Abstract
Evidence shows that reports of psychopathology symptoms by youth and their caregiver informants differ. To quantify youth-caregiver discrepancies in psychopathology symptoms and factors associated with such discrepancies, we investigated differences in how youth and their caregivers rated psychopathology symptoms. The sample (N = 5094) was extracted from the Philadelphia Neurodevelopmental Cohort, a community-based sample of youth and included participants ages 11–17 years old with both youth and caregiver reported symptom scores. Across psychopathology symptoms, youth-caregiver concordance was poor to fair (Cohens kappa for symptom items ranged between 0.03–0.41). Psychosis symptoms had the lowest concordance—Cohen’s kappa ranged from 0.03 to 0.17 across psychosis symptoms. Discrepancies between youth and caregiver symptom reports were greater than average for Black youth and for youth of low socioeconomic status; discrepancies were also higher than average in youth with any psychiatric disorder when compared to typically developing youth. Network analysis of difference scores obtained by subtracting youth symptom scores from caregiver reported symptom scores showed that network connectivity (i.e., correlated difference scores) was sparsest for psychosis spectrum compared to other psychiatric disorders. Using a large sample, we show that youth and their caregiver informants tend to report psychopathology symptoms differently. Youth-caregiver discrepancies were the most pronounced for Black youth and youth of low socio-economic status. Race and socioeconomic status contribute to significant differences in how youth and their caregivers report such symptoms and are important factors that should be accounted for to facilitate accurate mental health symptom assessment and evaluation.
Keywords: psychosis, anxiety, depression, youth-caregiver concordance, network analysis
Introduction
Collateral informants or secondary informants provide essential information for youth psychiatric and mental health assessment, but their responses often do not correlate well with participant self-reports (Duhig et al., 2000). Such discrepancies are dependent on the participant as well as the informant type - for example, in the case of youth participants the collateral informants can be the primary caregivers (i.e., mother, father) or the teacher. Youth-caregiver discrepancies can also arise from multiple other factors such as random errors, informant characteristics (race, gender etc.), contextual factors (the setting where the assessment was performed) and the nature of psychopathology under study (De Los Reyes, 2013). These factors serve as an important source of variation in the reports obtained and should be considered especially when data are collected from participants as well as caregiver informants (De Los Reyes & Kazdin, 2005).
The influence of informant—both youth and collateral informant—characteristics such as age and informant type (De Los Reyes et al., 2008; Duhig et al., 2000) on youth psychopathologies are well studied, whereas other factors such as race are understudied. Factors such as ethnic background and minority status can also determine what behaviors individuals see as problematic thus leading to discrepant reports (Lau et al., 2004). Psychopathology characteristics such as those with externalizing versus internalizing behaviors can also result in measurable discrepancies in informant reports. Conditions with externalizing behaviors have more observable symptoms than those with internalizing behaviors and are more overt in clinical presentation. Intuitively, participant and informant reports are more concordant for conditions with externalizing behaviors.
For psychopathologies where the individual’s insight or self-awareness of illness or symptoms is significantly affected, such as those in primary psychotic disorders, participant self-reports show little convergence with caregiver reports and is primarily driven by impaired insight affecting the participant’s ability to describe their symptoms and/or behaviors accurately (Ermel et al., 2017; Sabbag et al., 2012). In such psychopathologies, disagreements also seem to vary by symptoms assessed - in psychotic conditions, concordance on depressive symptoms is greater than for psychotic symptoms - suggesting modulations by informant type and psychopathology characteristics (Ermel et al., 2017). In clinical contexts, these discrepant informant reports offer valuable information that aid diagnostic decisions (Golembo-Smith et al., 2014; Klein, 1991). For example, caregivers provide valuable information on subthreshold psychotic symptoms when youth often have difficulty reporting when symptoms arose and the impact of such symptoms on behavior (Golembo-Smith et al., 2014).
Youth-caregiver discrepancies have been studied as external predictors of psychosocial functioning (Laird & De Los Reyes, 2013). The general consensus is that there is value in understanding such discrepancies but the choice of the measure of discrepancies is important. Historically, discrepancies have been studied using difference scores e.g., values obtained by subtracting youth reported symptom scores from caregiver reported scores or vice versa. But use of such difference scores as predictors have encountered criticisms as they offer the same information as the individual scores i.e., using individual scores as predictors is mathematically equivalent to using one of those scores and the difference score as predictors (Laird, 2020). However, studies examining difference scores as outcome variables show that they provide pertinent information that could potentially be leveraged to identify clinically at-risk youth such as in the case of subthreshold psychosis (Golembo-Smith et al., 2014).
In this study we pursued the following aims. First, we sought to quantify youth-caregiver concordance for psychopathology symptoms. Second, we aimed to identify discrepancies in how youth and caregivers reported symptoms across psychiatric disorder and demographic sub-groups. Third we examined if there were similar patterns of youth-caregiver discrepancies observed across psychiatric disorders (anxiety, behavior, mood and psychosis) and demographic sub-groups.
Methods
The sample for this study (N = 5094) was obtained from the Philadelphia Neurodevelopmental Cohort (PNC). We focused on participants between 11 and 17 years of age for whom we recorded both youth self-rating and caregiver ratings on a spectrum of psychopathology symptoms. Caregivers were either mothers (~86%), fathers (~10%) or other family members/legal guardians (~3%). Refer to Calkins et al., 2015 for details on the parent study design, recruitment, and other procedures for the PNC study. All study procedures were approved by the IRB at the University of Pennsylvania. Briefly, written assent from youths and written informed consent from caregivers were obtained after they received a description of study procedures. Youths and caregivers were assessed separately. All participants were informed of the confidentiality of the reports, except for required reporting in cases of suicidal ideation, suicidal intent, and/or abuse.
Psychopathology symptom items.
Youth and caregivers rated lifetime psychopathology symptom items on the computerized version of GOASSESS, a structured interview and assessment that incorporates well validated and reliable measures for psychopathology screening, evaluating (i) psychopathology symptoms, (ii) their frequency, duration, distress and/or (iii) impairment associated with psychopathology domains, in addition to (iv) treatment history and the lifetime prevalence of any disorder. Psychopathology measures in GOASSESS include the following measures. (1) NIMH Genetic Epidemiology Research Branch Kiddie-Schedule for Affective Disorders and Schizophrenia (K-SADS) (Merikangas et al., 2009, 1998) is an extensively validated widely used, highly reliable measure considered to be the “gold standard” to assess Diagnostic and Statistical Manual (DSM) psychopathology symptoms. Inter-rater and test-retest reliability for live test-retest, video, audio as well as joint interview formats have been published (Ambrosini, 2000). (2) Revised PRIME screen for assessment of positive sub-psychosis symptoms, a measure with high internal consistency, Cronbach’s alpha of 0.88 and high sensitivity (1.00) and specificity (0.74) (Kobayashi et al., 2008). (3) Scale of Prodromal Syndromes (SOPS) which assesses negative and disorganized psychotic symptoms with high internal consistency—Cronbach’s alpha 0.85 (Miller et al., 2003; Okewole et al., 2015).
For this study, we selected 113 symptom items (available at https://osf.io/v4wj5/ ) from GOASSESS that were consistently reported in the overall sample. These 113 items corresponded to symptom items from 14 different psychopathological domains (or discrete psychopathology conditions). These domains included attention deficit hyperactive (ADH), agoraphobia, conduct, generalized anxiety (GA), depression, mania, obsessive compulsive (OC), oppositional defiant (OD), panic, specific phobias, psychosis, separation anxiety, social anxiety, and post-traumatic stress disorder (PTD). 103 of the 113 items were discrete, coded with a ‘1’ for yes and ‘0’ for no response; unknown responses were re-coded to 0 since we use sum scores for all analyses; recoding values to 0 has shown to have little to no effect on validity (Rosen et al., 2019). Twelve items were Likert-type questions with 7 possible values ranging from definitely agree ‘6’ to definitely disagree ‘0’.
