Abstract
Long-term insomnia affects the normal life and work of individuals and increases the risk of various health problems, including mental illness. Therefore, there is an urgent need for an efficient and safe treatment for improving sleep. In this study, we report the case a 52-year-old woman who received repetitive transcranial magnetic stimulation (rTMS) combined with transcranial direct current stimulation (tDCS) after agreeing to publish her case. In order to evaluate the quality of sleep and the stability of emotional symptoms, clinical evaluations were conducted at baseline, after 10 treatment sessions, after 20 treatment sessions, and 1 month after the end of treatment. After completing rTMS combined with tDCS, the patient showed an overall clinical improvement, with clinical changes mainly observed in the Pittsburgh Sleep Quality Index, Hamilton Depression Scale, Hamilton Anxiety Scale scores and polysomnography, and this improvement was maintained 1 month after the intervention. This case provides the first evidence for the feasibility, tolerability, and safety of combined rTMS and tDCS in a patient with chronic insomnia.
Clinical Trial Registration:
Registry: Chinese Clinical Trial Registry; Name: Clinical study of repetitive transcranial magnetic stimulation combined with transcranial direct current stimulation in the treatment of chronic insomnia; URL: http://www.chictr.org.cn/edit.aspx?pid=57440&htm=4; Identifier: ChiCTR ChiCTR2100052681.
Citation:
Zhou Q, Liu Z, Zhao S, et al. Transcranial magnetic stimulation combined with transcranial direct current stimulation in patients with chronic insomnia: a case report. J Clin Sleep Med. 2022;18(12):2871–2873.
Keywords: transcranial magnetic stimulation, transcranial direct current stimulation, chronic insomnia, polysomnography
INTRODUCTION
Insomnia is a subjective experience of dissatisfaction with one’s sleep time and/or quality despite appropriate sleep opportunities and sleep environment, and it affects daytime social function. Chronic insomnia is defined as frequent nocturnal and daytime insomnia symptoms that persist for at least 3 months.1 The incidence of chronic insomnia in the general population is approximately 6–10%.2 Long-term insomnia affects the normal life and work of individuals and increases the risk of various health problems, including mental illness.3,4 With the progress of modern society, people’s work and life pressures are increasing, so the demand for high-quality sleep is also increasing. Therefore, there is an urgent need for an efficient and safe treatment for improving sleep.
Drug therapy and psychotherapy are the most common treatment modalities for chronic insomnia, but newer nondrug interventions, such as repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS), have shown promising results.5,6 rTMS is a safe and noninvasive physical therapy technology for brain function intervention. rTMS treatment improves sleep quality by modulating neuronal excitability and affecting the metabolism of neurotransmitters in the brain.7,8 tDCS effects on psychiatric disorders are the result of the induction of synaptic plasticity that occurs during and after treatment and modulates the dysfunctional neuroplasticity of these disorders.9 For patients with long-term chronic insomnia, simple rTMS stimulation or simple tDCS stimulation have certain curative effects, but the onset is slow and the effect is not very satisfactory. Both rTMS stimulation and tDCS stimulation are used as physical therapy techniques, with different mechanisms of action. Therefore, it is considered to combine the 2 physiotherapies to explore the clinical efficacy of rTMS combined with tDCS in the treatment of insomnia.
Previous studies found that patients with insomnia exhibited increased cortical excitability, decreased intracortical facilitation, and cortical hyperarousal during wakefulness and sleep compared with healthy participants.10 Therefore, we hypothesized that sleep can be improved by modulating the excitability of the cerebral cortex in an individual, but since physical therapy techniques are not widely used in sleep disorders, the optimal regimen for improving sleep is unknown.
REPORT OF CASE
In this study, we report the case of a 52-year-old woman who was diagnosed with insomnia according to International Classification of Sleep Disorders, third edition, criteria for more than 10 years. In the past 3 years, the patient has repeatedly experienced difficulty in falling asleep, poor sleep quality, irritability, palpitations, restlessness, lack of energy during the day, and fatigue, with no mental or nervous system complications.
