Abstract
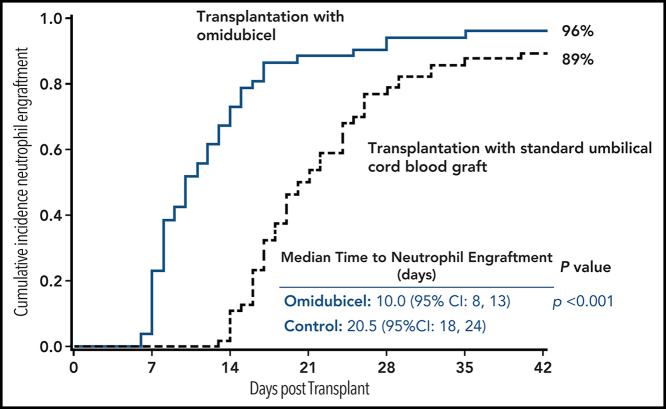
Omidubicel is an ex vivo expanded hematopoietic progenitor cell and nonexpanded myeloid and lymphoid cell product derived from a single umbilical cord blood unit. We report results of a phase 3 trial to evaluate the efficacy of omidubicel compared with standard umbilical cord blood transplantation (UCBT). Between January 2017 and January 2020, 125 patients age 13 to 65 years with hematologic malignancies were randomly assigned to omidubicel vs standard UCBT. Patients received myeloablative conditioning and prophylaxis with a calcineurin inhibitor and mycophenolate mofetil for graft-versus-host disease (GVHD). The primary end point was time to neutrophil engraftment. The treatment arms were well balanced and racially diverse. Median time to neutrophil engraftment was 12 days (95% confidence interval [CI], 10-14 days) for the omidubicel arm and 22 days (95% CI, 19-25 days) for the control arm (P < .001). The cumulative incidence of neutrophil engraftment was 96% for patients receiving omidubicel and 89% for patients receiving control transplants. The omidubicel arm had faster platelet recovery (55% vs 35% recovery by 42 days; P = .028), had a lower incidence of first grade 2 to 3 bacterial or invasive fungal infection (37% vs 57%; P = .027), and spent more time out of hospital during the first 100 days after transplant (median, 61 vs 48 days; P = .005) than controls. Differences in GVHD and survival between the 2 arms were not statistically significant. Transplantation with omidubicel results in faster hematopoietic recovery and reduces early transplant-related complications compared with standard UCBT. The results suggest that omidubicel may be considered as a new standard of care for adult patients eligible for UCBT. The trial was registered at www.clinicaltrials.gov as #NCT02730299.
Key Points
-
•
Transplantation with omidubicel provides faster neutrophil and platelet recovery compared with a standard umbilical cord blood graft.
-
•
Transplantation with omidubicel results in fewer early bacterial and viral infections and less time in hospital.
Introduction
For more than 30 years, umbilical cord blood (UCB) has been an important source of hematopoietic stem cells (HSCs) for use in allogeneic hematopoietic stem cell transplantation (allo-HSCT). It is a particularly critical stem cell source for non-White patients who are underrepresented in the international adult donor registries.1 Compared with transplants from adult donors, adult umbilical cord blood transplantation (UCBT) has been associated with increased early treatment-related morbidity and mortality stemming from delayed hematopoietic recovery and immunologic reconstitution. The advent of dual UCB grafts, refinement of pretransplant conditioning regimens, and improved supportive care have addressed many of the limitations of adult UCBT. However, delayed hematopoietic recovery remains a problem, resulting in increased use of resources.2, 3 Early-phase studies have demonstrated that ex vivo expansion of UCB stem cells before transplantation has the potential to address this critical shortcoming. By expanding both hematopoietic stem and progenitor cells, the time to neutrophil recovery after myeloablative conditioning can be even more rapid than the time after a mobilized peripheral blood stem cell (PBSC) graft.4, 5, 6, 7
Omidubicel (Gamida Cell, Jerusalem, Israel) is a patient-specific cell product derived from a single banked UCB unit. It consists of an ex vivo expanded CD133+ fraction and a nonexpanded CD133– fraction. Nicotinamide, the active agent in the culture system, inhibits differentiation and enhances functionality of cultured hematopoietic stem and progenitor cells. Preclinical studies demonstrated that when UCB-derived hematopoietic progenitor cells are cultured in the presence of nicotinamide and stimulatory hematopoietic cytokines, there is an outgrowth of phenotypically primitive CD34+CD38– cells and a substantial increase in bone marrow (BM) homing and engraftment potential.8 The ability of nicotinamide to expand both committed and long-term repopulating HSCs was confirmed in early-phase studies of omidubicel.6, 9 In this study, we compared the outcomes of a myeloablative allo-HSCT using omidubicel with standard UCB grafts.
Methods
Trial design and oversight
The trial was designed by the sponsor (Gamida Cell) in collaboration with a protocol steering committee. Enrollment began in January 2017 and was completed in January 2020. Random assignments were performed at the Emmes Company in a 1:1 ratio using minimization factors of age, center, disease risk index, and intention to use 1- or 2-unit UCB grafts if patients were randomly assigned to the control arm. As sites enrolled participants, they were randomly assigned using the centralized data entry system at Emmes Company. The primary end point was time to neutrophil engraftment. Secondary end points were platelet engraftment by 42 days, incidence of grade 2 to 3 bacterial or invasive fungal infection during the first 100 days, and days alive and out of the hospital for the first 100 days after transplantation. Additional planned end points included assessment of safety, nonrelapse mortality (NRM), relapse, overall survival (OS) and disease-free survival (DFS), acute graft-versus-host disease (aGVHD) and chronic GVHD (cGVHD), engraftment, and infectious complications. The trial was approved by the Institutional Review Boards of all participating institutions and the national regulatory authorities. All patients provided written informed consent. The study was performed in accordance with the International Conference on Harmonization, in agreement with local regulations and with the principals of Declaration of Helsinki.
