Abstract
Background Hypertension, persistent high blood pressures (HBP) leading to chronic physiologic changes, is a common condition that is a major predictor of heart attacks, strokes, and other conditions. Despite strong evidence, care teams and patients are inconsistently adherent to HBP guideline recommendations. Patient-facing clinical decision support (CDS) could help improve recommendation adherence but must also be acceptable to clinicians and patients.
Objective This study aimed to partly address the challenge of developing a patient-facing CDS application, we sought to understand provider variations and rationales related to HBP guideline recommendations and perceptions regarding patient role and use of digital tools.
Methods We engaged hypertension experts and primary care respondents to iteratively develop and implement a pilot survey and a final survey which presented five clinical cases that queried clinicians' attitudes related to actions; variations; prioritization; patient input; importance; and barriers for HBP diagnosis, monitoring, and treatment. Analysis of Likert's scale scores was descriptive with content analysis for free-text answers.
Results Fifteen hypertension experts and 14 providers took the pilot and final version of the surveys, respectively. The majority (>80%) of providers felt the recommendations were important, yet found them difficult to follow-up to 90% of the time. Perceptions of relative amounts of patient input and patient work for effective HBP management ranged from 22 to 100%. Stated reasons for variation included adverse effects of treatment, patient comorbidities, shared decision-making, and health care cost and access issues. Providers were generally positive toward patient use of electronic CDS applications but worried about access to health care, nuance of recommendations, and patient understanding of the tools.
Conclusion At baseline, provider management of HBP is heterogeneous. Providers were accepting of patient-facing CDS but reported preferences for that CDS to capture the complexity and nuance of guideline recommendations.
Keywords: hypertension, decision support systems, clinical, surveys and questionnaires, practice guideline, fast healthcare interoperable resources
Background and Significance
High blood pressure (HBP) is a common issue and hypertension, persistent high blood pressures leading to chronic physiologic changes, is a common condition among adults in the United States that, when uncontrolled, increases the risks of heart disease and stroke. 1 Medications can treat HBP but also have adverse events like hypotension and electrolyte derangements. 2 3 HBP also can be reduced through lifestyle and behavioral changes such as diet, exercise, reducing stress, and avoiding alcohol and smoking, yet these changes require substantial effort. 4 Hypertension guidelines vary, reflecting risks and benefits in variable ways. 5 For example, goals for hypertension control vary from 150/90 to 120/80 across guidelines depending on their synthesis of the evidence for key populations, such as from the SPRINT trial. 6 From diagnosis to prescription, hypertension treatment is a complex interplay among provider intent, patient capacity, and best available data and knowledge. 7
Clinical decision support (CDS) can provide the means to implement recommendations from hypertension guidelines but must consider variabilities in guidelines, clinical workflows, patient and provider preferences, and their attitudes and beliefs. 8 Past hypertension CDS efforts have had promising but mixed results and few are in current use, potentially due to these complexities. 9 CDS trials that involved multidisciplinary interventions yielded positive results and indicated hypertension CDS may have to balance needs and preferences to be effective. 10 11 12 13 The Kaiser Permanente reports control rates of >80% with multifactorial approaches including CDS. 14 These efforts, however, are not easily implemented in different systems; this is especially due to lack of interoperability between clinical information systems, CDS logic, and data. 15 16
As part of research funded by Agency for Healthcare Research and Quality, our team has explored the way eight separate guidelines for hypertension can be translated into CDS recommendations; initially, we took 71 recommendations covering more than 36 domains, transformed them into machine-interpretable logic, 17 18 19 and determined the adequacy of standard EHR data to assess them. 20 We created a content implementation guide (see Supplementary Figs. S1 and S2 [available in the online version] for details) 21 ; however, the implementation into an actual application requires consideration of many aspects such as usability, usefulness, adaptability, and, especially, the five rights of CDS, that is, right information to the right person in the right format to the right channel at the right time. 22 Given the complex, shared decision-making nature of hypertension, we sought to understand when the patient may be the right person to receive the alerts through the creation of a series of stakeholder surveys to implement the recommendations into an FHIR hypertension CDS application. This survey focused on the provider perspective, both hypertension experts and primary care providers, highlighting the variation in guidelines through different cases, their current practice preferences, and the potential approach when engaging patients with the CDS. Poorly designed CDS applications may exacerbate the variability and worsen clinical care and increase fatigue, while carefully designed CDS can aid in shared decision-making. 23
Objectives
Our objective for this paper was to understand the perception of hypertension experts and primary care providers in the role of the patient in responding to hypertension guideline recommendations to create a patient-facing clinical decision support tool.
Methods
We iteratively created a unique survey that queried primary care providers and hypertension specialists about their attitudes toward clinical practice guidelines for hypertension and patient-facing CDS.
For the Human Subject Research Approval, the Oregon Health and Science University Institutional Review Board approved this study (approval number: STUDY00020522).
