Abstract
Psychiatric comorbidity and abusive experiences in chronic pelvic pain (CPP) conditions may prolong disease course. This study investigated the psychometrics of the Depression Anxiety Stress Scale 8 (DASS-8) among women with CPP (N = 214, mean age = 33.3 ± 12.4 years). The DASS-8 expressed excellent fit, invariance across age groups and menopausal status, good know-group validity (differentiating women with psychiatric comorbidity from those without comorbidity: U = 2018.0, p = 0.001), discriminant validity (HTMT ratios < 0.85), excellent reliability (alpha = 0.90), adequate predictive and convergent validity indicated by strong correlation with the DASS-21 (r = 0.94) and high values of item-total correlations (r = 0.884 to 0.893). In two-step cluster analysis, the DASS-8 classified women into low- and high-distress clusters (n = 141 and 73), with significantly higher levels of distress, pain severity and duration, and physical symptoms in cluster 2. The DASS-8 positively correlated with pain severity/duration, subjective symptoms of depression/anxiety, experiences of sexual assault, fatigue, headache severity, and collateral physical symptoms (e.g., dizziness, bloating, fatigue etc.) at the same level expressed by the parent scale and the DASS-12, or even greater. Accordingly, distress may represent a target for early identification of psychiatric comorbidity, CPP severity, experiences of sexual assault, and collateral physical complaints. Therefore, the DASS-8 is a useful brief measure, which may detect mental distress symptoms among women with CPP.
Subject terms: Psychology, Health care, Risk factors, Signs and symptoms
Introduction
Pain in the pelvis unrelated to cancer, intercourse, or menstruation, which is experienced daily and persists for at least three consecutive months is known as chronic pelvic pain (CPP). CPP is commonly experienced by up to 22% of women1–3. It can be idiopathic or due to numerous urological, bowel-related, and gynecological reasons3,4. Because non-cancer CPP conditions in women worsen over time, especially during the peak reproductive years, fluctuations in ovarian hormones are suggested to be key modulators in the pathologies underlying CPP such as endometriosis and irritable bowel syndrome1,5,6.
Differences in CPP experience and pathology are reported between reproductive age women and peri/postmenopausal women4. Conditions entailing reduced levels of feminine hormones (e.g., menopause and during menses) are associated with increased sensitivity to visceral and pelvic pain5. In addition, ovarian collapse and subsequent reduction in estrogen during menopause is associated with numerous vegetative (e.g., hot flushes), physical (e.g., fatigue and back pain), urogenital/sexual (e.g., dyspareunia and urinary incontinence), cognitive (e.g., memory problems), and mental symptoms (e.g., depression and anxiety), which may aggravate pain sensitivity in midlife women and endanger their mental wellbeing7. In fact, CPP women within the age range of 25 to 35 years are reported to express less anxiety symptoms than their older counterparts8.
The annual healthcare expenditure of CPP is enormous, exceeding 6.5 billion dollars in Australia2. In addition, CPP alters women’s quality of life, reproductive capacity, social relations, work performance, and sexuality. As a result, CPP women experience high levels of distress, depression, and anxiety9. Depression, anxiety, and mixed anxiety depression disorder (MADD) prevail in 63%, 66%, and 54% of women experiencing CPP compared with 38%, 49%, and 28% of CPP-free women8. The etiopathogenesis of depression and anxiety in chronic pain is evoked by a complex mechanism through which pain signaling interferes with the pathophysiological and neurophysiological signaling, which induces mood dysfunction10,11. Moreover, chronic persistent rather than intermittent pain may exacerbate depressive and anxious manifestations by promoting constant patterns of cognitive biases (e.g., pain catastrophism), sleep disturbance, emotional dysregulation, behavioral inactivation, and loneliness12,13.
Exposure to different forms of abuse during early stages of life is associated with the development and persistence of numerous physical, emotional, mental, and sexual dysfunctions during adulthood14. Moreover, women in different parts of the world witness the highest exposure to different forms of abusive behavior against adults, along with numerous grave consequences15. Physical and sexual abuse represent a major risk factor for CPP3,8. Given the traumatic origins of CPP and the distressful course of the condition, CPP is frequently managed within the biopsychosocial model of chronic pain—an approach, which emphasizes the importance of wholistic management of chronic pain conditions “pain itself along with associated psychological and social problems” for more positive treatment outcomes2. However, CPP women experience varying levels of psychological distress. Greater comorbidity (e.g., depression, poor sleep, fatigue, somatic symptoms) is more common among women who experience higher distress than those with little or no distress16. Therefore, careful identification of highly distressed women with CPP through the assessment of psychopathological symptoms is extremely pivotal for designing effective interventions for CPP and evaluating the outcomes of such interventions2.
The Depression, Anxiety, and Stress Scale-21 (DASS-21) is a simple measure frequently used in research and clinical practice to capture the distinct features of depression, anxiety, and stress symptomatology17. However, numerous studies reported enormous flaws associated with the DASS-21: variations in its dimensional structure18–22, non-invariance across different groups23–25, and a ceiling effect26. As a result, many revisions of its item structure took place.
An 18-item DASS was reported to express good fit in Asian samples from Malaysia, Indonesia, Singapore, Sri Lanka, Taiwan, and Thailand27. Another short version, DASS-14, was produced in an Australian sample of rehabilitation medical professionals based on the removal of items, which expressed poor loadings or loaded onto more than one factor28. These revised versions had a three-factor structure same as the parent scale, albeit with smaller inter-factor correlations27. New shorter forms were reported in other studies22,29.
Using several non-clinical samples, Osman et al. reported that the DASS-21 may be best used as a unidimensional measure of psychological distress22—a state of emotional suffering, which combines non-specific symptoms of depression and anxiety30,31. They also reported that numerous items poorly correlated with the underlying latent construct covered by the DASS-21, noting that reducing its items to 13 or nine items would remedy such flaws22. Subsequently, a 12-item version of the DASS-21 has been tested in non-clinical and clinical Korean samples29. However, this version has not been tested in another population until recently. A current study used clinical and non-clinical samples from Saudi Arabia to investigate various models of the parent scale as well as all the available shortened versions32. The fit of different models of the DASS-21 was considerably lower than all its short versions. An extensive revision of the item structure of the DASS-21 based on statistics and conceptual methods resulted in an 8-item version. The DASS-8 expressed excellent psychometric properties compared with Osman’s 13-item/nine-item DASS and the Korean DASS-1232. Likewise, in another investigation involving healthy individuals from the US, Australia, and Ghana, the DASS-8 expressed a better fit than the DASS-12. Examinations of discriminant validity revealed minimal overlapping of its subscales compared with the DASS-21 and the DASS-12. Its convergent validity, in terms of item loadings and item total correlations, was considerably better than the DASS-12. It also demonstrated more robust criterion validity by correlating with measures of internet addiction, adult attention-deficit/hyperactivity disorder (ADHD), and individualistic cultural orientation at similar or greater levels of significance31. In another investigation involving three Arab samples (individuals from COVID-19 quarantine facilities, psychiatric patients, and healthy adults), the DASS-8 and all its subscales significantly (all values < 0.01) correlated with COVID-19 trauma and its different dimensions: intrusion, avoidance, hyperarousal, numbing, sleep disturbance, and dysphoria33. Thus, the DASS-8 maybe reliably used as a criterion variable to detect debilitating morbidities (e.g., internet addiction, ADHD, and post-traumatic stress disorder (PTSD)), which are less frequently reported by patients and less recognized in primary care settings31,33.
Because they maximize response rates, brief screening instruments are intended to be used more frequently as clinical tools to facilitate the identification of pathological cases and enable assessing response to treatment34,35. Thus, there is an intense need to ensure the relevance, local precision, and adequate sensitivity of these instrument35. Although the DASS-8 and DASS-12 were invariant across different groups in Arab samples32, both short scales exhibited variance at the scalar level across English-speaking and Ghanaian participants, with the latter expressing lower levels of distress31. Individuals’ responses to the items of distress scales, such as the DASS-8, in different cultures may vary since individuals tend to selectively express their distress symptoms through culturally acceptable ways36. Therefore, to benefit from the DASS-8 as an available brief form of the DASS-21, it needs to be evaluated in more diverse populations, including patient groups, to ensure the adequacy of its sensitivity. Accordingly, this study aimed to examine the psychometrics of the DASS-8 in a sample of Australian women with CPP. We hypothesized that (1) the DASS-8 would express better fit and less non-variance than the DASS-12; (2) the DASS-8 would discriminate CPP women experiencing mental comorbidities from those without mental comorbidities; (3) the DASS-8 would correlate with the DASS-21 at the same level expressed by the DASS-12; (4) the DASS-8 would correlate with pain symptoms and history of sexual assault at the same level expressed by the parent scale; and (5) the DASS-8 may classify CPP women into classes of high and low levels of distress and morbidity. Thus, this paper complements existing knowledge in the field by expanding the methods used to examine the properties of the DASS-8, such as cluster analysis. Examinations of its criterion validity have been extended to aspects not addressed in prior research such as pain, sexual abuse, and collateral physical symptoms. Such criteria represent a source of enormous discomfort in CPP3,8,11,37.