Patients
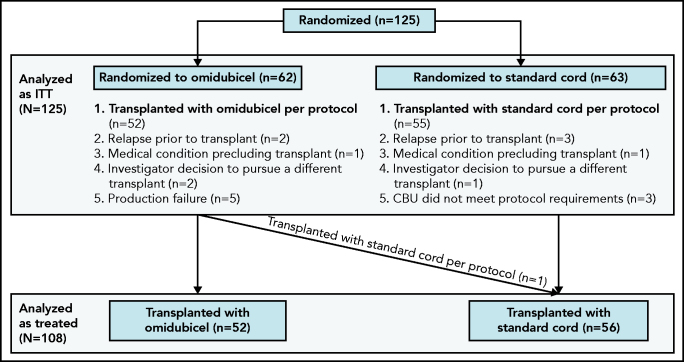
Eligible patients were age 12 to 65 years with high-risk hematologic malignancies, were candidates for myeloablative allo-HSCT, and had no readily available matched sibling or matched unrelated adult donor. Patients with marked or 3+ BM fibrosis or chronic lymphocytic leukemia were excluded. Patients were required to have an available UCB unit HLA-matched at 4 or more loci (HLA-A, B at the antigen-level, and DRB1 at the allele level) with a total nucleated cell (TNC) count ≥1.8 × 109, a TNC dose of ≥1.5 × 107 cells per kg, and CD34+ cell count of ≥8 × 106. This unit was designated for use before random assignments were made and was required to be used in both arms of the study. For patients randomly assigned to the control arm, a double cord blood graft was mandated when the omidubicel-designated unit (designated before random assignment and required to be used) was HLA-matched at 5 to 6/6 and contained <2.5 × 107 TNCs per kg or <1.2 × 105 CD34+ cells per kg, or were HLA 4/6 matched and contained <3.5 × 107 TNCs per kg or <1.7 × 105 CD34+ cells per kg. Patients were also required to have available backup cord blood unit(s). The presence of donor-specific antibodies to HLA-A, -B, -C, or DRB1 antigens (mean florescence intensity >3000) was not permitted. A detailed list of inclusion and exclusion criteria are provided in the protocol document (supplemental Material, available at the Blood Web site). Planned enrollment was 120 patients. In all, 125 patients were randomly assigned at 33 sites in North and South America, Europe, and Singapore. Participating centers and principal investigators are listed in supplemental Table 1. The population of 125 randomly assigned patients was analyzed as the intent-to-treat population (ITT), using the randomized treatment assignment. Of the 125 randomly assigned patients, 117 received an omidubicel or UCB transplant by day 90 after random assignment. This was the population that received transplants, which was also analyzed by treatment assignment. The as-treated population included 108 patients analyzed according to treatment received (Figure 1).
Figure 1.
CONSORT diagram. Randomization and treatment of patients. CBU, cord blood unit.
Graft production
The omidubicel-designated unit was transported from the cord blood bank to a Current Good Manufacturing Practice–compliant cell-processing facility (Lonza, Walkersville, MD, or Gamida Cell, Jerusalem, Israel). Omidubicel was manufactured as previously described.6 Briefly, the unit underwent immunomagnetic bead selection for CD133+ cells. The CD133–, T-cell–containing flow-through fraction was retained and recryopreserved. The CD133+ fraction was cultured in the presence of Flt-3 ligand, stem cell factor, thrombopoietin, interleukin-6, and nicotinamide for 21 ± 2 days and then cryopreserved. Both fractions were transported together to the transplantation center.
Treatment
Three alternative myeloablative conditioning regimens were permitted for study participants: 2 contained total body irradiation and 1 contained chemotherapy only (Table 1). GVHD prophylaxis was provided by a calcineurin inhibitor (tacrolimus with target trough levels of 5-15 ng/mL or cyclosporine with target trough levels of 200-400 ng/mL) and mycophenolate mofetil 15 mg/kg 3 times per day (maximum daily dose, 3 g) starting 3 days before transplantation. Mycophenolate mofetil was continued for a minimum of 60 days and the calcineurin inhibitor for minimum of 100 days after transplantation in the absence of toxicity or relapse.
Table 1.
Patient characteristics
| Characteristic | Treatment group | |
|---|---|---|
| Omidubicel | Standard UCB | |
| Total no. of patients randomly assigned | 62 (100) | 63 (100) |
| Sex | ||
| Female | 30 (48) | 23 (36) |
| Male | 32 (52) | 40 (64) |
| Age, y | ||
| Median (range) | 40 (13-62) | 43 (13-65) |
| 12-17 | 8 (13) | 6 (10) |
| 18-39 | 23 (37) | 23 (36) |
| 40-59 | 27 (44) | 31 (49) |
| 60-65 | 4 (6) | 3 (5) |
| Median weight, kg (range) | 78.6 (43-134) | 77.4 (46-133) |
| Race | ||
| White | 35 (57) | 37 (59) |
| Black | 11 (18) | 9 (14) |
| Asian | 7 (11) | 10 (16) |
| Hispanic or Latino | 10 (16) | 6 (10) |
| Other/unknown | 9 (14) | 7 (11) |
| Primary diagnosis | ||
| Acute myeloid leukemia | 27 (43) | 33 (52) |
| CR1 (morphologic) | 18 | 22 |
| CR2 | 9 | 11 |
| Acute lymphoblastic leukemia | 20 (32) | 21 (34) |
| High-risk CR1 (morphologic) | 13 | 11 |
| CR2 (morphologic) | 6 | 10 |
| CR3+ (morphologic) | 1 | 0 |
| Myelodysplastic syndrome | 6 (10) | 3 (5) |
| High | 2 | 0 |
| Intermediate-1 | 3 | 1 |
| Intermediate-2 | 1 | 2 |
| Chronic myeloid leukemia | 4 (7) | 2 (3) |
| Lymphoma | 3 (5) | 2 (3) |
| Hodgkin lymphoma, stable disease | 0 | 1 |
| T-cell non-Hodgkin lymphoma | 3 | 1 |
| Other rare disease | 2 (3) | 2 (3) |
| Adult T-cell leukemia/ lymphoma CR1 | 1 | 0 |
| Biphenotypic leukemia | 0 | 1 |
| Dendritic cell leukemia | 1 | 1 |
| Disease risk group | ||
| Low | 15 (24) | 15 (23) |
| Moderate | 27 (44) | 25 (40) |
| High/very high | 20 (32) | 23 (37) |
| HSCT-specific comorbidity index | ||
| 0 | 12 (19) | 13 (20) |
| 1-2 | 19 (31) | 18 (29) |
| 3+ | 31 (50) | 32 (51) |
| Intended UCB transplant | ||
| Single | 20 (32) | 21 (33) |
| Double | 42 (68) | 42 (67) |
| Antigen-level HLA match score (intended treatment CBU #1) | ||
| 4/6 | 46 (74) | 46 (73) |
| 5/6 | 15 (24) | 16 (25) |
| 6/6 | 1 (2) | 1 (2) |
| Antigen-level HLA match score (intended treatment CBU #2) | ||
| 4/6 | 31 (49) | |
| 5/6 | 10 (16) | |
| 6/6 | 1 (2) | |
| Conditioning regimens | ||
| TBI 1350 cGy, fludarabine 160 mg/m2, thiotepa 10 mg/kg | 7 (11) | 9 (15) |
| TBI 1320 cGy, fludarabine 75 mg/m2, cyclophosphamide 120 mg/kg | 24 (39) | 21 (33) |
| Thiotepa 10 mg/kg, busulfan 12.8 mg/kg, fludarabine 150 mg/m2 | 27 (44) | 28 (44) |
| Did not receive a transplant or off-protocol regimen | 4 (6) | 5 (8) |
All data are n (%), unless otherwise stated.
