Highlights
-
•
Vertebral osteoid osteoma is often diagnosed late because of misleading signs.
-
•
CT scan is the most effective radiological examination for the diagnosis of osteoid osteoma.
-
•
Sacroiliitis is the first differential diagnosis of sacral osteoid osteoma.
-
•
Treatment of laminar osteoid osteoma is surgical because radiofrequency can damage spinal nerve cells.
Keywords: Osteoid osteoma, Bone tumor, Sacrum, Surgery
Abstract
Introduction
Sacral osteoid osteoma (OO) is a rare location. The clinical signs are misleading, hence the delay in diagnosis. Through this case, we will put. The aim of this work was to put the light on a clinical sign that may suggest the diagnosis of OO and to report the therapeutic management.
Presentation of case
We report the case of an OO located in the left lamina of the first sacral vertebra, revealed by pain in the sacroiliac joint mimicking sacroileitis in a 12-year-old child. Computed tomography and MRI revealed bone lysis in the left lamina of the first sacral vertebra consistent with the diagnosis of OO. Anatomopathological examination of the resection piece confirmed the diagnosis. Surgical removal of the tumor resolved the pain.
Discussion
The lumbar spine is the most frequently affected area, followed by the cervical, thoracic and sacral regions. Diagnosis of OO is primarily clinical. In typical cases, it is characterized by nocturnal inflammatory pain. It can simulate sciatica or sacroilitis. Nonsteroidal anti-inflammatory drugs (NSAIDs) are used to relieve pain. This is a diagnostic test.
Conclusion
Sacral OO is a rare localization and is often diagnosed late because the symptoms are misleading and polymorphic. For locations in contact with nervous elements, open surgery is the gold standard.
1. Introduction
Osteoid osteoma (OO) is a benign and rare bone tumor. The spinal location represents 40 % of the entire bony skeleton. The elements of the posterior arch, such as the pedicles and the blades are the most concerned. Its sacred location is even rarer. The diagnosis is often late because the clinical signs are misleading. The aim of this work was to put the light on a clinical sign that may suggest the diagnosis of OO and to report the therapeutic management.
This topic has been reported online with the SCARE criteria [1]:
Agha RA, Franchi T, Sohrabi C, Mathew G, Kerwan A; SCARE Group. The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines Int J Surg. 2020;84:226–230.
2. Case report
We report the case of a 12-year-old child who consulted for a lameness associated with pain in the left buttock. The patient reported a history of nocturnal pain, evolving for 6 months with a progressive onset but reduced with the use of NSAIDs. She had no particular medical and surgical history. Sacroiliac compression test, thigh thrust test and palpation over to the left sacroiliac joint were positive on the left side and trigger pain. Lasegue's sign was negative. Examination of the spine and hips revealed no abnormalities. The temperature was normal, no notion of weight loss or tuberculosis infection. The parents revealed the consumption of unpasteurized dairy products. The pelvic X-ray and the biological assessment were normal. An additional MRI showed an inflammatory-type signal anomaly in T2 hypersignal and enhancement of the left hemi-arc of S1 after injection of gadolinium (Fig. 1). The CT scan of the pelvis, in addition to the MRI, objectified osteolysis with interruption of the cortical bone of the left lamina of S1, measuring 12 mm in diameter and coming into contact with the left S1 root (Fig. 2, Fig. 3, Fig. 4) evokes an OO. The patient underwent surgical resection of the bone tumor through a posterior surgical approach. She had a resection of the lower left articular process of L5 giving direct access to the bone lesion which was completely resected. The patient did not have osteosynthesis. The pain disappeared post-operatively. Histological examination of the resection specimen confirmed the diagnosis of OO. Usual sports activity is resumed after three months. At 24 months follow-up, the spine was stable and the patient had no functional complaints.
Fig. 1.
