Abstract
Background The purpose of this study was to evaluate the clinical outcomes of thoracic and lumbar spinal tuberculosis treated with isolated posterior instrumentation without radical debridement.
Methods This study retrospectively analyzed 73 patients with thoracic and lumbar spinal tuberculosis who were treated using isolated posterior instrumentation without radical debridement in our hospital between January 2012 to December 2019. The patient group was composed of 42 men and 31 women with a mean age of 67.3 ± 8.6 years. The tuberculosis spine instability score (TSIS) was used to evaluate spine stability. All patients received chemotherapy for 18 months after surgery. The time of surgery, blood loss, visual analogue score (VAS), kyphosis angle, Oswestry disability index (ODI), erythrocyte sedimentation rate (ESR), Frankel grading, SF-36 scores, and local recurrence and complications were analyzed to evaluate the efficacy of isolated posterior instrumentation surgery in the treatment of thoracic and lumbar spinal tuberculosis.
Results All patients were followed up for 12 to 24 months (mean 14 ± 3.2 months). The mean surgical time was 1.2 ± 1.4 h (range, 1.2–1.6 h), and mean blood loss was 107 ± 18 mL. The postoperative symptoms were obviously relieved. The VAS, kyphosis angle, DI, and ESR decreased, respectively, from 8.24 ± 1.32, 19.82 ± 3.42, 46.25 ± 3.62, and 49.64 ± 17.61 to 1.12 ± 0.21, 7.14 ± 0.81, 20.17 ± 5.11, and 0.35 ± 1.13 at final follow-up. In comparison to preoperative values, SF-36 scores were significantly improved at final follow-up and the differences were statistically significant (p < 0.05). All patients achieved neurological recovery at the final follow-up. There were no recurrences or complications in any of the patients.
Conclusion Isolated posterior instrumentation without radical debridement is a suitable minor surgical trauma that offers a remarkable advantage of effective pain relief, improvement in neurological function and performance status, and no local recurrence for selected patients with thoracic and lumbar spinal tuberculosis.
Keywords: chemotherapy, debridement, spinal tuberculosis, surgery
Zusammenfassung
Hintergrund Ziel dieser Studie war es, die klinischen Ergebnisse der thorakalen und lumbalen spinalen Tuberkulose zu bewerten, die mit isolierter posteriorer Instrumentation ohne radikales Debridement behandelt wurden.
Methoden Diese Studie analysierte retrospektiv 73 Patienten mit thorakaler und lumbaler Spinaltuberkulose. Die Patienten wurden zwischen Januar 2012 und Dezember 2019 in unserem Krankenhaus mit isolierter posteriorer Instrumentation ohne radikales Debridement behandelt. Die Patientengruppe umfasste 42 Männer und 31 Frauen mit einem Durchschnittsalter von 67,3 ± 8,6 Jahren. Zur Bewertung der Wirbelsäulenstabilität wurde der Tuberkulose-Wirbelsäulen-Instabilitäts-Score (TSIS) verwendet. Alle Patienten erhielten nach der Operation 18 Monate lang eine Chemotherapie. Der Zeitpunkt der Operation, der Blutverlust, der visuelle Analogwert (VAS), der Kyphosewinkel, der Oswestry Disability Index (ODI), die Erythrozytensedimentationsrate (ESR), das Frankel-Grading, die SF-36-Scores sowie das lokale Rezidiv und die Komplikationen wurden analysiert, um die Wirksamkeit der isolierten posterioren Instrumentationschirurgie bei der Behandlung der thorakalen und lumbalen Wirbelsäulentuberkulose zu bewerten.
