Abstract
Background
Gestational diabetes mellitus (GDM) can lead to adverse maternal and fetal outcomes, and early prevention is particularly important for their health, but there is no widely accepted approach to predict it in the early pregnancy. The aim of the present study is to build and evaluate predictive models for GDM using routine indexes, including maternal clinical characteristics and laboratory biomarkers, before 16 gestational weeks.
Methods
A total of 2895 pregnant women were recruited and maternal clinical characteristics and laboratory biomarkers before 16 weeks of gestation were collected from two hospitals. All participants were randomly stratified into the training cohort and the internal validation cohort by the ratio of 7:3. Using multivariable logistic regression analysis, two nomogram models, including a basic model and an extended model, were built. The discrimination, calibration, and clinical validity were used to evaluate the models in the internal validation cohort.
Results
The area under the receiver operating characteristic curve of the basic and the extended model was 0.736 and 0.756 in the training cohort, and was 0.736 and 0.763 in the validation cohort, respectively. The calibration curve analysis showed that the predicted values of the two models were not significantly different from the actual observations (p = 0.289 and 0.636 in the training cohort, p = 0.684 and 0.635 in the internal validation cohort, respectively). The decision-curve analysis showed a good clinical application value of the models.
Conclusions
The present study built simple and effective models, indicating that routine clinical and laboratory parameters can be used to predict the risk of GDM in the early pregnancy, and providing a novel reference for studying the prediction of GDM.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12884-022-05219-4.
Keywords: Gestational diabetes mellitus, Prediction model, Nomogram, Early pregnancy
Background
Gestational diabetes mellitus (GDM) is one of the most common complications of pregnancy, affecting about 2 to 25% of pregnancies worldwide [1]. GDM is defined as glucose intolerance with onset or first recognized during pregnancy [2]. GDM is associated with multiple adverse outcomes for both mother and baby during and beyond pregnancy. For pregnant women, GDM is associated with increased risk of cesarean section, gestational hypertension, and polyhydramnios, and even about 50% of them develop type II diabetes mellitus (DM) within 5 years [3, 4]. As for fetus, the risk of stillbirth, preterm labor, and macrosomia may be increased; moreover, the exposure of embryos or fetuses to a hyperglycemic environment in the uterus may result in increased risk of obesity, diabetes, metabolic syndrome, and other cardiometabolic disorders in the further [5, 6].
Currently, there is no clinical guideline and consensus about testing GDM before 75 g oral glucose tolerance test (OGTT) between 24 and 28 weeks of pregnancy [7]. However, epigenetic changes and abnormal fetal growth before the diagnosis of GDM create a limited time frame for physician intervention [8]. On one hand, testing performed universally on pregnant women may increase a burden to the women without GDM. On the other hand, selective testing in women at high risk for diabetes, GDM may be underdiagnosed [9, 10]. However, there is no international consensus for a preferred screening method or detection strategy. The current guidelines only suggest selective testing based on the maternal clinical risk factors, but this binary approach is limited by its poor sensitivity and specificity. For GDM prediction, some novel biomarkers have been reported as potential predictors, including plasma fatty acid-binding protein 4, sex hormone binding globulin, microRNA, and exosome [11–14], but their low availabilities in clinical practice limit their application. Studies have showed that routine biochemical measures, such as ferritin, glycosylated hemoglobin, triglycerides, and pregnancy-associated plasma protein A (PAPP-A), may be the predictive factors for GDM in the early pregnancy [15–18]. However, these novel biochemical measures have not been thoroughly examined and the equations are complex, which make them difficult to be used in clinic. Several studies have utilized electronic health records or laboratory tests to construct prediction models for GDM [19, 20], which can be used to predict this disease using the medical data of the early pregnancy. However, there is no widely accepted early prediction model for GDM until now.
In the present study, we selected some potential GDM-related parameters from clinical routine examinations to construct a model for predicting GDM based on Nomogram, which may be a valuable supplement and be helpful for improving the screening strategy for GDM.
