Abstract
Human skin is characterized by significant diversity in color and tone, which are determined by the quantity and distribution of melanin pigment in the epidermis. Melanin absorbs and reflects ultraviolet radiation (UVR), preventing the damage to genomic DNA in the epidermis and degradation of collagen in the dermis; therefore, darker skin types are thought to be well protected from the photodamage because of the high melanin content. However, increased content of melanin in combination with the extrinsic stress factors causing inflammation such as excess UVR, allergic reactions, or injury can also frequently lead to cosmetic problems resulting in discoloration and scarring. This review summarizes current knowledge on histopathology and likely molecular signatures of one of the most common problems, post-inflammatory hyperpigmentation (PIH). The mechanisms proposed so far are subsequently discussed in the context of other factors characterizing darker skin types. This includes the common cellular features, organization of upper skin layers, and major biomarkers, with particular emphasis on increased propensities to systemic and localized inflammation. Enhanced or prolonged inflammatory responses can not only affect the process of melanogenesis but also have been implicated in injury-related skin pathologies and aging. Finally, we summarize the major cosmetic treatments for PIH and their known anti-inflammatory targets, which can be beneficial for darker skin tones and combined with broad-spectrum filters against UVR.
Keywords: post-inflammatory hyperpigmentation, skin ethnicity, inflammation, extrinsic aging
Introduction
Post-inflammatory hyperpigmentation (PIH) appears as dark and flattened spots on the body, which can range in color from brown to black depending on the extent of damage and skin tone.1 The loss of even skin tone is caused by the enhanced synthesis and deposition of melanin in skin cells; these changes are frequently aggravated by exposure to excess sun and ultraviolet radiation (UVR). PIH can also be triggered by inflammatory skin conditions such as acne and atopic dermatitis, allergies, injuries, and cosmetic procedures such as chemical peels, laser treatment and dermabrasion.1–3 Hyperpigmentation can affect any person, regardless of age and gender. However, it is well documented that it is more frequent and can be more severe in individuals with darkly pigmented skin (Fitzpatrick III–VI), who are less likely to use photoprotection. In addition, excess melanogenesis and irregular melanin deposition are also more severely enhanced by inflammatory processes such as acne in darker skin.4 The cause of discoloration may be linked to exogenous factors, such as the use of certain cosmetics and medications or exposure of the skin to mechanical injuries. Endogenous factors, including hormonal changes or systemic diseases, can also contribute to the more prevalent occurrence of PIH.5 The current treatments of PIH involve products that lighten the pigment, prevent its accumulation or stimulate cell renewal. Cosmetic treatments for discoloration reduction are frequently based on chemical peelings, other treatments include laser technology, which is used not only to lighten the discoloration but also to reduce the appearance of some scars. However, such procedures can lead to complications involving dermal melanin deposition and exasperating inflammation, particularly in dark skin.6,7 This indicates the unique requirements for the treatment of PIH in these skin types.
In this review, we highlight the molecular aspects of post-inflammatory hyperpigmentation, focusing on the inflammatory markers and the structural changes in the upper compartments of the skin affected by PIH. We then discuss the unique characteristics of darkly pigmented skin that could be linked to the increased susceptibility to PIH. These factors include the predisposition to systemic inflammation combined with documented differences in the molecular organization and cellular activity between lightly- and darkly pigmented skin. We conclude that the increased occurrence of PIH could be driven by chronic low-grade inflammation, likely affecting local responses to stress such as UVR, injury and cell senescence. Finally, we discuss the anti-inflammatory activity of some of the active ingredients with an inhibitory effect on melanogenesis, pointing at the potentially most beneficial non-invasive route for the treatment of PIH in dark skin.
Molecular Basis and Occurrence of PIH
One of the major mechanistic explanations for the origin of PIH points to inflammation, which contributes to the damage of the basal layer of the epidermis and acts as a trigger for melanocytes to release melanosomes containing pigment to the surrounding skin cells; the pigment granules can persist for a prolonged time leading to further discoloration of the epidermis.7 When PIH affects the epidermis, cytokines, chemokines, and reactive oxygen species (ROS) released during inflammation stimulate melanocyte growth as well as the synthesis of melanin and its transport into the surrounding keratinocytes. Among the physiological factors promoting these events are epidermal growth factor (EGF), interleukin-1 (IL-1), interleukin-6 (IL-6), tumor necrosis factor (TNF) as well as leukotrienes such as LTc4 and LTd4, prostaglandins E2 and D2, and thromboxane-2.1,8,9 The pigment is usually increased in the basal compartment of the epidermis, which is also accompanied by up-regulated expression of melanoma marker antibody (NKI/beteb) and metalloproteinase 2 enzyme (MMP-2).10
Damage to the basement membrane and basal keratinocytes, which release melanin in large quantities in response to inflammation, can also lead to PIH in the dermis. In the upper dermis, the pigment is phagocytosed by macrophages, giving the skin a darkened appearance; this type of hyperpigmentation can be either prolonged or permanent.1,11 It is also characterized by relatively lower levels of pigmentation in the epidermis; however, this is accompanied by enhanced perivascular infiltration of lymphocytes and increased expression of the macrophage marker CD68 and mast/stem cell growth factor receptor c-kit in the dermis.10
PIH is observed in all skin types; however, it is significantly more frequent and severe in darkly pigmented skin affecting the populations of African American, Hispanic, Middle Eastern, Pacific Islands, Native Americans, and Asian heritage.1,12 For example, a population study documented acne-induced PIH in around 47–65% of African American, Hispanic and Asian patients.13 PIH was also recorded in around 23% of Afro-Caribbean skin types per 1000 individuals included in the population study.14 Notably, the occurrence of PIH could correspond more to the degree of pigmentation than the individual ethnic background; for example, the Asian population is characterized by a broad spectrum of darker and lighter skin types, ie, Malays and Indians versus Chinese.15
These data indicate a direct link between the predisposition to the development of PIH and darker skin tone. The clinical profiles and pathophysiology of PIH also implicate a significant involvement of inflammation as one of the major factors contributing to hyperpigmentation in darker skin.
