Abstract
Background
Credible evidence has established a link between the level of patient safety culture in healthcare environments and patient outcomes. Patient safety culture in the operating room has received scant attention despite the burden of adverse events among surgical patients. We aimed to evaluate the safety culture in our operating rooms and compare with existing data from other operating room settings.
Methods
We investigated the patient safety culture in the operating rooms of our hospital as perceived by the surgeons, nurse anaesthetists and perioperative nurses using the Hospital Survey on Patient Safety Culture (HSOPSC) instrument. IBM Statistical Package for Social Science software, version 25, was used for data entry and analysis. Differences were considered significant when p < 0.05.
Results
Only 122 completed surveys were returned out of a survey population of 132 frontline staff, yielding a response rate of 92.4%. The overall average composite score was 47%. The average composite scores ranged from 17–79.6% across the 12 dimensions of the HSOPSC, with teamwork within units being the only dimension with demonstrable strength. Non-punitive response to error, communication openness, feedback and communication about error”, frequency of events reported”, handoffs and transition and staffing need improvement. The perceived safety culture varied according to work areas and professional roles with nurse anaesthetists having the highest perception and the surgeons the least.
Conclusion
Patient safety culture in our operating rooms is adjudged to be weak, with only one of the twelve dimensions of HSOPSC demonstrating strength. This is notwithstanding its comparative strengths relative to other operating room settings.
Keywords: Operating rooms, Organizational culture, Perception, Safety management, Surgery
Introduction
Two decades ago, while adopting the resolution on patient safety in healthcare at the 55th World Health Assembly the World Health Organization (WHO) recognized the need to promote patient safety as a fundamental principle of all health systems and urged support for member states to promote a culture of safety within health care organizations and encourage research into patient safety [1]. But unsafe care has remained a major source of morbidity and mortality [2], prompting the WHO to launch the first World Patient Safety Day on 17 September, 2019. Beyond the ethical issues of patients suffering personal harm while undergoing care, the burden on the health system encompasses additional treatment, prolonged hospital length of stay, disability and deaths. Very profound too, is the associated phenomena of ‘second’ ‘third’ and ‘fourth’ victims; representing further impact on the involved healthcare professionals, the hospital reputation, and patients who may be harmed subsequently, respectively [3]. Reports from the Irish National Adverse Events Study (INAES) indicate that about 7% of the healthcare adverse events contribute to death, while as much as 70% of these events were considered preventable [4]. Surgical procedures probably account for the majority of healthcare adverse events [5–7]. Recent global estimates suggest that over 7 million people suffer surgical complications annually, with over 1 million deaths [8].
Patient safety culture is a product of individual and group values, attitudes, perceptions and competencies that determine a pattern of behavior and commitment to the safety of patients. Despite the established link between the level of patient safety culture in healthcare environments and patient outcomes [9–11], safety culture in the operating room (OR) has not received significant attention. Unfortunately too, the few available studies suggest that poor safety culture in the OR is pervasive. In one multicentre study poor scores were reported in all the 10 dimensions (composites) of patient safety culture evaluated [12]. While not losing sight of the numerous studies on other work areas in the hospital, the variability of safety culture even across units within a hospital make extrapolations with these other settings untenable [13].
The increasing interest in patient safety over the past two decades has led to the development of several tools for assessing safety culture and climate in healthcare. Among these the Hospital Survey on Patient Safety Culture (HSOPSC) [14] and the Safety Attitudes Questionnaire (SAQ) [15] are the most utilized. A direct comparison of the SAQ and the HSOPSC by simultaneous administration of both tools on healthcare workers (HCWs) had concluded that the reliability of both instruments showed marked similarity [16]. However, based on the analysis conducted on several safety culture assessment tools, the HSOPSC was adjudged to be the most psychometrically sound, by Fin et al. [17].
Earlier large scale studies in healthcare organizations indicate that frontline personnel’s perceptions of better safety climate were superior to management’s perceptions in predicting the risk of adverse outcomes [18, 19]. The perception of frontline personnel regarding the safety culture in the OR could therefore present a reliable basis for evaluating and improving the safety of surgical patients.
Our objective was to assess the current state of patient safety culture in the OR of our hospital, identifying strengths and areas that require improvement. We also sought to compare our safety culture with OR settings elsewhere. This process is in tandem with the Council of Europe’s recommendation on management of patient safety, to the effect that defining the existing safety culture in the organization is the first stage in developing a safety culture [20].
Methods
This is a cross-sectional descriptive paper-based survey of a purposive sample of frontline operating room personnel in a regional trauma and burns centre.
Study setting
The 400-bed referral centre which was established in 1973 serves a population of about 80 million encompassing the Southeast where it is located, but also the South-south and North-central geopolitical zones of Nigeria. It is one of the three tertiary hospitals in the city, located within 10 min drive from the Akanu Ibiam international airport, Enugu. The hospital also provides care to a substantial number of secondary, and even primary care patients. There are six operating theatres on-site, at different locations. The surgical specialties include trauma, orthopaedics, spine, plastic and reconstructive surgery, and burns care. Our OR personnel typically consists of; the resident surgeons (with, or without the consultant surgeon), the nurse anaesthetist (with, or without the consultant anaesthetist), the perioperative/circulating nurse, the operating room attendant, and sometimes the radiographer. Anaesthesia service in the institution is essentially nurse-based, with one resident doctor and three consultant anaesthetists.
Survey Tool
The Hospital Survey on Patient Safety Culture (HSOPSC)/ SOPS® Hospital Survey [14].
The HSOPSC was designed by the United States Agency of Healthcare Research and Quality (AHRQ) in 2004, for the purpose of measuring patient safety culture in individual health institutions [14]. It is a self-reported tool designed specifically for HCWs, requesting for their opinions about the culture of patient safety at their hospitals. It proposes the assessment of 12 dimensions/composite measures pertaining to the climate of patient safety in hospital setting. The culture of safety is measured from the staff perspective.
The HSOPSC consists of 42 items distributed among the 12 dimensions namely; overall perception of patient safety, teamwork within units, teamwork across units, supervisor/manager expectations and actions promoting safety, organizational learning-continuous improvement, executive management support for patient safety, feedback and communication about error, communication openness, frequency of error reporting, staffing, handoffs and transitions between units and shifts and non-punitive response to error. The answers to the items are scaled 1 to 5; 1 and 2 were considered negative towards patient safety, 3 was considered neutral and answer 4 and 5 were considered positive towards patient safety. Out of the 42 items, 17 were negatively framed for psychometric balancing; with the answers reverse-scored prior to recoding into positive, neutral or negative. In effect whereas “agree” and “strongly agree” are ordinarily positive responses, in the negatively framed items “disagree” and “strongly disagree” represent the positive responses. In sum higher values always indicate better perceived safety culture. The composite scores were expressed as the mean percentage of positive answers in the items within each dimension/composite. The overall average composite score was determined as the average of the 12 composite scores. In addition to the 42 items there were also one item each on the respondent’s perception of safety quality in their respective work area and the number of adverse events they have reported in the past 12 months. Six other items sought information regarding the respondent’s service background.
The English version of the survey instrument; SOPS® Hospital Survey Version 1.0. [14] which was obtained online was used for the paper survey.