Material and methods
Study design, participants, and procedure
This study is a secondary analysis based on a publicly accessible dataset from a previously published cross-sectional study3, which comprises a convenient sample of women with CPP. Data were collected via a pre-treatment self-administered questionnaire addressed to all clients attending a specialist pelvic pain clinic in South Australia over 18 months between January 2015 and July 2016. Women not signing informed consent, with several incomplete sections of the questionnaire, or solely experiencing period pain or dyspareunia were excluded from the study. Women or their guardian, if they were less than 18 years old, signed an informed consent. Because the protocol for data collection was previously approved by University of South Australia Human Research Ethics Committee (Application ID: 0000036598; 26/05/2017)3, and the dataset was publicly accessible38, we did not obtain an ethical approval for the current study.
Measures
The questionnaire used for data collection comprised a large set of questions about pain experienced, its intensity, duration, pain-free days per month, pain severity during sexual activity, severity of stabbing pelvic pain, pain severity on the day of data collection, experiencing (tiredness/fatigue, anxiety, low mood, bad headache), somatic symptoms (e.g., nausea, unusual sweating, dizziness, and bloating), history of sexual assault, current psychiatric disorders, etc. Questions addressing pain severity or intensity prompted the respondents to rate the intensity of pain on a scale from 0 (no pain) to 10 (extremely severe pain)3.
The Depression Anxiety Stress Scale (DASS-21) was used to measure psychological distress. It comprises 21 items, in three subscales, which assess the symptoms of depression, anxiety and stress. Item responses are rated on a four-point scale ranging from 0 (did not apply to me at all) to 3 (applied to me very much or most of the time). The minimum and maximum total scores of the DASS-21 are 0 and 6339. The DASS-8 comprises eight items, in three subscales: depression (three items e.g., felt down hearted and blue), anxiety (three items e.g., felt scared without reason), and stress (two items e.g., was using a lot of my mental energy)31,32. The total scores of the DASS-8 and its subscales range between 0 to 24, 0 to 9, 0 to 9, and 0 to 6, respectively. The DASS-12 comprises 12 items, in three subscales, each comprising four items. The total scores of the DASS-12 and its subscales range between 0 to 24 and 0 to 12, respectively29. The reliability of the DASS-21, DASS-8, and DASS-12 in this sample is excellent (coefficient alpha = 0.95, 0.90, and 0.90, respectively). The inclusion of the DASS-21/DASS-12 in this study aims to ensure adequate validity of the DASS-8 as the shortest version of the DASS-21 relative to the parent scale and the DASS-12 as another longer brief version.
Statistical analysis
First, we checked the dataset for missing responses. Because multiple items of the DASS-21 had missing responses, we removed all participants with incomplete data on the DASS-8 and DASS-12, which resulted in a final sample size of 214 participants—response rate = 90%. Meanwhile, 212 respondents were included in tests of the factor structure of the DASS-21. The normality of different versions of the DASS were tested by Shapiro Wilk W test. The statistics of non-normal variables are reported as median (MD) and interquartile range (IQR; Q1-Q3) while mean and standard deviation were used to report normally distributed variables. Number and percentage were used to describe categorical variables.
Based on two former investigations31,32, the factor structures of the DASS-8 and DASS-12 were examined using confirmatory factor analysis (CFA). To evaluate model fit as good or acceptable, we used chi square (χ2) index, ideally it should be non-significant, Comparative Fit Index (CFI) and Tucker–Lewis Index (TLI) equal to or above 0.95 and 0.90, respectively, in addition to standardized root-mean-square residual (SRMR) and root mean square error of approximation (RMSEA) less than 0.06 and 0.08, respectively40. This combination allows parsimonious evaluation of model fit because χ2 and RMSEA may be influenced by sample size, which if used alone may disqualify well-fitting models that express minor misspecifications41,42. Based on suggestions pointed by modification indices, few error terms were correlated to improve model fit.
To test measurement invariance of the DASS-8, age was categorized twice into two different groups: based on median age (110 women aged 31 years or below and 104 women above the age of 31) and based on the age reported to coincide with menopause transition (156 below the age of 40 versus 58 aged 40 years or above). This is because hormonal alterations in the perimenopause stage are associated with greater mood dysfunction than in the later post-menopause stage7. Then, multigroup CFA was conducted to compare invariance of the DASS-8 and DASS-12 at the configural, metric, scalar, and strict levels43,44 across groups of age, menopausal status (menopausal vs premenopausal), and psychiatric comorbidity (presence of comorbidity vs no comorbidity, the number of subjects in all categories are shown in Table 1). Significant changes in χ2 in constrained models, along with ΔCFI and ΔRMSEA above 0.02 and 0.015, respectively were used as criteria for non-invariance30,43.
Table 1.
Sociodemographic and clinical characteristics of the participants.
| Participant characteristics | Whole sample (N = 214) |
Cluster 1 (n = 141) |
Cluster 2 (n = 73) |
p |
|---|---|---|---|---|
| Age in years mean (SD) | 33.3 ± 12.4 | 33.8 ± 12.0 | 32.4 ± 13.4 | 0.477 |
| Pain days mean (SD) | 17.8 ± 9.6 | 16.9 ± 9.7 | 20.1 ± 9.1 | 0.014 |
| Pain free days MD (IQR) | 10.0 (2.8–20.0) | 15.0 (4.0–21.0) | 7.0 (1.0–15.0) | 0.017 |
| Stabbing pelvic pain | ||||
| Yes | 185 (87.7%) | 119 (85.6%) | 66 (91.7%) | 0.205 |
| No | 26 (12.3%) | 20 (14.4%) | 6 (8.3%) | |
| Stabbing pelvic pain severity mean (SD) | 7.6 ± 1.8 | 7.3 ± 1.8 | 8.0 ± 1.7 | 0.015 |
| Current pelvic pain severity MD (IQR) | 4.0 (1.0–5.0) | 3.0 (0–5.0) | 5.0 (2.0–7.0) | 0.001 |
| Sex pain | ||||
| Yes | 149 (82.8%) | 100 (80.6%) | 49 (87.5%) | 0.259 |
| No | 31 (17.2%) | 24 (19.4%) | 7 (12.5%) | |
| Sex pain severity mean (SD) | 6.0 ± 2.0 | 6.1 ± 2.0 | 7.3 ± 1.7 | 0.001 |
| Sexual assault | ||||
| Yes | 27 (16.1%) | 8 (7.2%) | 19 (33.3%) | 0.001 |
| No | 141 (83.9%) | 103 (92.8%) | 38 (66.7%) | |
| Headache severity mean (SD) | 7.0 ± 1.8 | 6.6 ± 1.9 | 7.7 ± 1.5 | 0.001 |
| Menopausal status | ||||
| Premenopausal | 188 (89.5%) | 123 (88.5%) | 65 (89.0%) | 0.764 |
| Menopausal | 24 (11.4%) | 16 (11.5%) | 8 (11.0%) | |
| Current psychiatric comorbidity | ||||
| Yes | 61 (29.3%) | 26 (18.8%) | 35 (50.0%) | 0.001 |
| No | 147 (70.7%) | 112 (81.2%) | 35 (50.0%) | |
| Comorbid psychiatric disorders | ||||
| MDD | 13 (21.3%) | 7 (26.9%) | 6 (17.1%) | 0.774 |
| GAD | 14 (23.0%) | 6 (23.1%) | 8 (22.9%) | |
| MDD comorbid with GAD | 28 (45.9%) | 11 (42.3%) | 17 (48.6%) | |
| Others | 6 (9.8%) | 2 (7.7%) | 4(11.4%) | |
| Bloating | ||||
| Yes | 163 (88.6%) | 103 (85.8%) | 60 (93.8%) | 0.108 |
| No | 21 (11.4%) | 17 (14.2%) | 4 (6.2%) | |
| Bowel pain | ||||
| Yes | 144 (78.7%) | 86 (72.9%) | 58 (89.2%) | 0.010 |
| No | 39 (21.3%) | 32 (27.1%) | 7 (10.8%) | |
| Subjective experience of anxiety | ||||
| Yes | 118 (58.1%) | 52 (39.4%) | 66 (93.0%) | 0.001 |
| No | 39 (41.9%) | 80 (60.6 ±) | 5 (7.0%) | |
| Subjective experience of low mood | ||||
| Yes | 118 (63.4%) | 55 (47.0%) | 63 (91.3%) | 0.001 |
| No | 68 (36.6%) | 62 (53.0%) | 6 (8.7%) | |
| Fatigue | ||||
| Yes | 146 (77.7%) | 81 (68.1%) | 65 (94.2%) | 0.001 |
| No | 42 (22.3%) | 38 (31.9%) | 4 (5.8%) | |
| Sleep problems | ||||
| Yes | 117 (59.4%) | 63 (49.6%) | 54 (77.1%) | 0.001 |
| No | 80 (40.6%) | 64(50.4%) | 16(22.9%) | |
| Dizziness | ||||
| Yes | 113 (58.9%) | 60 (49.6%) | 53 (77.9%) | 0.006 |
| No | 79 (41.1%) | 61(50.4%) | 15(22.1%) | |
| Unusual sweating | ||||
| Yes | 69 (34.8%) | 35 (26.9%) | 34 (50.0%) | 0.002 |
| No | 129 (65.2%) | 95 (73.1%) | 34 (50.0%) | |
| Nausea | ||||
| Yes | 92 (52.9%) | 49 (33.6%) | 43 (74.1%) | 0.001 |
| No | 82 (47.1%) | 97 (66.4%) | 15 (25.9%) | |
N ranges between 127 and 211, SD: standard deviation, MD: median, IQR: interquartile range, MDD: Major depression disorder, GAD: Generalized anxiety disorder.