Psychopathology symptom domain score is the sum of all item responses for the discrete psychopathology condition or domain. For example, the sum of all four symptom item scores for depression symptoms form the domain score for depression. The symptoms assessed, psychopathology domains, and number of symptom items per domain are available at https://osf.io/v4wj5/.
Youth and caregiver difference scores were calculated for all 14 psychopathology domains by subtracting youth reported domain scores from caregiver scores. Since the number of items varied by domain, absolute difference scores were standardized to z-scores based on mean and standard deviation of the sample.
Major psychiatric disorder categories included psychosis spectrum, mood, anxiety, and behavior disorder groups. Youth endorsing one or more symptoms and meeting DSM-IV criteria with significant impairment or distress were assigned a score of 1 and those who did not endorse any symptoms were assigned a score of 0 for a major psychiatric disorder. For example, youth approximating DSM-IV criteria for either generalized anxiety disorder, separation anxiety disorder, specific phobias, social anxiety disorder, panic disorder, agoraphobia, obsessive compulsive disorder, or post-traumatic stress disorder were grouped under the major psychiatric disorder category of anxiety. Youth approximating DSM-IV criteria for attention deficit hyperactive disorder, oppositional defiant disorder or conduct disorder, were grouped under the major psychiatric disorder category of behavior. Youth approximating DSM-IV criteria for depressive disorders, mania or hypomania were grouped under the major psychiatric disorder category of mood. Youth reporting significant hallucinations or delusions with distress but not associated with a medical disorder or substance were grouped under the major psychiatric disorder category of psychosis spectrum. Youth not meeting criteria for any of these major psychiatric disorder categories, were classified as typically developing (TD).
Statistical Analysis
Concordance.
Cohen’s kappa statistic was used to examine symptom item-wise concordance for youth and caregiver symptoms (Cohen, 1960). Intraclass correlation coefficients (ICCs) were used to examine domain-wise concordance for youth and caregiver ratings (Fisher, 1992). All statistical analyses were done in R.
Network Analysis.
We used network analysis to obtain multivariate associations of (1) youth reported symptoms, (2) caregiver reported symptoms and (3) youth-caregiver difference scores. A network analysis framework using symptoms allows to understand interrelationships symptoms and can help identify symptoms and psychopathology conditions that cooccur or are comorbid. A network analysis framework using difference scores allows to examine similarities in youth-caregiver discrepancies across different subgroups since it incorporates both youth and caregiver information in the same model.
A network model consists of “nodes” representing variables connected by “edges” or associations between variables (Epskamp et al., 2018). The network structure represents the organization of relationships between variables in the network model. In our network model, nodes are either youth or caregiver reported symptom scores, or youth-caregiver difference scores and the edges are correlations between the symptom or difference score nodes; we estimated network structure using regularized partial correlations. Strength centrality in a network model is a measure that indicates how many direct connections one node has to each other. In the youth and caregiver networks, we used strength centrality to infer which conditions were most strongly correlated to others to identify comorbidities. We did not evaluate strength centralities for difference scores networks as it does not allow for meaningful clinical interpretation.
We compared differences in networks between subgroups using network comparison’s tests (NCT) (van Borkulo et al., 2017). NCT is a permutation test which checks whether the network structure is similar across subgroups either in how the nodes and edges are organized (network invariance) or if there are similarities in the magnitude of correlations between edges in the network (global strength invariance). These results are presented as a p-value with the level of significance set at < 0.05.
Results
R codes used for analysis are available at osf.io. The overall youth sample consisted of 52% females; 57% were White participants, and 32% were Black participants. Approximately 20% of the overall sample were of age 11 years; 29% were between the ages of 12 and 13; 30% were between the ages of 14 and 15; and the remaining 22% were of age 17. 5% of the participants met criteria for psychosis spectrum, 13% of participants met criteria for a mood disorder, 44% for any behavioral disorder, and 50% for any anxiety disorder. 28% were categorized as TD. The proportion of missing data was very small: out of 113 psychopathology items, < 0.5% was missing for 110 items in caregiver reports and < 1% for 112 items in youth reports. The largest proportion of missing data was for a specific phobia item eliciting nonspecific fear of things or situations – 2.2% for youth and 1.4% for caregivers. Mean symptom scores as reported by the youth participant and the caregiver are provided in Table 1.
Table 1:
Mean and standard deviations of psychopathology domain scores
| Psychopathology Domain | Youth report | Caregiver report |
|---|---|---|
| (N=5094) | Mean(SD) | Mean(SD) |
| Attention deficit hyperactivity | 2.76 (2.68) | 2.46 (3.06) |
| Agoraphobia | 0.56 (1.15) | 0.25 (0.77) |
| Conduct | 0.48 (1.08) | 0.30 (0.88) |
| Depression | 1.09 (1.36) | 0.74 (1.21) |
| Mania | 1.45 (2.07) | 0.58 (1.36) |
| OCD | 1.26 (2.27) | 0.47 (1.28) |
| Oppositional defiance | 1.46 (1.58) | 1.17 (1.61) |
| Panic | 0.40 (0.78) | 0.23 (0.63) |
| Specific phobia | 2.11 (1.80) | 1.28 (1.39) |
| Social anxiety | 1.50 (1.62) | 1.01 (1.51) |
| Separation anxiety | 1.10 (1.28) | 0.77 (1.25) |
| Generalized anxiety | 0.79 (0.83) | 0.72 (0.87) |
| Psychosis spectrum | 10.20 (12.65) | 2.82 (6.31) |
| Post-traumatic stress | 0.80 (1.11) | 0.52 (0.87) |
Youth-Caregiver Symptom Concordance.
Domain ICCs ranged from 0.12 (mania) to 0.41 (ADH). Item level kappas ranged from 0.03 for a psychosis item eliciting tactile hallucinations to 0.74, a conduct item eliciting a history of probation. Item level concordance indices for all symptoms, and domain intra-class correlations (ICCs) are included in Supplemental figures 1 and 2.
