Abstract
Background
Point-of-care (POC) MRI is a bedside imaging technology with fewer than five units in clinical use in the United States and a paucity of scientific studies on clinical applications.
Purpose
To evaluate the clinical and operational impacts of deploying POC MRI in emergency department (ED) and intensive care unit (ICU) patient settings for bedside neuroimaging, including the turnaround time.
Materials and Methods
In this preliminary retrospective study, all patients in the ED and ICU at a single academic medical center who underwent noncontrast brain MRI from January 2021 to June 2021 were investigated to determine the number of patients who underwent bedside POC MRI. Turnaround time, examination limitations, relevant findings, and potential CT and fixed MRI findings were recorded for patients who underwent POC MRI. Descriptive statistics were used to describe clinical variables. The Mann-Whitney U test was used to compare the turnaround time between POC MRI and fixed MRI examinations.
Results
Of 638 noncontrast brain MRI examinations, 36 POC MRI examinations were performed in 35 patients (median age, 66 years [IQR, 57–77 years]; 21 women), with one patient undergoing two POC MRI examinations. Of the 36 POC MRI examinations, 13 (36%) occurred in the ED and 23 (64%) in the ICU. There were 12 of 36 (33%) POC MRI examinations interpreted as negative, 14 of 36 (39%) with clinically significant imaging findings, and 10 of 36 (28%) deemed nondiagnostic for reasons such as patient motion. Of 23 diagnostic POC MRI examinations with comparison CT available, three (13%) demonstrated acute infarctions not apparent on CT scans. Of seven diagnostic POC MRI examinations with subsequent fixed MRI examinations, two (29%) demonstrated missed versus interval subcentimeter infarctions, while the remaining demonstrated no change. The median turnaround time of POC MRI was 3.4 hours in the ED and 5.3 hours in the ICU.
Conclusion
Point-of-care (POC) MRI was performed rapidly in the emergency department and intensive care unit. A few POC MRI examinations demonstrated acute infarctions not apparent at standard-of-care CT examinations.
© RSNA, 2022
Online supplemental material is available for this article.
See also the editorial by Anzai and Moy in this issue.
Summary
This study demonstrates that point-of-care brain MRI can serve as a diagnostic tool in emergency departments and intensive care units to provide bedside image acquisition, with some limitations in diagnostic quality.
Key Results
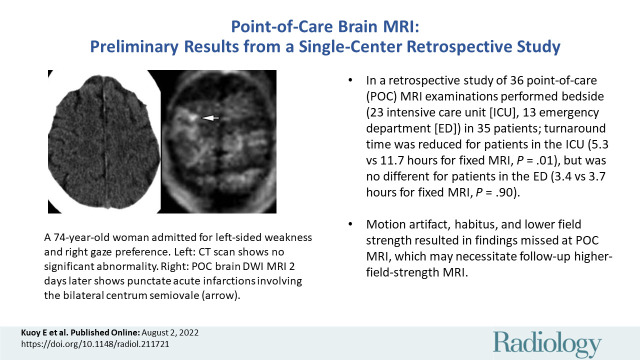
■ In this retrospective study of 36 point-of-care (POC) MRI examinations performed bedside (23 intensive care unit [ICU], 13 emergency department [ED]) in 35 patients, the turnaround time was reduced for patients in the ICU (5.3 vs 11.7 hours for fixed MRI; P = .01), but was no different for patients in the ED (3.4 vs 3.7 hours for fixed MRI; P = .90).
■ Motion artifact, habitus, and lower field strength resulted in findings missed at POC MRI, which may necessitate follow-up higher-field-strength MRI.
Introduction
For patients with acute neurologic injury, early diagnosis and management may reduce morbidity, mortality, and health care costs (1,2). Objective diagnostic imaging is particularly important when neurologic examinations are unattainable due to impaired or altered consciousness (3). While noncontrast head CT represents the first-line imaging choice due to its acquisition speed and availability, MRI is widely used following unrevealing CT examinations (4–6). Acquiring diagnostic brain MRI for critically ill patients remains challenging as patients may experience adverse events during intrahospital transport, and there are often substantial delays between the ordering and acquisition of MRI, which may further increase patients’ hospital length of stay (7–10).