Ergebnisse Alle Patienten wurden 12 bis 24 Monate lang nachbeobachtet (Mittelwert 14 ± 3,2 Monate). Die durchschnittliche Operationszeit betrug 1,2 ± 1,4 h (Bereich, 1,2–1,6 h) und der durchschnittliche Blutverlust lag bei 107 ± 18 ml. Die postoperativen Symptome wurden offensichtlich gelindert; VAS, Kyphosewinkel, DI und ESR sanken von 8,24 ± 1,32, 19,82 ± 3,42, 46,25 ± 3,62 und 49,64 ± 17,61 auf 1,12 ± 0,21, 7,14 ± 0,81, 20,17 ± 5,11 und 0,35 ± 1,13 bei der abschließenden Untersuchung. Im Vergleich zu präoperativen Werten verbesserten sich die SF-36-Scores deutlich bei der abschließenden Nachbeobachtung und die Unterschiede waren statistisch signifikant (p < 0,05). Alle Patienten erreichten bei der letzten Nachuntersuchung eine neurologische Genesung. Bei keinem der Patienten traten Rezidive oder Komplikationen auf.
Schlussfolgerung Die isolierte posteriore Instrumentierung ohne radikales Debridement ist ein geeignetes kleines chirurgisches Trauma, das den bemerkenswerten Vorteil einer wirksamen Schmerzlinderung, einer Verbesserung der neurologischen Funktion und des Leistungsstatus bietet. Bei ausgewählten Patienten mit thorakaler und lumbaler Wirbelsäulentuberkulose traten keine Lokalrezidive oder geringere postoperative Komplikationen auf.
Schlüsselwörter: Chemotherapie, Schuldverschreibungen, Wirbelsäulentuberkulose, Chirurgie
Introduction
Tuberculosis of the spine is the most common and hazardous type of bone tuberculosis that gives rise to several challenges, such as kyphotic deformity, neurological deficits, and compression of the spinal cord, if diagnosis and treatment are delayed 1 2 . China has shown an increasing trend in tuberculosis incidence in recent years 3 4 .
The “Hong Kong operation,” which involves radical resection of the tuberculous-infected focus and bone grafting, was developed prior to the advent of modern imaging modalities 5 6 . With the advent of computerized tomography (CT) scanning and magnetic resonance imaging (MRI), early diagnosis of spinal tuberculosis has become possible 7 . In addition, more effective regimens of antituberculous chemotherapy have become available 8 . Therefore, the treatment strategy for this disease entity has been revised and has become more conservative in recent years 9 .
Modern transpedicular instrumentation can provide rigid stabilization of the thoracolumbar and lumbar spine with only short segments required 10 11 . The operation, which is performed via a posterior approach, is especially feasible for treatment of spinal tuberculosis, because the tuberculosis infection usually involves the anterior column. Its main shortcomings are that it does not allow for radical resection of the infectious focus and does not enable satisfactory interbody fusion. However, the authors showed that medical treatment alone can achieve complete or partial fusion at the bone defect in more than 88% of the patients with spinal tuberculosis 12 . This result encouraged us to introduce transpedicular instrumentation for the treatment of spinal tuberculosis in patients whose spine is biomechanically stable and chemotherapy might be inadequate. Thus, whether radical debridement is necessary for the treatment of thoracic and lumbar spinal tuberculosis in all cases should be questioned. Our team has found in previous studies that there are some special cases of spinal tuberculosis that do not require debridement, and only require posterior internal fixation, which can achieve better results 13 .
However, the study still has some details that need to be discussed. The purpose of this study was to
summarize the surgical indications;
analyze the patients’ postoperative quality of life;
elaborate on the advantages of this method.
We hope that other surgeons can get some different inspiration from this study to find a more effective treatment for spinal tuberculosis.
Data and Methods
Inclusion and exclusion criteria
Study design
This retrospective clinical trial was conducted at the Department of Orthopedic Surgery in the Second Hospital of Anhui Medical University from January 2012 to December 2019. It was approved by the ethics committee of our hospital. All patients provided written informed consent for the study. Seventy-three patients were enrolled and isolated posterior instrumentation surgery for the treatment of thoracic and lumbar spinal tuberculosis was conducted. The researchers who enrolled the participants and analyzed the data did not take part in patient care.
