Abstract
Genetics has begun to be considered a key medical discipline which can have an impact on everyday clinical practice. Therefore, it is necessary to understand what the most effective way is of caring for people affected by or at risk of genetic disorders. In this context, the team dealing with such patients has evolved with the emergence of the Genetic Counsellor figure. The profession of Genetic Counsellor appeared in Europe in 1980, but it is still a much-debated profession and not yet recognized in all European countries. The aim of this research is to investigate both how a team should be composed in the care of patients affected by or at risk of genetic disorders and what the role of the Genetic Counsellor should be—the field of action and the competences. The research has been carried out at the European level, submitting an online questionnaire to geneticists who, having the ultimate responsibility for the diagnosis and being in the field for the longest time, expressing their opinion, can identify strengths and potential areas for improvement in genetic care. 200 responses were collected from all over Europe. This led to awareness of the importance of the role of the counsellor within the medical genetics multidisciplinary team, and, above all, what the counsellor’s skills and qualifications should be—for geneticists. Although this new profession has difficulties in being recognized in some countries, it seems clear that these highly competent professionals are essential for in-patient care and in the multidisciplinary team.
Subject terms: Genetic counselling, Genetics research, Ethics
Introduction
The rapid genetic development of recent years has addressed the understanding and management of common and rare diseases [1]. It became clear that almost all human diseases had genetic components. Therefore, Genetics begun to be considered a key discipline with an impact on everyday clinical practice [1, 2]. This has led to a growing need for professionals to be able to provide appropriate information to patients and their families about the disease and genetic testing, facilitating the decision-making process and supporting patients to adapt to the disease [3, 4]. This raises the question of who is the best team to care for patients in this new era.
The field of clinical genetics, which used to be solely responsibility of medical doctors, has evolved into a multidisciplinary service where non-medical professionals are an integral part of the team [5]. Nowadays, there are three principal professions involved in the team: medical geneticists (MD), clinical laboratory geneticists and Genetic Counsellors (GCs). All these three profiles are considered essential for providing care to patients. Medical geneticists are the key, longest-serving professionals in the field involved in the diagnosis and clinical management of families with genetic disorders. Their role is to assess, investigate and then diagnose genetic and hereditary medical conditions. Secondly, laboratory geneticists, who have also been in the field for many years and are responsible for the laboratory diagnostics and interpretation. If for these first two subspecialists the role and the fields of competence are clear, defined and recognized; for genetic counsellors however, this process of definition and recognition is not fully completed (especially in Europe). The profession of genetic counselling began in the United States in 1969, although GCs existed for a considerable time. Around 1990, there was a global expansion of the profession itself (appearing in Europe in 1980), bringing other healthcare professionals into genetic counselling, which had previously only been carried out by doctors. In 2019 it has been estimated that there are 7000 people worldwide working as GCs [6].
Many studies have focused on what the counsellor adds to medical care. In the context of providing services to patients with genetic disorders, five strengths – or responsibilities – of the GC have been identified that improve clinical outcomes. These are: “time to talk”, “quality of the relationship”, “local and accessible services”, “yearly follow-up”, “coordinated and tailored family care”. The client-counsellor relationship is fundamental to the clinical outcome, mainly because the trust and relationship established will allow the counsellor to help that specific person, considering his/her uniqueness and accompanying the patient to the best choice for him/her. It is believed that GCs add a more holistic view taking in consideration both the psychosocial and the familial dimensions [7]. At present, the activity of GCs in many countries is clear and well-defined especially in America, where there is a recognized and strictly regulated profession and where the majority of GCs are [8]. Although many GCs now work in research and in specialized laboratories, they are involved mostly in clinical activity concerning all those disorders with hereditary components and potential genetic tests, with the aim of informing patients and helping them both medically and emotionally when facing – or at risk of facing – a genetic condition [8]. Thanks to their training, professional and human experience, GCs can manage the counselling independently and autonomously, without the presence of a medical geneticist, but under medical responsibility and supervision.
Despite this, genetic counselling is still a much-debated profession, especially in Europe; this difference in role between different regions of the world and even different countries within a region may arise from global differences in the profession itself. Internationally there are conceptual similarities in the practice of the profession, but different patterns of training and practice exist. Some of these distinctions include different modules, different durations and areas of training and differences in university background that allows access to specialist training for becoming a GC. In addition to this, differences in the way professionals are registered with professional boards were highlighted [8, 9]. Taking the European situation as a reference, the aim of the European Board of Medical Genetics (EBMG) is to develop and promote academic and professional standards required to ensure the highest possible genetic counselling service [10, 11]. A Master’s degree in genetic counselling is required to be accredited by the EBMG. At present, there are only a limited number of master’s programmes in Europe that train GCs, thus, many professionals who have been in the field for a long time have trained in other ways. Currently, in Europe, there are some countries (e.g., France, Portugal, Romania, Spain, and the United Kingdom) that recognize the profession of GC, while others do not (e.g., Austria, Italy, Belgium, Germany and Portugal).
