Abstract
Context:
The Centers for Disease Control and Prevention (CDC) recommends that all persons aged 13-64 years are tested for HIV. However, results from U.S. surveys show that ≤ 50% of persons had ever tested for HIV.
Program:
CDC annually funds 60 health departments to conduct comprehensive HIV prevention and surveillance activities that include HIV testing.
Implementation:
We selected the 31 health departments with quality data (i.e., ≤ 20% missing or invalid values for variables to verify linkage to HIV medical care and new HIV diagnoses) in 2019. Main outcomes were new HIV diagnoses, linkage, and PrEP awareness and referrals. We used SAS® 9.4 to conduct descriptive, Chi-square, and multivariate regression analyses. Our objectives were to determine outcomes and characteristics of persons in non-healthcare settings who tested for HIV for the first time.
Evaluation:
Compared with persons who previously tested for HIV, persons who tested for the first time were more likely to be aged 13-29 years than aged >= 30 years, (62.0% [24 295/39 192] vs 42.1% [61 911/147 087], p<.0001) and have a higher percentage of new HIV diagnoses (0.6% [242/39 320] vs 0.5% [667/147 475], p<.0001). Among persons who tested for the first time, overall percentages of linkage, PrEP awareness, and PrEP referral were 73.4%, 33.3%, and 30.8%, respectively. Compared with referent groups, persons who tested for the first time in the South and had a new HIV diagnosis were less likely to be linked (aPR=0.72, 95% CI [0.59-0.89]); persons who inject drugs were less likely to be aware of PrEP (aPR=0.84, 95% CI [0.77-0.91]); and persons in the Northeast were less likely to receive PrEP referrals (aPR=0.28, 95% CI [0.26–0.31]).
Discussion:
Non-healthcare sites should consider increasing HIV testing, PrEP awareness, and prompt referrals to PrEP and HIV treatment services for persons who have never previously tested.
Keywords: Persons who test for HIV for the first time, linkage to medical care, pre-exposure prophylaxis
Introduction
In the United States, the estimated number of new human immunodeficiency virus (HIV) infections among adults/adolescents in 2019 was 34 800.1 Of the estimated 1.2 million adults/adolescents with HIV in 2019, 13% were unaware of their infection,1 yet likely accounted for more than one-third of all new infections,2 and 19% of persons with diagnosed HIV infection were not linked to HIV medical care within 30 days of their diagnosis.3 Although pre-exposure prophylaxis (PrEP), medicine taken to prevent acquisition of HIV, is an effective strategy to prevent HIV infection,4 only 23% of the estimated 1.2 million persons aged ≥ 16 years with indications for PrEP were prescribed PrEP in 2019.3
HIV testing is a foundation of the National HIV/AIDS Strategy to end the HIV epidemic in the United States,5 which includes a status neutral approach to HIV services. This approach uses HIV testing as the entry point of prevention and treatment services and engages a person with assistance, regardless of whether test results are positive or negative. For example, diagnosing HIV in persons who are unaware of their infection allows them to promptly receive medical care,6 because treatment of persons with HIV is recommended as soon as possible after infection. Testing persons at high risk for HIV acquisition, but not infected with HIV, allows them to receive HIV prevention services (e.g., PrEP) and remain uninfected. Objectives of the National HIV/AIDS Strategy by 2025 include increased HIV testing, 95% linkage to HIV medical care within 30 days after an HIV diagnosis, and 50% PrEP use by eligible persons.
The Centers for Disease Control and Prevention (CDC) recommends that all persons aged 13-64 years are tested for HIV at least once and that persons who are at high risk for HIV acquisition are tested at least annually.7 However, results from nationally representative U.S. surveys show that the percentage of persons who had ever tested for HIV was 44%-50% among persons at least 18 years old8,9 and 32%-34% among persons aged 18 to 24 years.9,10 Among studies that documented reasons for having never tested, the most common reasons were low HIV risk perception, fear of knowing that they were infected, and not having been offered an HIV test.11-13 Factors associated with never having been tested among gay, bisexual, and other men who have sex with men (collectively referred to as MSM) included younger age, use of a social network strategy, and a higher rate of HIV infection,14 and lower education, greater internalized homophobia, and a higher rate of HIV infection.12
CDC annually funds health departments to conduct comprehensive HIV prevention and surveillance activities that include HIV testing in healthcare and non-healthcare settings. In 2018, for the first time, CDC combined prevention and surveillance activities into one Funding Opportunity Announcement (referred to hereafter as PS18-1802) to increase collaboration and integration of these activities and to improve data quality.15 Although most HIV tests funded by PS18-1802 occur in healthcare settings, HIV positivity is higher in non-health care settings,16 thus persons who visit non-healthcare settings may be in more need of HIV services. HIV testing is important in non-healthcare settings, because persons at increased risk for HIV acquisition may not regularly access healthcare services where HIV testing is routinely conducted.17 We analyzed the CDC National HIV Prevention Program Monitoring and Evaluation (NHM&E) data from PS18-1802. Our objectives were to determine outcomes and characteristics of persons in non-healthcare settings who had never previously tested for HIV, but were being tested for the first time, particularly among those who were newly diagnosed with HIV infection, linked to HIV medical care, were aware of PrEP, and received PrEP referrals.
Methods
Data source:
This analysis uses NHM&E HIV testing data submitted to CDC as of March 15, 2021 by 60 health departments funded under PS18-1802 (i.e., 50 states, the District of Columbia, Puerto Rico, the U.S. Virgin Islands, and 7 Metropolitan Statistical Areas [Baltimore City, Chicago, Houston, Los Angeles, New York City, Philadelphia, and San Francisco]) for HIV tests conducted during January 1-December 31, 2019. Biannually, health departments electronically reported de-identified data to CDC through the NHM&E data system.
Criteria for selection of health departments:
PS18-1802 requires health departments to have complete, timely, and quality HIV prevention data. The PS18-1802 performance target for data completeness is that at least 80% of HIV-positive test records have all required fields and pass standard data edit checks for linkage to HIV medical care within 30 days after diagnosis and at least 80% of new diagnoses verified in a local HIV surveillance or other data system. To help ensure that performance targets are achieved, CDC applies standardized data cleaning and processing rules to NHM&E data. CDC then provides data quality feedback to health departments and requests that data quality is improved for records with missing or invalid data and when funding performance targets are not met (e.g., 85% of persons with newly diagnosed HIV who are linked to HIV medical care within 30 days after diagnosis).