CR1, first complete response; TBI, total body irradiation.
Supportive care
Granulocyte-colony stimulating factor (5 µg/kg of recipient body weight) was given once per day starting on day +1 after transplantation until the absolute neutrophil count exceeded 1000 cells per µL. Antiviral and antifungal prophylaxis were administered at the discretion of the transplantation center. Antibacterial prophylaxis after transplantation was required by protocol. The agent used was at the discretion of the transplant center.
Laboratory and clinical assessments
Donor chimerism was performed by the local transplant center on whole blood, CD15+ myeloid, and CD3+ T cells using quantitative analysis of informative microsatellite DNA sequences. Quantitative assessment of CD3, CD4, CD8, natural killer (NK) and B-cell recovery was performed on a subset of patients by the transplant center (or designated referral laboratory) at 1, 2, 3, 6, and 12 months after transplantation. The time to engraftment of neutrophils ≥500 cells per µL and platelets >20 000/µL was defined according to Center for International Blood and Marrow Transplant Research (CIBMTR) standards, requiring donor chimerism for neutrophil engraftment. Grading of bacterial and invasive fungal infections was adapted from definitions in the Blood and Marrow Transplant Clinical Trials Network technical manual of procedures (supplemental Table 2).
Statistical considerations
The main comparisons of the primary and secondary end points as well as mortality end points were conducted using ITT analysis. Cox proportional hazards models were used in the analysis of DFS and OS, with randomly assigned treatment and disease risk as covariates in the model. The incidence of engraftment and engraftment kinetics were also calculated in the as-treated population. GVHD was assessed in the population that received a transplant and was defined as all patients randomly assigned to receive a UCBT, grouped by the treatment to which they were allocated. GVHD-free relapse-free survival (RFS) was evaluated in the as-treated population, grouped by treatment received. The primary end point (time to neutrophil engraftment) was compared between treatment groups using a Mann-Whitney–based statistic. A value of 43 days was assigned for patients who had received a transplant who did not engraft by 42 days after transplantation or patients who did not receive a transplant. P values for this and other protocol-specified ITT analyses were calculated using the rerandomization distribution.10 Sample size was chosen to provide at least 90% power for the primary end point analysis, based on information on engraftment times derived from the phase 2 study and the CIBMTR database.
Secondary end points of proportion of patients with grade 2 to 3 bacterial or invasive fungal infections up to 100 days posttransplant and proportion with platelet engraftment by 42 days were compared using cumulative incidence rates. Time out of hospital in the first 100 days was compared using the Mann-Whitney statistic. Differences in cumulative incidence were also analyzed for NRM and for relapse. For non-ITT analyses, neutrophil engraftment was compared using the Wilcoxon rank sum test or Fisher's exact test, and time to platelet engraftment was compared using Gray's test. GVHD for patients who received transplants was compared using a z test on the cumulative incidence difference. Infection densities were compared using the generalized estimating equation (GEE) approach for a linear model with 2 periods (0-30 and 31-365 days posttransplant) and a negative binomial link. The associations of CD34+ total cells and CD34+ dose with time to engraftment were evaluated using linear regression and correlation analyses of the log-transformed values. Immune reconstitution analyses were evaluated using Wilcoxon rank sum tests. P values for the multivariable models and non-ITT analyses were calculated using asymptotic methods. Confidence intervals (CIs) were calculated using bootstrap methods; the multivariable models and GEE models used asymptotic CIs. The multivariable Cox models, the GEE models, CD34+ associations with neutrophil engraftment, Gray's test for platelet engraftment, GVHD-free RFS, and moderate-to-severe cGVHD analyses were post hoc analyses. The end points were evaluated after all evaluable patients completed 6 months of follow-up after transplantation; study follow-up is ongoing.
Results
Patient and stem cell transplant characteristics
Demographics and baseline characteristics were well-balanced across the 2 arms (Table 1). In all, 125 patients (median age, 41 years; range, 13-65 years) were randomly assigned to receive omidubicel (n = 62) or standard single (33%) or double (67%) UCB grafts (n = 63). Ten patients randomly assigned to the omidubicel arm did not receive omidubicel per protocol. Eight patients randomly assigned to the standard UCB arm did not receive a transplant per protocol (Figure 1). Most patients had acute myeloid leukemia (48%) or acute lymphoblastic leukemia (33%). The disease risk index was moderate in 42% and high in 34% of patients. The study population was diverse with 16% Black, 14% Asian, 3% multiracial, and 13% Hispanic or Latino patients. Patients treated with omidubicel received a transplant at a median of 41 days after random assignment compared with 26 days for patients treated with standard UCBT.