Objective
The aim of this work is to investigate how genetic counselling should be carried out, how a team should be composed in the care of patients affected by – or at risk of – genetic disorders and what the role of the GC should be.
It is hypothesized:
H1: A different value to actions is assigned depending on whether or not cooperation with the GC has occurred.
H2: The role of the GC is fundamental in the team.
H3: The GC is not recognized as being able to carry out all the actions that characterize counselling sessions.
H4.1: The knowledge of the role of the GC depends on the country of operation.
H4.2: The number of people who have collaborated with the GC differs between countries.
Design and methods
The structure was quali-quantitative research; it was decided to carry out structured interviews of medical geneticists (MD) in Europe by means of a questionnaire administered using the Qualtrics platform XM. The data obtained were processed using the functionalities provided in Qualtrics and with Excel and were analysed using descriptive analysis, T-test and ANOVA (Analysis of Variance).
Medical Geneticists working in European countries were contacted and asked for their willingness to participate in the research by sending an email on 2 July 2021 including:
The link to Qualtrics.
The Participation Information Sheet.
In subsequent reminders (beginning and end of September 2021) it was asked to those geneticists to extend the study by sending the documentation to their medical geneticists’ colleagues. In addition, the social network LinkedIn was used to sponsor the questionnaire (the same documentation was also posted on this platform). For this reason, it is not possible to indicate the precise number of subjects who were asked to participate. The deadline for the compilation of the survey was the 31st of January 2022.
The questionnaire was structured in five sections.
Consent form. Section consisting of three questions (C1–C3) stating the purpose of the study and requesting permission to use the data in anonymous form.
-
Sample characterization. It consists of 8 questions (Q1–Q8) necessary to know the characteristics of the sample: gender, age, sector of work, country of work, years of service, fields of specialization, knowledge of and/or collaboration with the GC. A negative answer to this last question (Q8) constitutes a block for the compilation of the last section.
In the next three sections it was asked to express own perception about:
Counselling procedures. Composed of two questions (Q9 and Q10). The first had 25 statements which were asked to be rated in terms of importance on a Likert scale of 1 to 7 (1: not important at all; 7: essential). To provide an application example, a second question, regarding the opinion on the three main procedures to be carried out in the preconception context was inserted.
Team composition. Section consisting of two questions (Q11 and Q12). In this section it was asked to express on a Likert scale from 1 to 7 (1: not important at all; 7: essential) the importance of the presence of certain professionals within the genetic counselling team. The topic of PGT was specifically addressed.
Role of the GC. Section consisting of three questions (Q13–Q15). This section could only be answered by those who stated collaboration with the GC (Q8). The same statements as in block 3 were carried over and it was asked to express on a Likert scale from 1 to 7 (1: not recommended; 7: highly recommended) which of the activities could be carried out by the GC. A second question reported the main areas of genetic counselling (prenatal, oncogenetic, preconception, etc.) and participants were asked to express, using a Likert scale from 1 to 7 (1: not important at all; 7: essential), in which area the figure of the GC was most beneficial. The last question asked participants to express, using a Likert scale from 1 to 7 (1: unsuitable; 7: perfectly suitable), which background was the most suitable for entering GC master programme.
Results
Within the given time frame (six months), 200 people completed the online survey, and the link was open 570 times.