Youth-Caregiver Symptom Networks (Figure 1A and 1B)
Figure 1:
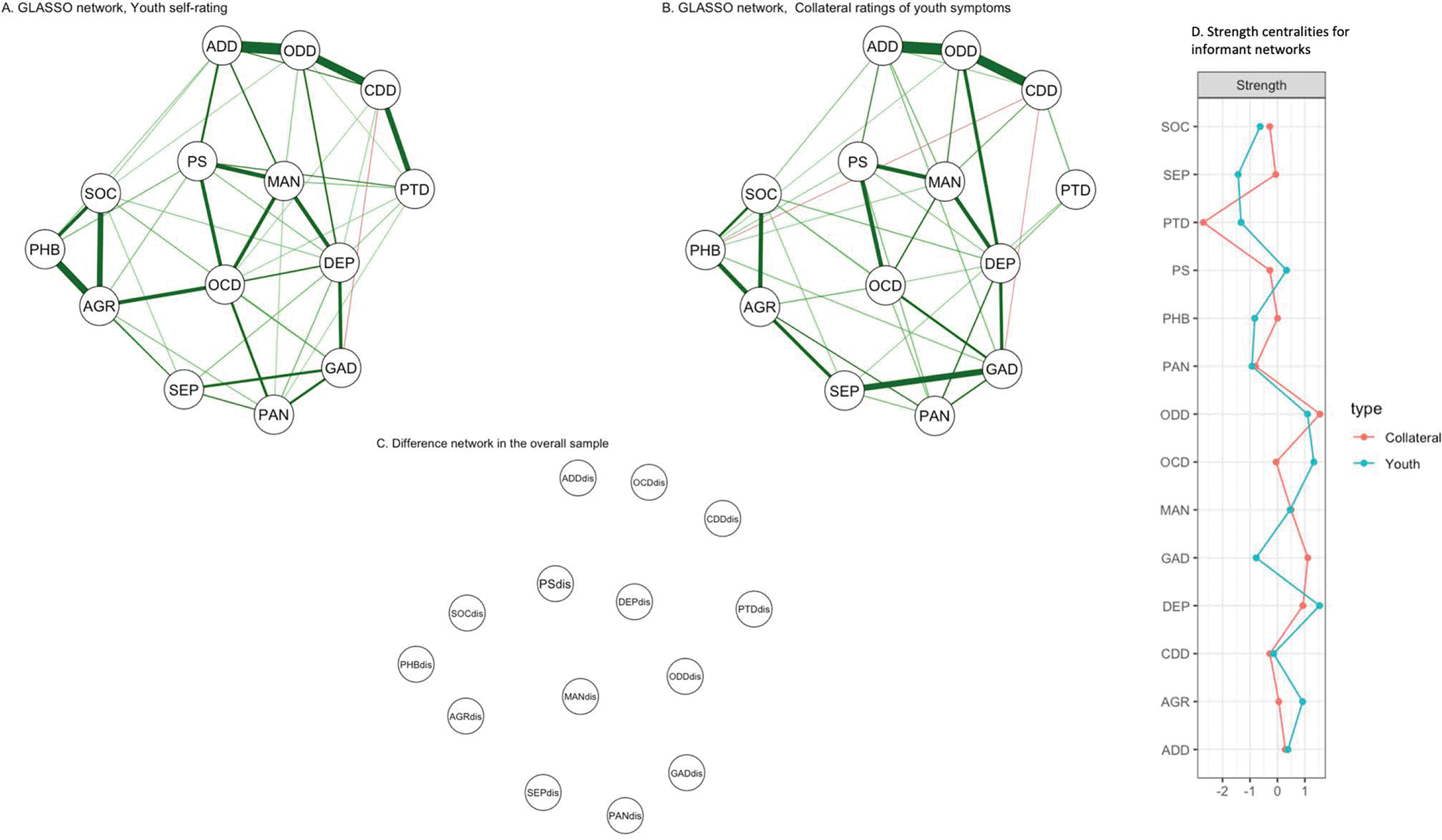
Networks for youth (1A) and collateral symptom (1B) reports constructed using a graphical lasso or GLASSO method. Nodes are psychopathology symptom domain scores and include ADD-Attention Deficit Hyperactivity ; AGR- Agoraphobia; CDD- Conduct ; DEP= Depression; GAD- Generalized Anxiety ; MAN- Mania; OCD- Obsessive Compulsive; ODD- Oppositional Defiant ; PAN- Panic ; PHB- Specific Phobias; PTD – post-traumatic stress; PSY-Psychosis; SEP-Separation Anxiety; SOC- Social Anxiety.
Green lines on the graph indicate positive associations between nodes, red is negative. Thickness and saturation of the edge weights indicates the strength of the association i.e., the thicker the edge, the stronger the association. In figure 1C, *dis indicates difference scores for the specific domain - e.g., PSdis is difference score for psychosis spectrum. Difference score network (1C) in the overall sample resulted in an empty network indicating no relationship between domain difference scores in the overall sample.
All but one edge in youth and two edges in caregiver symptom networks were positive indicating that when the informant reported more symptoms for one domain, they also reported more symptoms in the other domain. The edge between conduct and GA showed an inverse relationship in both networks indicating that when the informant reported more symptoms for conduct, they tended to report fewer symptoms for GA and vice versa. In the youth network, depression was the most central node indicating that depression symptoms was the most strongly correlated with other domains, whereas OD was the most central node in the caregiver network. NCTs showed a statistically significant difference in network structure (p = 0.02) as well as global connectivity (p = 0.023) indicating significant differences in how youth and caregivers reported symptoms. The difference score network in the overall sample was an empty network indicating no patterns or associations between any domain difference scores in the overall sample (Figure 1C).
Youth-Caregiver Discrepancies (Figure 2)
Figure 2:
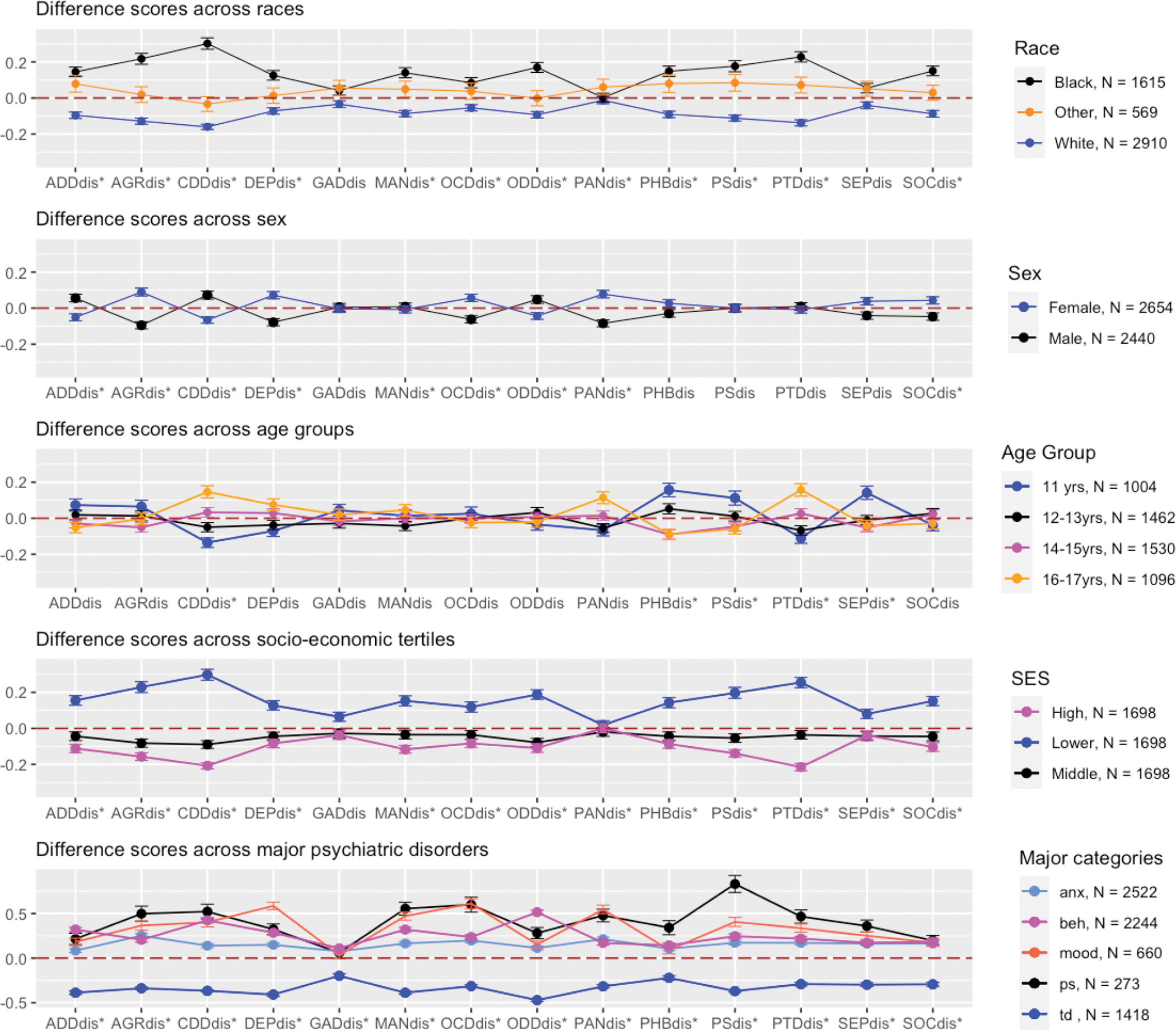
Difference scores (youth psychopathology symptom domain score minus the caregiver with standard errors for demographic and disorder groups; Y-axis indicates difference scores and are standardized z-scores; X-axes labels with * are statistically significant, analysis was corrected for multiple comparisons with significance level set at <0.004.