Methods
Study design
The present study was performed based on the retrospective data, involving 2895 pregnant women who delivered a singleton at the First Affiliated Hospital of Jinan University and Jiangmen Maternity and Child Health Care Hospital from January 2019 to December 2021, which was approved by the Scientific and Ethics Review Committees of the two hospitals. Notably, the Scientific and Ethics Review Committees had waived informed consent for the study as the nature of the present study is retrospective. Two models were built due to the differences of laboratory biomarkers among the two hospitals: the basic model (n = 2895) included all the laboratory biomarkers, including white blood cell count (WBC), neutrophil percentage (NEUT), red blood cell count (RBC), hemoglobin (HGB), hematocrit (HCT), platelet count (PLT), mean platelet volume (MPV), alanine aminotransferase (ALT), aspartate aminotransferase (AST), fasting blood glucose (FBG), creatinine, uric acid, prothrombin time (PT), activated partial thromboplastin time (APTT), fibrinogen (FIB), and PAPP-A, in the two hospitals, while the extended model (n = 2116) added several characteristics, including PT, APTT, FIB, and PAPP-A, which were potentially associated with GDM according to our previous preliminary analysis and collected only from the First Affiliated Hospital of Jinan University. All experiments were carried out in accordance with relevant guidelines and regulations.
Study participants
The inclusion criteria included: (1) age ≥ 18 years, (2) singleton pregnancy, and the exclusion criteria were as follow: (1) primary disease, such as type I or type II DM, chronic hypertension, congenital heart disease, thyroid disorders, and liver or renal insufficiency, (2) incomplete case data records. The OGTT were performed on all participants for the diagnosis of GDM. A pregnant woman was considered to be normotensive if she had a negative OGTT result and had no other pregnancy complications, such as pregnancy hypertension, oligohydramnios, or placental abruption. Additionally, GDM should be diagnosed if one or more values met the International Association of Diabetes and Pregnancy Study Groups’ criteria in 2010 [21]: 75 g OGTT FBG ≥ 5.1 mmol/L, 1 h plasma glucose ≥ 10 mmol/L, or 2 h plasma glucose ≥ 8.5 mmol/L.
Maternal characteristics and laboratory biomarkers
Maternal characteristics and laboratory parameters were obtained from electronic medical records at the first obstetric visit before 16 gestational weeks. Maternal characteristics included age, pre-pregnancy body mass index (BMI), parity, previous GDM history, family history of DM, polycystic ovary syndrome (PCOS), history of adverse pregnancy (such as spontaneous abortions ≥ 3 times, unexplained fetal death at > 20 weeks of gestation, and fetal anomalies despite normal karyotype), and macrosomia in previous gestation. Included laboratory parameters have been mentioned above.
Statistical analysis
Statistical analysis was performed using R 4.0.1 software. Nonnormal distribution continuous data were presented as median and interquartile ranges, and normal distribution continuous data were shown as mean ± standard deviation. Continuous variables were compared with the Welch’s t-test or the Wilcoxon rank sum test. Categorical variables were summarized by counts and percentages and compared by either the Pearson’s chi-square test or Fisher’s exact test. Next, multivariable logistic regression analysis was used to assess the significance of each variable to explore risk factors of GDM. A collinearity test based on a variance inflation factor was performed on the logistic regression models used in the training sets. All participants were randomly stratified into the training cohort and the internal validation cohort by the ratio of 7:3. Internal validation was performed using a bootstrapping with 1000 random samples drawn with replacement. Comparison of the present prediction models and a previously published model was carried out. Area under the receiver operating characteristic (ROC) curve (AUC) was applied to evaluate the differentiation ability of the models. The Hosmer–Lemeshow test was used to reflect the calibration of each model. Moreover, the net reclassification improvement (NRI) and integrated discrimination improvement (IDI) were used to compare the accuracy and comprehensiveness of the models. The consistency of GDM probabilities predicted using the nomogram with the actual situation was evaluated by drawing calibration plots. Finally, we used the decision-curve analysis (DCA) to evaluate the clinical validity of the models [20, 21]. Statistical significance was defined as p ≤ 0.05.