Skin Pigmentation and Predisposition to Inflammation at Systemic Levels
Recently, several studies have demonstrated the increased cases of impaired cutaneous vascular and microvascular function in African American individuals, which were more prevalent compared to European Americans and detected in healthy young adults, therefore not caused by aging. Flow-mediated dilation (FMD) and local skin heating measurements indicated attenuated responses.16–18 Such characteristics are thought to be associated with increased oxidative stress, reduced cutaneous vasodilation mediated by nitric oxide (NO), and impaired scavenging and enhanced production of superoxide radicals.18,19 Both the microvascular endothelial function and the oxidative stress could be significantly improved by supplementation of vitamin D, which is also known to be reduced with darker skin pigmentation.17 Individuals with darker skin could be also more prone to changes in the inflammatory profiles that are linked to low-grade chronic expression of the pro-inflammatory cytokines. Analyses of the population-based samples for the plasma cytokine profiles reveal the increased levels of several circulating inflammatory markers, such as IL-6 and C-reactive protein (CRP) in the bloodstream of African Americans compared to Mexican and light-skinned non-Hispanic Americans.20 The influence of ethnicity on the circulating cytokine levels has been also reported for tumor necrosis factor a (TNFα) in Mexican Americans and for interleukin-8 (IL-8) and granulocyte-colony-stimulating factor (G-CSF) in African Americans.21,22 Significant differences in the IL-6, CRP and fibrinogen (FBG) have been also documented through another population study involving middle-aged and older Japanese and African American participants in health and aging surveys, Midlife in Japan (MIDJA) and Midlife in the US (MIDUS). Mean systemic levels of all three pro-inflammatory markers were consistently lower in Japanese compared to African American individuals across the life span between 30 and 80 years of age; the increased levels of IL-6 also remained significant after the adjustment to the differences in body mass index (BMI). These differences were also reversely correlated with the levels of the soluble IL-6 receptor.23 Elevated levels of IL-6, which is produced mainly by lymphoid cells and adipocytes, have been associated with the risk of obesity and metabolic syndrome, indicating that the increase in the circulating cytokines and susceptibility to inflammation in African American individuals might be directly linked to the Western diet and lifestyle.23–25
Susceptibility to inflammation at systemic levels is also reflected by the immune signatures likely describing the darkly pigmented skin. For example, the skin of African Americans is more prone to the development of atopic dermatitis (AD), which is characterized by epidermal hyperplasia and hyperkeratosis.26 AD is directly linked to the multiple signaling pathways indicative of altered immune function, such as the upregulated activity of pro-inflammatory T helper cells Th2, Th17 and Th22 secreting interleukins, eosinophils, CRP and ferritin as well as B cell-mediated immunity and complement activation in the skin.27,28 Interestingly, due to inflammation AD frequently leads to the development of PIH in darkly pigmented skin.29 These data indicate that skin hyperpigmentation and impaired melanogenesis could be driven by inflammation at both systemic and localized levels. In addition, alterations in the pro-inflammatory pathways are also closely linked to changes in proliferation and differentiation profiles as well as the activity of skin cells, pointing to the likely differences in the structural organization and molecular signatures of lightly- and darkly pigmented skin.
Linking the Predisposition to PIH and Its Complications with Skin Type Differences on the Molecular Level
Skin is a complex organ composed of multiple layers that are communicating with each other through physical and signal transduction interactions involving defined biomarkers. Frequent occurrence of PIH in darkly pigmented skin can be placed in a broader context of the well-described differences in the architecture, cellular activity, and gene expression between lightly- and darkly pigmented skin types. In addition, a pro-inflammatory environment can also result in aberrant tissue remodeling, such as the events observed in the scarring. Excess scarring, including hypertrophic and keloid scars, is regarded as one of the complications of acne alongside PIH that also affects dark skin more frequently.30 Therefore, understanding the intrinsic differences between skin types on the cellular and molecular levels, particularly focusing on the epidermis and the epidermal-dermal junctions (DEJ) can offer an important step towards unraveling the mechanisms of PIH further.
Epidermis
A study comparing the epidermal thickness between the skin samples obtained from European and African skin biopsies revealed no significant variances.31 However, applications of 3D skin models constructed with site-matched fibroblasts and keratinocytes from European and African skin revealed marked differences in the epidermal morphology, pointing to more pronounced terminal differentiation and stratification of the European skin types.32 Gene expression at the transcriptomic and proteomic levels demonstrated the up-regulation of biomarkers involved in epidermal morphogenesis and lipid/ceramide metabolism, including keratin 14 (KRT14), keratin 10 (KRT10), filaggrin (FLG), filaggrin 2 (FLG2), choline transporter SLC44A5, γ-glutamylcyclotransferase (GGCT) and caspase-14 (CASP14). The differences in the patterns of epidermal differentiation and stratification could be attributed to enhanced synthesis and processing of FLG and FLG2 in the European skin type model. In contrast, the African skin type model was characterized by decreased expression and accumulation of the protein in less mature layers of the epidermis. Decreased terminal differentiation of keratinocytes in the African skin model was also indicated by up-regulated levels of the inhibitor of epidermal desquamation, SPINK6, and basal layer marker α6/β4 integrin.32 These specific profiles point to the likely less robust skin barrier and molecular signatures overlapping with the inflammatory skin disorders. Increased predisposition to inflammation through pro-inflammatory genes TNF-α and IL-32 could be also detected in full-thickness skin biopsies from healthy African Americans when compared to European individuals.16 Decreased terminal differentiation of keratinocytes and organization of the stratum corneum was additionally demonstrated in the keloid scars, which affect the darkly pigmented skin more frequently.33,34
Epidermal barrier activity can be considerably affected by the melanocyte-controlled degree of pigmentation. The mechanism relies on the acidification of the epidermis through secreted melanosomes, which can influence the enzymatic activities of several pH-dependent proteins in the stratum corneum. The degree of skin pigmentation is correlated with the size of melanocytes; in dark skin, the cells are significantly enlarged and transfer more melanosomes to the epidermis due to higher tyrosinase activity and larger and more acidic dendrites compared to light skin.35,36 Increased activity of melanocytes, in proximity to the damaged basement membrane, could be also a contributing factor to the formation of hypertrophic and keloid scars through sustained interactions with the dermal fibroblasts and activation of the inflammatory signaling pathways such as transforming growth factor β (TGF-β).37
Dermal-Epidermal Junctions (DEJ)
Dermal-epidermal junctions (DEJ) are crucial for the maintenance of skin homeostasis. DEJ supports physical interactions and molecular signaling between the keratinocytes and fibroblasts in the superficial (papillary) dermis; the secretory activity of fibroblasts is moreover thought to affect the physiology and morphogenesis of the epidermis.38,39 Darker skin is characterized by thicker dermis with more abundant macrophages and fibroblasts. Compared to light skin types, the papillary fibroblasts from darkly pigmented skin have also an increased secretory activity, producing higher amounts of signaling molecules such as monocyte chemotactic peptide-1 (MCP-1), keratinocyte growth factor (KGF), matrix metalloproteinase 1 (MMP1) and tissue inhibitor metalloproteinase protein 1 (TIMP-1).31
Differences in the cellular interactions between the dermis and the epidermis in light and dark skin are also indicated by a detailed analysis of the molecular organization of DEJ. Studies based on skin biopsies and reconstructed 3D skin models demonstrated that the DEJ compartment in African skin was significantly longer and more convoluted compared to European skin. However, DEJ from African skin biopsies contained lower levels of basement membrane markers, collagen IV (COL4), collagen VII (COL7), laminin 5 (LAMA5), and nidogen (NID1) glycoprotein compared to European skin.31,40 It could suggest likely differences in the organization, mechanical strength, and the activity of DEJ in lightly- and darkly pigmented skin.