Modification of the instrument
A minor modification was deemed necessary in order to facilitate effective communication and comprehension of the item in our cultural background. This was effected in Section F, item 3: “Things fall between the cracks” when transferring patients from one unit to another was changed to… “things escape attention” when transferring patients from one unit to another’, as the former is an unfamiliar phrase in our environment. Such minor modification which will minimally impact on the psychometric properties of the instrument is in compliance with the instrument guideline [14].
Inclusion criteria
All operating room frontline personnel (attending surgeons, resident surgeons, nurse anaesthetists and perioperative nurses) who have been in active clinical service in the hospital for a period of not less than six months were eligible to participate in the study.
Exclusion criteria
Eligible but non-consenting OR personnel were excluded. New employees who had spent less than 6 months in the hospital employment were deemed ineligible and consequently excluded.
Sampling method and respondent selection
The questionnaires were distributed to the entire population of eligible OR frontline personnel who consented to participate in the survey. The sparse number of physician anaesthetists and radiographers precluded them from consideration in the survey in line with the instrument guideline [14]. This recommendation was in consideration of the need to protect the confidentiality of the respondents. On the other hand, the operating room attendants in our setting who are less well-educated had considerable difficulty comprehending the instrument items during pretesting of the instrument and were thus excluded.
Study procedure
The eligible respondents were invited to participate in the survey in the understanding that their participation is voluntary and that they are at liberty to withdraw their consent at any stage, if they so wish. The paper survey instrument was distributed in-person by the research assistant to all the consenting HCWs at their duty posts for self-administration. The questionnaires were anonymized by leaving no identification code and distributing them enclosed in brown envelopes. Each respondent was urged not to discuss their responses with other staff while further assuring them that their responses will be kept confidential. In order to enhance capture, the nominal role obtained for each of the relevant units was used to tick off the respective staff during distribution and collection of the questionnaires. The questionnaire administration lasted until all those who were absent during the initial phases of the distribution on account of shift duty, or short periods of leave, were captured. Due to the busy schedule of duty the questionnaires were left with the staff to fill in at their soonest convenient time, while the research assistant made repeat visits to further distribute and recover the filled questionnaires. Each of the three groups of HCWs was surveyed sequentially, and the returned surveys marked with a group identifier to ensure that no false claim of group identity occurs. This is then followed the by another group; in the sequence; nurse anaesthetists, perioperative nurses, and surgeons. The survey was conducted from February 7, 2022 to March 11, 2022.
Data management
This paper survey did not use individual identifiers. Instead, group identifiers were marked on the returned surveys of each of the three categories of HCWs. Later, all the completed paper surveys were marked with identification numbers to serve as respondent identifier but without any information linking the identifiers to individual worker. The respondent and group identifiers were reflected as such in the electronic data file entry. All data entry was accomplished using the IBM SPSS version 25 statistical package. The obtained data were illustrated using tables and bar charts. The percent positive scores for each item of safety culture, as well as the composite scores were computed from the scaled responses of the HCWs. For each item, or composite measure, percentages greater than 75% are considered as strengths and deemed to have positive perception of patient safety culture, while those ≤ 50% indicate weak perceptions of safety culture and require improvement [21].
Comparison of mean scores between the three study groups was done using One-way analysis of variance (ANOVA) test while inter group comparisons were done using Tukey HSD post hoc test. A difference was considered significant when p < 0.05.
Research Ethics
The study protocol for the survey was reviewed and approved by the Research Ethics Committee of National Orthopaedic Hospital, Enugu. (IRB Number S.313/IV/; Protocol Number 2022/1/103). Only consenting eligible HCWs were recruited, having duly signed to a written informed consent form.
Results
The derived overall average composite score of patient safety culture was 47%. Out of the 132 eligible and consenting personnel that were invited to the survey, 122 surveys were returned yielding a response rate of 92.4% (122/132). Only three eligible OR personnel were not invited; one on account of maternity leave while two others were on annual leave. None of the returned surveys was excluded in the analysis as they were duly completed and deemed eligible, save for the few items that some respondents did not oblige a response. Twenty six surveys (21%) did not have complete answers to all the items but were utilized in the analysis. The incomplete surveys mostly have only one missing answer, but one survey had as many as 28 missing answers. Where the respondents marked two answers for one item, such inappropriate response is treated as missing/no response. Complete responses were provided in 96 (79%) of the surveys.
One hundred and twenty two (122) HCWs; comprising consultant surgeons (11), resident surgeons (48), nurse anaesthetists (27) and perioperative nurses (36) participated in the study. Over 93% of the respondents have worked in the hospital for more than a year, while 78.7% have worked in their current unit for more than a year and 95.1% have worked in their current specialty for more than one year. About 11% of the respondents reported working for more than 100 h per week (Table 1).
Table 1.
Background information of the respondents
| Variable | Frequency (n = 122) |
Percent (%) |
|---|---|---|
| Hospital unit | ||
| Anesthesiology | 27 | 22.1 |
| Surgery | 59 | 48.4 |
| Peri-operative nursing | 36 | 29.5 |
| Duration of work in the hospital | ||
| < 1 year | 8 | 6.6 |
| 1–5 years | 44 | 36.1 |
| 6–10 years | 24 | 19.7 |
| 11–15 years | 28 | 23.0 |
| 16–20 years | 5 | 4.1 |
| ≥ 21 years | 13 | 10.7 |
| Duration of work in current hospital unit | ||
| < 1 year | 26 | 21.3 |
| 1–5 years | 42 | 34.4 |
| 6–10 years | 22 | 18.0 |
| 11–15 years | 22 | 18.0 |
| 16–20 years | 4 | 3.3 |
| ≥ 21 years | 6 | 4.9 |
| Number of hours per week you work in the hospital | ||
| 20–39 h | 13 | 10.7 |
| 40–59 h | 51 | 41.8 |
| 60–79 h | 29 | 23.8 |
| 80–99 h | 16 | 13.1 |
| ≥ 100 h | 13 | 10.7 |
| Staff position in hospital | ||
| Registered nurse | 63 | 51.6 |
| Resident surgeon | 48 | 39.3 |
| Consultant surgeon | 11 | 9.0 |
| Duration of work in current specialty | ||
| < 1 year | 6 | 4.9 |
| 1–5 years | 34 | 27.9 |
| 6–10 years | 26 | 21.3 |
| 11–15 years | 35 | 28.7 |
| 16–20 years | 14 | 11.5 |
| ≥ 21 years | 7 | 5.7 |
The item with the highest percentage positive response was “People support one another in this unit” (91.8%) while “Staff feel free to question the decisions or actions of those with some authority” received the lowest percentage positive response (10.2%); (Table 2). Only five (A1, A3, A4, A6, B4) out of the 42 items of the HSOPSC instrument were perceived as having ‘strength’ regarding safety culture by the OR personnel (Table 2).
Table 2.
