Abstract
Objective
This study aimed to evaluate the safety and tolerability of OP-724, a CREB-binding protein/β-catenin inhibitor, in patients with advanced primary biliary cholangitis (PBC).
Design
An open-label, non-randomised, phase 1 trial was conducted at two hospitals in Japan. Patients with advanced PBC classified as stage III or higher according to the Scheuer classification by liver biopsy between 4 September 2019 and 21 September 2021 were enrolled. Seven patients received intravenous OP-724 infusions at escalating dosages of 280 and 380 mg/m2/4 hours two times weekly for 12 weeks. The primary endpoint was the incidence of serious adverse events (SAEs). The secondary endpoints were the incidence of AEs and the improvement in the modified Histological Activity Index (mHAI) score.
Results
Seven patients (median age, 68 years) were enrolled. Of these seven patients, five completed twelve cycles of treatment, one discontinued prematurely for personal reasons in the 280 mg/m2/4 hours cohort, and one in the 380 mg/m2/4 hours cohort was withdrawn from the study due to drug-induced liver injury (grade 2). Consequently, the recommended dosage was determined to be 280 mg/m2/4 hours. SAEs did not occur. The most common AEs were abdominal discomfort (29%) and abnormal hepatic function (43%). OP-724 treatment was associated with histological improvements in the fibrosis stage (2/5 (40%)) and mHAI score (3/5 (60%)) on histological analysis.
Conclusion
Administration of intravenous OP-724 infusion at a dosage of 280 mg/m2/4 hours two times weekly for 12 weeks was well tolerated by patients with advanced PBC. However, further evaluation of antifibrotic effects in patients with PBC is warranted.
Trial registration number
Keywords: PRIMARY BILIARY CIRRHOSIS, HEPATIC FIBROSIS, CLINICAL TRIALS, LIVER BIOPSY
WHAT IS ALREADY KNOWN ON THIS TOPIC.
Ursodeoxycholic acid (UDCA) and obeticholic acid are currently used as therapeutic agents for primary biliary cholangitis (PBC), an autoimmune cholestatic liver disease, and have been reported to suppress liver and bile duct damage and to improve the prognosis.
UDCA-refractory PBC may lead to persistent liver damage, progressive liver fibrosis and cirrhosis. In advanced PBC, liver failure and related complications, such as rupture of oesophageal varices, have become problems and the development of antifibrotic therapeutic drugs is desired.
WHAT THIS STUDY ADDS
OP-724 selectively inhibits the interaction between the CREB-binding protein and β-catenin and has already been confirmed to be safe and tolerated in patients with cirrhosis due to hepatitis C virus or hepatitis B virus; in this study, OP-724 was evaluated in patients with advanced PBC.
The recommended dosage for patients with advanced PBC was determined to be 280 mg/m2/4 hours.
In the exploratory efficacy study, the liver biopsy results indicated that several patients exhibited improvement in fibrosis after administration.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
This study revealed that OP-724 has the potential to be a therapeutic drug for PBC-induced liver cirrhosis, which has not been put into practical use to date. Further investigations are required in the future.
Introduction
Primary biliary cholangitis (formerly termed primary biliary cirrhosis, PBC) is a chronic and progressive autoimmune cholestatic liver disease of unknown aetiology.1 PBC has a prevalence of 140 cases/million.2 Without treatment, the disease generally progresses to cirrhosis and liver failure over 10–20 years.3 Aside from liver transplantation (LT), it has been thought that there is currently no effective treatment for PBC.4 However, after several years of controversy, there is now a consensus to accept ursodeoxycholic acid (UDCA) as the standard therapy. UDCA has been shown to extend transplantation-free survival, especially when started early in the course of the disease.5–7 In a recent study, approximately 30%–40% of patients did not have an optimal biochemical response to UDCA. These patients exhibited more rapid disease progression than those with normalisation of serum alkaline phosphatase (ALP), aminotransferases and bilirubin.1 3 Furthermore, after contradictory meta-analyses and extensive debates, although UDCA has been recognised to slow disease progression and reduce mortality and the need for LT, this effect is more significant when UDCA is started at the early stages of the disease and is continued for life.8 This fact suggests that while UDCA is considered the first-line agent for treatment, it is ineffective in halting the progression of advanced PBC, which means established fibrosis. Obeticholic acid (OCA) was the second drug to successfully reduce serum ALP, aminotransferases and bilirubin for patients with PBC.9 10 OCA was conditionally approved by the US and EU regulatory authorities in 2016 for the treatment of PBC in patients with incomplete response or intolerance to UDCA. OCA is a synthetic bile acid derivative with a high affinity for farnesoid X receptor (FXR), a nuclear receptor that closely regulates bile acid synthesis and secretion, and has been shown to mediate anti-inflammatory and antifibrotic effects.9 11 Bezafibrate is also the third treatment option, after UDCA and OCA, to have shown clear beneficial effects in large, well-powered, placebo-controlled trials in PBC.12 13 However, antifibrotic drugs for liver cirrhosis associated with PBC are yet to be put into practical use.3 7 11 Bile acid receptors, such as FXR (as well as its transporter system) and fibroblast growth factor 19, are attracting attention as therapeutic targets for cholestatic liver disease and liver fibrosis.14 15 Although numerous clinical trials are underway, there is currently no therapeutic drug that can improve fibrosis in cirrhosis due to cholestasis.1 Abnormal Wnt/β-catenin signalling has been reported by several studies to be involved in liver fibrosis.16 17 Transforming growth factor-β/Smad3 signalling, a key mediator of abnormal extracellular matrix production, cross-talks with the Wnt/β-catenin pathway.18 19 β-catenin recruits the CREB-binding protein (CBP) or P300 (a homolog of CBP) as a coactivator to induce target gene transcription, with CBP and P300 playing distinct roles.20 21 We have recently shown that PRI-724, a low-molecular-weight compound that selectively inhibits the interaction between CBP and β-catenin, exerts antifibrotic effects in liver fibrosis models.22 PRI-724 is highly tolerated, as it does not inhibit P300/β-catenin signalling.20 23 Furthermore, phase 1 or 1/2a clinical trials to date have confirmed that PRI-724 does not have harmful effects in humans.24 25 We have also recently reported that PRI-724 exerts an antifibrotic effect in cholestatic liver fibrosis models.26 Based on the results of this non-clinical study, we planned a phase 1 clinical trial to evaluate the safety and tolerability of OP-724 (the new development code name for PRI-724) as a treatment for patients with advanced PBC. We also investigated the exploratory efficacy of OP-724 in patients with PBC by histological analysis and serum fibrosis marker.