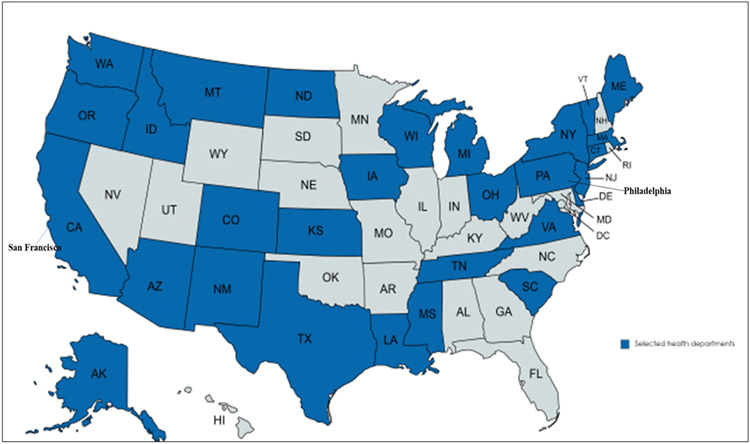
For this analysis, we selected health departments that met the PS18-1802 data completeness target (i.e., ≤ 20% missing or invalid values for variables to verify new HIV diagnoses and linkage to medical care, which includes checking local HIV surveillance and other databases to confirm the lack of a previous HIV diagnosis). Based on these criteria, we selected 31 health departments (Alaska, Arizona, California [excluding Los Angeles County and San Francisco], Colorado, Connecticut, Delaware, Idaho, Iowa, Kansas, Louisiana, Maine, Massachusetts, Michigan, Mississippi, Montana, New Jersey, New Mexico, New York State [excluding New York City], North Dakota, Ohio, Oregon, Pennsylvania [excluding Philadelphia], South Carolina, Tennessee, Texas [excluding Houston], Vermont, Virginia, Washington, Wisconsin, San Francisco, and Philadelphia)(Figure 1), which accounted for 39% (208 373/533 192) of all NHM&E tests conducted in non-health care settings in 2019. Completeness of variables used to verify new HIV diagnoses and linkage to care was 99% (3 622/3 672) and 91% (6 579/7 203), respectively. For all analyses, we excluded missing data depending on the requirements of a specific analysis (e.g., excluded records with an unknown age when calculating an age-specific outcome, excluded records with unknown PrEP eligibility when calculating the percentage of eligible persons who received a PrEP referral).
Figure 1. Map of the United States - Geographical distribution of the health departments selected for analysis of HIV testing among first time testers, 31 health departments, United States, 2019*.
*The selected health departments highlighted in blue on the map met the PS18-1802 data completeness target (i.e., ≤ 20% missing or invalid values for variables to verify linkage to medical care and new HIV diagnoses, which includes checking local HIV surveillance and other databases to confirm the lack of a previous HIV diagnosis). Following are health departments selected for the analysis: Alaska, Arizona, California [excluding Los Angeles County and San Francisco], Colorado, Connecticut, Delaware, Idaho, Iowa, Kansas, Louisiana, Maine, Massachusetts, Michigan, Mississippi, Montana, New Jersey, New Mexico, New York State [excluding New York City], North Dakota, Ohio, Oregon, Pennsylvania [excluding Philadelphia], South Carolina, Tennessee, Texas [excluding Houston], Vermont, Virginia, Washington, Wisconsin, San Francisco, and Philadelphia.
Measures:
Demographic characteristics.
We determined age at test by calculating the difference between the year of birth and year of the HIV test and grouped persons into ages 13 to 29 years, 30 to 49 years, and ≥ 50 years. We created the gender variable by combining the reported sex assigned at birth and self-reported current gender identity and categorized persons as male, female, transgender (i.e., sex assigned at birth female and those who identify as female-to-male transgender, or sex assigned at birth male and those who identify as male-to-female transgender, or reported a current gender that is different from the sex assigned at birth. We created the race and ethnicity variable by combining self-reported race and ethnicity (i.e., Hispanic or Latino) and categorized persons as Hispanic/Latino (of any race), non-Hispanic/Latino Black or African American (Black), non-Hispanic/Latino White, or other (includes non-Hispanic/Latino persons who are American Indian or Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, and of multiple races). We defined region as the location of the health department grouped into one of the four geographic areas that are designated by the U.S. Census Bureau.
Population groups.
Data on behavioral risk characteristics are determined for the five years prior to the HIV test. MSM includes males who reported male–to–male sexual contact. MSM who inject drugs includes males who reported both male-to-male sexual contact and injection drug use. Persons who inject drugs (PWID) includes persons who reported injection drug use. Heterosexual males include males who reported having sex only with a female, and heterosexual females include females who reported having sex only with a male.
HIV tests and testing status.
For our analysis, a test result represents the final determination of testing (e.g., positive or negative) for a person as part of a testing event that might have included multiple tests (e.g., a preliminary test followed by a confirmatory test) or only a single test. Valid tests are test records with confirmed results, excluding discordant and indeterminate results. A person who tested for the first-time was a person who indicated that they were not previously tested before the current test, excluding a client who reported a prior positive test from a different variable in the dataset and excluding a client with a previous positive result from a check of a local HIV surveillance or other database after a positive test result from the current test. A previously tested person is a person who said that they were tested before the current test or a person who said that they were not previously tested, but were known to have a prior positive test result from a check of a local HIV surveillance or other database.
HIV positivity.
A person with newly diagnosed HIV has a current HIV-positive test result, which includes unconfirmed preliminary positive rapid tests and confirmed positive tests, and no self-report of a prior positive test and no indication of a previous HIV-positive test in a local HIV surveillance or other data source. We calculated the percentage of positive tests for new diagnoses by dividing the number of new HIV-positive tests by the number of valid tests.
Linkage to HIV medical care and PrEP awareness and referral.
We defined linkage to HIV medical care as a person who attended their first medical appointment within 30 days after an HIV diagnosis with a provider who has the capacity to prescribe HIV medications. We defined PrEP awareness as a client who reported having ever heard of PrEP. We defined PrEP referral as a person who tested negative for HIV, met clinical criteria for using PrEP or was determined to be eligible for a PrEP referral based on CDC guidelines or local protocol, and was referred to a PrEP provider. Referral may be passive (e.g., client is provided information about a PrEP provider) or active (e.g., client is assisted with contacting and making an appointment with a PrEP provider).