Altered cellular and molecular characteristics of DEJ could have also a direct effect on paracrine interactions evident in excessive scarring, which can be more severe in darkly pigmented skin. For example, keloid keratinocytes stimulate the expression of growth factors and pro-fibrotic phenotypes in dermal fibroblasts.41,42 Keloid fibroblasts are characterized by the secretion of inflammatory mediators including TGF-β1, TGF-β2, IL-6 and IL-8.43–46 Enhanced inflammation also promotes the accumulation of activated immune cells, mainly macrophages, T-lymphocytes and mast cells in the skin.33,47,48
Hyperpigmentation and Inflammation: Link to Skin Aging
PIH is caused by the presence of excess melanin, which occurs primarily as the response of skin cells to injury or irritation, sometimes also triggered by specific cosmetic treatments such as chemical peels, laser therapy and dermabrasion. Based on the patterns and age distribution among the population, PIH can affect all age groups and it is very common amongst younger age groups, for example as a result of acne.49 PIH also represents the hyperpigmentation problems that fall into a broader category of abnormal melanogenesis and loss of even skin tone. This includes melasma and solar lentigos (age spots) that are considered to occur in all skin types with aging.50 All disorders are commonly characterized by the presence of inflammation, particularly the up-regulated expression and activity of cytokines secreted by keratinocytes and fibroblasts and the increased accumulation of inflammatory cells in skin lesions.51,52
Among the proinflammatory cytokines, both promoting abnormal melanogenesis in PIH and consistently associated with darker skin tones as a circulating biomarker is IL-6. It is suggested that the levels of IL-6 are influenced not only by ethnicity but also by age.20 Chronic low-grade inflammation and an increase in the circulating pro-inflammatory markers, particularly IL-6 have been reported by several large population studies to frequently occur in older adults.53,54 Upregulated levels of IL-6 are also considered to be a risk factor for age-related problems linked to inflammation, chronic stress, and metabolism.55–57
Pro-inflammatory cytokines constitute a part of the larger group of molecules, also comprised of chemokines, growth factors and matrix-remodeling proteins, which are secreted by senescent cells and thought to affect multiple tissues in a paracrine manner in vivo as part of the senescence-associated secretory phenotype (SASP). The physiological activity of SASP biomarkers is linked to the cellular responses to stress, such as oxidative stress and DNA damage caused by exposure to ultraviolet radiation (UVR).58 Senescent cells are also present in aging human skin; with SASP genes activated in fibroblasts, keratinocytes and melanocytes. The most abundant cytokine of the SASP and DNA damage-induced senescence is IL-6.59,60
Hyperpigmentation disorders, including PIH and melasma, are photosensitive skin conditions aggravated by exposure to UVR. The likely mechanism involves inflammatory responses mediated through ROS affecting melanocytes in the epidermis. The protective effect can be achieved with broad-spectrum filters against UVB, UVA and visible light, alternatively with additive anti-inflammatory and antioxidant ingredients.61,62 UVR exposure is also a major extrinsic factor responsible for premature aging of the skin. Both UVB and UVA can cause DNA damage and inflammation mediated by oxidative stress. Accumulation of senescent fibroblasts in the dermis is accelerated particularly by UVA (315–400 nm), which has longer wavelengths than UVB (280–315 nm) and can penetrate deeper layers of the skin. Chronic inflammation and photoaging are thought to be linked to SASP, which involves a broad group of growth factors, proteolytic enzymes and cytokines, with interleukins IL-1, IL-6, and IL-8 found to be secreted by both fibroblasts and keratinocytes.63–65
The senescent fibroblasts could also play an important role in abnormal pigmentation. A recent report demonstrated that the accumulation of senescent fibroblasts in senile lentigo (age spots) has a significant impact on the stromal-epithelial interactions in the pigmentary unit, which could ultimately drive pigmentation through melanocyte differentiation. Such a mechanism could be responsible for an increase in hyperpigmentation as part of the extrinsic aging process.66
Current Treatments for Skin Hyperpigmentation: Unique Requirements for Darker Skin Tones
Current popular skin care products on the market to treat hyperpigmentation include Perfectionist Pro Rapid Renewal Retinol Treatment, Rodial Super Acids Daily Serum, The Ordinary Azelaic Acid Suspension 10%, GiGi Bioplasma Azelaic Peel, ProActiv Complexion Perfecting Hydrator, Pureauty Naturals Skin Lightening Serum with Kojic Acid, Paula’s Choice Resist 10% Niacinamide Booster, Eva Naturals Vitamin B3 5% Niacinamide Serum, The Ordinary Niacinamide 10%, Differin Gel, Perfect Image Salicylic Acid 20% Gel Peel, Exuviance Performance Peel AP25, Juice Beauty Green Apple Peel Sensitive. Several molecular ingredients in cosmetic formulations are available for the treatment and prevention of hyperpigmentation, including PIH. These include photoprotection with broad-spectrum sunscreen with an SPF of 30, chemical peels containing small molecules such as alpha-hydroxy acid (AHA), glycolic acid (GA), salicylic acid (SA), trichloroacetic acid (TCA), kojic acid (KA) and pyruvic acid (PYR) as the active component of chemical peels used as a non-surgical procedure to exfoliate and resurface the upper layers of the skin.1 In addition to laser therapies with both shorter wavelengths for the surface layer that target the intracellular melanosomes and longer wavelengths for deep penetration of the skin, successful treatments have been also achieved with blue light photodynamic therapy.1 However, skin treatments such as chemical peels and laser therapy can often trigger wound healing responses, irritations, and scarring. The complications, which aggravate the uneven pigmentation further, are also more frequent in darker skin types.67
Another approach to hyperpigmentation involves the application of topical agents and natural ingredients that reduce melanogenesis and induce depigmentation through the inhibition of several factors involved in melanogenic pathways. Some of these factors include hydroquinone, thiamidol, mequinol, azelaic acid, kojic acid, arbutin, niacinamide, ellagic acid, luteolin, N-acetyl glucosamine, hexyl decanol, phytosterols, calycosin, aloesin, arginine, resorcinol and retinoids.1,50,68–70 Importantly, many of these ingredients have also a significant capacity to reduce inflammation, therefore can improve several aspects associated with PIH, particularly changes in the pigmentary unit linked to the abnormal stimulation of melanocytes in the epidermal environment. For example, azelaic acid can suppress UVB-induced expression and secretion of IL-1β, IL-6 and TNF-α and kojic acid has the potential to inhibit nuclear factor kappa B (NF-κB) activity in the keratinocytes.71,72 The expression of IL-6 and TNF-α in the keratinocytes is also inhibited by ellagic acid. The compound can moreover modulate the mitogen-activated protein kinase/extracellular signal-regulated protein kinase (MEK1/2-ERK) and the