Results
Characteristics of study population
The basic and extended populations respectively included 2895 (1601 normal pregnant women and 1294 patients with GDM) and 2116 pregnant women (1206 normal pregnant women and 910 patients with GDM). Additionally, there were 2026 and 869 participants in the training and validation cohorts in the basic model, and 1481 and 635 participants in the training and validation cohorts in the extended model, respectively. Maternal characteristics and laboratory biomarkers of the basic model and the extended model are shown in Tables 1 and 2, respectively. There was no significant difference on these maternal characteristics, including age, pre-pregnancy BMI, parity, previous GDM history, family history of DM, PCOS, history of adverse pregnancy, and history of macrosomia, and laboratory biomarkers, including WBC, NEUT, RBC, HGB, HCT, PLT, MPV, ALT, AST, FBG, creatinine, uric acid, PT, APTT, FIB, and PAPP-A, between the training and the validation cohorts in both the basic and the extended populations (p > 0.05).
Table 1.
Clinical characteristics and laboratory biomarkers among the basic population
| Variable | Training cohort (n = 2026) |
Validation cohort (n = 869) |
p |
|---|---|---|---|
| Age (year) | 30.0 (27.0–32.0) | 30.0 (27.0–32.0) | 0.753 |
| Nulliparous, n (%) | 0.443 | ||
| No | 1254 (61.9) | 524 (39.7) | |
| Yes | 772 (38.1) | 345 (60.3) | |
| History of GDM, n (%) | 0.276 | ||
| No | 1934 (95.5) | 838 (96.4) | |
| Yes | 92 (4.5) | 31 (3.6) | |
| History of macrosomia, n (%) | 0.099 | ||
| No | 1992 (98.3) | 862 (99.2) | |
| Yes | 34 (1.7) | 7 (0.8) | |
| History of abnormal pregnancy, n (%) | 0.474 | ||
| No | 1943 (95.9) | 828 (95.3) | |
| Yes | 83 (4.1) | 41 (4.7) | |
| Family history of DM, n (%) | 0.709 | ||
| No | 2000 (98.7) | 860 (99.0) | |
| Yes | 26 (1.3) | 9 (1.0) | |
| PCOS, n (%) | 0.911 | ||
| No | 2000 (98.7) | 859 (98.8) | |
| Yes | 26 (1.3) | 10 (1.2) | |
| Pre–pregnancy BMI (kg/m2) | 20.6 (18.9–22.7) | 20.5 (18.9–22.6) | 0.875 |
| WBC (109/L) | 8.9 (7.6–10.4) | 8.8 (7.7–10.1) | 0.420 |
| NEUT (%) | 72.3 (68.1–75.9) | 72.1 (68.1–76.0) | 0.881 |
| RBC (1012/L) | 4.0 (3.8–4.3) | 4.1 (3.8–4.3) | 0.316 |
| HGB (g/L) | 120.5 (114.0–127.0) | 120.4 (114.0–128.0) | 0.872 |
| HCT (%) | 36.0 (34.0–37.9) | 36.0 (34.0–38.0) | 0.457 |
| PLT (109/L) | 241.5 (207.7–278.7) | 238.5 (205.6–273.0) | 0.277 |
| MPV (fL) | 9.6 (8.6–10.4) | 9.5 (8.6–10.4) | 0.977 |
| ALT (U/L) | 12.1 (9.2–18.0) | 12.0 (9.5–17.0) | 0.591 |
| AST (U/L) | 16.0 (13.5–19.0) | 16.0 (13.6–18.4) | 0.494 |
| Creatinine (μmol/L) | 45.7 (41.0–51.0) | 46.0 (41.2–51.4) | 0.283 |
| Uric acid (μmol/L) | 239.0 (202.5–278.2) | 233.0 (203.0–270.0) | 0.202 |
| FBG (mmol/L) | 4.5 (4.2–4.9) | 4.5 (4.3–4.9) | 0.405 |
Abbreviations: GDM Gestational diabetes mellitus, DM Diabetes mellitus, PCOS Polycystic ovary syndrome, BMI Body mass index, WBC White blood cell count, NEUT Neutrophil percentage, RBC Red blood cell count, HGB Hemoglobin, HCT Hematocrit, PLT Platelet count, MPV Mean platelet volume, ALT Alanine aminotransferase, AST Aspartate aminotransferase, FBG Fasting blood glucose
Table 2.
