Abstract
Introduction
Postoperative atrial fibrillation (poAF) is a common complication of coronary artery bypass grafting, and its reasons are still the subject of research. The aim of this study was to evaluate whether QT interval is related to new onset of poAF occurrence.
Methods
This study included 167 patients undergoing elective isolated off-pump coronary artery bypass grafting (OPCAB) surgery. Patients were divided into two groups as poAF (+) and poAF (-), according to the development of poAF, and the results of the measurements were compared between the groups.
Results
PoAF was detected in 37 (22.1%) of 167 patients who underwent OPCAB surgery. When QT interval measurements were compared, preoperative and postoperative QT and corrected QT interval (QTc) values were significantly longer in the group with atrial fibrillation. Mean values of preoperative QT were 407.5±27.1 in the poAF (-) group vs. 438.5±48.5 in the poAF (+) group (P<0.001). Mean values of preoperative QTc were 419.1±14.5 in the poAF (-) group vs. 448.5±26.6 in the poAF (+) group (P<0.001). Mean values of postoperative QT were 416.3±48.3 in the poAF (-) group vs. 439.2±45.8 in the poAF (+) group (P=0.005). And mean values of postoperative QTc were 419.8±12.5 in the poAF (-) group vs. 452.0±23.3 in the poAF (+) group (P<0.001).
Conclusion
QT interval measurement may be a new parameter in predicting poAF development after OPCAB surgery.
Keywords: Atrial Fibrillation; Coronary Artery Bypass; Coronary Artery Bypass, Off-Pump; Elective Surgical Procedures; Postoperative Complications.
| Abbreviations, Acronyms & Symbols | ||
|---|---|---|
| ACE-I = Angiotensin-converting enzyme inhibitors | Hct = Hematocrit | |
| AF = Atrial fibrillation | IABP = Intra-aortic balloon pump | |
| ARB = Angiotensin receptor blockers | ICU = Intensive care unit | |
| AUC = Area under the curve | LA = Left atrial | |
| BMI = Body mass index | LVEF = Left ventricular ejection fraction | |
| CABG = Coronary artery bypass grafting | MPV = Mean platelet volume | |
| CI = Confidence interval | NPV = Negative predictive value | |
| COPD = Chronic obstructive pulmonary disease | OPCAB = Off-pump coronary artery bypass grafting | |
| CRP = C-reactive protein | poAF = Postoperative atrial fibrillation | |
| ECG = Electrocardiogram | PPV = Positive predictive value | |
| FEV1 = Forced expiratory volume in the first second | QTc = Corrected QT interval | |
| FVC = Forced vital capacity | RDW = Red cell distribution width | |
| Hb = Hemoglobin | ROC = Receiver operating characteristic |
INTRODUCTION
Postoperative atrial fibrillation (poAF) is one of the most common complications after cardiac surgery and a major risk factor that can result in mortality of the patients. It complicates about one third of cardiac surgery cases and is associated with major adverse events, prolonged hospitalization, increased healthcare costs, and increased re-hospitalization rates[1-7]. The first two weeks after surgery are the most critical, with patients at high risk for poAF[8].
New-onset poAF was shown to predict long-term newly developed atrial fibrillation (AF) in coronary artery bypass grafting (CABG) patients[9]. New-onset poAF is significantly associated with increased long-term risk of mortality independent of patient preoperative severity[10].
Although there have been some changes in medical treatment and surgery over time, the overall incidence of poAF has not changed significantly[11]. The incidence of poAF remains high, ranging between 15-40%[12-14]. The underlying pathophysiology of poAF is still unclear; however, numerous risk factors predisposing to its development have been identified, including advanced age, structural damage to the heart, left ventricular dysfunction, hypertension, and valve surgery[15]. Preventive strategies have been partially effective in reducing the overall incidence of AF in the past two decades[16]. If the underlying mechanisms can be identified, high-risk patients can be identified, and individual preventive strategies and treatments can be developed[12]. Several studies have investigated predictors of poAF[17,18]. In a recent meta-analysis including a total of 11 studies and 40,112 patients who underwent CABG, the predictors of poAF were found as older age, low ejection fraction, a history of cardiac failure or hypertension, prior peripheral arterial disease, and stroke[19].
The QT interval is obtained from a standard 12-lead electrocardiogram (ECG) and is a ready, cheap, and fast measure of ventricular repolarization. Several studies have shown that prolonged QT interval is independently correlated with an increased risk of AF and stroke[20-22]. In a recent systematic review and meta-analysis, prolonged QT interval was also associated with an increased risk of AF[19]. The association between prolongation of QT and AF has been explained by abnormalities in myocardial repolarization[23]. However, it is not known whether there is a clinically significant relationship between ventricular repolarization and atrial electrophysiology. Ventricular and atrial refractoriness is determined by many of the same potassium and sodium channels, and there is possibly a correlation between the two[20].
In this study, we aimed to investigate whether a longer QT interval might be an important predictor of poAF in off-pump CABG (OPCAB) patients.