Sample characterization
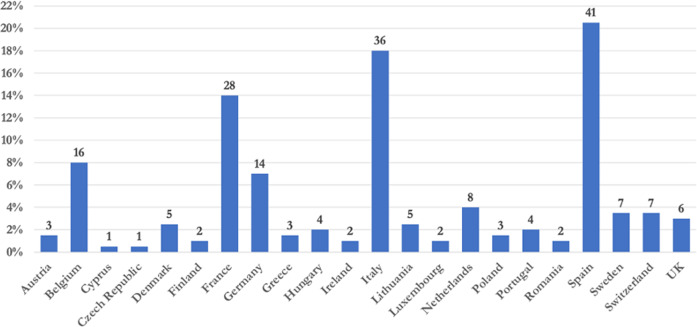
The respondents were mainly female subjects. More than half were aged 40 or under. 70% of the respondents worked in the public sector. More than half of the respondents had a work experience of 10 years or less. The predominant subspecialty in the sample is paediatrics (the participants could choose up to three options). In the option “other” some participants wrote their specialized field, the most frequent being ophthalmology and rare diseases (Supplementary Table 1). Most responses were from Spain, Italy, France, Belgium and Germany (Fig. 1), we assume that this is because there is a greater involvement of doctors from these countries in the networks used to disseminate the questionnaire link. No responses were obtained from Croatia, Estonia, Latvia, Malta, Slovakia, Slovenia, Iceland and Bulgaria, which is why they do not appear in the graph.
Fig. 1. Distribution of the work country of our sample.
On the y-axis is the percentage, on the individual samples the actual number of participants.
Twelve out of 200 (6%) participants were not aware of the existence of GCs and 62 participants in the sample (31%) have never collaborated with a GC, compared to 138 who collaborated or have collaborated with a GC. A negative answer to this latter question prevented the completion of the last three questions of the questionnaire. For the last two questions, a T-test was carried out, all paired differences in the averages of Q7 (Are you aware of the health profession of the GC?) and Q8 (Do you collaborate or have you ever worked with a GC?) were assessed, respectively, against the values of the categorical variable Q4 (In which country do you work?) and Q3 (do you work primarily in public or private sector?), but no difference emerged between knowledge of the GC or working with GC based on the different country of origin of the participants or based on the working sector.
Counselling procedures
All activities were relevant (Table 1), with a minimum average score for the “sample handling” item of 5.04. The sample identified three main activities during genetic counselling, “ensure patients’ understanding of the given genetic information”, “collect information for genetic investigation” and “Draw Pedigree”.
Table 1.
Importance of the main important activities during genetic counselling sections. The mean and standard deviation are shown on the right.
| Actions during counselling | Average | SD |
|---|---|---|
| Ensure the patients’ understanding of the given genetic information | 6.53 | 0.96 |
| Draw Pedigree | 6.50 | 0.99 |
| Collect information for genetic investigation | 6.47 | 0.88 |
| Help patients express their own questions | 6.46 | 0.91 |
| Inform the patient about prenatal testing | 6.34 | 1.14 |
| Make genetic risk assessment | 6.32 | 1.06 |
| Inform the patient about diagnostic testing | 6.27 | 1.24 |
| Inform the patient about reproductive options | 6.24 | 1.24 |
| Inform the patient about presymptomatic testing | 6.23 | 1.26 |
| Inform the patient about test result | 6.16 | 1.47 |
| Guide the patient in making the right decision for themselves | 6.05 | 1.38 |
| Inform the patients about familial risk (without known mutation) | 5.99 | 1.27 |
| Give the patient clinical and medical information | 5.99 | 1.44 |
| Discuss with the patient the potential effect on every-day life | 5.80 | 1.5 |
| Coordinate the care pathway with other health care practitioners as well | 5.78 | 1.53 |
| Provide psychological support to the patient | 5.77 | 1.4 |
| Identify and help patients in crisis | 5.70 | 1.47 |
| Provide follow-up after a clinical visit | 5.65 | 1.53 |
| Literature research | 5.64 | 1.59 |
| Discuss common psychological reactions and feelings | 5.59 | 1.35 |
| Education of the population | 5.45 | 1.52 |
| Inform the patient about genetic variants of unclear significance | 5.43 | 1.68 |
| Make a diagnosis | 5.15 | 2.04 |
| Write referrals | 5.11 | 1.7 |
| Sample handling | 5.04 | 1.74 |
For these 25 statements, ANOVA analyses was carried out. The ANOVA analysis was conducted to test whether the importance attributed to the different aspects examined (Q9_1–Q9_25) was different among the groups who stated that they have/have never collaborated or worked with a GC (answers at Q8). Participants were classified into two groups: No collaboration or work with a GC (n = 62) and those who stated that they had collaborated or worked with a GC (n = 138). Statistical significance emerged in the following activities (Supplementary Table 2).
“Inform the patient about familial risk (without known mutation)”. There was a significant difference (p = 0.014) in the importance given to that activity in the genetic counselling session between those who stated that they had (6.14 ± 1.15) or had not (5.66 ± 1.46) ever worked or collaborated with a GC.
