disability-adjusted life years are calculated. Different data sources are used in the OECD study, for example:
- The data used for the estimation of healthcare utilization costs in the Czech Republic are estimated from the Netherlands data. In our study, we use the data from the Czech Republic, specifically from the General Health Insurance Fund. Additionally, each study computes the costs for different set of diseases.
- The data used in the estimation of costs related to unemployment and absenteeism come from the SHARE survey, which focuses on population 50-63 years old and the data are self-reported. In our study, we have data from the Institute of Health Information and Statistics (IHIS) of the Czech Republic for all the age groups.
- The estimation of presenteeism related costs derives the days missed from absenteeism in a specific country using a study by Goetzel et al. (2004). From this study, the ratio of presenteeism:absenteeism missed days is derived for five health conditions: asthma, COPD, CVD, cancer and diabetes. The ratio is always larger than 1 (in three cases larger than 2), leading to very high estimated costs of presenteeism. In our study, we take a conservative approach based on a detailed literature review.
The OECD study does not provide the specific amount of components of total costs for each country. Instead, it provides an aggregate result.
We provide a very thorough sensitivity analysis where we vary the level of several key parameters of our analysis.
Appendix D: Results
D.1 Healthcare utilization costs
D.2 Costs of pharmacotherapy
See Table 11.
D.3 Costs of absenteeism
See Table 12.
D.4 Costs of presenteeism
See Table 13.
D.5 Costs of premature mortality
See Table 14.
Declarations
Conflict of interest
Partial financial support was received from not-for-profit organization Czech Priorities. The authors have no relevant financial or non-financial interests to disclose.
Footnotes
The extrapolation coefficient is equal to 1.79 as there were 5.95 million people insured at GHIF in 2018 and Czech population was 10.65 million.
PAF are used in 5-year age groups when the data allows it.
Total healthcare costs in the Czech Republic were 430.9 billion CZK in 2018 [54].
These data are stratified by gender and 10-year age groups.
ICD-10 codes are not available for prescribed medicaments.
We approximate this by average wage of cleaning services worker [46].
The wage of household worker is not available for men and women separately.
We do not distinguish salaries based on age in this part: .
A new survey started in 2019, but due to the lack of respondents, the data are not available in 5-year age groups.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Dobbs R, Sawers C, Thompson F, Manyika J, Woetzel J, Child P, McKenna S, Spatharou A. Overcoming obesity: An initial economic analysis. USA: McKinsey Global Institute; 2014. [Google Scholar]
- 2.OECD. The Heavy Burden of Obesity. OECD Publishing, 2019a. 10.1787/67450d67-en. https://www.oecd-ilibrary.org/content/publication/67450d67-en
- 3.Popkin, B.M., Du, S., Green, W.D., Beck, M.A., Algaith, T., Herbst, C.H., Alsukait, R.F., Alluhidan, M., Alazemi, N., Shekar, M.: Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obes. Rev. 21(11), e13128 (2020). 10.1111/obr.13128 [DOI] [PMC free article] [PubMed]
- 4.Bruthans, J.: Studie Czech post-MONICA a studie Czech EUROASPIRE: kardiovaskulární rizikové faktory a jejich kontrola v obecné populaci a u osob se stabilní ischemickou chorobou srdeční/Study Czech post-MONICA and study Czech EUROASPIRE: cardiovascular risc factors and their control in general population and in population with ischemic heart disease. http://www.szu.cz/uploads/documents/szu/akce/materialy/14.10.2019/BRUTHANS.pdf (2019). Accessed 17 May 2020