MRI in axial section showing an edematous type hypersignal at the level of the left lamina of S1 (blue arrows). Note that the left sacroiliac joint is without anomaly. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
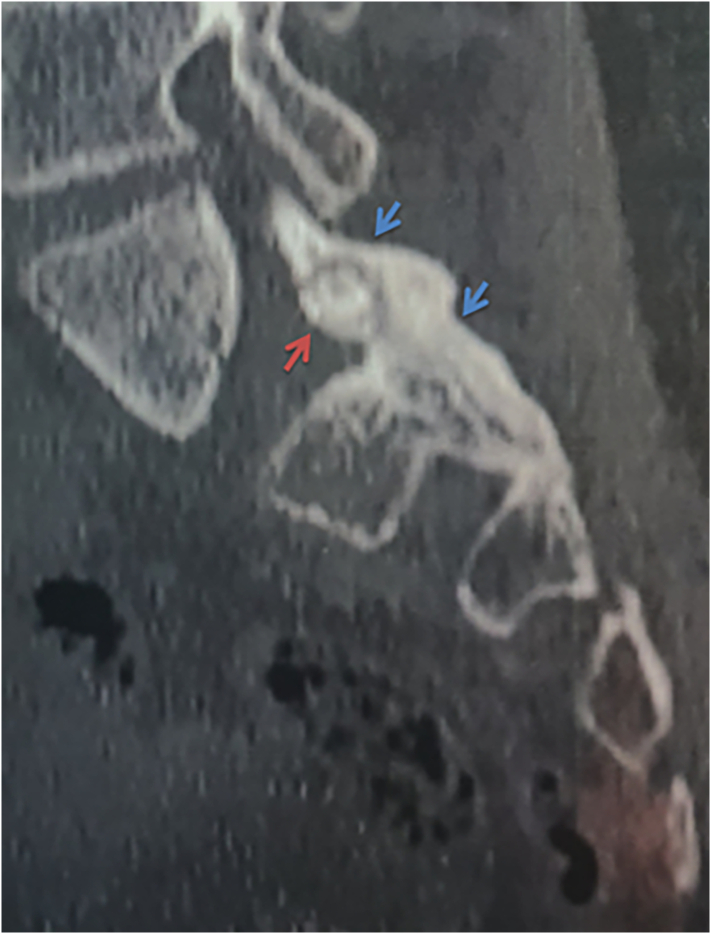
Fig. 2.
Axial section CT scan showing a typical OO aspect of the left lamina of S1: nidus (red arrows) surrounded by bony condensation (blue arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 3.
Sagittal section CT scan showing a typical OO aspect of the left lamina of S1: nidus (red arrows) surrounded by bony condensation (blue arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
Fig. 4.
Coronal section CT scan showing a typical OO aspect of the left lamina of S1: nidus (red arrows) surrounded by bony condensation (blue arrows). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
3. Discussion
OO is a benign bone lesion with a high incidence between 10 and 20 years [2]. It occurs more in the extremities than in the spine [3], [4]. The lumbar spine is the most frequently affected area, followed by the cervical, thoracic and sacral regions [5]. Diagnosis of OO is primarily clinical. In typical cases, it is characterized by nocturnal inflammatory pain [3], [6], [7], [8]. NSAIDs are used to relieve pain [6]. This is a diagnostic test. The pain is due to the irritation of nerve fibers in contact with the nidus [4] and to the peritumoral inflammatory reaction due to prostaglandins (cyclooxygenase-2) [8]. The diagnostic delay can reach 54 % in certain cases [9], [10] especially in the locations of the posterior arch of the pelvis. The clinical signs are those of sacroilitis [7], [10], [11]. The CT scan in thin sections centered on the lesion allows a good study of the OO by objectifying the nidus centered by the calcifications and the peripheral bone condensation [12] (Fig. 2, Fig. 3, Fig. 4).
MRI is an essential complement [7]. It makes it possible to eliminate a malignant tissue process, to check that there is no spinal or radicular compression [12]. Surgical treatment consists of resection of the entire tumor, preferably in one piece [6], [10], to ensure healing without risk of recurrence. The treatment of spinal OO can also be done by radiofrequency [13], [14], but the risk of neurological damage is high, especially for locations in the posterior column [15]. CT-guided resection is also possible for marginal locations without risk of damaging major organs [16]. The localization of the OO described in our case is a contraindication for radiofrequency and scan-guided resection because the tumor was in contact with the dura mater, hence an increased risk of breach or local burn.
4. Conclusion
Sacral OO is a rare localization and is often diagnosed late because the symptoms are misleading and polymorphic. CT of the pelvis is effective for the topography of the lesion. MRI is useful in ruling out differential diagnoses. For locations in contact with nervous elements, open surgery is the gold standard.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Sources of funding
None.
Ethical approval
Is exempt/waived at our institution.
Consent
Written informed consent was obtained from the patient's parent for publication of this case report and accompanying images.
Research registration
Not applicable.
Author contribution
Mohamed Zairi: Writing drafting the article, Conception and Design.
Mohamed Nabil Nessib: Final approval of the version to be published.
Guarantor
Mohamed Zairi.
Declaration of competing interest
None.