ADDdis-Attention Deficit Hyperactivity difference score ; AGRdis- Agoraphobia difference score; CDDdis- Conduct disorder difference score ; DEPdis= Depression difference score ; GADdis- Generalized Anxiety difference score; MANdis - Mania difference score; OCDdis - Obsessive Compulsive difference score; ODDdis - Oppositional Defiant difference score ; PANdis - Panic difference score ; PHBdis - Specific Phobias difference score; PSdis -Psychosis Spectrum difference score; SEPdis -Separation Anxiety difference score; SOCdis - Social Anxiety difference score
Difference scores across domains for socio-demographic and disorder groups are presented in Figure 2; Compared to males, difference scores were higher than average for females for several domains of anxiety (agoraphobia, panic, and social anxiety), depression and OC and lower than average for ADH and conduct. The biggest difference between sexes was for agoraphobia; other domains such as psychosis, PTD, mania and GA were not statistically significant.
Across races, difference scores were higher than average for Black youth and lower than average for White youth. These differences were statistically significant for all domains except GA and separation anxiety. The greatest discrepancy across races was seen for conduct between White and Black youth and is driven by Black youth self-reporting more symptoms than their caregivers (Figure 3); the smallest discrepancy was for panic. For age-groups, difference scores were significantly greater than average for higher age-groups in PTD, but lower than average for phobias, psychosis, and separation anxiety. Other differences were not statistically significant.
Figure 3.
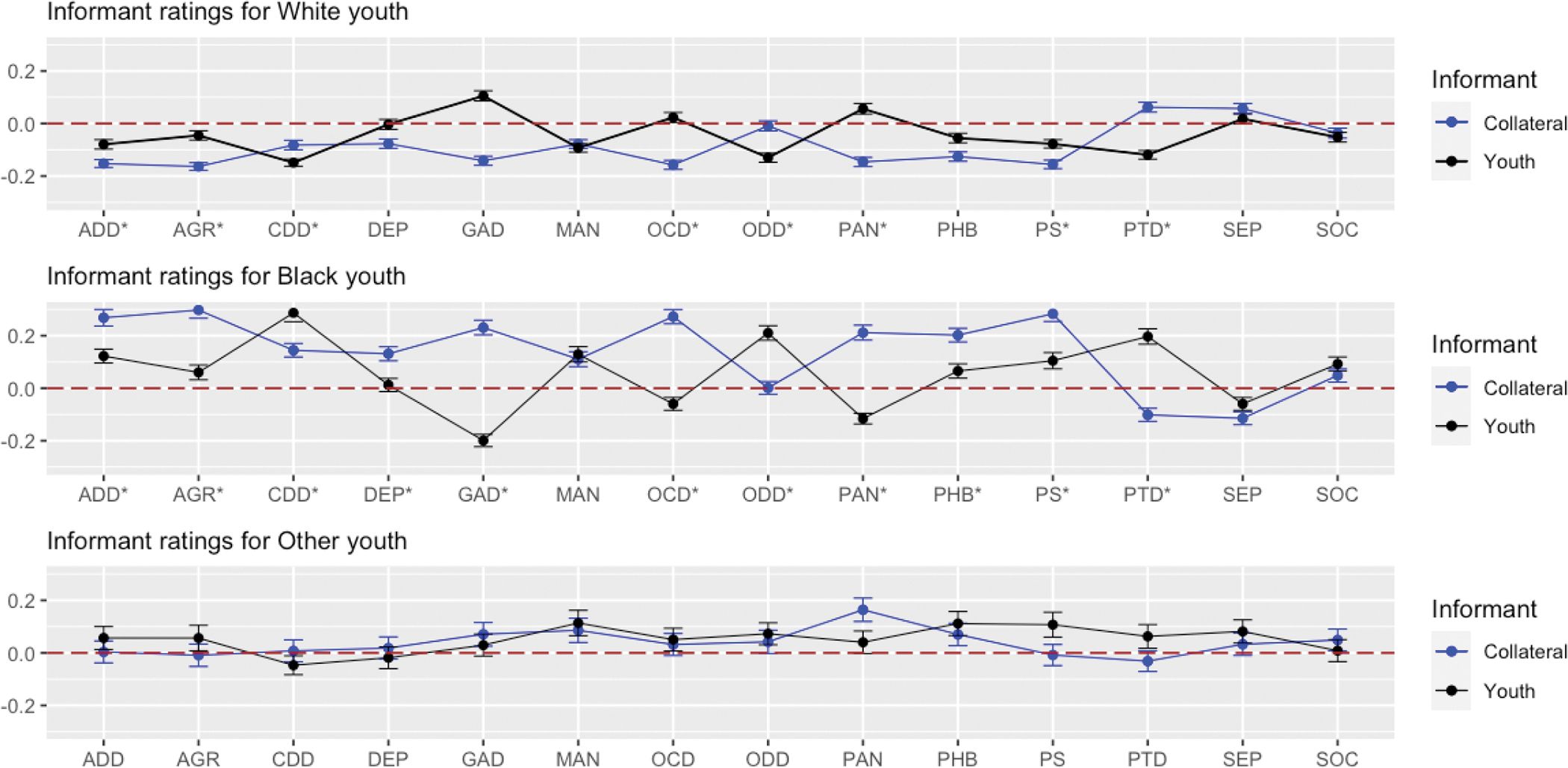
Youth and collateral (caregiver) psychopathology symptom domain level scores across race groups. Y-axis indicates domain level summary scores and are standardized z-scores; X-axes labels with * are statistically significant, analysis corrected for multiple comparisons with significance level set at <0.004.
Across SES, difference scores were higher than average for low SES and lower than average for middle and high SES across all domains with conduct showing the largest discrepancy; this arises from youth in the low SES group self-reporting more symptoms than their caregivers compared to both the middle and high SES groups.
Difference scores were higher than average for all disorder groups in all domains and lower than average for the TD group.
Network Analysis of Difference Scores
Network structure of difference scores for psychiatric disorders and the TD are presented in Figure 4. The network structure for all disorder groups and the TD group resulted only in positive edges indicating that when difference scores were higher in one domain, they also tended to be higher for all other interconnected domains. Across 14 psychopathology domains and 76 potential edges, the correlated domains are presented for each network. Among disorder categories, psychosis produced a sparse network with only two edges indicating no associations among domains. This is unlike other psychiatric disorders and TD group where the positive association between domain level difference scores were strong.