One potential solution for imaging critically ill patients with acute neurologic injury is point-of-care (POC) technology performed at the patient’s bedside. The U.S. Food and Drug Administration has recently provided 510 (k) premarket notification for a bedside, POC 0.064-T MRI device, which can perform brain MRI with basic MRI pulse sequences. Currently, there are few of these devices operating clinically in the United States. If demonstrated to be sufficiently accurate, POC technology may obviate the need to transport patients to and from radiology suites. Although expanding access to MRI can change patient management, poor diagnostic quality has been reported in some cases (11,12). Bedside POC MRI may additionally improve the throughput of existing fixed MRI machines by removing complicated and time-intensive critically ill patients from the scheduling queue.
In this retrospective single-center study, we sought to evaluate the preliminary impact of deploying POC MRI in emergency department (ED) and intensive care unit (ICU) settings, including the turnaround time.
Materials and Methods
Patients
This preliminary retrospective study protocol was approved by the local institutional review board with a waiver of patient informed consent. This study was Health Insurance Portability and Accountability Act–compliant. All consecutive patients in the ED and ICU at a single 411-bed academic medical center in Southern California who underwent noncontrast brain MRI during a 5-month period, from January 2021 to June 2021, were retrospectively evaluated. No patients were excluded.
POC Examinations
All 0.064-T POC MRI (Swoop Portable MR Imaging System, with RC8 software; Hyperfine) examinations were performed with the manufacturer’s standard protocol, which consists of axial T1-weighted fast spin-echo, T2-weighted fast spin-echo, T2-weighted fluid-attenuated inversion recovery (or FLAIR), and diffusion-weighted imaging with apparent diffusion coefficient sequences (Table 1). Appendix E1 (online) details the examination selection and staffing logistical information.
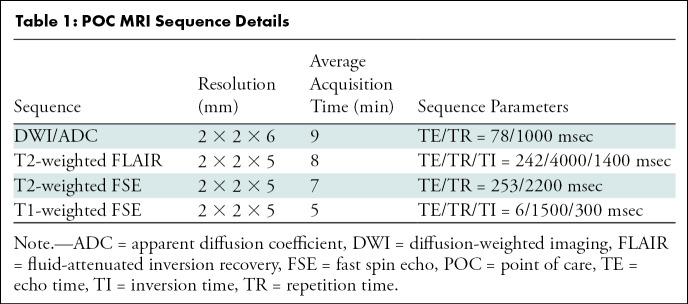
Table 1:
POC MRI Sequence Details
A Health Insurance Portability and Accountability Act–compliant database was created with data on all patients who underwent POC noncontrast brain MRI, including examination ordering and completion times, examination limitations, clinical indications, and relevant imaging findings. In addition, the medical records of each patient were searched for any standard-of-care head CT examinations performed within 3 days of the POC MRI examination, or subsequent fixed brain MRI performed in the 11-day period after the POC MRI examination. Any new findings appreciated on the follow-up examination were evaluated on the basis of three categories: new and/or interval acute findings (eg, acute infarction), unchanged relevant findings in comparison with the POC MRI examination (eg, intracranial hemorrhage or mass lesion), and no acute finding. All brain MRI examinations were interpreted prior to initiation of the study as part of routine clinical care by a fellowship-trained academic neuroradiologist, as is customary at our institution. One observer (E.K., with 1.5 years of experience in neuroradiology) performed a retrospective nonblinded comparison of examination findings.
Turnaround Times
The turnaround time was defined as the difference between the time when each POC MRI examination was ordered and when it was completed by the technologist. For evaluation of the turnaround time, an institutional analytics database (mPower Clinical Analytics; Nuance) was queried for all ED and ICU noncontrast brain MRI examinations performed during the same 5-month period from January 2021 to June 2021.