In this study, we examined whether CBP/β-catenin inhibitor, OP-724, can be safely administered to patients with advanced fibrosis, which is an unsolved and important issue of PBC, and investigated its efficacy exploratively.
Methods
Study design and patients
This two-centre, open-label, cohort, phase 1 dosage-escalation trial sequentially enrolled patients with PBC who were treated at the Cancer and Infectious Diseases Center of Tokyo Metropolitan Komagome Hospital (Tokyo, Japan) and Kyushu University Hospital (Fukuoka, Japan).
Ohara Pharmaceutical. provided OP-724 (previously named ‘PRI-724’ but then renamed following the acquisition of the relevant license), along with related safety information and scientific advice. Eligible participants included patients aged 20–74 years who were diagnosed with PBC according to the following criteria: (1) observation of histologically chronic non-suppurative destructive cholangitis (CNSDC) and laboratory findings consistent with PBC (including cholestatic findings such as increases in ALP and gamma-glutamyl transpeptidase (GGT) levels), as indicated by the British Society of Gastroenterology/UK-PBC treatment and management guidelines7; (2) testing positive for anti-mitochondrial antibodies (AMA) and tissue images consistent with PBC even if CNSDC was not observed histologically and (3) testing positive for AMA and PBC being seemingly probable, considering the clinical presentation and progression if there was no opportunity to obtain histological findings. Patients were also deemed to be eligible if there was a definitive diagnosis of advanced liver fibrosis classified as stage III or higher according to the Scheuer classification27 by a liver biopsy performed during the screening period. Patients with current or previous primary liver cancer (excluding patients who underwent curative liver cancer resection or radiofrequency ablation at ≥1 year prior) were not eligible for inclusion.
Procedure
Patients were assigned into two cohorts, for which OP-724 at a dosage of 280 or 380 mg/m2/4 hours, respectively, was intravenously administered. OP-724 was administered for 12 cycles, with each cycle consisting of OP-724 administration two times a week. A single dose was administered on day 7 (tolerance: −7 days) prior to the start of administration in the first cycle. The starting dose was designated as level 2 (280 mg/m2). After confirming tolerability at level 2, the dose was escalated to level 3 (380 mg/m2). In this case, we initially administered 280 mg/m2/4 hours in three patients, which was followed with a second dose of 380 mg/m2/4 hours. However, abnormal hepatic function was observed in the first patient, prompting discontinuation. Three additional patients were enrolled in the 280 mg/m2/4 hours cohort.
Safety and pharmacokinetic evaluations were conducted at this dosage level. Blood samples were drawn before dosing; at 30 min, 1 hour, 2 hours and 4 hours after dosing; and at 1 hour, 5 hours and 20 hours after administration. Plasma concentrations of OP-724 and C-82 (an active metabolite of OP-724) were measured in the blood samples obtained from the patients during phase 1. Throughout the study, adverse events (AEs) and clinical laboratory results were recorded, and AEs were graded according to the Common Terminology Criteria for Adverse Events version 4.0. The investigators regularly assessed safety and tolerability, including the presentation of serious AEs (SAEs), particularly those associated with treatment discontinuation.
Liver biopsy samples taken at screening were used to obtain the baseline data. Samples were also collected within 2 weeks of the final treatment. Three independent central pathologists examined all biopsy slides in a blinded fashion at baseline and 12 weeks. Two histological staging systems were used in this study. The Scheuer classification was used to determine if liver histology was stage III or higher to confirm advanced liver fibrosis with PBC at enrolment, whereas the Knodell scoring system and Ishak’s modified histological activity index (mHAI) were used as the histological staging system, as well as to assess fibrosis. The collagen proportionate area (CPA) was measured to determine whether the study drug had an anti-fibrotic effect.
Outcomes
The primary endpoint was the incidence of SAEs (ie, adverse drug reactions), for which a causal relationship with the investigational drug could not be ruled out. Safety was measured by analysing the frequency and severity of AEs. The secondary endpoint was the determination of OP-724 pharmacokinetics (PK) in vivo. Plasma PRI-724 and C-82 concentration-time data were analysed by non-compartmental methods and included the maximum drug concentration (Cmax), the time to Cmax (Tmax), the terminal half-life (t1/2) and the area under the curve (AUC). Other secondary endpoints were the incidence of AEs and the improvement in the mHAI score, as measured using liver biopsy at 12 weeks. Liver biopsy specimens were examined for fibrosis by staining with Masson’s trichrome, H&E and Sirius red. Staging and grading were conducted based on the mHAI score to assess treatment efficacy. The Treatment Effect Assessment Committee, which consisted of three liver pathologists, determined the final efficacy of OP-724 using liver biopsy. In addition, we assessed the change relative to baseline in liver stiffness measure (LSM) using FibroScan (Echosens, Waltham, Massachusetts, USA), Child-Pugh score (CP score) and Model for End-stage Liver Disease (MELD) score at 12 weeks as the secondary endpoint.
Statistical analyses
Sample size calculation
Here, we set the number of patients to ‘at least 7 patients to at most 12 patients’. This setting was not based on statistical evidence. Based on the fact that the number of patients with PBC in Japan is approximately 22 000, which is an extremely small number,28 and the number of patients with PBC treated at Tokyo Metropolitan Komagome Hospital, which was the medical institution at the start of this clinical trial, it was predicted that registration was possible within the clinical trial period and we decided the number of patients to be treated.