Survey Design
We used an iterative development process that focused on the constructs of high blood pressure guideline recommendations, variation, importance, challenges, and patient input and effort. We first searched the literature for similar surveys: we found work by Oliveria et al, 24 25 Koopman et al, 26 Kerr et al, 27 Kim et al, 28 Turer et al, 29 and several studies that optimized their CDS implementation approach through surveys. 30 31 32 33 We used the assessment of barriers to control by Kerr et al—clinical uncertainty, prioritization of BP, and organizational/system issues—and the five rights to drive the survey design. For demographics, shared decision-making, and use of hypertension tools, we used questions from these other surveys to assess these concepts. 34 However, since no surveys covered the most recent hypertension guidelines, we developed novel questions informed by the synthesis of hypertension guidelines into 71 recommendations described by Alper et al 5 . We organized the questions into five use cases that were meant to elicit provider preferences for diagnostic, monitoring, and treatment approaches to hypertension management with a focus on the five rights—especially the best person, channel, and time—and on variability in the guidelines, and barriers in following recommendations. Table 1 highlights the cases and their objectives.
Table 1. HBP case definitions and objectives.
| Case | Description | Objective |
|---|---|---|
| Case 1: initial diagnosis and screening | Patient with no recorded history of hypertension, nonsmoker, BMI of 31 kg/m 2 , prediabetic | Identify approaches to initial screening and diagnosis. Would participants diagnose with hypertension based on presented information or would they order additional screenings? |
| Case 2: nonpharmacologic interventions | Patient with untreated hypertension and no comorbidities | Identify approaches to prescribing non-pharmacologic interventions. Which lifestyle changes (diet, physical activity, etc.) would participants prioritize for patients? |
| Case 3: initial pharmacology for hypertension | Patient with untreated hypertension and no comorbidities | Identify approaches to initial pharmacology. Which antihypertensive medication(s) would participants prescribe for first-line therapy? |
| Case 4: pharmacology for moderate hypertension | Patient with hypertension, stage-3 CKD. Currently on low-sodium diet for hypertension | Identify approaches to initial pharmacology if patient had comorbidity. Which antihypertensive medication(s) would participants prescribe for first-line therapy? |
| Case 5: pharmacology for severe hypertension | Patient with severe hypertension, stage 4 CKD, controlled DM, prior left MCA ischemic stroke, currently taking 50 mg atenolol for hypertension | Identify approaches to modified pharmacology in severe case of hypertension. Which antihypertensive medication(s) would participants prescribe? Would they discontinue current treatment? |
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; DM, diabetes mellitus; MCA, middle cerebral artery.
The survey also asked providers to record their preferred hypertension care recommendations from four of the eight extant guidelines, eliminating those from outside the United States as follows: (1) Eighth Joint National Committee (JNC 8) 35 ; (2) American College of Cardiology/American Heart Association (ACC/AHA) 36 ; (3) American College of Physicians (ACP/AAFP) 2 ; and (4) U.S. Department of Veterans Affairs (VA). 37 We presented providers with these cases and asked them to record their preferences for various therapeutic interventions, select one of the guideline-based recommendations from a list, and rate their selections by importance, frequency of use, difficulty, patient input required, and patient work required. Ratings were on a 7-point scale with 7 as the highest, 1 as the lowest, and 4 as neutral. The survey also asked participants to provide free text answers as to why they made the decisions they did for each use case, as well as share their overall impressions of CDS and shared decision-making in hypertension care.
As shown in Fig. 1 , we first fielded a pilot version of the survey to a convenience sample of “hypertension experts” who (1) had completed the American Hypertension Specialist Certification Program (AHSCP) 38 and (2) had public contact information ( n = 280) to assess the understandability of the questions and the reliability of the responses (see Supplementary Appendix A “Draft Survey,” available in the online version). The pilot survey includes 90 questions within six sections with 14–18 questions per section. The pilot survey led to a final version of the survey with only 60 questions which we then administered to primary care providers. Results from both the pilot and final surveys guided our adaptation of the CDS application.
Fig. 1.
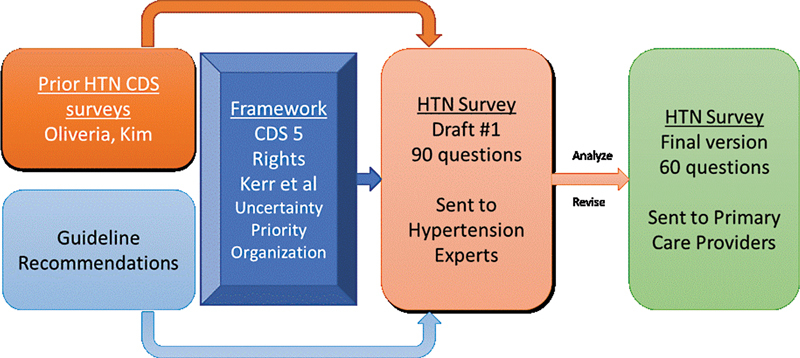
Selected action taken and related recommendation for each HBP case. CDS, clinical decision support; HBP, high blood pressure; HTN, hypertension.
Recruitment
We recruited hypertension experts who were nephrologists, cardiologists, internists, and family medicine physicians for the pilot survey from the AHSCP; and then between June 2020 and December 2020, we fielded the final survey to primary care providers from a convenience sample of 120 providers from 17 different primary care clinics. 39 Both groups received an e-mail invitation that included a consent form and a link to the online survey. Participants received $50.00 for completing the survey.
Data Analysis
Primary analysis summarized provider and clinic characteristics, and generated descriptive statistics for aggregates of each of the five cases. We generated binary values for questions with a 7-point scale by selecting answers that were scored five or higher. Two researchers (J.R. and C.D.) qualitatively reviewed all text answers and generated preliminary themes which were vetted and finalized by the research team.