“Inform the patient about pre-symptomatic testing”. There was a significant difference (p = 0.003) in the importance given to that activity in the genetic counselling session between those who stated that they had (6.40 ± 1.04) or had not (5.83 ± 1.59) ever worked or collaborated with a GC.
“Inform the patient about genetic variants of unclear significance”. There was a significant difference (p = 0.048) in the importance given to that activity “in the genetic counselling session between those who stated that they had (5.59 ± 1.57) or had not (5.08 ± 1.85) ever worked or collaborated with a GC.
From the question regarding the most important activities in the PGT process, which is not a compulsory field, 322 responses were obtained. Each participant could indicate up to three preferences. The two main activities mentioned were “Inform about reproductive options” (indicated by 17% of respondents) and “Guide the patient in making the right decision for themselves” (11%). Two activities follow with a score of 9.97%, “Ensure the patients’ understanding of the given genetic information” (7.5%), and “Give the patient clinical and medical information” (5.6%). In the category “other” all items individually have a percentage of less than 5%, including, among the main ones, “Collect information for genetic investigation”, “Inform the patients about familial risk” and “Inform the patient about test result”.
Team composition
The GC (Table 2) was the second most frequently mentioned profession (6.35 ± 1.0). In the category “other”, the role of laboratory technician was most frequently indicated. For these 6 statements, ANOVA analyses were carried out to test whether the importance attributed to the different health practitioners examined (medical geneticist, GC, biologist, psychologist, nurse, administrative) varies between groups who stated that they have/have never collaborated or worked with a GC (Supplementary Table 3).
Table 2.
Importance of professional figures on the team. The mean and the standard deviation are reported on the right.
| Role | Average | SD |
|---|---|---|
| Geneticist | 6.82 | 0.76 |
| Genetic counsellor | 6.35 | 1.05 |
| Biologist | 5.66 | 1.61 |
| Psychologist | 5.54 | 1.43 |
| Administrative | 4.88 | 1.82 |
| Nurse | 4.81 | 1.74 |
There was a significant difference (p = 0.011) in the importance given to the figure of the GC in the multidisciplinary team, between those who stated that they had (6.47 ± 0.9) or had not (6.06 ± 1.3) ever worked or collaborated with a GC.
A significant difference (p = 0.009) was also observed between these two groups for the administrative professional (5.10 ± 1.75 and 4.38 ± 1.87, respectively).
From the question regarding the most important profession in the PGT process, which was not a compulsory field, 334 responses were obtained. Each participant could indicate up to three preferences. The main figures in the PGT process are the medical geneticist (32%), followed by the GC (25%). Other key figures with lower percentages are the psychologist and the biologist.
Role of the GC
It can be seen (Table 3) that the respondents (138 people) identified in particular five central tasks of the profession of the GC with an average Likert score greater than 6: “Draw pedigree”, “ensure the patients’ understanding of the given genetic information”, “help patients express their own questions”, “collect information for genetic investigation” and “inform the patient about pre-symptomatic testing”. The least characteristic activity is “Make a diagnosis” with a mean of 3.64 and a standard deviation of 1.96.
Table 3.
Table of the activity that the Genetic Counsellor should perform. The mean and standard deviation are shown on the right.
| Actions the GC should perform | Average | SD |
|---|---|---|
| Draw Pedigree | 6.55 | 0.9 |
| Ensure the patients’ understanding of the given genetic information | 6.32 | 1.13 |
| Help patients express their own questions | 6.18 | 1.16 |
| Collect information for genetic investigation | 6.10 | 1.29 |
| Inform the patient about presymptomatic testing | 6.04 | 1.39 |
| Inform the patient about prenatal testing | 5.91 | 1.42 |
| Inform the patients about familial risk (without known mutation) | 5.91 | 1.43 |
| Make genetic risk assessment | 5.89 | 1.34 |
| Inform the patient about reproductive options | 5.89 | 1.48 |
| Inform the patient about diagnostic testing | 5.78 | 1.53 |
| Guide the patient in making the right decision for themselves | 5.74 | 1.46 |
| Inform the patient about test result | 5.61 | 1.72 |
| Discuss with the patient the potential effect on every-day life | 5.37 | 1.59 |
| Inform the patient about genetic variants of unclear significance | 5.22 | 1.76 |
| Discuss common psychological reactions and feelings | 5.17 | 1.4 |
| Coordinate the care pathway with other health care practitioners as well | 5.17 | 1.4 |
| Education of the population | 5.15 | 1.63 |
| Identify and help patients in crisis | 5.14 | 1.15 |
| Provide psychological support to the patient | 5.13 | 1.58 |
| Give the patient clinical and medical information | 4.99 | 1.71 |
| Provide follow-up after a clinical visit | 4.96 | 1.74 |
| Literature research | 4.89 | 1.66 |
| Write referrals | 4.38 | 1.85 |
| Sample handling | 4.09 | 1.89 |
| Make a diagnosis | 3.64 | 1.96 |
Regarding the fields in which the GC is most relevant (Table 4) respondents indicated that the main ones are: Oncogenetics, Prenatal and Pre-conceptional. In the category “other” (non-compulsory field), the need for counsellors in all medical disciplines was mentioned four times and the need for counsellors in rare diseases three times. Other categories that have been mentioned are sex-reversal-related genetic conditions, ophthalmic genetics and nephrogenetics.