Statistical Analysis
Statistical analysis was performed by two authors (E.K., J.G.B.). Descriptive statistics of clinical data are presented as medians with IQRs for continuous variables and as frequencies and percentages for categorical variables. The Mann-Whitney U test was used to compare the turnaround time between POC MRI and fixed brain MRI examinations in the ED and ICU settings. Statistical analysis was conducted with IBM SPSS Statistics version 1.0.0.1012 (IBM), and P < .05 was considered indicative of a statistically significant difference.
Results
Patient Characteristics
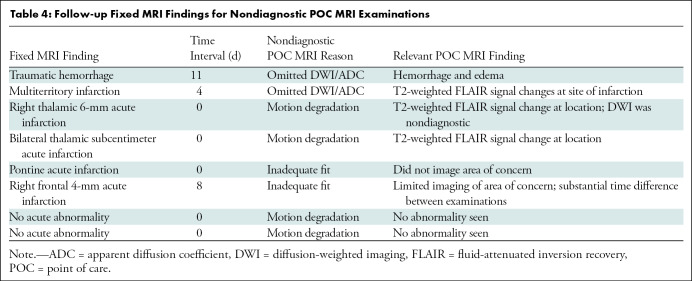
During the 5-month study period, a total of 638 noncontrast brain MRI examinations were performed in patients in the ED (486 of 638 [76%]) and ICU (152 of 638 [24%]). Of these, there were 36 POC MRI examinations performed in 35 patients (median age, 66 years [IQR, 57–77 years]; 21 women), representing 3% (13 of 486) of total ED and 15% (23 of 152) of total ICU examinations (one patient received two POC MRI examinations). The demographic characteristics of these patients are summarized in Table 2. No patients were excluded from analysis in the study.
Table 2:
Demographics of Patients Who Underwent POC MRI
POC MRI Examinations
Of the 36 noncontrast brain POC MRI examinations performed during the 5-month study period, 13 (36%) were in the ED and 23 (64%) were in the ICU. Clinical indications for these examinations included stroke (n = 24), altered mental status (n = 7), suspected intracranial mass (n = 4), and ventricular shunt placement (n = 1) (Fig 1 includes a comparison head CT scan). POC MRI examinations were performed on 28 days, with two examinations per day on 6 of those days, three examinations per day on 1 day, and one examination per day on the remaining 21 days.
Figure 1:
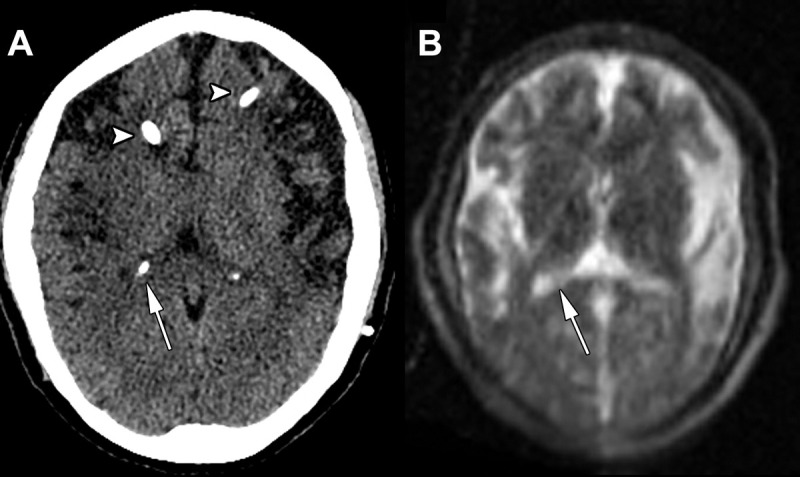
Images in a 42-year-old woman admitted for headaches with a history of congenital hydrocephalus after ventriculoperitoneal shunt placement. (A) Axial head CT scan without contrast shows no significant hydrocephalus at the level of the lateral ventricle atrium (arrow) and partially visualized ventriculostomy catheters (arrowheads). (B) Point-of-care brain MRI scan without contrast obtained with T2-weighted sequence 1 hour after axial head CT and on a similar level shows nonenlarged lateral ventricles at the level of the lateral ventricle atrium (arrow), and the ventriculostomy catheters are more difficult to visualize.