In order to evaluate the quality of sleep and the stability of emotional symptoms, clinical evaluations were conducted at baseline, after 10 treatment sessions, after 20 treatment sessions, and 1 month after the end of treatment. Assessments included polysomnography, Pittsburgh Sleep Quality Index (PSQI), Hamilton Depression Scale (HAMD), and Hamilton Anxiety Scale (HAMA).
rTMS stimulation was performed first, and a single pulse of TMS was delivered to the motor cortex (M1) via an octagonal coil (Magstim Ltd, Oxford, UK) to confirm the resting motor threshold.
First, a low-frequency, 1-Hz rTMS stimulation of the dorsolateral right prefrontal cortex (midpoint of F4–FP2 according to the 10/20 electroencephalography electrode placement system) was selected. The intensity was 80% of the motor threshold, the stimulation time was 6 seconds, the interval time was 4 seconds, the continuous stimulation was performed 1,800 times, and the total number of pulses was 1,800. Afterward, tDCS stimulation was performed using a battery-powered microprocessor-controlled constant current stimulator (Foc.us Ltd, London, UK), and two 25-cm2 sponge electrodes were used to soak the electrodes in saline. Two-milliampere stimulation (rise/fall of 30 seconds) was given once a day for 20 minutes. The anode was placed over the left prefrontal cortex (F3–FP1), and the cathode was placed over the right prefrontal cortex. The treatment mode was rTMS treatment first and tDCS treatment immediately after the end, once a day for 20 consecutive times, for a total of 20 days of treatment.
After each treatment, the tolerability and safety of rTMS and tDCS, including itching, pain, and skin reactions, were monitored using the Treatment Emergent Symptom Scale.11
The study was approved by the Ethics Committee of Ningbo Kangning Hospital.
DISCUSSION
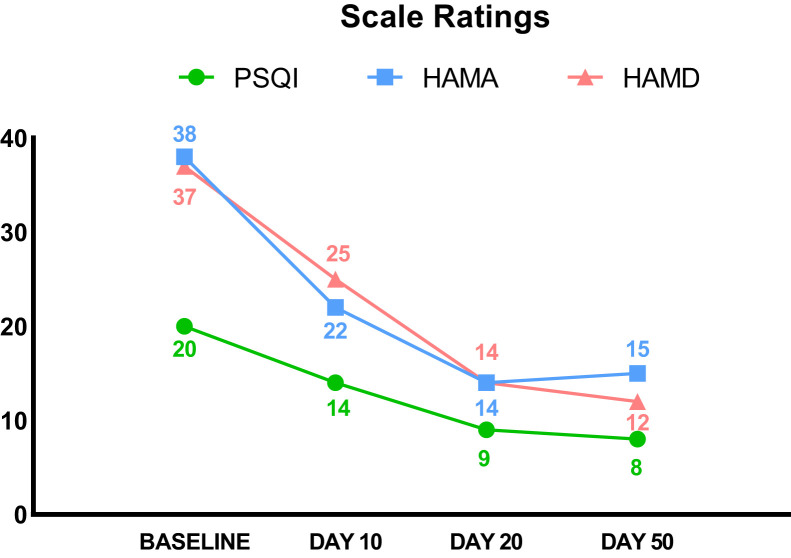
After completing rTMS combined with tDCS, the patient showed an overall clinical improvement, with clinical changes mainly observed in the PSQI, HAMD, HAMA scores and polysomnography, and this improvement was maintained 1 month after the intervention.