Analyses of primary and secondary endpoints
All patients were included in the analyses of OP-724 feasibility, safety and tolerability. All statistical analyses were descriptive and calculated for each treatment group. Data are expressed as the mean±SD. Clinical safety and pharmacokinetic data were included in safety analyses. There was no further allowance for missing data. In addition, values outside the permissible range of the evaluation implementation time were treated as missing values and were not included with other evaluation time data. PK analyses were conducted in patients with evaluable PK concentrations using non-compartmental methods with Microsoft Office Excel and WinNonlin V.6.1 (Pharsight, St. Louis, Missouri, USA).
We performed prespecified analyses of changes in LSM, the CP score and the MELD score from baseline to 12 weeks post-treatment. We also performed a prespecified secondary analysis of change from baseline histological scores, which focused on patients with biopsy samples from baseline and 12 weeks after OP-724 treatment. In this trial, the number of patients was small, and statistical analysis was considered meaningless and was not conducted. Seven patients were included in the analyses of OP-724 concerning its safety, tolerability and antifibrotic effect. Data are expressed as mean±SD.
Results
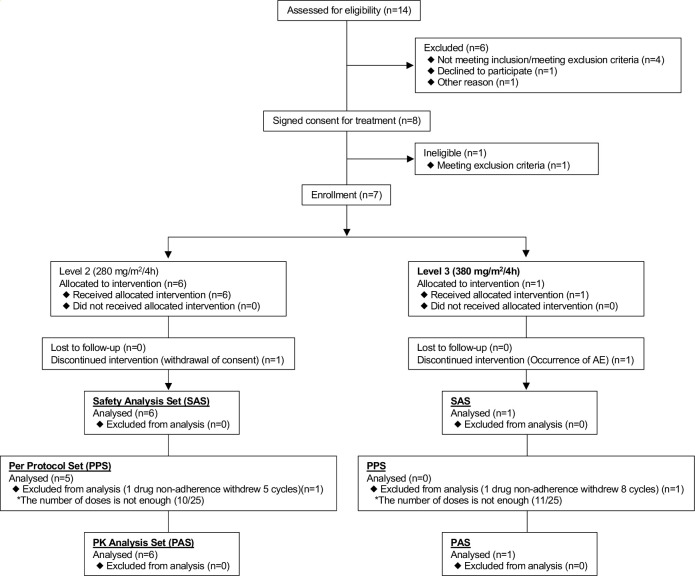
A phase 1 clinical trial was conducted to evaluate the safety and tolerability of OP-724 in patients with advanced PBC. A total of 14 patients were screened between 4 September 2019 and 21 September 2021; we followed the protocol of administering 280 mg/m2/4 hours of OP-724 to six patients and 380 mg/m2/4 hours to one patient (figure 1). Of the remaining six patients, four patients did not meet the inclusion or exclusion criteria and could not be registered. One patient declined to participate, and the others did not register for personal reasons. In addition, a patient withdrew due to a liver tumour detection in a screening test after consent was obtained.
Figure 1.
Trial profile.
Table 1 summarises the baseline patient characteristics. One patient was included in the 380 mg/m2/4 hours cohort based on the protocol followed for dosage escalation; however, one patient developed AE (grade 2 abnormal hepatic function), for which a causal relationship could not be ruled out. Consequently, the dosage level was lowered by one step, and three patients were added to the 280 mg/m2/4 hours cohort for safety evaluation.
Table 1.
Baseline characteristics
| Characteristics | 280 mg/m2/4 hours | 380 mg/m2/4 hours | All patients | ||
| (n=6) | (n=1) | (n=7) | |||
| Age (years) | 68 (52–73) | 70 | 68 (52–73) | ||
| Sex | |||||
| Female | 4 (66.7%) | 0 | 4 (57.1%) | ||
| Race | |||||
| Asian | 6 (100%) | 1 (100%) | 7 (100%) | ||
| White | 0 | 0 | 0 | ||
| Other | 0 | 0 | 0 | ||
| Treatment | |||||
| Ursodeoxycholic acid | |||||
| Use at baseline | 6 (100%) | 1 (100%) | 7 (100%) | ||
| Daily dose (mg) | |||||
| 600 | 3 (50%) | 1 (100%) | 4 (57%) | ||
| 900 | 3 (50%) | 0 | 3 (43%) | ||
| Fibrate | |||||
| Use at baseline | 2 (33%) | 0 | 2 (29%) | ||
| Laboratory data | Upper Limit of Normal | ||||
| Male | Female | ||||
| Total bilirubin (mg/dL) | 1.5 | 1.5 | 0.9 (0.5–3.9) | 0.9 | 0.9 (0.5–3.9) |
| ALT (U/L) | 42 | 23 | 30 (17–71) | 37 | 33 (17–71) |
| AST (U/L) | 30 | 30 | 40 (23–88) | 41 | 41 (23–88) |
| ALP (U/L) | 322 | 322 | 253 (139–948) | 297 | 283 (139–948) |
| γ-GTP (U/L) | 64 | 32 | 42 (13–210) | 57 | 57 (13–210) |
| Alb (g/dL) | 5.1 | 5.1 | 3.6 (2.9–4.2) | 4 | 3.6 (2.9–4.2) |
| PT (%) | 130 | 130 | 87 (55–100) | 95 | 90 (55–100) |
| PLT count (109/L) | 348 | 348 | 111 (47–181) | 89 | 104 (47–181) |
| Total cholesterol (mg/dL) | 219 | 219 | 184 (142–208) | 240 | 201 (142–240) |
| Fibrosis-related data | |||||
| Liver stiffness (kPa) | 17.0 (6.4–40.3) | 27.4 | 22.3 (6.4–40.3) | ||
| Liver histology | |||||
| Scheuer class | |||||
| III | 3 (50%) | 0 | 3 (43%) | ||
| IV | 3 (50%) | 1 (100%) | 4 (57%) | ||
| Ascites—no (%) | |||||
| None | 4 (67%) | 1 (100%) | 5 (71%) | ||
| Mild or moderate | 2 (33%) | 0 | 2 (29%) | ||
| Severe | 0 | 0 | 0 | ||
| Oesophageal varices | |||||
| None | 4 (67%) | 1 (100%) | 5 (71%) | ||
| (+) | 2 (33%) | 0 | 2 (29%) | ||
Alb, albumin; ALP, alkaline phosphatase; ALT, alanine aminotransferase; AST, aspartate aminotransferase; PLT, Platelet; PT, Prothrombin time; γ-GTP, γ-Glutamyl TransPeptidase.