Of the 36 examinations, 12 (33%) were interpreted as normal or negative, 10 (28%) demonstrated acute findings, such as acute infarction (Fig 2) or hemorrhage, and four (11%) demonstrated mass lesions. Ten of the 36 (28%) examinations were nondiagnostic; two due to technologist-related error in omitting the diffusion-weighted imaging sequence, five due to substantial motion degradation, one due to a substantial external or zipper artifact related to adjacent support machines, and two because the patient could not adequately fit into the machine.
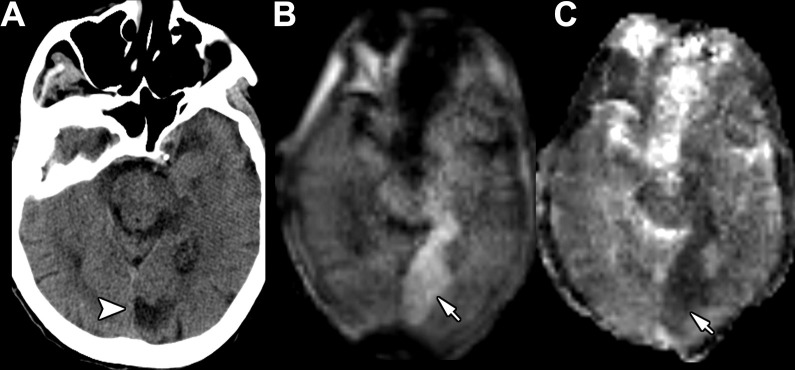
Figure 2:
Images in an 84-year-old woman admitted for new facial droop with a history of partial left posterior cerebral artery territory infarction. (A) Axial head CT scan without contrast shows a chronic left posterior cerebral artery infarction (arrowhead). (B, C) Point-of-care brain MRI scans without contrast obtained in the axial plane 1 day later with (B) diffusion-weighted imaging and (C) apparent diffusion coefficient imaging show an acute left posterior cerebral artery territory infarction (arrows) anterior to the area of chronic infarction demonstrated on earlier head CT scans.
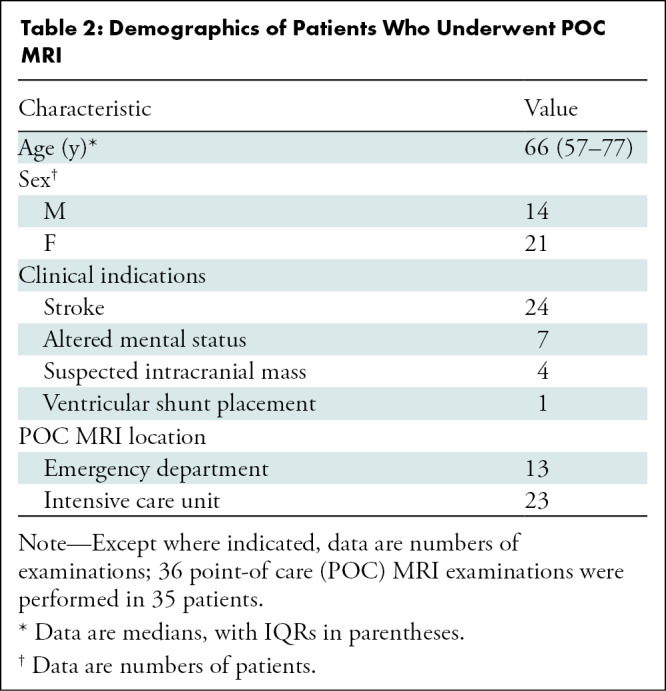
POC MRI Comparison to CT
Of the 26 (26 of 36, 72%) diagnostic POC MRI examinations, there was a comparison CT examination available for 23 (88%) (Table 3). Of these 23 examinations, 8 (35%) were normal or negative at both CT and POC MRI. There were findings seen with both modalities in 12 of 23 (52%) examinations (six with acute and/or subacute infarction, three with a mass, two with hemorrhage, and one with shunted ventricles). Acute infarction was demonstrated on POC MRI scans but not seen on CT scans in 3 of 23 (13%) examinations (Figs 2, 3).