Test setting.
For each CDC-funded test, test setting is the location where the test was conducted. Non–healthcare settings include nonclinical sites in which neither medical diagnostic nor treatment services are provided (e.g., HIV testing sites, community settings, field visits, syringe exchange programs, and correctional facilities).
Statistics:
We conducted descriptive analyses of characteristics of persons who tested for HIV for the first time and statistical significance of differences with Chi-square tests. We considered p-values <0.05 as significant. We used Robust Poisson multivariate regression with a log-link function and robust variance estimator to assess the association between the measures of interest (i.e., PrEP awareness, PrEP referral, and linkage to HIV medical care within 30 days after a new HIV diagnosis) and the fixed main effects of the independent factors (i.e., age group, gender, race and ethnicity, U.S. census region of the health department, and population group). We considered referent groups as at the lowest risk for HIV based on HIV surveillance incidence data from 2019 (1). We used adjusted prevalence ratios (aPRs) and 95% confidence intervals (CIs) to interpret the final model and considered associations significant if the 95% CI did not include “1.00.” We stratified data by age group, gender, race and ethnicity, U.S. census region of the health department, and population group, and excluded missing and invalid data from denominators. We used SAS® 9.4 (SAS Institute Inc. Cary, NC) for all statistical analyses.
RESULTS
HIV testing
In 2019, the 31 HDs reported 187 032 tests with valid HIV status data from non-healthcare settings. Table 1 shows results for HIV testing in non-healthcare settings, by demographic characteristics and other factors. Health departments submitted 39 353 (21.0%) HIV tests among persons who tested for HIV for the first time and 147 679 (79.0%) HIV tests among persons who previously tested. For demographic characteristics and population groups, the largest difference (19.9%) between persons who tested for HIV for the first time and persons who previously tested was for persons aged 13-29 years (62.0% [24 295/39 192] vs 42.1% [61 911/147 087], p<.0001). Persons who tested for HIV for the first time also had a higher percentage of new HIV diagnoses (0.6% [242/39 320] vs 0.5% [667/147 475], p<.0001).
Table 1.
Number and percentage of HIV tests in non-healthcare settings, by HIV testing status, demographic characteristics, and other factors, 31 health departments in the United States, 2019
| HIV Testing Status | ||||
|---|---|---|---|---|
| Total* | First Time Tested | Previously Tested | Chi-Square test |
|
| Total | N=187 032 | n=39 353 | n=147 679 | |
| No. (Col %) | No. (Col %) | No. (Col %) | ||
| Age group (yrs) † | p<0.0001 | |||
| 13-29 | 86 206 (46.3) | 24 295 (62.0) | 61 911 (42.1) | |
| 30-49 | 74 134 (39.8) | 10 730 (27.4) | 63 404 (43.1) | |
| 50+ | 25 939 (13.9) | 4 167 (10.6) | 21 772 (14.8) | |
| Gender § | p<0.0001 | |||
| Male | 120 243 (64.7) | 22 910 (58.6) | 97 333 (66.3) | |
| Female | 62 552 (33.7) | 15 757 (40.3) | 46 795 (31.9) | |
| Transgender | 3 092 (1.7) | 458 (1.2) | 2 634 (1.8) | |
| Race and Ethnicity ¶ | p<0.0001 | |||
| White | 65 495 (35.6) | 15 141 (39.2) | 50 354 (34.7) | |
| Black/African American | 63 706 (34.6) | 10 671 (27.6) | 53 035 (36.5) | |
| Hispanic/Latino | 42 458 (23.1) | 9 783 (25.3) | 32 675 (22.5) | |
| Asian | 6 058 (3.3) | 1 512 (3.9) | 4 546 (3.1) | |
| American Indian or Alaska Native | 2 749 (1.5) | 761 (2.0) | 1 988 (1.4) | |
| Native Hawaiian or Pacific Islander | 545 (0.3) | 140 (0.4) | 405 (0.3) | |
| More than one race | 2 916 (1.6) | 648 (1.7) | 2 268 (1.6) | |
| Population Groups ** | p<0.0001 | |||
| MSM | 51 681 (29.9) | 5 834 (16.4) | 45 847 (33.5) | |
| MSM who inject drugs | 2 951 (1.7) | 385 (1.1) | 2 566 (1.9) | |
| PWID | 18 311 (10.6) | 3 973 (11.2) | 14 338 (10.5) | |
| Heterosexual males | 50 919 (29.5) | 13 099 (36.8) | 37 820 (27.6) | |
| Heterosexual females | 48 721 (28.2) | 12 295 (34.6) | 36 426 (26.6) | |
| U.S. Census Region | p<0.0001 | |||
| Northeast | 43 033 (23.0) | 6 398 (16.3) | 36 635 (24.8) | |
| Midwest | 27 136 (14.5) | 7 607 (19.3) | 19 529 (13.2) | |
| South | 84 002 (44.9) | 18 398 (46.8) | 65 604 (44.4) | |
| West | 32 861 (17.6) | 6 950 (17.7) | 25 911 (17.5) | |
| HIV Status †† | p<0.0001 | |||
| New positive tests | 909 (0.5) | 242 (0.6) | 667 (0.5) | |
| Previous positive tests | 783 (0.4) | 0 (0.0) | 783 (0.5) | |
| Negative tests | 185 103 (99.1) | 39 078 (99.4) | 146 025 (99.0) | |
Abbreviations: HIV = human immunodeficiency virus; MSM = gay, bisexual, and other men who have sex with men; PWID = persons who inject drugs.
Of the 208 373 tests conducted, 21 341 (10.2%) were missing HIV testing status”.
For age, the number of records missing or invalid are as follows: 753 (0.4%) in the column under “Total”, 161 (0.4%) in the column under “First Time Tested”, and 592 (0.4%) in the column under “Previously Tested”.
For gender, the number of records missing or invalid are as follows: 1 145 (0.6%) in the column under “Total”, 228 (0.6%) in the column under “First Time Tested”, and 917 (0.6%) in the column under “Previously Tested”.