Clinical characteristics and laboratory biomarkers among the extended population
| Variable | Training cohort (n = 1481) |
Validation cohort (n = 635) |
p |
|---|---|---|---|
| Age (year) | 30.0 (27.0–32.0) | 29.0 (27.0–32.0) | 0.438 |
| Nulliparous, n (%) | 0.147 | ||
| No | 898 (60.6) | 407 (64.1) | |
| Yes | 583 (39.4) | 228 (35.9) | |
| History of GDM, n (%) | 0.109 | ||
| No | 1406 (94.9) | 591 (93.1) | |
| Yes | 75 (5.1) | 44 (6.9) | |
| History of macrosomia, n (%) | 0.999 | ||
| No | 1456 (98.3) | 625 (98.4) | |
| Yes | 25 (1.7) | 10 (1.6) | |
| History of abnormal pregnancy, n (%) | 0.845 | ||
| No | 1427 (96.4) | 610 (96.1) | |
| Yes | 54 (3.6) | 25 (3.9) | |
| Family history of DM, n (%) | 0.911 | ||
| No | 1458 (98.4) | 624 (98.3) | |
| Yes | 23 (1.6) | 11 (1.7) | |
| PCOS, n (%) | 1.000 | ||
| No | 1457 (98.4) | 624 (98.3) | |
| Yes | 24 (1.6) | 11 (1.7) | |
| Pre-pregnancy BMI (kg/m2) | 20.5 (18.9–22.7) | 20.6 (18.9–22.6) | 0.631 |
| WBC (109/L) | 9.0 (7.8–10.4) | 9.2 (7.8–10.5) | 0.248 |
| NEUT (%) | 72.8 (68.7–76.5) | 72.9 (68.9–76.6) | 0.384 |
| RBC (1012/L) | 4.0 (3.8–4.3) | 4.0 (3.8–4.3) | 0.816 |
| HGB (g/L) | 121.1 (114.3–128.0) | 121.0 (114.0–128.0) | 0.950 |
| HCT (%) | 36.1 (34.0–38.0) | 36.0 (33.8–37.9) | 0.667 |
| PLT (109/L) | 235.0 (203.0–270.5) | 233.0 (202.5–271.0) | 0.826 |
| MPV (fL) | 9.1 (8.3–10.1) | 9.2 (8.3–10.0) | 0.494 |
| ALT (U/L) | 12.0 (9.0–19.0) | 12.0 (9.0–17.0) | 0.186 |
| AST (U/L) | 16.0 (13.9–20.0) | 16.0 (13.5–19.0) | 0.190 |
| Creatinine (μmol/L) | 46.6 (41.4–53.0) | 46.0 (41.5– 52.5) | 0.416 |
| Uric acid (μmol/L) | 237.0 (204.0–275.0) | 235.0 (201.0–275.3) | 0.793 |
| FBG (mmol/L) | 4.5 (4.2–4.9) | 4.5 (4.2–4.9) | 0.344 |
| PT (s) | 12.3 (10.9–12.8) | 12.3 (10.1–12.8) | 0.812 |
| APTT (s) | 32.6 (29.0–34.9) | 32.3 (28.8–34.6) | 0.213 |
| FIB (mg/dL) | 4.1 (3.7–4.5) | 4.1 (3.7–4.5) | 0.775 |
| PAPP-A (MoM) | 1.1 (0.7–1.6) | 1.1 (0.7–1.6) | 0.330 |
Abbreviations: GDM Gestational diabetes mellitus, DM Diabetes mellitus, PCOS Polycystic ovary syndrome, BMI Body mass index, WBC White blood cell count, NEUT Neutrophil percentage, RBC Red blood cell count, HGB Hemoglobin, HCT Hematocrit, PLT Platelet count, MPV Mean platelet volume, ALT Alanine aminotransferase, AST Aspartate aminotransferase, FBG Fasting blood glucose, PT Prothrombin time, APTT Activated partial thromboplastin time, FIB Fibrinogen, PAPP-A Pregnancy associated plasma protein A
