Abstract
This case report describes the use of the guided endodontics for a non-surgical endodontic retreatment of the mandibular molar. A 38-year-old female reported apical swelling and localized pain on the tooth #30, exacerbated when chewing hard food. Periapical radiographic examination showed pulp canal obliteration in the apical third associated with extensive radiolucent area. Cone-beam computed tomography (CBCT) images were requested to support the diagnosis and enable preparation of a surgical guide, used to direct access to the canals that were obliterated and incompletely filled. The follow-up at 24 months radiographically showed completely healed apical area in the involved tooth. This non-surgical technique demonstrated efficacy in case resolution.
Key Words: Cone-beam Computed Tomography, Endodontic, Guided Endodontics
Introduction
The success of endodontic treatment is measured by the tooth being clinically symptomless as well as the prevention or treatment of periapical pathologies. These biological objectives are achieved when the entire root canal system (RCS) is cleaned and disinfected with endodontic instruments and irrigation solutions, procedures that enable hermetic sealing of the RCS [1, 2].
Teeth with pulp canal obliterations (PCO) could be a challenge, especially because of the difficulties in locating and negotiating them to full working length, making the predictability of treatment outcomes uncertain even for experienced professionals [1, 3, 4]. PCO is characterized by progressive deposition of mineralized tissue in the root canal space; but the underlying mechanisms of PCO are unclear, and may be due to injury to the neurovascular supply of the pulp from dental trauma, carious lesions, abfraction, abrasion, pulp capping, occlusal imbalance, orthodontic treatment, harmful oral habits and individual aging [4, 5]. In some situations, the presence of incompletely filled teeth is observed in the day-to-day clinic, with the absence of a periapical pathological process and extremely tightened canals. This is certainly explained by the presence of a pulp remnant left in the root space, which, in the absence of infection, responds in a beneficial manner, with pulp obliteration [4, 5].
The occurrence of PCO increases the risks of iatrogenic errors such as excessive destruction of dental structures, perforation, glide path deviation and inadequate cleaning, shaping and obturation, leading to treatment failure [4, 5]. This failure can cause persistence of painful symptomatology and onset/growth of periapical lesions. In this context,the purpose of the endodontic retreatment is to completely remove the obturation material from the root canal and restore access to the apical foramen so that the entire RCS is properly cleaned, shaped, and obturated corroborating with periapical health [6, 7]. Nonsurgical endodontic retreatments, given the clinical complexities, require the use of resources to enable planning, facilitate its execution, and increase prognosis. Endodontic orientation is improved through cone-beam computed tomography (CBCT) images that provide 3D visualization of the areas to be treated [4, 8-10].
Guided endodontics, a recent approach, has been indicated for better management of teeth with partial or total obliterations of the canal [9, 11-13]. This technique uses a precise software (coDiagnostiXTM, Dental Wings Inc., Montreal, Canada), CBCT, and 3D scanning images to produce a surgical guide that directs the drill during access cavity preparation [7].
Although this technique will facilitate minimally invasive access to the obliterated canal [7, 9, 12], there are very few reports on its use in endodontic nonsurgical reinterventions [9, 14]. The aim of this study was to demonstrate that guided endodontics could be the treatment of choice in teeth that require root canal retreatment. In this case report, the tooth presented with apical obliteration in root canals adjacent to periapical lesion. These obliterations could have been present at the time of the first treatment or could have developed subsequently. Regardless of when it did occur, this approach showed to be an excellent tool to reach patency during retreatments.
Case Report
A Brazilian patient (38 years old, female, Caucasian) was referred to our institute for emergency treatment of tooth #30. The patient was healthy and presented without history, signs or symptoms of chronic diseases. Clinical inspection showed extensive coronary restoration, apical swelling, and positive percussion and palpation. Pulp vitality tests were negative. Periapical radiographic examination showed canals incompletely sealed with gutta-percha material (Figure 1A), associated with areas with severe obliteration in the distal canal. The final diagnosis was pulp necrosis with symptomatic apical periodontitis. Areas of hypercementosis in the apical region of the mesial and distal roots were also observed. The findings and treatment plan were completely explained to the patient, with all possible discomforts and risks, prognosis, cost and especially need for long-term follow-up were stressed to the patient and his consent was obtained. Hence, the first option was a nonsurgical root canal retreatment using Guided Endodontics.
