Dear Editors,
I read with interest the article by Pathadka et al. [1], and found the increased use of oral itraconazole in 27 middle-income countries intriguing. I was privileged to treat some of the first patients in the world with this new antifungal agent from 1987 onwards, contribute to the studies that led to its licensure in 1991 [2], and promulgate its use for non-approved indications such as allergic bronchopulmonary aspergillosis (ABPA). Our team at Global Action For Fungal Infections (GAFFI) successfully submitted itraconazole for inclusion on the World Health Organization (WHO)’s Essential Medicine List (EML) in 2017 [3, 4].
The authors show a big uptake in usage in 2015/6 preceding the WHO’s listing in 2017, and my speculations about the reasons for this is are as follows.
Chronic pulmonary aspergillosis (CPA) requires long-term, usually oral, antifungal therapy in most patients. The European Society of Clinical Microbiology and Infectious Diseases together with the European Respiratory Society developed guidelines for the management of CPA that were published in early 2016 [5]. In August 2014, I presented these draft guidelines to the pulmonary society in China (with a large audience). Subsequently we estimated that there were ~ 488,000 CPA patients in China [6]. Locally manufactured Aspergillus antigen and antibody tests were then available in China. Do the authors know if the increase seen in itraconazole was particularly marked in China?
Itraconazole is also useful for ABPA and what is now colloquially called ‘fungal asthma’. We published a slightly under-powered randomised, placebo-controlled study of itraconazole for severe asthma with fungal sensitisation showing significant benefit in quality of life in 2009 [7]. Other randomised studies of acute stage ABPA itraconazole versus corticosteroids from India [8] and all severe asthma also comparing itraconazole with (lower dose) corticosteroid from Iran [9] probably came too late to influence the consumption of itraconazole that the authors documented to 2018, and Iran is not included amongst the 38 middle-income countries. In low- and low-middle income countries, itraconazole remains a viable alternative to oral corticosteroid for severe asthma and ABPA in those who cannot afford biologics.
Both acute but also recurrent vulvovaginal candidiasis (RVVC) are very frequent, with an estimated 138 million women suffering from the latter globally [10]. RVVC responds to long-term antifungal suppression with fluconazole, but replacement of Candida albicans with C. glabrata and fluconazole resistance in C. albicans reduce its effectiveness. It is likely itraconazole has been more frequently used for this indication.
There has been increasing awareness of disseminated histoplasmosis in AIDS, thanks to the pioneering work of Mathieu Nacher, Antoine Adenis and colleagues in French Guiana [11]. Itraconazole is an important step-down and maintenance therapy for histoplasmosis, and some increased usage may have followed awareness and improved diagnostic capacity, with reduced deaths. The discovery of large numbers of such cases in Africa [12–15] should substantially increase usage further, although only three North African countries and South Africa were included in the survey.
A long-term program of estimating the incidence and prevalence of serious fungal diseases (including CPA, ABPA, fungal asthma, RVVC and histoplasmosis) has now encompassed over 80 countries [16]. Engagement of national experts in these countries has alerted them to the relatively high prevalence of these conditions, and this may have contributed to local awareness.
The first cases of terbinafine-resistant dermatophytosis (ringworm) were reported in India in 2016 [17]. Itraconazole for 3 weeks at a dose of 400 mg daily (more usually used for skin fungal infections) is about 75% effective in treating these inflammatory and disfiguring lesions. Do the authors know if there was a marked increase in consumption in India in 2017 and 2018 in response to this ongoing epidemic?
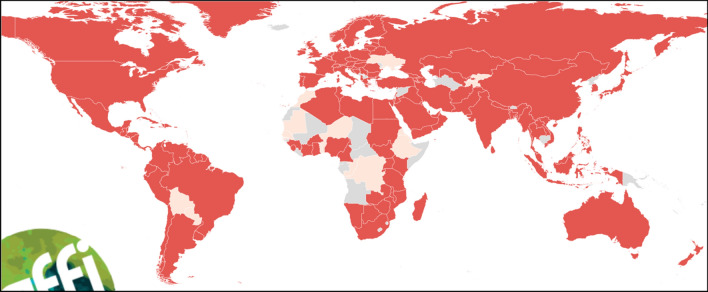
The authors reference GAFFI’s 2016 summary of antifungal drug availability across the world [18]. This has been regularly updated since and fortunately many more countries do now have itraconazole approved for use (Fig. 1), but not Bolivia, Morocco, Senegal, The Gambia, Mauritania, Benin, Niger, Democratic Republic of Congo, Ethiopia, Ukraine Kyrgyzstan and Tajikistan [19]. However, the price of itraconazole remains unaffordable for many, and in most low- and middle-income countries it is not included with universal health coverage or government-funded medications.
Fig. 1.
Countries in which itraconazole is licenced for use 2021/22. Source: https://gaffi.org/antifungal-drug-maps/. Dark red = approved for use. Pink = not approved for use. Grey = no data available.
Reproduced with permission
The authors’ survey was until 2018. The echinocandin antifungal agents were added to the WHO’s EML in 2021 [20]. It will be of interest to observe whether this has an appreciable impact on usage over the coming years, especially in middle-income countries.
Sincerely
David W. Denning
Professor of Infectious Diseases in Global Health, Manchester Fungal Infection Group, The University of Manchester, UK
Chief Executive, Global Action for Fungal Infections, Geneva, Switzerland
Declarations
Funding
No funding to declare.