All races are non-Hispanic/Latino. Hispanic/Latino ethnicity can be of any race. For race, the number of records missing or invalid are as follows: 3 105 (1.7%) in the column under “Total”, 697 (1.8%) in the column under “First Time Tested”, and 2 408 (1.6%) in the column under “Previously Tested”.
For population groups, the number of records missing or invalid are as follows: 1 255 (0.7%) in the column under “Total”, 343 (0.9%) in the column under “First Time Tested” and 912 (0.6%) in the column under “Previously Tested”. In addition, the number of records for “Other” excluded from this table are as follows: 13 194 (7.1%) in the column under “Total”, 3 424 (8.7%) in the column under “First Time Tested”, and 9 770 (6.6%) in the column under “Previously Tested”.
For HIV Status, the number of records missing or invalid are as follows: 237 (0.1%) in the column under “Total”, 33 (0.1%) in the column under “First Time Tested”, and 204 (0.1%) in the column under “Previously Tested”.
Among persons who tested for the first time, the highest percentages of new HIV diagnoses were among MSM (2.6% [151/5 834]), MSM who inject drugs (1.8% [7/385]), and transgender persons (1.7% [8/458])(Table 2). Compared with their referent groups, the findings were statistically significant based on aPRs and 95% CIs: 7.73 (2.46, 24.26) for MSM, 6.64 (1.72, 25.67) for MSM who inject drugs, and 12.3 (4.28, 35.62) for transgender persons.
Table 2.
Linkage to HIV medical care among persons in non-healthcare settings who tested for HIV for the first time, by demographic characteristics and other factors, 31 health departments in the United States, 2019
| First-time tested | ||||||
|---|---|---|---|---|---|---|
| Total HIV tests (first time tested) |
New HIV diagnosis |
aPR (95% CI) | New HIV diagnosis with valid data on linkage to HIV medical care |
Linkage to HIV medical care within 30 days of HIV diagnosis |
aPR (95% CI) | |
| Total (No.) | 39 353 | 242 | 237 | 174 | ||
| No. (Col %) | No. (Row %) | No. (Denominator) |
No. (Row %) | |||
| Age group (yrs) * | ||||||
| 50+ | 4 167 (10.6) | 28 (0.7) | Referent | 27 | 19 (70.4) | Referent |
| 13-29 | 24 295 (62.0) | 131 (0.5) | 0.64 (0.42, 0.97) | 128 | 92 (71.9) | 1.05 (0.80, 1.37) |
| 30-49 | 10 730 (27.4) | 83 (0.8) | 1.10 (0.71, 1.71) | 82 | 63 (76.8) | 1.12 (0.87, 1.45) |
| Gender † | ||||||
| Female | 15 757 (40.3) | 27 (0.2) | Referent | 27 | 20 (74.1) | Referent |
| Male | 22 910 (58.6) | 205 (0.9) | 2.48 (0.87, 7.08) | 200 | 149 (74.5) | 0.90 (0.36, 2.28) |
| Transgender | 458 (1.2) | 8 (1.7) | 12.34 (4.28, 35.62) | 8 | 3 (37.5) | 0.63 (0.19, 2.12) |
| Race and Ethnicity § | ||||||
| White | 15 141 (39.2) | 58 (0.4) | Referent | 57 | 42 (73.7) | Referent |
| Black/African American | 10 671 (27.6) | 92 (0.9) | 2.68 (1.91, 3.75) | 91 | 67 (73.6) | 1.03 (0.84, 1.26) |
| Hispanic/Latino | 9 783 (25.3) | 81 (0.8) | 2.56 (1.81, 3.60) | 78 | 58 (74.4) | 1.06 (0.85, 1.32) |
| Other | 3 061 (7.9) | 9 (0.3) | 0.95 (0.47, 1.92) | 9 | 5 (55.6) | 0.69 (0.39, 1.21) |
| Population Groups ¶ | ||||||
| Heterosexual females | 12 295 (34.6) | 20 (0.2) | Referent | 20 | 16 (80.0) | Referent |
| MSM | 5 834 (16.4) | 151 (2.6) | 7.73 (2.46, 24.26) | 149 | 111 (74.5) | 1.07 (0.42, 2.77) |
| MSM who inject drugs | 385 (1.1) | 7 (1.8) | 6.64 (1.72, 25.67) | 7 | 7 (100.0) | 1.38 (0.53, 3.59) |
| PWID | 3 973 (11.2) | 10 (0.3) | 1.14 (0.34, 3.87) | 9 | 4 (44.4) | 0.48 (0.16, 1.45) |
| Heterosexual males | 13 099 (36.8) | 32 (0.2) | 0.60 (0.18, 1.96) | 30 | 23 (76.7) | 1.10 (0.42, 2.90) |
| U.S. Census Region | ||||||
| Midwest | 7 607 (19.3) | 36 (0.5) | Referent | 33 | 28 (84.8) | Referent |
| Northeast | 6 398 (16.3) | 16 (0.3) | 0.50 (0.28, 0.91) | 16 | 15 (93.8) | 0.98 (0.79, 1.21) |
| South | 18 398 (46.8) | 164 (0.9) | 1.58 (1.09, 2.28) | 163 | 113 (69.3) | 0.72 (0.59, 0.89) |
| West | 6 950 (17.7) | 26 (0.4) | 0.62 (0.36, 1.05) | 25 | 18 (72.0) | 0.84 (0.62, 1.12) |
Abbreviations: HIV = human immunodeficiency virus; MSM = gay, bisexual, and other men who have sex with men; PWID = persons who inject drugs; aPR = adjusted prevalence ratio; CI = confidence interval
For age, the number of records missing or invalid are as follows: 161 (0.4%) in the column under “Total”.
For gender, the number of records missing or invalid are as follows: 228 (0.6%) in the column under “Total”, 2 (0.8%) in the column under “New HIV diagnosis”, 2 (0.8%) in the column under “New HIV diagnosis with valid data on linkage to HIV medical care”, and 2 (1.1%) in the column under “Linkage to HIV medical care within 30 days of HIV diagnosis”.