- 5.NIPH. Výskyt nadváhy a obezity (Prevalence of overweight and obesity). http://www.szu.cz/uploads/documents/chzp/info_listy/Vyskyt_nadvahy_a_obezity_2018.pdf (2018). Accessed 17 Oct 2020
- 6.Byford S, Torgerson DJ, Raftery J. Economic note: Cost of illness studies. BMJ. 2000;320(7245):1335. doi: 10.1136/bmj.320.7245.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guh, D.P., Zhang, W., Bansback, N., Amarsi, Z., Birmingham, C.L., Anis, A.H.: The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9(1), 88 (2009). 10.1186/1471-2458-9-88 [DOI] [PMC free article] [PubMed]
- 8.Dobbins, M., Decorby, K., Choi, B.C.K.: The association between obesity and cancer risk: a meta-analysis of observational studies from 1985 to 2011. ISRN Prevent. Med. 2013, 680536 (1985). 10.5402/2013/680536 [DOI] [PMC free article] [PubMed]
- 9.Effertz T, Engel S, Verheyen F, Linder R. The costs and consequences of obesity in germany: a new approach from a prevalence and life-cycle perspective. Eur. J. Health Econ. 2016;17(9):1141–1158. doi: 10.1007/s10198-015-0751-4. [DOI] [PubMed] [Google Scholar]
- 10.Cawley J, Meyerhoefer C. The medical care costs of obesity: an instrumental variables approach. J. Health Econ. 2012;31(1):219–230. doi: 10.1016/j.jhealeco.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 11.Konnopka, A., Bödemann, M., König, H.H.: Health burden and costs of obesity and overweight in Germany. Eur. J. Health Econ. 12(4), 345–352 (2011). 10.1007/s10198-010-0242-6 [DOI] [PubMed]
- 12.Arterburn, D.E., Maciejewski, M.L., Tsevat, J.: Impact of morbid obesity on medical expenditures in adults. Int. J. Obes. 29(3), 334–339 (2005). 10.1038/sj.ijo.0802896 [DOI] [PubMed]
- 13.Sturm R. The effects of obesity, smoking, and drinking on medical problems and costs. Health Aff. 2002;21(2):245–253. doi: 10.1377/hlthaff.21.2.245. [DOI] [PubMed] [Google Scholar]
- 14.Wang, F., McDonald, T., Bender, J., Reffitt, B., Miller, A., Edington, D.W.: Association of healthcare costs with per unit body mass index increase. J. Occup. Environ. Med. 48(7), 668–674 (2006). 10.1371/journal.pone.0247307 [DOI] [PubMed]
- 15.Raebel, M.A, Malone, D.C, Conner, D.A., Xu, S., Porter, J.A., Lanty, F.A.: Health services use and health care costs of obese and nonobese individuals. Arch. Int. Med. 164(19), 2135–2140 (2004). 10.1001/archinte.164.19.2135 [DOI] [PubMed]
- 16.Borg, S., Persson, U., Ödegaard, K., Berglund, G., Nilsson, J., Nilsson, P.M.: Obesity, survival, and hospital costs-findings from a screening project in Sweden. Value Health 8(5), 562–571 (2005). 10.1111/j.1524-4733.2005.00048.x [DOI] [PubMed]
- 17.Krueger, H., Krueger, J., Koot, J.: Variation across Canada in the economic burden attributable to excess weight, tobacco smoking and physical inactivity. Can. J. Public Health 106(4), e171–e177 (2015). 10.17269/cjph.106.4994 [DOI] [PMC free article] [PubMed]
- 18.Tuzarová, Kateřina: Společenské náklady obezity v České republice. Master’s thesis, Vysoká škola ekonomická v Praze, (2016)
- 19.Hodycová, T.: Ekonomické dopady rostoucí incidence obezity na zdravotnictví v ČR (diplomová práce)/Economic consequences of growing incidence of obesity on healthcare in the Czech Republic. Master’s thesis, Vysoká škola ekonomická, Institut managementu zdravotnických služeb (2009)
- 20.WHO. Absenteeism from work due to illness, days per employee per year. https://gateway.euro.who.int/en/indicators/hfa_411-2700-absenteeism-from-work-due-to-illness-days-per-employee-per-year/visualizations/#id=19398 &tab=table (2019). Accessed 27 Jan 2021