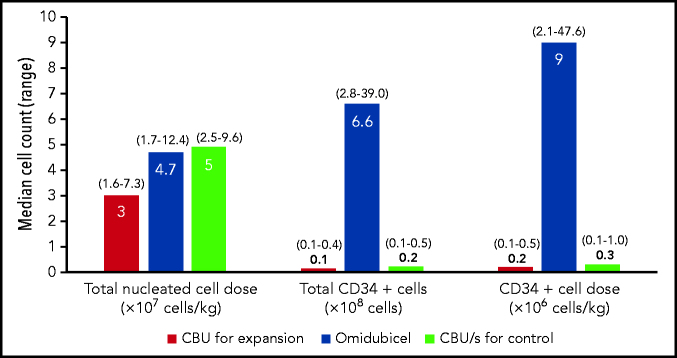
Graft characteristics
Characteristics of the standard single and double cord blood grafts and the omidubicel grafts are shown in Figure 2. The median total CD34+ cell content of the control cord blood unit(s) and the omidubicel unit before expansion (as reported by the cord blood bank before cryopreservation) was 0.23 × 108 cells (range, 0.11 × 108 to 0.55 × 108 cells) and 0.14 × 108 cells (range, 0.09 × 108 to 0.4 × 108 cells), respectively. After expansion, the content of the omidubicel unit increased to a median 6.6 × 108 CD34+ cells (range, 2.8 × 108 to 39 × 108 cells). Median CD34+ cell expansion was 130-fold (range, 32- to 233-fold). The median CD34+ cell dose of omidubicel and control grafts was 9.0 × 106 cells per kg (range, 2.1 × 106 to 47.6 × 106 cells per kg) and 0.3 × 106 cells per kg (range, 0.1 × 106 to 1 × 106 cells per kg), respectively. The CD3+ T cells in the omidubicel graft were contained solely in the unexpanded CD133– fraction.
Figure 2.
Omidubicel and control cord blood graft characteristics. Median (range) for TNC content, CD34+ cell content, and CD34+ cell doses before and after ex vivo expansion of the UCB unit. Pre-expansion values represent cell content as reported by the cord blood bank before cryopreservation of the UCB unit. AT, as treated population.
The median CD3+ content of the omidubicel grafts before cryopreservation was 210 × 106 CD3+ cells (range, 71 × 106 to 640 × 106 cells), and 3 × 106 CD3+ cells per kg (range, 1.1 × 106 to 12.4 × 106 CD3+ cells per kg). This compared with a median 412.9 × 106 CD3+ cells (range, 4.4 × 106 to 989.8 × 106 CD3+ cells), and 4.6 × 106 CD3+ cells per kg (range, 0 × 106 to 14.8 × 106 CD3+ cells per kg) for the control grafts. CD3 content was enumerated after thawing and before infusion from a subset of 25 control patients. Thus, the observed difference in CD3 content is underestimated because of additional cell loss after thawing the omidubicel product.
Hematopoietic recovery
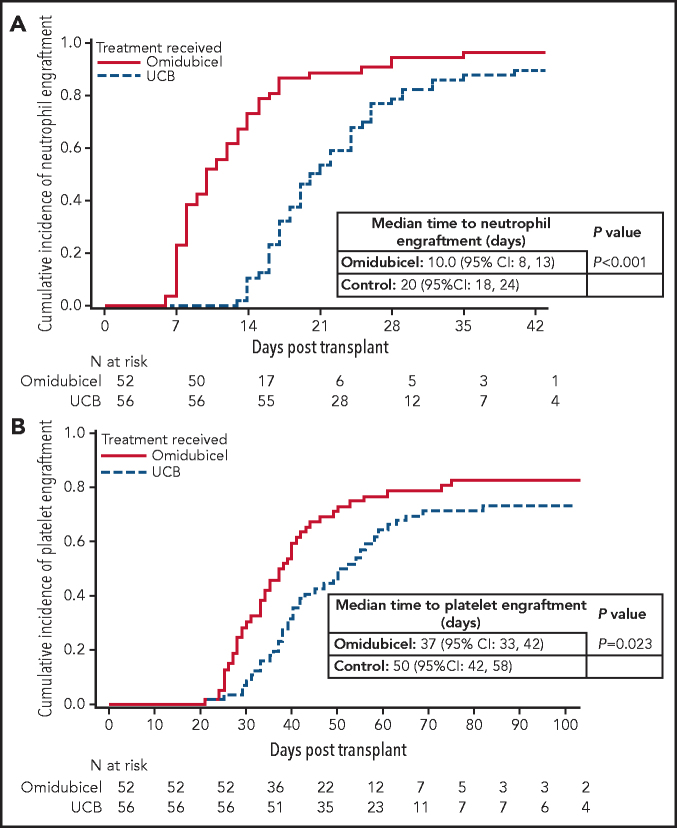
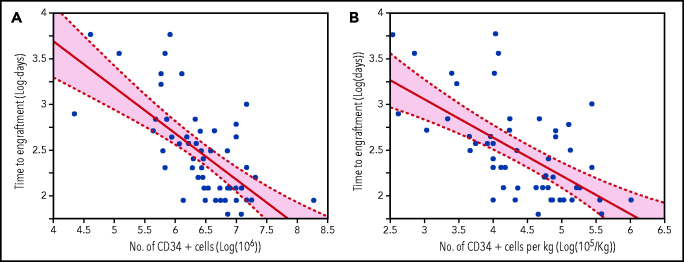
The median time to neutrophil recovery per ITT analysis was 12 days (95% CI, 10-14 days) for those randomly assigned to omidubicel and 22 days (95% CI, 19-25 days) for controls (P < .001) (Table 2). The cumulative incidence of neutrophil engraftment by day 42 after transplantation for patients receiving omidubicel (as-treated population, n = 52) was 96% at a median of 10 days (95% CI, 8-13 days) compared with 89% at a median of 20 days (95% CI, 18-24 days) for the controls (n = 56) (P < .001) (Figure 3A). For patients who received a transplant with omidubicel, higher total CD34+ cell counts and CD34+ cell doses (per weight) were associated with shorter times to neutrophil engraftment (Figure 4, correlations: total cells, r = –0.66; P < .001; cell dose, r = –0.62; P < .001).
Table 2.
Time to neutrophil engraftment
| Randomly assigned treatment group | No. | Cumulative incidence | Mann-Whitney P | |
|---|---|---|---|---|
| Median time to neutrophil engraftment (d)* | 95% CI | |||
| Omidubicel | 62 | 12.0 | 10.0-14.0 | <.001 |
| Control | 63 | 22.0 | 19.0-25.0 | |
Patients who did not receive a transplant or who did not engraft on or before day 42 after transplantation were assigned to day 43.
Figure 3.
Hematopoietic recovery. Analysis was performed in the as-treated population (n = 108). Cumulative incidence of neutrophil engraftment by day 42 (A) and platelet recovery by day 100 (B) among recipients of omidubicel or unmanipulated UCB.
Figure 4.