Janus kinase signal transducer/activator of transcription (JAK/STAT) pathways in response to the treatment of the cells with pro-inflammatory factors TNF-α and interferon γ (IFN-γ).73 Cellular targets of luteolin involve the major pathways regulating inflammation - Nf-κB, activator protein 1 (AP-1) and signal transducer and activator of transcription (STAT-3).74 N-acetyl glucosamine (NAG) normalizes the stratum corneum by up-regulation of the differentiation markers keratin 10 and involucrin. The compound also suppresses the expression of cyclooxygenase 2 (COX-2) and IL-6 as the main targets of inflammation.75,76 Calycosin has the potential to alleviate inflammation by inhibiting the PI3K/AKT and NFf-κB pathways.77 Aloesin has been shown to affect the levels of plasma leukotriene B(4) (LTB(4)) and the cellular levels of TNF-α and IL-1β.78 L-arginine can directly target the expression levels of IL-6, IL-8 and TNF-α.79 The anti-inflammatory effects of resorcinol are executed through the inhibition of COX-2 activity.80 The risk of PIH, particularly occurring after the applications of laser therapy, has been also shown to be minimized by topical applications of corticosteroids.81 These data point to the likely importance of the anti-inflammatory capacities of the ingredients used in the prevention and treatment of PIH. Despite their effectiveness and established mechanisms of action, the treatments for hyperpigmentation, particularly PIH in darkly pigmented skin, are expected to witness further rapid growth based on the availability of increasingly advanced products.
Discussion
Post-inflammatory hyperpigmentation (PIH) is characterized by an uneven distribution of melanin and dark spots, which can range in color depending on the severity of the damage and skin tone. Acne and atopic dermatitis, allergies, traumas, and cosmetic operations can all cause PIH triggered by the synthesis and release of extra melanin by melanocytes in the epidermis. Two major factors have been widely associated with the pathophysiology of PIH. Firstly, the localized inflammation caused by an accumulation of pro-inflammatory growth factors has a stimulatory effect on melanocytes and the process of melanogenesis. Secondly, abnormal and excessive pigment deposition is frequently linked to damage to the upper layers of the skin, specifically within the basement membrane and basal keratinocytes. Such damage most likely results in local changes to skin structure and topology, which could have a direct effect on the density of melanocytes in the epidermal melanin unit. Long-lasting hyperpigmentation in the dermis can be also caused by damage to the basement membrane and basal keratinocytes, which release melanin in reaction to ongoing inflammation and infiltration of immune cells.
PIH can occur on all skin types; however, it is more common and severe in darkly pigmented skin. Skin types on Fitzpatrick scale IV, V and VI are also more prone to experience long-lasting damage and complications in response to some chemical peelings or laser therapies, including erythema, hypertrophic scars and keloids.1
This rises the important question regarding the specific factors that could be responsible for unique molecular and cellular signatures contributing to the increased prevalence of PIH and susceptibility to more permanent damage such as scars after the mechanical intervention. Individuals with darker skin pigmentation might experience a reduced cutaneous microvascular function, together with low-grade chronic production of pro-inflammatory cytokines and susceptibility to inflammation and oxidative stress at a systemic level. Changes in the inflammatory profiles, likely enhanced by additional extrinsic factors, could be coupled with local alterations in the epidermal homeostasis and renewal accompanying atopic dermatitis leading to hyperpigmentation in dark skin. Interestingly, the skin is considered to be an immune organ, with inflammatory conditions closely associated with the disruption of the physical barrier.82 Upper layers of human skin also contain significant numbers of immune cells such as macrophages, natural killer (NK) and CD8+ T cells.83 It is likely that the subtle differences in the immune cell numbers and activity still exist between darkly and lightly pigmented skin. It would be of interest to uncover further the links between systemic and local inflammation with susceptibility to PIH. Increased paracrine signaling and secretion of inflammatory factors are one of the major events observed in excessive scarring, which are common complications of PIH.
It is well recognized that the proliferation and differentiation patterns of skin cells are also strongly affected by inflammation. Several studies described the cellular and molecular organization of darkly pigmented skin, which could provide additional insight into the mechanisms of PIH. Based on the analysis of skin biopsies and 3D skin models, there are considerable differences between light and dark skin, especially in the morphology of the dermal-epidermal junctions (DEJ) and expression of the biomarkers involved in the control of skin morphogenesis and metabolism. The most pronounced difference could be linked to the processes of terminal differentiation and organization of stratum corneum as indicated by decreased expression or activity of the biomarkers involved in these processes in dark skin. Different rates of maturation in the upper layers of the epidermis could be a consequence of the higher activity of melanocytes and changes in the enzymatic activities in the stratum corneum. Decreased desquamation is also linked to irregular pigmentation and acne, which can be presently addressed by applications of chemical peeling.
Both melanocytes and keratinocytes rely on the mechanical support of the basement membrane located and dermal-epidermal junctions (DEJ). Altered properties in the basement membrane are likely to affect the distribution, migration and renewal of the epidermal cells, damage in this compartment is frequently observed in PIH. Reduced mechanical strength of DEJ in darkly pigmented skin is indeed indicated by decreased levels of expression of basement membrane markers in light skin. The susceptibility of the basement membrane to damage can be also suggested by the enhanced secretory activity of fibroblasts in the superficial dermis, particularly matrix metalloproteinases and their inhibitors responsible for remodeling the extracellular matrix involved in structural support.
Hyperpigmentation diseases, such as PIH and melasma, are photosensitive skin abnormalities that are exacerbated by UVR exposure, which is also a major extrinsic skin aging factor linked to DNA damage, oxidative stress and inflammation. Photoaging, classified as an extrinsic aging process, has been extensively studied and characterized, pointing to the accumulation of senescent fibroblasts in the skin dermis. Such cells, also postulated to be present in chronologically aged skin and frequently bearing the DNA damage response (DDR) markers, are the source of pro-inflammatory cytokines that could stimulate abnormal pigmentation. Inflammatory responses mediated by ROS impacting melanocytes in the pigmentary units, together with the accumulation of senescent fibroblasts in the dermis that is accelerated by UVR, could be one of the mechanisms driving PIH.