Inclusion criteria
The inclusion criteria for this study were patients with
spinal tuberculosis involved in one adjacent segment located at the thoracic, thoracolumbar, or lumbar segment who underwent posterior fixation alone without radical debridement;
Frankel grading of grade D and E;
spinal biomechanical instability (TSIS score 14 > 10 point);
severe mechanical back pain caused by spinal instability after an antitubercular chemotherapy program was performed > 6 weeks before operation.
Exclusion criteria
The exclusion criteria for this study were patients
with multiple spinal tuberculosis;
with a widespread abscess anterior to the vertebral body involving multi-segments;
with active tuberculosis;
undergoing anterior surgery or anterior combined posterior approach surgery;
unwilling or unable to undergo MRI.
The same preoperative treatments included improvement in nutritional status, painkillers, and the limitation of lower back activities.
General information
From January 2012 to December 2019, 73 consecutive patients with a diagnosis of spinal tuberculosis underwent isolated posterior instrumentation without radical debridement at our tertiary care facility. There were 42 men and 31 women, with a mean age of 67.3 ± 8.6 years (range, 56–77 years). The diagnosis was first made based on medical history, clinical examination, laboratory results, radiologic imaging, and drug response. All included patients were confirmed with spinal tuberculosis by bacterial culture and/or histopathology or gene chip and underwent surgical treatment. All patients underwent isolated posterior instrumentation without radical debridement and received chemotherapy for 18 months after surgery.
Surgical procedures
After the administration of general endotracheal anesthesia, the patients were placed in a prone position, and based on preoperative presentation and imaging, the objective segments were located using fluoroscopy. The objective segments were exposed via the midline posterior approach. Pedicle screws were placed in the objective vertebral body above and below the involved vertebral body bilaterally. The pedicle screws were connected by two rods on both sides independently. A biopsy sample of the granulation tissue was obtained via a transpedicular route or by a limited laminectomy, depending on the location of the infectious focus. When accessible, the abscess was drained during the operation. However, extensive laminectomy or radical debridement was not attempted. The biopsy specimens were sent for pathological examination and for culture for mycobacterium tuberculosis.
Postoperative treatment
The drainage tube was removed when the drainage volume in the surgical area was < 50 mL/d. Four-drug combination chemotherapy regimen (isoniazid 0.3 g/d, rifampin 0.45 g/d, ethambutol 0.75 g/d, pyrazinamide 0.75 g/d) was continued for 18 months. The patients, who wore Taylor braces were encouraged to move around on the 7th postoperative day.
Evaluation of clinical outcome
The amount of operation bleeding was recorded. The patients were followed up once a month for the first 3 months after surgery, once every 3 months for the next 9 months within the first year after surgery, and once every 6 months within the second year after surgery. The imaging manifestations were used to evaluate whether the lesion was healed or recurred, and whether the graft was fused. The visual analogue score (VAS) of back pain, kyphosis angle, Oswestry disability index (ODI), erythrocyte sedimentation rate (ESR), Frankel grade, and SF-36 score were recorded for assessing the clinical efficacy. The definitive explanation of the measurement methods are follows:
Visual analogue score
The VAS is a self-reported scale consisting of a horizontal line (10 cm long) with anchor points of “no pain” and “worst possible pain.” The patient was asked to put a mark on the line that best described his pain severity.
Kyphotic (Cobb) angle
The angle is formed by the line of the upper endplate and that of the lower endplate of the end vertebras, which is also called the posterior convex angle. The end vertebras refer to the upper and lower vertebras with maximum inclination of the kyphosis.