Results
In all, 15 hypertension experts responded to the pilot survey (see Supplementary Appendix A : “Draft Survey,” available in the online version); significant revisions were made based on their feedback. We shortened and clarified the cases, provided clearer text from the recommendations, and expanded options where they suggested other treatments. The pilot questions related to screening, monitoring, and challenges were retained and are presented with the final survey. For the final survey ( Supplementary Appendix B : “Main Survey,” available in the online version), 14 primary care providers responded: 10 physicians and 4 advanced practice providers (two physician assistants and two nurse practitioners). A slight majority worked in urban practices ( n = 8, 57%) versus rural practices ( n = 6, 43%). Nine of the 14 (64%) had been practicing medicine for 5 years or longer.
All the experts and 8 out of 14 primary care respondents were very or extremely familiar with the process to develop guidelines. Half of the primary care providers (50%) reported their clinics primarily followed the Eighth Joint National Committee (JNC 8) guideline, while four (28%) used the ACC/AHA guideline, one (7%) followed the ACP/AAFP guideline, and two respondents (14%) were unsure. Experts were more likely to follow ACC/AHA guidelines. We next report the results for each of the five use cases. Fig. 2 summarizes the actions taken for each case.
Fig. 2.
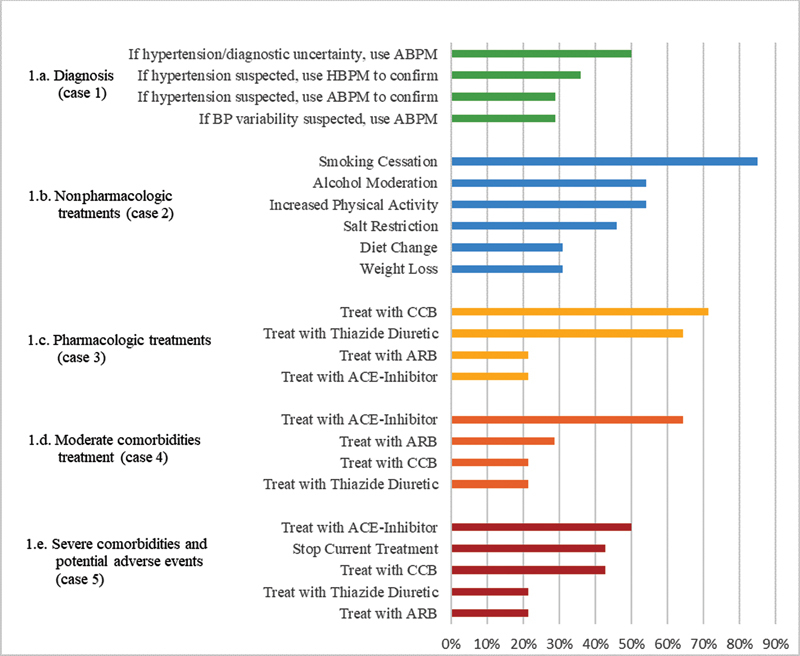
Self-rated perceptions of key recommendation areas ( n = 14). Percentage selecting one of the top 3 categories on a 7-point Likert scale. ABPM, ambulatory blood pressure monitoring; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker; CCB, calcium channel blocker; HBPM, home blood pressure monitoring.
Diagnosis and Monitoring (Case 1)
Case 1 presented recommendations for diagnosis and monitoring ( Table 2 ); here, the guidelines suggest home or ambulatory blood pressure monitoring. Of the primary care respondents, only one-third suggested that the patient should use home monitoring of blood pressure (HMBP) and half of them recommended ambulatory blood pressure monitoring (ABPM). In contrast, 100% of hypertension experts recommended monitoring, predominantly recommending ABPM (73%).
Table 2. Diagnosis and monitoring (case 1).
| Patient description | Blood pressure as mean SBP/DBP | Relevant history, medications, and/or labs |
|---|---|---|
| A 35-year-old Caucasian woman with no recorded history of hypertension | 132/83 mm/Hg | She is a nonsmoker, has a BMI of 31, and has prediabetes on her problem list |
Abbreviations: BMI, Body Mass Index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Nonpharmacologic Treatment (Case 2)
Case 2 presented nonpharmacologic treatment options ( Table 3 ); all options were potentially valid selections. Participants were asked to rank nonpharmacologic recommendations in order of priority for the patient. Of the primary care providers responding, a majority prioritized recommendations for smoking cessation (>80%), moderating alcohol consumption (>50%), and increasing physical activity (>50%) in their top three priorities, whereas less than half prioritized salt restriction, weight loss, and dietary changes.
Table 3. Non-pharmacologic treatment (case 2).
| Patient description | Blood pressure as mean SBP/DBP | Relevant history, medications, and/or labs |
|---|---|---|
| A 40-year-old Asian patient with hypertension presents to the clinic | 144/87 mm/Hg | This patient is not currently on antihypertensive medications. Relevant history is BMI of 31 kg/m 2 , pulse of 90 bpm, consuming two to three drinks per day, and current smoker |
Abbreviations: BMI, body mass index; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Pharmacologic Treatment: Cases 3–5 (in Order of Increasing Complexity)
Case 3 presented a patient with moderate severity hypertension ( Table 4 ); most guidelines recommend several medications as potential initial options. However, 71% of primary care providers recommended treating with a calcium channel blocker (CCB). Eighty-six percent of primary care respondents ( n = 12) would have prescribed an angiotensin-converting enzyme (ACE)-inhibitor or angiotensin receptor blocker (ARB) if the patient had diabetes and 50% ( n = 7) would have recommended a thiazide-type diuretic or CCB if the patient happened to be Black (following JNC8 and VA guidelines).