Figure 4:
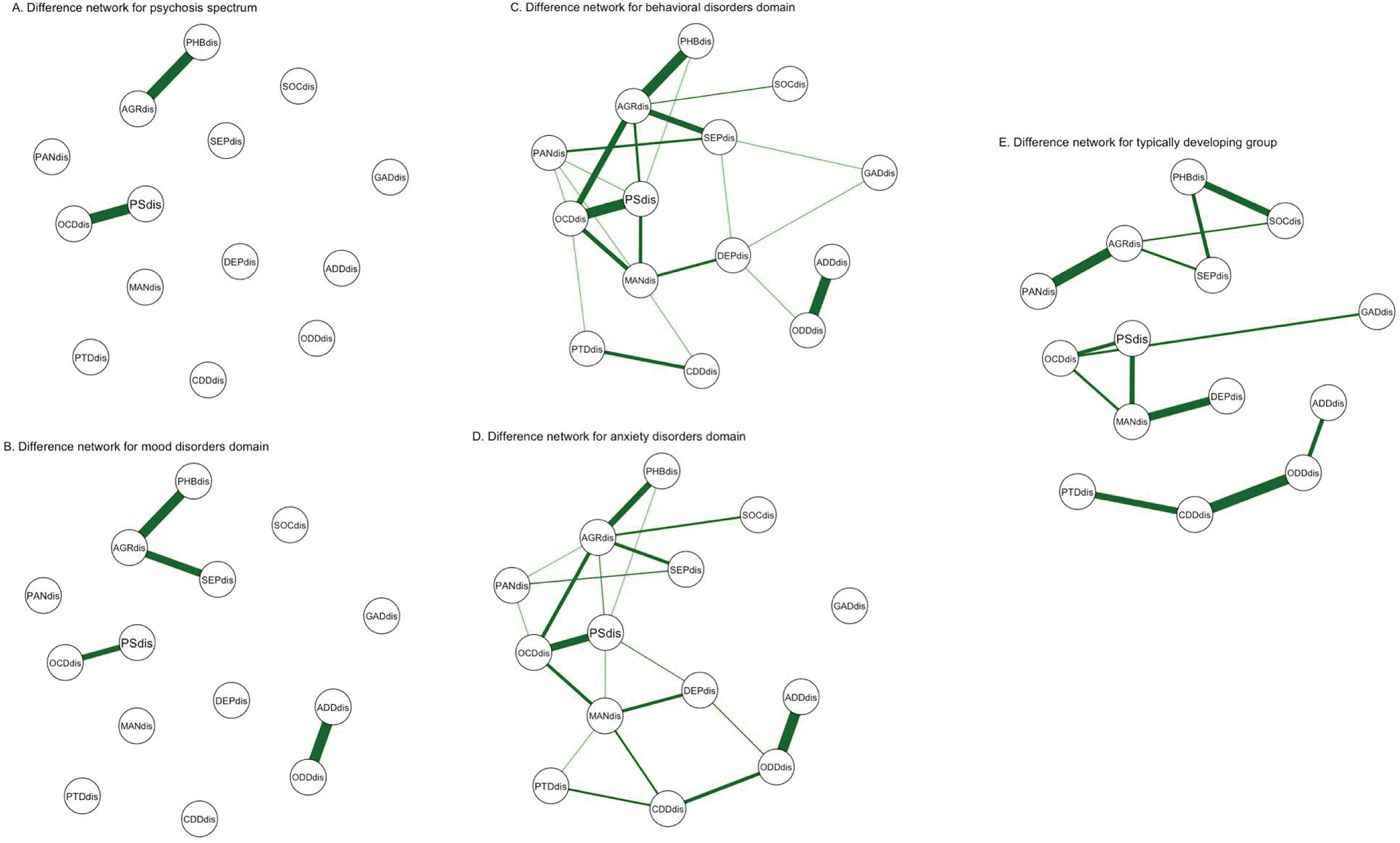
Difference score networks across major psychiatric disorder categories constructed using a graphical lasso or GLASSO method. ADDdis-Attention Deficit Hyperactivity difference score ; AGRdis- Agoraphobia difference score; CDDdis- Conduct disorder difference score ; DEPdis= Depression difference score ; GADdis- Generalized Anxiety difference score; MANdis - Mania difference score; OCDdis - Obsessive Compulsive difference score; ODDdis - Oppositional Defiant difference score ; PANdis - Panic difference score ; PHBdis - Specific Phobias difference score; PSdis -Psychosis Spectrum difference score; SEPdis -Separation Anxiety difference score; SOCdis - Social Anxiety difference score
NCT differences were seen only for global strength across the networks. Psychosis and TD networks were significantly different (p = 0.04); mood network was significantly different from anxiety (p = 0.03), behavior (p = 0.03) and TD networks (p = 0.001). Network invariance was not significant across disorders and TD.
Discussion
Our study examined youth-caregiver concordance and discrepancies in psychopathology symptoms as well patterns of discrepancies across demographic and major psychiatric disorder categories. These differences are observed in not just the criterion symptoms (i.e., the symptoms that define the psychopathology or diagnosis) of the disorder but also across other domains assessed. We report differences in network structure of difference scores for specific psychiatric disorders compared to TD group.
Youth and caregiver reported symptoms show different patterns of interrelationships
We found that youth and caregiver reported symptoms show high interconnectedness in their network structure with several psychopathology symptoms showing co-occurring relationships. The negative relationship between GA and conduct was seen in both youth and caregiver networks suggesting some similarity in symptom relationships regardless of the source of the information. Negative correlations between conduct and generalized anxiety disorder symptoms are documented in the literature (Humphreys et al., 2012; Kessler et al., 2005). Comorbid anxiety in conduct disorder has been hypothesized to offer a protective role counteracting the effects of conduct disorder (Short et al., 2016) and could explain the observed negative association regardless of who is providing the information.
There were also other significant differences between the youth and caregiver symptom networks. In addition to the negative association between conduct and general phobia, the PTD node in the caregiver network had only 3 connections to other domains (depression, separation, and conduct) when compared to the youth network. The PTD node in youth was additionally associated with psychosis spectrum, mania, OC and panic (Figure 1) showing the range of co-occurring symptoms observed with an internalizing condition such as PTD when self-reported. These findings highlight the value of distinct but important information that could be obtained when data is collected from multiple sources.
The most central or interconnected domain in the youth network was depression. This is important as youth with depression often carry a high family loading for psychiatric disorders and are at increased risk for a protracted clinical course (Birmaher et al., 2004). Our findings lend support to the importance of screening youth for depressive symptoms for early identification and intervention given its comorbidity with other psychopathologies. In contrast, the most interconnected domain in the caregiver network was OD. This observation is not surprising given that OD is a characteristic externalizing disorder and caregivers’ identity these overt symptoms more often when compared to internalizing disorders. Studies investigating informant discrepancies have found that parents tend to overreport externalizing symptoms such as OD symptoms in children who have ADH and other anxiety disorders (Humphreys et al., 2012; McNeilis et al., 2018). The strongest edge observed in our caregiver network was between ADH and OD symptoms. These findings highlight the importance of obtaining symptom information from both the youth as well as their caregivers for accurate mental health assessment and evaluation.
Youth-caregiver discrepancies are pronounced in Black Youth and Youth in the Low SES group.
Discrepancies between parent and youth reports on psychopathology symptoms have been consistently reported in the literature (Crystal et al., 2001; Curhan et al., 2020; De Los Reyes, 2013; De Los Reyes et al., 2008, 2013; Ferdinand et al., 2004; Kassam-Adams et al., 2006; McWey et al., 2018; Salbach-Andrae et al., 2009; Schiltz et al., 2021). In clinical samples parents tend to overreport symptoms for 11–17-year-olds in internalizing as well as externalizing conditions (Salbach-Andrae et al., 2009). Our study findings show that youth self-report and caregiver reported symptoms have limited concordance. In our sample the discrepancies in reported symptoms varied by age group—age indexes neurodevelopment and we identified greater discrepancies in our youngest sample.