METHODS
Study Population and Design
A total of 167 consecutive patients between 18-80 years of age who had no history of AF and underwent elective OPCAB surgery between January 2013 and December 2014 were included in this study. Patients were divided into two groups as poAF (+) and poAF (-), according to the development of poAF, and the results of the measurements were compared between the groups. Demographic data of the patients (age, gender); body mass index (BMI); history of hypertension, chronic kidney failure, diabetes, heart failure, chronic obstructive pulmonary disease (COPD), and stroke; preoperative drug use (angiotensin-converting enzyme inhibitors [ACE-I], angiotensin receptor blockers [ARB], beta blockers, and statins); and echocardiographic findings (ejection fraction, left atrial diameter, and valve disease) were obtained from the hospital records and retrospectively analyzed. All patients were operated by the same surgical team and Octopus IV (Medtronic, Minneapolis) was used as a stabilizer in all operations. Patients who needed preoperative inotropic support, those who underwent on-pump CABG, additional surgical procedures (valves, vascular, etc.), or emergency surgeries were excluded.
QT Interval and Corrected QT Interval (QTc) Measurements
In each patient, a 12-lead ECG was obtained before the surgery and immediately after extubation, in the postoperative period. QT interval and heart rate were detected on these ECGs and recorded. QTc was measured according to the Bazett formula.
Postoperative Monitoring
Patient data were retrospectively analysed for the development of new-onset AF in the postoperative period up to discharge. All patients were monitored continuously using five-lead telemetry in the intensive care unit (ICU) postoperatively. Daily routine ECGs were obtained until discharge from the hospital. In addition, when the patients complained of palpitation, dyspnea, and angina, an additional 12-lead ECG was obtained. The new-onset poAF was defined as the new AF requiring treatment during hospitalization after isolated CABG, as defined by the Society of Thoracic Surgeons Adult Cardiac Surgery Database[11].
Ethical Considerations
The study protocol was approved by the local ethics committee (decision nº: 2020/177, date: 21.07.2020). The study was conducted in accordance with the ethical principles of the Declaration of Helsinki. All patients included in the study were informed and their written consents were taken before the operation.
Statistical Analysis
Data obtained in this study were statistically analyzed using IBM Corp. Released 2016, IBM SPSS Statistics for Windows, Version 24, Armonk, NY: IBM Corp statistical software. To calculate the sample width, power of analysis for each variable was determined by taking at least 0.80 and Type 1 error 0.05. Descriptive statistics for continuous variables are expressed as median, mean, standard deviation, minimum, and maximum; and descriptive statistics for categorical variables, as numbers and percentages.
Kolmogorov-Smirnov and Shapiro-Wilk tests were used to check whether the measurement averages were normally distributed and nonparametric tests were applied since the measurement values of the variables were not normally distributed. Mann-Whitney U Test was used to compare the measurements of the AF groups. Wilcoxon test was used for nonparametric variables in comparisons of dependent variables.
In order to determine predictive values of measurements according to AF groups, the area under the curve (AUC), sensitivity-specificity values, and cutoff values were determined by receiver operating characteristic (ROC) analysis. Chi-square test was used to determine the relationship between categorical variables. P<0.05 values were considered statistically significant.
RESULTS
The present study included 167 consecutive patients who had no prior history of AF and underwent OPCAB. Thirty-seven of 167 patients (22.1%) developed AF before the discharge from the hospital in the postoperative period. Mean age was 66.7±9.0 years in the poAF (+) group and 61.7±10.4 years in the poAF (-) group. The mean age was statistically significantly higher in the poAF (+) group compared to poAF (-) group (P=0.007). Of the 37 patients who developed poAF, nine (24.3%) were female and 28 (75.7%) were male. Of the 130 patients without poAF, 24 (18.5%) were female and 106 (%81.5) were male. No significant difference was found between both groups in terms of gender distribution (P>0.05). In addition, there was no significant difference between the groups in terms of BMI (P>0.05). And no statistically significant difference was found between both groups in terms of frequency of comorbidities (diabetes mellitus, hypertension, hyperlipidemia, COPD, myocardial infarction, and smoking status) and drug use (beta blocker therapy, statin therapy, ACE-I/ARB therapy) (for all P>0.05) (Table 1).
Table 1.
Preoperative clinical characteristics of the groups.
| poAF (-) group | poAF (+) group | P-value | ||
|---|---|---|---|---|
| n=130 | n=37 | |||
| Age (years) | 61.7±10.4 | 66.7±9.0 | 0.007* | |
| BMI | 27.7±5.0 | 28.6±4.7 | 0.331* | |
| Gender, n (%) | Female | 24 (18.5) | 9 (24.3) | 0.429# |
| Male | 106 (81.5) | 28 (75.7) | ||
| Diabetes mellitus, n (%) | - | 73 (56.2) | 16 (43.2) | 0.165# |
| + | 57 (43.8) | 21 (56.8) | ||
| Hypertension, n (%) | - | 69 (53.1) | 16 (43.2) | 0.291# |
| + | 61 (46.9) | 21 (56.8) | ||
| Smoking, n (%) | - | 67 (51.5) | 19 (51.4) | 0.984# |
| + | 63 (48.5) | 18 (48.6) | ||
| Hyperlipidemia, n (%) | - | 46 (35.4) | 15 (40.5) | 0.566# |
| + | 84 (64.6) | 22 (59.5) | ||
| COPD, n (%) | - | 123 (94.6) | 34 (91.9) | 0.538# |
| + | 7 (5.4) | 3 (8.1) | ||
| Myocardial infarction, n (%) | - | 92 (70.8) | 21 (56.8) | 0.108# |
| + | 38 (29.2) | 16 (43.2) | ||
| Beta blocker therapy, n (%) | - | 120 (92.4) | 32 (86.5) | 0.428# |
| + | 10 (7.6) | 5 (13.5) | ||
| Statin therapy, n (%) | - | 42 (32.4) | 9 (24.3) | 0.527# |
| + | 88 (67.6) | 28 (75.7) | ||
| ACE-I/ARB therapy, n (%) | - | 57 (43.9) | 15 (40.6) | 0.608# |
| + | 73 (56.1) | 22 (59.4) | ||
Significance levels according to Mann-Whitney U test results.
