Abstract
Background:
The physical environmental risk factors for psychotic disorders are poorly understood. This study aimed to examine the associations between exposure to ambient air pollution, climate measures and risk of hospitalization for psychotic disorders and uncover potential disparities by demographic, community factors.
Methods:
Using Health Cost and Utilization Project (HCUP) State Inpatient Databases (SIDs), we applied zero-inflated negative binomial regression to obtain relative risks of hospitalization due to psychotic disorders associated with increases in residential exposure to ambient air pollution (fine particulate matter, PM2.5; nitrogen dioxide, NO2), temperature and cumulative precipitation. The analysis covered all-age residents in eight U.S. states over the period of 2002 – 2016. We additionally investigated modification by age, sex and area-level poverty, percent of blacks and Hispanics.
Results:
Over the study period and among the covered areas, we identified 1,211,100 admissions due to psychotic disorders. For each interquartile (IQR) increase in exposure to PM2.5 and NO2, we observed a relative risk (RR) of 1.11 (95% confidence interval (CI) = 1.09, 1.13) and 1.27 (95% CI = 1.24, 1.31), respectively. For each 1 °C increase of temperature, the RR was 1.03 (95% CI = 1.03, 1.04). Males were more affected by NO2. Older age residents (>= 30 yrs.) were more sensitive to PM2.5 and temperature. Population living in economically disadvantaged areas were more affected by air pollution.
Conclusions:
The study suggests that living in areas with higher levels of air pollutants and ambient temperature could contribute to additional risk of inpatient care for individuals with psychotic disorders.
Keywords: air pollution, temperature, precipitation, psychosis
1. Introduction
The total ambient environment has been adversely influencing human neurological and psychiatric health, including schizophrenia and other psychotic disorders, as demonstrated in recent studies.1–10 During the past few years, not only were air pollutants demonstrated to contribute to the development of psychiatric disorders, but they were also observed to act as triggers of acute psychiatric episodes and outcomes in the short-term. Daily levels of air pollutants were observed to be associated with significantly higher levels of emergency departments visits for mental disorders in a recent review paper consisting of 19 related studies.11 In particular, a large population-based study in China covering 75 cities found that short-term exposure to ambient air pollution is associated with increased risk of daily depression hospitalization in the general urban population.12 In another study looking at the risk in the Korean National Health Insurance data, the authors also found a harmful link between acute fine particles exposure and increased risk of emergency hospital admissions for mental disease. The associations retained even in low-exposure areas with levels below the World Health Air Quality guidelines.13 In addition, traffic-related air pollution (such as nitrogen dioxide, NO2) has also been linked to increased risk of psychiatric disorders.14, 15 A national cohort study in Denmark found that higher exposure to residential NO2 during childhood was associated with elevated schizophrenia risk with those exposed to daily mean concentrations of > 26·5 μg/m3 NO2 having a 1.62 (95% CI, 1.41–1.87) times increased risk compared with people exposed to a mean daily concentration of <14·5 μg/m3.16 The possible mechanisms for air pollutants to act on human neurological system could be through the regulation of stress hormones5 as well as systematic or neuro-inflammation in the body after absorption.4 Air pollution is usually a diverse mixture of substances including particles, gas, organic compounds and neuro-toxic metals, such as lead (Pb), which has been proven to be able to suppress the NMDA subtype of glutamate receptors (NMDAR) involved in the development of psychosis.17, 18
Although the current evidence for linking air pollution and risk of psychiatric disorders is rising, most of them did not fully account for other potential mental-related climatic factors, such as exposure to increased ambient temperature, sunlight or precipitation. The 70-kDa heat shock proteins (HSP70s) affected by temperature, specifically HSPA5 and HSPA1B, have been recently shown to be potentially associated with occurrence of anxiety, mood disorders, and schizophrenia.19 Serotonergic function is also believed to fluctuate along with light and temperature, and serotonin-related behavioral disorders similarly vary with climatic exposures with complex mechanism.20, 21 Climate change actively interacts with the levels of hazardous pollutants in the air that we breathe every day. In particular, temperature influences the rate of chemical reactions that form secondary organic aerosols, the largest single component of ambient particles. Therefore, it is critical importance to put air pollution and climatic conditions into the same picture when we investigated the impact of ambient environment on population mental health.
Psychotic disorders are a group of mental disorders characterized by adverse mental symptoms such as false beliefs, delusions, hallucinations and disorganized thoughts, etc.22 In the U.S., according to the estimates from the National Institute of Mental Health (NIMH), there are about 100,000 new cases of psychotic disorders being diagnosed annually.23 The prevalence rate was observed to be higher in males vs. females.24 As previous studies revealed, an individual with psychotic disorders is at a higher risk of premature mortality, suicidal behaviors, disability as well as chronic medical illness.25, 26 The life expectancy of a psychotic patient was estimated to reduce by approximately 10 years with suicide being the major cause of death.27 In addition to the direct burden posed to the patients themselves, it also takes considerable big efforts for the healthcare providers as well as the relatives who deliver the care. The serious consequences resulted from this group of mental illness add to the importance of studying modifiable risk factors for it.
In the study area of identifying more risk factors for psychotic disorders, there is limited evidence from the physical environment side. Besides semi-effective clinical interventions, large population-based solutions for treating or preventing psychotic illness are still limited. Due to the high-prevalence and universal exposure to the ambient environment, if significant associations could be established for modifiable risk factors such as air pollution and climate conditions (through air quality regulation and climate mitigation), related preventive measures could be applied to help control the disease burden. In this study, we investigated on the associations between living in areas of higher residential exposure to air pollution, temperature and precipitation and the risk of hospitalization for psychotic disorders in a U.S. general population over the study period of 2002 – 2016, using the Health Cost and Utilization Project State Inpatient Databases. We additionally explored the related health disparities by demographic and community factors.
2. Methods
2.1. Data Source & Study Population
We utilized the Health Cost and Utilization Project (HCUP) State Inpatient Databases (SIDs) to conduct this study.28 In this study, we had access to the SIDs for eight states including Arizona (AZ), Maryland (MD), Michigan (MI), New York (NY), New Jersey (NJ), North Carolina (NC), Rhode Island (RI) and Washington (WA). We explored inpatient admissions in the 8 states with a primary diagnosis of psychotic disorders. We further restricted the study sample to admissions between the years of 2002 – 2016, and with both hospital and residential addresses located in the same state. To reduce the noise from low population areas and increase the analytical power, we restricted to ZIP code areas with over 100 residents. Details about the inpatient databases and data availability could be found in the eMethods in the Supplement.
