Abstract
Objective
To identify the racial and ethnic representation of participants in mental health research conducted in the perinatal period during the COVID-19 pandemic.
Data Sources
MEDLINE, CINAHL, Cochrane Library, PsycINFO, Scopus, Web of Science.
Study Selection
We included peer-reviewed research articles in which researchers reported mental health outcomes of women during the perinatal period who were living in the United States or Canada during the COVID-19 pandemic. We included 25 articles in the final review.
Data Extraction
We extracted the citation, publication date, design, aim, country of origin, participant characteristics, sampling method, method of measurement of race and ethnicity, and mental health outcome(s).
Data Synthesis
The combined racial and ethnic representation of the 16,841 participants in the included studies was White (76.5%), Black (9.8%), other/multiracial (6.2%), Asian (3.9%), Hispanic/Latina (2.6%), Indigenous or Ethnic Minority Canadian (0.9%), and Native American or Alaska Native (0.1%). Most studies were conducted in the United States, used a cross-sectional design, and incorporated social media platforms to recruit participants. Depression, anxiety, and stress were the most frequently assessed mental health outcomes.
Conclusion
Relatively few women of color who were pregnant or in the postpartum period during the pandemic participated in mental health research studies. Future studies should develop intentional recruitment strategies to increase participation of women of color. Researchers should use updated guidance on reporting race and ethnicity to accurately represent every participant, minimize misclassification of women of color, and report meaningful results.
Keywords: COVID-19, mental health, mothers, postpartum period, pregnancy
The authors review the racial and ethnic diversity of women who participated in perinatal mental health research studies conducted during the pandemic.
Common mental health disorders that occur during the perinatal period between pregnancy and the first year postpartum include anxiety, depression, stress, and posttraumatic stress. In the United States, up to 14% of women experience symptoms of depression across the perinatal period (Gavin et al., 2005; Ko et al., 2017; Wisner et al., 2013), and approximately 15% to 21% experience depression and anxiety symptoms in pregnancy (Wisner et al., 2013). Depression and anxiety rates are similar among Canadian women (Gheorghe et al., 2021; Statistics Canada, 2019). Evidence suggests that between 3.3% and 4% of women in the United States experience posttraumatic stress symptoms after childbirth (Yildiz et al., 2017).
The COVID-19 public health crisis intensified the risk of antenatal mental health disorders because of related stressors that included (a) a shift to virtual health care and the inability to bring a partner or support person to in-person visits (C. H. Liu, Goyal, et al., 2021); (b) fear and the unknown effects of the virus on the fetus or newborn (Basu et al., 2021; Burgess et al. 2022; Kotlar et al., 2021); (c) the increased demand of juggling work from home, loss of child care, and school closures (Ajayi et al., 2021; Basu et al., 2021; Lee & Parolin, 2021; Mollard et al., 2021; Perzow et al., 2021); and (d) missed milestone celebrations, such as baby showers and gender reveals (Goyal, De La Rosa, et al., 2021; Goyal, Han, et al., 2021). Fear of exposure to COVID-19, partner/support restrictions during the birth, and being separated from the infant after the birth increased the risk of depression and anxiety in women in the postnatal period (Burgess et al., 2022; C. H. Liu et al., 2022; Shuman et al., 2022).
The racial and ethnic representation of participants in maternal mental health research conducted in North America during the COVID-19 pandemic is unknown.
The COVID-19 pandemic also highlighted racial inequities among women during the childbearing period. Even before the pandemic, women of color were at an increased risk of developing symptoms of depression in the perinatal period (Bauman et al., 2020; Daoud et al., 2019; Gheorghe et al., 2021; Groulx et al., 2021; Hetherington et al., 2020; Kendig et al., 2017; Miller et al., 2022; Mukherjee et al., 2016; Soffer et al., 2019; Wisner et al., 2013). Although data from 240,147 birth certificates in California indicated an increase in COVID-19 diagnosis across all racial and ethnic groups (Karasek et al., 2021), COVID-19 disproportionately affected the birth experiences of women of color. For example, compared with White women, those of color were more likely to experience discrimination in health care (e.g., Black women, 40.0% and Latina women, 35.3%; Janevic et al., 2021), be less satisfied with the birth (Breman et al., 2021; Janevic et al., 2021), and have less access to health care (Masters et al., 2021). Additionally, in a retrospective design, Pope et al. (2021) compared public health surveillance data of 162 pregnant women infected with COVID-19 to identify risk factors among Black (n = 81, 50%) and non-Black (n = 81, 50%) women. The results indicated that Black women infected with COVID-19 were significantly more likely to have preterm birth (p = .026) and be exposed to COVID-19 at work (p = .020) than non-Black women infected with COVID-19 (Pope et al., 2021).
Race and Ethnicity of Participants in Perinatal Mental Health Research Before COVID-19
Before the pandemic, in several large-scale studies on perinatal mental health issues conducted in the United States and Canada, researchers reported that most participants were White. For example, 80% of participants in a sequential case series study to identify symptoms of depression among 10,000 women who recently gave birth in the United States were White (Wisner et al., 2013). McCall-Hosenfeld et al. (2016) identified symptoms of depression among 3,006 women in the United States who participated in the First Baby Cohort Study, and 83.2% self-identified as White. In a secondary analysis of 8,784 pregnant women in the United States conducted by Miller et al. (2022) to identify the trajectory of symptoms of depression, 62.3% of the participants self-identified as White. In Canada, in a survey by Hetherington et al. (2020) survey of 3,387 women to assess symptoms of depression in the perinatal period, 78.6% self-identified as White.
The percentage of White participants in these large studies is not surprising because it mirrors the demographic characteristics of the North American population, in which 75% of Americans and Canadians self-identify as White (Statistics Canada, 2022; U.S. Census Bureau, 2021a). However, the population in North America is becoming increasingly racially and ethnically diverse. In the United States, the non-Hispanic White population decreased from 63.7% in 2010 to 57.8% in 2020 (U.S. Census, 2021b). Conversely, the Hispanic or Latino population grew from 16% of the total population in 2010 to 18.7% in 2020; similarly, the Asian population grew from 5% in 2010 to 6.2% in 2020 (U.S. Census Bureau, 2021b). In Canada, census data reveal that approximately one fifth (22.3%) of the population is classified as a visible minority, defined as “persons, other than Aboriginal peoples, who are non-Caucasian in race or non-White in colour” (Statistics Canada, 2021, para. 1), and this is projected to increase to 33% by 2036 (Morency et al., 2017).