All races are non-Hispanic/Latino. Hispanic/Latino can be of any race. Race category “Other” includes Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander and when more than one race is selected. For race, the number of records missing or invalid are as follows: 697 (1.8%) in the column under “Total”, 2 (0.8%) in the column under “New HIV diagnosis”, 2 (0.8%) in the column under “New HIV diagnosis with valid data on linkage to HIV medical care”, and 2 (1.1%) in the column under “Linkage to HIV medical care within 30 days of HIV diagnosis”.
For population groups, the number of records missing or invalid are as follows: 343 (0.9%) in the column under “Total”, 1 (0.4%) in the column under “New HIV diagnosis”, 1 (0.4%) in the column under “New HIV diagnosis with valid data on linkage to HIV medical care”, and 1 (0.6%) in the column under “Linkage to HIV medical care within 30 days of HIV diagnosis”. In addition, the number of records for “Other” excluded from this table are as follows: 3 424 (8.7%) in the column under “Total”, 21 (8.7%) in the column under “New HIV diagnosis”, 21 (8.9%) in the column under “New HIV diagnosis with valid data on linkage to HIV medical care”, and 12 (6.9%) in the column under “Linkage to HIV medical care within 30 days of HIV diagnosis”.
Linkage to HIV medical care
Table 2 shows results for linkage to HIV medical care, by demographic characteristics and other factors. Among persons who tested for the first time and had newly diagnosed HIV, 73.4% (174/237) were linked to HIV care within 30 days after their new HIV diagnosis. The lowest percentages of linkage to HIV care were among transgender persons (37.5% [3/8]), PWID (44.4% [4/9], and persons who tested in the South (69.3% [113/163]; however, compared with the referent group, persons who tested in the South was the only group with a statistically significant finding (aPR = 0.72, 95% CI = 0.59, 0.89).
PrEP awareness and referral
Table 3 shows results for PrEP awareness and referrals, by demographic characteristics and other factors. Among persons who tested for the first time and tested HIV negative, 33.3% (12 331/36 989) were aware of PrEP. The lowest percentages of PrEP awareness that were statistically significant occurred among PWID (24.5%[927/3 784)(aPR = 0.84, 95% CI [0.77, 0·91]) and Hispanic/Latino persons (30.8% [2 866/9 295])(aPR = 0.91, 95% CI [0.88, 0.94]). Among persons who tested for the first time, tested HIV negative, and were eligible for a referral to a PrEP provider, 30.8% (5,627/18 277) were referred; PrEP eligibility information was unknown for 3.7% (1,459/39 078) of HIV-negative tests. PrEP referrals were lowest among persons who tested in the Northeast (13.4% [591/4 410]), heterosexual males (23.5% [1 237/5 269], PWID (24.5% [518/2 111], and Hispanic/Latino persons (24.6% [958/3 894]); however, only the findings for persons who tested in the Northeast (aPR = 0.28, 95% CI = 0.26, 0.31), PWID (aPR = 0.87, 95% CI = 0.77, 0.97), and Hispanic/Latino persons (aPR = 0.83, 95% CI = 0.78, 0.89) were statistically significant.
Table 3.
PrEP awareness and referral to a PrEP provider among persons in non-healthcare settings who tested for HIV for the first time and tested HIV negative, by demographic characteristics and other factors, 31 health departments in the United States, 2019
| First-time tested | |||||||
|---|---|---|---|---|---|---|---|
| Total negative HIV tests (first time tested) |
PrEP awareness | Referral to a PrEP provider | |||||
| Total negative HIV tests with valid data on PrEP awareness |
Aware of PrEP |
aPR (95% CI) | Eligible for a PrEP referral* |
Referred to a PrEP provider |
aPR (95% CI) | ||
| Total (No.) | 39 078 | 36 989 | 12 331 (33.3) | 18 277 | 5 627 (30.8) | ||
| No. | No. (Col %) | No. (Row %) | No. | No. (Row %) | |||
| Age group (years) † | |||||||
| 50+ | 4 136 | 3 927 (10.7) | 1 006 (25.6) | Referent | 1 887 | 543 (28.8) | Referent |
| 13-29 | 24 146 | 22 852 (62.0) | 8 327 (36.4) | 1.37 (1.30, 1.44) | 11 497 | 3 605 (31.4) | 1.05 (0.98, 1.13) |
| 30-49 | 10 635 | 10 057 (27.3) | 2 961 (29.4) | 1.22 (1.15, 1.29) | 4 828 | 1 464 (30.3) | 1.07 (0.99, 1.16) |
| Gender § | |||||||
| Female | 15 722 | 14 787 (40.2) | 4 297 (29.1) | Referent | 6 575 | 1 751 (26.6) | Referent |
| Male | 22 683 | 21 568 (58.6) | 7 665 (35.5) | 0.93 (0.85, 1.02) | 11 329 | 3 741 (33.0) | 0.95 (0.84, 1.08) |
| Transgender | 447 | 429 (1.2) | 254 (59.2) | 2.15 (1.93, 2.41) | 243 | 87 (35.8) | 0.98 (0.82, 1.18) |
| Race and Ethnicity ¶ | |||||||
| White | 15 076 | 14 240 (39.2) | 4 871 (34.2) | Referent | 6 954 | 2 385 (34.3) | Referent |
| Black/African American | 10 558 | 9 945 (27.4) | 3 339 (33.6) | 1.05 (1.01, 1.09) | 5 823 | 1 793 (30.8) | 1.04 (0.99, 1.09) |
| Hispanic/Latino | 9 699 | 9 295 (25.6) | 2 866 (30.8) | 0.91 (0.88, 0.94) | 3 894 | 958 (24.6) | 0.83 (0.78, 0.89) |
| Other | 3 050 | 2 872 (7.9) | 1 065 (37.1) | 1.03 (0.98, 1.08) | 1 322 | 399 (30.2) | 0.90 (0.83, 0.98) |
| Population Groups ** | |||||||
| Heterosexual females | 12 270 | 11 579 (34.4) | 3 454 (29.8) | Referent | 5 167 | 1 351 (26.1) | Referent |
| MSM | 5 670 | 5 530 (16.4) | 3 481 (62.9) | 2.24 (2.04, 2.45) | 4 228 | 1 993 (47.1) | 1.74 (1.51, 1.99) |
| MSM who inject drugs | 378 | 371 (1.1) | 158 (42.6) | 1.53 (1.32, 1.77) | 273 | 117 (42.9) | 1.51 (1.24, 1.83) |
| PWID | 3 960 | 3 784 (11.3) | 927 (24.5) | 0.84 (0.77, 0.91) | 2 111 | 518 (24.5) | 0.87 (0.77, 0.97) |
| Heterosexual males | 13 059 | 12 368 (36.8) | 3 242 (26.2) | 0.92 (0.84, 1.01) | 5 269 | 1 237 (23.5) | 0.99 (0.86, 1.14) |
| U.S. Census Region | |||||||
| Midwest | 7 570 | 7 321 (19.8) | 1 978 (27.0) | Referent | 2 889 | 1 561 (54.0) | Referent |
| Northeast | 6 376 | 6 259 (16.9) | 3 981 (63.6) | 2.45 (2.35, 2.55) | 4 410 | 591 (13.4) | 0.28 (0.26, 0.31) |
| South | 18 215 | 16 621 (44.9) | 4 495 (27.0) | 1.00 (0.96, 1.05) | 9 089 | 2 833 (31.2) | 0.62 (0.59, 0.65) |
| West | 6 917 | 6 788 (18.4) | 1 877 (27.7) | 1.02 (0.97, 1.07) | 1 889 | 642 (34.0) | 0.69 (0.64, 0.74) |
Abbreviations: HIV = human immunodeficiency virus; MSM = gay, bisexual, and other men who have sex with men; PWID = persons who inject drugs; aPR = adjusted prevalence ratio; CI = confidence interval.