2.2. Exposure Assessment
We investigated on both air pollution (fine particulate matter, PM2.5; nitrogen dioxide, NO2) and climate conditions (near-surface air temperature and precipitation) in this study. Ambient daily PM2.5 and NO2 predictions at 1 km × 1 km resolution were obtained via a combination of machine learning algorithms taking as inputs land use, meteorology, several chemical transport models, and satellite remote sensing data. Details can be found in previous publications.29, 30 Annual averages of daily air pollutants levels were computed at each 1 km grid cell. Ambient near-surface annual mean temperature at 32 km × 32 km resolution was obtained from the North American Regional Reanalysis31 data (NARR). Annual cumulative precipitation at 1 km × 1 km resolution were obtained from the Daymet Annual Climate Summaries for the North America.32 We analyzed PM2.5 and NO2 here as the two key air pollutants in this study in that they are the major criteria pollutants established by the U.S. Environmental Protection Agency, and fine resolution high-performance spatiotemporal predictions were generated for them across the contiguous U.S. at our lab. PM2.5 was used as a proxy for regionally transported particle pollution and NO2 was used as a proxy for locally emitted traffic pollution. We did not include ozone in this study due to the fact that ozone and NO2 are often in strong negative correlation with each other, therefore including both in a multi-exposure model would lead to bias in the effect estimation. In addition, due to the complex photochemistry process involved in generating ozone, the residual confounding from other unmeasured atmospheric conditions and co-exposures for ozone to act on human health is big. Using the grid cells predictions, we aggregated the exposures to each ZIP code by 1) averaging the predictions at grid cells whose centroids were inside the polygonal area for general ZIP codes, or 2) assigning the prediction at the nearest grid cell for other ZIP codes that do not have polygon representations, for example an apartment building. We assigned the exposures based on participants’ residential address ZIP code, admission year and one year before the admission year. Precipitation data was total near-surface precipitation summing all forms of precipitation converted to a water-equivalent depth.
2.3. Outcome Measurement
Hospital admissions with primary diagnosis of psychotic disorders were identified from the SIDs referring to the International Classification of Diseases codes (9 and 10) list provided in the Centers for Medicare and Medicaid Services (CMS) Chronic Conditions Data Warehouse.33 The classification was also verified through the Diagnostic and Statistical Manual of Mental Disorders fifth edition (DSM–5).
2.4. Covariates
Besides the primary ambient exposure data, we also linked in area-level atmospheric relative humidity and solar shortwave radiation with each of the covered ZIP code areas, and controlled as climate covariates. The solar shortwave radiation was also investigated as the secondary exposure of interest in this study and is the near-surface incident shortwave radiation flux density taken as an average over the daylight period of the days across each year, serving as a proxy for daylight intensity. Information on individual age, sex, race/ethnicity, hospital discharge state, primary diagnosis codes, etc. was obtained for each psychiatric admission within the SIDs. We additionally controlled for admission state and admission year (2002 – 2016) to consider the locational and temporal variation in baseline risk. Area-level long-term socioeconomic, healthcare access, and behavioral factors (poverty, education, ambulatory visit level, smoking rate and Index of Concentration at the Extremes (ICE) comparing the proportions of high-income white vs. low-income black households) as well as population density (proxy for urbanity) were also adjusted. The ICE may represent the potential psychosocial stress resulted from within community income comparison due to racialized income extremes. Details about the covariates information and data source could be found in the eMethods in the Supplement.
2.5. Statistical Analysis
For each state, we aggregated the admissions to counts for each ZIP code and calendar year. We excluded ZIP code-year combinations with fewer than 100 residents to limit the noise from low population areas. Annual linear interpolated area-level population counts from the U.S. Census 2000–2010 and ACS after 201034–36 were linked with aggregated admission counts data by ZIP code and calendar year, and treated as an offset during modeling.
We used a multi-exposure zero-inflated negative binomial regression to model the over-dispersed admission counts with excess zero counts of admissions in certain ZIP code and years for all exposures concurrently.37 Annual average or cumulative (for precipitation only) levels of exposures were averaged across the admission year and one year past to represent the long-term average exposure levels in each covered ZIP code. Correlations between the exposures were investigated before model building and low-medium correlation was detected38 (eFigure 1 in the Supplement). Based on preliminary variable selection and epidemiological confounding structure (eFigure 2 in the Supplement), we adjusted for a key set of climate co-exposures, neighborhood factors as described in Covariates section. Calendar admission year and residential state were adjusted in the models to account for clustering by time and state. State-specific results were computed via fitting multiplicative interaction terms (to increase analytical power) between each exposure and the admission state indicator in the main multi-exposure model adjusting for key covariates as stated.
Exposure-response relationship was investigated by fitting natural splines with 3 degrees of freedom for each exposure of interest adjusting for the other exposures and covariates. For the curves, exposure levels were truncated <99.5th percentile since the higher end of the curves were poorly constrained.
Effect modification was examined via fitting stratified models in sub-populations and areas. Potential modifiers investigated were sex (male vs. female), age group (younger age, <30 yrs. vs. older age, >=30 yrs.), area level poverty, percent of black population and percent of Hispanic population. High and low poverty (or poor vs. less poor), percent of blacks and Hispanics were dichotomized using the upper 33% percentile cutoff. Z-test was conducted to test the difference of the effect estimates between sub-groups.
We also conducted the following sub-analyses: 1) step-by-step single to multi-exposure modeling to test the robustness of the effect estimates under single exposure or different co-exposure adjustment settings; 2) air pollution effect estimation under different climate conditions (high vs. low temperature/precipitation conditions using median as the cutoff); 3) alternative minimum residents size truncation (>250, >500, >1000) and truncating exposure ranges at <99.5th percentiles; 4) solar radiation main and sub-group effect estimation; 5) exploring solar radiation exposure-response curve via fitting natural splines of 3 degrees of freedom.
Relative risks (RRs) of hospitalization for psychotic disorders and its 95% confidence intervals (CIs) were reported per interquartile (IQR) increase in long-term averages of PM2.5, NO2, cumulative precipitation, and per 1 °C increase in ambient temperature. Robust variance was applied via sandwich estimators. The analysis was conducted using R 3.6.2. A two-sided p value < 0.05 was considered statistically significant.
3. Results
We included a total of 1,211,100 hospital admissions for psychotic disorders occurring over the study period. A total of 6,529 unique ZIP codes (with residents over 100) in the included eight states were covered. Among the admissions, adults and elderly take up more than 75%. More male admissions were recorded as compared with female (57.7% vs. 42.3%). Non-Hispanic whites contributed to 41.7% of the total admissions while non-Hispanic blacks contributed to 32.4% of all. Other details including levels of neighborhood contextual factors as well as ambient exposures were presented in Table 1.
Table 1.