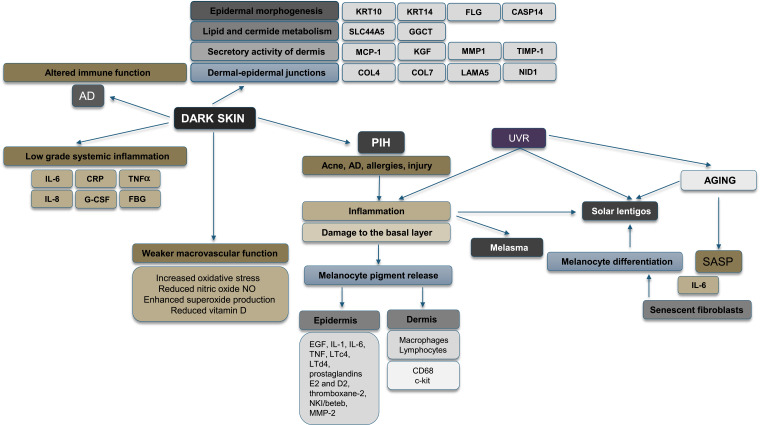
The proposed systemic mechanisms of hyperpigmentation in dark skin are outlined in Figure 1. The model predicts that the susceptibility to low-grade chronic inflammation combined with the structural organization and increased secretory activity of upper skin layers would constitute a partial mechanism driving the hyperpigmentation in darkly pigmented skin. Abnormal melanogenesis is furthermore exasperated by UVR; pointing to the hyperpigmentation as localized premature aging events driven by both inflammation and cell senescence.
Figure 1.
The proposed systemic mechanisms of hyperpigmentation in dark skin. Dark skin demonstrates unique characteristics regarding epidermal morphogenesis, secretory activity in the dermis and the architecture of dermal-epidermal junctions that are distinctive from light skin. Dark skin is prone to the development of PIH, AD and melasma, which are all linked to inflammation. A predisposition to low-grade chronic inflammation and weaker macrovascular function has been also detected in dark-skinned individuals. Abnormal melanogenesis is furthermore exasperated by UVR; both the UVR-induced inflammation and cell senescence have been demonstrated to drive age-related hyperpigmentation.
Prevention and treatment of PIH can be achieved with photoprotection using broad-spectrum sunscreens as well as natural ingredients inhibiting the melanogenic pathways and causing depigmentation whilst reducing inflammation. Current trends support the discovery of novel formulations to address both cosmetic and biomedical aspects of PIH. Such a goal can be achieved, for example, by screening and verification of existing libraries of the compounds and their synergies. Additional demand would rely on more insight into the molecular mechanisms of PIH, this could be initiated by the genetic screening and identification of the biomarkers in PIH skin lesions of darkly pigmented skin.
Conclusion
Post-inflammatory hyperpigmentation is a serious condition that requires an individualized approach and the right choice of treatment. In the past several years, a number of effective treatments based on several active ingredients have been implemented. One of the major factors associated with the increased occurrence and challenging prevention of PIH is dark pigmentation of the skin. Such outcome could be related to the unique characteristics of dark skin, associated with increased size and activity of melanocytes, expression levels of DEJ markers, epidermal stratification and paracrine signaling of fibroblasts combined with potential low-grade chronic inflammation at a systemic level. Despite the efficient protection against photodamage brought about by high melanin content in dark skin, PIH can be aggravated by excess exposure to UVR which is also recognized for stimulating further the inflammatory responses in the skin. Current and future prevention and treatment of PIH in dark skin could be based on formulations that combine the active ingredients with synergistic inhibitory effects on melanogenesis, anti-inflammatory activities and broad-spectrum UVR filters.
Disclosure
The authors report no conflicts of interest in relation to this work.
References
- 1.Davis EC, Callender VD. Postinflammatory hyperpigmentation: a review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol. 2010;3:20–31. [PMC free article] [PubMed] [Google Scholar]
- 2.Ruiz-Maldonado R, Orozco-Covarrubias ML. Postinflammatory hypopigmentation and hyperpigmentation. Semin Cutan Med Surg. 1997;16:36–43. doi: 10.1016/s1085-5629(97)80034-x [DOI] [PubMed] [Google Scholar]
- 3.Kaufman BP, Aman T, Alexis AF. Postinflammatory hyperpigmentation: epidemiology, clinical presentation, pathogenesis and treatment. Am J Clin Dermatol. 2018;19:489–503. doi: 10.1007/s40257-017-0333-6 [DOI] [PubMed] [Google Scholar]
- 4.Elbuluk N, Grimes P, Chien A, et al. The pathogenesis and management of acne-induced post-inflammatory hyperpigmentation. Am J Clin Dermatol. 2021;22:829–836. doi: 10.1007/s40257-021-00633-4 [DOI] [PubMed] [Google Scholar]
- 5.Silpa-Archa N, Kohli I, Chaowattanapanit S, et al. Postinflammatory hyperpigmentation: a comprehensive overview: epidemiology, pathogenesis, clinical presentation, and noninvasive assessment technique. J Am Acad Dermatol. 2017;77:591–605. doi: 10.1016/j.jaad.2017.01.035 [DOI] [PubMed] [Google Scholar]
- 6.Shenoy A, Madan R. Post-inflammatory hyperpigmentation: a review of treatment strategies. J Drugs Dermatol. 2020;19:763–768. doi: 10.36849/JDD.2020.4887 [DOI] [PubMed] [Google Scholar]
- 7.Grimes PE. Management of hyperpigmentation in darker racial ethnic groups. Semin Cutan Med Surg. 2009;28:77–85. doi: 10.1016/j.sder.2009.04.001 [DOI] [PubMed] [Google Scholar]
- 8.Tomita Y, Maeda K, Tagami H. Melanocyte-stimulating properties of arachidonic acid metabolites: possible role in postinflammatory pigmentation. Pigment Cell Res. 1992;5:357–361. doi: 10.1111/j.1600-0749.1992.tb00562.x [DOI] [PubMed] [Google Scholar]
- 9.Taylor SC, Grimes PE, Lim J, et al. Postinflammatory hyperpigmentation. J Cutan Med Surg. 2009;13:183–191. doi: 10.2310/7750.2009.08077 [DOI] [PubMed] [Google Scholar]
- 10.Park JY, Park JH, Kim SJ, et al. Two histopathological patterns of postinflammatory hyperpigmentation: epidermal and dermal. J Cutan Pathol. 2017;44:118–124. doi: 10.1111/cup.12849 [DOI] [PubMed] [Google Scholar]
- 11.Lacz NL, Vafaie J, Kihiczac NI, et al. Postinflammatory hyperpigmentation: a common but troubling condition. Int J Dermatol. 2004;4:362–365. doi: 10.1111/j.1365-4632.2004.02267.x [DOI] [PubMed] [Google Scholar]