The increasing racial and ethnic diversity in North America, together with the recent national focus on the increased maternal mortality and morbidity among women of color (Howell, 2018; Kozhimannil et al., 2020), has led to renewed social justice movements that call out structural racism and implicit bias (Harris et al., 2021; Huggins et al., 2020; Matthews et al., 2021; Taylor, 2020). Although review articles have mapped the influence of the COVID-19 pandemic on maternal mental health issues across the globe, the race and ethnicity of research participants have not been discussed (Iyengar et al., 2021; Kotlar et al., 2021; Suwalska et al., 2021; Yan et al., 2020) and remain unknown. Therefore, we conducted a scoping review to identify the racial and ethnic representation of participants in mental health research conducted in the perinatal period during the COVID-19 pandemic.
Methods
Design
We used the scoping review methodology of Arksey and O’Malley (2005), which includes the following steps: identifying the research question; identifying relevant studies; study selection; charting the data; and collating, summarizing, and reporting the results. We developed a review protocol to identify research studies that examined mental health outcomes among women who were pregnant or in the postpartum period during the COVID-19 pandemic. Next, we consulted with two research librarians on the topic and scope of the review. We conducted literature searches between December 9, 2021, and December 12, 2021, using MEDLINE (via PubMed), CINAHL, Cochrane Library, PsycINFO, Scopus, and Web of Science. Searches are inclusive of the results indexed at that time.
Study Selection
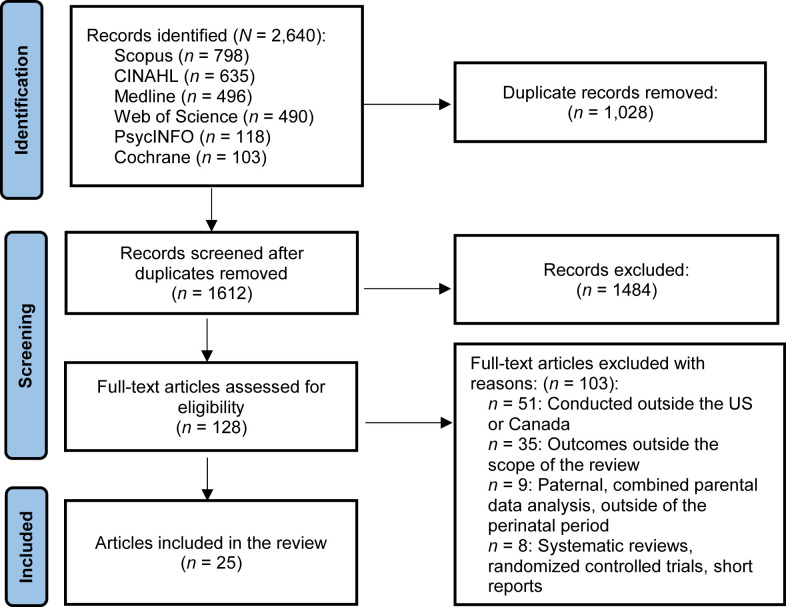
We included articles if they were published between January 1, 2020, and December 12, 2021, in English in peer-reviewed journals and if authors examined the influence of the pandemic on mental health outcomes (e.g., depression, anxiety, stress, posttraumatic stress) among women who were pregnant or within the first year postpartum at the time of data collection and who were living in the United States or Canada. We excluded studies on combined maternal and paternal outcomes, paternal outcomes only, and ones that were published in countries other than the United States or Canada. We also excluded studies with randomized controlled designs, short communications, psychometric evaluation of screening instruments, or reports of preliminary studies. See Supplementary Table S1 for the final search strings. Two research librarians conducted the searches (G.B. and E.K.C.). G.B. exported 2,640 citations into the review software manager Covidence and removed 1,028 duplicate citations, which left us to review 1,612 citations (Covidence, n. d.). Figure 1 depicts the search strategy.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) diagram of scoping review methods.
Data Extraction and Synthesis
We screened articles in two phases. First, we conducted a title and abstract review and then a full-text review. The first and third authors (D.G. and M.L.) independently completed the title and abstract review for 1,612 articles, of which 1,484 were excluded and 128 were identified for full-text screening. At this stage, we excluded 103 articles for the following reasons: research was conducted outside of the United States or Canada; main outcomes were not depression symptoms, such as anxiety, stress, or posttraumatic stress disorder; inclusion of paternal or parental results; research was conducted outside the perinatal period; or the articles reported on preliminary studies or short communications. We discussed any discrepancies with the second author (J.D.). Twenty-five articles met the review criteria (see Figure 1). Data abstraction included the following information: publication date, design, aim, country of origin, participant sociodemographic characteristics, sampling method, method of measurement of race and ethnicity, and mental health outcome(s) measured. We extracted racial and ethnic data from the results sections, tables, and supplementary materials of the published articles. We compiled a spreadsheet to count the frequency of the racial and ethnic categories reported in the included studies and collapsed them into the following categories for this review: Asian, Hawaiian Pacific Islander; Black, African American, non-Hispanic Black; White, Non-Hispanic White, Caucasian; Hispanic, Latina; multiracial; Native American, Indigenous, First Nations; and other. The third (M.L.) and fourth (S.N.) authors independently extracted data, and the first author (D.G.) verified all data extraction and discussed discrepancies with the rest of the research team. We used the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flowchart to guide screening along with the PRISMA extension for scoping reviews checklist (Tricco et al., 2016).
Results
We identified 25 articles that met the inclusion criteria: 15 were reports of quantitative studies, four were reports of qualitative studies, and six were reports of studies that used mixed methods. Most of the studies took place between March 2020 and January 2021, were conducted in the United States (n = 20, 80%), used cross-sectional designs (n =15, 60%), and incorporated social media platforms to recruit participants (n = 19, 76%). The total combined number of participants in the included studies was 16,841; individual sample sizes ranged from 31 (Farewell et al., 2020) to 4,604 (Groulx et al., 2021). See Table 1 for a summary of the articles and Supplementary Table S2 for detailed information on the data extracted from each article.
Table 1.