Frankel grade
The Frankel grade classification provides an assessment of spinal cord function and is used as a tool in spinal cord injury as follows:
Grade A: Complete neurological injury – No motor or sensory function detected below the level of the lesion
Grade B: Preserved sensation only – No motor function detected below the level of the lesion, some sensory function below the level of the lesion preserved
Grade C: Preserved motor, nonfunctional – Some voluntary motor function preserved below the level of the lesion but too weak to serve any useful purpose, sensation may or may not be preserved
Grade D: Preserved motor, functional – Functionally useful voluntary motor function below the level of the injury is preserved
Grade E: Normal motor function – Normal motor and sensory function below the level of the lesion, abnormal reflexes may persist
Tuberculosis spine instability score
TSIS is a comprehensive scoring system used to diagnose instability in the tuberculosis spine and comprises age, location of the lesion, pain, degree of kyphosis, vertebral body loss, involvement of posterior spinal elements, multifocal contiguous disease, and presence of an intervertebral or para-spinal abscess. The TSIS score is calculated by adding up individual scores from each criterion. The minimum and maximum possible scores are 0 and 21, respectively. Scores less than 7 indicate a stable spine, between 7 to 10 denote “impending instability,” and scores greater than 10 denote unstable spine and the possible need for surgical fixation.
Oswestry disability index
The ODI consists of 10 items on the degree of severity to which back (or leg) trouble has affected the ability to manage everyday life. The 10 sections cover pain and daily function (including pain intensity, personal hygiene, lifting, walking, sitting, standing, sleeping, sexual activity, social activity, and traveling). Each item is rated on 6-point scale (0–5); the higher score means the higher level of disability related to back pain. The present study used the traditional Chinese version of the ODI 2.1 15 .
SF-36
The SF-36 is a set of generic, coherent, and easily administered quality-of-life measures developed by the RAND Corporation. These measures rely upon patient self-reporting and are now widely used by managed care organizations and by Medicare for routine monitoring and assessment of care outcomes in adult patients. Patients completed handwritten responses to this survey. Assistance was available if needed. The clinical significance of the SF-36 is that it allows for quantitative analysis.
Statistical analysis
All continuous data are presented as the mean ± SD. All data were statistically analyzed using SPSS 22.0 (IBM Cop., Armonk, NY, USA). Pre- and final follow-up comparisons of VAS scores, kyphosis angle, ODI, ESR, and SF-36 scores were performed by the paired samples t-test. Values of p < 0.05 were considered to be significantly different.
Results
General data
The baseline characteristics of 73 patients are presented in Table 1 .
Table 1 Demographic and clinical characteristics of the sample (n = 73).
| Characteristics | Statistics |
|
a
Visual analog scale (VAS) ≥ 7
b Associated leg symptoms included leg radiation pain, leg numbness, intermittent claudication, and neurological deficits TB = tuberculosis | |
| Age, mean (SD), years | 67.3 (8.6) |
| Female, N (%) | 31 (42.5%) |
| Involved segment | |
| Thoracic segment, N (%) | 19 (26.0%) |
| Thoracolumbar segment, N (%) | 26 (35.6%) |
| Lumbar segment, N (%) | 28 (38.4%) |
| Associated leg symptoms a, b , N (%) | 24 (32.9%) |
| Past operative history, N (%) | 9 (12.3%) |
| Severe back pain a , N (%) | 73 (100%) |
| Medical comorbidities, N (%) | 30 (41.1%) |
| Diabetes, N (%) | 18 (24.7%) |
| Pulmonary TB, N (%) | 12 (16.4%) |
| Diabetes and pulmonary TB, N (%) | 7 (9.6%) |
Operation condition
The average operation time was 1.2 ± 1.4 h (range, 1.2–1.6 h). Average blood loss was 107 ± 18 mL (range, 80–130 mL).
Clinical efficacy
Patients were followed up for 12 to 24 months with the average of 14 ± 3.2 months.
Visual analogue score, kyphosis angle, and erythrocyte sedimentation rate
The value of VAS was 8.24 ± 1.32 preoperatively and it significantly decreased to 1.12 ± 0.21 (p < 0.05) at final fellow-up, indicating that the method can significantly reduce pain in patients. Compared to the preoperative kyphosis angle, ODI and ESR, the kyphosis angle improved while ODI and ESR were significantly depressed (p < 0.05) at final fellow-up, which showed that isolated posterior instrumentation without radical debridement surgery significantly corrects kyphosis, and markedly improved the therapeutic effects ( Table 2 ).