The 42 items scores
| Variable | Negative (%) | Neutral (%) | Positive (%) | Remarks/Recommendation |
|---|---|---|---|---|
| A1 People support one another in this unit | 8 (6.6) | 2 (1.6) | 112 (91.8) | Strength |
| A2 We have enough staff to handle the workload | 103 (84.4) | 2 (1.6) | 17 (14.0) | Needs improvement |
| A3 When a lot of work needs to be done quickly, we work together as a team to get the work done | 12 (9.9) | 7 (5.7) | 103 (84.4) | Strength |
| A4 In this unit, we treat each other with respect | 12 (9.8) | 18 (14.8) | 92 (75.5) | Strength |
| A5 Staff in this unit work longer hours than is best for patient care | 93 (76.8) | 14 (11.6) | 14 (11.6) | Needs improvement |
| A6 We are actively doing things to improve patient safety | 8 (6.7) | 13 (10.7) | 100 (82.6) | Strength |
| A7 We use more temporary staff than is best for patient care | 16 (23.3) | 22 (18.2) | 83 (68.6) | |
| A8 Staff feel that their mistakes are held against them | 77 (63.7) | 22 (18.2) | 22 (18.2) | Needs improvement |
| A9 Mistakes have led to positive changes here | 30 (15.2) | 27 (22.7) | 62 (52.1) | |
| A10 It is just by chance that more serious mistakes don’t happen around here | 38 (31.6) | 15 (12.5) | 67 (55.8) | |
| A11 When one area in this unit gets easily busy, others help out | 26 (21.5) | 14 (11.6) | 81 (66.9) | |
| A12 When an event is reported, it feels like the person is being written up, not the problem | 75 (63.6) | 21 (17.8) | 22 (18.6) | Needs improvement |
| A13 After we made changes to improve patient safety, we evaluate their effectiveness | 21 (17.5) | 30 (25.0) | 69 (57.5) | |
| A14 We work in ‘crisis mode’ trying to do too much, too quickly | 71 (59.2) | 25 (20.8) | 24 (20.0) | Needs improvement |
| A15 Patient safety is never sacrificed to get more work done | 44 (37.0) | 13 (10.90) | 62 (52.1) | |
| A16Staff worry that mistakes they make are kept in their personnel file | 79 (65.8) | 24 (20.0) | 17 (14.2) | Needs improvement |
| A17 We have patient safety problems in this unit | 38 (31.7) | 27 (22.5) | 55 (45.8) | Needs improvement |
| A18 Our procedures and systems are good at preventing errors from happening | 30 (24.8) | 27 (22.3) | 64 (52.9) | |
| B1 My supervisor says a good word when he/she sees a job done according to established pattern safety procedures | 15 (12.3) | 17 (13.9) | 90 (73.8) | |
| B2 My supervisor seriously considers staff suggestions for improving patient safety | 19 (15.7) | 17 (14.0) | 85 (70.3) | |
| B3 Whenever pressure builds up, my supervisor wants us to work faster even if it means taking shortcuts | 34 (27.9) | 29 (23.8) | 59 (48.4) | Needs improvement |
| B4 My supervisor overlooks patient safety problems that happen over and over | 9 (7.4) | 14 (11.5) | 99 (81.2) | Strength |
| C1 We are given feedback about changes put into place based on event reports | 41 (33.9) | 47 (38.8) | 33 (27.2) | Needs improvement |
| C2 Staff will freely speak up if they see something that may negatively affect patient care | 18 (25.0) | 43 (35.8) | 59 (49.2) | Needs improvement |
| C3 We are informed about errors that happen in this unit | 17 (14.1) | 41 (33.9) | 63 (42.0) | Needs improvement |
| C4 Staff feel free to question the decisions or actions of those with some authority | 86 (72.9) | 20 (16.9) | 12 (10.2) | Needs improvement |
| C5 In this unit, we discuss ways to prevent errors from happening | 21 (18.0) | 27 (23.1) | 69 (59.0) | |
| C6 Staff are afraid to ask questions when something does not seem right | 48 (40.3) | 44 (37.0) | 27 (22.7) | Needs improvement |
| D1 When a mistake is made but is caught and corrected before affecting the patient, how often is this reported? | 50 (41.3) | 39 (32.2) | 32 (26.4) | Needs improvement |
| D2 When a mistake is made but has no potential to harm the patient, how often is this reported? | 62 (51.2) | 39 (32.2) | 20 (16.6) | Needs improvement |
| D3 When a mistake is made, that could harm the patient but does not, how often is this reported? | 41 (34.1) | 41 (34.2) | 38 (31.6) | Needs improvement |
| F1 Hospital management provides a work climate that promotes patient safety | 35 (28.7) | 27 (22.1) | 60 (49.2) | Needs improvement |
| F2 Hospital units do not coordinate well with each other | 48 (39.4) | 20 (16.4) | 54 (44.3) | Needs improvement |
| F3 Things escape attention when transferring patients from one unit to another | 39 (31.9) | 32 (26.2) | 51 (41.8) | Needs improvement |
| F4 There is poor cooperation among hospital units that need to work together | 26 (21.4) | 23 (18.9) | 73 (59.8) | |
| F5 Important patient care information is often lost during shift changes | 41 (24.2) | 18 (15.0) | 61 (50.8) | |
| F6 It is often unpleasant to work with staff from other hospital units | 23 (19.2) | 26 (21.7) | 71 (59.1) | |
| F7 Problems often occur in the exchange of information across hospital units | 42 (35.0) | 25 (20.8) | 53 (44.2) | Needs improvement |
| F8The actions of hospital management show that patient safety is top priority | 18 (14.9) | 34 (28.1) | 69 (57.0) | |
| F9 Hospital management seems interested in patient safety only after an adverse event happens | 42 (34.7) | 25 (20.7) | 54 (44.6) | Needs improvement |
| F10 Hospital units work well together to provide the best care for patients | 8 (6.7) | 27 (22.5) | 85 (70.9) | |
| F11 Shift changes are problematic for patients in the hospital | 33 (27.3) | 27 (22.3) | 61 (50.4) |
The composite that has the lowest average percentage positive score was non-punitive response to error, at 17%. This composite, along with communication openness, feedback and communication about error, frequency of events reported, handoffs and transition and staffing was perceived by the HCWs as having weak safety culture (composite score ≤ 50%) and therefore need improvement. Out of the 12 composites, teamwork within units has the highest average percentage positive score and was the only area of demonstrable strength (composite score ˃75%), with a score of 79.6% (Table 3) The derived overall average composite score was 47%, indicating that overall the HCWs have a weak perception of safety culture in the hospital, necessitating an improvement.
Table 3.