Correlation of CD34+ cell content with neutrophil engraftment. Correlation of CD34+ total cell count and cell dose with time to neutrophil engraftment. (A) Regression of the time to engraftment on the total number of CD34+ cells (both on the natural logarithmic scale). The shaded interval is the pointwise 95% CI around the predicted log time. The regression line is log days to engraftment (5.70-0.50 log [106 total cells]). (B) Regression of the time to engraftment on the number of CD34+ cells per patient actual body weight (both on the natural logarithmic scale). The shaded interval is the pointwise 95% CI around the predicted log time. The regression line is log days to engraftment (4.30-0.42 log [105 cells per kg]).
The cumulative incidence of platelet engraftment by day 42 after transplantation for patients randomly assigned to omidubicel was 55% vs 35% for controls (P = .028) (Table 3). For the patients transplanted with omidubicel, the cumulative incidence of platelet engraftment by day 100 after transplantation was 83% at a median of 37 days (95% CI, 33-42 days) vs 73% at a median of 50 days (95% CI, 42-58 days) for the controls (P = .023) (Figure 3B).
Table 3.
Platelet engraftment by day 42
| Randomly assigned treatment group | No. | Cumulative incidence | 95% CI | P | |
|---|---|---|---|---|---|
| Day 42 | Difference | ||||
| Omidubicel | 62 | 0.55 | 0.20 | 0.03-0.35 | .028 |
| Control | 63 | 0.35 | |||
Full donor chimerism (defined as >90% in the whole blood fraction) was observed at day +30 and day +100 after transplantation in all but 2 omidubicel recipients; one experienced early relapse and the other experienced primary graft failure. Six standard UCBT recipients experienced graft failure on day +42. The remaining evaluable standard UCBT recipients had full donor chimerism at day +30 and day +100 after transplantation.
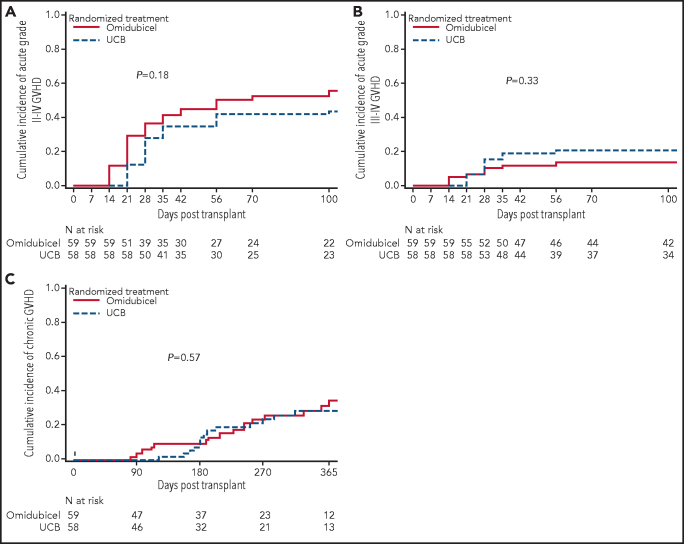
GVHD
Among the patients who received a transplant who were randomly assigned to omidubicel (n = 59) or standard cord blood (n = 58), the incidence of grade 2 to 4 aGVHD at day 100 was similar at 56% vs 43% (13% difference: 95% CI, −6% to 30%; P = .18), respectively (Figure 5A). Grade 3 to 4 aGVHD at day 100 was also similar in the omidubicel and control arms at 14% vs 21% (–7% difference; 95% CI, −21% to 7%; P = .33) (Figure 5B). The cumulative incidence of all cGVHD at 1 year was 35% for the omidubicel arm and 29% for the controls (6% difference; 95% CI, −14% to 25%; P = .57) (Figure 5C). The 1-year cumulative incidence of moderate-to-severe cGVHD was 27% for the omidubicel arm and 21% for the controls (6% difference; 95% CI, −11% to 24%; P = .49).
Figure 5.
GVHD. Cumulative incidence of grade 2 to 4 aGVHD (A), grade 3 to 4 aGVHD (B), and cGVHD (C). Analysis was performed in the transplanted population by randomly assigned treatment.
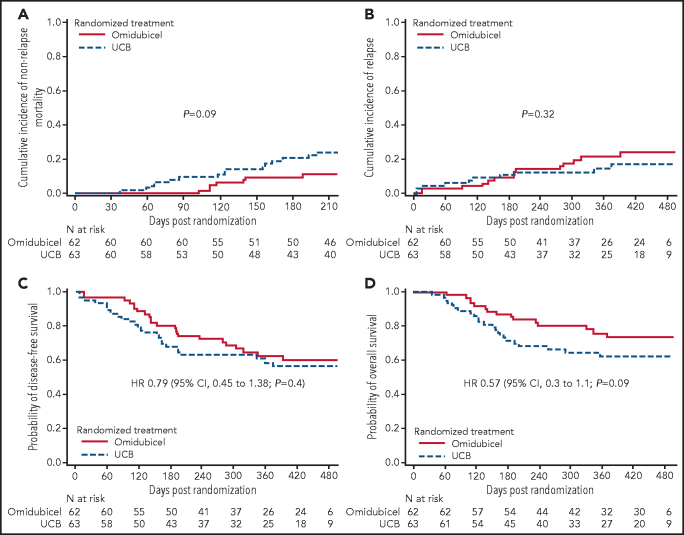
NRM, relapse, DFS, and OS
The median follow-up of all patients was 10 months after transplantation (range, 1-19 months). Using ITT analysis, the cumulative incidence of NRM at 210 days after random assignment was 11% for the omidubicel arm and 24% for the control arm (P = .09) (Figure 6A). The cumulative incidence of disease relapse at 15 months after random assignment was 25% for the omidubicel arm and 17% for the control arm (P = .32) (Figure 6B). During the time from random assignment to transplantation, relapse was reported in 4 patients allocated to the omidubicel arm and 4 patients allocated to the standard UCBT arm. Among these, relapse prevented 2 patients allocated to the omidubicel arm and 3 patients allocated to the UCBT arm from receiving a transplant by day 90 after random assignment (Figure 1).
Figure 6.
Outcomes of omidubicel and standard UCBT, ITT analysis. (A-B) Cumulative incidence of NRM (A) and relapse (B). (C-D) Probability of DFS (C) and OS (D). HR, hazard ratio.