Summary characteristics of study population, ambient exposures and neighborhood contextual factors
| Characteristics | Levels |
|---|---|
| Total admissions a, No. (%) | 1,211,100 (−) |
| Arizona | 77,355 (6.4) |
| Maryland (after 2009) | 64,231 (5.3) |
| Michigan | 176,521 (14.6) |
| New York | 521,710 (43.1) |
| New Jersey (after 2008) | 122,676 (10.1) |
| North Carolina | 153,123 (12.6) |
| Rhode Islands | 31,309 (2.6) |
| Washington | 64,175 (5.3) |
| Zip codes covered (>100 residents) | 6,529 |
| Study period | 2002–2016 |
| Age, No. (%) | |
| Children (age<=9 yrs.) | 1,741 (0.1) |
| Adolescents (10–19 yrs.) | 53,441 (4.4) |
| Young Adults (20–29 yrs.) | 240,495 (19.9) |
| Adults (30–64 yrs.) | 809,470 (66.8) |
| Elderly (>=65 yrs.) | 105,919 (8.7) |
| Other unidentified | 34 (0.0) |
| Sex, No. (%) | |
| Male | 698,781 (57.7) |
| Female | 512,275 (42.3) |
| Other unidentified | 44 (0.0) |
| Race/Ethnicity, No. (%) | |
| Non-Hispanic black | 391,924 (32.4) |
| Non-Hispanic white | 505,256 (41.7) |
| Other combined racesb | 179,247 (14.8) |
| Other unidentifiedc | 134,673 (11.1) |
| Neighborhood contextual factors, median (IQR) | |
| Poverty rate, % | 7.5 (4.4, 12.2) |
| High school or less education, % | 22.0 (13.5, 32.9) |
| Ambulatory visits per year per 100 population | 80.0 (76.3, 83.0) |
| Population density, people per mile2 | 107.9 (24.2, 895.2) |
| Smoking rated, % | 0.48 (0.44, 0.52) |
| ICEwbincomee | 0.18 (0.09, 0.30) |
| Ambient annual exposures, median (IQR) | |
| Fine particulate matter (PM2.5), μg/m3 | 9.0 (7.3, 10.8) |
| Nitrogen dioxide (NO2), ppb | 15.8 (10.5, 25.1) |
| Temperature, °C | 10.6 (9.0, 13.3) |
| Cumulative precipitation, m | 1.2 (1.0, 1.3) |
Total admissions included in this table are primary admissions we used for this study after restriction criteria (described in Methods, Data Source & Study Population);
Other combined races include Asians/Pacific Islanders, Hispanic/Latino, Native Americans and other races;
Other unidentified includes admissions without information on race/ethnicity (In particular, Washington state does not provide information on race/ethnicity);
ZIP code level smoking rate, data source: CDC The Behavioral Risk Factor Surveillance System (BRFSS).
Index of Concentration at the Extremes (high income white households versus low income black households*), data source: Krieger N, Chen JT, Waterman PD. Using the methods of the Public Health Disparities Geocoding Project to monitor COVID-19 inequities and guide action for social justice. Available as of May 15, 2020 at: https://www.hsph.harvard.edu/thegeocodingproject/covid-19-resources
We found significant harmful associations between long-term residential exposure to air pollution and risk of admission due to psychotic disorders. For each IQR increase in exposure to PM2.5 and NO2, we observed an RR of 1.11 (95% CI = 1.09, 1.13) and 1.27 (95% CI = 1.24, 1.31), respectively (Table 2). For each 1 °C increase in long-term residential temperature increase, we observed an RR of 1.03 (95% CI = 1.03, 1.04). For one IQR increase in cumulative precipitation, the RR was 1.02 (95% CI = 1.00, 1.03) (Table 3).
Table 2.
Relative risks of hospitalization for psychotic disorders per interquartile increases in levels of PM2.5 (μg/m3), NO2 (ppb) in total study population and stratified by sex, age range, area level poverty, percent of blacks and Hispanics
| PM2.5 | NO2 | |||
|---|---|---|---|---|
| Group | RRa | 95% CI | RR | 95% CI |
| Total | 1.11 | 1.09, 1.13 | 1.27 | 1.24, 1.31 |
| Sex | ||||
| Male | 1.11 | 1.08, 1.13 | 1.33 | 1.28, 1.37 |
| Female | 1.14 | 1.12, 1.16 | 1.24 | 1.20, 1.27 |
| P for differenceb | 0.062 | 0.001 | ||
| Age range | ||||
| Younger age <30 years | 1.00 | 0.97, 1.02 | 1.28 | 1.24, 1.32 |
| Older age >=30 years | 1.17 | 1.14, 1.19 | 1.30 | 1.26, 1.34 |
| P for difference | <0.001 | 0.438 | ||
| Poor vs. less poor areasc | ||||
| Poor | 1.29 | 1.24, 1.34 | 1.42 | 1.33, 1.51 |
| Less poor | 1.00 | 0.98, 1.02 | 1.19 | 1.16, 1.22 |
| P for difference | <0.001 | 0.001 | ||
| Percent of Blacksd | ||||
| High | 1.08 | 1.05, 1.11 | 1.07 | 1.02, 1.13 |
| Low | 1.08 | 1.05, 1.11 | 1.17 | 1.14, 1.21 |
| P for difference | 0.387 | <0.001 | ||
| Percent of Hispanicse | ||||
| High | 1.18 | 1.14, 1.22 | 1.18 | 1.11, 1.25 |
| Low | 1.02 | 0.99, 1.04 | 1.21 | 1.18, 1.23 |
| P for difference | <0.001 | <0.001 | ||
Relative risks (RR) of hospitalization for psychotic disorders per interquartile (IQR) increase in PM2.5 (μg/m3) and NO2 (ppb);
P value for effect heterogeneity (difference) z test between the comparison sub-groups;
Poor areas defined as above 67% percentile of community poverty level, less poor areas defined as less than 67% percentile of community poverty level;
High indicates high percent of blacks in the area vs. low indicates (relatively) low percent of blacks in the area using 67% as the cutoff;
High indicates high percent of Hispanics in the area vs. low indicates (relatively) low percent of Hispanics in the area using 67% as the cutoff;
Analyses were conducted for areas with population on the subgroup based on multi-exposure model including air pollutants, temperature, precipitation, relative humidity, daylight intensity, admission state, admission year, population density, area-level long-term socioeconomic, healthcare access and behavioral factors as described in Covariates section.
Table 3.
Relative risks of hospitalization for psychotic disorders per 1 °C increase in temperature and per interquartile increase in cumulative precipitation (mm) in total study population and stratified by sex, age range, area level poverty, percent of blacks and Hispanics
| Temperature | Precipitation | |||
|---|---|---|---|---|
| Group | RRa | 95% CI | RR | 95% CI |
| Total | 1.03 | 1.03, 1.04 | 1.02 | 1.00, 1.03 |
| Sex | ||||
| Male | 1.02 | 1.02, 1.03 | 1.01 | 0.99, 1.04 |
| Female | 1.01 | 1.01, 1.02 | 1.02 | 0.99, 1.05 |
| P for differenceb | 0.053 | 0.617 | ||
| Age range | ||||
| Younger age <30 years | 1.01 | 1.00, 1.02 | 1.01 | 0.98, 1.05 |
| Older age >=30 years | 1.03 | 1.02, 1.03 | 1.01 | 0.99, 1.03 |
| P for difference | 0.001 | 0.965 | ||
| Poor vs. less poor areasc | ||||
| Poor | 1.04 | 1.03, 1.05 | 0.90 | 0.87, 0.93 |
| Less poor | 1.03 | 1.02, 1.04 | 1.07 | 1.05, 1.09 |
| P for difference | 0.141 | <0.001 | ||
| Percent of Blacksd | ||||
| High | 1.02 | 1.01, 1.03 | 1.04 | 1.02, 1.06 |
| Low | 1.03 | 1.02, 1.03 | 1.02 | 1.00, 1.05 |
| P for difference | 0.455 | 0.074 | ||
| Percent of Hispanicse | ||||
| High | 1.00 | 0.99, 1.01 | 1.00 | 0.98, 1.02 |
| Low | 1.05 | 1.04, 1.06 | 1.02 | 1.00, 1.05 |
| P for difference | <0.001 | 0.216 | ||
Relative risks (RR) of hospitalization for psychotic disorders per interquartile (IQR) increase in cumulative precipitation (mm) level, and per 1 °C increase in ambient temperature;
P value for effect heterogeneity (difference) z test between the comparison sub-groups;
Poor areas defined as above 67% percentile of community poverty level, less poor areas defined as less than 67% percentile of community poverty level;
High indicates high percent of blacks in the area vs. low indicates (relatively) low percent of blacks in the area using 67% as the cutoff;
High indicates high percent of Hispanics in the area vs. low indicates (relatively) low percent of Hispanics in the area using 67% as the cutoff;
Analyses were conducted for areas with population on the subgroup based on multi-exposure model including air pollutants, temperature, precipitation, relative humidity, daylight intensity, admission state, admission year, population density, area-level long-term socioeconomic, healthcare access and behavioral factors as described in Covariates section.