Table 4.
Distribution of the different fields in which the figure of the Genetic Counsellor is relevant (mean, SD).
| Field | Average | SD |
|---|---|---|
| Oncogenetics | 6.19 | 1.19 |
| Prenatal | 5.98 | 1.34 |
| Pre-conceptional | 5.95 | 1.37 |
| Cardiogenetics | 5.38 | 1.6 |
| Neurogenetics | 5.11 | 1.59 |
| Paediatrics | 4.67 | 1.86 |
| Autoimmune | 4.04 | 1.77 |
From the sample surveyed, it emerges that to enter the master’s programme to become a GC, the education required mainly is Biology, with an average of 5.34. This is followed by a degree in Nursing and Midwifery with values just below 5 (Fig. 2).
Fig. 2. Educational background required to access training for Genetic Counsellors.
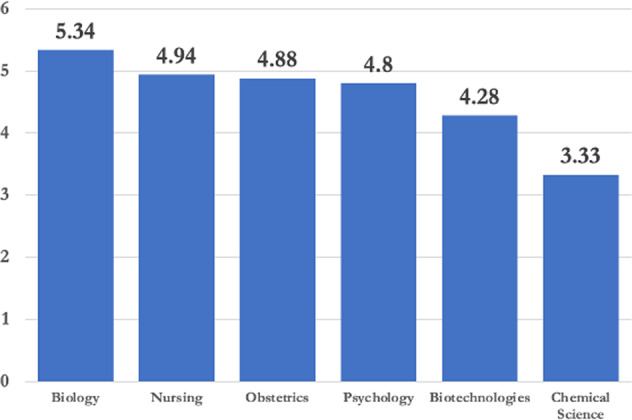
On top average and SD.
Discussion
This research brought to light the importance of the multidisciplinary team in caring for patients with or at risk of genetic disorders by highlighting the role and necessity of the genetic counsellor within the team. The fields of action of the Gc and the tasks that most characterize this figure according to the scientific medical community were highlighted. In addition, interesting insights have emerged to work towards a European recognition of this profession.
A critical analysis of the results would seem to imply that all respondents consider that the team should be multidisciplinary as all the professional profiles surveyed scored very high, reflecting their importance in the team, indeed the importance of the multidisciplinary team is referred to in many articles [12–16].
The respondents identified the GC as second in importance only to the medical geneticist. This result seems in contradiction with the fact that the GC is very often not involved in the team and in many countries is not even recognized [7–9]. Notably, most of the responses to the questionnaire came from countries where the figure is not yet recognized. Support from health professionals, particularly medical doctors, is fundamental in recognizing the role of the GC, and where such support has emerged it has been successfully incorporated leading to improved care. It would appear from our survey that such support from the medical geneticist community does exist. Indeed, our data show good awareness on the part of the medical geneticists although there is not always a working collaboration with a counsellor; this finding is not in line with some articles reporting that the non-involvement of the GC within the team was due to a lack of support and acceptance on the part of the doctors [13, 16, 17]. The question therefore arises as to what the problem is behind the non-recognition in some regions. One of the limitations of this study is that only those with a higher regard for GCs might have answered.
Our results show that close collaboration with the GC increases awareness of their value and the need to collaborate even more, but it appears that there is already greater awareness and knowledge than a few years ago. On average, the value of importance assigned to the GC is higher in the sample that claims to have collaborated with this figure, but at the same time the GC was indicated by the entire sample as the second most important. The second hypothesis H2: The role of the GC is fundamental in the team is confirmed.