To examine known-group validity of the DASS-21, DASS-12, DASS-8, Mann Whitney U test was used to determine whether these measures and their subscales can differentiate CPP women with comorbid psychiatric disorders from those without psychopathology. It was also used to differentiate women with depressive disorder from those with anxiety disorder. For discriminant validity, heterotrait-monotrait (HTMT) ratio of correlations of items comprising the DASS-21, DASS-12, DASS-8 were computed31,45. Moreover, two-step cluster analysis was used to determine whether the participants can be grouped according to the scores of the DASS-8 and its subscales. Clustering is a technique, which uses uncovered characteristics in a dataset to divide cases or variables into non-overlapping groups, with a high degree of similarity within each group and a low degree of similarity between groups46. Two-step cluster analysis is a hybrid technique that operates via two steps. The first step (pre-clustering) employs a sequential approach to separate groups by pre-clustering cases based on a distance measure that defines dense regions in the analyzed attribute-space. In the second step (clustering), a probabilistic approach is used to statistically merge pre-clusters stepwise until the optimal subgroup model is determined. This technique is highly reliable; in terms of the number of subgroups detected, classification probability of individuals into subgroups, and reproducibility of the findings on different types of data. It has additional merits: analyzing atypical values (i.e., outliers), determining the number of clusters based on a statistical measure of fit rather than on an arbitrary choice, using categorical and continuous variables simultaneously, and handling large datasets47. Independent sample t-test, Mann Whitney test, and χ2 were used to compare the differences in mental symptomatology and characteristics of the participants across clusters.
The reliability of the DASS-21, DASS-12, DASS-8, and their subscales was assessed by coefficient alpha, alpha-if-item deleted, and item-total correlations. The predictive validity of the DASS-12, DASS-8, and their subscales was detected by Spearman’s r correlating these measures to the original scale and its subscales. This test was also used to evaluate the criterion validity of the three measures by correlating their scores with sexual assault experience, number of pain days/pain-free days per month, pain severity during sexual activity, pain severity on the day of data collection, severity of stabbing pelvic pain, experiencing bad headache, experiencing tiredness/fatigue, experiencing anxiety, and experiencing low mood. All analyses were conducted in SPSS version 24, and significance was considered at a probability level less than 0.05 in two-tailed tests.
Ethics approval and consent to participate
The protocol of data collection was approved by University of South Australia Human Research Ethics Committee (Application ID: 0000036598; 26/05/2017). All participants or their guardians signed a written informed consent before data collection3. No ethical approval was obtained for the current study because the analysis is based on a publicly accessible dataset38. The present study was conducted according to the Declaration of Helsinki.
Results
Characteristics of the participants
Participants in this study (N = 214, mean age = 33.1 ± 12.4 years) were women complaining from CPP. The participants experienced several types of pain (stabbing pelvic pain, sex pain, bowel pain, and headache), somatic symptoms (e.g., bloating, nausea, dizziness, unusual sweating), along with symptoms of low mood, anxiety, and psychiatric comorbidity. Table 1 shows more information on the sociodemographic and clinical characteristics of the participants in the overall sample as well as differences in these variables between women groups of low distress and high distress.
Results of confirmatory factor analysis and invariance analysis
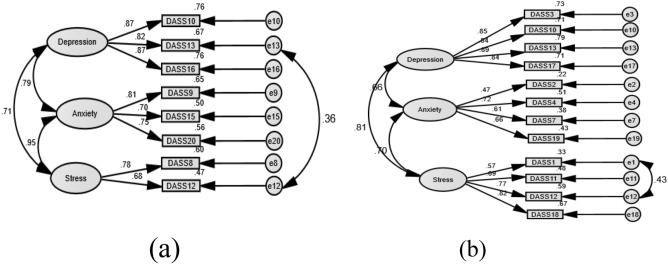
As shown in Table 2, the one-factor structure of the DASS-8/DASS-12 expressed unsatisfactory fit. The crude models of the three-factor structures of the DASS-8 and the DASS-12 expressed good fit. However, RMSEA was on the high side for the DASS-8, suggesting minor misspecifications in item loadings, which may be overlooked given that all other fit indices indicated good fit (discussed in detail below). The fit of this model was considerably improved by correlating the residuals of item 12 and item 13. Likewise, the fit of the DASS-12 was slightly improved by correlating the residuals of item 1 and item 12 (Fig. 1b). On the other hand, the fit of all the crude models of the DASS-21 was poor. Correlating several error terms was necessary to produce an acceptable fit (Appendix 1: Fig. 1b). The fit of the second order structure was similar to that of the three-factor structure of all the DASS scales (Appendix 1, Appendix 2). While the bifactor structure of the DASS-8 expressed good fit with all items significantly loading on the general factor, item 12 and item 20 failed to load on their domain-specific factors of stress and anxiety, respectively (p > 0.05). In addition, item 15 loaded significantly on the anxiety factor (p = 0.04), but its loading on this factor was weak (β = 0.26). All the items of the anxiety subscale of the DASS-12 (Appendix 2: Supplementary Table 5) and the DASS-21 (Appendix 1: Table 2) failed to load on their corresponding factor in the bifactor model, and SRMR was not produced (Table 2, Appendix 1: Table 1), denoting failure of the model to converge adequately. Therefore, the three-factor structures of the DASS-8/DASS-12/DASS-21 represent the best fit for the data.
Table 2.
Goodness-of-fit of the confirmatory factor analysis models representing the Depression Anxiety Stress Scale-8 (DASS-8) and the DASS-12 in the whole sample.
| Models | Samples | χ2 | p | Df | CFI | TLI | RMSEA | RMSEA 90% CI | SRMR |
|---|---|---|---|---|---|---|---|---|---|
|
Model 1 1F DASS-8 |
Crude | 154.108 | 0.001 | 20 | 0.869 | 0.817 | 0.171 | 0.146 to 0.198 | 0.0709 |
| Correlated error | 106.028 | 0.001 | 19 | 0.909 | 0.866 | 0.147 | 0.120 to 174 | 0.0684 | |
|
Model 2 3F DASS-8 |
Crude | 51.086 | 0.001 | 17 | 0.964 | 0.941 | 0.097 | 0.067 to 0.128 | 0.0341 |
| Correlated error | 31.261 | 0.012 | 16 | 0.984 | 0.972 | 0.067 | 0.030 to 0.102 | 0.0332 | |
| Model 3 bifactor DASS-8 | Crude | 30.999 | 0.013 | 16 | 0.984 | 0.973 | 0.066 | 0.030 to 0.101 | 0.0329 |
|
Model 4 1F DASS-12 |
Crude | 268.420 | 0.001 | 54 | 0.840 | 0.805 | 0.137 | 0.121 to 0.153 | 0.0790 |
| Correlated error | 176.317 | 0.001 | 52 | 0.907 | 0.882 | 0.106 | 0.089 to 0.123 | 0.0684 | |
|
Model 5 3F DASS-12 |
Crude | 117.403 | 0.001 | 51 | 0.951 | 0.936 | 0.078 | 0.060 to 0.097 | 0.0460 |
| Correlated error | 88.049 | 0.001 | 50 | 0.972 | 0.963 | 0.060 | 0.038 to 0.080 | 0.0379 | |
| Model 6 bifactor DASS-12 | Crude | 113.763 | 0.001 | 51 | 0.953 | 0.937 | 0.078 | 0.060 to 0.097 | – |
| Correlated error | 104.279 | 0.001 | 47 | 0.957 | 0.940 | 0.076 | 0.056 to 0.095 | – |
χ2, chi-square; df, degrees of freedom; CFI, comparative fit index; TLI, Tucker–Lewis index; RMSEA, root mean square error of approximation; CI, confidence interval; SRMR, standardized root mean residual; –, SRMR was not produced denoting improper convergence of the model.
Figure 1.
Factor structure of the short versions of the Depression Anxiety Stress Scale (DASS)-21: the DASS-8 (a) and the DASS-12 (b) among women with chronic pelvic pain.
As shown in Table 3, the three-factor structures of the DASS-8 and DASS-12 were invariant at the configural, metric, scalar, and strict levels across groups of age and menopausal status. For median-based age groups, there was a tendency toward non-invariance of the DASS-8 at the scalar level (ΔCFI > 0.02); however, ΔRMSEA was still within the acceptable range < 0.15. Obviously, the DASS-8 was non-invariant at the scalar level across groups of psychiatric comorbidity (ΔCFI > 0.02 and ΔRMSEA > 0.15). The DASS-12 was non-invariant at the strict level (ΔCFI > 0.02 and ΔRMSEA > 0.15), and it also tended to be non-invariant at the scalar level across comorbidity groups (SRMR = 0.1117).
Table 3.