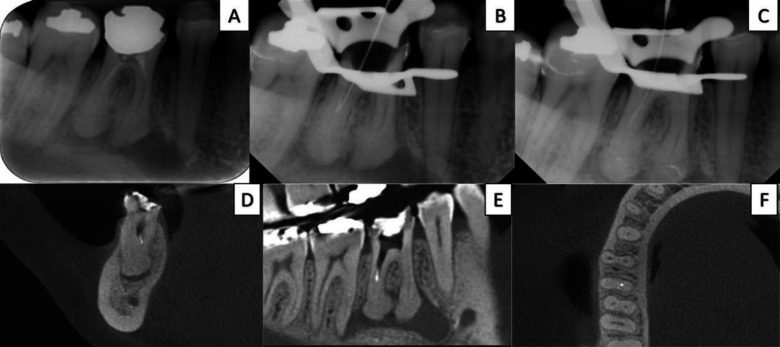
Figure 1.
A) Initial digital radiograph suggesting pulp canal obliteration, periapical radiolucent area, and inadequate root canal filling in the mandibular first molar; B, C) Transoperative radiographs exhibiting the gutta-percha removal and fractured file confirmation; D, E, F) CBCT sagittal, frontal, and axial preoperative images, respectively, revealing inadequate canal filling, distal pulp canal obliteration region and extensive periapical bone resorption area associated with the right mandibular first molar
The procedure was performed under local anaesthesia with inferior alveolar nerve block using 2% lidocaine with epinephrine 1:200000 (Alphacaine, DFL, Rio de Janeiro, RJ, Brazil). After previous restoration and carious tissue removal, a rubber dam had been placed. Under an optical microscope (DF Vasconcelos, SP, Brazil), three orifices of the canals were identified (mesiobuccal-MB, mesiolingual-ML, and distal-D). The gutta-percha cones were removed from the MB and ML canals with Reciproc R25 (VDW, Munich, Germany). The working lengths (WL) in both canals were determined with an electronic apex locator (Root ZX II; Morita, Osaka, Japan) using a C-Pilot #10 (VDW, Munich, Germany) and were confirmed with digital radiography. Then, the MB and ML canals were shaped and cleaned using a single-file system with reciprocating movement (Reciproc R25, VDW) with profuse irrigation using 5.25% sodium hypochlorite (NaOCl), 17% ethylenediaminetetraacetic acid (EDTA) and passive ultrasonic activation. In the distal (D) canal, severe calcification prevented the C-Pilot #10 from reaching the WL (Figure 1B). During the negotiation of the D canal, the C-Pilot #10 fractured (Figure 1C). The canals were dressed with calcium hydroxide (Ultracal, Ultradent do Brasil Produtos Odontológicos Ltda, Indaiatuba, SP, Brazil), and the tooth was sealed with a provisional glass ionomer restoration (Vidrion R, S.S. White Duflex, Rio de Janeiro, RJ, Brazil). CBCT images were requested to elucidate the tooth condition.
An evaluation of sagittal, frontal, and axial images showed extensive hypodense areas associated with the apex of #30 that presented two canals on the distal root (Figures 1D-F). Guided endodontic treatment was conducted to negotiate both canals and reach the WL in the distal root.