This is also evident in the field of pre-implantation genetic testing. The main activities highlighted in this process are to inform patients about reproductive options, guide patients in making the right decision for themselves and ensure the patients’ understanding of the given genetic information. These are all characteristic actions of the GC. It would seem that the key competency is not to reach a diagnosis but to inform, support and help the patient to understand reproductive options and prenatal tests (explaining both the medical and emotional implications) to reach together with the patient, the best decision for the family [3, 7, 18, 19]. The patient-centred approach is fundamental, as the patient’s medical health, ethics and parental desire must be balanced [10, 20].
Those who declared working with the GC identified oncology, prenatal and preconception as the main fields in which GC is most appropriate. In these fields, the healthcare team is already multidisciplinary. It is essential, given the recent discoveries in the field of genetics, to include a GC who does not make a diagnosis but has an informative role in which he explains the possible causes of the disorders, the possible analyses, therapeutic and/or preventive actions [21–23]. These activities are not carried out by other professionals, thus leaving a well-defined field of action for the counsellor that does not overlap with that of other professionals [10, 24]. The fact that the other options in our questionnaire all received a score that can be considered high and that in the “other” section the need for counsellors in all medical disciplines was mentioned several times is in line with the fact that the advancement of genetics is recognized across all medical fields and that therefore in every specialty it would be appropriate to have access to genetic counsellors. It should also be emphasized that the technological progress has led digitalization to be a fundamental tool in the field of genetic counselling as well (e.g., Invitae, Genomeaxcess, Optrahealth etc.). This will increasingly help and facilitate communication, leaving once again a well-defined place for this profession [25].
The participants were asked to rank the importance of 25 items which, according to the authors, are important during the genetic counselling session. The first 10 actions in terms of importance turn out to be actions characterizing the competency of the GC and also reported in other articles as fundamental to the counselling profession [3, 4, 19, 26]. All of them fall within the semantic sphere of informing the patient, explaining what is happening, showing all possible options and helping patients to make the best decision. The activities which are more closely related to the doctor – such as making a diagnosis—result from our analysis to be less significant than those mentioned above. It follows from this that the two specialists – the doctor and the GC –have distinct and complementary fields of action. To be precise, out of the top 10 actions ranked by importance, 9 coincide with the top 10 ranked by GC competencies. There is a small difference on the action “Give test results to the patients” ranked 10 for importance and 12 for correlation with the activities to be carried out by the GC. There has always been a debate on this issue, but it would seem that this action can be responsibility of the GC although not in the top 10. Moreover, in the authors’ opinion, to maintain the essential relationship established between the patient and the GC, it is essential that if the counsellor has carried out the first counselling, it is always he/she who gives the results. What seems to emerge is the autonomy of the counsellor, who can perform all the main actions of a counselling session and only interface with the geneticist if he needs to - and where his expertise cannot reach. The third hypothesis H3: The GC is not recognized as being able to carry out all the actions that characterize counselling sessions is not accepted.
An analysis was then carried out on these 25 items to test difference in the answers between those who stated working with a GC and those who had never worked with one. In three of these actions, we saw difference. The first hypothesis H1: Assigning a different value to actions depending on whether collaboration with the GC is declared is confirmed. These were “Inform the patient about pre-symptomatic testing”, “Inform the patient about genetic variants of unclear significance” and “Inform the patient about familial risk (without known mutation)”. It has been previously suggested [7, 11] that situations of this kind should mostly be a medical responsibility, because of their complexity. Our analysis shows, however, that such situations can be the responsibility of the GC. The fact that the group that collaborated with the GC gives on average more importance to the three actions make us reflect on the strengths of the counsellor figure which seems to be recognized, reinforced, and positively valued by the doctor.
As our sample came from most of the European countries, we thought to see if there was a correlation between the percentage of participants who knew about the GC and who work with it and their place of origin. No statistical significance was found (the hypothesis H4.1 and H4.2 are not accepted) and this, in our opinion, can be explained in two ways, either there is no correlation or the data from some parts of Europe are too few to draw such a conclusion. It would be important to grow the study to test whether such differences exist. However, the research showed that the figure of the GC is well known and that more than half of the respondents collaborate or have collaborated with a GC. This collaboration also emerged in countries where GCs are not actually recognized. The GC’s fields of action therefore exist. According to the authors, it is a major issue to harmonize academic requirements and training and therefore it was asked which university background is the most appropriate according to the doctors, also because there is still an ongoing debate on this subject. The three bachelor’s degrees that were found to be most appropriate were, in order, Biology, Nursing and Midwifery. The importance of both theoretical and more clinical and practical knowledge would seem to emerge. A suggestion from our side is to unify, on a European level, the degree classes that can access the specialist training to become a GC.