Significance levels according to the Chi-square test results.
ACE-I=angiotensin-converting enzyme inhibitors; ARB=angiotensin receptor blockers; BMI=body mass index; COPD=chronic obstructive pulmonary disease; poAF=postoperative atrial fibrillation
When pre- and postoperative laboratory data and clinical findings were evaluated, no statistically significant difference was observed between both groups in terms of preoperative left ventricular ejection fraction, preoperative left atrial diameter, preoperative hemoglobin (Hb), preoperative hematocrit (Hct), preoperative red cell distribution width (RDW), preoperative mean platelet volume (MPV), preoperative C-reactive protein, preoperative troponin I, postoperative Hb, postoperative Hct, and postoperative troponin I (for all P>0.05).
On the contrary, preoperative QT (P<0.001), preoperative QTc (P<0.001), postoperative QT (P=0.005), and postoperative QTc values were statistically significantly higher in the poAF (+) group compared to the poAF (-) group (Table 2, Figure 1).
Table 2.
Laboratory and other parameters of the groups.
| poAF (-) group | poAF (+) group | *P-value | |
|---|---|---|---|
| n=130 | n=37 | ||
| Preoperative LVEF | 51.8±9.0 | 48.7±9.1 | 0.053 |
| Preoperative left atrial diameter | 38.2±5.7 | 40.1±6.0 | 0.083 |
| Preoperative QT | 407.5±27.1 | 438.5±45.8 | < 0.001 |
| Preoperative QTc | 419.1±14.5 | 448.5±26.6 | < 0.001 |
| Postoperative QT | 416.3±48.3 | 439.2±45.8 | 0.005 |
| Postoperative QTc | 419.8±12.5 | 452.0±23.3 | < 0.001 |
| Preoperative Hb | 13.4±2.0 | 13.7±2.1 | 0.577 |
| Preoperative Hct | 40,8±5,9 | 41,3±6,0 | 0.906 |
| Preoperative RDW | 16.3±2.2 | 16.4±2.7 | 0.857 |
| Preoperative MPV | 8.2±1.6 | 8.2±1.4 | 0.740 |
| Preoperative CRP | 18.0±29.6 | 13.0±27.4 | 0.140 |
| Preoperative troponin I | 980.3±3095.1 | 350.6±849.0 | 0.900 |
| Postoperative Hb | 10.6±1.3 | 10.9±1.4 | 0.389 |
| Postoperative Hct | 31.6±3.7 | 32.5±4.7 | 0.480 |
| Postoperative troponin I | 6961.6±13958.9 | 8311.6±14162.2 | 0.197 |
Significance levels according to Mann-Whitney U test results.
CRP=C-reactive protein; Hb=hemoglobin; Hct=hematocrit; LVEF=left ventricular ejection fraction; MPV=mean platelet volume; poAF=postoperative atrial fibrillation; QTc=corrected QT interval; RDW=red cell distribution width
Fig 1.
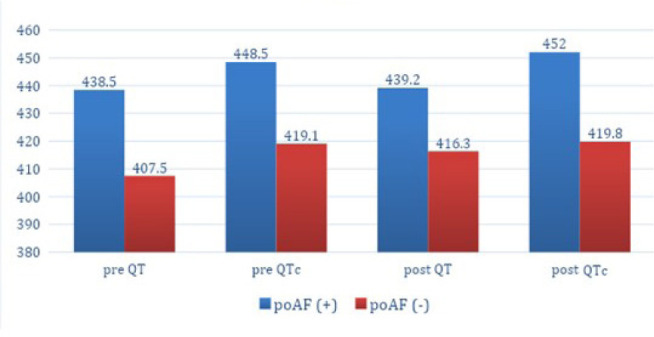
Pre- and postoperative QT and corrected QT interval (QTc) values of postoperative atrial fibrillation (poAF) (+) and poAF (-) groups.
When operative and postoperative characteristics of CABG operations were evaluated, no statistically significant difference was found between poAF (+) and poAF (-) groups in terms of heart rate, forced expiratory volume in the first second/forced vital capacity, bypassed vessels, transfusion (unit), length of stay in ICU (hours), hospital stay (days), extubation time (hours), postoperative lactate, the need for transfusion, the presence of intra-aortic balloon pump, the need for inotropic support, neurologic deficit, and mortality (for all P>0.05). On the other hand, the amount of total drainage was statistically significantly higher in the poAF (+) group than in the poAF (-) group (P=0.034) (Table 3).
Table 3.