Summary Characteristics of Studies Included in Review (N = 25)
| Characteristics | n (%) |
|---|---|
| Country | |
| United States | 20 (80) |
| Canada | 5 (20) |
| Study design | |
| Quantitative | 15 (60) |
| Qualitative | 4 (16) |
| Mixed methods | 6 (24) |
| Recruitment strategy | |
| Social media, online | 19 (76) |
| Ongoing study | 3 (12) |
| Electronic medical records | 2 (8) |
| No method provided | 1 (4) |
| Language criteria | |
| English only | 22 (88) |
| French | 2 (8) |
| Spanish | 1 (4) |
| Method of race/ethnicity data collection | |
| Self-report | 23 (92) |
| Electronic medical records | 2 (8) |
| Participant race/ethnicity | |
| Asiana | 665 (3.9) |
| Blackb | 1,655 (9.8) |
| Canadianc | 157 (0.9) |
| Hispanic or Latina | 445 (2.6) |
| Native American, Alaskan Native | 10 (0.1) |
| Other, non-White, multiracial | 1,041 (6.2) |
| Whited | 12,882 (76.5) |
| Perinatal period | |
| Pregnancy | 10 (40) |
| Postpartum period | 6 (24) |
| Pregnancy and postpartum | 9 (36) |
| Mental health outcomes | |
| Anxiety alone | 1 (4) |
| Depression alone | 2 (8) |
| Stress alone | 4 (16) |
| Anxiety and depression | 8 (32) |
| Anxiety, depression, and stress | 7 (28) |
| Anxiety, depression, and posttraumatic stress | 3 (12) |
Includes Asian, Asian Indian, Asian/Hawaiian Pacific Islander, Chinese, Filipino, and Korean.
Includes Black, African American, and non-Hispanic Black.
Includes Indigenous, Ethnic Minority, First Nations, Inuit, and Metis.
Includes Caucasian and non-Hispanic White.
Race and Ethnicities of Participants
Most researchers in the included studies, including two who used electronic medical record data, used conventional race categories outlined by the Office of Management and Budget (1997): American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or other Pacific Islander, White, and Hispanic ethnicity (see Table 2 and Supplementary Table S2). The racial and ethnic representation of the 16,841 participants in the included studies was White (76.5%), Black (9.8%), other/multiracial (6.2%), Asian (3.9%), Hispanic/Latina (2.6%), Indigenous or Ethnic Minority Canadian (0.9%), and Native American or Alaska Native (0.1%; see Table 2). Three researchers (12%) provided details for White participants without any further detail on the rest of the sample; McMillian et al. (2021) described participants as primarily "White and Non-Hispanic/Non-Latino (83.7%)" (p. 181). Moyer et al. (2020) described participants as "mostly White (87.7%)" (p. 761). Ollivier et al. (2021) described participants as "primarily Caucasian (96.6%)" (p. 2).
Table 2.
Races and Ethnicities of Participants, %
| Authors and Year | Asian, Hawaiian, and Pacific Islander | Black African American and Non-Hispanic Black | White, Non-Hispanic White, and Caucasian | Hispanic and Latina | Multiracial | Native American, Indigenous, and First Nations | Other |
|---|---|---|---|---|---|---|---|
| Ahlers-Schmidt et al. (2020) | — | 19.3 | 43 | 26.3 | 5.3 | — | 6.1 |
| Anderson et al. (2022) | 1.7 | 3.3 | 71.7 | 15 | 8.3 | — | — |
| Barbosa-Leiker et al. (2021) | 4 | 5 | 79 | 7 | 5 | — | — |
| Claridge et al. (2021)a | 2.6 | 2.4 | 88.2 | 16.7 | 6.9 | — | |
| Farewell et al. (2020)a | — | 7.1 | 85.7 | 14.8 | — | — | 3.6 |
| Goyal, Beck, et al (2021) | 8.4 | 0.8 | 82 | 6.1 | — | — | 2.7 |
| Goyal, Han, et al. (2021) | 86.8 | — | — | — | — | — | 13.2 |
| Groulx et al. (2021) | 7.5 | 1.7 | 81.6 | 2.1 | 4.9 | 2.2 | — |
| Joy et al. (2020)b | — | — | — | — | — | — | — |
| Khoury et al. (2021) | 6.9 | — | 84.8 | — | 3.0 | 0.7 | 4.6 |
| Kinser et al. (2021) | 3 | 8 | 83 | 2 | 3 | 1 | 2 |
| Kornfield et al. (2021) | — | 18.1 | 71.9 | 5 | — | — | — |
| Lebel et al. (2020) | 6 | 0.7 | 87.1 | 1.1 | 3.3 | 2 | — |
| C. H. Liu, Erdei, & Mittal (2021) | 3.5 | 0.9 | 89.9 | 3.6 | — | — | 2.1 |
| C. H. Liu, Hyun, et al. (2021) | 3 | 1 | 92.9 | 3.1 | — | — | |
| J. Liu et al. (2021) | — | 44.1 | 38.9 | 9.4 | — | — | 7.7 |
| McMillan et al. (2021) | — | — | 83.7 | — | — | — | |
| Mollard et al. (2021) | 2.9 | 1.4 | 84.8 | 9.2 | — | — | 1.8 |
| Moyer et al. (2020) | — | — | 88 | — | — | — | — |
| Ollivier et al. (2021) | — | — | 96.6 | — | — | — | — |
| Omowale et al. (2021) | — | 38 | 62 | — | — | — | — |
| Perzow et al. (2021)c | 5.1 | 11.1 | 54.8 | 25.9 | 3.7 | 6.7 | — |
| Silverman, Burgos, et al. (2020) and Silverman, Medeiros, & Burgos (2020)d | — | — | — | — | — | — | — |
| Wheeler et al. (2021) | — | 100 | — | — | — | — | — |
Total >100% as data includes participants from a separate Latina/Hispanic ethnicity question.
Majority Caucasian, predominantly White or non-Hispanic White.
Total >100% author reports N = 135, Table 1, p. 3 shows N = 145.
Hispanic or African American (90%) and Asian (10%).
In 17 studies (68%), researchers categorized participants as ethnic minorities, other, mixed race, one or more races, multiracial, or non-White, accounting for 6.2% of the total sample (Ahlers-Schmidt et al., 2020; Anderson et al., 2022; Barbosa-Leiker et al., 2021; Claridge et al., 2021; Farewell et al., 2020; Goyal, Beck, et al., 2021; Goyal, De La Rosa, et al. 2021; Groulx et al., 2021; Khoury et al., 2021; Kinser et al., 2021; Kornfield et al., 2021; Lebel et al., 2020; C. H. Liu, Erdei, & Mittal, 2021; J. Liu et al., 2021; McMillan et al., 2021; Mollard et al., 2021; Perzow et al., 2021).