Out of seven patients who received the study drug, four were women, with a median age of 68 years (range: 52–73 years). UDCA was administered as a therapeutic drug at doses of 600 mg/day in four patients (4/7 (57%)) and 900 mg/day in three patients (3/7 (43%)). On the other hand, bezafibrate was administered to two patients (2/7 (29%)). In addition, liver biopsy at baseline revealed that three and four patients were in stages III and IV, respectively, according to the Scheuer classification (table 1).
With respect to safety, no SAEs were observed; however, a causal relationship with abnormal hepatic function could not be ruled out in the 380 mg/m2/4 hours group. Therefore, the recommended dosage was determined to be 280 mg/m2/4 hours. In the 280 mg/m2/4 hours group, a slight increase in serum alanine aminotransferase (ALT) levels was observed in two (33%) out of six patients. Nonetheless, the serum ALT levels did not increase in level 2 patients, even with the continuation of investigational drug administration, showing a downward trend. In addition, the peak values of serum ALT and aspartate aminotransferase (AST) levels were 189 U/L and 128 U/L, respectively, in the level 3 patient but were 95 U/L and 82 U/L, respectively, in level 2 patients, which were less than three times the normal values. Based on these observations, the safety committee deemed this event to be transient, indicating no issue with safety and tolerability (table 2).
Table 2.
Adverse events and laboratory abnormalities
| (280 mg/m2/4 hours) | (380 mg/m2/4 hours) | |||||
| (n=6) | (n=1) | |||||
| Events | Grade 1 | Grade 2 | Grades 3–5 | Grade 1 | Grade 2 | Grades 3–5 |
| Common adverse events | ||||||
| Nasopharyngitis | 0 | 0 | 0 | 1 (100%) | 0 | 0 |
| Open angle glaucoma | 0 | 1 (17%) | 0 | 0 | 0 | 0 |
| Haemorrhage | 0 | 1 (17%) | 0 | 0 | 0 | 0 |
| Abdominal discomfort | 2 (33%) | 0 | 0 | 0 | 0 | 0 |
| Constipation | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Diarrhoea | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Nausea | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Vomiting | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Hepatic function abnormal | 1 (17%) | 1 (17%) | 0 | 0 | 1 (100%) | 0 |
| Dermatitis contact | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Dry skin | 0 | 1 (17%) | 0 | 0 | 0 | 0 |
| Back pain | 0 | 1 (17%) | 0 | 0 | 0 | 0 |
| Renal impairment | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
| Fever | 1 (17%) | 0 | 0 | 1 (100%) | 0 | 0 |
| Infusion site extravasation | 0 | 1 (17%) | 0 | 0 | 0 | 0 |
| Tooth fracture | 1 (17%) | 0 | 0 | 0 | 0 | 0 |
We measured the Cmax, AUC using the last concentration extrapolated based on constant elimination, and Tmax (table 3 and online supplemental figure 1). Plasma OP-724 concentration for a single dose reached the Cmax at 0.5–4 hours after initiating administration in all patients (online supplemental figure 1A). In addition, the Tmax at level 2 (280 mg/m2/4 hours) and level 3 (380 mg/m2/4 hours) were 1.9±1.2 hour and 1.0 hour, respectively; the Cmax was 1850 ± 510 ng/mL and 3980 ng/mL, respectively; and the AUC0–24 h was 6420±1910 ng∙h/mL and 10 200 ng∙h/mL, respectively. At level 2, the half-life was calculated for four out of six patients; the mean half-life was calculated as 0.438±0.107 hour. On the other hand, plasma C-82 concentration for a single dose reached the Cmax at 1 hour or 4 hours after initiating administration in all patients (table 3 and online supplemental figure 1B). The Tmax at level 2 (280 mg/m2/4 hours) and level 3 (380 mg/m2/4 hours) was 2.8±1.3 hour and 2 hours, respectively; the Cmax was 2020 ± 390 ng/mL and 2370 ng/mL, respectively; and the AUC0–24 h was 10 700±2400 ng∙h/mL and 12 600 ng·h/mL, respectively (table 3). There was no difference in these parameters between levels 2 and 3; however, we observed that the Cmax and AUC of C-82 increased with increasing doses. Moreover, the half-life was calculated as 3.51±0.84 hour, 3.45 hours for each level.
Table 3.
Pharmacokinetic parameters for OP-724 and C-82 after OP-724 infusion
| OP-724 | C-82 | ||||||||
| Dose | Tmax | Cmax | AUC0-24h | T1/2(h) | Tmax | Cmax | AUC0-24h | T1/2(h) | |
| (mg/m2/4 hours) | (h) | (ng/mL) | (ng・h/mL) | (h) | (ng/mL) | (ng・h/mL) | |||
| 280 | N | 6 | 6 | 6 | 4 | 6 | 6 | 6 | 6 |
| Mean | 1.9 | 1850 | 6420 | 0.438 | 2.8 | 2020 | 10 700 | 3.51 | |
| SD | 1.2 | 510 | 1910 | 0.107 | 1.3 | 390 | 2400 | 0.84 | |
| CV(%) | 63.2 | 27.6 | 29.8 | 24.4 | 46.4 | 19.3 | 22.4 | 23.9 | |
| Min | 0.5 | 1080 | 3880 | 0.336 | 1 | 1350 | 7070 | 2.45 | |
| Max | 4 | 2460 | 9210 | 0.588 | 4 | 2310 | 13 500 | 4.73 | |
| Median | 2 | 2000 | 6340 | 0.414 | 3 | 2220 | 11 200 | 3.5 | |
| 380 | N | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
| Mean | 1 | 3980 | 10 200 | 0.497 | 2 | 2370 | 12 600 | 3.45 | |
For the calculation of AUC0–24 hours, BLQ were assumed as 0 ng/mL.