Operative and postoperative data of the groups.
| poAF (-) group | poAF (+) group | P-value | ||
|---|---|---|---|---|
| n=130 | n=37 | |||
| Heart rate | 64.2±6.9 | 64.3±9.4 | 0.869* | |
| FEV1/FVC | 77.1±10.6 | 74.9±13.3 | 0.344* | |
| Bypassed vessel | 4.6±1.0 | 4.5±1.1 | 0.386* | |
| Transfusion (unit) | 2.0±1.4 | 1.7±1.0 | 0.444* | |
| Total drainage | 579.1±298.1 | 675.8±279.4 | 0.034* | |
| Intensive care unit (hours) | 69.6±45.0 | 71.4±42.3 | 0.623* | |
| Hospital stay (days) | 3.3±2.2 | 3.0±2.0 | 0.635* | |
| Extubation time (hours) | 6.3±3.0 | 5.9±1.7 | 0.678* | |
| Postoperative lactate | 1.5±0.7 | 2.3±3.1 | 0.508* | |
| Transfusion | - | 72 (56.3) | 22 (59.5) | 0.728# |
| + | 56 (43.8) | 15 (40.5) | ||
| IABP | - | 123 (94.6) | 35 (94.6) | 0.996# |
| + | 7 (5.4) | 2 (5.4) | ||
| Inotropic support | - | 109 (83.8) | 27 (73.0) | 0.133# |
| + | 21 (16.2) | 10 (27.0) | ||
| Neurologic deficit | - | 127 (97.7) | 36 (97.3) | 0.890# |
| + | 3 (2.3) | 1 (2.7) | ||
| Mortality | + | 2 (1.5) | 1 (2.7) | 0.638# |
| - | 128 (98.5) | 36 (97.3) | ||
Significance levels according to Mann-Whitney U test results.
Significance levels according to the Chi-square test results.
FEV1=forced expiratory volume in the first second; FVC=forced vital capacity; IABP=intra-aortic balloon pump; poAF=postoperative atrial fibrillation
Risk factors for the development of poAF were evaluated by univariate logistic regression analysis. Age (odds ratio [95% confidence interval, CI] 1.062 [1.015-1.111], P=0.009) and postoperative QTc (odds ratio [95% CI] 1.147 [1.064-1.238], P=0.001) were detected to be significantly higher for poAF. In multivariate logistic regression analysis, only postoperative QTc was found to be an independent predictor for the development of poAF (odds ratio [95% CI] 1.093 [1.063-1.122], P=0.001) (Table 4).
Table 4.
Univariate and multivariate logistic regression analyses of independent parameters for atrial fibrillation.
| Univariate | Multivariate | |||
|---|---|---|---|---|
| Variables | Odds ratio (95% CI) | P-value | Odds ratio (95% CI) | P-value |
| Age | 1.062 (1.015-1.111) | 0.009 | 1.013 (0.961-1.069) | 0.621 |
| Postoperative QTc | 1.147 (1.064-1.238) | 0.001 | 1.093 (1.063-1.122) | 0.001 |
| Preoperative QTc | 0.973 (0.905-1.045) | 0.448 | ||
| Postoperative QT | 0.994 (0.980-1.009) | 0.438 | ||
| Preoperative QT | 0.992 (0.968-1.017) | 0.540 | ||
| LVEF | 0.979 (0.921-1.041) | 0.500 | ||
| LA diameter | 1.095 (0.997-1.203) | 0.058 | ||
| Total drainage | 0.999 (0.997-1.002) | 0.564 | ||
CI=confidence interval; LA=left atrial; LVEF=left ventricular ejection fraction; QTc=corrected QT interval
In the ROC curve analysis we performed to determine cutoff values, sensitivity and specificity values of QT and QTc, and AUC cutoff, sensitivity and specificity values were calculated for preoperative QT, preoperative QTc, postoperative QT, and postoperative QTc in predicting poAF at 95% CI and are shown in Table 5 and Figure 2. In addition, after ROC analysis of four QT values was performed, a pairwise analysis was also performed for the ROC curves. The results of pairwise analysis are shown in Table 6 and the result of cutoff values, positive predictive value, and negative predictive value are shown in Table 7.
Table 5.
Area under the curve (AUC), cutoff value, and diagnostic tests according to atrial fibrillation groups.
| Test results | AUC | Standard error | P-value | Cutoff | Sensitivity | Specificity | 95% Confidence interval | |
|---|---|---|---|---|---|---|---|---|
| Variables | Lower | Upper | ||||||
| Preoperative QT | 0.728 | 0.057 | 0.001 | 419 | 0.703 | 0.692 | 0.617 | 0.839 |
| Preoperative QTc | 0.814 | 0.057 | 0.001 | 434.5 | 0.784 | 0.869 | 0.703 | 0.925 |
| Postoperative QT | 0.651 | 0.056 | 0.005 | 423.5 | 0.595 | 0.585 | 0.541 | 0.76 |
| Postoperative QTc | 0.845 | 0.051 | 0.001 | 431 | 0.811 | 0.885 | 0.744 | 0.945 |
QTc=corrected QT interval
Fig 2.