Prediction risk factors of identification
Potential clinical characteristics and laboratory biomarkers for GDM were explored by the univariable logistic regression (Tables 3 and 4). The age of the participants in the GDM group was significantly older than the normal group (p < 0.001). Compared with the normal group, the proportion of nulliparous of the GDM group was significantly lower (p < 0.001), and the proportions of history of macrosomia, history of GDM, family history of DM, and PCOS of the GDM group were significantly higher (p < 0.05). The pre-pregnancy BMI of the GDM group was higher than that of the normal group (p < 0.001). The levels of WBC, RBC, HCT, PLT, MPV, ALT, uric acid, and FBG in the GDM group were significantly higher than those in the normal group, but the level of creatinine of the GDM group was significantly lower (p < 0.05). In the extended population, the levels of PT, APTT, and PAPP-A of the GDM group were significantly lower than those of the normal group, but the level of FIB of the GDM group was significantly higher (p < 0.001). HGB level of the GDM group was higher than that of the normal group in the extended population (p = 0.005), while there was no significant difference in the basic population (p = 0.209).
Table 3.
Univariable analysis of the GDM and the normal groups among the basic population
| Variable | GDM group (n = 909) |
Normal group (n = 1117) |
p |
|---|---|---|---|
| Age (year) | 31.0 (28.0–33.0) | 29.0 (27.0–31.0) | < 0.001 |
| Nulliparous, n (%) | < 0.001 | ||
| No | 610 (67.1) | 644 (42.3) | |
| Yes | 299 (32.9) | 473 (57.7) | |
| History of GDM, n (%) | < 0.001 | ||
| No | 829 (91.2) | 1105 (98.9) | |
| Yes | 80 (8.8) | 12 (1.1) | |
| History of macrosomia, n (%) | 0.001 | ||
| No | 884 (97.2) | 1108 (99.2) | |
| Yes | 25 (2.8) | 9 (0.8) | |
| History of abnormal pregnancy, n (%) | 0.063 | ||
| No | 864 (95.0) | 1080 (96.7) | |
| Yes | 45 (5.0) | 37 (3.3) | |
| Family history of DM, n (%) | < 0.001 | ||
| No | 887 (97.6) | 1113 (99.6) | |
| Yes | 22 (2.4) | 4 (0.4) | |
| PCOS, n (%) | 0.006 | ||