AUC, area under curve; BLQ, Below the Limit of Quantitation.
bmjgast-2022-001001supp001.pdf (21.4KB, pdf)
We analysed paired liver biopsy samples obtained from five patients before (baseline) and after 12 weeks of OP-724 administration. Among the five patients with pathologically analysable samples, three (60%) showed a decrease in the CPA, three (60%) exhibited a decrease in the mHAI score, and two (40%) showed a decrease in the fibrosis stage by 1 or more (table 4). Histological evaluation of two patients (P101-01 and P101-08) with decreased CPA by liver biopsy is shown in online supplemental figure 2. In both patients, a reduction in septal thickness was observed by Masson’s trichrome staining in the liver parenchyma after OP-724 administration.
Table 4.
Modified HAI score, CPA, MELD score, CP score, liver stiffness measure and ELF score after OP-724 treatment
| Patient ID | Age | Time point | Modified HAI score | Collagen proportional area | MELD score | Child-Pugh score | FibroScan (kPa) | ELF score | |||||
| Interface hepatitis | Confluent necrosis | Lobular inflammation | Portal inflammation | HAI score | Stage | Sirius red positive area (%) | |||||||
| P101-01 | 66 | Baseline | 2 | 0 | 1 | 3 | 6 | 4 | 7.8010627 | 15 | 6 | 9.1 | 1.2 |
| 12 weeks | 2 | 0 | 1 | 3 | 6 | 3 | 2.7389579 | 15 | 7 | 8.9 | 0.9 | ||
| P101-02 | 73 | Baseline | 2 | 0 | 2 | 2 | 6 | 5 | 4.9477138 | 2 | 6 | 40.3 | 0.78 |
| 12 weeks | 1 | 0 | 1 | 1 | 3 | 5 | 3.7144629 | 2 | 6 | 33.8 | 0.24 | ||
| P101-04 | 68 | Baseline | 2 | 0 | 1 | 1 | 4 | 3 | 6.8891091 | 6 | 7 | 26.3 | 2.46 |
| 12 weeks | 3 | 1 | 2 | 3 | 9 | 5 | 7.5842215 | 8 | 7 | 23.6 | 3.16 | ||
| P101-07 | 67 | Baseline | 2 | 2 | 3 | 3 | 10 | 3 | 3.8731926 | 5 | 5 | 11.6 | −0.1 |
| 12 weeks | 2 | 0 | 2 | 2 | 6 | 3 | 3.6462028 | 5 | 5 | 9.2 | −0.07 | ||
| P101-08 | 52 | Baseline | 4 | 3 | 3 | 3 | 13 | 5 | 7.7587483 | 6 | 6 | 22.3 | 0.96 |
| 12 weeks | 1 | 0 | 3 | 2 | 6 | 2 | 3.4838244 | 6 | 6 | 36.3 | 1.48 | ||
CPA, collagen proportionate area; CP score, Child-Pugh score; ELF, The Enhanced Liver Fibrosis; HAI, Histological Activity Index; MELD, Model for End-stage Liver Disease.
We monitored liver function in serum during OP-724 administration and measured ALP, total bilirubin, GGT, total bile acid and ALT levels. Online supplemental figure 3A shows the results for these liver function-related parameters, which changed from baseline and were measured at 5, 9 and 12 weeks after administration and at 16 weeks (1 month after the end of administration). Because UDCA and bezafibrate had already been taken, the majority of patients had normal ALP and GGT levels at baseline. However, at least OP-724 administration did not show a tendency to decrease these parameters. Similar results were obtained for total bilirubin and ALT levels, but the total bile acid level alone showed a downward trend, although with no significant difference.
Finally, we also examined the changes in the CP score and MELD score as secondary endpoints to explore whether OP-724 improved liver function. We detected no changes in the mean CP score and MELD score at 12 weeks after PRI-724 administration. Similarly, to examine the antifibrotic therapeutic effect, liver stiffness was measured by FibroScan29 30 and the Enhanced Liver Fibrosis score31 was determined; no significant change was observed before and after administration, although there were some patients who improved after administration (table 4 and online supplemental table 1).
Discussion
This study was conducted on patients with advanced PBC to evaluate the feasibility, safety and pharmacokinetics of OP-724 administration and to determine the recommended dosage of OP-724 in the next phase. Although the number of patients treated in this study was as small as seven, no SAE was observed during the administration period, and no deaths related to drug administration were observed, suggesting its safety. From an exploratory study of efficacy, it was found that the fibrotic area of the liver tissue was improved in some treated patients. These results are expected to be further investigated in the future, and it is necessary to accumulate patients and examine their effectiveness in the next clinical trial.
According to the study protocol, the study was started from level 2 (280 mg/m2/4 hours) and subsequently proceeded to level 3 (380 mg/m2/4 hours) after confirming safety up to cycle 4 on day 7 in three patients. However, the first level 3 patient (P101-05) exhibited liver dysfunction. Although this event is not an SAE in a previous study25 investigating PRI-724–2101 in patients with liver cirrhosis induced by hepatitis B or C virus, one patient who received level 3 (380 mg/m2/4 hours) had severe liver dysfunction. Considering that liver dysfunction was reported as an SAE in one patient who received the drug, enrolment to level 3 was discontinued owing to the importance of the event. In this patient, serum ALT and AST levels increased more than three times the reference values; however, an increase of more than two times in the total bilirubin level was not observed. Therefore, we deemed that the requirements of Hy’s law were not satisfied. Since serum ALP and GGT levels slightly exceeded the upper limit of standard values at certain time points, we considered drug-induced liver injury, which was mainly hepatocellular, and possible bile duct injury. Neither ascites nor encephalopathy was observed. Due to the elevated ALT and AST levels, we decided to withdraw C5D4 and C6D1. Moreover, since we considered liver damage due to other suspected drugs at this point, we decided to continue administering the investigational drug. Once serum ALT and AST levels were noted to have improved, administration of the investigational drug C7D4 was started. However, ALT and AST levels increased again with C8D1 administration (online supplemental table 2).