Conflicts of interest
None pertain to this letter. Dr Denning and family hold Founder shares in F2G Ltd, a University of Manchester spin-out antifungal discovery company, and share options in TFF Pharma. He acts or has recently acted as a consultant to Pulmatrix, Pulmocide, Biosergen, TFF Pharmaceuticals, Pfizer, Omega, Novacyt and Cipla. He sat on the DSMB for a SARS CoV2 vaccine trial. In the last 3 years, he has been paid for talks on behalf of Hikma, Gilead, BioRad, Basilea, Mylan and Pfizer. He is a longstanding member of the Infectious Disease Society of America Aspergillosis Guidelines group, the European Society for Clinical Microbiology and Infectious Diseases Aspergillosis Guidelines group and recently joined the One World Guideline for Aspergillosis.
Author contributions
Not applicable.
References
- 1.Pathadka S, Yan VKC, Neoh CF, et al. Global consumption trend of antifungal agents in humans from 2008 to 2018: data from 65 middle- and high-income countries. Drugs. 2022;82:1193–1205. doi: 10.1007/s40265-022-01751-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Denning DW, Lee JY, Hostetler JS, Pappas P, et al. NIAID Mycoses Study Group multicenter trial of oral itraconazole therapy of invasive aspergillosis. Am J Med. 1994;97:135–144. doi: 10.1016/0002-9343(94)90023-X. [DOI] [PubMed] [Google Scholar]
- 3.https://gaffi.org/itraconazole-voriconazole-and-natamycin-5-ophthalmic-preparation-proposed-as-essential-antifungal-medicines/. Accessed 19 Sept 2022.
- 4.https://gaffi.org/ruling-by-world-health-organisation-delights-doctors/. Accessed 19 Sept 2022.
- 5.Denning DW, Cadranel J, Beigelman-Aubry C, et al. Chronic pulmonary aspergillosis—rationale and clinical guidelines for diagnosis and management. Eur Resp J. 2016;47:45–68. doi: 10.1183/13993003.00583-2015. [DOI] [PubMed] [Google Scholar]
- 6.Zhou LH, Li RY, Denning DW, Zhu LP. Risk-based estimate of human fungal disease burden, China: old pathogen, new host, and new patterns. Emerg Infect Dis. 2020;26:2137–2147. doi: 10.3201/eid2609.200016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Denning DW, O’Driscoll BR, Powell G, et al. Randomized controlled trial of oral antifungal treatment for severe asthma with fungal sensitisation (SAFS), the FAST study. Am J Resp Crit Care Med. 2009;179:11–18. doi: 10.1164/rccm.200805-737OC. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal R, Dhooria S, Singh Sehgal I, et al. A randomized trial of itraconazole vs prednisolone in acute-stage allergic bronchopulmonary aspergillosis complicating asthma. Chest. 2018;153(3):656–664. doi: 10.1016/j.chest.2018.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Mirsadraee M, Dehghan S, Ghaffari S, Mirsadraee N. Long-term effect of antifungal therapy for the treatment of severe resistant asthma: an active comparator clinical trial. Curr Med Mycol. 2019;5(4):1–7. doi: 10.18502/cmm.5.4.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Denning DW, Kneale M, Sobel JD, Rautemaa-Richardson R. Global burden of recurrent vulvovaginal candidiasis. Lancet Infect Dis. 2018;18:e339–e347. doi: 10.1016/S1473-3099(18)30103-8. [DOI] [PubMed] [Google Scholar]
- 11.Adenis A, Nacher M, Hanf M, et al. HIV-associated histoplasmosis early mortality and incidence trends: from neglect to priority. PLoS Negl Trop Dis. 2014;8(8):e3100. doi: 10.1371/journal.pntd.0003100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mandengue CE, Ngandjio A, Atangana PJ. Histoplasmosis in HIV-infected persons, Yaoundé, Cameroon. Emerg Infect Dis. 2015;21(11):2094–2096. doi: 10.3201/eid2111.150278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oladele R, Ayanlowo OO, Richardson MD, Denning DW. Histoplasmosis in Africa: an emerging or a neglected disease? PLoS Negl Trop Dis. 2018;12:e0006046. doi: 10.1371/journal.pntd.0006046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ocansey BK, Otoo B, Asamoah I, et al. Cryptococcal and histoplasma antigen screening among people with HIV in Ghana and comparative analysis of OIDx histoplasma lateral flow assay and IMMY histoplasma enzyme immunoassay. Open Forum Infect Dis. 2022;9(7):ofac277. doi: 10.1093/ofid/ofac277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oladele RO, Osaigbovo II, Akanmu AS, Adekanmbi O, Ekeng B, Yahaya M, Alex-Wele M, Okolo M, Ayanbeku T, Unigwe U, Akase I, Dan-Jumbo A, Israelski D, Denning DW, Pasqualotto AC, Chiller T. Ascertaining the current prevalence of Histoplasmosis in Nigeria’s Advanced HIV disease population. Emerg Infect Dis. 2022;28:2261–9. [DOI] [PMC free article] [PubMed]
- 16.https://gaffi.org/media/country-fungal-disease-burdens/. Accessed 19 Sept 2022.
- 17.Majid I, Sheikh G, Kanth F, Hakak R. Relapse after oral terbinafine therapy in dermatophytosis: a clinical and mycological study. Indian J Dermatol. 2016;61(5):529–533. doi: 10.4103/0019-5154.190120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kneale M, Bartholomew JS, Davies E, Denning DW. Global access to antifungal therapy and its variable cost. J Antimicrob Chemother. 2016;71:3599–3606. doi: 10.1093/jac/dkw325. [DOI] [PubMed] [Google Scholar]
- 19.https://gaffi.org/antifungal-drug-maps/. Accessed 19 Sept 2022.
- 20.https://gaffi.org/antifungal-echinocandins-added-to-the-whos-essential-medicines-list/. Accessed 19 Sept 2022.