Data availability
All data is available to readers.
References
- 1.Agha R.A., Franchi T., Sohrabi C., Mathew G., Kerwan A., SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 2.Uehara M., Takahashi J., Kuraishi S., Shimizu M., Ikegami S., Futatsugi T., et al. Osteoid osteoma presenting as thoracic scoliosis. Spine J. 2015;15(12):e77–e81. doi: 10.1016/j.spinee.2015.08.064. [DOI] [PubMed] [Google Scholar]
- 3.Zhang H., Niu X., Wang B., He S., Hao D. Scoliosis secondary to lumbar osteoid osteoma: a case report of delayed diagnosis and literature review. Medicine. 2016;95(47) doi: 10.1097/MD.0000000000005362. (Baltimore) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Etemadifar M.R., Hadi A. Clinical findings and results of surgical resection in 19 cases of spinal osteoid osteoma. Asian Spine J. 2015;9:386–393. doi: 10.4184/asj.2015.9.3.386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ali Ö., Köksal A., Çimen O., Osman E.A., Akman Y.E. Painful scoliosis and osteoid osteoma of the spine. J. Turk. Spinal Surg. 2020;31(1):6. [Google Scholar]
- 6.Chen Y.L., Jiang W.Y., Ma W.H. Osteoid osteoma: lower back pain combined with scoliosis. J. Int. Med. Res. 2020;48(2) doi: 10.1177/0300060520903873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moreno-Martinez M.J., Moreno-Ramos M.J., Díaz-Navarro M.J., Linares-Ferrando L.F. Osteoma osteoide pélvico simulando sacroileitis. Reumatol. Clin. 2016;12:177–178. doi: 10.1016/j.reuma.2015.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Boscainos P.J., Cousins G.R., Kulshreshtha R., Oliver T.B., Papagelopoulos P.J. Osteoid osteoma. Orthopedics. 2013;36(10):792–800. doi: 10.3928/01477447-20130920-10. [DOI] [PubMed] [Google Scholar]
- 9.Pourfeizi H.H., Tabrizi A., Bazavar M., Sales J.G. Clinical findings and results of surgical resection of thoracolumbar osteoid osteoma. Asian Spine J. 2014;8(2):150–155. doi: 10.4184/asj.2014.8.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Duman I., Aydemir K., Tan A.K., Dinçer K., Kalyon T.A. Anunusual case of osteoid osteoma clinically mimickingsacroiliitis. Clin.Rheumatol. 2006;26(7):1158–1160. doi: 10.1007/s10067-006-0280-8. [DOI] [PubMed] [Google Scholar]
- 11.Chandwar K., Lathiya H., Gohel A., et al. Sacral osteoid osteoma: a rare cause of inflammatory back pain and sacroiliitis in a young man. BMJ Case Rep. 2021;14 doi: 10.1136/bcr-2021-244074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harish S., Saifuddin A. Imaging features of spinal osteoid osteoma with emphasis on MRI findings. Eur. Radiol. 2005;15:2396–2403. doi: 10.1007/s00330-005-2816-8. [DOI] [PubMed] [Google Scholar]
- 13.Weber M.A., Sprengel S.D., Omlor G.W., Lehner B., Wiedenhöfer B., Kauczor H.U., et al. Clinical long-term outcome, technical success, and cost analysis of radiofrequency ablation for the treatment of osteoblastomas and spinal osteoid osteomas in comparison to open surgical resection. Skelet. Radiol. 2015;44:981–993. doi: 10.1007/s00256-015-2139-z. [DOI] [PubMed] [Google Scholar]
- 14.Morassi L.G., Kokkinis K., Evangelopoulos D.S., Karargyris O., Vlachou I., Kalokairinou K., et al. Percutaneous radiofrequency ablation of spinal osteoid osteoma under CT guidance. Br. J. Radiol. 2014;87 doi: 10.1259/bjr.20140003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Theumann N., Hauser P., Schmidt S., Schnyder P., Leyvraz P.F., Mouhsine E. Thermoablation par radiofréquence de l'ostéome ostéoïde [Osteoid osteoma and radiofrequency] Rev. Med. Suisse. 2005;1(46):2989–2994. [PubMed] [Google Scholar]
- 16.Fukuda S., Susa M., Watanabe I., Nishimoto K., Horiuchi K., Toyama Y., et al. Computed tomography-guided resection of osteoid osteoma of the sacrum: a case report. J. Med. Case Rep. 2014;8:206. doi: 10.1186/1752-1947-8-206. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data is available to readers.