There were 37 619 negative HIV tests with valid PrEP eligibility information (i.e., “Yes/No” response indicated for the question “Is the client eligible for PrEP referral?”). PrEP eligibility information was unknown for 3.7% (1 459/39 078) of negative HIV tests. Among persons who were eligible for a PrEP referral, 0.69% (127/18 404) had unknown PrEP referral information.
For age, the number of records missing or invalid are as follows: 161 (0.4%) in the column under “Total negative HIV tests”, 153 (0.4%) in the column under “Total negative HIV tests with valid data on PrEP awareness”, 37 (0.3%) in the column under “Aware of PrEP”, 65 (0.4%) in the column under “Eligible for a PrEP referral”, and 15 (0.3%) in the column under “Referred to a PrEP provider”.
For gender, the number of records missing or invalid are as follows: 226 (0.6%) in the column under “Total negative HIV tests”, 205 (0.6%) in the column under “Total negative HIV tests with valid data on PrEP awareness”, 115 (0.9%) in the column under “Aware of PrEP”, 130 (0.7%) in the column under “Eligible for a PrEP referral”, 48 (0.9%) in the column under “Referred to a PrEP provider”.
All races are non-Hispanic/Latino. Hispanic/Latino can be of any race. Race category “Other” includes Asian, American Indian/Alaska Native, Native Hawaiian/Pacific Islander and when more than one race is selected. For race, the number of records missing or invalid are as follows: 695 (1.8%) in the column under “Total negative HIV tests”, 637 (1.7%) in the column under “Total negative HIV tests with valid data on PrEP awareness”, 190 (1.5%) in the column under “Aware of PrEP”, 284 (1.6%) in the column under “Eligible for a PrEP referral”, and 92 (1.6%) in the column under “Referred to a PrEP provider”.
For population groups, the number of records missing or invalid are as follows: 342 (0.9%) in the column under “Total negative HIV tests”, 84 (0.2%) in the column under “Total negative HIV tests with valid data on PrEP awareness”, 55 (0.4%) in the column under “Aware of PrEP”, 90 (0.5%) in the column under “Eligible for a PrEP referral”, and 40 (0.7%) in the column under “Referred to a PrEP provider”. In addition, the number of records for “other” excluded from this table are as follows: 3,399 (8.7%) in the column under “Total negative HIV tests”, 3 273 (8.8%) in the column under “Total negative HIV tests with valid data on PrEP awareness”, 1 014 (8.2%) in the column under “Aware of PrEP”, 1 139 (6.2%) in the column under “Eligible for a PrEP referral”, and 371 (6.6%) in the column under “Referred to a PrEP provider”.
Discussion and Conclusion
In our analysis, persons in non-healthcare settings who tested for the first time were more likely to have a higher percentage of new HIV positivity than persons who previously tested, which is consistent with prior studies.12,14 This finding underscores the importance of reaching and engaging persons who have never previously tested with effective HIV prevention interventions, particularly for MSM, MSM who inject drugs, and transgender persons who had the highest percentages of new HIV positivity. We also found that persons who tested for the first time, compared with persons who previously tested, were more likely to be young. This finding is of particular concern because young persons have reported a statistically significant decline in HIV testing during 1999-2018,18 which might indicate missed opportunities to receive prevention and treatment services. Successful strategies and services to engage persons who are young and have never previously tested for HIV might include a social network strategy, geosocial networking applications, changing risk perceptions, self-efficacy, and increased opportunities for testing in non-healthcare settings.13,19,20
The overall percentage of persons who tested for the first time, had newly diagnosed HIV, and were linked to HIV medical care within 30 days after HIV diagnosis was 73.4%, which is lower than the PS18-1802 performance target (85%) and national average based on surveillance data of all persons reported with new HIV diagnoses in the United States (81%).3 To meet the PS18-1802 performance standard and national target from the National HIV/AIDS Strategy (95% by 2025)5 for linkage to HIV medical care within 30 days after HIV diagnosis, additional efforts are needed. For example, non-healthcare sites might provide linkage coordinators and establish close collaborations with healthcare sites that provide rapid HIV treatment.6 Promptly linking to care persons with newly diagnosed HIV is of particular concern in the South, because persons tested in the South in our analysis had the lowest percentage of linkage and highest percentage of new HIV diagnoses. Effective approaches in the South might include structural interventions that are tailored to client needs and comfort levels (e.g., phone call reminders, text messages, mobile apps) and peer navigation programs, which could help overcome fear and stigma that some clients experience.21
Results from a nationally representative survey show that 37% of U.S. respondents with increased risk for HIV acquisition were aware of PrEP.22 Results from another study showed that persons aged less than 25 years and from the South had the lowest levels of PrEP use and the greatest need.23 These results and ours (i.e., 33% overall PrEP awareness and 31% referrals among persons who tested for the first time) suggest that a lot of progress is needed to meet the national goal of 50% PrEP coverage. Our findings suggest that efforts to increase PrEP awareness are important for all groups, particularly for PWIDs and Hispanic/Latino persons. Interventions that may help increase awareness could include social networks, such as related to syringe exchange programs.24 Interventions that might be effective to increase PrEP awareness among Hispanic/Latino persons include social media strategies, social marketing, community education materials, peer networks, support groups, and culturally and linguistically competent staff.25,26
Non-healthcare sites, particularly community-based organizations (CBOs), are known and trusted by their communities and have culturally-competent providers of HIV testing and referrals to HIV care and PrEP sites,27 thus able to make a substantial impact with persons at risk for HIV acquisition and persons with newly diagnosed HIV. For example in one study, being tested for HIV and receiving free condoms from an HIV/AIDS CBO were associated with PrEP awareness.28 However, based on a survey of non-clinical CBOs, the most commonly reported challenge for PrEP referrals was the lack of connection to clinicians who provide PrEP services.29 Therefore, additional approaches for non-healthcare sites could be active or facilitated referral systems that include scheduled appointments, navigators for PrEP and HIV treatment services, and developing new collaborations with clinical providers and healthcare systems that more effectively integrate prevention and clinical services.6,17,20,30 Such integration is a main goal of the status neutral approach, which can also decrease stigma by using strategies that address social determinants of health.5
There are at least three limitations to this analysis. First, data represent HIV testing events and are not client level; however, focusing the analysis on persons who have tested for HIV for the first time minimizes the possibility that data include a client who tested more than once. Second, data do not represent all CDC-funded tests conducted in non-healthcare settings in 2019 under PS18-1802, but do represent health departments that CDC considers to have the highest quality data. Third, for some calculations with small numbers that do not show statistical significance, a characteristic of concern may not be apparent from our analyses.