Patient safety culture composite scores
| Composite | Component items | Positive responses | Total responses | % Positive response to item | ||
|---|---|---|---|---|---|---|
| Overall perception of patient safety |
A10 A15 A17 A18 |
67 62 55 64 |
120 119 120 121 |
67/120 = 55.8% 62/119 = 52.1% 55/120 = 45.8% 64/121 = 52.9% |
||
| Average composite score = 51.7% | ||||||
| Communication openness |
C2 C4 C6 |
59 12 27 |
120 118 119 |
59/120 = 49.2% 12/118 = 10.2% 27/119 = 22.7% |
||
| Average composite score = 27.4% (Needs improvement) | ||||||
| Feedback and communication about error |
C1 C3 C5 |
33 63 69 |
121 121 117 |
33/121 = 27.2% 63/121 = 52.1% 69/117 = 59.0% |
||
| Average composite score = 46.1% (Needs improvement) | ||||||
| Frequency of events reported |
D1 D2 D3 |
32 20 38 |
121 121 120 |
32/121 = 26.4% 20/121 = 16.5% 38/120 = 31.7% |
||
| Average composite score = 24.9% (Needs improvement) | ||||||
| Handoffs and transition |
F3 F5 F7 F11 |
51 61 53 61 |
122 120 120 121 |
51/122 = 41.8% 61/120 = 50.8% 53/120 = 44.2% 61/121 = 50.4% |
||
| Average composite score = 46.8% (Needs improvement) | ||||||
| Management support for patient safety |
F1 F8 F9 |
60 69 54 |
122 121 121 |
60/122 = 49.2% 69/121 = 57.0% 54/121 = 44.6% |
||
| Average composite score = 50.3% | ||||||
| Non-punitive response to error |
A8 A12 A16 |
22 22 17 |
121 118 120 |
22/121 = 18.2% 22/118 = 18.6% 17/120 = 14.2% |
||
| Average composite score = 17% (Needs improvement) | ||||||
| Organizational learning-Continuous improvement |
A6 A9 A13 |
100 62 69 |
121 119 120 |
100/121 = 82.6% 62/119 = 52.1% 69/120 = 57.5% |
||
| Average composite score = 64.1% | ||||||
| Staffing |
A2 A5 A7 A14 |
17 14 83 24 |
122 121 121 120 |
17/122 = 14.0% 14/121 = 11.6% 83/121 = 68.6% 24/120 = 20.0% |
||
| Average composite score = 28.6% (Needs improvement) | ||||||
| Supervisor/ Manager actions promoting patient safety |
B1 B2 B3 B4 |
90 85 59 99 |
122 121 122 122 |
90/122 = 73.8% 85/121 = 70.2% 59/122 = 48.4% 99/122 = 81.1% |
||
| Average composite score = 68.4% | ||||||
| Teamwork across units |
F2 F4 F6 F10 |
54 73 71 85 |
122 122 120 120 |
54/122 = 44.3% 73/122 = 59.8% 71/120 = 59.1% 85/120 = 70.8% |
||
| Average composite score = 58.5% | ||||||
| Teamwork within units |
A1 A3 A4 A11 |
112 103 92 81 |
122 122 122 121 |
112/122 = 91.8% 103/122 = 84.4% 92/122 = 75.4% 81/121 = 66.9% |
||
| Average composite score = 79.6% (Strength) | ||||||
In this study the professional roles of the surgeon, nurse anaesthetist and perioperative nurse, correspond with the work areas of surgery, anesthesiology and perioperative nursing, respectively. There were significant differences between the various work areas/ professional groups perception of safety culture in as many as seven out of the twelve composites/dimensions; with the nurse anaesthetists having the highest perception of safety culture and the surgeons having the least (Table 4). Tukey HSD post-hoc test for inter-group comparability further highlighted the relative position of the various professional roles regarding the respective composites (Table 4). The perception of safety culture by the various work areas/professional groups regarding the other five composites was similar.
Table 4.
Comparison of patient safety composite scores of the different groups of OR personnel
| Variable | Nurse anesthetists (n = 27) Mean ± SD |
Surgeons (n = 59) Mean ± SD |
Peri-op nurses (n = 36) Mean ± SD |
P value | Tukey HSD post-hoc test (p < 0.05) |
|---|---|---|---|---|---|
| Overall perception of patient safety | 3.2 ± 0.8 | 3.1 ± 0.8 | 3.4 ± 0.7 | 0.175 | |
| Communication openness | 3.0 ± 0.6 | 2.8 ± 0.8 | 2.7 ± 0.6 | 0.199 | |
| Feedback and communication about error | 3.8 ± 0.6 | 3.2 ± 0.7 | 3.2 ± 0.8 | 0.001 | Nurse anaesthetists ˃ periop nurses, surgeons |
| Frequency of events reported | 3.2 ± 0.9 | 2.6 ± 0.9 | 3.0 ± 0.9 | 0.023 | Nurse anaesthetists ˃ surgeons |
| Handoffs and transition | 3.4 ± 0.8 | 2.9 ± 0.8 | 3.4 ± 0.7 | < 0.001 | Nurse anaesthetists, periop nurses ˃ surgeons |
| Management support for patient safety | 3.6 ± 0.7 | 3.1 ± 0.9 | 3.5 ± 0.9 | 0.011 | Nurse anaesthetists, periop nurses ˃ surgeons |
| Non-punitive response to error | 2.4 ± 0.6 | 2.5 ± 0.7 | 2.3 ± 0.7 | 0.193 | |
| Organizational learning- Continuous improvement | 4.0 ± 0.5 | 3.4 ± 0.7 | 3.6 ± 0.6 | 0.001 | Nurse anaesthetists ˃ surgeons |
| Staffing | 2.6 ± 0.5 | 2.5 ± 0.7 | 2.6 ± 0.5 | 0.403 | |
| Supervisor/ Manager actions promoting patient safety | 4.0 ± 0.4 | 3.6 ± 0.7 | 3.7 ± 0.7 | 0.035 | Nurse anaesthetists ˃ surgeons |
| Teamwork across units | 3.6 ± 0.7 | 3.3 ± 0.7 | 3.6 ± 0.6 | 0.064 | |
| Teamwork within units | 4.1 ± 0.5 | 3.7 ± 0.7 | 3.9 ± 0.6 | 0.006 | Nurse anaesthetists ˃ surgeons |
| Group mean composite score | 3.5 ± 0.3 | 3.1 ± 0.5 | 3.3 ± 0.4 | 0.003 | Nurse anaesthetists ˃ surgeons |
As much as 85.2% of the respondents (104/122) did not report any adverse event in the past 12 months (Table 5). Only 38.2% of the respondents (44/115) regarded the patient safety quality in their own work area as very good or excellent (Table 5).
Table 5.
Respondent’s grading of patient safety in their respective work area and number of adverse events reported during the last 12 months
| Variable | Frequency | Percent (%) |
|---|---|---|
| In past 12 months, number of EVENT REPORTS made | (n = 122) | |
| None | 104 | 85.2 |
| 1–2 event reports | 12 | 9.8 |
| 3–5 event reports | 3 | 2.5 |
| 6–10 event reports | 3 | 2.5 |
| Respondent’s grading of patient safety in their respective work areas | (n = 115) | |
| Excellent | 9 | 7.8 |
| Very Good | 35 | 30.4 |
| Acceptable | 56 | 48.7 |
| Poor | 15 | 13.0 |
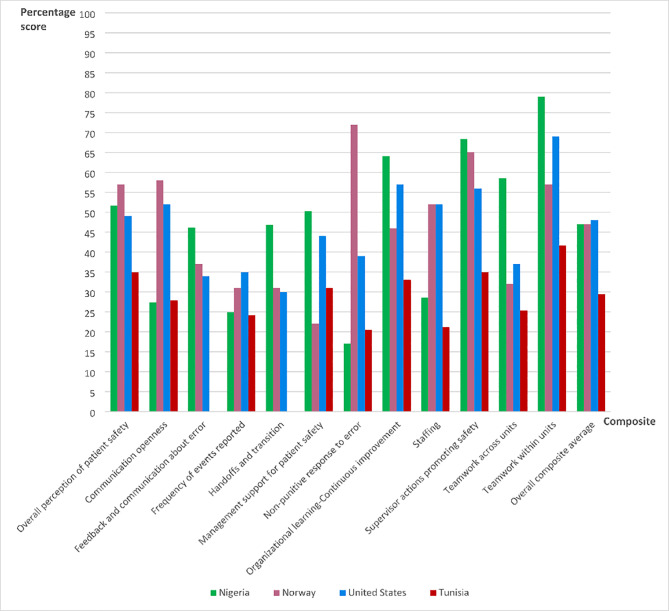
Figure 1 summarizes the percentage scores of the patient safety composites and overall average composite score in our operating rooms, alongside others from different countries where the HSOPSC instrument was used for safety culture assessment.