The adjusted hazard ratio for treatment failure (relapse or death, inverse of RFS) with omidubicel vs standard UCB was 0.79 (95% CI, 0.45-1.38; P = .4). The adjusted hazard ratio for mortality with omidubicel vs standard UCB was 0.57 (95% CI, 0.3-1.1; P = .09) (Figure 6C-D). The 1-year GVHD-free RFS for the omidubicel arm was 36% and 45% for standard UCBT (P = .56).
Eleven deaths were reported among the as-treated population of patients who received a transplant with omidubicel, and 18 deaths among the patients treated with a standard UCB graft. As reported by the study investigators, 2 patients who received a transplant with omidubicel died of relapsed disease compared with 4 patients who received a transplant with a standard UCB graft. Among the treatment-related causes of death, GVHD was the setting for death for 4 patients in each group.
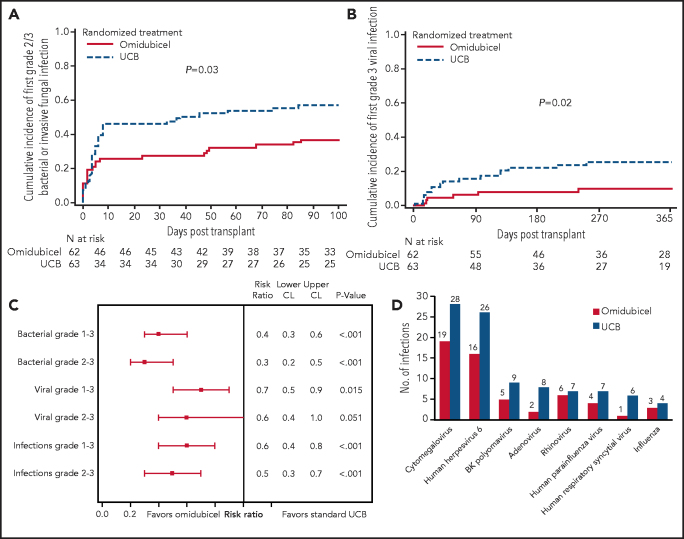
Transplant course and toxicity
Patients randomly assigned to the omidubicel graft spent more days alive and out of hospital in the first 100 days after transplantation than those randomly assigned to UCBT; the median time was 61 days (range, 0-89 days) and 48 days (range, 0-84 days), respectively (P = .005). The median time from transplant to discharge from the hospital was 27 days for the omidubicel arm and 35 days for the control arm (P = .005). From random assignment and up to 100 days after transplantation, the cumulative incidence of first grade 2 to 3 bacterial or invasive fungal infections was 37% for patients randomly assigned to the omidubicel arm and 57% for patients who received the standard UCBT (P = .03) (Figure 7A). The cumulative incidence of first grade 3 viral infection during the first year after transplantation was also lower for those randomly assigned to the omidubicel arm (10% vs 26%; P = .02) (Figure 7B).
Figure 7.
Infections after transplantation. (A) Cumulative incidence of first grade 2 to 3 bacterial infection or invasive fungal infections during the first 100 days after transplantation for the ITT population. (B) Cumulative incidence of first grade 3 viral infection during the first year for the ITT population. All infection events that occurred after random assignment are accounted for in the analysis. (C) Relative risk (95% CI) for bacterial, viral, and all infections at 1 year after transplantation in the omidubicel and the standard UCB groups for the as-treated population. (D) Grade 1 to 3 viral infections at 1 year after transplantation by species for the as-treated population. CL, confidence level.
To account for the possibility of multiple infections per single patient and relative differences in periods of risk between the treatment groups, we compared infection density during the first year after transplantation. The risk ratio for all infections, irrespective of severity, was significantly lower among recipients of omidubicel compared with those who received standard UCBT. The same observation was made when bacterial and viral infections were analyzed individually (Figure 7C). Overall, fewer infections from all reported viral species were observed for omidubicel recipients (Figure 7D); however, these differences did not reach statistical significance. Invasive fungal infections were uncommon in both arms of the study.
The incidence of treatment-emergent serious adverse events (SAEs) possibly related to the stem cell product was similar in the 2 arms (40% for omidubicel and 41% for standard cord blood grafts). A breakdown of the treatment-emergent adverse events in both arms of the study is provided in supplemental Table 3. Those treatment-emergent events reported as related to the cord blood infusion are outlined in supplemental Table 4. After random assignment and before starting pretransplant conditioning, 10 serious adverse events (SAEs) were reported for those assigned to the omidubicel arm and 8 SAEs were reported for those assigned to a standard UCB graft.
Immune reconstitution
Quantitative recovery of lymphoid subsets was monitored at 1, 3, 6, and 12 months after transplantation in subsets of patients on both arms of the study. Despite the lower numbers of CD3+ cells in patients on the omidubicel arm compared with those who received standard UCB grafts, the pace of recovery to normal levels of CD3+, CD4+, CD8+, CD19+, and CD56+/CD16+ NK cells was similar in both groups (supplemental Figure 1A-E).
Discussion
Omidubicel is an ex vivo expanded, UCB-derived stem cell graft that was designed to address the major limitations of adult UCBT. There were 3 main findings from this multicenter randomized trial comparing omidubicel to a standard UCB graft. (1) The study confirmed that omidubicel safely addresses the most vexing limitation of UCBT, which is the delay in hematopoietic recovery. Omidubicel reduced the median time to neutrophil recovery by 10 days and the median time to platelet recovery by 13 days. (2) Omidubicel reduced the incidence of infectious complications and time spent in the hospital during the early posttransplantation period. (3) The study demonstrated the feasibility and safety of delivering a personalized, manufactured HSC product to transplantation centers around the world.
Multiple techniques designed to expand UCB stem and progenitor cells have been reported.5, 6, 7, 11, 12, 13 Omidubicel (previously known as NiCord) is the first drug to complete phase 3 testing, the results of which were consistent with observations from earlier studies that examined both safety and efficacy.6, 9 The omidubicel graft provides a CD34+ cell dose that is comparable to an adult mobilized PBSC graft. The 12-day median time to neutrophil recovery is similar to that for mobilized PB, suggesting that both graft sources are enriched for active hematopoietic progenitor cells.14 Furthermore, long-term follow-up from the earlier studies of omidubicel6 suggest robust, durable engraftment for more than 10 years, confirming the persistence and possible expansion of long-term repopulating cells during the ex vivo culture period. The clinical impact of reducing the time to hematopoietic recovery has been well characterized in the literature. A prospective multicenter study of BM vs PBSC grafts showed that a 5-day reduction in time to neutrophil recovery after PBSC graft translated into a reduction in bacterial infections.15 Conversely, a large multicenter study using the CIBMTR database demonstrated delayed hematopoietic recovery after standard adult UCBT resulted in prolonged hospital use.3 In line with the previous studies, rapid hematopoietic recovery after omidubicel transplantation translated into clinical benefit by reducing infections and time spent in the hospital during the first 100 days after transplantation. Importantly, although omidubicel grafts had a lower T-cell content, the recovery of T cells after transplantation is comparable to that with standard UCB, and the risk of viral infections was lower than that with standard UCB throughout the first year after transplantation. The reduced risk of viral infections for recipients of omidubicel was an unexpected finding and could perhaps be attributable to more robust NK cell reconstitution. Further studies of the T-cell receptor diversity are planned and may provide additional insight into this observation.