Our work supports future research. First we analyzed data from 2019, which was the last year of data collection and program service delivery that was not adversely impacted by COVID-19. Research might address how best to deliver HIV services during times of severe disruption such as with COVID-19. Second, non-healthcare sites are a critical component of effective approaches to reach national HIV prevention and treatment goals. However, an insufficient number of relevant evidence-based interventions exist that are tailored to HIV non-healthcare sites. For example, in an era in which expectations are that linkage to HIV care occurs within 30 days after a diagnosis, interventions that take longer than 30 days to implement are unlikely to substantially help meet national goals and standard of care expectations. Thus, more relevant research is needed to better address needs and context within which HIV non-healthcare sites function, particularly for young persons, MSM, transgender persons, PWID, Hispanic/Latino persons, and persons tested in the South. Third, although our methods were not designed to provide detailed analyses of health disparities, our results support the need for additional pragmatic research that addresses how best to deliver services that address health disparities and inequities.31
Our findings support efforts in non-healthcare sites to increase HIV testing, PrEP awareness, and prompt referrals to PrEP and HIV treatment services for persons who have never previously tested. Non-healthcare sites working with health departments should consider enhancing outreach efforts to increase HIV testing and PrEP education, particularly for young persons who have never tested, offering PrEP and HIV treatment services or engaging providers who do, and obtaining capacity building assistance to support persons most in need of services. Additionally, because quality data from all health departments are critical to accurately monitor national goals and help inform decision making at the national and local levels, non-healthcare sites and local surveillance programs should collaborate on quality data to meet national and local goals and help end the HIV epidemic.
Implications for Policy and Practice.
Increased HIV testing, PrEP awareness, and prompt referrals to PrEP and HIV treatment services are needed for persons who have never previously tested.
Non-healthcare sites should consider offering PrEP and HIV medical care or engaging providers who do.
Collaboration between non-healthcare sites and local surveillance programs on quality data is important to meet national and local goals and help end the HIV epidemic.
Acknowledgement
The authors appreciate the work of Yolanda Strayhorn, MLIS, the CDC Reference Librarian who assisted with the literature search for this article.
Funding
CDC funds health departments to collect and submit HIV testing data with Funding Opportunity Announcement PS18-1802.
Footnotes
Financial disclosure
None of the authors have any financial relationships relevant to this submitted work.
Author approval and conflicts of interest
All authors have approved the final manuscript and have no conflicts of interest to disclose.
Human participant compliance statement
The Centers for Disease Control and Prevention determined the work to be a routine program monitoring activity, so Institutional Review Board approval was not needed.
Disclaimers
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Because inclusiveness and respect are critically important, concerted effort was made to avoid stigmatizing or offensive words and terms in this article, recognizing that sensitivities and preferred language may be different among persons or change with time.