Fig. 1.
Bar chart showing the composite scores of patient safety culture in our ORs with others from different countries [12, 22, 23]
The comparative surveys were conducted among OR personnel in five Tunisian hospitals [12] and a single-center survey each in Norway [22] and the United States [23]. The overall average composite score of patient safety culture in our ORs was 47%, compared to the ORs in Tunisia; 29.5%, Norway; 47% and the United States; 48% (Fig. 1). Our ORs had the lowest scores in the dimensions of “non-punitive response to error”; 17% and communication openness”; 27.4% compared to the ORs in Tunisia, Norway and the United States.
Discussion
This study investigated the safety culture in the operating rooms of a Nigerian referral hospital using the HSOPSC. The overall average composite was 47%, but dimension scores ranged from 17% for non-punitive response to error to 79.6% for teamwork within units.
Very few publications have evaluated the patient safety culture in the operating room, among them a Tunisian multicenter study [12], a Norwegian single- institution survey [22] and an American single-institution survey [23]. A few others utilized survey tools other than the HSOPS [24–26] but comparisons with these are not tenable owing to differences in the factor components.
The high response rate of 92.4% obtained in our study may in part derive from the paper-based mode of the survey, single-site location and the size of the sample population. It compares well with the 70.8% response rate of the paper-based multicenter survey that targeted 544 OR staff in five Tunisian hospitals [12]. The Norwegian survey that utilized the mixed distribution method of survey (web and paper modes) in assessing patient safety culture among 575 OR staff had reported a response rate of 62% [22], whereas the online survey that evaluated patient safety culture among 431 OR staff in a United States hospital recorded a response rate of 67% [23]. Paper-based surveys yield higher response rates compared to web-based surveys making them less prone to non-response bias and more reflective of the sample population [27, 28].
The overall average composite score of patient safety culture in our ORs compares well with that of operating rooms in Norway [22] and the United States [23], but exceeds that in Tunisia [12]. Nigeria currently has no national policy on patient safety. However, the implementation of the WHO Surgical Safety Checklist (SSC) in our hospital since 2013 may have impacted on the safety culture despite the obvious constraints of infrastructure and socioeconomic limitations in our environment. Kawano et al. had earlier documented the positive effect of WHO SSC implementation by surgical teams on safety attitudes and climate in the hospital setting in Japan [29]. With the implementation of a National Patient Safety Campaign in Norway (2011–2013) which has SSC compliance rates at hospital level as a quality indicator, a longitudinal cross-sectional study was conducted in a large Norwegian tertiary hospital to evaluate its impact on safety culture by comparing the pre- and post-intervention safety culture perception among OR personnel [30]. Their study revealed that introduction of the WHO SSC brought about improvement in all the patient safety culture composites and that compliance rate in the use of the SSC correlated positively with improvements in safety culture composites/dimensions. We observed wide disparity across the patient safety composites, being highest in teamwork within hospital units and lowest in non-punitive response to error. Teamwork within hospital units defines the extent to which the respondents in a unit support each other, treat each other with respect, and work together as a team. This composite was the strongest in our study as well as the studies conducted in the United States [23, 31] and Tunisia [12]. Non-punitive response to error defines the extent to which the respondents feel that their mistakes and event reports are not held against them and that mistakes are not kept in their personnel record. The very low score is indicative of a prevalent culture of blame. Blame, and the fear of blame have been recognized as constituting pernicious impediment to patient safety as they are associated with lack of trust and poor reporting culture [32]. The poorest perception attributed to this safety culture composite in our study was shared by other studies [12, 31] but contrasts sharply with the Norwegian ORs where it was the strongest composite [22]. The high score of this composite in the Norwegian ORs could be reflective of an enduring “system approach” as against the more prevalent “person approach” to error management [32].
The very low perception regarding non-punitive response to error in our ORs correspond with an equally low tally of frequency of events reported; both signifying a poor reporting culture. Compared to the ORs in Tunisia, Norway and the United States, our personnel had better perception of seven patient safety composites regarding; teamwork within units, teamwork across units, organizational learning-continuous improvement, management support for patient safety, supervisor actions promoting safety, handoffs and transition, and feedback and communication about error. None of the three considered studies in previous literature could pride itself of any area of strength with respect to the 12 patient safety dimensions [12, 22, 23]. Equally dismal were the findings of a recent survey of five cardiovascular surgical centers in the United States, further alluding to pervasive poor safety culture in the ORs [33].
The safety culture perception in our ORs is comparable, and arguably better, than that in ORs cited in Norway and the United States despite the huge socioeconomic disparities. It would thus appear that factors beyond the socioeconomic milieu, such as the implementation of the WHO Surgical Safety Checklist (SSC) in our hospital may have played a positive role in the perception of patient safety culture by the OR personnel. The impact of such protocol implementation on safety attitudes is documented, and has been stated earlier [29]. Thus, even resource-poor environments could have better or comparable patient safety culture with those that have economic advantage.
In the light of suggestions that variations exist in the perception of safety culture by HCWs with different professional backgrounds [33], we conducted a subanalysis of the responses based on professional roles and work areas. We observed that the various categories of personnel in the OR rated safety culture differently. Our finding was supported by the Norwegian study wherein anesthesiologists and nurse anaesthetists had higher mean scores than the surgeons and operating theatre nurses [22]. Similarly, the Tunisian study reported that physicians rated the safety culture of operating rooms lower than the paramedical staff (nurses, anaesthetic and surgical technicians, nurses’ assistants) in most of the dimensions [12]. The lowest perception of patient safety among the surgeons implies that they were the least optimistic of the existing safety culture. An international survey on safety culture and attitudes among spine professionals had earlier revealed that most of the respondents believe that the surgeon has responsibility for both the prevention of adverse events and improvement of the safety culture in the operating room [25]. Such a mindset could influence a more critical appraisal of patient safety among the surgeons compared to the perioperative nurses and the nurse anaesthetists. Remarkable variation in perception between the different categories of personnel had also been reported by studies on safety climate conducted with the SAQ among OR personnel in Brazil and Sweden [34, 35].
As much as 85% of our respondents made no report of adverse events over the past 12 months. The Tunisian study which presented data on adverse event reporting also declared that 90.2% of the respondents had reported no adverse event in the past 12 months [12]. It is likely that events were underreported in these settings and several potential patient safety problems may not have been recognized and addressed, posing further danger to the patients.
The systems approach has been recommended and effectively implemented in error management in high risk industries like aviation [36]. However, its application in healthcare is still constrained while the persisting ‘culture of blame’ propels wanton administrative, professional and legal liabilities on HCWs for medical errors [37]. This culture arguably contributes to the festering poor scores in the dimensions of non-punitive response to error and frequency of adverse events reported. Furthermore, the decision to report errors by HCWs is influenced by their proneness to shame and their perception of the organizational attitude towards restoring their self-image [38]. This would suggest that both non-punitive response to errors and management support for patient safety would enhance error reporting which is a crucial process in medical error management and patient safety.