Table 2 VAS, kyphosis angle, ODI, and ESR of comparison between preoperation and final follow-up (mean ± SD).
| VAS | Kyphosis angle | ODI | ESR | |
| ESR = erythrocyte sedimentation rate; ODI = Oswestry disability index; VAS = visual analogue score | ||||
| Preoperation | 8.24 ± 1.32 | 19.82± 3.42 | 46.25 ± 3.62 | 49.64 ± 17.61 |
| Final follow-up | 1.12 ± 0.21 | 7.14 ± 0.81 | 20.17 ± 5.11 | 0.35 ± 1.13 |
| P value | 0.00 | 0.00 | 0.00 | 0.00 |
Frankel grade
Twenty-four patients were preoperatively classified as Frankel grade D and 49 as Frankel grade E. At final follow-up, all patients showed normal neurological function, indicating that the isolated posterior instrumentation without debridement surgery can significantly improve spinal cord function.
SF-36
Compared to the preoperative SF-36, at final follow-up, the SF-36 scores were found to be improved for all individual scales, and most pronounced for the physical role ( Table 3 ).
Table 3 SF-36 scores of comparison between preoperation and final follow-up (mean ± SD).
| Preoperation | Final follow-up | P value | |
| BP = bodily pain; GH = general health; MH = mental health; PF = physical functioning; RE = role – emotional; RP = role – physical; SF = social functioning; VT = vitality | |||
| RF | 64.25 ± 4.32 | 82.76 ± 8.22 | 0.00 |
| RP | 14.63 ± 8.95 | 89.13 ± 13.22 | 0.00 |
| BP | 43.77 ± 7.33 | 86.03 ± 6.71 | 0.00 |
| GH | 26.37 ± 11.32 | 82.36 ± 9.81 | 0.00 |
| VT | 45.52 ± 10.91 | 88.47 ± 7.34 | 0.00 |
| SF | 27.82 ± 8.92 | 79.45 ± 5.62 | 0.00 |
| RE | 35.76 ± 13.43 | 88.93 ± 14.27 | 0.00 |
| MH | 30.23 ± 7.91 | 83.84 ± 9.78 | 0.00 |
Postoperative complications
No autologous bone graft was performed in the 73 patients. However, it was interesting to find a spontaneous bony fusion between vertebral bodies in 35 cases at final follow-up. There was no local recurrence or serious complications observed in this study during the follow-up evaluation ( Fig. 1 , Fig. 2 ).
Fig. 1.
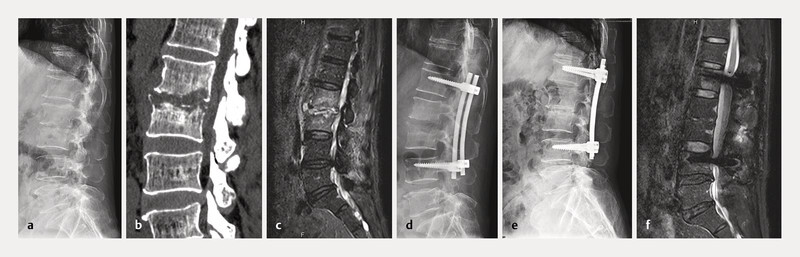
A 68-year-old man patient with L2, L3 tuberculosis. The instrumentation was performed from the posterior approach without radical debriding of the lesion. a,b Preoperative plain radiograph and 3D CT demonstrating bone erosion at the inferior portion of the L2 and superior portion of the L3 vertebral bodies. c Preoperative T2-weighted MRI revealing spinal cord compression at the level of L2 and L3. Areas of high signal intensity can be seen at the involved bodies, abscess, and the paravertebral soft tissue mass. d Plain radiograph 1 week postoperatively. Only long-segment posterior instrumentation was performed without extensive decompressive surgery. e Postoperative plain radiograph obtained at the 20-month follow-up demonstrating that the transpedicular instrumentation has not loosened, and spontaneous bone fusion was observed in the L2 and L3 vertebral bodies. f Postoperative T2-weighted MRI at the 20-month follow-up examination revealing almost complete disappearance of the paravertebral soft tissue mass and abscess, and normalization of the signal intensity of the L2 and L3 vertebral bodies. Spontaneous bone fusion was observed in the L2 and L3 vertebral bodies.