In our stratified analysis (Table 2 & 3), we found that sex significantly modified the associations between long-term exposure to NO2 and risk of psychotic admission with males being more affected. Each IQR increase in the long-term average exposure to NO2 was associated with an RR of 1.33 (95% CI = 1.28 – 1.37) among males vs. 1.24 (95% CI = 1.20 – 1.27) among females (P for difference = 0.001). In addition, older age residents (>= 30 yrs.) were more sensitive to particle air pollution and ambient temperature. In particular, per IQR increase in long-term average PM2.5 was associated with an RR of 1.17 (95% CI = 1.14, 1.19) in older age group while the estimate was not significant in younger age group (RR = 1.00; 95% CI = 0.97, 1.02). We also found population living in poor areas were, in general, more susceptible to air pollution (both PM2.5 and NO2) as compared to those in less poor areas (P for difference <0.001, = 0.001 respectively). Population living in areas with lower percent of blacks was associated with a significantly higher risk (RR = 1.17, 95% CI = 1.14, 1.21) from NO2 as compared with those in areas with higher percent of blacks (RR = 1.07, 95% CI = 1.02, 1.13) (P for difference <0.001). Area level percent of Hispanics also modified the associations between two air pollutants, temperature and risk of admission for psychotic disorders. Interestingly, while we saw a marginally positive RR estimate for cumulative precipitation in the total population, there was effect heterogeneity of precipitation by area level poverty level. Among population living in areas with higher poverty level, we observed a negative association with the outcome risk. However, among population living in areas with lower poverty level, we observed a positive association with the outcome risk.
Figure 1 showed the exposure – response relationships between each of our ambient exposures and risk of hospital admission in our study population. The curve was close to linear for PM2.5. For NO2, the curve had a slightly downward trend before about 10 ppb and then linearly increased. Temperature also followed a close to linear relationship with the RR of hospitalization with the slope of the curve slightly decreased after around 10 °C. For cumulative precipitation, the curve was linear before around 1000 mm and then flattened after that.
Figure 1. Exposure – response curves for the associations between ambient exposures and risk for hospitalization due to psychotic disorders.
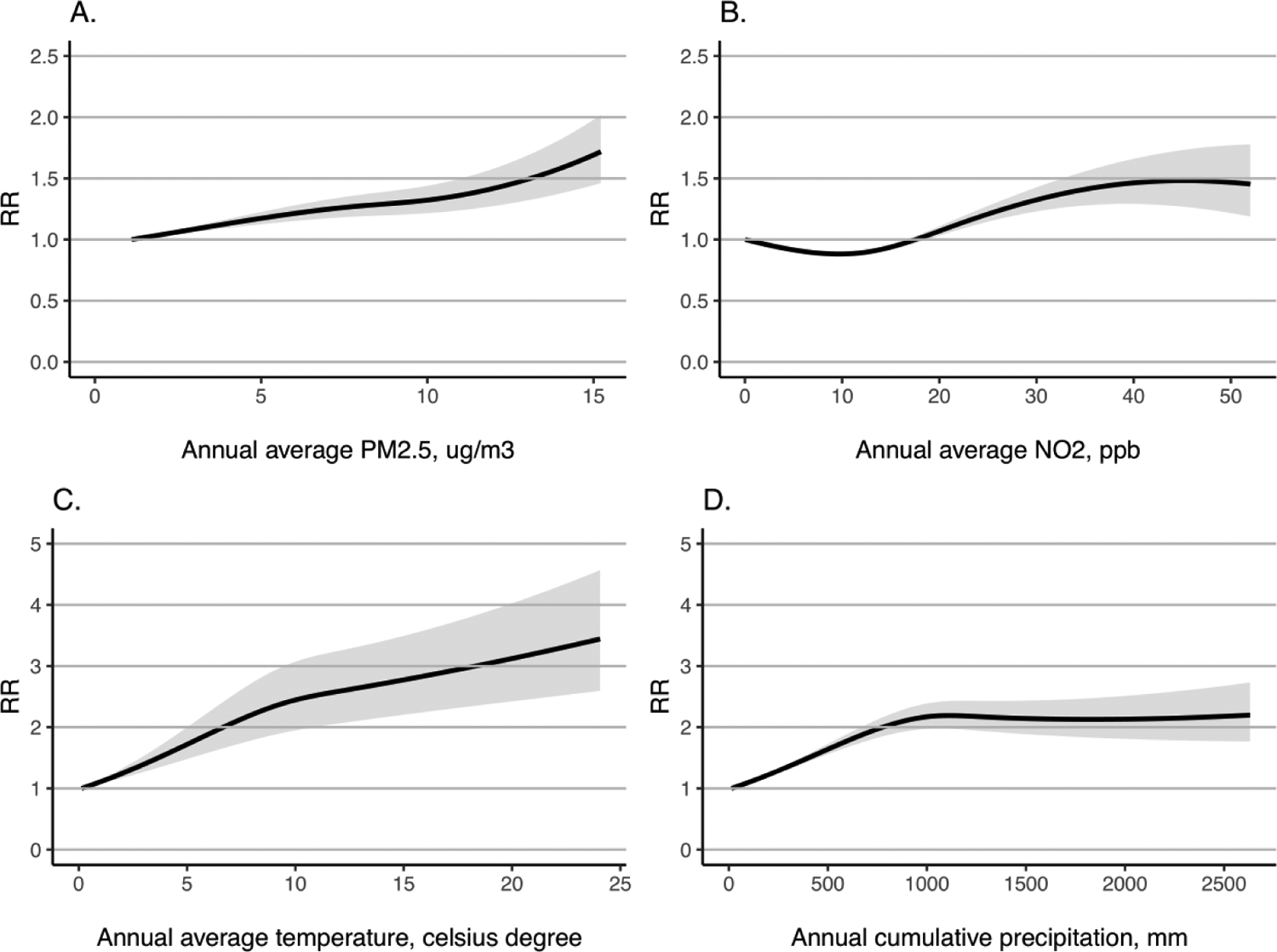
a The relative risks (RRs) are based on calculation using the lowest level for each exposure as the reference group. Black solid lines indicate point estimates. Grey shaded areas indicate 95% confidence interval.