The subscore analysis of the 7 dimensions of the PSQI scale revealed the effects of rTMS combined with tDCS treatment on various aspects of sleep status. On the 5 dimensions of sleep quality, sleep onset time, sleep duration, sleep disturbance, and daytime dysfunction, the scores gradually decreased as the number of treatments accumulated and remained stable at one-month follow-up. After 10 days of intervention, the HAMA score decreased by 42% and the HAMD score decreased by 32%. After 20 days of intervention, the HAMA score decreased by 63% and the HAMD score decreased by 62%. After 30 days of follow-up at the end of treatment, the HAMA score decreased by 61% and the HAMD score decreased by 68%.
With the accumulation of the number of treatments, in the polysomnogram, we found that the sleep latency and rapid eye movement (REM) latency gradually shortened and the total sleep time and sleep efficiency gradually increased, which again confirmed the previous results of the PSQI scale (Table 1 and Figure 1).
Table 1.
Clinical outcomes.
| Baseline | Day 10 | Day 20 | Day 50 | |
|---|---|---|---|---|
| PSQI total score | 20 | 14 | 9 | 8 |
| Sleep quality | 3 | 2 | 1 | 1 |
| Sleep latency | 3 | 2 | 1 | 0 |
| Sleep duration | 3 | 2 | 1 | 1 |
| Sleep efficiency | 3 | 2 | 2 | 2 |
| Sleep disturbance | 2 | 1 | 1 | 1 |
| Sleep medication | 3 | 3 | 2 | 2 |
| Daytime dysfunction | 3 | 2 | 1 | 1 |
| HAMA score | 38 | 22 | 14 | 15 |
| HAMD score | 37 | 25 | 14 | 12 |
| Polysomnography | ||||
| Sleep continuity | ||||
| Sleep-onset latency (SOL), min | 41 | 35.9 | 21.5 | 27 |
| Total sleep time (TST), min | 420 | 431 | 502.5 | 521 |
| Sleep efficiency, % | 65.4 | 67.8 | 82.9 | 87.7 |
| Apnea-hypopnea index (AHI), events/h | 8.6 | 5.1 | 5.2 | 4.6 |
| Sleep architecture, % of total sleep time | ||||
| Stage 1 sleep | 15.1 | 5.5 | 10 | 5.4 |
| Stage 2 sleep | 70.2 | 80.9 | 65.9 | 81.7 |
| Slow-wave sleep | 6.1 | 1.4 | 2.2 | 4.7 |
| REM sleep | 8.6 | 12.3 | 21.9 | 8.3 |
| REM sleep parameters | ||||
| REM latency, min | 214.5 | 221.5 | 116.5 | 111 |
HAMA = Hamilton Anxiety Scale, HAMD = Hamilton Depression Scale, PSQI = Pittsburgh Sleep Quality Index, REM = rapid eye movement.
Figure 1. Scale ratings.
HAMA = Hamilton Anxiety Scale, HAMD = Hamilton Depression Scale, PSQI = Pittsburgh Sleep Quality Index.
After all treatments, not only were the objective indicators, such as scale scores, improved but the patient also reported that her sleep conditions were significantly improved and her emotions were relieved. The patient had good tolerance for rTMS combined with tDCS, and no serious adverse reactions were reported. At the end of daily stimulation, only slight and transient skin redness was observed on the scalp, which subsided soon after the stimulation stopped.
This case provides the first evidence for the feasibility, tolerability, and safety of combined rTMS and tDCS in a patient with chronic insomnia. We also used the Treatment Emergent Symptom Scale to assess adverse reactions to ensure the safety of the treatment regimen.
This study found that the decrease in PSQI, HAMA, and HAMD scores and the change in sleep structure, which appeared to be similar to those reported in previous clinical trials.12
Our exploratory research provides a new perspective for the treatment of patients with simple insomnia so that follow-up research can further replicate this intervention. In future studies, we suggest adding more participants to explore different treatment modes, including the number of treatments, duration of treatment, and methods for assessing the effectiveness of treatment options.