Invariance of the three-factor structures of the Depression Anxiety Stress Scale 8 (DASS-8) and DASS-12 across groups of age, menopausal status, and psychiatric comorbidity.
| Model | Groups | Invariance levels | χ2 | df | P | Δχ2 | Δdf | p(Δχ2) | CFI | ΔCFI | TLI | ΔTLI | RMSEA | ΔRMSEA | SRMR |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DASS-8 | Age (≤ 31, > 31 years) | Configural | 61.939 | 32 | 0.001 | 0.969 | – | 0.946 | – | 0.066 | 0.0382 | ||||
| Metric | 64.824 | 37 | 0.003 | 2.884 | 5 | 0.718 | 0.971 | 0.002 | 0.957 | 0.011 | 0.060 | 0.006 | 0.0373 | ||
| Strong | 91.766 | 43 | 0.001 | 26.942 | 6 | 0.001 | 0.950 | 0.021 | 0.935 | 0.022 | 0.073 | − 0.013 | 0.0680 | ||
| Strict | 100.302 | 52 | 0.001 | 8.537 | 9 | 0.481 | 0.950 | 0.000 | 0.947 | 0.012 | 0.066 | 0.007 | 0.0669 | ||
| DASS-12 | Age (≤ 31, > 31 years) | Configural | 164.318 | 100 | 0.001 | 0.954 | 0.939 | – | 0.055 | 0.0459 | |||||
| Metric | 175.896 | 109 | 0.001 | 11.579 | 9 | 0.238 | 0.952 | 0.002 | 0.941 | 0.002 | 0.054 | 0.001 | 0.0516 | ||
| Strong | 201.610 | 115 | 0.001 | 25.714 | 6 | 0.001 | 0.937 | 0.015 | 0.928 | 0.013 | 0.060 | − 0.006 | 0.0818 | ||
| Strict | 248.104 | 128 | 0.001 | 46.494 | 13 | 0.001 | 0.913 | 0.024 | 0.911 | 0.017 | 0.067 | − 0.07 | 0.0764 | ||
| DASS-8 | Age (< 40, ≥ 40 years) | Configural | 47.004 | 32 | 0.042 | 0.984 | – | 0.973 | – | 0.047 | 0.0349 | ||||
| Metric | 50.139 | 37 | 0.073 | 3.136 | 5 | 0.679 | 0.986 | 0.002 | 0.979 | 0.006 | 0.041 | 0.006 | 0.0348 | ||
| Strong | 60.908 | 43 | 0.037 | 10.769 | 6 | 0.096 | 0.981 | 0.005 | 0.976 | 0.003 | 0.044 | − 0.003 | 0.0371 | ||
| Strict | 73.699 | 52 | 0.026 | 12.791 | 9 | 0.172 | 0.977 | 0.004 | 0.976 | 0.000 | 0.044 | 0.000 | 0.0407 | ||
| DASS-12 | Age (< 40, ≥ 40 years) | Configural | 164.205 | 100 | 0.001 | 0.954 | 0.940 | 0.055 | 0.0455 | ||||||
| Metric | 188.199 | 109 | 0.001 | 23.994 | 9 | 0.004 | 0.944 | 0.010 | 0.932 | 0.008 | 0.059 | − 0.004 | 0.0465 | ||
| Strong | 201.257 | 115 | 0.001 | 13.058 | 6 | 0.042 | 0.939 | 0.005 | 0.930 | 0.002 | 0.059 | 0.000 | 0.0556 | ||
| Strict | 244.418 | 128 | 0.001 | 43.161 | 13 | 0.001 | 0.917 | 0.022 | 0.915 | 0.015 | 0.065 | − 0.006 | 0.0545 | ||
| DASS-8 | Menopausal status | Configural | 52.020 | 32 | 0.014 | 0.979 | 0.011 | 0.964 | 0.055 | 0.0353 | |||||
| Metric | 67.719 | 37 | 0.002 | 15.699 | 5 | 0.008 | 0.968 | 0.008 | 0.952 | 0.012 | 0.063 | 0.008 | 0.0341 | ||
| Strong | 81.087 | 43 | 0.001 | 13.369 | 6 | 0.038 | 0.960 | – | 0.949 | 0.003 | 0.065 | − 0.002 | 0.0375 | ||
| Strict | 89.725 | 52 | 0.001 | 8.638 | 9 | 0.471 | 0.961 | 0.001 | 0.958 | 0.009 | 0.059 | 0.006 | 0.0376 | ||
| DASS-12 | Menopausal status | Configural | 207.346 | 100 | 0.001 | 0.924 | – | 0.899 | – | 0.071 | 0.0406 | ||||
| Metric | 213.566 | 109 | 0.001 | 6.220 | 9 | 0.718 | 0.926 | 0.002 | 0.910 | 0.011 | 0.068 | 0.003 | 0.0412 | ||
| Strong | 219.012 | 115 | 0.001 | 5.446 | 6 | 0.488 | 0.926 | 0.000 | 0.915 | 0.005 | 0.066 | 0.002 | 0.0429 | ||
| Strict | 249.779 | 128 | 0.001 | 30.767 | 13 | 0.767 | 0.913 | 0.013 | 0.911 | 0.003 | 0.067 | − 0.001 | 0.0448 | ||
| DASS-8 | Psychiatric comorbidity | Configural | 61.049 | 32 | 0.014 | 0.960 | 0.931 | 0.066 | 0.0598 | ||||||
| Metric | 75.127 | 37 | 0.002 | 14.078 | 5 | 0.015 | 0.948 | 0.012 | 0.921 | 0.010 | 0.071 | − 0.005 | 0.0677 | ||
| Strong | 114.929 | 43 | 0.001 | 39.803 | 6 | 0.001 | 0.902 | 0.046 | 0.872 | 0.049 | 0.090 | 0.019 | 0.1384 | ||
| Strict | 140.861 | 52 | 0.001 | 25.932 | 9 | 0.002 | 0.879 | 0.023 | 0.870 | 0.002 | 0.091 | − 0.001 | 0.0964 | ||
| DASS-12 | Psychiatric comorbidity | Configural | 161.746 | 100 | 0.001 | 0.943 | 0.925 | 0.055 | 0.0798 | ||||||
| Metric | 175.878 | 109 | 0.001 | 14.132 | 9 | 0.118 | 0.938 | 0.005 | 0.925 | 0.000 | 0.055 | 0.000 | 0.0814 | ||
| Strong | 198.757 | 115 | 0.001 | 22.879 | 6 | 0.001 | 0.923 | 0.016 | 0.911 | 0.014 | 0.059 | − 0.004 | 0.1117 | ||
| Strict | 268.320 | 128 | 0.001 | 69.562 | 13 | 0.001 | 0.871 | 0.052 | 0.867 | 0.044 | 0.073 | − 0.014 | 0.0965 |
χ2, chi-square; df, degrees of freedom; CFI, comparative fit index; TLI, Tucker–Lewis index; RMSEA, root mean square error of approximation; CI, confidence interval; SRMR, standardized root mean residual.
Significant values are given in bold.
Results of known-group validity and discriminant validity tests
As noted in Table 4, the DASS-21, DASS-8, DASS-12 differentiated women with a current psychiatric disorder from those without psychiatric comorbidity at the same level of significance (p < 0.001), which supports known-group validity of these measures. However, the z scores of the DASS-8 and its subscales were higher than those of the DASS-12 and the DASS-21, indicating a higher level of discriminant validity. Nonetheless, neither the DASS-21, DASS-8, DASS-12 nor their subscales could differentiate women with a diagnosis of depression from those with a diagnosis of anxiety. Likewise, the DASS-21, DASS-8, DASS-12, and their subscales significantly correlated with subjective experience of anxiety and low mood at the same levels (all p values < 0.01, Table 5). HTMT ratio of correlations showed that the constructs covered by the subscales of the DASS-8 and DASS-12 were distinct (< 0.85). However, the stress and anxiety subscales on the DASS-8 were overlapping (HTMT ratio = 0.95, Appendix 2: Supplementary Table 11). All the subscales of the parent scale exhibited overlap, albeit it was marginal for the stress-anxiety subscales (HTMT ratio = 0.85, Appendix 2: Supplementary Table 15).
Table 4.
Descriptive statistics and discriminant validity of the Depression Anxiety Stress Scale 21 and its shortened versions among women with chronic pelvic pain.
| DASS versions | Whole sample (N = 214) |
Mann Whitney test | z | Cluster 1 (n = 141) |
Cluster 2 (n = 73) |
Mann Whitney test | z |
|---|---|---|---|---|---|---|---|
| MD (IQR) | MD (IQR) | MD (IQR) | |||||
| DASS-21 | 11.5 (6.0–23.8) | 2247.5 | − 5.49 | 7.0 (4.0–11.8) | 29.5 (23.0–36.8) | 210.0 | − 11.43 |
| Depression | 2.0 (1.0–7.0) | 2495.5 | − 5.08 | 1.0 (0–3.0) | 9.0 (5.0–14.0) | 1041.0 | − 9.65 |
| Anxiety | 3.0 (1.0–7.0) | 2482.0 | − 5.11 | 1.0 (0–3.0) | 8.0 (6.0–11.0) | 728.0 | − 10.39 |
| Stress | 6.0 (3.0–11.0) | 2641.0 | − 4.48 | 4.0 (2.0–6.0) | 12.0 (10.0–16.0) | 436.5 | − 10.91 |
| DASS-12 | 7.0 (3.0–13.3) | 2320.0 | − 5.48 | 4.0 (2.0–7.0) | 17.0 (13.0–21.0) | 397.0 | − 11.08 |
| Depression | 1.0 (1.0–4.0) | 2266.5 | − 5.80 | 0 (0–1.0) | 5.0 (3.0–8.5) | 1082.0 | − 9.77 |
| Anxiety | 2.0 (0–4.0) | 2842.0 | − 4.24 | 1.0 (0–2.0) | 4.0 (3.0–6.0) | 1514.5 | − 8.63 |
| Stress | 4.0 (2.0–7.0) | 2849.5 | − 4.16 | 2.0 (1.0–4.0) | 8.0 (6.0–9.5) | 856.0 | − 10.05 |
| DASS-8 | 4.0 (1.0–8.0) | 2018.0 | − 6.27 | 2.0 (1.0–3.0) | 12.0 (8.0–15.0) | 36.0 | − 11.95 |
| Depression | 1.0 (0–3.0) | 2346.5 | − 5.60 | 0 (0–1.0) | 4.0 (2.0–6.0) | 1214.0 | − 9.47 |
| Anxiety | 1.0 (0–3.0) | 2521.0 | − 5.21 | 0 (0–1.0) | 4.0 (3.0–6.0) | 674.0 | − 10.93 |
| Stress | 2.0 (1.0–3.0) | 2447.0 | − 5.26 | 1.0 (0–2.0) | 4.0 (3.0–5.0) | 364.0 | − 11.37 |
DASS: Depression Anxiety Stress Scale, MD: median, IQR: interquartile range, U: Mann Whitney U test, p values were all significant at 0.001 level. For the DASS-21 (N = 212).