| No | 890 (97.9) | 1110 (99.4) | |
| Yes | 19 (2.1) | 7 (0.6) | |
| Pre–pregnancy BMI (kg/m2) | 21.3 (19.4–23.5) | 20.1 (18.5–21.9) | < 0.001 |
| WBC (109/L) | 9.2 (7.9– 10.8) | 8.7 (7.4–10.0) | < 0.001 |
| NEUT (%) | 72.5 (68.2–76.0) | 72.2 (67.9–75.9) | 0.419 |
| RBC (1012/L) | 4.1 (3.8–4.3) | 4.0 (3.8–4.3) | 0.014 |
| HGB (g/L) | 121.0 (114.0–127.0) | 120.3 (113.0–127.0) | 0.209 |
| HCT (%) | 36.0 (34.0–37.9) | 35.8 (33.7–37.9) | 0.012 |
| PLT (109/L) | 245.4 (210.0–286.6) | 237.6 (204.0–272.0) | < 0.001 |
| MPV (fL) | 9.7 (8.8–10.4) | 9.4 (8.4–10.4) | < 0.001 |
| ALT (U/L) | 12.9 (9.6–18.9) | 12.0 (9.0–17.7) | 0.025 |
| AST (U/L) | 15.8 (13.3–19.0) | 16.0 (13.8–19.9) | 0.494 |
| Creatinine (μmol/L) | 45.0 (40.6–49.4) | 46.0 (41.2–52.2) | < 0.001 |
| Uric acid (μmol/L) | 245.0 (209.0–287.0) | 233.0 (198.0–270.0) | < 0.001 |
| FBG (mmol/L) | 4.6 (4.3–5.0) | 4.5 (4.2–4.8) | < 0.001 |
Abbreviations: GDM Gestational diabetes mellitus, DM Diabetes mellitus, PCOS Polycystic ovary syndrome, BMI Body mass index, WBC White blood cell count, NEUT Neutrophil percentage, RBC Red blood cell count, HGB Hemoglobin, HCT Hematocrit, PLT Platelet count, MPV Mean platelet volume, ALT Alanine aminotransferase, AST Aspartate aminotransferase, FBG Fasting blood glucose
Table 4.
Univariable analysis of the GDM and the normal groups among the extended population
| Variable | GDM group (n = 637) |
Normal group (n = 844) |
p |
|---|---|---|---|
| Age (year) | 30.0 (28.0–33.0) | 29.0 (27.0–31.0) | < 0.001 |
| Nulliparous, n (%) | < 0.001 | ||
| No | 432 (67.8) | 466 (55.2) | |
| Yes | 205 (32.2) | 378 (44.8) | |
| History of GDM, n (%) | < 0.001 | ||
| No | 573 (90.0) | 833 (98.7) | |
| Yes | 64 (10.0) | 11 (1.3) | |
| History of macrosomia, n (%) | 0.005 | ||
| No | 619 (97.2) | 837 (99.2) | |
| Yes | 18 (2.8) | 7 (0.8) | |
| History of abnormal pregnancy, n (%) | 0.182 | ||
| No | 609 (95.6) | 818 (96.9) | |
| Yes | 28 (4.4) | 26 (3.1) | |
| Family history of DM, n (%) | < 0.001 | ||
| No | 615 (96.5) | 841 (99.6) | |
| Yes | 22 (3.5) | 3 (0.4) | |
| PCOS, n (%) | 0.003 | ||
| No | 619 (97.2) | 838 (99.3) | |
| Yes | 18 (2.8) | 6 (0.7) | |
| Pre-pregnancy BMI (kg/m2) | 21.2 (19.4–23.7) | 20.1 (18.6–39.1) | < 0.001 |