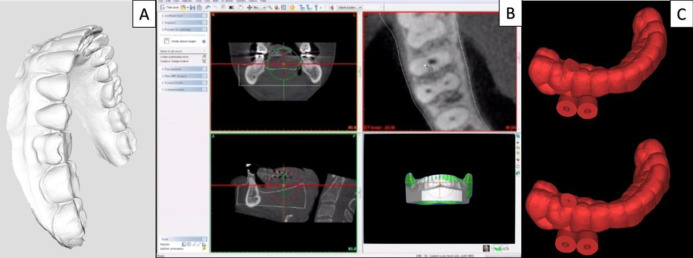
For accurate determination of the access guides, three-dimensional (3D) documentation was obtained by CBCT (I-Cat Classic, Kavo Ind, Saguaçu, Joinville, SC, Brazil). Intraoral scanning of the buccal cavity was performed using a TRIOS Color Pod scanner (3Shape A/S, Holmens Kanal 7.4, 1060
Copenhagen, Denmark, P: +45 7027 2620), which generated two models. Subsequently, the two models were aligned (Figures 2A-C) and exported to virtual planning software (Simplant 15.0 Pro®, Materialise®, Brussels, Belgium).
Figure 2.
A) 3D model of the oral cavity obtained with intraoral scanning; B) 3D root canal planned for access; C) virtual surgical guides constructed
Based on the features obtained from the CBCT images, a plan was developed. The diameter of the drill compatible with the root diameter to be accessed was determined. The drill needed had a diameter of 1.3 mm (Ref.: 103179; Neodent, Curitiba, PR, Brazil). A virtual copy of the drill was overlapped on the imagesat a position that allowed visual access to the apical root canals. The position of the drill was verified in three dimensions -axial, sagittal and coronal- to guarantee that the drill would reach the radiographically visible lumen of the distolingual (DL) canal. Two virtual guides were obtained using coDiagnostiX software (Dental Wings GmbH, Chemnitz, Germany).
The models were exported as a standard tessellation language (STL) file (a file format native to the stereolithography CAD software created by 3D Systems) and sent to a 3D printer (Objet Eden 260 V, Material: MED610, Stratasys Ltd., Minneapolis, MN, USA). The respective guide was created, ensuring the creation of a stabilization point on the tooth to be re-treated that would guarantee perfect stabilization of the guide and drill.
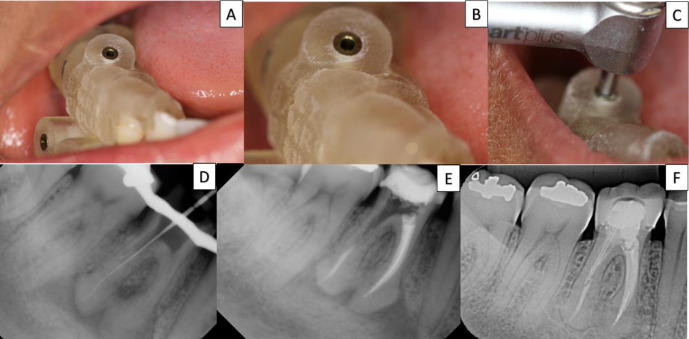
During the patient’s second visit, clinical procedures were performed under local anaesthesia. The provisory glass ionomer was removed. The guide was positioned on the teeth and the adaptation and drill position were verified (Figures 3A and 3B). Then, the drill was carefully guided into the DL canal at 350 rotations per min and 5 newtons (N) of torque with short apical force movements until the length planned was reached (Figure 3C). Posteriorly, the guides were removed, and the rubber dam was returned. Radiographs at different angles were obtained, confirming the correct direction of the drill. Surprisingly, a fragmented file was removed during the drill penetration. Then, a C-Pilot #10 (VDW) was introduced into the DL and distobuccal (DB) canals, and the WL were determined (Figure 3D). The working length was confirmed with an apical locator (Raypex 5, VDW, Munich, Germany). The chemical mechanical preparation was performed using ProTaper Next files (Dentsply Maillefer, Chemin du Verger, Ballaigues, Switzerland) until the X3 instrument reached the WL under constant irrigation with 5.25% NaOCl. The intracanal dressing with calcium hydroxide (Ultracal, Ultradent do Brasil Produtos Odontológicos Ltda, Indaiatuba, SP, Brazil) was maintained for 15 days.
Figure 3.