Table 5.
Internal consistency, predictive validity, normality, and criterion validity of the Depression Anxiety Stress Scale (DASS) 21, DASS-12, DASS-8, and their subscales among women with chronic pelvic pain.
| Criteria | DASS-21 | Depression | Anxiety | Stress | DASS-12 | Depression | Anxiety | Stress | DASS-8 | Depression | Anxiety | Stress |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient alpha | 0.945 | 0.931 | 0.837 | 0.878 | 0.898 | 0.845 | 0.693 | 0.827 | 0.901 | 0.892 | 0.794 | 0.705 |
| Range of corrected item-total correlations | 0.401–0.776 | 0.598–0.847 | 0.370–0.713 | 0.593–0.735 | 0.401–0.785 | 0.607–0.719 | 0.371–0.550 | 0.607–0.746 | 0.629–0.744 | 0.882–0.944 | 0.634–0.662 | 0.545 |
| Range of alpha if-item-deleted | 0.940–0.946 | 0.914–0.939 | 0.795–0.853 | 0.851–0.869 | 0.881–0.902 | 0.787–0.833 | 0.585–0.708 | 0.742–0.809 | 0.884–0.893 | 0.831–0.870 | 0.702–0.733 | – |
| Correlation with subscale of the DASS-21 | – | – | – | – | – | 0.930*** | 0.919*** | 0.948*** | – | 0.934*** | 0.871*** | 0.871*** |
| Correlation with the DASS-21 | – | 0.856*** | 0.823*** | 0.929*** | 0.966*** | 0.838*** | 0.718*** | 0.863*** | 0.943*** | 0.811*** | 0.789*** | 0.818*** |
| Shapiro Wilk test | 0.892*** | 0.812*** | 0.848*** | 0.936*** | 0.906*** | 0.787*** | 0.843*** | 0.933*** | 0.864*** | 0.788*** | 0.790*** | 0.891*** |
| Correlation with sexual assault experience | 0.203** | 0.264*** | 0.196** | 0.134 | 0.192* | 0.278*** | 0.095 | 0.106 | 0.259** | 0.245** | 0.261*** | 0.188* |
| Correlation with pain days/month | 0.183** | 0.137 | 0.221** | 0.183** | 0.193** | 0.190** | 0.204** | 0.136 | 0.180* | 0.177* | 0.172* | 0.163* |
| Correlation with pain-free days/month | − 0.182** | − 0.132 | − 0.217** | − 0.174* | − 0.193** | − 0.188** | − 0.201** | − 0.139* | − 0.179* | − 0.173* | − 0.168* | − 0.168* |
| Correlation with severity of pain today | 0.265*** | 0.217** | 0.331*** | 0.238** | 0.290*** | 0.255*** | 0.291*** | 0.239** | 0.265*** | 0.225** | 0.274*** | 0.234** |
| Correlation with severity of stabbing pelvic pain | 0.200** | 0.167* | 0.287** | 0.138 | 0.209** | 0.174* | 0.246** | 0.143 | 0.205** | 0.149* | 0.246** | 0.153* |
| Correlation with severity of pain during sexual activity | 0.262** | 0.308*** | 0.210* | 0.222** | 0.280** | 0.326*** | 0.187* | 0.229** | 0.257** | 0.285** | 0.218** | 0.227** |
| Correlation with severity of bad headache | 0.387*** | 0.300** | 0.253** | 0.378*** | 0.395*** | 0.324*** | 0.221* | 0.363*** | 0.299** | 0.303** | 0.225* | 0.234** |
| Correlation with experienced anxiety | 0.517** | 0.430** | 0.412** | 0.491** | 0.498** | 0.427** | 0.323** | 0.478** | 0.531** | 0.425** | 0.473** | 0.467** |
| Correlation with experienced low mood | 0.487** | 0.482** | 0.323** | 0.446** | 0.478** | 0.512** | 0.227** | 0.447** | 0.514** | 0.492** | 0.400** | 0.412** |
| Correlation with experienced fatigue | 0.345** | 0.296** | 0.333** | 0.305** | 0.348** | 0.300** | 0.346** | 0.288** | 0.322** | 0.283** | 0.231** | 0.298** |
| Correlation with poor sleep | 0.303** | 0.250** | 0.337** | 0.248** | 0.305** | 0.227** | 0.329** | 0.238** | 0.283** | 0.246** | 0.240** | 0.257** |
| Correlation with dizziness | 0.251** | 0.174** | 0.333** | 0.191** | 0.243** | 0.192** | 0.335** | 0.150* | 0.244** | 0.181** | 0.262** | 0.211** |
| Correlation with unusual sweating | 0.238** | 0.182** | 0.280** | 0.215** | 0.239** | 0.174* | 0.306** | 0.197** | 0.222** | 0.179** | 0.189** | 0.257** |
| Correlation with nausea | 0.256** | 0.240** | 0.339** | 0.180* | 0.259** | 0.221** | 0.349** | 0.145* | 0.236** | 0.219** | 0.260** | 0.154* |
| Correlation with bloating | 0.259** | 0.216** | 0.255** | 0.206** | 0.247** | 0.213** | 0.234** | 0.193** | 0.279** | 0.245** | 0.234** | 0.246** |
*, **, ***: correlation is significant at a level of 0.05, 0.01, 0.001, respectively.
In two-step cluster analysis, the DASS-8 and its subscales classified the participants into two clusters: low distress (cluster 1: n = 141, 65.9%) and high distress (cluster 2: n = 73, 34.1%). The model expressed good fit as indicated by Silhouette measure of cohesion and separation of around 0.7 and ratio of sizes less than 3 (1.93). Values of the predictor importance of the DASS-8 followed by stress, anxiety, and depression were 1, 0.85, 0.73, and 0.5, respectively. Mann Whitney U test revealed significant differences in the level of all mental distress symptoms among participants in both clusters—they were all significantly higher in cluster 2 than in cluster 1 (all p values < 0.001), with the DASS-8 and its stress subscale expressing the highest z scores (Table 4).
Age, menopausal status, bloating, and the frequency of stabbing pelvic pain and sex pain did not vary significantly across clusters. However, participants in cluster 2 demonstrated significantly higher number of pain days (t(146.9) = − 2.50, p = 0.014), less pain free days (U = 3654.0, z = − 2.39, p = 0.017); more severity of stabbing pelvic pain (t(134.42) = − 2.47, p = 0.015), sex pain (t(105.22) = − 3.74, p = 0.001), current pelvic pain (U = 3095.0, z = − 3.29, p = 0.001), concurrent headache (t(118.11) = − 3.51, p = 0.001); as well as higher frequency of bowel pain (χ2(1) = 6.68, p = 0.010), greater occurrence of sexual assault (χ2(1) = 19.06, p = 0.001), psychiatric co-morbidity (χ2(2) = 23.61, p = 0.001), subjective experience of psychiatric symptoms ((low mood (χ2(16) = 29.8, p = 0.001) and anxiety (χ2(1) = 50.50, p = 0.001)), fatigue (χ2(1) = 14.12, p = 0.001), and sleep problems (χ2(16) = 12.13, p = 0.001)), as well as somatic symptoms ((dizziness (χ2(1) = 7.57, p = 0.006), unusual sweating (χ2(1) = 9.52, p = 0.002), and nausea (χ2(1) = 13.65, p = 0.001)).
Results of tests of reliability, normality, and criterion validity
The reliability of the DASS-21, DASS-8, and DASS-12 was excellent. Meanwhile, the reliability of the shortened subscales ranged from very good to poor (Table 5)—poor reliability was reported only for the anxiety subscale of the DASS-12. The predictive validity of the DASS-8, DASS-12, and their subscales was depicted by their strong correlation with the original scale and its subscales (Table 5). The normality of the DASS-8 and the DASS-12 was comparable with that of the DASS-21 as noted by Shapiro–Wilks’ W. As shown in Table 5, all the DASS versions and most of their subscales negatively correlated with pain-free days and positively correlated with pain experience on the survey day, pain days per month, concurrent headache, poor sleep, fatigue, somatic symptoms (nausea, bloating, dizziness, unusual sweating), experience of low mood and anxiety, as well as sexual assault experience. Notably, all the subscales of the DASS-8 had significant positive correlations with sexual assault experience while the anxiety and stress subscales of the DASS-12 as well as the stress subscale of the DASS-21 did not significantly correlate with this variable. Similarly, all the subscales of the DASS-8 significantly correlated with the severity of stabbing pelvic pain while the stress subscale of the DASS-12 and the DASS-21 failed to significantly correlate with this variable (Table 5).
Discussion
Distress management may considerably affect CPP recovery2. This is because a considerable proportion of CPP patients experience excessive levels of distress2,8,9,16. Because resources allocated for disease management are limited16, there is a great need for brief measures that may facilitate the identification of highly distressed patients as well as their response to treatment35. Using numerous robust psychometric testing techniques, the present study suggests usefulness of the DASS-8 as a measure of distress, depression, anxiety, and stress symptomatology among Australian women with CPP.