The 2021 User Comparative Database Report for Version 1.0 obtained from 191,977 hospital staff in 320 hospitals in the United States who were surveyed between December 2017 and.
October 2020, recorded a much better ‘overall average composite score’ of 65% compared to the 47% of our study [31]. But a major flaw in comparing OR patient safety culture reports with the 2021 User Comparative Database Report for Version 1.0 of the United States derives from the fact that the latter surveyed hospital-wide personnel encompassing administrative staff, rehabilitation, medicine, pharmacy, et cetera. Interestingly, respondents in the work areas of anesthesiology and surgery constituted only 1% and 11% of the surveyed population, respectively; suggesting that the majority of the respondents were non-OR personnel. With such differing characteristics in work area and staff position the perception of the respondents in the latter could not be adjudged to represent the culture of the OR environment in view of known professional and work area-related disparities in safety culture perception. For instance, the work area characteristics of the 2021 User Comparative Database Report revealed that respondents from rehabilitation section (work area) had the highest average composite score of 72%, while respondents from administration (staff position) had the highest average composite score of 78%. These were much higher than the composite scores attributed to anesthesiology, surgery, attending surgeons, residents and registered nurses who characterize the OR environment. Moreover, as much as 22% of the respondents in the comparative database do not have any direct interaction with the patients.
Several broad-based initiatives have been embarked upon by governments to systemically and specifically improve patient safety. In Sweden patient safety got a boost in 2011 with the enactment of the patient safety act and implementation of government-supported financial incentive for patient safety actions in healthcare facilities, including safety culture improvement [39]. In Denmark too, the legislation on patient safety was passed in 2003 and sought to improve patient safety by; ensuring that (i) frontline personnel report all adverse events (ii) hospital acts on the reports (iii) the National Board of Health disseminate learning from them while protecting the personnel from disciplinary investigations and legal sanctions [40]. In aligning with the above initiatives, ‘improvement in organizational culture to encourage reporting and avoid blame’ received the strongest recommendation of 22 suggested options for enhancing patient safety by Swedish patient safety-oriented healthcare professionals, whereas increasing the number of physicians, nurses, and hospital beds were rated 12th, 15th and 17th respectively and ‘increased penalty for personnel who make mistakes’ got the least recommendation [39].
The HSOPSC survey, like the other patient safety instruments measure abstract phenomena termed composite/ dimensions from self-reported perceptions of safety culture and attitudes. Such models facilitate data reduction by means of orderly simplification of a number of interrelated measures. The use of instruments with sound psychometric property is thus critical since the multiple items measured are presumed to represent the fewer underlying constructs. The HSOPSC has been validated in over 62 studies conducted in over 29 countries [41]. However, in spite of its popularity and wide application its psychometric properties have been challenged, with some researchers advocating revision of some of the instrument’s items and composites [22, 41]. A revision of the original Hospital Survey on Patient Safety Culture version 1.0 survey has recently been released by AHRQ (HSOPS 2.0) [42].
Furthermore, the survey being a self-reported perception the potential for response bias cannot be ruled out. Our assessment of patient safety culture in the OR was not comprehensive, as the very few number of physician anaesthetists precluded them from the study (in line with the instrument guideline), while health attendants were not considered owing to their poor comprehension of the instrument. Nevertheless, the surveyed personnel represent over 85% of the OR staff and could justifiably be deemed representative.
Despite having the English language as the lingua franca in Nigeria, we did not conduct cultural adaptation and further validation of the original English version of the HSOPSC which was developed within the American cultural environment in order to ensure the equivalence of meaning for this cross-cultural research as it were. Hence, whereas we did not substantially alter the original validated English version which would contribute to psychometric distortions the results we obtained may not have accurately reflected what they are supposed to measure. Thus, we concede that the use of a previously validated instrument does not necessarily imply validity in another culture or context [43, 44]. However, such limitations that may arise from variations in the psychometric properties of measurement instruments are a common feature in cross-cultural research, including those conducted with the HSOPSC [45]. It must also be acknowledged that the multiplicity of other factor models proposed for the HSOPSC instrument in different studies such as the 11- factor [22], 10-factor [46], 9-factor [47] and 8-factor models [48] complicate the process of comparing outcomes. Our study instituted only a minor modification of item F3 by rewording it as indicated in the methods section; a minimum which is permissible by the instrument developers [14]. The French validated version of the Hospital Survey on Patient Safety Culture questionnaire used by Mallouli et al. comprised only of 10 composites with 45 items [12], as against 10 composites and 42 items in the original version which we used. In view of such variations which are rather common with the different adaptations of the instrument direct comparison of the results of different surveys demands circumspection.
Recommendations
It is hoped that the implementation of relevant interventions that this study has spurred will bring about improvement in the safety culture of our ORs, as have been observed in follow-up studies conducted in Saudi Arabia [49], Japan [29] and Norway [30]. Furthermore, with this benchmark a follow-up survey to evaluate the outcome of implemented interventions would be necessary, and is highly recommended.
Conclusion
So far, despite subtle variations in the versions of the HSOPSC questionnaire used in the different studies, our study appears to be the first to record even one area of strength across the composites of patient safety culture. With a low overall average composite score and as many as half of the composites requiring improvement our OR safety culture could be adjudged to be weak, its comparative strengths notwithstanding. The finding is disconcerting owing to the association between weak patient safety climate and poor patient outcomes. The picture of safety culture emanating from the ORs discussed herein is worrisome and may indeed be a major contributor to the gloomy statistics of surgery-related morbidity and mortality, globally.
Acknowledgements
We appreciate the kind effort of Dr Osita Ede in helping out with the data analysis.
Abbreviations
- AHRQ
Agency of Healthcare Research and Quality
- ANOVA
Analysis of variance
- HCW
Healthcare worker
- HSOPSC
Hospital survey on patient safety culture
- INAES
Irish National Adverse Events Study
- OR
Operating room
- SAQ
Safety attitudes questionnaire
- SPSS
Statistical package for social science
- SSC
Surgical safety checklist
- WHO
World health organization
Authors’ contributions
AN: Conceptualization, study design, data collection and writing of the manuscript. EO: Manuscript development, data analysis and interpretation, revision of the draft manuscript. FA: Conceptualization, data collection, revision of the draft manuscript. OO: Conceptualization, manuscript development and revision of the draft manuscript. AA: Study design, manuscript development and revision of the draft manuscript. IA: Study design, manuscript development and revision of the draft manuscript. All authors read and approved the final manuscript.
Funding
Nil.
Data availability
All data generated or analyzed during this study are included in this published article.
Declarations
Ethics approval and consent to participate
The study protocol for the survey was reviewed and approved by the Research Ethics Committee of National Orthopaedic Hospital, Enugu. (IRB Number S.313/IV/; Protocol Number 2022/1/103). Only consenting eligible HCWs were recruited, having duly signed to a written informed consent form. We affirm that all methods were carried out in accordance with the ‘Declaration of Helsinki’ regarding ethical principles for medical research involving human subjects.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization. Quality of care: patient safety. In: Fifty-Fifth World Health Assembly WHA 55.18. Agenda Item 13.9. (2002). Available online at: https://apps.who.int/gb/archive/pdf_files/WHA55/ewha5518.pdf. Accessed 12 Nov 2021.