Table 3:
Diagnostic POC MRI and Comparison Head CT Findings
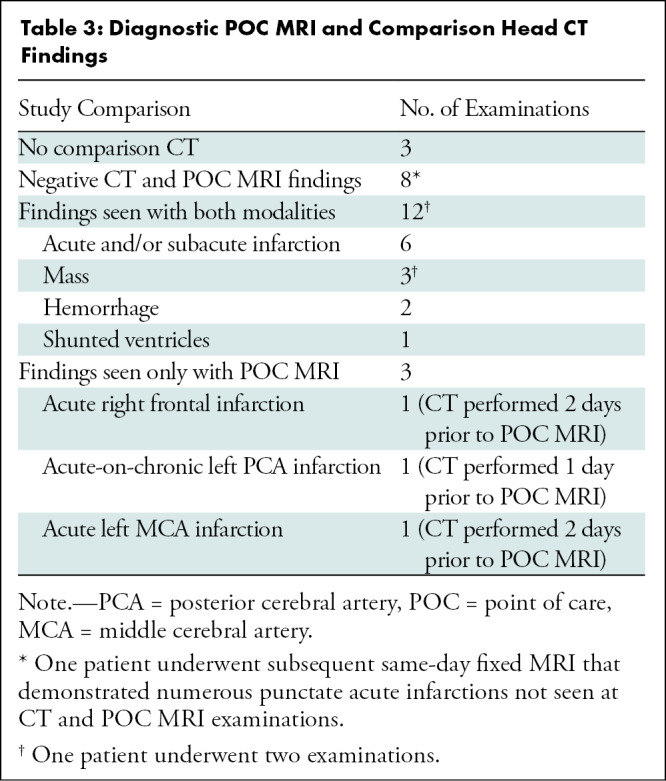
Figure 3:
Images in a 74-year-old woman admitted for left-sided weakness and right gaze preference. (A) Axial head CT scan without contrast shows no significant abnormality. (B–D) Point-of-care brain MRI scans without contrast obtained in the axial plane 2 days later with (B) diffusion-weighted imaging, (C) apparent diffusion coefficient imaging, and (D) T2-weighted fluid-attenuated inversion recovery imaging show a right middle cerebral artery territory acute infarction with restricted diffusion (arrows) and associated T2-weighted fluid-attenuated inversion recovery signal abnormality (arrowhead).
POC MRI Comparison to Fixed MRI
Among the 10 nondiagnostic POC MRI examinations, eight required follow-up with fixed MRI. Of the eight follow-up fixed MRI examinations, two demonstrated no acute findings, one redemonstrated traumatic intraparenchymal hemorrhage (the diffusion-weighted imaging sequence was erroneously omitted from the ischemic stroke workup), and five showed acute and/or subacute infarctions (Table 4). Of the latter five examinations, two were not visualized either because they were new in the interval or missed due to a combination of both motion degradation and punctate infarction size less than 6 mm in the maximal axial dimension, two were not visualized due to the inability of the patient to fit in the scanner, and one was not characterized because the diffusion-weighted imaging sequence was erroneously omitted.