Fig. 2.

A 71-year-old female patient with T12, L1 tuberculosis. Isolated posterior instrumentation for the spinal tuberculosis without radical debridement. a,b Preoperative plain radiograph and 3D CT demonstrating bone erosion at the inferior portion of the T12 and superior portion of L1 vertebral bodies. c Preoperative T2-weighted MRI revealing areas of high signal intensity can be seen at the involved bodies, abscess, and the paravertebral soft tissue mass. d Plain radiograph 1 week postoperatively. Only long-segment posterior instrumentation was performed without extensive decompressive surgery. e Postoperative 3D CT obtained at the 17-month follow-up demonstrating that the transpedicular instrumentation has not loosened. f Postoperative T2-weighted MRI at the 17-month follow-up examination revealing almost complete disappearance of the paravertebral soft tissue mass and abscess, and normalization of the signal intensity of the L2 and L3 vertebral bodies. However, absence of trabeculae inside the solid mass implies that there is no strong evidence of fusion in the L2 and L3 vertebral bodies.
Discussion
Despite chemotherapy alone being efficacious for spinal tuberculosis, even when myelopathy or obvious bone destruction is present, a recent study in India by Bhosale found that drug resistance in spinal tuberculosis was found to be 28.6% 16 . Of these, multidrug resistant was found in 16.2%, preextensive drug resistance in 20.9%, and extensive drug resistance in 9.3% patients 12 16 . In addition, there are many spinal tuberculosis patients with progressive neurologic deficit, progressive increase in spinal deformity (coronal or sagittal), severe pain due to spinal instability, and uncertain diagnosis. The “Hong Kong operation,” which involves radical resection of the tuberculous-infected focus and bone grafting, was accepted, in general, for the treatment of spinal tuberculosis a long time ago 5 6 . In recently published papers, authors have tended to emphasize the importance of tailoring the management options to the individual needs of the patients with spinal tuberculosis. Yin et al. 17 have treated patients with spinal tuberculosis according to the number of damaged vertebral bodies. In their series, aggressive debridement and fusion were performed in patients in whom the damaged vertebral bodies were more than three. Zhang and associates 12 have suggested that neurological function as well as bone involvement should be carefully evaluated before making surgery-related decisions for the treatment of patients with spinal tuberculosis. They recommend that patients with ASIA grade A, B, or C lesions undergo rapid decompressive surgery, while those with grade D or E lesions may be treated expectantly with chemotherapy alone.
Because the patients had Frankel grade D or E in our series and had no severe bone destruction, theoretically, they could be expected to have had good treatment outcomes by undergoing antituberculous chemotherapy alone. However, this conservative method cannot prevent the possible progression of kyphotic deformity and the severe mechanical back pain caused by spinal instability. Based on analysis of the literature, a rigid stabilization system provides the best solution, not only to prevent kyphosis but also to achieve relief of pain due to spinal instability 18 19 20 .
In this study, isolated posterior instrumentation without radical debridement can be used in the management of Pott’s disease, as we have observed that the surgery provided a visible resolution of severe back pain, neurologic deficits or deformity, and poor performance status. The value of VAS was 8.24 ± 1.32 preoperatively and it significantly decreased to 1.12 ± 0.21 (p < 0.05) at the final follow-up. The ODI was 46.25 ± 3.62 preoperatively and it decreased to 20.17 ± 5.11 (p < 0.05). The ESR was 49.64 ± 17.61 preoperatively and it decreased to 0.35 ± 1.13 (p < 0.05). There was a minor loss of kyphosis correction at the final follow-up. The neurological function of 24 patients was recovered at the final follow-up. In addition to providing rapid relief from instability catch, the instrumentation also preserved spinal alignment and stabilized the involved segment in these patients. It was interesting to find a spontaneous bony fusion between vertebral bodies in 35 cases at final follow-up. There were no local recurrences and serious complications observed in this study during the follow-up evaluation. The quality of life for all patients significantly improved compared to that preoperatively. The advantages of this method include the following 18 :
Single-stage operation.