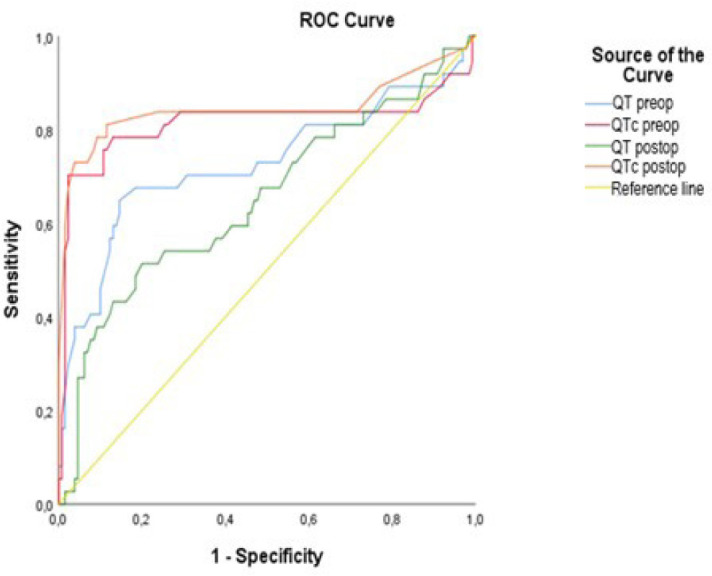
Receiver operating characteristic (ROC) curve and the area under the curve for QT and corrected QT interval (QTc) to predict postoperative atrial fibrillation.
Table 6.
Paired comparison results of variables with significant cutoff values after ROC analysis.
| N | Mean | Standard deviation | Min. | Max. | *P-value | ||
|---|---|---|---|---|---|---|---|
| Preoperative QT | AF (+) | 130 | 407,4923 | 27,11281 | 290 | 510 | < 0,001 |
| AF (-) | 37 | 438,5135 | 45,84431 | 348 | 538 | ||
| Total | 167 | 414,3653 | 34,55454 | 290 | 538 | ||
| Preoperative QTc | AF (+) | 130 | 419,1154 | 14,52271 | 374 | 474 | < 0,001 |
| AF (-) | 37 | 448,4865 | 26,62666 | 389 | 491 | ||
| Total | 167 | 425,6228 | 21,61788 | 374 | 491 | ||
| Postoperative QT | AF (+) | 130 | 416,3 | 48,32363 | 168 | 592 | 0,011 |
| AF (-) | 37 | 439,2162 | 45,82463 | 322 | 537 | ||
| Total | 167 | 421,3772 | 48,59218 | 168 | 592 | ||
| Postoperative QTc | AF (+) | 130 | 419,8 | 12,48093 | 380 | 462 | <0,001 |
| AF (-) | 37 | 452 | 23,29998 | 401 | 486 | ||
| Total | 167 | 426,9341 | 20,46188 | 380 | 486 | ||
Significance levels according to independent t-test results.
AF=atrial fibrillation; QTc=corrected QT interval; ROC=receiver operating characteristic
Table 7.
Cutoff levels for QT and QTc preoperative and postoperative measurements in atrial fibrillation groups.
| Cutoff | Sensitivity % (95% CI) | Sensitivity % (95% CI) | PPV % | NPV % | AUC | P-value | |
|---|---|---|---|---|---|---|---|
| Preoperative QT | 419,0 | 70,3 (59,4-79,3) | 69,2 (41,3-87,8) | 39,4 | 89,1 | 0,728 | 0,001 |
| Preoperative QTc | 434,5 | 78,4 (68,5-86,1) | 86,9 (59,1-96,8) | 65,1 | 9,34 | 0,814 | 0,001 |
| Postoperative QT | 423,5 | 59,5 (48,4-69,7) | 58,5 (32,1-80,8) | 29 | 83,5 | 0,651 | 0,005 |
| Postoperative QTc | 431,0 | 81,1 (71,0-88,3) | 88,5 (60,9-97,4) | 66,7 | 94,3 | 0,845 | 0,001 |
AUC=area under the curve; CI=confidence interval; NPV=negative predictive value; PPV=positive predictive value; QTc=corrected QT interval
DISCUSSION
In the present study, preoperative QT, preoperative QTc, postoperative QT, and postoperative QTc interval measurements were significantly longer in patients who underwent OPCAB surgery and developed AF in the postoperative period. In addition, advanced age was found to be an independent risk factor for the development of poAF. In a study by Velioglu et al.[24] investigating the development of poAF after beating heart CABG, age was significantly higher in the poAF (+) group. In a study by Turkkan and Bozbeyoğlu, conducted on 311 patients undergoing elective CABG, poAF (+) patients were significantly older than poAF (-) patients[25]. In another study, the rate of patients aged > 85 years was significantly higher in the poAF (+) group[26]. And in a study by Lotfi et al.[27], the mean age was statistically significantly higher in poAF (+) patients. As is seen, older age is a risk factor of developing poAF in most of the studies. In addition, age is the only risk factor that has been systematically proven in the literature[28].
No statistically significant difference was found between poAF (+) and poAF (-) groups in terms of comorbidities (diabetes mellitus, hypertension, hyperlipidemia, COPD, myocardial infarction, and smoking status) in the present study. Conversely, there are studies in the literature that have reported several comorbidities as risk factors for poAF including a history of prior AF, hypertension, congestive heart failure, COPD, chronic lung disease, and chronic kidney disease[17,29]. However, many of these studies are retrospectively designed and have a relatively short follow-up. Findings of the studies regarding other possible preoperative risk factors are inconsistent[30-32]. Therefore, we still do not have an accurate understanding about the association between comorbidities and poAF. For example, unlike the other studies, Akintoye et al.[33] found that the frequency of hypertension and prior history of AF were significantly higher in poAF (-) patients.
In this study, no correlation was found between preoperative RDW and preoperative MPV values and poAF development. In another previous study, it was found that preoperative RDW and preoperative MPV levels did not have a predictive value for poAF in patients undergoing OPCAB surgery[34].