DISCLOSURE STATEMENT
All authors have seen and approved the final version of the manuscript being submitted. Work for this report was performed at Ningbo Kangning Hospital, Affiliated Mental Health Center of Ningbo University, Ningbo, Zhejiang, China. The study was supported by grants from the Ningbo Health Branding Subject Fund (PPXK2018-08), the Pharmaceutical Science and Technology Project in Zhejiang Province (2020KY895), the Natural Science Foundation of Ningbo (2018A610292), and the Taizhou Science and Technology Plan Project (20ywa56). The authors report no conflicts of interest.
ABBREVIATIONS
- HAMA
Hamilton Anxiety Scale
- HAMD
Hamilton Depression Scale
- PSQI
Pittsburgh Sleep Quality Index
- REM
rapid eye movement
- rTMS
repetitive transcranial magnetic stimulation
- tDCS
transcranial direct current stimulation
REFERENCES
- 1. American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: : American Academy of Sleep Medicine; ; 2014. . [Google Scholar]
- 2. Morin C , Inoue Y , Kushida C , Poyares D , Winkelman J . Endorsement of European guideline for the diagnosis and treatment of insomnia by the World Sleep Society . Sleep Med . 2021. ; 81 : 124 – 126 . [DOI] [PubMed] [Google Scholar]
- 3. Natsky AN , Vakulin A , Chai-Coetzer CL , et al . Economic evaluation of cognitive behavioural therapy for insomnia (CBT-I) for improving health outcomes in adult populations: a systematic review . Sleep Med Rev. 2020. ; 54 : 101351 . [DOI] [PubMed] [Google Scholar]
- 4. Ferini-Strambi L , Auer R , Bjorvatn B , et al . Insomnia disorder: clinical and research challenges for the 21st century . Eur J Neurol . 2021. ; 28 ( 7 ): 2156 – 2167 . [DOI] [PubMed] [Google Scholar]
- 5. Herrero Babiloni A , Bellemare A , Beetz G , et al . The effects of non-invasive brain stimulation on sleep disturbances among different neurological and neuropsychiatric conditions: a systematic review . Sleep Med Rev. 2021. ; 55 : 101381 . [DOI] [PubMed] [Google Scholar]
- 6. Oroz R , Kung S , Croarkin PE , Cheung J . Transcranial magnetic stimulation therapeutic applications on sleep and insomnia: a review . Sleep Sci Pract . 2021. ; 5 ( 1 ): 3 . [Google Scholar]
- 7. Lefaucheur J , Aleman A , Baeken C , et al . Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS): an update (2014–2018) . Clin Neurophysiol . 2020. ; 131 ( 2 ): 474 – 528 . [DOI] [PubMed] [Google Scholar]
- 8. Collins A , Cheung J , Croarkin P , Kolla B , Kung S . Effects of transcranial magnetic stimulation on sleep quality and mood in patients with major depressive disorder . J Clin Sleep Med . 2022. ; 18 ( 5 ): 1297 – 1305 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kronberg G , Bridi M , Abel T , Bikson M , Parra LC . Direct current stimulation modulates LTP and LTD: activity dependence and dendritic effects . Brain Stimul. 2017. ; 10 ( 1 ): 51 – 58 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Riemann D , Spiegelhalder K , Feige B , et al . The hyperarousal model of insomnia: a review of the concept and its evidence . Sleep Med Rev . 2010. ; 14 ( 1 ): 19 – 31 . [DOI] [PubMed] [Google Scholar]
- 11. Antal A , Alekseichuk I , Bikson M , et al . Low intensity transcranial electric stimulation: safety, ethical, legal regulatory and application guidelines . Clin Neurophysiol . 2017. ; 128 ( 9 ): 1774 – 1809 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhou Q , Yu C , Yu H , Zhang Y , Zhou D . The effects of repeated transcranial direct current stimulation on sleep quality and depression symptoms in patients with major depression and insomnia . Sleep Med . 2020. ; 70 ( 11 ): 17 – 26 . [DOI] [PubMed] [Google Scholar]