- 2.Jha AK, Larizgoitia I, Audera-Lopez C, Prasopa-Plaizier N, Waters H, Bates DW. The global burden of unsafe medical care: analytic modeling of observational studies. BMJ Qual Saf. 2013;22(10):809–15. doi: 10.1136/bmjqs-2012-001748. [DOI] [PubMed] [Google Scholar]
- 3.Ozeke O, Ozeke V, Coskun O, Budakoglu II. Second victims in health care: current perspectives. Adv Med Educ Pract. 2019;10:593–603. doi: 10.2147/AMEP.S185912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rafter N, Hickey A, Conroy RM, Condell S, O’Connor P, Vaughan D, et al. The Irish National Adverse Events Study (INAES): the frequency and nature of adverse events in Irish hospitals-a retrospective record review study. BMJ Qual Saf. 2017;26(2):111–9. doi: 10.1136/bmjqs-2015-004828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schwendimann R, Blatter C, Dhaini S, Simon M, Ausserhofer D. The occurrence, types, consequences and preventability of in-hospital adverse events - a scoping review. BMC Health Serv Res. 2018;18(1):521. doi: 10.1186/s12913-018-3335-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sousa P, Uva AS, Serranheira F, Nunes C, Leite ES. Estimating the incidence of adverse events in Portuguese hospitals: a contribution to improving quality and patient safety. BMC Health Serv Res. 2014;14:311. doi: 10.1186/1472-6963-14-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Halfon P, Staines A, Burnand B. Adverse events related to hospital care: a retrospective medical records review in a Swiss hospital. Int J Qual Health Care. 2017;29(4):527–33. doi: 10.1093/intqhc/mzx061. [DOI] [PubMed] [Google Scholar]
- 8.Weiser TG, Gawande A. Excess Surgical Mortality: Strategies for Improving Quality of Care. In: Debas HT, Donkor P, Gawande A, et al., editors. Essential Surgery: Disease Control Priorities, Third Edition (Volume 1). Washington (DC): The International Bank for Reconstruction and Development / The World Bank; 2015 Apr 2. Chapter 16. Available from: https://www.ncbi.nlm.nih.gov/books/NBK333498. Accessed 10 Apr 2022.
- 9.Hansen LO, Williams MV, Singer SJ. Perceptions of hospital safety climate and incidence of readmission. Health Serv Res. 2011;46(2):596–616. doi: 10.1111/j.1475-6773.2010.01204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Najjar S, Nafouri N, Vanhaecht K, Euwema M. The relationship between patient safety culture and adverse events: a study in Palestinian hospitals. Saf Health. 2015;1(1):16. doi: 10.1186/s40886-015-0008-z. [DOI] [Google Scholar]
- 11.Braithwaite J, Herkes J, Ludlow K, Testa L, Lamprell G. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open. 2017;7(11):e017708. doi: 10.1136/bmjopen-2017-017708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mallouli M, Tlili MA, Aouicha W, Rejeb MB, Zedini C, Salwa A, et al. Assessing patient safety culture in Tunisian operating rooms: A multicenter study. Int J Qual Health Care. 2017;29(2):176–82. doi: 10.1093/intqhc/mzw157. [DOI] [PubMed] [Google Scholar]
- 13.Campbell EG, Singer S, Kitch BT, Iezzoni LI, Meyer GS. Patient safety climate in hospitals: act locally on variation across units. Jt Comm J Qual Patient Saf. 2010;36(7):319–26. doi: 10.1016/s1553-7250(10)36048-x. [DOI] [PubMed] [Google Scholar]
- 14.Sorra J, Gray L, Streagle S, Famolaro T, Yount N, Behm J. AHRQ Hospital Survey on Patient Safety Culture: User’s Guide. (Prepared by Westat, under Contract No. HHSA290201300003C). AHRQ Publication No. 15-0049-EF (Replaces 04–0041). Rockville, MD: Agency for Healthcare Research and Quality. January 2016. http://www.ahrq.gov/professionals/quality-patientsafety/patientsafetyculture/hospital/index.html. Accessed 12 Nov 2021.
- 15.Sexton JB, Helmreich RL, Neilands TB, Rowan K, Vella K, Boyden J, et al. The Safety Attitudes Questionnaire: psychometric properties, benchmarking data, and emerging research. BMC Health Serv Res. 2006;6:44. doi: 10.1186/1472-6963-6-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Etchegaray JM, Thomas EJ. Comparing two safety culture surveys: safety attitudes questionnaire and hospital survey on patient safety. BMJ Qual Saf. 2012;21(6):490–8. doi: 10.1136/bmjqs-2011-000449. [DOI] [PubMed] [Google Scholar]
- 17.Flin R, Burns C, Mearns K, Yule S, Robertson EM. Measuring safety climate in health care. Qual Saf Health Care. 2006;15(2):109–15. doi: 10.1136/qshc.2005.014761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singer S, Lin S, Falwell A, Gaba D, Baker L. Relationship of safety climate and safety performance in hospitals. Health Serv Res. 2009;44(2 Pt 1):399–421. doi: 10.1111/j.1475-6773.2008.00918.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosen AK, Singer S, Zhao S, Shokeen P, Meterko M, Gaba D. Hospital safety climate and safety outcomes: is there a relationship in the VA? Med Care Res Rev. 2010;67(5):590–608. doi: 10.1177/1077558709356703. [DOI] [PubMed] [Google Scholar]
- 20.Council of Europe. (2006), “Recommendation Rec(2006)7 of the Committee of Ministers to member states on management of patient safety and prevention of adverse events in health care”. Available at: https://www.coe.int/t/dg3/health/recommendations_en.asp. Accessed 10 Oct 2021.
- 21.Sorra JS, Nieva VF. Hospital Survey on Patient Safety Culture. (Prepared by Westat, under Contract No. 290-96-0004). AHRQ Publication No. 04–0041. Rockville, MD: Agency for Healthcare Research and Quality. September 2004. Available at: https://proqualis.net/sites/proqualis.net/files/User%20guide%20HSOPSC.pdf. Accessed 9 Jul 2022.