Greater directional discrepancies with children reporting more symptoms than parents is predictive of greater internalizing effects but parents reporting greater symptoms could point to greater severity of symptoms as in the case of depression (Guion et al., 2009; Pelton & Forehand, 2001). In our sample, in contrast to White and Other youth, Black youth underreported depression symptoms compared to caregivers (t = −3.26, df = 3167.8, p = 0.001). Self-reports of depression are useful in identifying the current depression status whereas parent reports are useful for predicting future depression (Lau et al., 2004). Because our study is cross-sectional, we are unable to make any prospective estimations on depression. We also report higher than average difference scores for Black youth compared to White youth as well as youth-caregiver discrepancies across multiple other domains. Greater discrepancies are also seen in the low SES group compared to the middle and high SES groups. These findings suggest a greater need to further study the causes, potential interaction effects and the implications of the discrepancy specifically observed in Black youth and youth of low SES. For example, clinicians use both youth and their caregivers’ reports to evaluate and diagnose mental health conditions. It is unclear how clinicians account for discrepant reports in their evaluation, diagnosis, and subsequent treatment decisions. This is particularly important given that Black population and those from low SES groups experience significant obstacles to receiving mental health care and experience health disparities including receiving poor quality of mental health care (Primm et al., 2010).
‘Other’ youth had discrepancies higher than White youth but less than Black youth. Other youth participants in our study includes everyone who self-reported their racial identity as either Asians, Native Americans, Alaska Natives or multiracial. Though the role of cultural differences in symptom expressions, distress thresholds (Lau et al., 2004) and intergenerational acculturation on informant discrepancies for Asians and other immigrant groups (Nguyen et al., 2018) is documented, we do not make any such inferences in our study given our Other youth sample is heterogeneous.
Across sex categories, the largest discrepancy noted was for agoraphobia with higher-than-average scores for females with youth overreporting symptoms and lower than average for males with youth underreporting symptoms compared to caregivers. Agoraphobia was the most central symptom for females. These findings align with reports that agoraphobia is diagnosed more commonly in females than males and is possibly explained by the influence of low independence and autonomy in agoraphobia and sex relationships (Bekker, 1996; Tibi et al., 2015).
Youth-caregiver discrepancy patterns across disorders
Caregivers’ reports were higher than average across most domains for psychosis, mood and anxiety categories, were similar to youth reports for behavior and were lower than average for TD. Though the greatest discrepancy in youth-caregiver reports was seen for psychosis, the difference score network was very sparse with only two edges; the behavioral disorder network had the most connected edges. The association between ADH and OD difference scores was consistently the strongest edge for TD and all disorders except psychosis spectrum. ADH and OD are both externalizing conditions that often co-occur (Harvey et al., 2016) with comorbidity rates ranging between 42–93% (Jensen et al., 1997). They both have phenomenological similarities that are common in normal development as well as overlapping symptoms that are common to mood, behavior and anxiety conditions such as impulsivity (Avila et al., 2004), social and peer relationship problems arising from decreased resistance to provocation from peers (Frankel & Feinberg, 2002). The absence of association between ADH and OD in psychosis spectrum could reflect the distinct pathological nature of psychosis spectrum symptoms in contrast to mood, behavior and anxiety disorders where “abnormality” is considered relevant only if manifestations are beyond a normal range or threshold.
Psychosis spectrum has distinct youth-caregiver discrepancy patterns
Compared to TD and other disorders, in psychosis spectrum youth-caregiver difference score associations were limited to OC, general phobia and agoraphobia domains. The difference score network for psychosis spectrum was also significant different from TD group. As reported by others (Ooi et al., 2017), we also report the lowest youth-caregiver concordance for psychosis symptoms. In the psychosis spectrum this low concordance is limited to just psychosis spectrum symptoms and domains which are known to be strongly associated with it, such as OC and agoraphobia. These distinct youth-caregiver discrepancies potentially arise from specific psychopathology characteristics of psychosis spectrum. For example, impaired insight i.e., impaired self-awareness of illness is a characteristic feature of psychosis spectrum but not depression. It is thus not surprising that insight impairment leads to greater discrepancies for psychosis specific symptoms but not depressive symptoms. To further understand the mechanisms that drives these relationships and how psychopathology characteristics modulate these patterns is beyond the scope of this study but warrants further investigation.
Implications for psychiatric nursing practice and research
As the first to often assess mental health concerns and/or crisis at point of care, findings from this study holds significant relevance for psychiatric nurses. For youth mental health evaluations, where obtaining collateral information from caregivers is critical to inform diagnostic and care decisions, these discrepancies are important factors that needs to accounted for during such evaluations. Future studies that explicitly examines the causes of such youth-caregiver discrepancies, the interactive effects of race and SES on how youth and caregivers identify symptoms and the implications of such discrepancies on access to mental health care services is warranted given the significant disparities that already exist for Black and other minority youth. Further research is needed to examine the implications of low concordance in how youth and caregivers report psychosis symptoms. Given that psychotic disorders present in late adolescence or early adulthood and that early intervention is key to preventing long term adverse outcomes in psychosis, such a line of inquiry could potentially aid early diagnosis.
Limitations
Our study findings are limited in that the symptoms we used to construct the difference scores are limited to the ones that were consistently reported by youth-caregiver dyads and as such we do not have all criterion symptoms (i.e., all symptoms that define a specific diagnosis) for disorders or psychopathology domains. One criticism of using difference scores is that mathematically similar and clinically interpretable results can be obtained from the informant scores themselves. But in our study, we exploit this mathematical similarity to account for the effects of informants while attempting to understand psychopathology that correlate with discrepancies. Our study sample is a community based sample so findings may not generalize to specific clinical populations. But in our sample a significant proportion did meet criteria for clinically relevant symptoms, and we examined discrepancies for major psychiatric disorder groups. Investigation of discrepancies by a specific psychiatric diagnosis is beyond the scope of this study. Lastly, applying network analysis to understand interrelationships and patterns of associations of difference scores across multiple psychopathology domain is novel, but it is still at the associational level and therefore cannot determine causes or mechanisms of such discrepancies.
Conclusion
Youth-caregiver discrepancies are clinically useful in several ways: discrepancies provide valuable insights to aid accurate clinical assessment and diagnosis, and may even predict therapeutic responses in youth psychopathology (Becker-Haimes et al., 2018; De Los Reyes, 2011; Goolsby et al., 2018). Our study findings related to youth-caregiver concordance align with what is already known. We report sociodemographic differences in youth and caregiver reports of psychopathology symptoms extending results from previous studies and underscore the importance of accounting for these factors in psychopathology assessment. Future studies that explicitly examines the interactive effects and implications of race and SES on how youth and caregivers identify symptoms is warranted given the significant disparities that currently exist for Black youth and youth from lower SES groups. Our findings show discrepancy patterns especially in psychosis which is different from other major disorders and is likely from phenomenological differences in psychosis compared to mood, anxiety, behavioral disorders as well as typically developing youth. Since our study findings are from a community sample, these findings could be potentially useful for screening and/or early identification of clinically at-risk youth in community or general practice settings (Golembo-Smith et al., 2014). Future studies are needed to determine whether our findings on discrepant patterns can be leveraged to identify youth who are at increased risk for developing psychosis and how such discrepancies can be used as a tool to aid early identification especially in psychosis.