Two of the 25 studies (Groulx et al., 2021; Lebel et al., 2020) provided in-depth racial and ethnic descriptions of non-White participants: Black Chinese, Filipino, First Nations, Hispanic, Korean, Metis, mixed, South Asian, South-east Asian, and West Asian. Both studies were conducted in Canada, and the researchers reported on participants from the same prospective study; Lebel et al. (2020) evaluated data collected in April 2020, and Groulx et al. (2021) reported data collected from April to June 2020.
The results of our review indicate that few women of color participated in maternal mental health research conducted in North America during the COVID-19 pandemic.
In two studies, researchers evaluated the experiences of women of color during the pandemic. Goyal, Han et al. (2021) assessed symptoms of depression and experiences in women of Asian American descent. Researchers asked participants to self-report their Asian ethnicity resulting in the following 10 ethnicities: Asian Indian, Chinese, Filipino, Hmong, Japanese, Laotian, Korean, Thai, and Vietnamese (Goyal, Han et al., 2021). In a prospective, longitudinal cohort design, Wheeler et al. (2021) evaluated stress and coping among 33 pregnant Black women before and during the COVID-19 pandemic using data from an ongoing study.
Mental Health Outcomes
Of the 25 included studies that reported mental health outcomes, the most frequently assessed mental health outcomes were symptoms of depression, anxiety, and stress (n = 15, 60%; see Table 1). Mental health outcomes were assessed in 10 studies during pregnancy (Claridge et al., 2021; Groulx et al., 2021; Khoury et al., 2021; Lebel et al., 2020; C. H. Liu, Hyun, et al., 2021; J. Liu et al., 2021; McMillan et al., 2021; Moyer et al., 2020; Silverman, Medeiros, & Burgos, 2020; Wheeler et al., 2021), in six studies during the postnatal period (Goyal, Beck, et al., 2021; Goyal, Han, et al., 2021; Joy et al., 2020; Mollard et al., 2021; Ollivier et al., 2021; Silverman, Burgos, et al., 2020), and in nine studies across the perinatal period (Ahlers-Schmidt et al., 2020; Anderson et al., 2022; Barbosa-Leiker et al., 2021; Farewell et al., 2020; Kinser et al., 2021; Kornfield et al., 2021; C. H. Liu, Erdei, & Mittal, 2021; Omowale et al., 2021; Perzow et al., 2021).
Mental Health Outcomes by Race and Ethnicity
In four studies, researchers evaluated mental health outcomes by race and ethnicity (Khoury et al., 2021; Kornfield et al., 2021; J. Liu et al., 2021; Mollard et al., 2021). In the study by J. Liu et al. (2021), a greater percentage of non-Hispanic White women (60.4%) reported symptoms of depression compared with Hispanic (44.8%), non-Hispanic Black (14.0%), or non-Hispanic other (32.7%) participants. Conversely, Black, Indigenous, or other women of color were more likely to report stress symptoms than White women (Mollard et al., 2021). Kornfield et al. (2021) assessed postpartum depression risk and found no significant difference between Black and White participants. Finally, the results of Khoury et al. (2021) results indicated an association between race and symptoms of anxiety and depression, without any further detail.
Discussion
In our scoping review, we mapped the racial and ethnic representation of participants in perinatal mental health studies conducted during the COVID-19 pandemic. Our findings indicate that very few Black, Indigenous, or other people of color (23.5%) participated in these pandemic studies. The stigma that is associated with mental health issues among African American (Ward et al., 2013), American Indian/Alaska Native (Grandbois, 2005), Asian American (Goyal et al., 2015; Han et al., 2020; Ta Park et al., 2017, 2019), and Hispanic individuals (Benuto et al., 2019) may account for the lower numbers of participants of color. Moreover, the fear, distrust (George et al., 2014), and historical misconduct associated with the Tuskegee study (Shavers et al., 2000) may be related to the low percentage of Black or African American participants (8.9%). On a more practical level, during the pandemic, women of color were more likely to be classified as essential workers (Pope et al., 2021; Rogers et al., 2020) and faced unemployment if they did not continue to work (Pew Research Center, 2020), which may have left women without the time or desire to participate in research.
Researchers’ implicit bias during study design and data reporting phases may also contribute to the underrepresentation of women of color. Most of the studies in our review used cross-sectional designs (n =15, 60%) and incorporated social media platforms to recruit participants (n = 19, 76%), which may be a problem, given that Facebook and Instagram are used more frequently by individuals with higher income levels (Pew Research Center, 2021). Researchers should consider using other social media platforms that attract younger and lower-income individuals, such as TikTok, to recruit a more diverse sample (Pew Research Center, 2021).
To increase the participation of women of color in research, culturally sensitive recruitment strategies should be used and effort should be made to develop trusting relationships within diverse communities.
The articles in our review reported racial and ethnic categories outlined by the Office of Management and Budget (1997): White, Black or African American, Latino or Hispanic, Asian American, Native Hawaiian and Pacific Islander, and American Indian and Alaska Native. The use of these broad racial and ethnic categories fails to accurately describe every participant and perpetuates the misrepresentation of many. Although more than 75% of the population in the United States and Canada self-identifies as White (Statistics Canada, 2022; U.S. Census Bureau, 2021a), it is important to note that the category “White” may include persons from Western/Eastern Europe, North Africa, or the Middle East. This may promote the misrepresentation of large groups of people with different experiences, cultures, and histories (Kauh et al., 2021). Misrepresentation also occurs when other broad racial and ethnic categories, such as Black, Asian, and Hispanic/Latino, are used to classify study participants (Kauh et al., 2021).
To ensure accurate representation in prospective research studies, participants should self-identify their racial and ethnic identity (Ross et al., 2020). Updated guidance on the reporting of race and ethnicity in medical and science journals suggests that researchers should collect specific racial and ethnic categories versus broad terms and describe how racial and ethnic data were collected (e.g., self-report, electronic health record; Flanagin et al., 2021). American Indian and Alaska Native individuals accounted for 0.1% of the participants in our review, which may be due to misrepresentation. Researchers should consider best practices for American Indian and Alaska Native data collection recommendations, including allowing participants to report multiple races to accurately represent all American Indian and Alaska Native individuals (Urban Indian Health Institute, 2022).
Limitations
The purpose of our review methodology (Arksey & O’Malley, 2005) was to rapidly map key concepts in a research area, and we did not include a quality appraisal of the included articles, so the rigor and potential biases of the included studies are unknown. Our review was limited to English language articles with samples from the United States or Canada. Sampling bias and limitations inherent in the primarily descriptive, quantitative, and cross-sectional designs of the studies included in the review may also be reasons for inadequate racial and ethnic representation.