Table 4. Pharmacologic treatment: case 3–5 (in order of increasing complexity).
| Case number | Patient description | Blood pressure as mean SBP/DBP | Relevant history, medications, and/or labs |
|---|---|---|---|
| 3 | A 55-year-old African-American man with hypertension presents with the following blood pressures taken at home | 137/86 mm/Hg | This patient has no history of diabetes, heart disease, or stroke. He smokes half a pack of cigarettes per day. He does not currently take medication for any conditions. His most recent laboratories include: total cholesterol 180 mg/dl; HDL 50 mg/dl; LDL 120 mg/dl; creatinine of 0.95 mg/dl; urine albumin/creatinine ratio of 25 mg/g Gr |
| 4 | A 65-year-old Latino man with hypertension and Stage 3 CKD has the following BP history. He is on a low-sodium diet for hypertension | 147/91 mm/Hg | Total cholesterol 180 mg/dl; HDL 50 mg/dl; LDL 120 mg/dl; creatinine of 1.4 mg/dl; Urine albumin/creatinine ratio of 150 mg/g Cr |
| 5 | A 79-year-old African-American woman comes to see you in clinic | 149/92 mm/Hg | 50 mg atenolol for hypertension. She has a history of proteinuric CKD stage 4 (eGFR 25–30 mL/min), controlled DM, hypertension, a stroke, and recent hypotension |
Abbreviations: BMI, body mass index; CKD, chronic kidney disease; DM, diabetes mellitus; eGFR, estimated glomerular filtration rate; HDL, high-density lipoprotein; LDL, low-density lipoprotein; MCA, middle cerebral artery.
Case 4 provided a scenario where patient had several comorbidities, including chronic kidney disease (CKD). In response, 67% ( n = 8) of primary care respondents selected the therapeutic option of an ACE Inhibitor, congruent with all guidelines. Case 5 described an older adult with complex comorbidities and a likely adverse event (hypotension) from treatment. No single recommendation received a majority of responses, the selection with the highest proportion at 45% of primary care providers was, “In adults with hypertension and CKD with proteinuria, target a BP of <130/80 mm Hg.” When asked about preferred pharmacologic treatment actions, only one option achieved 50% agreement among the 14 primary care providers, “Add treatment with an ACE-Inhibitor.”
Despite this variability, primary care providers chose guideline-supported recommendations, the majority of the time: in all, 70% of the time for diagnosis and monitoring (case 1), although only 50% used the ambulatory blood pressure monitoring option preferred by some guidelines; 100% for nonpharmacologic options (case 2); and 65% for pharmacologic options (case 3–5).
Attitudes toward the Recommendations and Reasons for Variation
Fig. 3 highlights the attitudes toward the recommendations in each case: their perceived importance, the frequency they are followed, the difficulty in following them, the amount of patient input, and the amount of patient effort. When averaged across the cases, more than 80% of primary care respondents rated the guidelines as important; however, the values were slightly lower for the simplest case (case 1) where the guidelines only called for monitoring. Primary care respondents reported being able to adhere to guidelines from 10 to 78% of the time, with nonpharmacologic recommendations followed the least frequently. Patient input and effort were highest for nonpharmacologic treatments; these are largely self-managed. However, the amount of patient effort and input did not increase with the complexity of their situation.
Fig. 3.
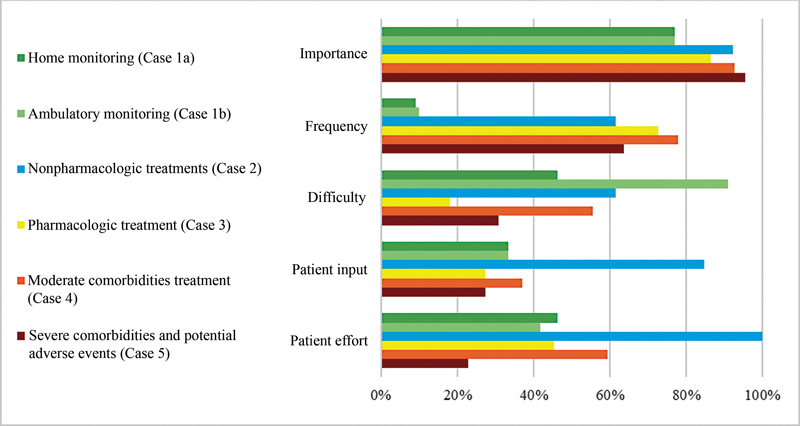
Percentage of patients selecting one of the top 3 categories on a 7-point Likert's scale.
When primary care providers were asked for free-text reasons for varying from guidelines, 30% of those who responded focused on drug allergies or side effects, while 28% focused on patient comorbidities. The remainder of responses focused on items such as family history, patient compliance or preferences, shared decision-making, cost or access concerns, or deferring to a specialist. Seventy-one percent of hypertension experts focused on allergies or side effects and 21% on comorbidities. Shared decision-making and age were suggested once while patient preference, cost/access, or other factors were not mentioned.