Studies have investigated routine ECG parameters as potential predictors of incident AF. Perez et al.[35] identified several P-wave characteristics - including P-wave index - that independently increased the risk of incident AF.
The prolonged QT interval, previously thought to be associated only with ventricular arrhythmias, has been associated with an increased risk of AF incidence[20]. In a study conducted to determine the characteristics of cardiac autonomic modulation and repolarization, preoperative QT and QTc intervals were found to be longer in the group that developed poAF[36].
Nielsen et al.[21] investigated the development of AF in subjects who were followed for an average of 5.7 years in a study in the general population. Compared to the reference group (40th to < 60th percentile, 411 to 419 ms), in the 99th percentile and over (≥ 464 ms) and 1st percentile and below (≤ 372 ms) groups, there was a statistically significant increased risk of AF in QTcFram (QTc calculated using the Framingham formula) intervals. When lone AF subgroup analysis was performed, it was revealed that the relationship between the QTc interval and the lone AF result was at least stronger for the QTc intervals in the upper range compared to AF.
Patel et al.[37] compared the QT interval components (QRS duration and JT interval) with the incidence of AF. In the study in which 4,181 participants were analyzed, it was found that the JT interval is a more important marker of AF risk in the QT interval among other personal delays[38]. In another study with 14,625 participants, 1,505 (10.3%) developed AF in mean 17.6 years of follow-up. When the ECG parameters of patients who developed AF were examined, QT-interval components involved
Limitations
Retrospective study design and lack of follow-up after discharge are important limitations of the study. In addition, patients who developed short-term AF attacks may not be detected because there was no continuous ECG monitoring. Since it is performed without excluding some risk factors for the development of AF, we cannot clearly express the relationship between the QT interval and poAF. Further studies are needed to support our findings.
CONCLUSION
In this study, a strong relationship was detected between QT interval prolongation and poAF. Qt interval measurement is a simple and cost-free process. It is clear that there is a need for a prospective, randomized studies, with and larger number of patients to prove the relationship between the QT interval and its components and poAF. If this relationship can be detected, more effective preventive and therapeutic strategies can be developed as patients at risk for the development of poAF can be identified in advance.
in repolarization, but not depolarization, exhibited significant associations with incident AF. Kinoshita et al.[39] determined that preoperative QT interval is an independent predictor of overall death and sudden cardiac death after coronary bypass surgery.
In the present study, we found that preoperative QT (cutoff: 419, sensitivity: 0.703, specificity: 0.692), preoperative QTc (cutoff: 434.5, sensitivity: 0.784, specificity: 0.869), postoperative QT (cutoff: 423.5, sensitivity: 0.595, specificity: 0.585), and postoperative QTc (cutoff: 419, sensitivity: 0.703, specificity: 0.692) were potential predictors of poAF. However, our results should be supported by larger series prospective studies.
Footnotes
No financial support.
This study was carried out at the Department of Cardiovascular Surgery, Faculty of Medicine, Abant Izzet Baysal University, Bolu, Turkey.
No conflict of interest.
| Authors’ Roles & Responsibilities | |
|---|---|
| GK | Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved; final approval of the version to be published |
| ERU | Drafting the work or revising it critically for important intellectual content; final approval of the version to be published |
REFERENCES
- 1.Hogue CW Jr, Creswell LL, Gutterman DD, Fleisher LA. American College of Chest Physicians. Epidemiology, mechanisms, and risks: American college of chest physicians guidelines for the prevention and management of postoperative atrial fibrillation after cardiac surgery. Chest. 2005;128(2 Suppl):9S–16S. doi: 10.1378/chest.128.2_suppl.9s. [DOI] [PubMed] [Google Scholar]
- 2.Mitchell LB; CCS Atrial Fibrillation Guidelines Committee Canadian cardiovascular society atrial fibrillation guidelines 2010: prevention and treatment of atrial fibrillation following cardiac surgery. Can J Cardiol. 2011;27(1):91–97. doi: 10.1016/j.cjca.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 3.Lahey SJ, Campos CT, Jennings B, Pawlow P, Stokes T, Levitsky S. Hospital readmission after cardiac surgery. Does "fast track" cardiac surgery result in cost saving or cost shifting? Circulation. 1998;98(19 Suppl):II35–40. [PubMed] [Google Scholar]
- 4.Aksoy F, Uysal D, Ibrişim E. Relationship between c-reactive protein/albumin ratio and new-onset atrial fibrillation after coronary artery bypass grafting. Rev Assoc Med Bras (1992) 2020;66(8):1070–1076. doi: 10.1590/1806-9282.66.8.1070. [DOI] [PubMed] [Google Scholar]