Conclusion
Based on our review, we conclude that the majority of women who participated in studies about mental health while pregnant or in the postpartum period during the COVID-19 pandemic were White. Our findings call for urgent action from researchers to make a targeted effort to recruit participants that reflect population demographics. Furthermore, researchers must use standard methods of reporting race and ethnicity (Flanagin et al., 2021) to shed light on how public health crises such as COVID-19 affect the mental health of pregnant and postpartum women of color. Additional recommendations to increase the participation of women of color in future research studies include building a diverse research team, developing culturally sensitive recruitment materials, and identifying key community contacts (Shavers et al., 2002; Webber-Ritchey et al., 2021).
Acknowledgments
Conflict of Interest
The authors report no conflicts of interest or relevant financial relationships.
Funding
Funded by the San Jose State University Research, Scholarship, and Creative Activity assigned time program.
Biographies
Deepika Goyal, PhD, MS, FNP-C, is a professor in the Valley Foundation School of Nursing, San José State University, San Jose, CA.
Justine Dol, PhD, is a postdoctoral fellow, St Michael’s Hospital, Toronto, Canada.
Madeline Leckey, is an MSc student, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, Canada.
Sarah Naraine, is an MSc student, Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, Canada.
Cindy-Lee Dennis, PhD, is a professor in the Lawrence S. Bloomberg Faculty of Nursing, University of Toronto, Toronto, Canada; Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, Canada; and Department of Psychiatry, University of Toronto, Toronto, Canada.
Emily K. Chan, is the Associate Dean for Research & Scholarship, Dr. Martin Luther King, Jr. Library, San José State University, San Jose, CA.
Geetali Basu, is an academic liaison librarian, San José State University, Dr. Martin Luther King, Jr. Library, San Jose, CA.
Footnotes
Note: To access the supplementary material that accompanies this article, visit the online version of the Journal of Obstetric, Gynecologic, & Neonatal Nursing at http://jognn.org and at https://doi.org/10.1016/j.jogn.2022.11.003.
Supplementary Material
Supplementary Tables S1 and S2
References
- Ahlers-Schmidt C.R., Hervey A.M., Neil T., Kuhlmann S., Kuhlmann Z. Concerns of women regarding pregnancy and childbirth during the COVID-19 pandemic. Patient Education and Counseling. 2020;103(12):2578–2582. doi: 10.1016/j.pec.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajayi K.V., Harvey I.S., Panjwani S., Uwak I., Garney W., Page R.L. Narrative analysis of childbearing experiences during the COVID-19 pandemic. MCN. The American Journal of Maternal/Child Nursing. 2021;46(5):284–292. doi: 10.1097/nmc.0000000000000742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson M.R., Salisbury A.L., Uebelacker L.A., Abrantes A.M., Battle C.L. Stress, coping and silver linings: How depressed perinatal women experienced the COVID-19 pandemic. Journal of Affective Disorders. 2022;298(2022):329–336. doi: 10.1016/j.jad.2021.10.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arksey H., O’Malley L. Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology. 2005;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- Barbosa-Leiker C., Smith C.L., Crespi E.J., Brooks O., Burduli E., Ranjo S., Gartstein M.A. Stressors, coping, and resources needed during the COVID-19 pandemic in a sample of perinatal women. BMC Pregnancy Childbirth. 2021;21(1) doi: 10.1186/s12884-021-03665-0. Article 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basu A., Kim H.H., Basaldua R., Choi K.W., Charron L., Kelsall N., Koenen K.C. A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLOS ONE. 2021;16(4) doi: 10.1371/journal.pone.0249780. Article e0249780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauman B.L., Ko J.Y., Cox S., D’Angelo D.V., Warner L., Folger S., Barfield W.D. Vital signs: Postpartum depressive symptoms and provider discussions about perinatal depression—United States, 2018. MMWR. Morbidity and Mortality Weekly Report. 2020;69(19):575–581. doi: 10.15585/mmwr.mm6919a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benuto L.T., Gonzalez F., Reinosa-Segovia F., Duckworth M. Mental health literacy, stigma, and behavioral health service use: The case of Latinx and non-Latinx Whites. Journal of Racial and Ethnic Health Disparities. 2019;6(6):1122–1130. doi: 10.1007/s40615-019-00614-8. [DOI] [PubMed] [Google Scholar]
- Breman R.B., Neerland C., Bradley D., Burgess A., Barr E., Burcher P. Giving birth during the COVID-19 pandemic, perspectives from a sample of the United States birthing persons during the first wave: March–June 2020. Birth. 2021;48(4):524–533. doi: 10.1111/birt.12559. [DOI] [PubMed] [Google Scholar]
- Burgess A., Breman R.B., Roane L.A., Dada S., Bradley D., Burcher P. Impact of COVID-19 on pregnancy worry in the United States. Birth. 2022;49(3):420–429. doi: 10.1111/birt.12608. [DOI] [PubMed] [Google Scholar]
- Claridge A.M., Beeson T., Wojtyna A., Hoxmeier J. Pregnant women’s experiences during the COVID-19 pandemic: A mixed method exploration of prenatal depression. Couple and Family Psychology. 2021;10(3):168–178. doi: 10.1037/cfp0000178. [DOI] [Google Scholar]
- Covidence systematic review software (n. d.), Veritas Health Innovation, Melbourne, Australia. Available at www.covidence.org.