Main Themes from Free Text Responses
The hypertension experts and primary care providers described their preferences and experiences with CDS and shared decision-making in the context of hypertension management through free text. Primary themes were needs for effective communication and patient education materials, having consensus among provider and patient recommendations, and having clear understanding of risk and benefit in this process (see Supplementary Table S1 , available in the online version). For instance, one provider requested, “a nuanced tool that accounts for fall risk, non-life-threatening side effects, like erectile dysfunction (ED),” and then asked, “how much lifestyle change is really possible?” Several respondents mentioned wanting risk tools (like an atherosclerotic cardiovascular disease [ASCVD] risk calculator) that could provide “simple visualizations.” Others reported the desire to have consensus targets for treatment and be sure that recommendations were from updated guidelines.
Diagnosis and monitoring challenges were commonly reported. Although participants described the importance of home monitoring, they had many concerns, including financial or insurance barriers to obtaining a home cuff or ABPM, the need for calibration of home devices over time, lack of available ABPM devices, and physical or mental challenges to completing home monitoring. This was balanced against the potential inaccuracy of office measurements (e.g., white coat effect, the physical/mental stresses of a visit) and limited patient follow-up or access to the clinic.
For treatment variations, many identified narrative recommendations embedded in the guidelines that we did not transform into logic; for instance, secondary hypertension, motivation, psychiatric comorbidities, social factors, and mental health (e.g., stress reduction, sleep, and psychiatric care). Similarly, other variations in treatment included known allergies, cost, knowledge about patient compliance, or other patient context (including estimated glomerular filtration rate [eGFR] for CKD and more details related to frailty and fall risk).
Discussion
Our objective was to identify ways that hypertension guideline recommendations could be implemented in a patient-facing CDS tool, given the need to vary from guidelines and diversity of opinions about the role of the patient; to that end, hypertension experts and primary care providers identified several potential options. Providers found recommendations for hypertension guidelines to be important (>80%) and, when provided cases, had substantial variation in their responses despite primarily following guideline recommendations. Primary care providers identified nonpharmacologic options as challenging and requiring the most patient effort and input; less patient input and effort was thought to be needed from pharmacologic approaches. Diagnosis and monitoring had several challenges, from the unreliability of office blood pressures to the burden on patients to monitor reliably and accurately. ABPM was infrequently chosen despite guidelines recommending its use, providers noted barriers to cost and availability.
We used this work to adapt the CDS application. The major step we took, given the variability from providers, was focused on shared decision-making between patients and providers. We did so by making the application entirely patient facing in design (although accessible directly by providers) and focus on nonpharmacologic recommendations ( Supplementary Fig. S3 , available in the online version). We also created mechanisms to input preferences and goals, such as blood pressure goals, and drove screening and monitoring based off these goals ( Supplementary Figs. S4 and S5 , available in the online version). Given the substantial expectation of monitoring and clinical uncertainty expressed, we built the capacity to self-monitor home blood pressures and incorporated metrics for when enough blood pressures from home and office were present to be confident of the assessment for control. 14 26 27 We opted not to suggest specific blood pressure medication changes but instead prompted for when a change should be made and presented current treatments. Our previous work in data adequacy also highlighted the need for key data to be added before the recommendations could be processed, we prompted for these data first. 40
One limitation of this survey approach was the relatively small sample size which limits generalizability. However, the respondents did identify multiple different areas where they would potentially diverge from the standards and the reasons for these decisions. Varying from the recommendations reflected variation between guidelines (lack of consensus) and specific patient characteristics (like social need, comorbidities, adherence issues, or frailty). Although some recommendations can encode these differences (common comorbidities, for instance), adjusting recommendations for these factors require accurate, clear data which was not available in two out of four cases in our prior work, 20 and consensus on how to include these factors. Providers' response to increasing complexity was sometimes to get more input from the patients and acknowledge their effort, and sometimes to decide to vary more frequently. The challenges in managing guidelines with multiple comorbidities has been well studied; however, more recent work has highlighted the value in sharing the decision-making for these cases by eliciting patient priorities and values and deciding the best course of action together. 41 42
The impact of these findings on CDS systems are substantial. First, presenting the recommendations in certain situations, recommending nonpharmacologic therapy, could be highly successful if issues around workflow and patient input could be addressed. Providing self-management support through patient-facing applications, for instance, that are tied to clinical teams' support may be one way to accomplish this. Second, many providers asked for visualization tools and guidance on consensus or agreement which could be presented as part of the recommendations to help guide the discussions. Third, support for the challenges of home monitoring to get information reliable for diagnosis and overcome challenges could address a major gap. Finally, even when there is not consensus from guidelines, prioritization is still possible and highlighting potential patient factors that could aid in prioritization while referencing the most frequently chosen options could improve personalization and social trust, both factors that impact behavior and could increase adherence. Work in cognitive psychology and behavioral economics indicate social norms and nudging toward highly prioritized options while still providing choices may increase responsiveness while not diminishing autonomy. 43 44
Based on the survey results, we have adapted the CDS application which we call COACH, the Collaboration Oriented Approach to Controlling High blood pressure. These changes, shown in the Supplementary Figure S2 (available in the online version) section, led to prioritization of patient-facing elements (largely home blood pressure monitoring and nonpharmacologic counseling, goal setting, and follow-up), given the need for input and work for patients, allowance for variation in pharmacologic treatment, and the capture of “nuance” or personalization like previous adverse events or blood pressure goals in the CDS application. In addition, the prioritized clinician recommendations for lifestyle changes, like smoking cessation and alcohol moderation if relevant to the patient, are presented with the level of support (e.g., 80% of providers recommend).