We are aware of the limitations of this research, such as above all the fact that perhaps mainly physicians who have a high regard for the role of the CG responded to the questionnaire, but we think that the high number of responses obtained nonetheless shows the interest of the medical community in the figure of the CG and it would seem that the majority of specialists in the field have a clear idea of what the tasks and roles of the CG might be. We hope in the future to continue this survey by interviewing patients as well, to move more and more towards a personalized medicine that puts the patient at the centre, improving clinical outcome and quality of life despite the disease.
Supplementary information
Acknowledgements
Two of several authors of this publication are members of the European Reference Network for rare malformation syndromes and rare intellectual and neurodevelopmental disorders, ERN-ITHACA.
Author contributions
FC: developed the research project and wrote the manuscript. MEH: oversaw data collection. NK-H: took care of the online questionnaire and the link to be distributed. AR: was in charge of sponsoring this project and, above all, analysing the data collected. FM: identified the best statistical tests and analyses for data processing. MM: supervised the entire structure of the research project. Thanks to his experience, he reviewed the entire structure of the manuscript, from the contents to the English language. CC: coordinated the work of all by offering his experience in reading reality and proposing possible solutions for the problems that emerged from the research.
Funding
No funding was needed.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Ethical approval
For all participants involved in the present study, written informed consent was obtained from the subjects themselves. All methods were performed in accordance with the Ethical Principles for Medical Research involving Human Subject of the Helsinki Declaration.
Footnotes
The original online version of this article was revised: Update in the Acknowledgment section.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Change history
1/30/2023
Update in the Acknowledgment section.
Change history
2/9/2023
A Correction to this paper has been published: 10.1038/s41431-023-01289-w
Supplementary information
The online version contains supplementary material available at 10.1038/s41431-022-01189-5.
References
- 1.Calzone KA, Jenkins J, Nicol N, Skirton H, Feero WG, Green ED. Relevance of genomics to healthcare and nursing practice. J Nurs Scholarsh. 2013;45:1–2. doi: 10.1111/j.1547-5069.2012.01464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Collins FrancisS. Implications of the human genome project for medical science. JAMA. 2001;285:540. doi: 10.1001/jama.285.5.540. [DOI] [PubMed] [Google Scholar]
- 3.Cordier C, Taris N, Moldovan R, Sobol H, Voelckel MA. Genetic professionals’ views on genetic counsellors: a French survey. J Community Genet. 2016;7:51–55. doi: 10.1007/s12687-015-0250-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skirton H, Cordier C, Ingvoldstad C, Taris N, Benjamin C. The role of the genetic counsellor: a systematic review of research evidence. Eur J Hum Genet. 2015;23:452–58. doi: 10.1038/ejhg.2014.116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Paneque M, Moldovan R, Cordier C, Serra-Juhé C, Feroce I, Skirton H, et al. The perceived impact of the European registration system for genetic counsellors and nurses. Eur J Hum Genet. 2017;25:1075–77. doi: 10.1038/ejhg.2017.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Crimi M, Mineri R, Godino L, Cordier C, Coviello DA, Feroce I, et al. Building awareness on genetic counselling: the launch of italian association of genetic counsellors (AIGeCo) J Community Genet. 2020;11:495–96. doi: 10.1007/s12687-020-00483-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pestoff R, Moldovan R, Cordier C, Serra-Juhé C, Paneque M, Ingvoldstad CM. How practical experiences, educational routes and multidisciplinary teams influence genetic counselors’ clinical practice in Europe. Clin Genet. 2018;93:891–98. doi: 10.1111/cge.13197. [DOI] [PubMed] [Google Scholar]
- 8.Abacan MA, Alsubaie L, Cordier C, Moldovan R, Ormond KE, Paneque M, et al. The global state of the genetic counseling profession. Eur J Hum Genet. 2019;27:183–97. doi: 10.1038/s41431-018-0252-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Godard B, Kääriäinen H, Kristoffersson U, Tranebjaerg L, Coviello D, Aymé Ségolène. Provision of genetic services in Europe: current practices and issues. Eur J Hum Genet. 2003;11:S13–48. doi: 10.1038/sj.ejhg.5201111. [DOI] [PubMed] [Google Scholar]