- Daoud N., O’Brien K., O’Campo P., Harney S., Harney E., Bebee K., Smylie J. Postpartum depression prevalence and risk factors among Indigenous, non-Indigenous and immigrant women in Canada. Canadian Journal of Public Health. 2019;110(4):440–452. doi: 10.17269/s41997-019-00182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farewell C.V., Jewell J., Walls J., Leiferman J.A. A mixed-methods pilot study of perinatal risk and resilience during COVID-19. Journal of Primary Care & Community Health. 2020;11 doi: 10.1177/2150132720944074. Article 2150132720944074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flanagin A., Frey T., Christiansen S.L. Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA. 2021;326(7):621–627. doi: 10.1001/jama.2021.13304. [DOI] [PubMed] [Google Scholar]
- Gavin N.I., Gaynes B.N., Lohr K.N., Meltzer-Brody S., Gartlehner G., Swinson T. Perinatal depression: A systematic review of prevalence and incidence. Obstetrics & Gynecology. 2005;106(5 Pt. 1):1071–1083. doi: 10.1097/01.AOG.0000183597.31630.db. [DOI] [PubMed] [Google Scholar]
- George S., Duran N., Norris K. A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health. 2014;104(2):e16–e31. doi: 10.2105/AJPH.2013.301706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gheorghe M., Varin M., Wong S.L., Baker M., Grywacheski V., Orpana H. Symptoms of postpartum anxiety and depression among women in Canada: Findings from a national cross-sectional survey. Canadian Journal of Public Health. 2021;112(2):244–252. doi: 10.17269/s41997-020-00420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D., Beck C.T., Webb R., Ayers S. Postpartum depressive symptoms and experiences during COVID-19. MCN. The American Journal of Maternal/Child Nursing. 2021;47(2):77–84. doi: 10.1097/nmc.0000000000000802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D., De La Rosa L., Mittal L., Erdei C., Liu C.H. Unmet prenatal expectations during the COVID-19 pandemic. MCN. The American Journal of Maternal/Child Nursing. 2021;47(2):66–70. doi: 10.1097/nmc.0000000000000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D., Han M., Feldman-Schwartz T., Le H.N. Perinatal experiences of Asian American women during COVID-19. MCN. The American Journal of Maternal/Child Nursing. 2021;47(2):71–76. doi: 10.1097/nmc.0000000000000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D., Park V.T., McNiesh S. Postpartum depression among Asian Indian mothers. MCN. The American Journal of Maternal/Child Nursing. 2015;40(4):256–261. doi: 10.1097/nmc.0000000000000146. [DOI] [PubMed] [Google Scholar]
- Grandbois D. Stigma of mental illness among American Indian and Alaska Native nations: Historical and contemporary perspectives. Issues in Mental Health Nursing. 2005;26(10):1001–1024. doi: 10.1080/01612840500280661. [DOI] [PubMed] [Google Scholar]
- Groulx T., Bagshawe M., Giesbrecht G., Tomfohr-Madsen L., Hetherington E., Lebel C.A. Prenatal care disruptions and associations with maternal mental health during the COVID-19 pandemic. Frontiers in Global Women’s Health. 2021;2 doi: 10.3389/fgwh.2021.648428. Article 648428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han M., Goyal D., Lee J., Cho H., Kim A. Korean immigrant women’s postpartum experiences in the United States. MCN. The American Journal of Maternal/Child Nursing. 2020;45(1):42–48. doi: 10.1097/NMC.0000000000000585. [DOI] [PubMed] [Google Scholar]
- Harris L.M., Forson-Dare Z., Gallagher P.G. Critical disparities in perinatal health: Understanding risks and changing the outcomes. Journal of Perinatology. 2021;41(2):181–182. doi: 10.1038/s41372-020-00913-7. [DOI] [PubMed] [Google Scholar]
- Hetherington E., McDonald S., Williamson T., Tough S. Trajectories of social support in pregnancy and early postpartum: Findings from the all our families cohort. Social Psychiatry and Psychiatric Epidemiology. 2020;55(2):259–267. doi: 10.1007/s00127-019-01740-8. [DOI] [PubMed] [Google Scholar]
- Howell E.A. Reducing disparities in severe maternal morbidity and mortality. Clinical Obstetrics and Gynecology. 2018;61(2):387–399. doi: 10.1097/grf.0000000000000349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huggins B., Jones C., Adeyinka O., Ofomata A., Drake C., Kondas C. Racial disparities in perinatal mental health. Psychiatric Annals. 2020;50(11):489–493. doi: 10.3928/00485713-20201007-02. [DOI] [Google Scholar]
- Iyengar U., Jaiprakash B., Haitsuka H., Kim S. One year into the pandemic: A systematic review of perinatal mental health outcomes during COVID-19. Frontiers in Psychiatry. 2021;12 doi: 10.3389/fpsyt.2021.674194. Article 674194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janevic T., Maru S., Nowlin S., McCarthy K., Bergink V., Stone J., Howell E.A. Pandemic birthing: Childbirth satisfaction, perceived health care bias, and postpartum health during the COVID-19 pandemic. Maternal Child Health. 2021;25(6):860–869. doi: 10.1007/s10995-021-03158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joy P., Aston M., Price S., Sim M., Ollivier R., Benoit B., Iduye D. Blessings and curses: Exploring the experiences of new mothers during the COVID-19 pandemic. Nursing Reports. 2020;10(2):207–219. doi: 10.3390/nursrep10020023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karasek D., Baer R.J., McLemore M.R., Bell A.J., Blebu B.E., Casey J.A., Jelliffe-Pawlowski L.L. The association of COVID-19 infection in pregnancy with preterm birth: A retrospective cohort study in California. Lancet Regional Health. Americas. 2021;2 doi: 10.1016/j.lana.2021.100027. Article 100027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kauh T.J., Read J.G., Scheitler A.J. The critical role of racial/ethnic data disaggregation for health equity. Population Research and Policy Review. 2021;40(1):1–7. doi: 10.1007/s11113-020-09631-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendig S., Keats J.P., Hoffman M.C., Kay L.B., Miller E.S., Simas T.A.M., Lemieux L.A. Consensus bundle on maternal mental health: Perinatal depression and anxiety. Journal of Midwifery Women’s Health. 2017;62(2):232–239. doi: 10.1111/jmwh.12603. [DOI] [PubMed] [Google Scholar]