This study establishes for the first time, the feasibility of providing a personalized, ex vivo expanded HSC graft to recipients throughout the world. This was made possible with logistical support provided by both the sponsor and the regional UCB registries. For example, the National Marrow Donor Program provided participating centers with advice on selecting units that meet prespecified characteristics for expansion. Furthermore, they worked with the sponsor to facilitate transportation of the unit from the cord blood bank to the cell processing facility. Of note, although the added logistical complexity of producing an ex vivo expanded UCB graft led to a median 2-week delay in time from random assignment to transplantation, this did not result in an increased risk of pretransplant relapse. The study suggests that what is now possible with a commercial, personalized T-cell product in the form of chimeric antigen receptor T-cell therapy can be accomplished at the same scale with a personalized HSC graft.
The encouraging results of transplantation with omidubicel have important implications for minority populations in need of allo-HSCT. Forty-four percent of the patients treated on study were non-White, a population known to be underrepresented in the world-wide unrelated adult donor and UCB registries. The underrepresentation of UCB grafts from Black donors has necessitated the use of smaller units compared with those used for White recipients, which results in inferior outcome.16 UCB expansion technologies allow for the use of smaller, better matched units with the aim of improving outcome.
The study has important limitations. Although the progression-free survival (PFS) and OS end points trended higher for those receiving omidubicel, the study was not powered to detect a statistically significant difference in these critical end points. Adult UCBT trials have been notoriously difficult to complete, with many previous multicenter trials closing early because of incomplete accrual.17, 18 For this reason, alternative end points of clinical benefit were chosen to allow for a more realistic sample size. Use of resources for transplantation of UCB grafts has historically exceeded that for adult donor stem cell grafts. The reduction in time to engraftment, hospitalization duration, and infectious complications is expected to reduce the need to use resources over those for a standard UCB graft. Although data on use of resources are not presented in this report, those data have been captured and will allow for confirmation of this expectation. These, and other pressing questions such as the performance of omidubicel transplantation after reduced intensity conditioning and comparative outcomes to other graft sources and specific disease types will need to be addressed in future studies.
Hematopoietic recovery after transplantation with omidubicel was faster, reduced early transplant-related complications, and reduced the number of days patients were hospitalized compared with standard UCBT. The results of this trial demonstrate that omidubicel represents a major therapeutic advance and should be considered as a new standard of care for adult patients eligible for UCBT.
Authorship
Contribution: E.G.-C., M.E.H., L.S.F., and G.S. conceived the study design and protocol; L.S.F., B.B., and S.W. performed statistical analyses; M.E.H. performed the research and wrote the manuscript; and M.E.H., P.J.S., C.C., C.B., R.H., R.T.M., A.R.R., N.A.K., J.M., D.V., G.J.S., C.A.L., W.Y.K.H., L.P.K., A.K., Y.K., N.H., O.F., T.P., I.S., B.B., S.W., L.S.F., E.G.-C., and G.S. collected, assembled, analyzed, and interpreted the data, reviewed and approved the manuscript, and are accountable for all aspects of the work.
Conflict-of-interest disclosure: M.E.H. served as consultant to AbbVie, CareDx, and Magenta, received honoraria from Kadmon, and received research funding from Gamida Cell. P.J.S. served as a consultant to CRISPR and received research funding from Gamida Cell, Atara Biotherapeutics, Amgen, Incyte, Takeda, Macrogenics, and Eisai. C.C. served as a consultant and member of the board of directors or advisory committee for Incyte, Kadmon, Jazz Pharmaceuticals, Medsenic, Generon, and Mesoblast. C.B. received research funding from Magenta, Gamida Cell, and Astex and is an advisor to AlloVir. R.T.M. received research funding from Novartis and Juno, data safety monitoring board membership for Novartis and Athersys, received honoraria from Incyte, Kite Pharma, Bristol Myers Squibb/Celgene, PACT Pharma, Orca BioSystems, and Omeros, has patents with and receives royalties from Athersys, and served as a consultant for Novartis, Incyte, CRISPR Therapeutics, Artiva Biotherapeutics, and Allovir. A.R.R. received research funding from Pharmacyclics. J.M. received research funding from Novartis, Fresenius Biotech, Astellas, Bellicum Pharmaceuticals, Gamida Cell, and Pluristem, and received honoraria and served as a consultant for Kite Pharma, Juno, and AlloVir. G.J.S. served as a consultant for Agios, Amgen, AstraZeneca, Incyte, Novartis, and Ono, served on the speakers bureau for Celgene, Sanofi, Gilead, and Stemline, and received research funding from AbbVie, Actinium, Ariad, Astellas, Celgene, Celator, Constellation, Cyclacel, Daiichi Sankyo, Deciphera, DeltaFly, Forma, FujiFilm, Gamida Cell, Genentech, Roche, Geron, Jazz Pharmaceuticals, Karyopharm, Kite Pharma, Mateon, Medimmune, Onconova, Pfizer, Regimmune, Samus, Sangamo, Tolero, Trovagene, Kaiser Permanente, and Johnson & Johnson, and has equity in Bristol Myers Squibb and Pfizer. Y.K. was a member of the board of directors, advisory committee, or speakers bureau for Celgene, Seattle Genetics, Jazz Pharmaceuticals, and Takeda. G.S. served on an advisory committee for AbbVie, Hoffman-LaRoche, Helsinn, and Takeda. I.S. and E.G.-C. are employed by and have equity holdings in Gamida Cell. T.P. reports equity holdings in Gamida Cell. B.B. and S.W. are employed by Emmes Company. L.S.F. declares that Gertner Institute for Epidemiology and Health Policy Research received remuneration from Gamida Cell for the statistical consultation that he provided to the trial. The remaining authors declare no competing financial interests.