Table 4:
Follow-up Fixed MRI Findings for Nondiagnostic POC MRI Examinations
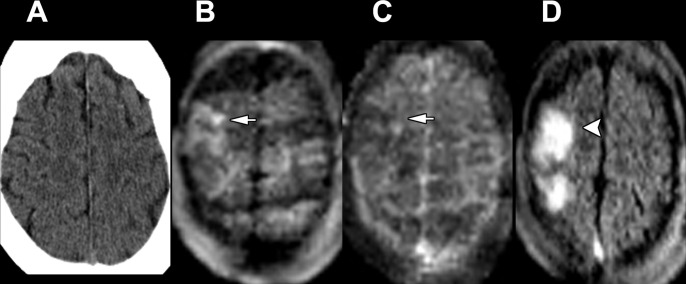
A total of seven diagnostic POC MRI examinations resulted in subsequent fixed MRI examination (excluding a short-interval unchanged duplicated examination) at the discretion of the clinical team. Of these, one demonstrated interval versus missed numerous punctate acute infarctions measuring 4 mm or less in the maximal axial dimension (Fig 4), one demonstrated interval versus new punctate cerebellar acute infarctions measuring 4 mm or less in the maximal axial dimension in addition to acute infarctions already characterized at POC MRI, two had no change with redemonstrated recent infarctions characterized at POC MRI, two had no change with redemonstrated mass lesions (meningioma and brainstem glioma), and one had no change with a redemonstrated lack of acute findings.
Figure 4:
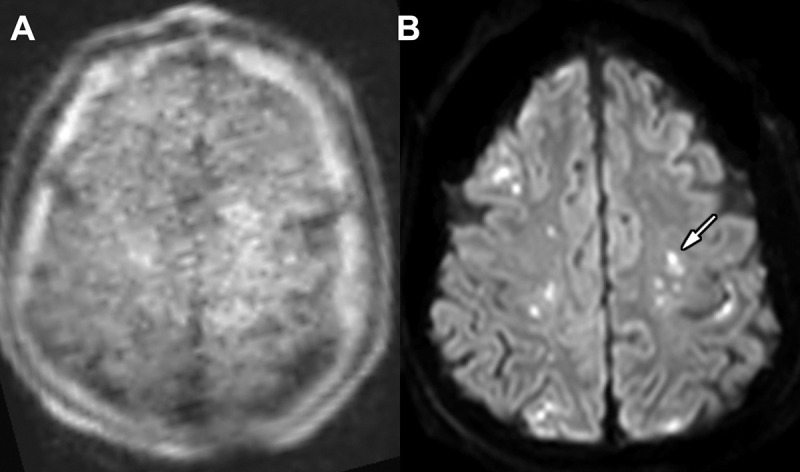
Images in an 89-year-old woman admitted for multiple injuries following a motor vehicle collision. (A) Point-of-care brain MRI scan without contrast obtained in the axial plane with diffusion-weighted imaging shows no significant abnormality. (B) Brain MRI scan without contrast obtained in the axial plane 1 day later with a fixed 3-T scanner and diffusion-weighted imaging shows punctate acute infarctions involving the bilateral centrum semiovale (arrow, left-sided involvement).
Turnaround Times
In the ED, the median turnaround time was 3.4 hours (IQR, 3.0–4.3 hours) for POC MRI compared with 3.7 hours (IQR, 2.4–7.0 hours) for fixed MRI (P = .90). In the ICU, the median turnaround time was 5.3 hours (IQR, 3.8–10.3 hours) for POC MRI compared with 11.7 hours (IQR, 10.3–27.2 hours) for fixed MRI (P = .01).