A, B, C) The guide was positioned on the teeth and the adaptation and drill position verification; D) radiographic examination proves that patency patience was achieved in the distal canals; E) obturation was performed; F) digital radiography 24-month follow-up showing complete healing of the lesion
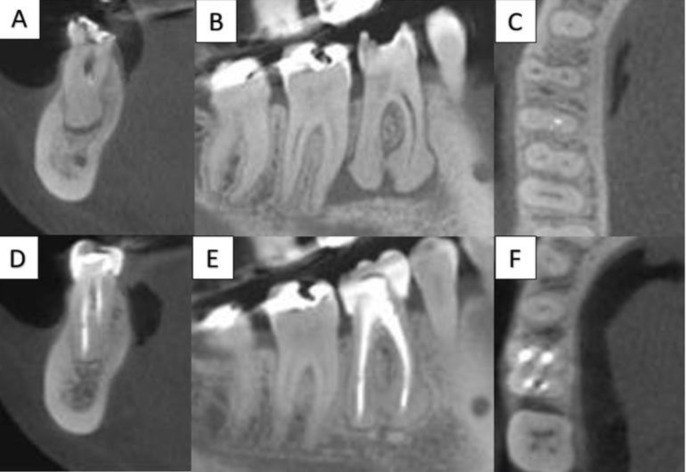
At the patient’s return visit, no symptoms were reported. Obturation was performed by vertical compaction technique using gutta-percha cones (Dentsply Maillefer, Chemin du Verger, Ballaigues, Switzerland) associated with an endodontic sealer (Sybron Kerr, Washington, USA) (Figure 3E). After the procedures, the patient was given all necessary information and referred for prosthetic rehabilitation. A considerable reduction of the periapical lesion, suggestive of complete healing, was observed at 24-month follow-up and confirmed by radiographic examination (Figure 3F) and CBCT (Figure 4).
Figure 4.
A, B, C) Initial CBCT images showing unsatisfactory obturation, pulp canal obliteration and apex-associated hypodense imaging in the mandibular first molar in comparison with; D, E, F) 24-month follow-up CBCT images demonstrating the complete reduction of the periradicular lesion
Discussion
Currently, the use of surgical guides in endodontic procedures is common [5, 9-11]. Traditionally, these guides have been recommended for accessing severely obliterated canals in single-root teeth [5, 12, 15, 16], adhesive fiber post-removal [9, 14], endodontic access to dens evaginatus [17], and periapical microsurgeries [6, 18]. This case report demonstrates a case report of the use of an EndoGuide for nonsurgical endodontic retreatment of one mandibular molar.
PCO is challenging in endodontic treatment. Several techniques, such as the use of CBCT, digital radiography, dental operating microscopy (DOM), and ultrasonic tips, have been indicated to overcome this challenge [5, 8]. However, DOM and ultrasonic tips, used in attempt to access obliterated root canals, have been associated with clinical success indices of approximately 74% [19]. When these modalities fail, guided endodontics can be indicated. As reported, this novel technique resolved an uncertain case, suggesting its efficiency. Furthermore, guided endodontics is a new option that does not require specific training, presents high predictability and guaranteed results in treatment. This method is becoming more accessible and does not require much investment by the operator [9, 15, 18].
CBCT has become an essential tool for endodontic practice. While providing 3D visualization of the structures examined, it facilitates diagnosis and allows for a more careful treatment plan [9, 10]. In the present case, CBCT enabled the detection of two canals in the distal root, that radiographic examination alone with a periapical could not ascertain. In addition, with CBCT, the obliteration was better visualized, especially by location and extension [17, 20-23]. The use of tomographic images is well established and is becoming progressively more accessible for clinical use. However, implementation of the EndoGuide for performing procedures is still limited since it requires computer-aided design, computer-aided manufacturing (CAD/CAM) software, and 3D-printing capability [2-26].
This case also reported the occurrence of a fractured file obliterating the glide path. After using the drill to access the apical segment of the canal, fragment removal was verified. This fact may suggest the mechanical action of the drill is able to displace fractured files in the canal. Therefore, we propose evaluating the possibility of indicating guided endodontics for the removal of file fragments that prevent access to the apical third of the root. Research and reports of similar clinical cases should be performed to confirm this possibility.
Although this case report describes the optimized use of guided endodontics in one retreatment case, clinical studies involving a larger number of patients and follow-up time are suggested to strengthen the evidence.