Supplementary Material
Funding:
The authors would like to acknowledge funding from the National Institute of Mental Health 5T32MH019112 (RX, JHT). This work was also supported by NIH grant MH-107235, MH-089983, MH-096891, MH-P50MH06891, K08-MH-079364 (MEC), the Dowshen Neuroscience Fund, and the Lifespan Brain Institute of Children’s Hospital of Philadelphia and Penn Medicine, University of Pennsylvania. The funding organizations had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
References
- Ambrosini PJ (2000). Historical development and present status of the schedule for affective disorders and schizophrenia for school-age children (K-SADS). Journal of the American Academy of Child and Adolescent Psychiatry, 39(1), 49–58. 10.1097/00004583-200001000-00016 [DOI] [PubMed] [Google Scholar]
- Avila C, Cuenca I, Félix V, Parcet M-A, & Miranda A (2004). Measuring impulsivity in school-aged boys and examining its relationship with ADHD and ODD ratings. Journal of Abnormal Child Psychology, 32(3), 295–304. 10.1023/b:jacp.0000026143.70832.4b [DOI] [PubMed] [Google Scholar]
- Becker-Haimes EM, Jensen-Doss A, Birmaher B, Kendall PC, & Ginsburg GS (2018). Parent-youth informant disagreement: Implications for youth anxiety treatment. Clinical Child Psychology and Psychiatry, 23(1), 42–56. 10.1177/1359104516689586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekker MHJ (1996). Agoraphobia and gender: A review. Clinical Psychology Review, 16(2), 129–146. 10.1016/0272-7358(96)00012-8 [DOI] [Google Scholar]
- Birmaher B, Williamson DE, Dahl RE, Axelson DA, Kaufman J, Dorn LD, & Ryan ND (2004). Clinical presentation and course of depression in youth: does onset in childhood differ from onset in adolescence? Journal of the American Academy of Child and Adolescent Psychiatry, 43(1), 63–70. 10.1097/00004583-200401000-00015 [DOI] [PubMed] [Google Scholar]
- Cohen J (1960). A Coefficient of Agreement for Nominal Scales. Educational and Psychological Measurement, 20(1), 37–46. 10.1177/001316446002000104 [DOI] [Google Scholar]
- Crystal DS, Ostrander R, Chen RS, & August GJ (2001). Multimethod assessment of psychopathology among DSM-IV subtypes of children with attention-deficit/hyperactivity disorder: self-, parent, and teacher reports. Journal of Abnormal Child Psychology, 29(3), 189–205. 10.1023/a:1010325513911 [DOI] [PubMed] [Google Scholar]
- Curhan AL, Rabinowitz JA, Pas ET, & Bradshaw CP (2020). Informant discrepancies in internalizing and externalizing symptoms in an at-risk sample: The role of parenting and school engagement. Journal of Youth and Adolescence, 49(1), 311–322. 10.1007/s10964-019-01107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A (2011). Introduction to the Special Section: More Than Measurement Error: Discovering Meaning Behind Informant Discrepancies in Clinical Assessments of Children and Adolescents. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 40(1), 1–9. 10.1080/15374416.2011.533405 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A (2013). Strategic objectives for improving understanding of informant discrepancies in developmental psychopathology research. Development and Psychopathology, 25(3), 669–682. 10.1017/S0954579413000096 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Goodman KL, Kliewer W, & Reid-Quiñones K (2008). Whose depression relates to discrepancies? Testing relations between informant characteristics and informant discrepancies from both informants’ perspectives. Psychological Assessment, 20(2), 139–149. 10.1037/1040-3590.20.2.139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes A, & Kazdin AE (2005). Informant discrepancies in the assessment of childhood psychopathology: a critical review, theoretical framework, and recommendations for further study. Psychological Bulletin, 131(4), 483–509. 10.1037/0033-2909.131.4.483 [DOI] [PubMed] [Google Scholar]
- De Los Reyes A, Thomas SA, Goodman KL, & Kundey SMA (2013). Principles underlying the use of multiple informants’ reports. Annual Review of Clinical Psychology, 9, 123–149. 10.1146/annurev-clinpsy-050212-185617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duhig AM, Renk K, Epstein MK, & Phares V (2000). Interparental Agreement on Internalizing, Externalizing, and Total Behavior Problems: A Meta-analysis. Clinical Psychology: Science and Practice, 7(4), 435–453. 10.1093/clipsy.7.4.435 [DOI] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50(1), 195–212. 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ermel J, Carter CS, Gold JM, MacDonald AW 3rd, Daniel Ragland J, Silverstein SM, Strauss ME, & Barch DM (2017). Self versus informant reports on the specific levels of functioning scale: Relationships to depression and cognition in schizophrenia and schizoaffective disorder. Schizophrenia Research. Cognition, 9, 1–7. 10.1016/j.scog.2017.04.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferdinand RF, van der Ende J, & Verhulst FC (2004). Parent-Adolescent Disagreement Regarding Psychopathology in Adolescents From the General Population as a Risk Factor for Adverse Outcome. Journal of Abnormal Psychology, 113(2), 198–206. 10.1037/0021-843X.113.2.198 [DOI] [PubMed] [Google Scholar]
- Fisher RA (1992). Statistical Methods for Research Workers. In Kotz S & Johnson NL (Eds.), Breakthroughs in Statistics: Methodology and Distribution (pp. 66–70). Springer; New York. 10.1007/978-1-4612-4380-9_6 [DOI] [Google Scholar]
- Frankel F, & Feinberg D (2002). Social problems associated with ADHD vs. ODD in children referred for friendship problems. Child Psychiatry and Human Development, 33(2), 125–146. 10.1023/a:1020730224907 [DOI] [PubMed] [Google Scholar]
- Golembo-Smith S, Bachman P, Senturk D, Cannon TD, & Bearden CE (2014). Youth-caregiver Agreement on Clinical High-risk Symptoms of Psychosis. Journal of Abnormal Child Psychology, 42(4), 649–658. 10.1007/s10802-013-9809-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goolsby J, Rich BA, Hinnant B, Habayeb S, Berghorst L, De Los Reyes A, & Alvord MK (2018). Parent–Child Informant Discrepancy is Associated with Poorer Treatment Outcome. Journal of Child and Family Studies, 27(4), 1228–1241. 10.1007/s10826-017-0946-7 [DOI] [Google Scholar]
- Guion K, Mrug S, & Windle M (2009). Predictive value of informant discrepancies in reports of parenting: relations to early adolescents’ adjustment. Journal of Abnormal Child Psychology, 37(1), 17–30. 10.1007/s10802-008-9253-5 [DOI] [PubMed] [Google Scholar]
- Harvey EA, Breaux RP, & Lugo-Candelas CI (2016). Early development of comorbidity between symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD). Journal of Abnormal Psychology, 125(2), 154–167. 10.1037/abn0000090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys KL, Aguirre VP, & Lee SS (2012). Association of anxiety and ODD/CD in children with and without ADHD. Journal of Clinical Child and Adolescent Psychology: The Official Journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 41(3), 370–377. 10.1080/15374416.2012.656557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen PS, Martin D, & Cantwell DP (1997). Comorbidity in ADHD: implications for research, practice, and DSM-V. Journal of the American Academy of Child and Adolescent Psychiatry, 36(8), 1065–1079. 10.1097/00004583-199708000-00014 [DOI] [PubMed] [Google Scholar]