- Khoury J.E., Atkinson L., Bennett T., Jack S.M., Gonzalez A. COVID-19 and mental health during pregnancy: The importance of cognitive appraisal and social support. Journal of Affective Disorders. 2021;282:1161–1169. doi: 10.1016/j.jad.2021.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinser P.A., Jallo N., Amstadter A.B., Thacker L.R., Jones E., Moyer S., Salisbury A.L. Depression, anxiety, resilience, and coping: The experience of pregnant and new mothers during the first few months of the COVID-19 pandemic. Journal of Women’s Health. 2021;30(5):654–664. doi: 10.1089/jwh.2020.8866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko J.Y., Rockhill K.M., Tong V.T., Morrow B., Farr S.L. Trends in postpartum depressive symptoms—27 states, 2004, 2008, and 2012. MMWR. Morbidity and Mortality Weekly Report. 2017;66(6):153–158. doi: 10.15585/mmwr.mm6606a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornfield S.L., White L.K., Waller R., Njoroge W., Barzilay R., Chaiyachati B.H., Gur R.E. Risk and resilience factors influencing postpartum depression and mother-infant bonding during COVID-19. Health Affairs. 2021;40(10):1566–1574. doi: 10.1377/hlthaff.2021.00803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotlar B., Gerson E., Petrillo S., Langer A., Tiemeier H. The impact of the COVID-19 pandemic on maternal and perinatal health: A scoping review. Reproductive Health. 2021;18(1) doi: 10.1186/s12978-021-01070-6. Article 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kozhimannil K.B., Interrante J.D., Tofte A.N., Admon L.K. Severe maternal morbidity and mortality among Indigenous women in the United States. Obstetrics & Gynecology. 2020;135(2):294–300. doi: 10.1097/AOG.0000000000003647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giesbrecht G. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. Journal of Affective Disorders. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee E.K., Parolin Z. The care burden during COVID-19: A national database of child care closures in the United States. Socius. 2021;7 Article 23780231211032028. [Google Scholar]
- Liu C.H., Erdei C., Mittal L. Risk factors for depression, anxiety, and PTSD symptoms in perinatal women during the COVID-19 Pandemic. Psychiatry Research. 2021;295 doi: 10.1016/j.psychres.2020.113552. Article 113552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Goyal D., Mittal L., Erdei C. Patient satisfaction with virtual-based prenatal care: Implications after the COVID-19 pandemic. Maternal and Child Health Journal. 2021;25:1735–1743. doi: 10.1007/s10995-021-03211-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Hyun S., Erdei C., Mittal L. Prenatal distress during the COVID-19 pandemic: Clinical and research implications. Archives of Gynecology and Obstetrics. 2021;306(2):397–405. doi: 10.1007/s00404-021-06286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Koire A., Erdei C., Mittal L. Unexpected changes in birth experiences during the COVID-19 pandemic: Implications for maternal mental health. Archives of Gynecology and Obstetrics. 2022;306(3):687–697. doi: 10.1007/s00404-021-06310-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu J., Hung P., Alberg A.J., Hair N.L., Whitaker K.M., Simon J., Taylor S.K. Mental health among pregnant women with COVID-19–related stressors and worries in the United States. Birth. 2021;48(4):470–479. doi: 10.1111/birt.12554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Masters G.A., Asipenko E., Bergman A.L., Person S.D., Brenckle L., Moore Simas T.A., Byatt N. Impact of the COVID-19 pandemic on mental health, access to care, and health disparities in the perinatal period. Journal of Psychiatric Research. 2021;137:126–130. doi: 10.1016/j.jpsychires.2021.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthews K., Morgan I., Davis K., Estriplet T., Perez S., Crear-Perry J.A. Pathways to equitable and antiracist maternal mental health care: Insights from Black women stakeholders. Health Affairs. 2021;40(10):1597–1604. doi: 10.1377/hlthaff.2021.00808. [DOI] [PubMed] [Google Scholar]
- McCall-Hosenfeld J.S., Phiri K., Schaefer E., Zhu J., Kjerulff K. Trajectories of depressive symptoms throughout the peri- and postpartum period: Results from the first baby study. Journal of Women’s Health. 2016;25(11):1112–1121. doi: 10.1089/jwh.2015.5310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillan I.F., Armstrong L.M., Langhinrichsen-Rohling J. Transitioning to parenthood during the pandemic: COVID-19 related stressors and first-time expectant mothers’ mental health. Couple and Family Psychology. 2021;10(3):179–189. doi: 10.1037/cfp0000174. [DOI] [Google Scholar]
- Miller E.S., Saade G.R., Simhan H.N., Monk C., Haas D.M., Silver R.M., Grobman W.A. Trajectories of antenatal depression and adverse pregnancy outcomes. American Journal of Obstetrics and Gynecology. 2022;226(1):108.e1–108.e9. doi: 10.1016/j.ajog.2021.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollard E., Kupzyk K., Moore T. Postpartum stress and protective factors in women who gave birth in the United States during the COVID-19 pandemic. Women’s Health. 2021;17 doi: 10.1177/17455065211042190. Article 17455065211042190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morency J.-D., Malenfant É.C., MacIsaac S. Immigration and diversity: Population projections for Canada and its regions, 2011 to 2036. Statistics Canada. 2017, January 25. https://www150.statcan.gc.ca/n1/pub/91-551-x/91-551-x2017001-eng.htm
- Moyer C.A., Compton S.D., Kaselitz E., Muzik M. Pregnancy-related anxiety during COVID-19: A nationwide survey of 2740 pregnant women. Archives of Women’s Mental Health. 2020;23(6):757–765. doi: 10.1007/s00737-020-01073-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukherjee S., Trepka M.J., Pierre-Victor D., Bahelah R., Avent T. Racial/ethnic disparities in antenatal depression in the United States: A systematic review. Maternal and Child Health Journal. 2016;20(9):1780–1797. doi: 10.1007/s10995-016-1989-x. [DOI] [PubMed] [Google Scholar]
- Office of Management and Budget Revisions to the standards for the classification of federal data on race and ethnicity. Federal Register. 1997. https://www.govinfo.gov/content/pkg/FR-1997-10-30/pdf/97-28653.pdf
- Ollivier R., Aston D.M., Price D.S., Sim D.M., Benoit D.B., Joy D.P., Nassaji N.A. Mental health & parental concerns during COVID-19: The experiences of new mothers amidst social isolation. Midwifery. 2021;94 doi: 10.1016/j.midw.2020.102902. Article 102902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Omowale S.S., Casas A., Lai Y.-H., Sanders S.A., Hill A.V., Wallace M.L., Mendez D.D. Trends in stress throughout pregnancy and postpartum period during the COVID-19 pandemic: Longitudinal study using ecological momentary assessment and data from the postpartum mothers mobile study. JMIR Mental Health. 2021;8(9) doi: 10.2196/30422. Article e30422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perzow S.E.D., Hennessey E.-M.P., Hoffman M.C., Grote N.K., Davis E.P., Hankin B.L. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. Journal of Affective Disorders Reports. 2021;4 doi: 10.1016/j.jadr.2021.100123. Article 100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center Unemployment rate is higher than officially recorded, more so for women and certain other groups. 2020. https://www.pewresearch.org/fact-tank/2020/06/30/unemployment-rate-is-higher-than-officially-recorded-more-so-for-women-and-certain-other-groups/ June 30.