The crude models of the three-factor structure of the DASS-8/DASS-12/DASS-21 expressed better fit than all other crude models. As for the DASS-8, the value of RMSEA was on high while other fit indices indicated good fit. In simple CFA and path models, which have few degrees of freedom (df), RMSEA may incorrectly indicate poor fit, even when data actually fit the model well48,49. However, other absolute fit indicators such as SRMR and CFI are less influenced by the effects of df in these models compared with RMSEA. The confidence intervals and p-values of SRMR and CFI are recorded to provide more accurate information on differentiating models with various levels of misfit49. Therefore, in models with small df, researchers are recommended to rely more on SRMR and CFI and take caution when interpreting RMSEA or completely avoid its use49,50. The value of RMSEA for the bifactor structure based on the three-factor model of the DASS-8 (Model 3, Table 2) was within the acceptable bound, without a need to correlate any errors, which suggests that RMSEA produced for the three-factor structure of the DASS-8 reflects a pseudo-misfit.
The fit of the three-factor structure of all the DASS scales was improved by correlating few error terms (Fig. 1, Appendix 1: Fig. 1b). The correlation involving item 12 “I found it difficult to relax” on the stress subscale and item 13 “I felt down-hearted and blue” on the depression subscale of the DASS-8 may suggest overlap of negative affect with comorbidities in this sample. This logic is based on the findings of network analyses comprising data from community-dwelling adults with a history of trauma: “inability to relax” and “diminished positive emotions” were key hub symptoms, which connected major distinct symptom groups that were identified as presentations of the disorders of depression, generalized anxiety, and PTSD, denoting psychopathological comorbidity in that sample51. In our study, item 12 and item 13 were strongly correlated (r = 0.58, p = 0.001). Moreover, the levels of symptoms expressed by both items, in order, were significantly higher among those with a formal current diagnosis of mental disorders (U = 2745.5, 2507.5; z = − 4.6 4, − 5.38; p values = 0.001) as well as those who reported sexual assault (U = 1315.5, 1037.5; z = − 2.684, − 4.03; p = 0.001 and 0.007) compared with disease- and abuse-free women. On the other hand, correlations involving item 12 and item 1 “I found it difficult to wind down” on the stress subscale of the DASS-12 (Fig. 1b) and the DASS-21 may obviously be related to the fact that the meanings of “difficult to relax” and “difficult to wind down” are almost the same—a possible indicator of item redundancy. In fact, several items of the stress subscale of the DASS-21 were removed in a former testing in numerous Asian samples, resulting in the revised DASS-18. This short version demonstrated a cleaner factorial structure and smaller inter-factor correlations relative to the DASS-2127.
The final model of the DASS-8 (Model 2 with correlated errors) expressed a perfect fit on all CFA fit indices, superior to the DASS-12, indicating a better construct validity of the DASS-8 as we hypothesized. Meanwhile, the fit of the second-order factor structure of all DASS scales was similar to the three-factor structure (Appendix 1, Appendix 2), indicating usability of the total score and the scores of the subscales of these scales. Evidently more error correlations were necessary to achieve an acceptable fit of the three-factor structure of the DASS-21 (Appendix 1: Fig. 1b). Of interest, correlated errors noticed in the structures of the DASS-8/DASS-12 were among those suggested to improve the fit of three-factor structure of the parent scale, which supports an interaction of comorbidities in this population and item redundancy as argued above.
The three-factor structures of both short scales exhibited configural, metric, scalar, and strict invariance across groups of age and menopausal status. Across groups of psychiatric comorbidity, the DASS-8 was non-invariant at the scalar level and the DASS-12 expressed misfit (indicating tendency toward non-invariance) at the scalar level and it was non-invariant at the strict level. Critical ratios for differences between parameters indicated that non-invariance of the DASS-8 involved: (1) lower loadings of item 20 “I felt scared without any good reason” on the anxiety subscale and item 12 on the stress subscale, (2) weaker correlation between the anxiety and depression subscales, and (3) less covariance between items 12 and 13. All were noted among participants not diagnosed with a mental disorder compared with those having a psychiatric disorder. This result is congruent with our aforementioned argument concerning a possible effect of comorbidity on the interactions taking place among the items and factors of the DASS-8. Non-invariance of the DASS-12 involved differences in the loading of item 17 “I felt I was not worth much as a person” and the variances of items 1, 3 “I couldn’t seem to experience any positive feeling at all”, and 10 “I felt that I have nothing to look forward”—all on the depression subscale.
The DASS-8 can be a beneficial brief measure for identifying CPP women with psychiatric comorbidity, high level of distress, and other debilitating symptoms (e.g., greater pain severity, poor sleep, concurrent headache, gastrointestinal discomfort, etc.). This is because the DASS-8 adequately differentiated CPP women with psychiatric comorbidities from those who are mental illness free. Although known-group validity of the DASS-8, DASS-12, and DASS-21 was expressed at the same level of significance (p = 0.001), the z scores associated with the DASS-8 were higher than those of the DASS-12 and DASS-21 (Table 4). This finding along with HTMT ratios denote superior discriminant validity of the DASS-8. This finding is consistent with a former investigation in which the DASS-8 potently identified psychiatric patients from healthy subjects32. On the other side, the DASS-8 as well as the DASS-12 and the DASS-21 could not discriminate CPP women with depression disorder from those with anxiety disorder. In line, the DASS-21 and the DASS-12 have been previously reported to lack the capacity to differentiate depression disorder from anxiety disorder21,29,52. These findings are consistent with other results on the reported comorbidity of both depression and anxiety disorders, confirming that the DASS measure is not a clinically diagnostic tool, but it can efficiently identify individuals prone to both depression and anxiety psychopathologies53,54. This can be a merit of a brief self-administered measure. Extra diagnostic workout can be performed in a next step to attain a formal diagnosis.
In two-step cluster analysis, the DASS-8 and its subscales classified CPP women into two clusters with low and high levels of distress. The DASS-8 and its stress subscale had higher predictor importance values than anxiety and depression. Mann Whitney U test revealed significant differences (all p values = 0.001) in the scores of all the DASS measures among women in both clusters, with the DASS-8 and its stress subscale exhibiting the highest z scores (Table 4). As shown in Table 1, participants in cluster 2 (high distress) scored significantly higher on symptoms of pain severity, bowel pain, depression, anxiety, fatigue, dizziness, nausea, and unusual sweating than participants in cluster 1. This finding is consistent with a former study, which classified women into two clusters: one cluster comprised women high on depression, fatigue, and poor sleep while the other cluster comprised women experiencing no or minimal levels of these symptoms16. However, Mann Whitney U test and cluster analysis in the present study indicate stronger discriminant validity of the DASS-8 and its stress and anxiety subscales than the depression subscale. Overall, the DASS-8 can be efficiently used to differentiate highly distressed CPP women (e.g., with psychiatric comorbidity and more severity of mental symptoms, pain, and physical symptoms) from those with low levels of distress.
Apart from good fit, invariance, and adequate discriminant validity, the DASS-8 demonstrates other excellent psychometric characteristics. As shown in Table 5, the internal consistency of the DASS-8 and all its subscale was good—considerably higher than that of the DASS-12 as we hypothesized, except for the stress subscale, which comprises half the number of items on the corresponding subscale of the DASS-12. Whereas the values of alpha-if-item deleted indicated reduction in the reliability of the DASS-8, they indicated an increase in the reliability of the DASS-12 and its anxiety subscale (Table 5), lending support to the more robust convergent validity of the DASS-8. Consistent with our preset hypothesis, strong correlations of the DASS-8 and its subscales with the DASS-21 and its subscales convey adequate item coverage, predictive validity, and convergent validity. Generally, these results highlight the high homogeneity, specificity, and sensitivity of the items comprising the DASS-8, which have been reported among Arab and English-speaking participants31,32.
In parallel, the DASS-8 and all its subscales exhibited significant correlations with sexual assault, pain duration (pain days per months), pain-free days, pain intensity, somatic symptoms, fatigue, poor sleep, bad headache, etc. On the other hand, the stress and depression subscales of the DASS-21 failed to significantly correlate with sexual assault and pain-free days, respectively. Likewise, the anxiety and depression subscales of the DASS-12 failed to significantly correlate with sexual assault while the correlation of the overall DASS-12 with sexual assault was at a lower level than that expressed by the DASS-8 (r = 0.192, p = 0.05 vs r = 0.259, p = 0.01). These findings indicate better criterion validity of the DASS-8. They are also congruent with recent studies reporting significant correlations of the subscales of the DASS-21 with stabbing pelvic pain, migraine, intimate partner violence/domestic violence; as well as early childhood physical, sexual and emotional abuse among women3,14,15,55. Therefore, the DASS-8 can be reliably used as a valid criterion to predict different noxious symptoms and experiences in CPP.