References
- 1.Centers for Disease Control and Prevention. Estimated HIV incidence and prevalence in the United States, 2015–2019. HIV Surveillance Supplemental Report 2021;26(No. 1). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2021. Accessed June 6, 2021. [Google Scholar]
- 2.Li Z, Purcell DW, Sansom SL, Hayes D, Hall HI. Vital Signs: HIV transmission along the continuum of care – United States, 2016. MMWR Morb Mortal Wkly Rep. 2019;68(11):267–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Monitoring selected national HIV prevention and care objectives by using HIV surveillance data—United States and 6 dependent areas, 2019. HIV Surveillance Supplemental Report 2021;26(No. 2). http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html. Published May 2021. Accessed June 6, 2021. [Google Scholar]
- 4.Centers for Disease Control and Prevention: US Public Health Service: Preexposure prophylaxis for the prevention of HIV infection in the United States—2021 Update: A clinical practice guideline. https://www.cdc.gov/hiv/pdf/risk/prep/cdc-hiv-prep-guidelines-2021.pdf. Published December 2021. Accessed December 11, 2021. [Google Scholar]
- 5.The White House. 2021. National HIV/AIDS Strategy for the United States 2022–2025. Washington, DC. https://www.whitehouse.gov/wp-content/uploads/2021/11/National-HIV-AIDS-Strategy.pdf. Accessed December 4, 2021. [Google Scholar]
- 6.Coffey S, Halperin J, Rana AI, Colasanti JA. Rapid Antiretroviral Therapy: Time for a new standard of care. Clin Infect Dis. 2021;73(1):134–136. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55(No. RR-14). https://www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm. Accessed November 10, 2021. [PubMed] [Google Scholar]
- 8.Villarroel MA, Blackwell DL, Jen A. Tables of Summary Health Statistics for U.S. Adults: 2018 National Health Interview Survey. National Center for Health Statistics. 2019. https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2018_SHS_Table_A-20.pdf. Accessed December 6, 2021. [Google Scholar]
- 9.Patel D, Williams WO, Heitgerd J, Taylor-Aidoo N, DiNenno EA. Estimating gains in HIV testing by expanding HIV screening at routine checkups. Am J Public Health. 2021; 111(8):1530–1533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alang S, Bornstein S. HIV testing history among young adults: The roles of sex, race, and sexual orientation. J HIV AIDS Soc Serv. 2018; 17(3):180–194. [Google Scholar]
- 11.Febo-Vazquez I, Copen CE, Daugherty J. Main reasons for never testing for HIV among women and men aged 15-44 in the United States, 2011-2015. National Health Statistics Reports; no 107. Hyattsville, MD: National Center for Health Statistics. 2018. https:/www.cdc.gov/nchs/data/nhsr/nhsr107.pdf. Accessed December 6, 2021. [PubMed] [Google Scholar]
- 12.Matthews DD, Sang JM, Chandler CJ, et al. Black men who have sex with men and lifetime HIV testing: Characterizing the reasons and consequences of having never tested for HIV. Prev Sci. 2019;20(7):1098–1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramirez-Ortiz D, Sheehan DM, Ibanez GE, Ibrahimou B, De La Rosa M, Cano MA. Self-efficacy and HIV testing among Latino emerging adults: Examining the moderating effects of distress tolerance and sexual risk behaviors. AIDS Care. 2020;32(12):1556–1564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clark HA, Oraka E, DiNenno EA, et al. Men who have sex with men (MSM) who have not previously tested for HIV: Results from the MSM Testing Initiative, United States (2012-2015). AIDS Behav. 2019;23(2):359–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Funding opportunity announcement (FOA) PS18-1802: Integrated HIV Surveillance and Prevention Programs for Health Departments. 2017. https://www.cdc.gov/hiv/funding/announcements/ps18-1802/index.html. Accessed January 25, 2021. [Google Scholar]
- 16.Centers for Disease Control and Prevention. CDC-Funded HIV Testing in the United States, Puerto Rico, and the U.S. Virgin Islands, 2019. http://www.cdc.gov/hiv/library/reports/index.html. Published March 2021. Accessed June 6, 2021. [Google Scholar]
- 17.Centers for Disease Control and Prevention. Implementing HIV Testing in Nonclinical Settings: A Guide for HIV Testing Providers. https://www.cdc.gov/hiv/pdf/testing/cdc_hiv_implementing_hiv_testing_in_nonclinical_settings.pdf. Published March 2016. Accessed November 11, 2021. [Google Scholar]
- 18.McQuillan GM, Kruszon-Moran D, Masciotra S, Gu Q, Storandt R. Prevalence and trends in HIV infection and testing among adults in the United States: The National Health and Nutrition Examination Surveys, 1999-2018. J Acquir Immune Defic Syndr. 2021;86(5):523–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McGoy SL, Pettit AC, Morrison M, et al. Use of social network strategy among young Black men who have sex with men for HIV testing, linkage to care, and reengagement in care, Tennessee, 2013-2016. Public Health Rep. 2018;133(Supplement 2):43S–51S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Patel RR, Harrison LC, Patel VV, et al. HIV pre-exposure prophylaxis programs incorporating social applications can reach at-risk men who have sex with men for successful linkage to care in Missouri, USA. J Assoc Nurses AIDS Care. 2017;28(3):428–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Taylor BS, Fornos L, Tarbutton J, et al. Improving HIV care engagement in the South from the patient and provider perspective: The role of stigma, social support, and shared decision-making. AIDS Patient Care STDs. 2018;32(9):368–378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keddem S, Dichter ME, Hamilton AB, Chhatre S, Sonalkar S. Awareness of HIV preexposure prophylaxis among people at risk for HIV: Results from the 2017–2019 National Survey of Family Growth. Sex Transm Dis. 2021;48(12):967–972. [DOI] [PubMed] [Google Scholar]
- 23.Siegler AJ, Mouhanna F, Giler RM, et al. The prevalence of pre-exposure prophylaxis use and the pre-exposure prophylaxis-to-need ratio in the fourth quarter of 2017, United States. Ann Epidemiol. 2018;28(12):841–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walters SM, Reilly KH, Neaigus A, Braunstein S. Awareness of pre-exposure prophylaxis (PrEP) among women who inject drugs in NYC: The importance of networks and syringe exchange programs for HIV prevention. Harm Reduct. 2017;14:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kudrati SZ, Hayashi K, Taggart T. Social media & PrEP: A systematic review of social media campaigns to increase PrEP awareness & uptake among young black and Latinx MSM and women. AIDS Behav. 2021;25(5):4225–4234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Page KR, Martinez O, Nieves-Lugo K, et al. Promoting pre-exposure prophylaxis to prevent HIV infections among sexual and gender minority Hispanics/Latinxs. AIDS Educ Prev. 2017;29(5):389–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marano-Lee M, Williams W, Uhl G, et al. Contributions of community-based organizations funded by the Centers for Disease Control and Prevention. J Public Health Manag Pract. 2022;28(2):E461–E466. [DOI] [PubMed] [Google Scholar]
- 28.Raifman JRG, Flynn C, German D. Healthcare provider contact and pre-exposure prophylaxis in Baltimore men who have sex with men. Am J Prev Med. 2017;52(1):55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Smith DK, Maier E, Betts J, Gray S, Kolodziejski B, Hoover KW. What community-based HIV prevention organizations say about their role in biomedical HIV prevention. AIDS Educ Prev. 2016;28(5):426–439. [DOI] [PubMed] [Google Scholar]
- 30.Hosek SG. HIV pre-exposure prophylaxis diffusion and implementation issues in nonclinical settings. Am J Prev Med. 2013;44(1S2):S129–S132. [DOI] [PubMed] [Google Scholar]
- 31.Bonacci RA, Smith DK, Ojikutu BO. Toward greater pre-exposure prophylaxis equity: Increasing provision and uptake for Black and Hispanic/Latino individuals in the U.S. Am J Prev Med. 2021;61(5S1):S60–S72. [DOI] [PMC free article] [PubMed] [Google Scholar]