Although this was not an SAE, abnormal hepatic function was reported as an SAE in one patient who received the drug at level 3 (380 mg/m2/4 hours) in the prior PRI-724-2101 study conducted on patients with cirrhosis due to hepatitis C or B. As such, the administration of the study drug was suspended. Following resumption, abnormal hepatic function (re-elevation of AST and ALT levels) was observed again, and the results of lymphocyte stimulation tests for other suspected drugs were negative. Hence, the relevant event was considered to be an AE, possibly indicating a causal relationship with the investigational drug (grade 2). Furthermore, due to persistent liver dysfunction, the clinical study was discontinued for the patient. In this way, patients suspected with drug-induced hepatic dysfunction other than the investigational drug could be stopped prior to resumption for a rechallenge test. In response to this, registration to level 3 was discontinued, and another three patients were added to level 2 for safety evaluation. Consequently, six patients (three of whom were additional patients after discontinuation of level 3 enrolment) were enrolled in level 2, and one patient was enrolled in level 3.
In the safety evaluation, the incidence of SAEs (ie, the primary endpoint) was 0% (0/7). The occurrence rates of AEs and side effects (ie, the secondary endpoints) were 100% (7/7) and 85.7% (6/7), respectively. With respect to AEs, the number of patients who developed ‘gastrointestinal disorder’ was the highest at 4/7 (57.1%), followed by ‘hepatobiliary system disorder’ and ‘general/systemic disorder and administration site status’ (3/7 (42.9%) each). Gastrointestinal disorders, such as nausea and vomiting, showed no clear dose-related trends, although a correlation with vomiting was suggested by PK analyses. OP-724 was thus considered to be mildly or moderately emetogenic but effectively managed with standard-of-care antiemetics and routine prophylaxis. ‘Liver dysfunction (grade 2)’ occurred in one level 3 patient, which led to the discontinuation of investigational drug administration as mentioned above.
Although there is significant interest in the therapeutic potential of targeting the Wnt pathway for cancer and fibrosis treatment, this has proven challenging due to the essential role of this pathway in stem cell maintenance and tissue homoeostasis, which raises concerns regarding significant toxicity.32–34 Wnt signalling is known to play an important role in bone homoeostasis.35 36 Several studies with Wnt inhibitor, ipafricept and vantictumab, demonstrated an increased risk for fragility fractures among treated patients.37 38 However, no fragility fractures were recorded in this study. The mean laboratory test values fluctuated during the study period, and the decrease in the total bile acid level was considered as clinically important. The number of patients from whom baseline and 12-week data were obtained was small at five; nevertheless, abnormally high values at baseline decreased at 12 weeks in four patients.
One of the limitations of this study was the small sample size, particularly after the participants were divided into different dose cohorts. Furthermore, one patient in the 380 mg/m2/4 hours had to leave the trial before completing 12 cycles of treatment owing to AEs, resulting in inadequate data to evaluate the safety and tolerability of OP-724 in the maximum dose cohort. Consequently, the analysis was exploratory in order to investigate the efficacy (antifibrotic effect) of OP-724 in PBC with fibrosis. Among the examination items, pathological evaluation by liver biopsy revealed that the CPA decreased before and after OP-724 administration in several patients (table 4 and online supplemental figure 2). Furthermore, two patients (2/5 (40%)) showed a decrease in the fibrosis stage by 1 or more, suggesting that it could potentially serve as a therapeutic drug in the future. Over recent years, antifibrosis evaluation by liver biopsy has often been replaced with FibroScan or magnetic resonance elastography owing to its invasiveness and sampling error; nevertheless, it is still considered the golden standard.29 30 39 40 LSM obtained using FibroScan is a simple and widely used method; however, limitations have been identified. In particular, it may be difficult to measure the accuracy of numerical values in cases of hepatitis or cholestasis, or areas with accumulated ascites.29 41 Recently, de Franchis et al reported a clinically significant decrease in LSM, which is associated with a substantially reduced risk of decompensation and liver-related mortality.42 This is defined as a ≥20% decrease in LSM associated with LSM<20 kPa or any decrease in LSM<10 kPa. By applying this definition to our study, 20% (1/5) was judged to be a clinically significant decrease that warrants further investigation.
Previous clinical trials24 25 reported that OP-724 caused an increase in the albumin level; in contrast, this tendency was not observed in this study (online supplemental figure 3B). Thus, although the number of treated patients was small, no significant improvement in liver function as a result of OP-724 administration was observed.
The antifibrotic effect of OP-724 mainly improves cholestasis mediated by Egr-1 signal (decreased bile acid) in hepatocytes and suppresses the infiltration of inflammatory cells such as macrophages, resulting in the suppression of hepatocyte and bile duct disorders.26 In the treated patients, the serum total bile acid concentration showed a tendency to decrease; however, no statistically significant difference was observed. Most patients in this trial were taking UDCA or bezafibrate, suggesting that OP-724 lower the bile acids via a different mechanism of action.
In conclusion, the 12-week intravenous administration of OP-724 to patients with advanced PBC was confirmed to be safe and well tolerated, although the number of patients studied was small. Here, the recommended dose was determined to be 280 mg/m2/4 hours. In the future, we plan to proceed with a next-phase study to verify the effectiveness and tolerability of OP-724 with a larger number of patients.
Acknowledgments
The authors thank all of the research and clinical staff at the Tokyo Metropolitan Komagome Hospital, especially Akemi Ikoma, Kozue Kobayashi, Maiko Nishihara, Yasuo Azuma, Noriyo Okamoto, and Naoko Horikawa, for their hard work and valuable contribution to the study. The authors also thank Editage (www.editage.jp) for English language editing.