- 12.Alexis AF, Sergay AB, Taylor SC. Common dermatologic disorders in skin of color: a comparative practice survey. Cutis. 2007;80:387–394. [PubMed] [Google Scholar]
- 13.Taylor SC, Cook-Bolden F, Rahman Z, et al. Acne vulgaris in skin of color. J Am Acad Dermatol. 2002;46(2 Suppl):S98–S106. doi: 10.1067/mjd.2002.120791 [DOI] [PubMed] [Google Scholar]
- 14.Dunwell P, Rose A. Study of the skin disease spectrum occurring in an Afro-Caribbean population. Int J Dermatol. 2003;42:287–289. doi: 10.1046/j.1365-4362.2003.01358.x [DOI] [PubMed] [Google Scholar]
- 15.Chua-Ty G, Goh CL, Koh SL. Pattern of skin diseases at the national skin centre (Singapore) from 1989–1990. Int J Dermatol. 1992;31:555–559. doi: 10.1111/j.1365-4362.1992.tb02717.x [DOI] [PubMed] [Google Scholar]
- 16.Klopot A, Baida G, Kel A, et al. Transcriptome analysis reveals intrinsic proinflammatory signaling in healthy African American skin. J Invest Dermatol. 2022;142:1360–1371. doi: 10.1016/j.jid.2021.09.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wolf ST, Jablonski NG, Ferguson SB, et al. Four weeks of vitamin D supplementation improves nitric oxide-mediated microvascular function in college-aged African Americans. Am J Physiol Heart Circ Physiol. 2020;319:H906–H914. doi: 10.1152/ajpheart.00631.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hurr C, Patik JC, Kim K, et al. Tempol augments the blunted cutaneous microvascular thermal reactivity in healthy young African Americans. Exp Physiol. 2018;103:343–349. doi: 10.1113/EP086776 [DOI] [PubMed] [Google Scholar]
- 19.Kim K, Hurr C, Patik JC, Matthew Brothers R. Attenuated cutaneous microvascular function in healthy young African Americans: role of intradermal L-arginine supplementation. Microvasc Res. 2018;118:1–6. doi: 10.1016/j.mvr.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 20.Stowe RP, Peek MK, Cutchin MP, Goodwin JS. Plasma cytokine levels in a population-based study: relation to age and ethnicity. J Gerontol a Biol Sci Med Sci. 2010;65A:429–433. doi: 10.1093/gerona/glp198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ho RC, Davy KP, Hickey MS, Melby C. Circulating tumor necrosis factor alpha is higher in non-obese, non-diabetic Mexican Americans compared to non-Hispanic white adults. Cytokine. 2005;30:14–21. doi: 10.1016/j.cyto.2004.10.015 [DOI] [PubMed] [Google Scholar]
- 22.Mayr FB, Spiel AO, Leitner JM, et al. Ethnic differences in plasma levels of interleukin-8 (Il-8) and granulocyte colony stimulating factor (G-CSF). Transl Res. 2007;149:10–14. doi: 10.1016/j.trsl.2006.06.003 [DOI] [PubMed] [Google Scholar]
- 23.Coe CL, Love GD, Karasawa M, et al. Population differences in proinflammatory biology: Japanese have healthier profiles than Americans. Brain Behav Immun. 2001;25(3):494–502. doi: 10.1016/j.bbi.2010.11.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Xu H, Barnes GT, Yang Q, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamashita A, Soga Y, Iwamoto Y, et al. Macrophage-adipocyte interaction: marked interleukin-6 production by lipopolysaccharide. Obesity. 2007;15:2549–2552. doi: 10.1038/oby.2007.305 [DOI] [PubMed] [Google Scholar]
- 26.Czarnowicki T, He H, Krueger JG, Guttman-Yassky E. Atopic dermatitis endotypes and implications for targeted therapeutics. J Allergy Clin Immunol. 2019;143:1–11. doi: 10.1016/j.jaci.2018.10.032 [DOI] [PubMed] [Google Scholar]
- 27.Wongvibulsin S, Sutaria N, Kannan S, et al. Transcriptomic analysis of atopic dermatitis in African Americans is characterized by Th2/Th17‑centered cutaneous immune activation. Sci Rep. 2021;11:11175. doi: 10.1038/s41598-021-90105-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Park HR, Min SK. Expression of S100A2 and S100B proteins in epithelial tumors of the skin. J Cutan Pathol. 2003;30:373–378. doi: 10.1034/j.1600-0560.2003.00081.x [DOI] [PubMed] [Google Scholar]
- 29.Grayson C, Heath CR. Dupilumab improves atopic dermatitis and post-inflammatory hyperpigmentation in patient with skin of color. J Drugs Dermatol. 2020;19:776–778. doi: 10.36849/JDD.2020.4937 [DOI] [PubMed] [Google Scholar]
- 30.Callender VD. Considerations for treating acne in ethnic skin. Cutis. 2005;76(2 Suppl):19–23. [PubMed] [Google Scholar]
- 31.Girardeau S, Mine S, Pageon H, Asselineau D. The Caucasian and African skin types differ morphologically and functionally in their dermal component. Exp Dermatol. 2009;18:704–711. doi: 10.1111/j.1600-0625.2009.00843.x [DOI] [PubMed] [Google Scholar]
- 32.Girardeau-Hubert S, Deneuville C, Pageon H, et al. Reconstructed skin models revealed unexpected differences in epidermal African and Caucasian skin. Sci Rep. 2019;9:7456. doi: 10.1038/s41598-019-43128-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Limandjaja GC, Niessen FB, Scheper RJ, Gibbs S. The keloid disorder: heterogeneity, histopathology, mechanisms and models. Front Cell Dev Biol. 2020;8:360. doi: 10.3389/fcell.2020.00360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wolfram D, Tzankov A, Pülzl P, Piza-Katzer H. Hypertrophic scars and keloids – a review of their pathophysiology, risk factors, and therapeutic management. Dermatologic Surg. 2009;35:171–181. doi: 10.1111/j.1524-4725.2008.34406.x [DOI] [PubMed] [Google Scholar]
- 35.Gunathilake R, Schurer NY, Shoo BA, et al. pH-regulated mechanisms account for pigment-type differences in epidermal barrier function. J Invest Dermatol. 2009;129:1719–1729. doi: 10.1038/jid.2008.442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alaluf S, Atkins D, Barrett K, et al. Ethnic variation in melanin content and composition in photoexposed and photoprotected human skin. Pigment Cell Res. 2002;15:112–118. doi: 10.1034/j.1600-0749.2002.1o071.x [DOI] [PubMed] [Google Scholar]