The state-specific results indicated the existence of spatial effect heterogeneity by admission state (Figure 2). Overall, we observed significantly harmful or null associations between long-term average residential exposure to NO2, temperature and precipitation for most of the included states we studied. There is more heterogeneity in the associations for PM2.5 with some protective associations showing up in the state of AZ, NC and RI.
Figure 2.
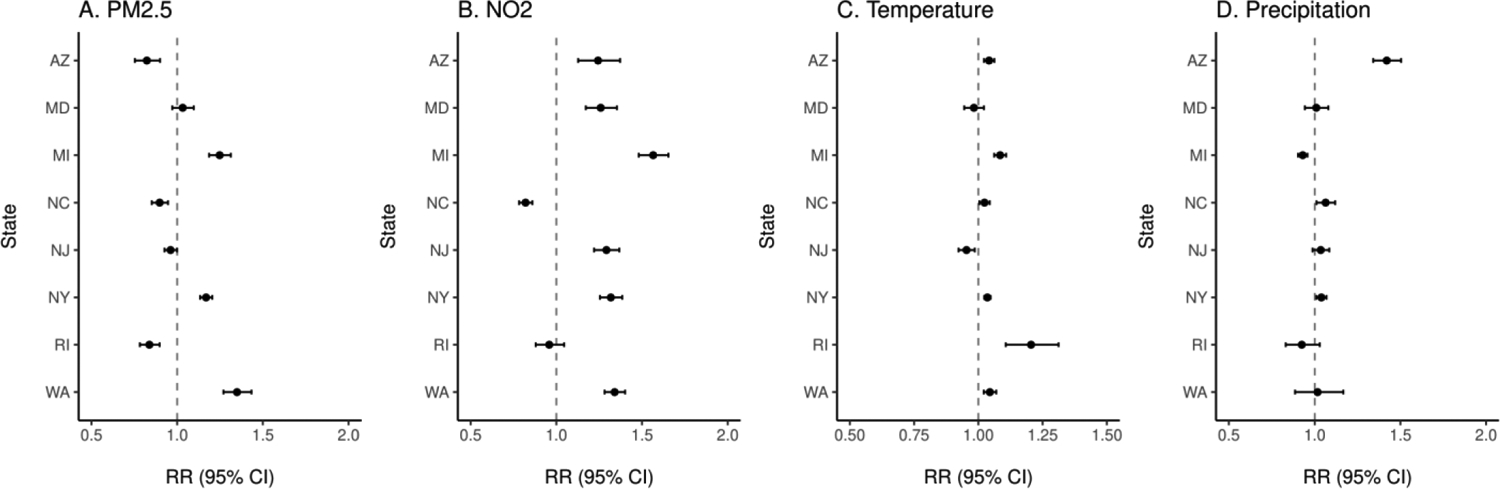
State-specific relative risks (RR) and 95% confidence intervals (95% CI) of hospitalization for psychotic disorders per interquartile increases in long-term annual average levels of A. PM2.5 (μg/m3), B. NO2 (ppb), per 1 °C increase in C. temperature (°C) and per interquartile increase in D. cumulative precipitation (mm) in total study population.
In sensitivity analyses, results remained robust under different settings. In the step-by-step adjustment modeling for the exposures, PM2.5, NO2 and temperature remained significantly associated (eTable 1 in the Supplement). The estimates were stronger in single-exposure setting for both air pollutants but may be biased from residual confounding by co-exposures. Climate conditions may influence the effect of air pollution on health outcomes. In this study, we found the association between NO2 and risk of admission for psychotic disorders was significantly strengthened in high temperature and low precipitation conditions (P for difference =0.006, <0.001, respectively). Besides, PM2.5 was only significantly associated with risk of psychotic admission in high temperature and low precipitation conditions. Further details were presented in eTable 2 in the Supplement. Our main findings remained robust when we tried truncation on alternative minimum area residents size and exposure upper extremes (<99.5th) (eTable 3 in the Supplement). The state-specific relative risk estimates related to Figure 2 can be found in eTable 4 in the Supplement. The main as well as subgroup associations between increased exposure to annual average daily solar radiation level and outcome risk can be found in eTable 5 in the Supplement. Overall, we found that increases in long-term average daily solar radiation level was associated with reduced risk of admission for psychotic disorders without adjusting for air pollutants, temperature and precipitation. However, the estimates were attenuated towards the null when we controlled for temperature, precipitation and further for air pollutants. There was also effect heterogeneity by residence state, area percent of poverty, percent of blacks and Hispanics. Exposure – response relationship for solar radiation can be found in eFigure 3 in the Supplement.
4. Discussion
In this population-based study covering all-age residents of eight U.S. states, we observed population living in areas with higher levels of air pollution and ambient temperature experienced a higher risk of inpatient care for psychotic disorders while the associations for cumulative precipitation was marginally harmful. The above findings were observed after accounting for ambient co-exposures, admission state, admission year, population density, area-level long-term socioeconomic, healthcare access and psychosocial/behavioral factors (such as smoking rate, income extreme index). Due to the high-prevalence and universal exposure to ambient environment, the attributable risk difference and additional admissions associated with increased exposure to harmful ambient environment are not negligible. In addition, the observed associations were further amplified in certain sex/age subpopulations, and in people living in economically disadvantaged areas. Although inpatient care usually represent the more severe cases, our findings represent the risk of the outcome in the entire population of the eight states. Necessarily, they do not indicate the associations for less severe psychopathologies that do not result in hospitalization, and those outcomes should be investigated as well.
Evidence supporting a meaningful link between air pollution and psychiatric health related outcomes is growing worldwide, including from North America,39 East Asia7, 40 and Europe.41–43 In a time-series analysis looking at the association between fine particles and mental health-related emergency department visits in California, same-day mean PM2.5 was associated with a 0.42% (95% CI, 0.14% - 0.70%) increase in all mental health visits.44 In this study, we also found evidence supporting the link between residential exposure to higher levels of PM2.5, and in particular, risk of hospitalization for psychotic disorders. A prospective longitudinal survey study conducted in South East London found, in their multivariate model, IQR increases in PM2.5 and NO2 were associated with an odds ratio (OR) of 1.18 (95% CI, 1.02 – 1.37) and 1.39 (95% CI, 1.05 – 1.85) in risk of common mood disorders (CMD) but no significant associations with the risk of psychotic experiences.41 In comparison, per IQR increase in exposure to PM2.5 (3.6 μg/m3) and NO2 (14.6 ppb), we observed an RR of 1.11 (95% CI = 1.09, 1.13) and 1.27 (95% CI = 1.24 – 1.31) of psychotic disorder-related hospitalization looking at the U.S. population. Although the related evidence on air pollution and psychiatric health is increasing in recently years, we found it difficult to have directly comparable studies in that they differed in the designs of the exposure/outcome assessment, study population/locations as well as covariates adjustment.