Discussion
Point-of-care (POC) MRI is a technology currently used clinically at fewer than five institutions in the United States. Herein, we present our preliminary experience in the first 5 months since clinical deployment at our academic medical center. We have seen that POC MRI can be performed rapidly at the patient’s bedside for noncontrast brain MRI examinations, with a median turnaround time of 3.4 hours for POC MRI in the emergency department and 5.3 hours in the intensive care unit. Of 36 total POC MRI examinations performed in 35 patients, POC MRI was diagnostic in 26 (72%). In terms of diagnostic POC MRI examinations that required subsequent fixed MRI follow-up, two of seven (29%) did not demonstrate the punctate acute infarctions observed at the subsequent fixed examination, which was performed up to 2 days later. Of 23 POC MRI examinations with preceding head CT, three (13%) demonstrated acute infarctions that were not apparent on comparison CT scans.
In our study, the percentage of diagnostic POC MRI examinations (72%) was lower than prior reports of POC MRI quality adequate for interpretation; 51 of 60 (85%) examinations in the study by Turpin et al (12) and 104 of 119 (87%) examinations in the study by Mazurek et al (13). We note two major challenges that limited the diagnostic quality. The first challenge relates to the patient’s habitus and ability to fit in the POC MRI head coil. Positioning can be improved with angulation, lowering shoulders, and using support material. In some instances, the habitus may ultimately inhibit the ability to acquire POC MRI. Training is necessary in proper selection of patients based on habitus. Habitus can pose an imaging dilemma not just to POC MRI but across different imaging modalities (14). The second major challenge presents in patients with substantial motion, which, although amplified with a more prolonged scan, is an issue across various imaging modalities. A more minor challenge that arose during the initial phase was erroneous exclusion of the diffusion-weighted imaging with apparent diffusion coefficient sequence, which was corrected through MRI technologist training and removal of unused examination protocols from the device. When comparing diagnostic POC MRI with subsequent fixed MRI, two of seven (29%) POC MRI examinations did not demonstrate the punctate acute infarctions, either new or missed, observed at the subsequent fixed examination performed the same day or 2 days later. It is important to examine the extent to which POC MRI can resolve small lesions and lesion locations. These highlight potential real-world limitations we experienced with this technology during our preliminary study period.
Noncontrast head CT is the current standard of care for acute neuroimaging. In this study, 23 of 26 (88%) diagnostic POC MRI examinations had comparison preceding head CT examinations available. While 12 of 23 (52%) examinations demonstrated imaging findings at least partially characterizable at both examinations and 8 of 23 (35%) had negative findings at both examinations, MRI is more sensitive in the evaluation of early infarction and can better define the extent, or lack thereof, of early ischemic infarction. During the study period, three of 23 (13%) diagnostic POC MRI examinations demonstrated acute infarctions not characterizable at comparison head CT.
Our study had limitations. First, this was a small, retrospective single-center study that presents preliminary results over an initial 5-month period, and the results may have been affected by selection bias. Second, not all patients who received POC MRI underwent head CT or follow-up fixed MRI examinations for comparison. The decision to perform a follow-up fixed examination was left to the discretion of the caring physician team.
Our results indicate that point-of-care (POC) MRI may have a role in facilitating timely imaging of critically ill patients by providing easier bedside image acquisition. In instances of motion artifact or suspected subtle findings, it may be necessary to perform subsequent imaging with a 1.5-T or 3-T fixed unit MRI scanner. Ongoing technologist training, selection of patients with appropriate body habitus who can limit motion, and further research are necessary to determine the accuracy of POC MRI, clinical indications, and patients for whom it may be particularly useful. Further studies are needed to determine the real-world incremental value of POC MRI compared with noncontrast head CT and the concordance between POC MRI and traditional fixed MRI, as well as the contrast and spatial resolution to detect subtle neurologic abnormalities, to determine the appropriateness of POC MRI and guide clinical patient selection.