- 10.Paneque M, Serra-Juhé C, Pestoff R, Cordier C, Moldovan R, Ingvoldstad C, et al. Complementarity between medical geneticists and genetic counsellors: its added value in genetic services in Europe. Eur J Hum Genet. 2017;25:918–23. doi: 10.1038/ejhg.2017.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cordier C, McAllister M, Feroce I, Moldovan R, Paneque M, EBGM, Genetic Nurses and Genetic Counsellors 2018 et al. The recognition of the profession of genetic counsellors in Europe. Eur J Hum Genet. 2018;26:1719–20. doi: 10.1038/s41431-018-0260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Battista RN, Blancquaert I, Laberge AM, van Schendel N, Leduc N. Genetics in health care: an overview of current and emerging models. Public Health Genomics. 2012;15:34–45. doi: 10.1159/000328846. [DOI] [PubMed] [Google Scholar]
- 13.Cordier C, Lambert D, Voelckel MA, Hosterey-Ugander U, Skirton H. A profile of the genetic counsellor and genetic nurse profession in European countries. J Community Genet. 2012;3:19–24. doi: 10.1007/s12687-011-0073-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Skirton H, Cordier C, Lambert D, Hosterey Ugander U, Voelckel MA, O’Connor A. A study of the practice of individual genetic counsellors and genetic nurses in Europe. J Community Genet. 2013;4:69–75. doi: 10.1007/s12687-012-0119-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hannig VL, Cohen MP, Pfotenhauer JP, Williams MD, Morgan TM, Phillips JA., III Expansion of genetic services utilizing a general genetic counseling clinic. J Genet Counseling. 2014;23:64–71. doi: 10.1007/s10897-013-9608-0. [DOI] [PubMed] [Google Scholar]
- 16.Cordier C, Mandel JL, SOBOL H, and Voelckel. 2013. Insertion Professionnelle et Intégration des Conseillers en Génétique: Une Nouvelle Coopération Dans Le Domaine De La Santé. La Faculté De Médecine De Marseille.
- 17.Schwaninger G, Benjamin C, Rudnik-Schöneborn S, Zschocke J. The genetic counseling profession in austria: stakeholders’ perspectives. J Genet Counseling. 2021;30:861–71. doi: 10.1002/jgc4.1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McAllister M, Payne K, MacLeod R, Nicholls S, Donnai D, Davies L. What process attributes of clinical genetics services could maximise patient benefits? Eur J Hum Genet. 2008;16:1467–76. doi: 10.1038/ejhg.2008.121. [DOI] [PubMed] [Google Scholar]
- 19.Pestoff R, Ingvoldstad C, Skirton H. Genetic counsellors in Sweden: their role and added value in the clinical setting. Eur J Hum Genet. 2016;24:350–55. doi: 10.1038/ejhg.2015.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mounts EL, Besser AG. Genetic counseling for preimplantation genetic testing (PGT). Pp. 43–52 in Human Embryos and Preimplantation Genetic Technologies. Elsevier. 2019.
- 21.Fox M. A guide to genetic counseling, 2nd edition. Am J Hum Genet. 2010;87:315. doi: 10.1016/j.ajhg.2010.07.024. [DOI] [Google Scholar]
- 22.Firth, HV., and JA Hurst. 2017. Oxford desk reference clinical genetics and genomics by Firth & Hel…’ Fruugo. Retrieved 18 October 2021. https://www.fruugo.it/oxford-desk-reference-clinical-genetics-and-genomics-by-firth-helen-v-consultant-in-clinical-genetics-consultant-in-clinical-genetics-cambridge-university-hospitals-cambridge-uk-and-hon-faculty-member-wellcome-trust-sanger-institute-hinxton-ukh/p3982877681769071?language=en&ac=croud&gclid=EAIaIQobChMIp7TW6_vT8wIVy-d3Ch3b-AgmEAYYAiABEgI3nfD_BwE.
- 23.Nussbaum RL, McInnes RR, and Willard F. 2016. Thompson & Thompson Genetics in Medicine. 8th ed.
- 24.Joseph FM. 2018. A key role of the genetic counsellors in the genomic era. 10.12688/f1000research.14222.2. [DOI] [PMC free article] [PubMed]
- 25.Mahon Suzanne M. Telegenetics: remote counseling during the COVID-19 pandemic. Number 3 / June 2020 24:244–48. 10.1188/20.CJON.244-248. [DOI] [PubMed]
- 26.Rantanen E, Hietala M, Nippert I, Schmidtke J, Sequeiros J, Kääriäinen H, et al. What is ideal genetic counselling? A survey of current international guidelines. Eur J Hum Genet. 2008;16:445–52. doi: 10.1038/sj.ejhg.5201983. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated and/or analysed during the current study are available from the corresponding author on reasonable request.