- Pew Research Center Social media fact sheet. 2021, April 7. https://www.pewresearch.org/internet/fact-sheet/social-media/
- Pope R., Ganesh P., Miracle J., Brazile R., Wolfe H., Rose J., Gullett H. Structural racism and risk of SARS-CoV-2 in pregnancy. EClinicalMedicine. 2021;37 doi: 10.1016/j.eclinm.2021.100950. Article 100950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers T.N., Rogers C.R., VanSant-Webb E., Gu L.Y., Yan B., Qeadan F. Racial disparities in COVID-19 mortality among essential workers in the United States. World Medical & Health Policy. 2020;12(3):311–327. doi: 10.1002/wmh3.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross P.T., Hart-Johnson T., Santen S.A., Zaidi N.L.B. Considerations for using race and ethnicity as quantitative variables in medical education research. Perspectives on Medical Education. 2020;9(5):318–323. doi: 10.1007/s40037-020-00602-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers V.L., Lynch C.F., Burmeister L.F. Knowledge of the Tuskegee study and its impact on the willingness to participate in medical research studies. Journal of the National Medical Association. 2000;92(12):563–572. [PMC free article] [PubMed] [Google Scholar]
- Shavers V.L., Lynch C.F., Burmeister L.F. Racial differences in factors that influence the willingness to participate in medical research studies. Annals of Epidemiology. 2002;12(4):248–256. doi: 10.1016/s1047-2797(01)00265-4. [DOI] [PubMed] [Google Scholar]
- Shuman C.J., Morgan M.E., Pareddy N., Chiangong J., Veliz P., Peahl A., Dalton V. Associations among postpartum posttraumatic stress disorder symptoms and COVID-19 pandemic-related stressors. Journal of Midwifery & Women’s Health. 2022;67(5):626–634. doi: 10.1111/jmwh.13399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman M.E., Burgos L., Rodriguez Z.I., Afzal O., Kalishman A., Callipari F., Loudon H. Postpartum mood among universally screened high and low socioeconomic status patients during COVID-19 social restrictions in New York City. Scientific Reports. 2020;10(1) doi: 10.1038/s41598-020-79564-9. Article 22380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman M.E., Medeiros C., Burgos L. Early pregnancy mood before and during COVID-19 community restrictions among women of low socioeconomic status in New York City: A preliminary study. Archives of Women’s Mental Health. 2020;23(6):779–782. doi: 10.1007/s00737-020-01061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soffer M.D., Adams Z.M., Chen Y.S., Fox N.S. Risk factors for positive postpartum depression screen in women with private health insurance and access to care. Journal of Maternal-Fetal & Neonatal Medicine. 2019;32(24):4154–4158. doi: 10.1080/14767058.2018.1484096. [DOI] [PubMed] [Google Scholar]
- Statistics Canada Maternal mental health in Canada, 2018/2019. 2019, June 24. https://www150.statcan.gc.ca/n1/daily-quotidien/190624/dq190624b-eng.htm
- Statistics Canada Visible minority of a person. 2021, January 11. https://www23.statcan.gc.ca/imdb/p3Var.pl?Function=DEC&Id=45152
- Statistics Canada Census profile, 2021 census of population. 2022, February 9. https://www12.statcan.gc.ca/census-recensement/2021/dp-pd/prof/index.cfm?Lang=E
- Suwalska J., Napierała M., Bogdański P., Łojko D., Wszołek K., Suchowiak S., Suwalska A. Perinatal mental health during COVID-19 pandemic: An integrative review and implications for clinical practice. Journal of Clinical Medicine. 2021;10(11) doi: 10.3390/jcm10112406. Article 2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ta Park V.M., Goyal D., Nguyen T., Lien H., Rosidi D. Postpartum traditions, mental health, and help-seeking considerations among Vietnamese American women: A mixed-methods pilot study. Journal of Behavioral Health Services Research. 2017;44(3):428–441. doi: 10.1007/s11414-015-9476-5. [DOI] [PubMed] [Google Scholar]
- Ta Park V.M., Goyal D., Suen J., Win N., Tsoh J. Chinese American women’s experiences with postpartum depressive symptoms and mental health help-seeking behaviors. MCN. The American Journal of Maternal/Child Nursing. 2019;44(3):150–156. doi: 10.1097/NMC.0000000000000518. [DOI] [PubMed] [Google Scholar]
- Taylor J.K. Structural racism and maternal health among Black women. Journal of Law, Medicine & Ethics. 2020;48(3):506–517. doi: 10.1177/1073110520958875. [DOI] [PubMed] [Google Scholar]
- Tricco A.C., Lillie E., Zarin W., O’Brien K., Colquhoun H., Kastner M., Straus S.E. A scoping review on the conduct and reporting of scoping reviews. BMC Medical Research Methodology. 2016;16(1) doi: 10.1186/s12874-016-0116-4. Article 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urban Indian Health Institute Best practices for American Indian and Alaska Native data collection. 2022, August 6. https://aipi.asu.edu/sites/default/files/best-practices-for-american-indian-and-alaska-native-data-collection.pdf
- U.S. Census Bureau Quick facts: United States. 2021. https://www.census.gov/quickfacts/fact/table/US/PST045219
- U.S. Census Bureau 2020 U.S. population more racially and ethnically diverse than measured in 2010. 2021. https://www.census.gov/library/stories/2021/08/2020-united-states-population-more-racially-ethnically-diverse-than-2010.html
- Ward E.C., Wiltshire J.C., Detry M.A., Brown R.L. African American men and women’s attitude toward mental illness, perceptions of stigma, and preferred coping behaviors. Nursing Research. 2013;62(3):185–194. doi: 10.1097/NNR.0b013e31827bf533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webber-Ritchey K.J., Aquino E., Ponder T.N., Lattner C., Soco C., Spurlark R., Simonovich S.D. Recruitment strategies to optimize participation by diverse populations. Nursing Science Quarterly. 2021;34(3):235–243. doi: 10.1177/08943184211010471. [DOI] [PubMed] [Google Scholar]
- Wheeler J.M., Misra D.P., Giurgescu C. Stress and coping among pregnant Black women during the COVID-19 pandemic. Public Health Nursing. 2021;38(4):596–602. doi: 10.1111/phn.12909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner K.L., Sit D.K., McShea M.C., Rizzo D.M., Zoretich R.A., Hughes C.L., Hanusa B.H. Onset timing, thoughts of self-harm, and diagnoses in postpartum women with screen-positive depression findings. JAMA Psychiatry. 2013;70(5):490–498. doi: 10.1001/jamapsychiatry.2013.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan H., Ding Y., Guo W. Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: A systematic review and meta-analysis. Frontiers in Psychology. 2020;11 doi: 10.3389/fpsyg.2020.617001. Article 617001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yildiz P.D., Ayers S., Phillips L. The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. Journal of Affective Disorders. 2017;208:634–645. doi: 10.1016/j.jad.2016.10.009. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Tables S1 and S2