Supported by the RSNA Research & Education Foundation (grant RSD2121). Y.A. supported by a National Institutes of Health/National Institute of Biomedical Imaging and Bioengineering grant (R21EB024793)
Disclosures of conflicts of interest: E.K. No relevant relationships. J.G.B. No relevant relationships. G.H. No relevant relationships. B.Y. No relevant relationships. A.B. No relevant relationships. L.A.M. No relevant relationships. L.A.N. No relevant relationships. J.L. No relevant relationships. J.E.S. Research grants from the RSNA and Canon Medical Systems. P.D.C. No relevant relationships. E.C. No relevant relationships. Y.A. No relevant relationships. V.Y. No relevant relationships. J.C.F. No relevant relationships. W.Y. No relevant relationships. D.S.C. Grants from Canon Medical Systems and Avicenna.ai; consulting fees from Canon Medical Systems; expert testimony payment from Cullins & Grandy; stockholder, Avicenna.ai.
Abbreviations:
- ED
- emergency department
- ICU
- intensive care unit
- POC
- point of care
References
- 1.Fakhry SM, Trask AL, Waller MA, Watts DD; IRTC Neurotrauma Task Force . Management of brain-injured patients by an evidence-based medicine protocol improves outcomes and decreases hospital charges. J Trauma 2004;56(3):492–499;discussion 499–500. [DOI] [PubMed] [Google Scholar]
- 2.Watts DD, Hanfling D, Waller MA, Gilmore C, Fakhry SM, Trask AL. An evaluation of the use of guidelines in prehospital management of brain injury. Prehosp Emerg Care 2004;8(3):254–261. [DOI] [PubMed] [Google Scholar]
- 3.Lee B, Newberg A. Neuroimaging in traumatic brain imaging. NeuroRx 2005;2(2):372–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ogawa T, Sekino H, Uzura M, et al. Comparative study of magnetic resonance and CT scan imaging in cases of severe head injury. Acta Neurochir Suppl (Wien) 1992;55:8–10. [DOI] [PubMed] [Google Scholar]
- 5.Doezema D, King JN, Tandberg D, Espinosa MC, Orrison WW. Magnetic resonance imaging in minor head injury. Ann Emerg Med 1991;20(12):1281–1285. [DOI] [PubMed] [Google Scholar]
- 6.Mittl RL, Grossman RI, Hiehle JF, et al. Prevalence of MR evidence of diffuse axonal injury in patients with mild head injury and normal head CT findings. AJNR Am J Neuroradiol 1994;15(8):1583–1589. [PMC free article] [PubMed] [Google Scholar]
- 7.Smith I, Fleming S, Cernaianu A. Mishaps during transport from the intensive care unit. Crit Care Med 1990;18(3):278–281. [DOI] [PubMed] [Google Scholar]
- 8.Drose JA, Pritchard NL, Honce JM, Snuttjer DK, Borgstede JP. Utilizing Process Improvement Methodology to Improve Inpatient Access to MRI. RadioGraphics 2019;39(7):2103–2110. [DOI] [PubMed] [Google Scholar]
- 9.Redd V, Levin S, Toerper M, Creel A, Peterson S. Effects of fully accessible magnetic resonance imaging in the emergency department. Acad Emerg Med 2015;22(6):741–749. [DOI] [PubMed] [Google Scholar]
- 10.Cournane S, Conway R, Creagh D, Byrne DG, Sheehy N, Silke B. Radiology imaging delays as independent predictors of length of hospital stay for emergency medical admissions. Clin Radiol 2016;71(9):912–918. [DOI] [PubMed] [Google Scholar]
- 11.Sheth KN, Mazurek MH, Yuen MM, et al. Assessment of Brain Injury Using Portable, Low-Field Magnetic Resonance Imaging at the Bedside of Critically Ill Patients. JAMA Neurol 2021;78(1):41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Turpin J, Unadkat P, Thomas J, et al. Portable Magnetic Resonance Imaging for ICU Patients. Crit Care Explor 2020;2(12):e0306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mazurek MH, Cahn BA, Yuen MM, et al. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun 2021;12(1):5119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uppot RN. Technical challenges of imaging & image-guided interventions in obese patients. Br J Radiol 2018;91(1089):20170931. [DOI] [PMC free article] [PubMed] [Google Scholar]