- 37.Gao FL, Jin R, Zhang L, Zhang YG. The contribution of melanocytes to pathological scar formation during wound healing. Int J Clin Exp Med. 2013;6:609–613. [PMC free article] [PubMed] [Google Scholar]
- 38.Langton AK, Sherratt MJ, Sellers WI, et al. Geographical ancestry is a key determinant of epidermal morphology and dermal composition. Br J Dermatol. 2014;171:274–282. doi: 10.1111/bjd.12860 [DOI] [PubMed] [Google Scholar]
- 39.Woodley DT, Chen M. The basement membrane zone. In: Freinkel RK, Woodley DT, editors. The Biology of the Skin. Parthenon publishing; 2001:133–152. [Google Scholar]
- 40.Girardeau-Hubert S, Pageon H, Asselineau D. In vivo and in vitro approaches in understanding the differences between Caucasian and African skin types: specific involvement of the papillary dermis. Int J Dermatol. 2012;51:1–4. doi: 10.1111/j.1365-4632.2012.05553.x [DOI] [PubMed] [Google Scholar]
- 41.Lim IJ, Phan TT, Bay BH, et al. Fibroblasts cocultured with keloid keratinocytes: normal fibroblasts secrete collagen in a keloid-like manner. Am J Physiol Cell Physiol. 2002;283:C212–C222. doi: 10.1152/ajpcell.00555.2001 [DOI] [PubMed] [Google Scholar]
- 42.Phan TT, Lim IJ, Bay BH, et al. Role of IGF system of mitogens in the induction of fibroblast proliferation by keloid-derived keratinocytes in vitro. Am J Physiol Cell Physiol. 2003;284:C860–C869. doi: 10.1152/ajpcell.00350.2002 [DOI] [PubMed] [Google Scholar]
- 43.Mikulec AA, Hanasono MM, Lum J, et al. Effect of tamoxifen on transforming growth factor β 1 production by keloid and fetal fibroblasts. Arch Facial Plast Surg. 2001;3:111–114. doi: 10.1001/archfaci.3.2.111 [DOI] [PubMed] [Google Scholar]
- 44.Xia W, Longaker MT, Yang GP. P38 MAP kinase mediates transforming growth factor-β2 transcription in human keloid fibroblasts. Am J Physiol Regul Integr Comp Physiol. 2005;290:R501–R508. doi: 10.1152/ajpregu.00472.2005 [DOI] [PubMed] [Google Scholar]
- 45.Ghazizadeh M, Tosa M, Shimizu H, et al. Functional implications of the IL-6 signaling pathway in keloid pathogenesis. J Invest Dermatol. 2007;127:98–105. doi: 10.1038/sj.jid.5700564 [DOI] [PubMed] [Google Scholar]
- 46.Do DV, Ong CT, Khoo YT, et al. Interleukin-18 system plays an important role in keloid pathogenesis via epithelial-mesenchymal interactions. Br J Dermatol. 2012;166:1275–1288. doi: 10.1111/j.1365-2133.2011.10721.x [DOI] [PubMed] [Google Scholar]
- 47.Boyce DE, Ciampolini J, Ruge F, et al. Inflammatory cell subpopulations in keloid scars. Br J Plast Surg. 2001;54:511–516. doi: 10.1054/bjps.2001.3638 [DOI] [PubMed] [Google Scholar]
- 48.Ammendola M, Zuccalà V, Patruno R, et al. Tryptase-positive mast cells and angiogenesis in keloids: a new possible post-surgical target for prevention. Updates Surg. 2013;65:53–57. doi: 10.1007/s13304-012-0183-y [DOI] [PubMed] [Google Scholar]
- 49.Zawar VP, Agarwal M, Vasudevan B. Treatment of postinflammatory pigmentation due to acne with Q-switched neodymium-doped yttrium aluminum garnet in 78 Indian cases. J Cutan Aesthet Surg. 2015;8:222–226. doi: 10.4103/0974-2077.172196 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hakozaki T, Swanson CL, Bissett DL. Hyperpigmentation in aging skin. In: Farage M, Miller K, Maibach H, editors. Textbook of Aging Skin. Berlin, Heidelberg: Springer; 2017. doi: 10.1007/978-3-662-47398-6_51 [DOI] [Google Scholar]
- 51.Noh TK, Choi SJ, Chung BY, et al. Inflammatory features of melasma lesions in Asian skin. J Dermatol. 2014;41:788–794. doi: 10.1111/1346-8138.12573 [DOI] [PubMed] [Google Scholar]
- 52.Iriyama S, Ono T, Aoki H, Amano S. Hyperpigmentation in human solar lentigo is promoted by heparanase-induced loss of heparan sulfate chains at the dermal-epidermal junction. J Dermatol Sci. 2011;64:223–228. doi: 10.1016/j.jdermsci.2011.09.007 [DOI] [PubMed] [Google Scholar]
- 53.Hager K, Machein U, Krieger S, et al. Interleukin-6 and selected plasma proteins in healthy persons of different ages. Neurobiol Aging. 1994;15:771–772. doi: 10.1016/0197-4580(94)90066-3 [DOI] [PubMed] [Google Scholar]
- 54.Ballou SP, Lozanski FB, Hodder S, et al. Quantitative and qualitative alterations of acute-phase proteins in healthy elderly persons. Age Ageing. 1996;25:224–230. doi: 10.1093/ageing/25.3.224 [DOI] [PubMed] [Google Scholar]
- 55.Ershler WB, Sun WH, Binkley N, et al. Interleukin-6 and aging: blood levels and mononuclear cell production increase with advancing age and in vitro production is modifiable by dietary restriction. Lymphokine Cytokine Res. 1993;12:225–230. [PubMed] [Google Scholar]
- 56.Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, et al. Chronic stress and age-related increases in the proinflammatory cytokine Il-6. Proc Natl Acad Sci U S A. 2003;100:9090–9095. doi: 10.1073/pnas.1531903100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Maggio M, Guralnik JM, Longo DL, Ferrucci L. Interleukin-6 in aging and chronic disease: a magnificent pathway. J Gerontol a Biol Sci Med Sci. 2006;61:575–584. doi: 10.1093/gerona/61.6.575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ohtani N. The roles and mechanisms of senescence-associated secretory phenotype (SASP): can it be controlled by senolysis? Inflamm Regener. 2022;42:11. doi: 10.1186/s41232-022-00197-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Ho CY, Dreesen O. Faces of cellular senescence in skin aging. Mech Ageing Dev. 2021;198:111525. doi: 10.1016/j.mad.2021.111525 [DOI] [PubMed] [Google Scholar]