Gaining end-user perspectives and preferences is fundamental to user-centered design, particularly for new technologies such as shareable and interoperable CDS. 45 46 47 These data are informing the designs of our provider-facing CDS tool which we anticipate will increase the likelihood of provider adoption. Using this survey method in which providers ranked preferences for guideline-based recommendations given patient scenarios has provided important insights as to how providers perceive the benefits of some recommendations over others when weighed against specific patient scenarios. We used these insights to transform our CDS application, now implemented at our institution.
Furthermore, surveys like ours may be sufficient for designing CDS applications; however we encourage informaticians to incorporate more advanced methods. For example, methods from cognitive science may better elucidate user perceptions and replicate real-world decisions around guideline-based care for hypertension management. 44 48
Limitations
This study has limitations that are important to note. First, we recruited providers from a convenience sample rather than a random sample 49 ; however, this is common in qualitative and user acceptance designs. Similarly, we did not intend to validate the survey beyond its utility in adapting the tool. Second, our analysis incorporated a “top three” approach to represent priority recommendations which has the potential to conflate priority recommendations. Also, we reported summary scores for each of the cases but due to the variety of nonresponses throughout the survey, we only removed survey scores when any provider did not answer an entire battery of survey questions. Lastly, we did not vet our qualitative themes (“member check”) based on participants' free-text answers.
Conclusion
In general, providers had highly variable approaches to HBP management and were accepting of patient-facing CDS tools, but emphasized the importance of CDS recommendations that capture the complexity and nuance of the recommendations. The results from our survey are informing the project team's decisions around designing a SMART-on-FHIR CDS application that supports provider and patient needs for hypertension management.
Clinical Relevance Statement
This study assessed attitudes toward clinical decision support and treatment priorities of clinicians who treat hypertension (high blood pressure), assessing how participants would monitor, diagnose, or treat five fictional patients with conditions including and related to hypertension. The results of this survey have been used to inform the development of a new clinical decision support tool for hypertension diagnosis and treatment.
Multiple Choice Questions
-
Which domain of high blood pressure guideline recommendations did providers find most difficult to follow?
Screening
Monitoring
Pharmacologic treatments
Nonpharmacologic treatments
Correct Answer: The correct answer is option d. Providers found nonpharmacologic recommendations, on the whole, most difficult to follow; this was partially.
-
What challenges to prescribing ambulatory blood pressure monitoring (ABPM) did providers note as barriers to its use in practice?
Challenges related to interpreting the results
Clinical practice guidelines not supporting its use
Cost and availability
Patient reluctance to monitor blood pressure
Correct Answer : The correct answer is option c. Providers noted that cost and availability of ambulatory blood pressure monitoring presented the primary challenges to prescribing it in clinical practice.
Funding Statement
Funding This work was supported by the Agency for Healthcare Research and Quality (grant no.: U18 HS26849-01). The project was also supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through grant award number of UL1TR002369.
Conflict of Interest None declared.
Protection of Human and Animal Subjects
This research was performed in compliance with current standards for human subjects research and was reviewed by the Oregon Health & Science University Institutional Review Board.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or Agency for Healthcare Research and Quality.
Supplementary Material
References
- 1.Fryar C D, Ostchega Y, Hales C M, Zhang G, Kruszon-Moran D. Hypertension prevalence and control among adults: United States, 2015-2016. NCHS Data Brief. 2017;(289):1–8. [PubMed] [Google Scholar]
- 2.Clinical Guidelines Committee of the American College of Physicians and the Commission on Health of the Public and Science of the American Academy of Family Physicians . Qaseem A, Wilt T J, Rich R. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017;166(06):430–437. doi: 10.7326/M16-1785. [DOI] [PubMed] [Google Scholar]
- 3.SPRINT Research Group . Wright J T, Jr., Williamson J D, Whelton P K. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015;373(22):2103–2116. doi: 10.1056/NEJMoa1511939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Connor E A, Evans C V, Rushkin M C, Redmond N, Lin J S. Behavioral counseling to promote a healthy diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: updated evidence report and systematic review for the US Preventive Services Task Force. JAMA. 2020;324(20):2076–2094. doi: 10.1001/jama.2020.17108. [DOI] [PubMed] [Google Scholar]