As a recent review pointed out, there appears to be strong evidence supporting that climate change can adversely impact population mental health.45 Using sample of nearly 2 million randomly sampled US residents between 2002 and 2012, researchers from the Media Lab of Massachusetts Institute of Technology found that each 1 °C increase of 5-year warming associated with a 2% point increase in the prevalence of mental health issues in the U.S. residents.46 This is close to what we observed in this study although our estimation was based on admission for psychotic disorders (RR = 1.03, 95% CI =1.03, 1.04 per 1 °C increase of long-term average residential temperature level).
In this study, sex was observed to strongly modify the associations between NO2 exposure and risk of hospitalization for psychotic disorders with males being more sensitive. Similar findings were reported in previous studies looking at acute effects of NO2 on admission risk for schizophrenia.47 This might be related with sex-dependent toxicological mechanism of NO2 on human nervous system. Recent mice-based animal study has suggested that NO2 inhalation can damage the ultrastructure of myelin sheath and cause abnormal expression of associated genes for mental disorders in male mice. In addition, the level of prolactin (Prl) might also play a major role in the sex-specific neurobehavioral responses.48 We also observed that adults over 30 yrs. were associated with a higher risk increase in admission risk when exposed to increases in residential fine particulate matter and ambient temperature. This could indicate higher physiological sensitivity of older individuals to ambient exposures or better ability of them to get inpatient care for psychotic experiences as compared with younger adults. Further studies are needed to test and explain these findings. Interestingly, we observed population in poor areas were more affected by air pollution. Previously, mental health disparity from air pollution was observed with the associations stronger among individuals with lower SES.39 The observed susceptibility for people living in poorer areas could stem from multiple risk factors, i.e. higher levels of stress from economic disadvantages, weaker community response to the environmental changes and less social cohesion, all of which could predispose the residents to a higher risk of developing or worsening of psychiatric problems, including psychotic disorders. In addition, people living in socioeconomically disadvantaged areas and worse psychosocial conditions are potentially at a higher stress and pre-neuroinflammatory stage.4 Therefore, external toxic and inflammatory triggers, such as air pollution, can more easily trigger inflammation and cause mental outbreaks among them. They are also observed to live in neighborhoods with poorer air quality, houses with weaker protection from adverse climate events and have limited access to mental healthcare services.49–51 All of these underlying factors reduce their resilience to environmental hazards and stressors. However, area poverty seemed to act differently in the case of modifying the effect of cumulative precipitation. A protective link between increased precipitation level and a reduced outcome risk was observed among population living in poor areas. Possible reasons remain unclear and more precipitation focused studies are needed to further explore this finding. We also saw mixed results of modification by area level percent of blacks and Hispanics depending on the exposures. Areas with lower percent of blacks (usually white dominant communities) are associated with significantly higher risk of admission when exposed to higher levels of NO2. However, such a difference was not shown when we looked at exposure to PM2.5, temperature or precipitation. This finding is somewhat consistent with one recent study looking at long-term exposure to NO2 and risk of mortality among the Southeastern US elderly population.52 In the mortality study, the authors found a higher average risk of mortality related to exposure to NO2 among White populations when compared with other races. Area level percent of Hispanics also modified the exposure – outcome associations. Areas of higher percent of Hispanics are associated with higher risk of admission for increased exposure to PM2.5. This could be due to that areas of higher percent of Hispanics are usually more economically disadvantaged areas. Unlike PM2.5, areas of higher percent of Hispanics are not significantly affected by increased ambient temperature as seen in the total population or population living in areas with lower percent of Hispanics. This may indicate higher adaptability to warmer temperature among Hispanic Americans since they or their ancestors usually came from warm geographical locations, such as Mexico or other Latin American countries. Similar null associations for temperature increase/heat and health outcomes among Hispanics were also seen in other studies.53, 54
Our state-specific results indicated the existence of spatial effect heterogeneity by admission state. More heterogeneity was observed for the effect of long-term PM2.5 exposure. This could be due to the particle composition/toxicity difference across the different states, as well as more potential residual confounding by unmeasured area-level factors for this particular exposure. Overall, we observed significantly harmful or null associations between long-term average residential exposure to NO2, temperature and cumulative precipitation for most of the included states. More regional studies are needed to further explore these findings. Further discussion on the exposure – response relationship, climate – air pollution interaction as well as the solar radiation findings is provided in eDiscussion in the Supplement.
The unique contributions of this study lie in the following aspects. First, the current evidence on air pollution, climate and psychiatric health outcomes is more commonly investigated in short-term periods using a time series or case-crossover study design to see if there are acute effects on triggering psychiatric episodes. In this study, we provide direct evidence on the additional risk of hospitalization due to psychotic disorders for population living in areas with higher long-term average air pollution and temperature levels. This provides more direct guidance on the long-term regulation of air pollution levels and climate mitigation for the communities. Second, many of the existing air pollution focused studies have not considered the role of climate co-exposures, such as temperature, precipitation and solar radiation, and did not sufficiently control for them in their modeling. This could result in substantial bias in the accuracy of the effect estimation since climate exposures, especially temperature, are also important contributors to the outcome risk. Third, the sub-group/area analyses provide evidence to help identify potential vulnerable populations and communities. In this study, we identified that older age population as well as those living in poor areas are more affected. More efforts should be devoted to these susceptible populations and areas. Last, we also explored the exposure – response relationships between air pollution, climate exposures and outcome risk, which is lacking in the current literature.
This study also has its limitations. First, exposure misclassification is likely due to the assignment of area-level ambient exposures based on the participants residential addresses. However, people tend to conduct most of their activities in or near where they live, and ambient exposures are usually regional exposures that cover large areas and population. Second, residual confounding is likely from other co-exposures, community-level psychosocial factors, greenness or noise55 that we do not have information on. Yet, in order for these factors to act as confounders, they ought to be associated with the ambient exposures. Further studies with more comprehensive confounding adjustment are warranted. Third, ecological bias is likely in this study since we analyzed the aggregated admission counts per population by ZIP codes, which may not properly reflect the individual-level associations.56 However, the geographical coverage of a ZIP code is not large, such as in city level analysis, and has fewer within-area differences in background rates. Last, the outcome hospitalization rates could be spatially auto-correlated, meaning that the ZIP code near each other within a state are likely to have more similar admission rates. While the robust confidence intervals we used from sandwich variance estimators are robust to auto-correlation, residual effects on the precision of the RR estimates is possible.
5. Conclusions
In psychiatric epidemiology, little attention has been paid to the possible harmful effects from the physical environment, even though it may have the broadest impact on population health. We demonstrate that living in areas with higher long-term average exposure to air pollutants and certain climatic conditions (i.e. higher ambient temperature) could contribute to additional risk of hospitalization for psychotic disorders in a U.S. general population covering the residents of eight states. More efforts should be devoted to help ease the additional psychiatric healthcare burden via strict air pollutants regulation and climate mitigation.
Supplementary Material
Highlights.
This study covered residents of eight US states from children to elderly.
A total of 1,211,100 admissions for psychotic disorders were identified.