- 60.Coppé JP, Desprez PY, Krtolica A, Campisi J. The senescence-associated secretory phenotype: the dark side of tumor suppression Annu Rev Pathol. 2010;5:99–118. doi: 10.1146/annurev-pathol-121808-102144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Fatima S, Braunberger T, Mohammad TF, et al. The role of sunscreen in melasma and postinflammatory hyperpigmentation. Indian J Dermatol. 2020;65:5–10. doi: 10.4103/ijd.ijd_295_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Puaratanaarunkon T, Asawanonda P. A randomized, double blinded, split-face study of the efficacy of using a broad spectrum sunscreen with anti-inflammatory agent to reduce post inflammatory hyperpigmentation after picosecond laser. Clin Cosmet Investig Dermatol. 2022;15:331–337. doi: 10.2147/CCID.S355329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ansary TM, Hossain MR, Kamiya K, et al. inflammatory molecules associated with ultraviolet radiation-mediated skin aging. Int J Mol Sci. 2021;22:3974. doi: 10.3390/ijms22083974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wlaschek M, Maity P, Makrantonaki E, Scharffetter-Kochanek K. Connective tissue and fibroblast senescence in skin aging. J Investig Dermatol. 2021;141:985–992. doi: 10.1016/j.jid.2020.11.010 [DOI] [PubMed] [Google Scholar]
- 65.Ansel J, Perry P, Brown J, et al. Cytokine modulation of keratinocyte cytokines. J Investig Dermatol. 1990;94:s101–s107. doi: 10.1111/1523-1747.ep12876053 [DOI] [PubMed] [Google Scholar]
- 66.Yoon JE, Kim Y, Kwon S, et al. Senescent fibroblasts drive ageing pigmentation: a potential therapeutic target for senile lentigo. Theranostics. 2018;8:4620–4632. doi: 10.7150/thno.26975 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nikalji N, Godse K, Sakhiya J, et al. Complications of medium depth and deep chemical peels. J Cutan Aesthet Surg. 2012;5:254–260. doi: 10.4103/0974-2077.104913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Searle T, Al-Niaimi F, Ali FR. The top 10 cosmeceuticals for facial hyperpigmentation. Dermatol Ther. 2020;33:e14095. doi: 10.1111/dth.14095 [DOI] [PubMed] [Google Scholar]
- 69.Tan MG, Kim WB, Jo CE, et al. Topical treatment for postinflammatory hyperpigmentation: a systematic review. J Dermatolog Treat. 2022;33:2518–2526. doi: 10.1080/09546634.2021.1981814 [DOI] [PubMed] [Google Scholar]
- 70.Callender VD, Baldwin H, Cook-Bolden FE, et al. Effects of topical retinoids on acne and post-inflammatory hyperpigmentation in patients with skin of color: a clinical review and implications for practice. Am J Clin Dermatol. 2022;23:69–81. doi: 10.1007/s40257-021-00643-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mastrofrancesco A, Ottaviani M, Aspite N, et al. Azelaic acid modulates the inflammatory response in normal human keratinocytes through PPARgamma activation. Exp Dermatol. 2010;19:813–820. doi: 10.1111/j.1600-0625.2010.01107.x [DOI] [PubMed] [Google Scholar]
- 72.Saeedi M, Eslamifar M, Khezri K. Kojic acid applications in cosmetic and pharmaceutical preparations. Biomed Pharmacother. 2019;110:582–593. doi: 10.1016/j.biopha.2018.12.006 [DOI] [PubMed] [Google Scholar]
- 73.Gil TY, Hong CH, An HJ. Anti-inflammatory effects of ellagic acid on keratinocytes via MAPK and STAT pathways. Int J Mol Sci. 2021;22:1277. doi: 10.3390/ijms22031277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Aziz N, Kim MY, Cho JY. Anti-inflammatory effects of luteolin: a review of in vitro, in vivo, and in silico studies. J Ethnopharmacol. 2018;225:342–358. doi: 10.1016/j.jep.2018.05.019 [DOI] [PubMed] [Google Scholar]
- 75.Mammone T, Gan D, Fthenakis C, Marenus K. The effect of N-acetyl-glucosamine on stratum corneum desquamation and water content in human skin. J Cosmet Sci. 2009;60:423–428. [PubMed] [Google Scholar]
- 76.Shikhman AR, Kuhn K, Alaaeddine N, Lotz M. N-acetylglucosamine prevents IL-1 beta-mediated activation of human chondrocytes. J Immunol. 2001;166:5155–5160. doi: 10.4049/jimmunol.166.8.5155 [DOI] [PubMed] [Google Scholar]
- 77.Shi X, Jie L, Wu P, et al. Calycosin mitigates chondrocyte inflammation and apoptosis by inhibiting the PI3K/AKT and NF-κB pathways. J Ethnopharmacol. 2022;297:115536. doi: 10.1016/j.jep.2022.115536 [DOI] [PubMed] [Google Scholar]
- 78.Park MY, Kwon HJ, Sung MK. Dietary aloin, aloesin, or aloe-gel exerts anti-inflammatory activity in a rat colitis model. Life Sci. 2011;88:486–492. doi: 10.1016/j.lfs.2011.01.010 [DOI] [PubMed] [Google Scholar]
- 79.Qiu Y, Yang X, Wang L, et al. L-arginine inhibited inflammatory response and oxidative stress induced by lipopolysaccharide via arginase-1 signaling in IPEC-J2 cells. Int J Mol Sci. 2019;20:1800. doi: 10.3390/ijms20071800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Shahinozzaman M, Ishii T, Halim MA, et al. Cytotoxic and anti-inflammatory resorcinol and alkylbenzoquinone derivatives from the leaves of Ardisia sieboldii. Z Naturforsch C J Biosci. 2019;74:303–311. doi: 10.1515/znc-2019-0114 [DOI] [PubMed] [Google Scholar]
- 81.Cheyasak N, Manuskiatti W, Maneeprasopchoke P, Wanitphakdeedecha R. Topical corticosteroids minimise the risk of postinflammatory hyper-pigmentation after ablative fractional CO2 laser resurfacing in Asians. Acta Derm Venereol. 2015;95:201–205. doi: 10.2340/00015555-1899 [DOI] [PubMed] [Google Scholar]
- 82.Nguyen AV, Soulika AM. The dynamics of the skin’s immune system. Int J Mol Sci. 2019;20:1811. doi: 10.3390/ijms20081811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Ho AW, Kupper TS. T cells and the skin: from protective immunity to inflammatory skin disorders. Nat Rev Immunol. 2019;19:490–502. doi: 10.1038/s41577-019-0162-3 [DOI] [PubMed] [Google Scholar]