- 21.Dall TM, FulgoniIII VL, Zhang Y, Reimers KJ, Packard PT, Astwood JD. Predicted national productivity implications of calorie and sodium reductions in the american diet. Am. J. Health Promot. 2009;23(6):423–430. doi: 10.4278/ajhp.081010-QUAN-227. [DOI] [PubMed] [Google Scholar]
- 22.Finkelstein E, Fiebelkorn IC, Wang G. The costs of obesity among full-time employees. Am. J. Health Promot. 2005;20(1):45–51. doi: 10.4278/0890-1171-20.1.45. [DOI] [PubMed] [Google Scholar]
- 23.Dee, A., Callinan, A., Doherty, E., O’Neill, C., McVeigh, T., Sweeney, M.R., Staines, A., Kearns, K., Fitzgerald, S., Sharp, L. et al.: Overweight and obesity on the island of Ireland: an estimation of costs. BMJ Open 5(3) (2015). 10.1136/bmjopen-2014-006189corr1 [DOI] [PMC free article] [PubMed]
- 24.Lehnert, T., Streltchenia, P., Konnopka, A., Riedel-Heller, S.G., König, H.H.: Health burden and costs of obesity and overweight in Germany: an update. Eur. J. Health Econ. 16(9), 957–967 (2015). 10.1007/s10198-014-0645-x [DOI] [PubMed]
- 25.Kang JH, Jeong BG, Cho YG, Song HR, Kim KA. Socioeconomic costs of overweight and obesity in korean adults. J. Korean Med. Sci. 2011;26(12):1533–1540. doi: 10.3346/jkms.2011.26.12.1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Andreyeva, T., Luedicke, J., Wang, Y.C.: State-level estimates of obesity-attributable costs of absenteeism. J. Occup. Environ. Med. Am. Coll. Occup. Environ. Med. 56(11), 1120 (2014). 10.1097/JOM.0000000000000298 [DOI] [PMC free article] [PubMed]
- 27.Johns G. Presenteeism in the workplace: A review and research agenda. J. Organ. Behav. 2010;31(4):519–542. doi: 10.1002/job.630. [DOI] [Google Scholar]
- 28.Finkelstein, E.A., DiBonaventura, M.dC., Burgess, S.M., Hale, B.C., et al.: The costs of obesity in the workplace. J. Occup. Environ. Med. 52(10), 971–976 (2010). 10.1097/JOM.0b013e3181f274d2 [DOI] [PubMed]
- 29.Collins JJ, Baase CM, Sharda CE, Ozminkowski RJ, Nicholson S, Billotti GM, Turpin RS, Olson M, Berger ML. The assessment of chronic health conditions on work performance, absence, and total economic impact for employers. J. Occup. Environ. Med. 2005;47(6):547–557. doi: 10.1097/01.jom.0000166864.58664.29. [DOI] [PubMed] [Google Scholar]
- 30.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting us employers. J. Occup. Environ. Med. 2004;46(4):398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 31.Goetzel RZ, Gibson TB, Short ME, Chu B-C, Waddell J, Bowen J, Lemon SC, Fernandez ID, Ozminkowski RJ, Wilson MG, et al. A multi-worksite analysis of the relationships among body mass index, medical utilization, and worker productivity. J. Occup. Environ. Med. 2010;52(1S):S52–S58. doi: 10.1097/JOM.0b013e3181c95b84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boles M, Pelletier B, Lynch W. The relationship between health risks and work productivity. J. Occup. Environ. Med. 2004;46(7):737–745. doi: 10.1097/01.jom.0000131830.45744.97. [DOI] [PubMed] [Google Scholar]
- 33.Burton WN, Chen C-Y, Conti DJ, Schultz AB, Pransky G, Edington DW. The association of health risks with on-the-job productivity. J. Occup. Environ. Med. 2005;47(8):769–777. doi: 10.1097/01.jom.0000169088.03301.e4. [DOI] [PubMed] [Google Scholar]
- 34.Ricci JA, Chee E. Lost productive time associated with excess weight in the us workforce. J. Occup. Environ. Med. 2005;47(12):1227–1234. doi: 10.1097/01.jom.0000184871.20901.c3. [DOI] [PubMed] [Google Scholar]
- 35.Gupta S, Richard L, Forsythe A. The humanistic and economic burden associated with increasing body mass index in the eu5. Diabetes Metab. Syndr Obes. Targets Ther. 2015;8:327–338. doi: 10.2147/DMSO.S83696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peeters A, Barendregt JJ, Willekens F, Mackenbach JP, Mamun AA, Bonneux L. Obesity in adulthood and its consequences for life expectancy: a life-table analysis. Ann. Intern. Med. 2003;138(1):24–32. doi: 10.7326/0003-4819-138-1-200301070-00008. [DOI] [PubMed] [Google Scholar]