- 5.Ronsoni RM, Souza AZM, Leiria TLL, Lima GG. Update on management of postoperative atrial fibrillation after cardiac surgery. Braz J Cardiovasc Surg. 2020;35(2):206–210. doi: 10.21470/1678-9741-2019-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cerit L, Özcem B, Cerit Z, Duygu H. Preventive effect of preoperative vitamin D supplementation on postoperative atrial fibrillation. Braz J Cardiovasc Surg. 2018;33(4):347–352. doi: 10.21470/1678-9741-2018-0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aksoy F, Uysal D, Ibrişim E. Predictive values of C-reactive protein/albumin ratio in new-onset atrial fibrillation after coronary artery bypass grafting. Rev Assoc Med Bras (1992) 2020;66(8):1049–1056. doi: 10.1590/1806-9282.66.8.1049. [DOI] [PubMed] [Google Scholar]
- 8.Agrawal DK, Boosani CS. Gene therapy to keep the QT rhythms "on the QT". J Thorac Cardiovasc Surg. 2017;154(5):1641–1643. doi: 10.1016/j.jtcvs.2017.07.005. [DOI] [PubMed] [Google Scholar]
- 9.Lee SH, Kang DR, Uhm JS, Shim J, Sung JH, Kim JY, et al. New-onset atrial fibrillation predicts long-term newly developed atrial fibrillation after coronary artery bypass graft. Am Heart J. 2014;167(4):593–600.e1. doi: 10.1016/j.ahj.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Filardo G, Hamilton C, Hebeler RF Jr. Hamman B, Grayburn P. New-onset postoperative atrial fibrillation after isolated coronary artery bypass graft surgery and long-term survival. Circ Cardiovasc Qual Outcomes. 2009;2(3):164–169. doi: 10.1161/CIRCOUTCOMES.108.816843. [DOI] [PubMed] [Google Scholar]
- 11.Turagam MK, Mirza M, Werner PH, Sra J, Kress DC, Tajik AJ, et al. Circulating biomarkers predictive of postoperative atrial fibrillation. Cardiol Rev. 2016;24(2):76–87. doi: 10.1097/CRD.0000000000000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elahi M, Hadjinikolaou L, Galiñanes M. Incidence and clinical consequences of atrial fibrillation within 1 year of first-time isolated coronary bypass surgery. Circulation. 2003;108(Suppl 1):II207–12. doi: 10.1161/01.cir.0000089188.45285.fd. [DOI] [PubMed] [Google Scholar]
- 13.Villareal RP, Hariharan R, Liu BC, Kar B, Lee VV, Elayda M, et al. Postoperative atrial fibrillation and mortality after coronary artery bypass surgery. J Am Coll Cardiol. 2004;43(5):742–748. doi: 10.1016/j.jacc.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 14.Yüksel A, Velioglu Y, Tecimer ME, Kan II, Bicer M, Gurbuz O, et al. Is there any relationship of postoperative atrial fibrillation with the use of blood products and postoperative hemoglobin levels in patients undergoing coronary artery bypass grafting? Medicine Science. 2019;8(1):16–20. doi: 10.5455/MEDSCIENCE.2018.07.8861. [DOI] [Google Scholar]
- 15.Yadava M, Hughey AB, Crawford TC. Postoperative atrial fibrillation: incidence, mechanisms, and clinical correlates. Heart Fail Clin. 2016;12(2):299–308. doi: 10.1016/j.hfc.2015.08.023. [DOI] [PubMed] [Google Scholar]
- 16.Shen J, Lall S, Zheng V, Buckley P, Damiano RJ Jr, Schuessler RB. The persistent problem of new-onset postoperative atrial fibrillation: a single-institution experience over two decades. J Thorac Cardiovasc Surg. 2011;141(2):559–570. doi: 10.1016/j.jtcvs.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mathew JP, Fontes ML, Tudor IC, Ramsay J, Duke P, Mazer CD, et al. A multicenter risk index for atrial fibrillation after cardiac surgery. JAMA. 2004;291(14):1720–1729. doi: 10.1001/jama.291.14.1720. [DOI] [PubMed] [Google Scholar]
- 18.Zaman AG, Archbold RA, Helft G, Paul EA, Curzen NP, Mills PG. Atrial fibrillation after coronary artery bypass surgery: a model for preoperative risk stratification. Circulation. 2000;101(12):1403–1408. doi: 10.1161/01.cir.101.12.1403. [DOI] [PubMed] [Google Scholar]
- 19.Kaw R, Hernandez AV, Masood I, Gillinov AM, Saliba W, Blackstone EH. Short- and long-term mortality associated with new-onset atrial fibrillation after coronary artery bypass grafting: a systematic review and meta-analysis. J Thorac Cardiovasc Surg. 2011;141(5):1305–1312. doi: 10.1016/j.jtcvs.2010.10.040. [DOI] [PubMed] [Google Scholar]
- 20.Mandyam MC, Soliman EZ, Alonso A, Dewland TA, Heckbert SR, Vittinghoff E, et al. The QT interval and risk of incident atrial fibrillation. Heart Rhythm. 2013;10(10):1562–1568. doi: 10.1016/j.hrthm.2013.07.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nielsen JB, Graff C, Pietersen A, Lind B, Struijk JJ, Olesen MS, et al. J-shaped association between QTc interval duration and the risk of atrial fibrillation: results from the Copenhagen ECG study. J Am Coll Cardiol. 2013;61(25):2557–2564. doi: 10.1016/j.jacc.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 22.Soliman EZ, Howard G, Cushman M, Kissela B, Kleindorfer D, Le A, et al. Prolongation of QTc and risk of stroke: The REGARDS (REasons for Geographic and Racial Differences in Stroke) study. J Am Coll Cardiol. 