- 5.Alper B S, Price A, van Zuuren E J. Consistency of recommendations for evaluation and management of hypertension. JAMA Netw Open. 2019;2(11):e1915975. doi: 10.1001/jamanetworkopen.2019.15975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.SPRINT Research Group . Lewis C E, Fine L J, Beddhu S. Final report of a trial of intensive versus standard blood-pressure control. N Engl J Med. 2021;384(20):1921–1930. doi: 10.1056/NEJMoa1901281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.United States Preventive Services Task Force High blood pressure in adults: screeningAccessed September 10, 2022 at:https://health.gov/healthypeople/tools-action/browse-evidence-based-resources/high-blood-pressure-adults-screening
- 8.Ash J S, Sittig D F, Campbell E M, Guappone K P, Dykstra R H. Some unintended consequences of clinical decision support systems. AMIA Annu Symp Proc. 2007:26–30. [PMC free article] [PubMed] [Google Scholar]
- 9.Hicks L S, Sequist T D, Ayanian J Z. Impact of computerized decision support on blood pressure management and control: a randomized controlled trial. J Gen Intern Med. 2008;23(04):429–441. doi: 10.1007/s11606-007-0403-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Persson M, Mjörndal T, Carlberg B, Bohlin J, Lindholm L H. Evaluation of a computer-based decision support system for treatment of hypertension with drugs: retrospective, nonintervention testing of cost and guideline adherence. J Intern Med. 2000;247(01):87–93. doi: 10.1046/j.1365-2796.2000.00581.x. [DOI] [PubMed] [Google Scholar]
- 11.Roumie C L, Elasy T A, Greevy R. Improving blood pressure control through provider education, provider alerts, and patient education: a cluster randomized trial. Ann Intern Med. 2006;145(03):165–175. doi: 10.7326/0003-4819-145-3-200608010-00004. [DOI] [PubMed] [Google Scholar]
- 12.Anchala R, Kaptoge S, Pant H, Di Angelantonio E, Franco O H, Prabhakaran D. Evaluation of effectiveness and cost-effectiveness of a clinical decision support system in managing hypertension in resource constrained primary health care settings: results from a cluster randomized trial. J Am Heart Assoc. 2015;4(01):e001213. doi: 10.1161/JAHA.114.001213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.LOYAL Study Investigators . Rinfret S, Lussier M T, Peirce A. The impact of a multidisciplinary information technology-supported program on blood pressure control in primary care. Circ Cardiovasc Qual Outcomes. 2009;2(03):170–177. doi: 10.1161/CIRCOUTCOMES.108.823765. [DOI] [PubMed] [Google Scholar]
- 14.American Heart Association; American College of Cardiology; Centers for Disease Control and Prevention . Go A S, Bauman M A, Coleman King S M. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014;63(04):878–885. doi: 10.1161/HYP.0000000000000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Middleton B, Sittig D F, Wright A.Clinical Decision Support: a 25 Year Retrospective and a 25 Year Vision Yearb Med Inform 2016;(suppl 1):S103–S116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Semenov I, Osenev R, Gerasimov S, Kopanitsa G, Denisov D, Andreychuk Y. Experience in developing an fhir medical data management platform to provide clinical decision support. Int J Environ Res Public Health. 2019;17(01):E73. doi: 10.3390/ijerph17010073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.International H LS.FHIR Accessed September 10, 2022 at:http://hl7.org/fhir/
- 18.Services UDoHH Pharmacist eCare plan. Accessed September 10, 2022 at:https://www.healthit.gov/techlab/ipg/node/4/submission/1376
- 19.FHIR clinical guidelines. Accessed September 10, 2022 at:http://hl7.org/fhir/uv/cpg/2019Sep/index.html#home
- 20.Dorr D A, D'Autremont C, Pizzimenti C. Assessing data adequacy for high blood pressure clinical decision support: a quantitative analysis. Appl Clin Inform. 2021;12(04):710–720. doi: 10.1055/s-0041-1732401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dorr D, Storer M.Content Implementation Guide, High Blood PressureAccessed September 10, 2022 at:https://build.fhir.org/ig/OHSUCMP/htnu18ig/index.html
- 22.Osheroff J A, Teich J M, Levick D.Improving Outcomes with Clinical Decision Support: An Implementer's Guide2nd ed.Boca Raton, FL: CRC Press; 2012 [Google Scholar]
- 23.Bright T J, Wong A, Dhurjati R. Effect of clinical decision-support systems: a systematic review. Ann Intern Med. 2012;157(01):29–43. doi: 10.7326/0003-4819-157-1-201207030-00450. [DOI] [PubMed] [Google Scholar]
- 24.Oliveria S A, Lapuerta P, McCarthy B D, L'Italien G J, Berlowitz D R, Asch S M. Physician-related barriers to the effective management of uncontrolled hypertension. Arch Intern Med. 2002;162(04):413–420. doi: 10.1001/archinte.162.4.413. [DOI] [PubMed] [Google Scholar]
- 25.Oliveria S A, Chen R S, McCarthy B D, Davis C C, Hill M N. Hypertension knowledge, awareness, and attitudes in a hypertensive population. J Gen Intern Med. 2005;20(03):219–225. doi: 10.1111/j.1525-1497.2005.30353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Koopman R J, Canfield S M, Belden J L. Home blood pressure data visualization for the management of hypertension: designing for patient and physician information needs. BMC Med Inform Decis Mak. 2020;20(01):195. doi: 10.1186/s12911-020-01194-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kerr E A, Zikmund-Fisher B J, Klamerus M L, Subramanian U, Hogan M M, Hofer T P. The role of clinical uncertainty in treatment decisions for diabetic patients with uncontrolled blood pressure. Ann Intern Med. 2008;148(10):717–727. doi: 10.7326/0003-4819-148-10-200805200-00004. [DOI] [PubMed] [Google Scholar]