Conclusions
The EndoGuide technique demonstrated efficacy in resolving this retreatment case, as suggested in the two year follow-up at 24 months that revealed a completely healed apical area in the molar tooth. It seems that this technique can be indicated as a fast, available and accurate solution for endodontic therapy in calcified root canals.
Conflict of Interest:
‘None declared’.
References
- 1.Ricucci D, Siqueira JF Jr. Recurrent apical periodontitis and late endodontic treatment failure related to coronal leakage: a case report. J Endod. 2011;37(8):1171–5. doi: 10.1016/j.joen.2011.05.025. [DOI] [PubMed] [Google Scholar]
- 2.Ricucci D, Loghin S, Siqueira JF Jr. Exuberant Biofilm infection in a lateral canal as the cause of short-term endodontic treatment failure: report of a case. J Endod. 2013;39(5):712–8. doi: 10.1016/j.joen.2012.12.008. [DOI] [PubMed] [Google Scholar]
- 3.Torabinejad M, Corr R, Handysides R, Shabahang S. Outcomes of nonsurgical retreatment and endodontic surgery: a systematic review. J Endod. 2009;35(7):930–7. doi: 10.1016/j.joen.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 4.de Toubes KMS, de Oliveira PAD, Machado SN, Pelosi V, Nunes E, Silveira FF. Clinical Approach to Pulp Canal Obliteration: A Case Series. Iranian endodontic journal. 2017;12(4):527–33. doi: 10.22037/iej.v12i4.18006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Torres A, Shaheen E, Lambrechts P, Politis C, Jacobs R. Microguided Endodontics: a case report of a maxillary lateral incisor with pulp canal obliteration and apical periodontitis. Int Endod J. 2019;52(4):540–9. doi: 10.1111/iej.13031. [DOI] [PubMed] [Google Scholar]
- 6.Ye S, Zhao S, Wang W, Jiang Q, Yang X. A novel method for periapical microsurgery with the aid of 3D technology: a case report. BMC Oral Health. 2018;18(1):85. doi: 10.1186/s12903-018-0546-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Connert T, Krug R, Eggmann F, Emsermann I, ElAyouti A, Weiger R, et al. Guided Endodontics versus Conventional Access Cavity Preparation: A Comparative Study on Substance Loss Using 3-dimensional-printed Teeth. J Endod. 2019;45(3):327–31. doi: 10.1016/j.joen.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 8.Toubes KM, Tonelli SQ, Oliveira BJ, Duarte G, Nunes E, Silveira FF. Apical periodontitis associated with a calculus-like deposit: A case report of a rare fan-shaped manifestation. Ann Med Surg (Lond). 2019;41:1–5. doi: 10.1016/j.amsu.2019.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Maia LM, de Carvalho Machado V, da Silva N, Brito Junior M, da Silveira RR, Moreira Junior G, et al. Case Reports in Maxillary Posterior Teeth by Guided Endodontic Access. J Endod. 2019;45(2):214–8. doi: 10.1016/j.joen.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 10.Buchgreitz J, Buchgreitz M, Bjorndal L. Guided root canal preparation using cone beam computed tomography and optical surface scans - an observational study of pulp space obliteration and drill path depth in 50 patients. Int Endod J. 2019;52(5):559–68. doi: 10.1111/iej.13038. [DOI] [PubMed] [Google Scholar]
- 11.Krastl G, Zehnder MS, Connert T, Weiger R, Kuhl S. Guided Endodontics: a novel treatment approach for teeth with pulp canal calcification and apical pathology. Dent Traumatol. 2016;32(3):240–6. doi: 10.1111/edt.12235. [DOI] [PubMed] [Google Scholar]
- 12.Zehnder MS, Connert T, Weiger R, Krastl G, Kuhl S. Guided endodontics: accuracy of a novel method for guided access cavity preparation and root canal location. Int Endod J. 2016;49(10):966–72. doi: 10.1111/iej.12544. [DOI] [PubMed] [Google Scholar]