PM2.5, NO2, temperature increase is linked with higher admission risk.
Precipitation was adjusted and also investigated as an exposure.
Disparities were found by demographical and contextual backgrounds.
Acknowledgements
This work was supported by National Institute of Environmental Health Sciences (NIEHS) grants (P30-ES-000002, R01-ES-032418-01) and US Environmental Protection Agency (EPA) grant (RD-83615601). Its contents are solely the responsibility of the grantee and do not necessarily represent the official views of the USEPA. Further, USEPA does not endorse the purchase of any commercial products or services mentioned in the publication. The funders had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. We want to specially thank U.S. Agency for Healthcare Research and Quality Health Cost and Utilization Project (HCUP) for giving us access to the State Inpatient Databases (SIDs) to conduct this study. Dr. Qiu, the first and corresponding author of the study, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Publisher's Disclaimer: This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of Interest
All the authors report no conflicts of interest.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Informed consent was obtained for experimentation with human subjects. The privacy rights of human subjects were observed. The institutional review board for human subjects or animal research at Harvard University has reviewed and approved this study.
Data availability
The State Inpatient Databases are not publically available since it is level 3 and above confidential data. Researchers interested in using the data can submit their data use request and purchase the data from U.S. Agency for Healthcare Research and Quality Health Cost and Utilization Project. The air pollution, climate exposures and covariates data will be made available upon request.
References
- 1.Attademo L, Bernardini F. Air Pollution as Risk Factor for Mental Disorders: In Search for a Possible Link with Alzheimer’s Disease and Schizophrenia. Journal of Alzheimer’s disease : JAD 2020;76(3):825–830. [DOI] [PubMed] [Google Scholar]
- 2.Braithwaite I, Zhang S, Kirkbride JB, Osborn DPJ, Hayes JF. Air Pollution (Particulate Matter) Exposure and Associations with Depression, Anxiety, Bipolar, Psychosis and Suicide Risk: A Systematic Review and Meta-Analysis. Environmental health perspectives Dec 2019;127(12):126002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tallon LA, Manjourides J, Pun VC, Salhi C, Suh H. Cognitive impacts of ambient air pollution in the National Social Health and Aging Project (NSHAP) cohort. Environment international Jul 2017;104:102–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thomson EM. Air Pollution, Stress, and Allostatic Load: Linking Systemic and Central Nervous System Impacts. Journal of Alzheimer’s disease : JAD 2019;69(3):597–614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thomson EM, Filiatreault A, Guénette J. Stress hormones as potential mediators of air pollutant effects on the brain: Rapid induction of glucocorticoid-responsive genes. Environmental research Nov 2019;178:108717. [DOI] [PubMed] [Google Scholar]
- 6.Tost H, Champagne FA, Meyer-Lindenberg A. Environmental influence in the brain, human welfare and mental health. Nature neuroscience Oct 2015;18(10):1421–1431. [DOI] [PubMed] [Google Scholar]
- 7.Xue T, Guan T, Zheng Y, Geng G, Zhang Q, Yao Y, Zhu T. Long-term PM(2.5) exposure and depressive symptoms in China: A quasi-experimental study. The Lancet regional health Western Pacific Jan 2021;6:100079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoo EH, Eum Y, Gao Q, Chen K. Effect of extreme temperatures on daily emergency room visits for mental disorders. Environmental science and pollution research international Aug 2021;28(29):39243–39256. [DOI] [PubMed] [Google Scholar]
- 9.Yoo EH, Eum Y, Roberts JE, Gao Q, Chen K. Association between extreme temperatures and emergency room visits related to mental disorders: A multi-region time-series study in New York, USA. The Science of the total environment Jun 8 2021;792:148246. [DOI] [PubMed] [Google Scholar]
- 10.Shi L, Wu X, Danesh Yazdi M, et al. Long-term effects of PM(2·5) on neurological disorders in the American Medicare population: a longitudinal cohort study. The Lancet Planetary health Dec 2020;4(12):e557–e565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernardini F, Trezzi R, Quartesan R, Attademo L. Air Pollutants and Daily Hospital Admissions for Psychiatric Care: A Review. Psychiatric services (Washington, DC) Dec 1 2020;71(12):1270–1276. [DOI] [PubMed] [Google Scholar]
- 12.Gu X, Guo T, Si Y, et al. Association between ambient air pollution and daily hospital admissions for depression in 75 Chinese cities. American Journal of Psychiatry 2020;177(8):735–743. [DOI] [PubMed] [Google Scholar]
- 13.Lee S, Lee W, Kim D, Kim E, Myung W, Kim SY, Kim H. Short-term PM(2.5) exposure and emergency hospital admissions for mental disease. Environmental research Apr 2019;171:313–320. [DOI] [PubMed] [Google Scholar]
- 14.Bai L, Zhang X, Zhang Y, et al. Ambient concentrations of NO(2) and hospital admissions for schizophrenia. Occupational and environmental medicine Feb 2019;76(2):125–131. [DOI] [PubMed] [Google Scholar]
- 15.Pelgrims I, Devleesschauwer B, Guyot M, et al. Association between urban environment and mental health in Brussels, Belgium. BMC public health Apr 1 2021;21(1):635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Antonsen S, Mok PL, Webb RT, et al. Exposure to air pollution during childhood and risk of developing schizophrenia: a national cohort study. The Lancet Planetary Health 2020;4(2):e64–e73. [DOI] [PubMed] [Google Scholar]
- 17.Guilarte TR, Opler M, Pletnikov M. Is lead exposure in early life an environmental risk factor for Schizophrenia? Neurobiological connections and testable hypotheses. Neurotoxicology 2012;33(3):560–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marchetti C. Interaction of metal ions with neurotransmitter receptors and potential role in neurodiseases. Biometals 2014;27(6):1097–1113. [DOI] [PubMed] [Google Scholar]
- 19.Solarz A, Majcher-Maślanka I, Kryst J, Chocyk A. A Search for Biomarkers of Early-life Stress-related Psychopathology: Focus on 70-kDa Heat Shock Proteins. Neuroscience May 21 2021;463:238–253. [DOI] [PubMed] [Google Scholar]
- 20.Wortzel JR, Norden JG, Turner BE, Haynor DR, Kent ST, Al-Hamdan MZ, Avery DH, Norden MJ. Ambient temperature and solar insolation are associated with decreased prevalence of SSRI-treated psychiatric disorders. Journal of psychiatric research Mar 2019;110:57–63. [DOI] [PubMed] [Google Scholar]
- 21.Gupta A, Sharma P, Garg V, Singh A, Mondal S. Role of serotonin in seasonal affective disorder. Eur Rev Med Pharmacol Sci 2013;17(1):49–55. [PubMed] [Google Scholar]
- 22.Lieberman JA, First MB. Psychotic Disorders. The New England journal of medicine Jul 19 2018;379(3):270–280. [DOI] [PubMed] [Google Scholar]
- 23.Understanding Psychosis. Available at: https://www.nimh.nih.gov/health/publications/understanding-psychosis.