- 37.Fontaine KR, Redden DT, Wang C, Westfall AO, Allison DB. Years of life lost due to obesity. JAMA. 2003;289(2):187–193. doi: 10.1001/jama.289.2.187. [DOI] [PubMed] [Google Scholar]
- 38.OECD. The Heavy Burden of Obesity, Technical country notes. OECD Publishing, 2019b. URL http://www.oecd.org/health/the-heavy-burden-of-obesity-67450d67-en.htm
- 39.Nejedlá M. Zdravotní a hospodářské důsledky epidemie obezity a možnosti její prevence ve školách/health and economic consequences of obesity epidemic and possibilities of its prevention in schools. Česká Antropologie. 2014;64:20–24. [Google Scholar]
- 40.GHIF. Healthcare costs of selected diseases, 2018. Data obtained upon author’s request
- 41.IHIS. Information system incapacity for work, 2018a. Data obtained upon author’s request
- 42.IHIS. Information system deaths, 2018b. Data obtained upon author’s request
- 43.Abarca-Gómez, L., Abdeen, Z.A., Abdul Hamid, Z., Abu-Rmeileh, N.M., Acosta-Cazares, B., Acuin, C., Adams, R.J., Aekplakorn, W., Afsana, K., Aguilar-Salinas, C.A. et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet, 390(10113), 2627–2642 (2017). 10.1016/S0140-6736(17)32129-3 [DOI] [PMC free article] [PubMed]
- 44.CSO. Structure of Earnings Survey - 2018. https://www.czso.cz/csu/czso/structure-of-earnings-survey-2018 (2019). Accessed 20 Nov 2020
- 45.AVČR. Jak Češi tráví čas? Výsledky 1. ročníku výzkumu proměny české společnosti 2015 (How Czechs spend time? Results of first research of changes in Czech society) (2016). https://www.promenyceskespolecnosti.cz/aktuality/aktualita22/Jak_Cesi_travi_cas_TK_20-06-2016.pdf. Accessed 1 Mar 2021
- 46.ISPV. Informační systém o průměrném výdělku - Mzdová sféra ČR 2018 (Information system on average earnings). https://www.ispv.cz/cz/Vysledky-setreni/Archiv/2018.aspx (2020). Accessed 18 Dec 2020
- 47.CSO. Life tables for the Czech Republic, cohesion regions, and regions - 2017 - 2018. https://www.czso.cz/csu/czso/life-tables-for-the-czech-republic-cohesion-regions-and-regions-2017-2018 (2020a). Accessed 18 Dec 2020
- 48.Eurostat. Employment and activity by sex and age - annual data. https://ec.europa.eu/eurostat/data/database (2018). Accessed 19 Jan 2021
- 49.Bloom, D.E., Cafiero, E., Jané-Llopis, E., Abrahams-Gessel, S., Bloom, L.R., Fathima, S., Feigl, A.B., Gaziano, T., Hamandi, A., Mowafi, M., et al.: The global economic burden of noncommunicable diseases. Technical report, Program on the Global Demography of Aging, (2012)
- 50.WHO. WHO guide to identifying the economic consequences of disease and injury. Technical report, 2009
- 51.IHIS. Health interview surveys in the Czech Republic: European Health Interview Survey 2014. https://ehis.uzis.cz/index-en.php?pg=ehis-2014 (2014). Accessed 19 Sep 2020
- 52.NIPH. Evropský průzkum zdravotního stavu (European health examination survey)—EHES. http://www.szu.cz/ehes (2014). Accessed 19 Sep 2020
- 53.CSO. Key macroeconomic indicators. https://www.czso.cz/csu/czso/hmu_ts (2021). Accessed 01 Mar 2021
- 54.CSO. Výsledky zdravotnických účtů ČR 2010–2018 (Health accounts results). https://www.czso.cz/csu/czso/vysledky-zdravotnickych-uctu-cr-2010-2018 (2020). Accessed 1 Mar 2021
- 55.Segel JE. Cost-of-illness studies - a primer. RTI-UNC Center Excell. Health Promot. Econ. 2006;1:39. [Google Scholar]
- 56.NIPH. Vybrané výsledky studie EHES 2019 (Selected results of EHES 2019). http://www.szu.cz/ehes/vybrane-vysledky-studie-ehes-2019 (2019). Accessed 5 Nov 2020