Relatively low cost compared to a double-stage operation.
Better correction and maintenance of correction using an implant.
Early patient mobilization with a simple brace.
Complications peculiar to anterior approaches to the spine can be avoided.
The principal aims of the surgery method are to correct and prevent kyphosis by rigid stabilization in a single-stage operation, confirm the diagnosis by biopsy, and mobilize the patient early.
We suggest the indications of this surgery method include:
patients with spinal tuberculosis involved in one adjacent segment and there is no flow abscess formation;
vertebral destruction less than ½;
Frankel grading grade D or E;
the patients’ general condition is poor and cannot tolerate prolonged anesthesia;
spinal biomechanical instability (TSIS score > 10 point);
severe mechanical back pain caused by spinal instability.
Limitations
There are a few limitations to this study. First, this was a retrospective study with a small number of patients, which limits the power of the results. Second, the follow-up period in this study was limited to middle-term neurological and radiological outcomes. Therefore, further prospective studies with long-term follow-up in a larger number of patients is required.
Conclusion
Surgical treatment in appropriate patients with thoracic and lumbar spinal tuberculosis may result in a pain-free comfortable status. In the present study, palliative surgery for thoracic and lumbar spinal tuberculosis using isolated posterior instrumentation without radical debridement can reduce operative time, blood loss, surgical trauma, and complications and achieve good clinical outcomes in terms of pain palliation, neurological function, and performance status and result in no local recurrence. Accordingly, we support the use of isolated posterior instrumentation without debridement for the treatment of select patients.
Funding
The study was supported by the Clinical Research Cultivation Project of the Second Affiliated Hospital of Anhui Medical University (no.2020LCYB07), supported by the Hefei Municipal Natural Science Foundation (no.2021010) and Natural Science Foundation of Anhui Province Universities (no. KJ2020A0182).
Footnotes
Conflict of Interest The authors declare that they have no conflict of interest.
References
- 1.Khanna K, Sabharwal S. Spinal tuberculosis: a comprehensive review for the modern spine surgeon. Spine J. 2019;19:1858–1870. doi: 10.1016/j.spinee.2019.05.002. [DOI] [PubMed] [Google Scholar]
- 2.Sun G, Wang Q, Liang Q et al. Clinical efficacy and safety of ultra-short-course chemotherapy in treatment of spinal tuberculosis after complete debridement: an observational study. J Int Med Res. 2021;49:3.00060520967611E14. doi: 10.1177/0300060520967611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhou Y, Li W, Liu J et al. Comparison of single posterior debridement, bone grafting and instrumentation with single-stage anterior debridement, bone grafting and posterior instrumentation in the treatment of thoracic and thoracolumbar spinal tuberculosis. BMC Surg. 2018;18:71. doi: 10.1186/s12893-018-0405-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liu Z, Zhang P, Zeng H et al. A comparative study of single-stage transpedicular debridement, fusion, and posterior long-segment versus short-segment fixation for the treatment of thoracolumbar spinal tuberculosis in adults: minimum five year follow-up outcomes. Int Orthop. 2018;42:1883–1890. doi: 10.1007/s00264-018-3807-0. [DOI] [PubMed] [Google Scholar]
- 5.Hodgson AR, Stock FE. Anterior spine fusion for the treatment of tuberculosis of the spine. J Bone Joint Surg (Am) 1960;42:295–310. [Google Scholar]