- 24.Jongsma HE, Turner C, Kirkbride JB, Jones PB. International incidence of psychotic disorders, 2002–17: a systematic review and meta-analysis. The Lancet Public health May 2019;4(5):e229–e244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hjorthøj C, Stürup AE, McGrath JJ, Nordentoft M. Years of potential life lost and life expectancy in schizophrenia: a systematic review and meta-analysis. The lancet Psychiatry Apr 2017;4(4):295–301. [DOI] [PubMed] [Google Scholar]
- 26.Whiteford HA, Degenhardt L, Rehm J, et al. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet (London, England) Nov 9 2013;382(9904):1575–1586. [DOI] [PubMed] [Google Scholar]
- 27.Rössler W, Salize HJ, van Os J, Riecher-Rössler A. Size of burden of schizophrenia and psychotic disorders. European neuropsychopharmacology : the journal of the European College of Neuropsychopharmacology Aug 2005;15(4):399–409. [DOI] [PubMed] [Google Scholar]
- 28.HCUP. HCUP Databases. Healthcare Cost and Utilization Project (HCUP). www.hcup-us.ahrq.gov/sidoverview.jsp.: Agency for Healthcare Research and Quality, Rockville, MD; April 2021. [Google Scholar]
- 29.Di Q, Amini H, Shi L, et al. An ensemble-based model of PM(2.5) concentration across the contiguous United States with high spatiotemporal resolution. Environment international Sep 2019;130:104909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Di Q, Amini H, Shi L, et al. Assessing NO(2) Concentration and Model Uncertainty with High Spatiotemporal Resolution across the Contiguous United States Using Ensemble Model Averaging. Environmental science & technology Feb 4 2020;54(3):1372–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kalnay E, Kanamitsu M, Kistler R, et al. The NCEP/NCAR 40-year reanalysis project. Bulletin of the American meteorological Society 1996;77(3):437–472. [Google Scholar]
- 32.Thornton MM, Shrestha R, Wei Y, Thornton PE, Kao S, Wilson BE. Daymet: Annual Climate Summaries on a 1-km Grid for North America, Version 4. 10.3334/ORNLDAAC/1852: ORNL DAAC; 2020. [DOI] [Google Scholar]
- 33.CMS. Chronic Conditions Data Warehouse CCW Chronic Conditions Categories. Available at: https://www2.ccwdata.org/web/guest/condition-categories.
- 34.BureauUC. Summary File 3; 2000.
- 35.BureauUC. Census Demographic Profile Summary File; 2010.
- 36.NationalResearchCouncil. Using the American Community Survey: benefits and challenges: National Academies Press; 2007. [Google Scholar]
- 37.Long JS. Regression models for categorical and limited dependent variables. Vol 7: Sage; 1997. [Google Scholar]
- 38.Hinkle DE, Wiersma W, Jurs SG. Applied statistics for the behavioral sciences. Vol 663: Houghton Mifflin College Division; 2003. [Google Scholar]
- 39.Pun VC, Manjourides J, Suh H. Association of Ambient Air Pollution with Depressive and Anxiety Symptoms in Older Adults: Results from the NSHAP Study. Environmental health perspectives Mar 2017;125(3):342–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wang R, Liu Y, Xue D, Yao Y, Liu P, Helbich M. Cross-sectional associations between long-term exposure to particulate matter and depression in China: The mediating effects of sunlight, physical activity, and neighborly reciprocity. Journal of affective disorders Apr 15 2019;249:8–14. [DOI] [PubMed] [Google Scholar]
- 41.Bakolis I, Hammoud R, Stewart R, et al. Mental health consequences of urban air pollution: prospective population-based longitudinal survey. Social psychiatry and psychiatric epidemiology Oct 24 2020:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Altuğ H, Fuks KB, Hüls A, Mayer AK, Tham R, Krutmann J, Schikowski T. Air pollution is associated with depressive symptoms in elderly women with cognitive impairment. Environment international Mar 2020;136:105448. [DOI] [PubMed] [Google Scholar]
- 43.Vert C, Sánchez-Benavides G, Martínez D, et al. Effect of long-term exposure to air pollution on anxiety and depression in adults: A cross-sectional study. International journal of hygiene and environmental health Aug 2017;220(6):1074–1080. [DOI] [PubMed] [Google Scholar]
- 44.Nguyen AM, Malig BJ, Basu R. The association between ozone and fine particles and mental health-related emergency department visits in California, 2005–2013. PloS one 2021;16(4):e0249675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Cianconi P, Betrò S, Janiri L. The impact of climate change on mental health: a systematic descriptive review. Frontiers in psychiatry 2020;11:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Obradovich N, Migliorini R, Paulus MP, Rahwan I. Empirical evidence of mental health risks posed by climate change. Proceedings of the National Academy of Sciences 2018;115(43):10953–10958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Duan J, Cheng Q, Luo X, et al. Is the serious ambient air pollution associated with increased admissions for schizophrenia? The Science of the total environment Dec 10 2018;644:14–19. [DOI] [PubMed] [Google Scholar]
- 48.Li D, Ji S, Guo Y, Sang N. Ambient NO(2) exposure sex-specifically impairs myelin and contributes to anxiety and depression-like behaviors of C57BL/6J mice. Journal of hazardous materials Aug 15 2021;416:125836. [DOI] [PubMed] [Google Scholar]
- 49.Hajat A, Hsia C, O’Neill MS. Socioeconomic Disparities and Air Pollution Exposure: a Global Review. Current environmental health reports Dec 2015;2(4):440–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Paavola J. Health impacts of climate change and health and social inequalities in the UK. Environmental health : a global access science source Dec 5 2017;16(Suppl 1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Balbus JM, Malina C. Identifying vulnerable subpopulations for climate change health effects in the United States. Journal of occupational and environmental medicine Jan 2009;51(1):33–37. [DOI] [PubMed] [Google Scholar]
- 52.Qian Y, Li H, Rosenberg A, et al. Long-term exposure to low-level NO 2 and mortality among the elderly population in the southeastern United States. Environmental health perspectives 2021;129(12):127009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Basu R, Ostro BD. A multicounty analysis identifying the populations vulnerable to mortality associated with high ambient temperature in California. American journal of epidemiology 2008;168(6):632–637. [DOI] [PubMed] [Google Scholar]
- 54.Hansen A, Bi L, Saniotis A, Nitschke M. Vulnerability to extreme heat and climate change: is ethnicity a factor? Global health action 2013;6(1):21364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tzivian L, Winkler A, Dlugaj M, Schikowski T, Vossoughi M, Fuks K, Weinmayr G, Hoffmann B. Effect of long-term outdoor air pollution and noise on cognitive and psychological functions in adults. International journal of hygiene and environmental health Jan 2015;218(1):1–11. [DOI] [PubMed] [Google Scholar]
- 56.Greenland S, Morgenstern H. Ecological bias, confounding, and effect modification. International journal of epidemiology 1989;18(1):269–274. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The State Inpatient Databases are not publically available since it is level 3 and above confidential data. Researchers interested in using the data can submit their data use request and purchase the data from U.S. Agency for Healthcare Research and Quality Health Cost and Utilization Project. The air pollution, climate exposures and covariates data will be made available upon request.