- 57.Ross H. Critique of the philip morris study of the cost of smoking in the Czech Republic. Nicot. Tob. Res. 2004;6(1):181–189. doi: 10.1080/14622200310001657000. [DOI] [PubMed] [Google Scholar]
- 58.Chadimova K, Mlcoch T, Dolejsi D, Hajickova B, Mazalova M, Lamblova K, Dolezal T. The economic burden of alcohol consumption in the Czech Republic. Value Health. 2019;22:S686. doi: 10.1016/j.jval.2019.09.1506. [DOI] [Google Scholar]
- 59.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N. Engl. J. Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 60.Schmid A, Schneider H, Golay A, Keller U. Economic burden of obesity and its comorbidities in Switzerland. Soc. Prevent. Med. 2005;50(2):87–94. doi: 10.1007/s00038-004-4067-x. [DOI] [PubMed] [Google Scholar]
- 61.Kleinman N, Abouzaid S, Andersen L, Wang Z, Powers A. Cohort analysis assessing medical and nonmedical cost associated with obesity in the workplace. J. Occup. Environ. Med. 2014;56(2):161–170. doi: 10.1097/JOM.0000000000000099. [DOI] [PubMed] [Google Scholar]
- 62.An R. Health care expenses in relation to obesity and smoking among us adults by gender, race/ethnicity, and age group: 1998–2011. Public Health. 2015;129(1):29–36. doi: 10.1016/j.puhe.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 63.Sander B, Bergemann R. Economic burden of obesity and its complications in Germany. Eur. J. Health Econ. 2003;4(4):248–253. doi: 10.1007/s10198-003-0178-1. [DOI] [PubMed] [Google Scholar]
- 64.Lehnert T, Stuhldreher N, Streltchenia P, Riedel-Heller SG, König H-H. Sick leave days and costs associated with overweight and obesity in Germany. J. Occup. Environ. Med. 2014;56(1):20–27. doi: 10.1097/JOM.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 65.Neovius K, Rehnberg C, Rasmussen F, Neovius M. Lifetime productivity losses associated with obesity status in early adulthood. Appl. Health Econ. Health Policy. 2012;10(5):309–317. doi: 10.1007/BF03261865. [DOI] [PubMed] [Google Scholar]
- 66.Pelletier B, Boles M, Lynch W. Change in health risks and work productivity over time. J. Occup. Environ. Med. 2004;46(7):746–754. doi: 10.1097/01.jom.0000131920.74668.e1. [DOI] [PubMed] [Google Scholar]
- 67.Gates DM, Succop P, Brehm BJ, Gillespie GL, Sommers BD. Obesity and presenteeism: The impact of body mass index on workplace productivity. J. Occup. Environ. Med. 2008;50(1):39–45. doi: 10.1097/JOM.0b013e31815d8db2. [DOI] [PubMed] [Google Scholar]
- 68.Kirkham HS, Clark BL, Bolas CA, Lewis GH, Jackson AS, Fisher D, Duncan I. Which modifiable health risks are associated with changes in productivity costs? Popul. Health Manag. 2015;18(1):30–38. doi: 10.1089/pop.2014.0033. [DOI] [PubMed] [Google Scholar]
- 69.OECD. Ageing and employment policies—statistics on average effective age of retirement. https://www.oecd.org/els/emp/average-effective-age-of-retirement.htm (2018). Accessed 18 Dec 2020
- 70.Hodgson, T. A., Meiners, M.R.: Cost-of-illness methodology: a guide to current practices and procedures. Milbank Mem. Fund Q. Health Soc. 429–462 (1982). 10.2307/3349801 [PubMed]
- 71.Lobstein, T., Leach, R.J.: DYNAMO-HIA: Report on data collection for overweight and obesity prevalence and related relative risks. https://webgate.ec.europa.eu/chafea_pdb/assets/files/pdb/2006116/2006116_d4_dynamo_hia.pdf, 2010. Accessed: 10 (May 2022)
- 72.de Oliveira, M.L., Pacheco Santos, L.M., da Silva, E.N.: Direct healthcare cost of obesity in Brazil: an application of the cost-of-illness method from the perspective of the public health system in 2011. PLOS One 10(4), e0121160 (2015). 10.1371/journal.pone.0121160 [DOI] [PMC free article] [PubMed]