- 6.Hodgson AR, Yau ACMC, Kwon JS. A clinical study of 100 consecutive cases of Pott’s paraplegia. Clin Orthop. 1964;36:128–150. [Google Scholar]
- 7.Sinan T, Al-Khawari H, Ismail M et al. Spinal tuberculosis: CT and MRI feature. Ann Saudi Med. 2004;24:437–441. doi: 10.5144/0256-4947.2004.437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajasekaran S, Khandelwal G. Drug therapy in spinal tuberculosis. Eur Spine J. 2013;22 04:587–593. doi: 10.1007/s00586-012-2337-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang B, Wang Y, Hao D. Current Study of Medicinal Chemistry for Treating Spinal Tuberculosis. Curr Med Chem. 2021;28:5201–5212. doi: 10.2174/0929867328666201222125225. [DOI] [PubMed] [Google Scholar]
- 10.Yue JJ, Sossan A, Selgrath C et al. The treatment of unstable thoracic spine fractures with transpedicular screw instrumentation: a 3-year consecutive series. Spine (Phila Pa 1976) 2002;27:2782–2787. doi: 10.1097/00007632-200212150-00008. [DOI] [PubMed] [Google Scholar]
- 11.Sapkas G, Kateros K, Papadakis SA et al. Treatment of unstable thoracolumbar burst fractures by indirect reduction and posterior stabilization: short-segment versus long-segment stabilization. Open Orthop J. 2010;4:7–13. doi: 10.2174/1874325001004010007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zhang Z, Luo F, Zhou Q et al. The outcomes of chemotherapy only treatment on mild spinal tuberculosis. J Orthop Surg Res. 2016;11:49. doi: 10.1186/s13018-016-0385-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qian J, Rijiepu A, Zhu B et al. Outcomes of radical debridement versus no debridement for the treatment of thoracic and lumbar spinal tuberculosis. Int Orthop. 2016;40:2081–2088. doi: 10.1007/s00264-016-3234-z. [DOI] [PubMed] [Google Scholar]
- 14.Ahuja K, Kandwal P, Ifthekar S et al. Development of Tuberculosis Spine Instability Score (TSIS): An Evidence-Based and Expert Consensus-Based Content Validation Study Among Spine Surgeons. Spine (Phila Pa 1976) 2022;47:242–251. doi: 10.1097/BRS.0000000000004173. [DOI] [PubMed] [Google Scholar]
- 15.Lue YJ, Hsieh CL, Huang MH et al. Development of a Chinese version of the Oswestry Disability Index version 2.1. Spine (Phila Pa 1976) 2008;33:2354–2360. doi: 10.1097/BRS.0b013e31818018d8. [DOI] [PubMed] [Google Scholar]
- 16.Bhosale S, Prabhakar A, Srivastava S et al. Pattern of Drug Resistance in Primary Spinal Tuberculosis: A Single-Center Study From India. Global Spine J. 2021;11:1070–1075. doi: 10.1177/2192568220941445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yin XH, Liu SH, Li JS et al. The role of costotransverse radical debridement, fusion and postural drainage in the surgical treatment of multisegmental thoracic spinal tuberculosis: a minimum 5-year follow-up. Eur Spine J. 2016;25:1047–1055. doi: 10.1007/s00586-015-4283-5. [DOI] [PubMed] [Google Scholar]
- 18.Güven O, Kumano K, Yalçin S et al. A single stage posterior approach and rigid fixation for preventing kyphosis in the treatment of spinal tuberculosis. Spine (Phila Pa 1976) 1994;19:1039–1043. doi: 10.1097/00007632-199405000-00007. [DOI] [PubMed] [Google Scholar]
- 19.Chen YC, Chang MC, Wang ST et al. One-stage posterior surgery for treatment of advanced spinal tuberculosis. J Chin Med Assoc. 2003;66:411–417. [PubMed] [Google Scholar]
- 20.Kumar MN, Joseph B, Manur R. Isolated posterior instrumentation for selected cases of thoraco-lumbar spinal tuberculosis without anterior instrumentation and without anterior or posterior bone grafting. Eur Spine J. 2013;22:624–632. doi: 10.1007/s00586-012-2528-0. [DOI] [PMC free article] [PubMed] [Google Scholar]