- 28.Kim M T, Song H J, Han H R. Development and validation of the high blood pressure-focused health literacy scale. Patient Educ Couns. 2012;87(02):165–170. doi: 10.1016/j.pec.2011.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turer C B, Doney A, Bowen M E. Determining pediatric hypertension criteria: concordance between observed physician methods and guideline-recommended methods. J Hypertens. 2021;39(09):1893–1900. doi: 10.1097/HJH.0000000000002869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moise N, Phillips E, Carter E. Design and study protocol for a cluster randomized trial of a multi-faceted implementation strategy to increase the uptake of the USPSTF hypertension screening recommendations: the EMBRACE study. Implement Sci. 2020;15(01):63. doi: 10.1186/s13012-020-01017-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith J D, Mohanty N, Davis M M. Optimizing the implementation of a population panel management intervention in safety-net clinics for pediatric hypertension (The OpTIMISe-Pediatric Hypertension Study) Implement Sci Commun. 2020;1(01):57. doi: 10.1186/s43058-020-00039-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Silveira D V, Marcolino M S, Machado E L. Development and evaluation of a mobile decision support system for hypertension management in the primary care setting in Brazil: mixed-methods field study on usability, feasibility, and utility. JMIR Mhealth Uhealth. 2019;7(03):e9869. doi: 10.2196/mhealth.9869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gordon W J, Blood A J, Chaney K. Workflow automation for a virtual hypertension management program. Appl Clin Inform. 2021;12(05):1041–1048. doi: 10.1055/s-0041-1739195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Duhm J, Fleischmann R, Schmidt S, Hupperts H, Brandt S A. Mobile electronic medical records promote workflow: physicians' perspective from a survey. JMIR Mhealth Uhealth. 2016;4(02):e70. doi: 10.2196/mhealth.5464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.James P A, Oparil S, Carter B L. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8) JAMA. 2014;311(05):507–520. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 36.Whelton P K, Carey R M, Aronow W S. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(06):e13–e115. doi: 10.1161/HYP.0000000000000065. [DOI] [PubMed] [Google Scholar]
- 37.Tschanz C MP, Cushman W C, Harrell C TE, Berlowitz D R, Sall J L. Synopsis of the 2020 U.S. Department of Veterans Affairs/U.S. Department of Defense Clinical Practice Guideline: The Diagnosis and Management of Hypertension in the Primary Care Setting. Ann Intern Med. 2020;173(11):904–913. doi: 10.7326/M20-3798. [DOI] [PubMed] [Google Scholar]
- 38.Specialist C H.(CHS) – American Hypertension Specialist Certification ProgramAccessed September 10, 2022 at:http://www.ahscp.org/certified-hypertension-specialist/
- 39.Oregon Health Authority Patient-centered primary care home program: patient-centered primary care home programAccessed September 10, 2022 at:https://www.oregon.gov/oha/hpa/dsi-pcpch/Pages/index.aspx
- 40.Dorr D A, D'Autremont C, Pizzimenti C. Assessing data adequacy for high blood pressure clinical decision support: a quantitative analysis. Appl Clin Inform. 2021;12(04):710–720. doi: 10.1055/s-0041-1732401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blaum C S, Rosen J, Naik A D. Feasibility of implementing patient priorities care for older adults with multiple chronic conditions. J Am Geriatr Soc. 2018;66(10):2009–2016. doi: 10.1111/jgs.15465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boyd C, Smith C D, Masoudi F A. Decision making for older adults with multiple chronic conditions: executive summary for the American Geriatrics Society Guiding Principles on the care of older adults with multimorbidity. J Am Geriatr Soc. 2019;67(04):665–673. doi: 10.1111/jgs.15809. [DOI] [PubMed] [Google Scholar]
- 43.Shaffer V A. Nudges for health policy: effectiveness and limitations. Miss Law Rev. 2017;82:727. [Google Scholar]
- 44.Shaffer V A, Wegier P, Valentine K D. Patient judgments about hypertension control: the role of variability, trends, and outliers in visualized blood pressure data. J Med Internet Res. 2019;21(03):e11366. doi: 10.2196/11366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Chokshi S K, Belli H M, Troxel A B. Designing for implementation: user-centered development and pilot testing of a behavioral economic-inspired electronic health record clinical decision support module. Pilot Feasibility Stud. 2019;5:28. doi: 10.1186/s40814-019-0403-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chokshi S K, Mann D M. Innovating from within: a process model for user-centered digital development in academic medical centers. JMIR Human Factors. 2018;5(04):e11048. doi: 10.2196/11048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mann D, Hess R, McGinn T. Adaptive design of a clinical decision support tool: What the impact on utilization rates means for future CDS research. Digit Health. 2019;5:2.055207619827716E15. doi: 10.1177/2055207619827716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shaffer V A, Wegier P, Valentine K D. Use of Enhanced Data Visualization to Improve Patient Judgments about Hypertension Control. Med Decis Making. 2020;40(06):785–796. doi: 10.1177/0272989X20940999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nielsen J, Landauer T K.A mathematical model of the finding of usability problemsProceedings of the INTERACT '93 and CHI '93 Conference on Human Factors in Computing Systems; Amsterdam, The Netherlands: Association for Computing Machinery;1993206–213.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