| WBC (109/L) | 9.4 (8.0–10.9) | 8.8 (7.6–10.1) | < 0.001 |
| NEUT (%) | 72.7 (68.5–76.7) | 72.9 (68.7–76.4) | 0.997 |
| RBC (1012/L) | 4.1 (3.8–4.3) | 4.0 (3.7–4.3) | 0.001 |
| HGB (g/L) | 122.0 (116.0–128.4) | 121.8 (113.6–127.0) | 0.005 |
| HCT (%) | 36.5 (34.5–38.3) | 35.8 (33.6–37.8) | < 0.001 |
| PLT (109/L) | 239.0 (205.6–276.1) | 233.5 (199.9–268.0) | 0.004 |
| MPV (fL) | 9.4 (8.5–10.2) | 9.0 (8.1–9.9) | < 0.001 |
| ALT (U/L) | 13.0 (9.9–20.0) | 12.0 (9.0–18.0) | 0.003 |
| AST (U/L) | 16.0 (13.6–20.0) | 16.0 (14.0–20.0) | 0.621 |
| Cr (μmol/L) | 46.0 (41.4–51.0) | 47.1 (42.0– 55.0) | < 0.001 |
| Uric acid (μmol/L) | 241.0 (207.7–241.0) | 235.3 (201.5–269.0) | 0.008 |
| FBG (mmol/L) | 4.6 (4.3–5.0) | 4.5 (4.2–4.8) | < 0.001 |
| PT (s) | 12.2 (10.8–12.7) | 12.4 (11.1–12.9) | < 0.001 |
| APTT (s) | 31.8 (28.6–34.3) | 33.2 (29.6–35.2) | < 0.001 |
| FIB (mg/dL) | 4.2 (3.8–4.6) | 4.1 (3.6–4.5) | < 0.001 |
| PAPP-A (MoM) | 1.0 (0.7–1.5) | 1.1 (0.8–1.6) | < 0.001 |
Abbreviations: GDM Gestational diabetes mellitus, DM Diabetes mellitus, PCOS Polycystic ovary syndrome, BMI Body mass index, WBC White blood cell count, NEUT Neutrophil percentage, RBC Red blood cell count, HGB Hemoglobin, HCT Hematocrit, PLT Platelet count, MPV Mean platelet volume, ALT Alanine aminotransferase, AST Aspartate aminotransferase, FBG Fasting blood glucose, PT Prothrombin time, APTT Activated partial thromboplastin time, FIB Fibrinogen, PAPP-A Pregnancy associated plasma protein A
Variables that were significantly associated with GDM in univariate logistic regression were included in the multivariable logistic regression. The basic model and the extended model were constructed to identify potential risk factors associated with GDM (Table 5). The basic model showed that there were 10 independent predictors, including age, family history of diabetes, history of GDM, pre-pregnancy BMI, WBC, PLT, MPV, creatinine, uric acid, and FBG. The extended model showed that age, history of GDM, pre-pregnancy BMI, HCT, MPV, creatinine, uric acid, FBG, ALT, APTT, FIB, and PAPP-A were potential risk factors for GDM. The results of the collinearity test show that the variance inflation factors of all variables are less than 2, which preliminarily indicated that the problem of collinearity can be ignored.