- 13.Chong BS, Dhesi M, Makdissi J. Computer-aided dynamic navigation: a novel method for guided endodontics. Quintessence Int. 2019;50(3):196–202. doi: 10.3290/j.qi.a41921. [DOI] [PubMed] [Google Scholar]
- 14.Perez C, Finelle G, Couvrechel C. Optimisation of a guided endodontics protocol for removal of fibre-reinforced posts. Aust Endod J. 2019 doi: 10.1111/aej.12379. [DOI] [PubMed] [Google Scholar]
- 15.Lara-Mendes STO, Barbosa CFM, Machado VC, Santa-Rosa CC. A New Approach for Minimally Invasive Access to Severely Calcified Anterior Teeth Using the Guided Endodontics Technique. J Endod. 2018;44(10):1578–82. doi: 10.1016/j.joen.2018.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Fonseca Tavares WL, Diniz Viana AC, de Carvalho Machado V, Feitosa Henriques LC, Ribeiro Sobrinho AP. Guided Endodontic Access of Calcified Anterior Teeth. J Endod. 2018;44(7):1195–9. doi: 10.1016/j.joen.2018.04.014. [DOI] [PubMed] [Google Scholar]
- 17.Mena-Alvarez J, Rico-Romano C, Lobo-Galindo AB, Zubizarreta-Macho A. Endodontic treatment of dens evaginatus by performing a splint guided access cavity. J Esthet Restor Dent. 2017;29(6):396–402. doi: 10.1111/jerd.12314. [DOI] [PubMed] [Google Scholar]
- 18.Giacomino CM, Ray JJ, Wealleans JA. Targeted Endodontic Microsurgery: A Novel Approach to Anatomically Challenging Scenarios Using 3-dimensional-printed Guides and Trephine Burs-A Report of 3 Cases. J Endod. 2018;44(4):671–7. doi: 10.1016/j.joen.2017.12.019. [DOI] [PubMed] [Google Scholar]
- 19.Wu D, Shi W, Wu J, Wu Y, Liu W, Zhu Q. The clinical treatment of complicated root canal therapy with the aid of a dental operating microscope. Int Dent J. 2011;61(5):261–6. doi: 10.1111/j.1875-595X.2011.00070.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinsky HM, Champleboux G, Sarment DP. Periapical surgery using CAD/CAM guidance: preclinical results. J Endod. 2007;33(2):148–51. doi: 10.1016/j.joen.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 21.21 Tavares WLF, de Carvalho Machado V, Fonseca FO, Vasconcellos BC, Magalhães LC, Viana ACD, et al. Guided Endodontics in Complex Scenarios of Calcified Molars. Iran Endod J. 2020;15(1):50–56. doi: 10.22037/iej.v15i1.26709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Anderson J, Wealleans J, Ray J. Endodontic applications of 3D printing. Int Endod J. 2018;51(9):1005–18. doi: 10.1111/iej.12917. [DOI] [PubMed] [Google Scholar]
- 23.Nayak A, Jain PK, Kankar PK, Jain N. Computer-aided design-based guided endodontic: A novel approach for root canal access cavity preparation. Proc Inst Mech Eng H. 2018;232(8):787–95. doi: 10.1177/0954411918788104. [DOI] [PubMed] [Google Scholar]
- 24.Ahn SY, Kim NH, Kim S, Karabucak B, Kim E. Computer-aided Design/Computer-aided Manufacturing-guided Endodontic Surgery: Guided Osteotomy and Apex Localization in a Mandibular Molar with a Thick Buccal Bone Plate. J Endod. 2018;44(4):665–70. doi: 10.1016/j.joen.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 25.van der Meer WJ, Vissink A, Ng YL, Gulabivala K. 3D Computer aided treatment planning in endodontics. J Dent. 2016;45:67–72. doi: 10.1016/j.jdent.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 26.Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C. Guided Modern Endodontic Surgery: A Novel Approach for Guided Osteotomy and Root Resection. J Endod. 2017;43(3):496–501. doi: 10.1016/j.joen.2016.11.001. [DOI] [PubMed] [Google Scholar]