This study is the first attempt to confirm the psychometric soundness of the DASS-8 as a measure of mental symptomatology among Australian women with CPP. Results obtained from different robust testing techniques in this study emphasize excellent psychometric properties of the DASS-8; in terms of fit, invariance, predictive validity, convergent validity, discriminant validity, criterion validity, and reliability. These finding are all in line with those previously reported in Arab psychiatric patients as well as in healthy respondents from Saudi Arabia, Australia, the US, and Ghana31,32. In the meantime, this study is different from previous studies given the chronic and complicated nature of CPP. It extended the criterion validity of the DASS-8 by relating it to collateral physical complaints, pain variables, and history of sexual abuse—the latter was not correlated to one subscale of the DASS-21 and two subscales of the DASS-12. Another key originality aspect of the present study was revealed by cluster analysis—the DASS-8 classified CPP women into a low-distress group and a high-distress group. As shown in Tables 1 and 4, the high-distress group is evidently in needed for further diagnostic investigations and treatment because its members scored high on pain severity variables, several physical complaints, the DASS-21, and the DASS-12. Therefore, the DASS-8 can be used as a brief scale to identify CPP women who are prone to physical comorbidity and psychopathology, which may have implications for the diagnosis and treatment of psychiatric comorbidity among these women, eventually resulting in improved pelvic pain recovery.
This study has also many limitations, which should be acknowledged. The generalizability of the finding is limited out of possible risk for selection bias: (1) the sample is collected from a single clinic, (2) a priori power analysis for determining the sample size is lacking, (3) data on the respondents who declined participation in the survey are lacking, (4) the inclusion and exclusion criteria are not clearly defined, and (5) the results are based on a convenience sample, which may not represent all CPP women in other settings or countries. The cross-sectional design used precludes test–retest reliability testing. There is no information available on the validity of the measures of pain and physical complaints, which may cast doubt on the soundness of the relationships that are reported in criterion validity tests. Thus, future investigations may use a longitudinal design to examine the properties of the DASS-8 as well as causal direction of effects addressed in this study, along with mechanisms underlying links between psychological distress, pain, sleep problems, concurrent headache, etc. Moreover, all the published evaluations of the DASS-8 are produced by the same group of authors/co-authors, which may entail a risk of bias for reporting and interpreting the available results. Therefore, more investigations by independent researchers are needed.
Conclusion
Psychometric evaluation of the DASS-8 among CPP women by numerous robust techniques revealed its proper fit, invariance, high reliability, good convergent validity, sound discriminant validity, adequate predictive validity, and good criterion validity. The results indicate usability of the DASS-8 as a brief, reliable, invariant measure of mental symptoms in reproductive age and menopausal women with CPP. Timely identification of highly distressed women would encourage prompt use of relevant psychiatric intervention. Owing to its brevity, the DASS-8 can facilitate frequent monitoring of common mental symptomatology over the course of CPP treatment, supporting efforts directed toward improving recovery in CPP population.
Supplementary Information
Author contributions
A.A. and R.A. conceptualized the study. A.A., G.S., and S.M.T.L. designed the methodology. A.O.H., N.I., A.H.A., and E.M.A. obtained the materials from the original study and rewritten them, obtained the data from Zenodo repository, and cleaned the data. A.A. and A.O.H., and A.A.A. performed the statistical analysis. N.I., S.M.T.L., E.M.A. prepared the figures and the tables. R.A., G.S., and A.A. interpreted the data. A.H.A., G.S., A.A.A., and A.O.H. wrote the initial draft of the manuscript. A.A. and R.A. edited and revised the final draft. Supervision and project administration—A.A. All the authors have critically revised and approved the final draft of the manuscript.
Data availability
The dataset38 supporting the conclusions of this article is available in Zenodo repository, (https://zenodo.org/record/1307252#.YckoVWhBw2w), and also the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-15005-z.
References
- 1.Hassan S, Muere A, Einstein G. Ovarian hormones and chronic pain: A comprehensive review. PAIN®. 2014;155:2448–2460. doi: 10.1016/j.pain.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 2.Brooks T, Sharp R, Evans S, Baranoff J, Esterman A. Psychological interventions for women with persistent pelvic pain: A survey of mental health clinicians. J. Multidiscip. Healthc. 2021;14:1725–1740. doi: 10.2147/jmdh.s313109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brooks T, Sharp R, Evans S, Baranoff J, Esterman A. Predictors of depression, anxiety and stress indicators in a cohort of women with chronic pelvic pain. J. Pain Res. 2020;13:527–536. doi: 10.2147/jpr.s223177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartl T, Wolf F, Dadak C. Pelvic congestion syndrome (PCS) as a pathology of postmenopausal women: A case report with literature review. BMC Womens Health. 2021;21:181. doi: 10.1186/s12905-021-01323-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend. Med. 2009;6:152–167. doi: 10.1016/j.genm.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang Y, Cao C, Du S, Fan L, Zhang D, Wang X, He M. Estrogen regulates endoplasmic reticulum stress-mediated apoptosis by ERK-p65 pathway to promote endometrial angiogenesis. Reprod. Sci. 2021;28:1216–1226. doi: 10.1007/s43032-020-00414-0. [DOI] [PubMed] [Google Scholar]
- 7.Ali AM, Ahmed AH, Smail L. Psychological climacteric symptoms and attitudes toward menopause among Emirati women. Int. J. Environ. Res. Public Health. 2020;17:5028. doi: 10.3390/ijerph17145028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siqueira-Campos VME, Da Luz RA, de Deus JM, Martinez EZ, Conde DM. Anxiety and depression in women with and without chronic pelvic pain: Prevalence and associated factors. J. Pain Res. 2019;12:1223–1233. doi: 10.2147/jpr.s195317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Della Corte L, Di Filippo C, Gabrielli O, Reppuccia S, La Rosa VL, Ragusa R, Fichera M, Commodari E, Bifulco G, Giampaolino P. The burden of endometriosis on women’s lifespan: A narrative overview on quality of life and psychosocial wellbeing. Int. J. Environ. Res. Public Health. 2020;17:4683. doi: 10.3390/ijerph17134683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Arango-Dávila CA, Rincón-Hoyos HG. Depressive disorder, anxiety disorder and chronic pain: Multiple manifestations of a common clinical and pathophysiological core. Revista Colombiana de Psiquiatría (English ed.) 2018;47:46–55. doi: 10.1016/j.rcpeng.2017.12.003. [DOI] [PubMed] [Google Scholar]
- 11.Dunbar EK, Saloman JL, Phillips AE, Whitcomb DC. Severe pain in chronic pancreatitis patients: Considering mental health and associated genetic factors. J. Pain Res. 2021;14:773–784. doi: 10.2147/jpr.s274276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Soltani S, Kopala-Sibley DC, Noel M. The co-occurrence of pediatric chronic pain and depression: A narrative review and conceptualization of mutual maintenance. Clin. J. Pain. 2019;35:633–643. doi: 10.1097/ajp.0000000000000723. [DOI] [PubMed] [Google Scholar]
- 13.Consonni M, Telesca A, Grazzi L, Cazzato D, Lauria G. Life with chronic pain during COVID-19 lockdown: The case of patients with small fibre neuropathy and chronic migraine. Neurol. Sci. 2021;42:389–397. doi: 10.1007/s10072-020-04890-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dye HL. Is emotional abuse as harmful as physical and/or sexual abuse? J. Child Adolesc. Trauma. 2020;13:399–407. doi: 10.1007/s40653-019-00292-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Malik M, Munir N, Ghani MU, Ahmad N. Domestic violence and its relationship with depression, anxiety and quality of life: A hidden dilemma of Pakistani women. Pak. J. Med. Sci. 2021;37:191–194. doi: 10.12669/pjms.37.1.2893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ayorinde AA, Bhattacharya S, Druce KL, Jones GT, Macfarlane GJ. Chronic pelvic pain in women of reproductive and post-reproductive age: A population-based study. Eur. J. Pain. 2017;21:445–455. doi: 10.1002/ejp.938. [DOI] [PubMed] [Google Scholar]
- 17.Lovibond PF, Lovibond SH. Manual for the Depression Anxiety Stress Scales. 2. Psychology Foundation; 1995. [Google Scholar]
- 18.Jiang LC, Yan YJ, Jin ZS, Hu ML, Wang L, Song Y, Li NN, Su J, Wu DX, Xiao T. The depression anxiety stress scale-21 in Chinese hospital workers: Reliability, latent structure, and measurement invariance across genders. Front. Psychol. 2020;11:247. doi: 10.3389/fpsyg.2020.00247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaughan RS, Edwards EJ, MacIntyre TE. Mental health measurement in a post Covid-19 world: Psychometric properties and invariance of the DASS-21 in athletes and non-athletes. Front. Psychol. 2020;11:590559. doi: 10.3389/fpsyg.2020.590559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Henry JD, Crawford JR. The short-form version of the Depression Anxiety Stress Scales (DASS-21): Construct validity and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2005;44:227–239. doi: 10.1348/014466505x29657. [DOI] [PubMed] [Google Scholar]