- Kassam-Adams N, García-España JF, Miller VA, & Winston F (2006). Parent-child agreement regarding children’s acute stress: the role of parent acute stress reactions. Journal of the American Academy of Child and Adolescent Psychiatry, 45(12), 1485–1493. 10.1097/01.chi.0000237703.97518.12 [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, & Walters EE (2005). Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62(6), 617–627. 10.1001/archpsyc.62.6.617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein RG (1991). Parent-child agreement in clinical assessment of anxiety and other psychopathology: A review. Journal of Anxiety Disorders, 5(2), 187–198. 10.1016/0887-6185(91)90028-R [DOI] [Google Scholar]
- Kobayashi H, Nemoto T, Koshikawa H, Osono Y, Yamazawa R, Murakami M, Kashima H, & Mizuno M (2008). A self-reported instrument for prodromal symptoms of psychosis: testing the clinical validity of the PRIME Screen-Revised (PS-R) in a Japanese population. Schizophrenia Research, 106(2–3), 356–362. 10.1016/j.schres.2008.08.018 [DOI] [PubMed] [Google Scholar]
- Laird RD (2020). Analytical challenges of testing hypotheses of agreement and discrepancy: Comment on Campione-Barr, Lindell, and Giron (2020) [Review of Analytical challenges of testing hypotheses of agreement and discrepancy: Comment on Campione-Barr, Lindell, and Giron (2020)]. Developmental Psychology, 56(5), 970–977. 10.1037/dev0000763 [DOI] [PubMed] [Google Scholar]
- Laird RD, & De Los Reyes A (2013). Testing Informant Discrepancies as Predictors of Early Adolescent Psychopathology: Why Difference Scores Cannot Tell You What You Want to Know and How Polynomial Regression May. Journal of Abnormal Child Psychology, 41(1), 1–14. 10.1007/s10802-012-9659-y [DOI] [PubMed] [Google Scholar]
- Lau AS, Garland AF, Yeh M, Mccabe KM, Wood PA, & Hough RL (2004). Race/Ethnicity and Inter-Informant Agreement in Assessing Adolescent Psychopathology. Journal of Emotional and Behavioral Disorders, 12(3), 145–156. 10.1177/10634266040120030201 [DOI] [Google Scholar]
- McNeilis J, Maughan B, Goodman R, & Rowe R (2018). Comparing the characteristics and outcomes of parent- and teacher-reported oppositional defiant disorder: findings from a national sample. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 59(6), 659–666. 10.1111/jcpp.12845 [DOI] [PubMed] [Google Scholar]
- McWey LM, Cui M, Cooper AN, & Ledermann T (2018). Caregiver-adolescent disagreement on the mental health of youth in foster care: The moderating role of the caregiver relationship. Child Maltreatment, 23(3), 294–302. 10.1177/1077559518769375 [DOI] [PubMed] [Google Scholar]
- Merikangas, Avenevoli S, Costello EJ, Koretz D, & Kessler RC (2009). National comorbidity survey replication adolescent supplement (NCS-A): I. Background and measures. Journal of the American Academy of Child and Adolescent Psychiatry, 48(4), 367–379. 10.1097/CHI.0b013e31819996f1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas Dierker, L. C., & Szatmari P (1998). Psychopathology among offspring of parents with substance abuse and/or anxiety disorders: a high-risk study. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 39(5), 711–720. https://www.ncbi.nlm.nih.gov/pubmed/9690934 [PubMed] [Google Scholar]
- Miller TJ, McGlashan TH, Rosen JL, Cadenhead K, Cannon T, Ventura J, McFarlane W, Perkins DO, Pearlson GD, & Woods SW (2003). Prodromal assessment with the structured interview for prodromal syndromes and the scale of prodromal symptoms: predictive validity, interrater reliability, and training to reliability. Schizophrenia Bulletin, 29(4), 703–715. 10.1093/oxfordjournals.schbul.a007040 [DOI] [PubMed] [Google Scholar]
- Nguyen DJ, Kim JJ, Weiss B, Ngo V, & Lau AS (2018). Prospective relations between parent-adolescent acculturation conflict and mental health symptoms among Vietnamese American adolescents. Cultural Diversity & Ethnic Minority Psychology, 24(2), 151–161. 10.1037/cdp0000157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okewole AO, Ajogbon D, Adeniji AA, Omotoso OO, Awhangansi SS, Fasokun ME, Agboola AA, & Oyekanmi AK (2015). Psychosis risk screening among secondary school students in Abeokuta, Nigeria: Validity of the Prodromal Questionnaire - Brief Version (PQ-B). Schizophrenia Research, 164(1–3), 281–282. 10.1016/j.schres.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Ooi YP, Glenn AL, Ang RP, Vanzetti S, Falcone T, Gaab J, & Fung DS (2017). Agreement Between Parent- and Self-Reports of Psychopathic Traits and Externalizing Behaviors in a Clinical Sample. Child Psychiatry and Human Development, 48(1), 151–165. 10.1007/s10578-016-0659-y [DOI] [PubMed] [Google Scholar]
- Pelton J, & Forehand R (2001). Discrepancy between Mother and Child Perceptions of Their Relationship: I. Consequences for Adolescents Considered within the Context of Parental Divorce. Journal of Family Violence, 16(1), 1–15. 10.1023/A:1026527008239 [DOI] [Google Scholar]
- Primm AB, Vasquez MJT, Mays RA, Sammons-Posey D, McKnight-Eily LR, Presley-Cantrell LR, McGuire LC, Chapman DP, & Perry GS (2010). The role of public health in addressing racial and ethnic disparities in mental health and mental illness. Preventing Chronic Disease, 7(1), A20. https://www.ncbi.nlm.nih.gov/pubmed/20040235 [PMC free article] [PubMed] [Google Scholar]
- Rosen AFG, Moore TM, Calkins ME, Gur RC, & Gur RE (2019). Effects of Skip-Logic on the Validity of Dimensional Clinical Scores: A Simulation Study. Psychopathology, 52(6), 358–366. 10.1159/000505075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabbag S, Twamley EW, Vella L, Heaton RK, Patterson TL, & Harvey PD (2012). Predictors of the accuracy of self assessment of everyday functioning in people with schizophrenia. Schizophrenia Research, 137(1), 190–195. 10.1016/j.schres.2012.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salbach-Andrae H, Klinkowski N, Lenz K, & Lehmkuhl U (2009). Agreement between youth-reported and parent-reported psychopathology in a referred sample. European Child & Adolescent Psychiatry, 18(3), 136–143. 10.1007/s00787-008-0710-z [DOI] [PubMed] [Google Scholar]
- Schiltz HK, Magnus BE, McVey AJ, Haendel AD, Dolan BK, Stanley RE, Willar KA, Pleiss SJ, Carson AM, Carlson M, Murphy C, Vogt EM, Yund BD, & Van Hecke AV (2021). A psychometric analysis of the Social Anxiety Scale for adolescents among youth with autism spectrum disorder: Caregiver-adolescent agreement, factor structure, and validity. Assessment, 28(1), 100–115. 10.1177/1073191119851563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Short RML, Sonuga-Barke EJS, Adams WJ, & Fairchild G (2016). Does comorbid anxiety counteract emotion recognition deficits in conduct disorder? Journal of Child Psychology and Psychiatry, and Allied Disciplines, 57(8), 917–926. 10.1111/jcpp.12544 [DOI] [PubMed] [Google Scholar]
- Tibi L, van Oppen P, Aderka IM, van Balkom AJLM, Batelaan NM, Spinhoven P, Penninx BW, & Anholt GE (2015). An admixture analysis of age of onset in agoraphobia. Journal of Affective Disorders, 180, 112–115. 10.1016/j.jad.2015.03.064 [DOI] [PubMed] [Google Scholar]
- van Borkulo C, Boschloo L, Kossakowski J, Tio P, & Waldorp L (2017). Comparing network structures on three aspects: A permutation test. 10.13140/RG.2.2.29455.38569 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