Footnotes
Contributors: KK was the coordinating principal investigator and led the clinical conduct at the Komagome Hospital. EO was the principal investigator at the Kyushu University Hospital. MK and JI were study subinvestigators at the Komagome Hospital, whereas EO was the study subinvestigator at the Kyushu University Hospital. KK contributed to the conception of the clinical trial, acquired funding, interpreted the clinical data, and wrote the original draft of the manuscript. EO, II and AT collected, analysed and interpreted the data. MK and EO reviewed and edited the manuscript. MK and JI investigated and interpreted the clinical data. KH, MS and YI analysed and interpreted the histological data. HY, KaM and KoM interpreted the clinical data and organised the safety of the study. II contributed to the pharmacokinetic analysis. All authors have read and approved the final version of the manuscript. KK was guarantor of this study.
Funding: This investigator-initiated study was supported by the Japan Agency for Medical Research and Development (AMED) (to K.K.; JP20ek0109457 and JP21ek0109457).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Consent obtained from next of kin.
Ethics approval
This study was approved by the Institutional Review Board of Komagome Hospital (approval number: 19-006). Participants gave informed consent to participate in the study before taking part.
References
- 1.Lleo A, Wang G-Q, Gershwin ME, et al. Primary biliary cholangitis. Lancet 2020;396:1915–26. 10.1016/S0140-6736(20)31607-X [DOI] [PubMed] [Google Scholar]
- 2.Lv T, Chen S, Li M, et al. Regional variation and temporal trend of primary biliary cholangitis epidemiology: a systematic review and meta-analysis. J Gastroenterol Hepatol 2021;36:1423–34. 10.1111/jgh.15329 [DOI] [PubMed] [Google Scholar]
- 3.Corpechot C, Poupon R, Chazouillères O. New treatments/targets for primary biliary cholangitis. JHEP Rep 2019;1:203–13. 10.1016/j.jhepr.2019.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Trivedi PJ, Hirschfield GM. Recent advances in clinical practice: epidemiology of autoimmune liver diseases. Gut 2021;70:1989–2003. 10.1136/gutjnl-2020-322362 [DOI] [PubMed] [Google Scholar]
- 5.Lindor KD, Bowlus CL, Boyer J, et al. Primary biliary cholangitis: 2021 practice guidance update from the American association for the study of liver diseases. Hepatology 2022;75:1012–3. 10.1002/hep.32117 [DOI] [PubMed] [Google Scholar]
- 6.Hirschfield GM, Chazouillères O, Cortez-Pinto H, et al. A consensus integrated care pathway for patients with primary biliary cholangitis: a guideline-based approach to clinical care of patients. Expert Rev Gastroenterol Hepatol 2021;15:929–39. 10.1080/17474124.2021.1945919 [DOI] [PubMed] [Google Scholar]
- 7.Hirschfield GM, Dyson JK, Alexander GJM, et al. The British Society of Gastroenterology/UK-PBC primary biliary cholangitis treatment and management guidelines. Gut 2018;67:1568–94. 10.1136/gutjnl-2017-315259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Harms MH, van Buuren HR, Corpechot C, et al. Ursodeoxycholic acid therapy and liver transplant-free survival in patients with primary biliary cholangitis. J Hepatol 2019;71:357–65. 10.1016/j.jhep.2019.04.001 [DOI] [PubMed] [Google Scholar]
- 9.Nevens F, Andreone P, Mazzella G, et al. A placebo-controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med 2016;375:631–43. 10.1056/NEJMoa1509840 [DOI] [PubMed] [Google Scholar]
- 10.Kowdley KV, Luketic V, Chapman R, et al. A randomized trial of obeticholic acid monotherapy in patients with primary biliary cholangitis. Hepatology 2018;67:1890–902. 10.1002/hep.29569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mayo MJ. Mechanisms and molecules: what are the treatment targets for primary biliary cholangitis? Hepatology 2022;76:518–31. 10.1002/hep.32405 [DOI] [PubMed] [Google Scholar]
- 12.Corpechot C, Chazouillères O, Rousseau A, et al. A placebo-controlled trial of bezafibrate in primary biliary cholangitis. N Engl J Med 2018;378:2171–81. 10.1056/NEJMoa1714519 [DOI] [PubMed] [Google Scholar]
- 13.Tanaka A, Hirohara J, Nakano T, et al. Association of bezafibrate with transplant-free survival in patients with primary biliary cholangitis. J Hepatol 2021;75:565–71. 10.1016/j.jhep.2021.04.010 [DOI] [PubMed] [Google Scholar]
- 14.Trauner M, Fuchs CD. Novel therapeutic targets for cholestatic and fatty liver disease. Gut 2022;71:194–209. 10.1136/gutjnl-2021-324305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Trauner M, Fuchs CD, Halilbasic E, et al. New therapeutic concepts in bile acid transport and signaling for management of cholestasis. Hepatology 2017;65:1393–404. 10.1002/hep.28991 [DOI] [PubMed] [Google Scholar]
- 16.Thompson MD, Monga SPS. Wnt/Beta-Catenin signaling in liver health and disease. Hepatology 2007;45:1298–305. 10.1002/hep.21651 [DOI] [PubMed] [Google Scholar]
- 17.Russell JO, Monga SP. Wnt/β-Catenin Signaling in Liver Development, Homeostasis, and Pathobiology. Annu Rev Pathol 2018;13:351–78. 10.1146/annurev-pathol-020117-044010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Distler JHW, Györfi A-H, Ramanujam M, et al. Shared and distinct mechanisms of fibrosis. Nat Rev Rheumatol 2019;15:705–30. 10.1038/s41584-019-0322-7 [DOI] [PubMed] [Google Scholar]
- 19.Vannella KM, Wynn TA. Mechanisms of organ injury and repair by macrophages. Annu Rev Physiol 2017;79:593–617. 10.1146/annurev-physiol-022516-034356 [DOI] [PubMed] [Google Scholar]