- 22.Haugen AS, Søfteland E, Eide GE, Nortvedt MW, Aase K, Harthug S. Patient safety in surgical environments: cross-countries comparison of psychometric properties and results of the Norwegian version of the Hospital Survey on Patient Safety. BMC Health Serv Res. 2010;10:279. doi: 10.1186/1472-6963-10-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pimentel MPT, Choi S, Fiumara K, Kachalia A, Urman RD. Safety Culture in the Operating Room: Variability Among Perioperative Healthcare Workers. J Patient Saf. 2021;17(6):412–6. doi: 10.1097/PTS.0000000000000385. [DOI] [PubMed] [Google Scholar]
- 24.Nilsson U, Göras C, Wallentin FY, Ehrenberg A, Unbeck M. The Swedish Safety Attitudes Questionnaire– Operating Room Version: Psychometric Properties in the Surgical Team. J Perianesth Nurs. 2018;33(6):935–45. doi: 10.1016/j.jopan.2017.09.009. [DOI] [PubMed] [Google Scholar]
- 25.Gadjradj PS, Harhangi BS. Safety Culture and Attitudes Among Spine Professionals: Results of an International Survey. Global Spine Journal. 2019;9(6):642–9. doi: 10.1177/2192568218825247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zeynep T, Ayfer O, Ikbal C, Gozde TS, Tuluha A, Nuray A. Determining the Patient Safety Culture of Operating Room Nurses in Turkey. Int J Caring Sci. 2020;13(1):708. [Google Scholar]
- 27.Ebert JF, Huibers L, Christensen B, Christensen MB. Paper- or Web-Based Questionnaire Invitations as a Method for Data Collection: Cross-Sectional Comparative Study of Differences in Response Rate, Completeness of Data, and Financial Cost. J Med Internet Res. 2018;20(1):e24. doi: 10.2196/jmir.8353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Daikeler J, Bošnjak M, Lozar Manfreda K. Web versus other survey modes: an updated and extended meta-analysis comparing response rates. J Surv Stat Methodol. 2020;8(3):513–39. doi: 10.1093/jssam/smz008. [DOI] [Google Scholar]
- 29.Kawano T, Taniwaki M, Ogata K, Sakamoto M, Yokoyama M. Improvement of teamwork and safety climate following implementation of the WHO surgical safety checklist at a university hospital in Japan. J Anesth. 2014;28(3):467–70. doi: 10.1007/s00540-013-1737-y. [DOI] [PubMed] [Google Scholar]
- 30.Haugen AS, Søfteland E, Sevdalis N, Eide GE, Nortvedt MW, Vincent C, et al. Impact of the Norwegian National Patient Safety Program on implementation of the WHO Surgical Safety Checklist and on perioperative safety culture. BMJ Open Qual. 2020;9(3):e000966. doi: 10.1136/bmjoq-2020-000966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Famolaro T, Hare R, Yount ND, Fan L, Liu H, Sorra J. Surveys on Patient Safety CultureTM (SOPS®) Hospital Survey 1.0: 2021 User Database Report. (Prepared by Westat, Rockville, MD, under Contract No. HHSP233201500026I/HHSP23337004T). Rockville, MD: Agency for Healthcare Research and Quality; March 2021. AHRQ Publication No. 21 – 0016. Accessed 4 Sep 2022.
- 32.Reason J. Human error: models and management. BMJ. 2000;320(7237):768–70. doi: 10.1136/bmj.320.7237.768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marsteller JA, Wen M, Hsu YJ, Bauer LC, Schwann NM, Young CJ, et al. Safety Culture in Cardiac Surgical Teams: Data From Five Programs and National Surgical Comparison. Ann Thorac Surg. 2015;100(6):2182–9. doi: 10.1016/j.athoracsur.2015.05.109. [DOI] [PubMed] [Google Scholar]
- 34.Carvalho PA, Göttems LB, Pires MR, de Oliveira ML. Safety culture in the operating room of a public hospital in the perception of healthcare professionals. Rev Lat Am Enfermagem. 2015;23(6):1041–8. doi: 10.1590/0104-1169.0669.2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Göras C, Unbeck M, Nilsson U, Ehrenberg A. Interprofessional team assessments of the patient safety climate in Swedish operating rooms: a cross-sectional survey. BMJ Open. 2017;7(9):e015607. doi: 10.1136/bmjopen-2016-015607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helmreich RL. On error management: lessons from aviation. BMJ. 2000;320(7237):781–5. doi: 10.1136/bmj.320.7237.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Glauser W. Should medical errors ever be considered criminal offences? CMAJ. 2018;190(16):E518–9. doi: 10.1503/cmaj.109-5588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zabari M, Southern NL. Effects of Shame and Guilt on Error Reporting Among Obstetric Clinicians. J Obstet Gynecol Neonatal Nurs. 2018;47:468–78. doi: 10.1016/j.jogn.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 39.Nygren M, Roback K, Öhrn A, Rutberg H, Rahmqvist M, Nilsen P. Factors influencing patient safety in Sweden: perceptions of patient safety officers in the county councils. BMC Health Serv Res. 2013;13:52. [DOI] [PMC free article] [PubMed]
- 40.Bjørn B, Anhøj J, Lilja B. Rapportering af utilsigtede haendelser: fem års erfaringer med et nationalt rapporteringssystem [Reporting of patient safety incidents: experience from five years with a national reporting system] Ugeskr Laeger. 2009;171(20):1677–80. [PubMed] [Google Scholar]
- 41.Waterson P, Carman EM, Manser T, Hammer A. Hospital Survey on Patient Safety Culture (HSPSC): a systematic review of the psychometric properties of 62 international studies. BMJ Open. 2019;9(9):e026896. doi: 10.1136/bmjopen-2018-026896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sorra J, Yount N, Famolaro T, Gray L. AHRQ Hospital Survey on Patient Safety Culture Version 2.0: User’s Guide. (Prepared by Westat, under Contract No. HHSP233201500026I/ HHSP23337004T). Rockville, MD: Agency for Healthcare Research and Quality; September 2019. AHRQ Publication No. 19–0076. https://www.ahrq.gov/sops/surveys/hospital/index.html. Accessed 4 Sep, 2022.
- 43.Stevelink SA, van Brakel WH. The cross-cultural equivalence of participation instruments: a systematic review. Disabil Rehabil. 2013;35(15):1256–68. doi: 10.3109/09638288.2012.731132. [DOI] [PubMed] [Google Scholar]
- 44.Buil I, de Chernatony L, Martínez E. Methodological issues in cross-cultural research: An overview and recommendations. J Target Meas Anal Mark. 2012;20:223–34. doi: 10.1057/jt.2012.18. [DOI] [Google Scholar]
- 45.Palmieri PA, Leyva-Moral JM, Camacho-Rodriguez DE, Granel-Gimenez N, Ford EW, Mathieson KM, et al. Hospital survey on patient safety culture (HSOPSC): a multi-method approach for target-language instrument translation, adaptation, and validation to improve the equivalence of meaning for cross-cultural research. BMC Nurs. 2020;19:23. doi: 10.1186/s12912-020-00419-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Perneger TV, Staines A, Kundig F. Internal consistency, factor structure and construct validity of the French version of the Hospital Survey on Patient Safety Culture. BMJ Qual Saf. 2014;23:389–97. doi: 10.1136/bmjqs-2013-002024. [DOI] [PubMed] [Google Scholar]
- 47.Waterson P, Griffiths P, Stride C, Murphy J, Hignett S. Psychometric properties of the Hospital Survey on Patient Safety Culture: findings from the UK. Qual Saf Health Care. 2010;19(5):e2. doi: 10.1136/qshc.2008.031625. [DOI] [PubMed] [Google Scholar]
- 48.Brajshori N, Behrens J, Translation Cultural Adaption and Validation of Hospital Survey on Patient Safety Culture in Kosovo. Open J Nurs. 2016;06:483–90. doi: 10.4236/ojn.2016.66050. [DOI] [Google Scholar]
- 49.Alswat K, Abdalla RAM, Titi MA, Bakash M, Mehmood F, Zubairi B, et al. Improving patient safety culture in Saudi Arabia (2012–2015): trending, improvement and benchmarking. BMC Health Serv Res. 2017;17(1):516. doi: 10.1186/s12913-017-2461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.