- 21.Yıldırım A, Boysan M, Kefeli MC. Psychometric properties of the Turkish version of the Depression Anxiety Stress Scale-21 (DASS-21) Br. J. Guidance Counsel. 2018 doi: 10.1080/03069885.2018.1442558. [DOI] [Google Scholar]
- 22.Osman A, Wong JL, Bagge CL, Freedenthal S, Gutierrez PM, Lozano G. The Depression Anxiety Stress Scales-21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol. 2012;68:1322–1338. doi: 10.1002/jclp.21908. [DOI] [PubMed] [Google Scholar]
- 23.Bibi A, Lin M, Zhang XC, Margraf J. Psychometric properties and measurement invariance of Depression, Anxiety and Stress Scales (DASS-21) across cultures. Int. J. Psychol. 2020 doi: 10.1002/ijop.12671. [DOI] [PubMed] [Google Scholar]
- 24.Scholten S, Velten J, Bieda A, Zhang XC, Margraf J. Testing measurement invariance of the Depression, Anxiety, and Stress Scales (DASS-21) across four countries. Psychol. Assess. 2017;29:1376–1390. doi: 10.1037/pas0000440. [DOI] [PubMed] [Google Scholar]
- 25.Zanon C, Brenner RE, Baptista MN, Vogel DL, Rubin M, Al-Darmaki FR, Gonçalves M, Heath PJ, Liao HY, Mackenzie CS, et al. Examining the dimensionality, reliability, and invariance of the Depression, Anxiety, and Stress Scale-21 (DASS-21) across eight countries. Assessment. 2020 doi: 10.1177/1073191119887449. [DOI] [PubMed] [Google Scholar]
- 26.Page AC, Hooke GR, Morrison DL. Psychometric properties of the Depression Anxiety Stress Scales (DASS) in depressed clinical samples. Br. J. Clin. Psychol. 2007;46:283–297. doi: 10.1348/014466506x158996. [DOI] [PubMed] [Google Scholar]
- 27.Oei TPS, Sawang S, Goh YW, Mukhtar F. Using the Depression Anxiety Stress Scale 21 (DASS-21) across cultures. Int. J. Psychol. 2013 doi: 10.1080/00207594.2012.755535. [DOI] [PubMed] [Google Scholar]
- 28.Wise FM, Harris DW, Olver JH. The DASS-14: Improving the construct validity and reliability of the Depression, Anxiety, and Stress Scale in a cohort of health professionals. J. Allied Health. 2017;46:e85–e90. [PubMed] [Google Scholar]
- 29.Lee EH, Moon SH, Cho MS, Park ES, Kim SY, Han JS, Cheio JH. The 21-item and 12-item versions of the Depression Anxiety Stress Scales: Psychometric evaluation in a Korean population. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2019;13:30–37. doi: 10.1016/j.anr.2018.11.006. [DOI] [PubMed] [Google Scholar]
- 30.Ali AM, Alkhamees AA, Elhay ESA, Taha SM, Hendawy AO. COVID-19-related psychological trauma and psychological distress among community-dwelling psychiatric patients: People struck by depression and sleep disorders endure the greatest burden. Front Public Health. 2022 doi: 10.3389/fpubh.2021.799812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ali AM, Hori H, Kim Y, Kunugi H. The Depression Anxiety Stress Scale 8-items expresses robust psychometric properties as an ideal shorter version of the Depression Anxiety Stress Scale 21 among healthy respondents from three continents. Front. Psychol. 2022;13:799769. doi: 10.3389/fpsyg.2022.799769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ali AM, Alkhamees AA, Hori H, Kim Y, Kunugi H. The Depression Anxiety Stress Scale 21: Development and validation of the Depression Anxiety Stress Scale 8-item in psychiatric patients and the general public for easier mental health measurement in a post-COVID-19 world. Int. J. Environ. Res. Public Health. 2021;18:10142. doi: 10.3390/ijerph181910142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ali AM, Al-Amer R, Kunugi H, Stănculescu E, Taha SM, Saleh MY, Alkhamees AA, Hendawy AO. The Arabic version of the Impact of Event Scale—Revised: Psychometric evaluation in psychiatric patients and the general public within the context of COVID-19 outbreak and quaran-tine as collective traumatic events. J. Pers. Med. 2022;12:681. doi: 10.3390/jpm12050681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Robinson MA. Using multi-item psychometric scales for research and practice in human resource management. Hum. Resour. Manag. 2018;57:739–750. doi: 10.1002/hrm.21852. [DOI] [Google Scholar]
- 35.Sweetland AC, Belkin GS, Verdeli H. Measuring depression and anxiety in sub-saharan Africa. Depress Anxiety. 2014;31:223–232. doi: 10.1002/da.22142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Office of the Surgeon General (US); Center for Mental Health Services (US); National Institute of Mental Health (US). Mental Health: Culture, R., and Ethnicity: A Supplement to Mental Health: A Report of the Surgeon General. Rockville (MD): Substance Abuse and Mental Health Services Administration (US);. Chapter 2 Culture Counts: The Influence of Culture and Society on Mental Health. 2001 Aug. [PubMed]
- 37.McCracken LM, Faber SD, Janeck AS. Pain-related anxiety predicts non-specific physical complaints in persons with chronic pain. Behav. Res. Ther. 1998;36:621–630. doi: 10.1016/S0005-7967(97)10039-0. [DOI] [PubMed] [Google Scholar]
- 38.Brooks, T. Predictors of depression, anxiety and stress indicators in a cohort of women with chronic pelvic pain data set. Zenodo 10.5281/zenodo.1307252 (2018). [DOI] [PMC free article] [PubMed]
- 39.Ali AM, Green J. Factor structure of the depression anxiety stress Scale-21 (DASS-21): Unidimensionality of the Arabic version among Egyptian drug users. Subst. Abuse Treat. Prev. Policy. 2019;14:40. doi: 10.1186/s13011-019-0226-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ali AM, Hori H, Kim Y, Kunugi H. Predictors of nutritional status, depression, internet addiction, Facebook addiction, and tobacco smoking among women with eating disorders in Spain. Front. Psychiatry. 2001;2021:12. doi: 10.3389/fpsyt.2021.735109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ali AM, Hendawy AO, Ahmad O, Sabbah HA, Smail L, Kunugi H. The Arabic version of the Cohen perceived stress scale: Factorial validity and measurement invariance. Brain Sci. 2021;11:419. doi: 10.3390/brainsci11040419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ali AM, Al-Amer R, Atout M, Ali TS, Mansour AMH, Khatatbeh H, Alkhamees AA, Hendawy AO. The nine-item Internet Gaming Disorder Scale (IGDS9-SF): Its psychometric properties among Sri Lankan students and measurement invariance across Sri Lanka, Turkey, Australia, and the USA. Healthcare. 2022;10:490. doi: 10.3390/healthcare10030490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ali AM, Hendawy AO, Almarwani AM, Alzahrani N, Ibrahim N, Alkhamees AA, Kunugi H. The Six-item Version of the Internet Addiction Test: Its development, psychometric properties, and measurement invariance among women with eating disorders and healthy school and university students. Int. J. Environ. Res. Public Health. 2021;18:12341. doi: 10.3390/ijerph182312341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ali AM, Hendawy AO, Elhay ESA, Ali EM, Alkhamees AA, Kunugi H, Hassan NI. The Bergen Facebook Addiction Scale: Its psychometric properties and invariance among women with eating disorders. BMC Women’s Health. 2022;22:99. doi: 10.1186/s12905-022-01677-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Henseler J, Ringle CM, Sarstedt M. A new criterion for assessing discriminant validity in variance-based structural equation modeling. J. Acad. Market. Sci. 2015;43:115–135. doi: 10.1007/s11747-014-0403-8. [DOI] [Google Scholar]
- 46.Yu Y, Liu Z-W, Zhou W, Zhao M, Tang B-W, Xiao S-Y. Determining a cutoff score for the family burden interview schedule using three statistical methods. BMC Med. Res. Methodol. 2019;19:93. doi: 10.1186/s12874-019-0734-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Benassi M, Garofalo S, Ambrosini F, Sant'Angelo RP, Raggini R, De Paoli G, Ravani C, Giovagnoli S, Orsoni M, Piraccini G. Using Two-step cluster analysis and latent class cluster analysis to classify the cognitive heterogeneity of cross-diagnostic psychiatric inpatients. Front. Psychol. 2020;11:1085. doi: 10.3389/fpsyg.2020.01085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in models with small degrees of freedom. Sociol. Methods Res. 2015;44:486–507. doi: 10.1177/0049124114543236. [DOI] [Google Scholar]
- 49.Shi D, DiStefano C, Maydeu-Olivares A, Lee T. Evaluating SEM model fit with small degrees of freedom. Multivariate Behav. Res. 2021 doi: 10.1080/00273171.2020.1868965. [DOI] [PubMed] [Google Scholar]
- 50.Lai K, Green SB. The problem with having two watches: Assessment of fit when RMSEA and CFI disagree. Multivariate Behav. Res. 2016;51:220–239. doi: 10.1080/00273171.2015.1134306. [DOI] [PubMed] [Google Scholar]
- 51.Price M, Legrand AC, Brier ZMF, Hébert-Dufresne L. The symptoms at the center: Examining the comorbidity of posttraumatic stress disorder, generalized anxiety disorder, and depression with network analysis. J. Psychiatr. Res. 2019;109:52–58. doi: 10.1016/j.jpsychires.2018.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gloster AT, Rhoades HM, Novy D, Klotsche J, Senior A, Kunik M, Wilson N, Stanley MA. Psychometric properties of the depression anxiety and stress scale-21 in older primary care patients. J. Affect. Disord. 2008;110:248–259. doi: 10.1016/j.jad.2008.01.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995;33:335–343. doi: 10.1016/0005-7967(94)00075-U. [DOI] [PubMed] [Google Scholar]
- 54.Caetano AC, Oliveira D, Gomes Z, Mesquita E, Rolanda C. Psychometry and Pescatori projective test in coloproctological patients. Ann. Gastroenterol. 2017;30:433–437. doi: 10.20524/aog.2017.0145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Al-Hayani M, AboTaleb H, Bazi A, Alghamdi B. Depression, anxiety and stress in Saudi migraine patients using DASS-21: Local population-based cross-sectional survey. Int. J. Neurosci. 2021 doi: 10.1080/00207454.2021.1909011. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset38 supporting the conclusions of this article is available in Zenodo repository, (https://zenodo.org/record/1307252#.YckoVWhBw2w), and also the datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.