- 20.Kahn M. Can we safely target the Wnt pathway? Nat Rev Drug Discov 2014;13:513–32. 10.1038/nrd4233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yu J, de Belle I, Liang H, et al. Coactivating factors p300 and CBP are transcriptionally crossregulated by EGR1 in prostate cells, leading to divergent responses. Mol Cell 2004;15:83–94. 10.1016/j.molcel.2004.06.030 [DOI] [PubMed] [Google Scholar]
- 22.Osawa Y, Oboki K, Imamura J, et al. Inhibition of Cyclic Adenosine Monophosphate (cAMP)-response Element-binding Protein (CREB)-binding Protein (CBP)/β-Catenin Reduces Liver Fibrosis in Mice. EBioMedicine 2015;2:1751–8. 10.1016/j.ebiom.2015.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kahn M. Symmetric division versus asymmetric division: a tale of two coactivators. Future Med Chem 2011;3:1745–63. 10.4155/fmc.11.126 [DOI] [PubMed] [Google Scholar]
- 24.Kimura K, Ikoma A, Shibakawa M, et al. Safety, tolerability, and preliminary efficacy of the anti-fibrotic small molecule PRI-724, a CBP/β-Catenin inhibitor, in patients with hepatitis C virus-related cirrhosis: a single-center, open-label, dose escalation phase 1 trial. EBioMedicine 2017;23:79–87. 10.1016/j.ebiom.2017.08.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kimura K, Kanto T, Shimoda S, et al. Safety, tolerability, and anti-fibrotic efficacy of the CBP/β-catenin inhibitor PRI-724 in patients with hepatitis C and B virus-induced liver cirrhosis: an investigator-initiated, open-label, non-randomised, multicentre, phase 1/2A study. EBioMedicine 2022;80:104069. 10.1016/j.ebiom.2022.104069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kimura M, Nishikawa K, Osawa Y, et al. Inhibition of CBP/β-catenin signaling ameliorated fibrosis in cholestatic liver disease. Hepatol Commun 2022;6:2732–47. 10.1002/hep4.2043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindor KD, Bowlus CL, Boyer J, et al. Primary biliary cholangitis: 2018 practice guidance from the American association for the study of liver diseases. Hepatology 2019;69:394–419. 10.1002/hep.30145 [DOI] [PubMed] [Google Scholar]
- 28.Tanaka A, Mori M, Matsumoto K, et al. Increase trend in the prevalence and male-to-female ratio of primary biliary cholangitis, autoimmune hepatitis, and primary sclerosing cholangitis in Japan. Hepatol Res 2019;49:881–9. 10.1111/hepr.13342 [DOI] [PubMed] [Google Scholar]
- 29.Castera L, Forns X, Alberti A. Non-Invasive evaluation of liver fibrosis using transient elastography. J Hepatol 2008;48:835–47. 10.1016/j.jhep.2008.02.008 [DOI] [PubMed] [Google Scholar]
- 30.Papatheodoridi M, Hiriart JB, Lupsor-Platon M, et al. Refining the Baveno VI elastography criteria for the definition of compensated advanced chronic liver disease. J Hepatol 2021;74:1109–16. 10.1016/j.jhep.2020.11.050 [DOI] [PubMed] [Google Scholar]
- 31.Lichtinghagen R, Pietsch D, Bantel H, et al. The enhanced liver fibrosis (ELF) score: normal values, influence factors and proposed cut-off values. J Hepatol 2013;59:236–42. 10.1016/j.jhep.2013.03.016 [DOI] [PubMed] [Google Scholar]
- 32.Nusse R, Clevers H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell 2017;169:985–99. 10.1016/j.cell.2017.05.016 [DOI] [PubMed] [Google Scholar]
- 33.Clevers H, Loh KM, Nusse R. Stem cell signaling. an integral program for tissue renewal and regeneration: Wnt signaling and stem cell control. Science 2014;346:1248012. 10.1126/science.1248012 [DOI] [PubMed] [Google Scholar]
- 34.Barker N, Clevers H. Mining the Wnt pathway for cancer therapeutics. Nat Rev Drug Discov 2006;5:997–1014. 10.1038/nrd2154 [DOI] [PubMed] [Google Scholar]
- 35.Rachner TD, Khosla S, Hofbauer LC. Osteoporosis: now and the future. Lancet 2011;377:1276–87. 10.1016/S0140-6736(10)62349-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wagner ER, Zhu G, Zhang B-Q, et al. The therapeutic potential of the Wnt signaling pathway in bone disorders. Curr Mol Pharmacol 2011;4:14–25. 10.2174/1874467211104010014 [DOI] [PubMed] [Google Scholar]
- 37.Jimeno A, Gordon M, Chugh R, et al. A first-in-human phase I study of the anticancer stem cell agent Ipafricept (OMP-54F28), a decoy receptor for Wnt ligands, in patients with advanced solid tumors. Clin Cancer Res 2017;23:7490–7. 10.1158/1078-0432.CCR-17-2157 [DOI] [PubMed] [Google Scholar]
- 38.Davis SL, Cardin DB, Shahda S, et al. A phase 1B dose escalation study of Wnt pathway inhibitor vantictumab in combination with nab-paclitaxel and gemcitabine in patients with previously untreated metastatic pancreatic cancer. Invest New Drugs 2020;38:821–30. 10.1007/s10637-019-00824-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ginès P, Krag A, Abraldes JG, et al. Liver cirrhosis. Lancet 2021;398:1359–76. 10.1016/S0140-6736(21)01374-X [DOI] [PubMed] [Google Scholar]
- 40.Gulamhusein AF, Hirschfield GM. Primary biliary cholangitis: pathogenesis and therapeutic opportunities. Nat Rev Gastroenterol Hepatol 2020;17:93–110. 10.1038/s41575-019-0226-7 [DOI] [PubMed] [Google Scholar]
- 41.Baranova A, Lal P, Birerdinc A, et al. Non-Invasive markers for hepatic fibrosis. BMC Gastroenterol 2011;11:91. 10.1186/1471-230X-11-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.de Franchis R, Bosch J, Garcia-Tsao G, et al. Baveno VII - Renewing consensus in portal hypertension. J Hepatol 2022;76:959–74. 10.1016/j.jhep.2021.12.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgast-2022-001001supp001.pdf (21.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.