2012;59(16):1460–1467. doi: 10.1016/j.jacc.2012.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson JN, Tester DJ, Perry J, Salisbury BA, Reed CR, Ackerman MJ. Prevalence of early-onset atrial fibrillation in congenital long QT syndrome. Heart Rhythm. 2008;5(5):704–709. doi: 10.1016/j.hrthm.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Velioglu Y, Yuksel A. Predictors of postoperative atrial fibrillation after beating-heart coronary artery bypass surgery: is cardiopulmonary bypass a risk factor? Acta Cardiol Sin. 2019;35(5):468–475. doi: 10.6515/ACS.201909_35(5).20190325A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Turkkan C and Bozbeyoglu E Impact of Electrocardiographic Diastolic Parameters and Diastolic ECG Index in Predicting Postoperative Atrial Fibrillation. Int J Basic Clin Studies. 2018;7(1):51–58. [Google Scholar]
- 26.Sigurdsson MI, Longford NT, Heydarpour M, Saddic L, Chang TW, Fox AA, et al. Duration of postoperative atrial fibrillation after cardiac surgery is associated with worsened long-term survival. Ann Thorac Surg. 2016;102(6):2018–2026. doi: 10.1016/j.athoracsur.2016.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lotfi A, Wartak S, Sethi P, Garb J, Giugliano GR. Postoperative atrial fibrillation is not associated with an increase risk of stroke or the type and number of grafts: a single-center retrospective analysis. Clin Cardiol. 2011;34(12):787–790. doi: 10.1002/clc.21001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Perrier S, Meyer N, Hoang Minh T, Announe T, Bentz J, Billaud P, et al. Predictors of atrial fibrillation after coronary artery bypass grafting: a bayesian analysis. Ann Thorac Surg. 2017;103(1):92–97. doi: 10.1016/j.athoracsur.2016.05.115. [DOI] [PubMed] [Google Scholar]
- 29.Sun X, Boyce SW, Hill PC, Bafi AS, Xue Z, Lindsay J, et al. Association of body mass index with new-onset atrial fibrillation after coronary artery bypass grafting operations. Ann Thorac Surg. 2011;91(6):1852–1858. doi: 10.1016/j.athoracsur.2011.03.022. [DOI] [PubMed] [Google Scholar]
- 30.Magee MJ, Herbert MA, Dewey TM, Edgerton JR, Ryan WH, Prince S, et al. Atrial fibrillation after coronary artery bypass grafting surgery: development of a predictive risk algorithm. Ann Thorac Surg. 2007;83(5):1707–1712. doi: 10.1016/j.athoracsur.2006.12.032. discussion 1712. [DOI] [PubMed] [Google Scholar]
- 31.Hernandez AV, Kaw R, Pasupuleti V, Bina P, Ioannidis JP, Bueno H, et al. Association between obesity and postoperative atrial fibrillation in patients undergoing cardiac operations: a systematic review and meta-analysis. Ann Thorac Surg. 2013;96(3):1104–1116. doi: 10.1016/j.athoracsur.2013.04.029. [DOI] [PubMed] [Google Scholar]
- 32.Tayyareci Y, Yildirimtürk O, Aytekin V, Memic K, Behramoglu F, Demiroglu IC, et al. Preoperative left atrial mechanical dysfunction predicts postoperative atrial fibrillation after coronary artery bypass graft operation - a velocity vector imaging-based study - Circ J. 2010;74(10):2109–2117. doi: 10.1253/circj.cj-10-0197. [DOI] [PubMed] [Google Scholar]
- 33.Akintoye E, Sellke F, Marchioli R, Tavazzi L, Mozaffarian D. Factors associated with postoperative atrial fibrillation and other adverse events after cardiac surgery. J Thorac Cardiovasc Surg. 2018;155(1):242–51.e10. doi: 10.1016/j.jtcvs.2017.07.063. [DOI] [PubMed] [Google Scholar]
- 34.Ozsin KK, Sanri US, Toktas F, Yavuz S. Relationship between red cell distribution width and mean platelet volume with new onset atrial fibrillation afteroff-pump coronary artery bypass grafting. Bratisl Lek Listy. 2018;119(6):335–340. doi: 10.4149/BLL_2018_063. [DOI] [PubMed] [Google Scholar]
- 35.Perez MV, Dewey FE, Marcus R, Ashley EA, Al-Ahmad AA, Wang PJ, et al. Electrocardiographic predictors of atrial fibrillation. Am Heart J. 2009;158(4):622–628. doi: 10.1016/j.ahj.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 36.Kališnik JM, Hrovat E, Hrastovec A, Avbelj V, Žibert J, Geršak B. Severe cardiac autonomic derangement and altered ventricular repolarization pave the way to postoperative atrial fibrillation. Innovations (Phila) 2015;10(6):398–405. doi: 10.1097/IMI.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 37.Patel N, O'Neal WT, Whalen SP, Soliman EZ. The association of QT interval components with atrial fibrillation. Ann Noninvasive Electrocardiol. 2018;23(2):e12467. doi: 10.1111/anec.12467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Roberts JD, Soliman EZ, Alonso A, Vittinghoff E, Chen LY, Loehr L, et al. Electrocardiographic intervals associated with incident atrial fibrillation: dissecting the QT interval. Heart Rhythm. 2017;14(5):654–660. doi: 10.1016/j.hrthm.2017.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kinoshita T, Asai T, Suzuki T, Matsubayashi K, Horie M. Time course and prognostic implications of QT interval in patients with coronary artery disease undergoing coronary bypass surgery. J Cardiovasc Electrophysiol. 2012;23(6):645–649. doi: 10.1111/j.1540-8167.2011.02244.x. [DOI] [PubMed] [Google Scholar]