Acknowledgments
The authors thank Bruno Boulanger and Elena Maurer from BPE for their contribution to the CD34 correlative analyses, and Sarah Anderson, Alice Henning, Shashidhar Joshy, Laura Morrison, and Amarnath Vijayarangan from the Emmes Company for their support for statistical analyses. This work was supported by funding from Gamida Cell.
Footnotes
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Delayed engraftment and risk of graft failure have restricted the use of cord blood (CB) in allotransplantation. Horwitz et al report results of a phase 3 trial comparing use of a single CB unit expanded ex vivo for 21 days with nicotinamide in combination with stem cell factor, Flt3 ligand, interleukin-6, and thrombopoietin (omidubicel) with a standard unmanipulated single or double CB transplant. Omidubicel resulted in faster neutrophil engraftment (12 vs 22 days), platelet recovery, and B-cell and natural killer cell reconstitution than unmanipulated CB products, with lower incidence of viral and fungal infections and more time out of hospital.
Supplementary Material
REFERENCES
- 1.Gragert L, Eapen M, Williams E, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N Engl J Med. 2014;371(4):339–348. doi: 10.1056/NEJMsa1311707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ballen K, Woo Ahn K, Chen M, et al. Infection rates among acute leukemia patients receiving alternative donor hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2016;22(9):1636–1645. doi: 10.1016/j.bbmt.2016.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ballen KK, Joffe S, Brazauskas R, et al. Hospital length of stay in the first 100 days after allogeneic hematopoietic cell transplantation for acute leukemia in remission: comparison among alternative graft sources. Biol Blood Marrow Transplant. 2014;20(11):1819–1827. doi: 10.1016/j.bbmt.2014.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Delaney C, Heimfeld S, Brashem-Stein C, Voorhies H, Manger RL, Bernstein ID. Notch-mediated expansion of human cord blood progenitor cells capable of rapid myeloid reconstitution. Nat Med. 2010;16(2):232–236. doi: 10.1038/nm.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de Lima M, McNiece I, Robinson SN, et al. Cord-blood engraftment with ex vivo mesenchymal-cell coculture. N Engl J Med. 2012;367(24):2305–2315. doi: 10.1056/NEJMoa1207285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Horwitz ME, Chao NJ, Rizzieri DA, et al. Umbilical cord blood expansion with nicotinamide provides long-term multilineage engraftment. J Clin Invest. 2014;124(7):3121–3128. doi: 10.1172/JCI74556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wagner JE, Jr, Brunstein CG, Boitano AE, et al. Phase I/II trial of StemRegenin-1 expanded umbilical cord blood hematopoietic stem cells supports testing as a stand-alone graft. Cell Stem Cell. 2016;18(1):144–155. doi: 10.1016/j.stem.2015.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Peled T, Shoham H, Aschengrau D, et al. Nicotinamide, a SIRT1 inhibitor, inhibits differentiation and facilitates expansion of hematopoietic progenitor cells with enhanced bone marrow homing and engraftment. Exp Hematol. 2012;40(4):342. doi: 10.1016/j.exphem.2011.12.005. 55.e1. [DOI] [PubMed] [Google Scholar]
- 9.Horwitz ME, Wease S, Blackwell B, et al. Phase I/II study of stem-cell transplantation using a single cord blood unit expanded ex vivo with nicotinamide. J Clin Oncol. 2019;37(5):367–374. doi: 10.1200/JCO.18.00053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Proschan M, Brittain E, Kammerman L. Minimize the use of minimization with unequal allocation. Biometrics. 2011;67(3):1135–1141. doi: 10.1111/j.1541-0420.2010.01545.x. [DOI] [PubMed] [Google Scholar]
- 11.Cohen S, Roy J, Lachance S, et al. Hematopoietic stem cell transplantation using single UM171-expanded cord blood: a single-arm, phase 1-2 safety and feasibility study. Lancet Haematol. 2020;7(2):e134–e145. doi: 10.1016/S2352-3026(19)30202-9. [DOI] [PubMed] [Google Scholar]
- 12.Delaney C, Milano F, Shelley H, Nicoud I, Bernstein ID. Infusion of non-HLA matched, off-the-shelf ex vivo expanded cord blood progenitor cells in patients undergoing myeloablative cord blood transplantation is safe and decreases the time to neutrophil recovery. Biol Blood Marrow Transplant. 2012;18(2):S203. [Google Scholar]
- 13.Wagner JE, Brunstein C, McKenna D, Sumstad D., StemRegenin-1 (SR1) expansion culture abrogates the engraftment barrier associated with umbilical cord blood transplantation (UCBT) [abstract]. Blood., 2014;124(21). Abstract 728.
- 14.Bishop MR, Tarantolo SR, Geller RB, et al. A randomized, double-blind trial of filgrastim (granulocyte colony-stimulating factor) versus placebo following allogeneic blood stem cell transplantation. Blood. 2000;96(1):80–85. [PubMed] [Google Scholar]
- 15.Young JH, Logan BR, Wu J, et al. Blood and Marrow Transplant Clinical Trials Network Trial 0201 Infections after transplantation of bone marrow or peripheral blood stem cells from unrelated donors. Biol Blood Marrow Transplant. 2016;22(2):359–370. doi: 10.1016/j.bbmt.2015.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ballen KK, Klein JP, Pedersen TL, et al. Relationship of race/ethnicity and survival after single umbilical cord blood transplantation for adults and children with leukemia and myelodysplastic syndromes. Biol Blood Marrow Transplant. 2012;18(6):903–912. doi: 10.1016/j.bbmt.2011.10.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sanz J, Montoro J, Solano C, et al. Prospective randomized study comparing myeloablative unrelated umbilical cord blood transplantation versus HLA-haploidentical related stem cell transplantation for adults with hematologic malignancies. Biol Blood Marrow Transplant. 2020;26(2):358–366. doi: 10.1016/j.bbmt.2019.10.014. [DOI] [PubMed] [Google Scholar]
- 18.Fuchs EJ, O'Donnell PV, Eapen M, et al. Double unrelated umbilical cord blood vs HLA-haploidentical bone marrow transplantation: the BMT CTN 1101 trial. Blood. 2021;137(3):420–428. doi: 10.1182/blood.2020007535. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.