Table 5.
Multivariable logistic regression analysis based on the data from the training cohort
| Characteristics | Basic model (n = 2895) |
Extended model (n = 2116) |
||||
|---|---|---|---|---|---|---|
| β-coefficient | p | OR (95%CI) | β-coefficient | p | OR (95%CI) | |
| Age (year) | 0.11 | < 0.001 | 1.11 (1.08–1.14) | 0.14 | < 0.001 | 1.15 (1.11–1.18) |
| History of GDM, n (%) | ||||||
| No | Reference | Reference | ||||
| Yes | 1.92 | < 0.001 | 6.80 (3.73–13.40) | 1.84 | < 0.001 | 6.27 (3.39–12.56) |
| Family history of DM, n (%) | Not included | |||||
| No | Reference | |||||
| Yes | 2.36 | < 0.001 | 10.60 (3.61–39.53) | |||
| Pre-pregnancy BMI (kg/m2) | 0.97 | < 0.001 | 1.10 (1.07–1.14) | 0.10 | < 0.001 | 1.10 (1.06–1.15) |
| WBC (109/L) | 0.12 | < 0.001 | 1.13 (1.08–1.20) | Not included | ||
| PLT (109/L) | 0.00 | 0.021 | 1.00 (1.00–1.00) | Not included | ||
| MPV (fL) | 0.19 | < 0.001 | 1.21 (1.12–1.31) | 0.15 | 0.004 | 1.16 (1.05–1.29) |
| Creatinine (μmol/L) | -0.04 | < 0.001 | 0.96 (0.95–0.98) | -0.02 | < 0.001 | 0.98 (0.96–0.99) |
| Uric acid (μmol/L) | 0.00 | 0.001 | 1.00 (1.00–1.01) | 0.00 | 0.008 | 1.00 (1.00–1.00) |
| FBG (mmol/L) | 0.39 | < 0.001 | 1.47 (1.24–1.75) | 0.48 | < 0.001 | 1.61 (1.33–1.96) |
| HCT (%), | Not included | 0.05 | 0.013 | 1.05 (1.01–1.10) | ||
| ALT (U/L) | Not included | 0.01 | 0.014 | 1.01 (1.00–1.02) | ||
| APTT (s) | Not included | -0.07 | < 0.001 | 0.93 (0.90–0.96) | ||
| FIB (mg/dL) | Not included | 0.24 | 0.009 | 1.27 (1.06–1.52) | ||
| PAPP-A (MoM) | Not included | -0.27 | 0.002 | 0.76 (0.64–0.90) | ||
Abbreviations: CI Confidence interval, GDM Gestational diabetes mellitus, DM Diabetes mellitus, PCOS Polycystic ovary syndrome, BMI Body mass index, WBC White blood cell count, NEUT Neutrophil percentage, RBC Red blood cell count, HGB Hemoglobin, HCT Hematocrit, PLT Platelet count, MPV Mean platelet volume, ALT Alanine aminotransferase, AST Aspartate aminotransferase, FBG Fasting blood glucose, PT Prothrombin time, APTT Activated partial thromboplastin time, FIB Fibrinogen, PAPP-A Pregnancy associated plasma protein A
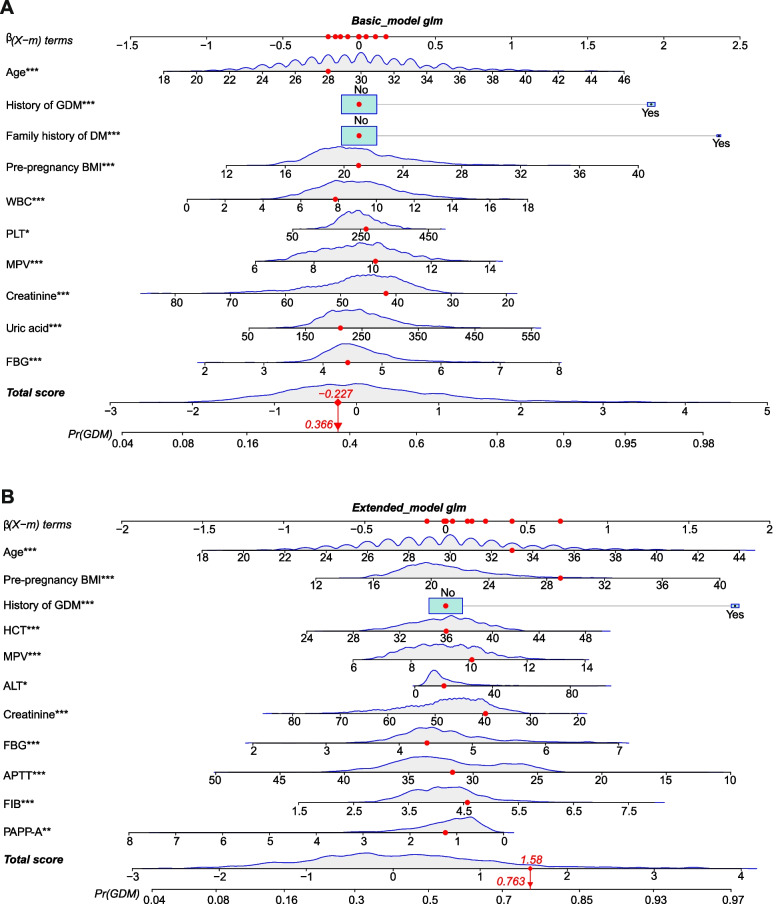
Nomograms and evaluation of nomograms
Based on the outcomes of multivariable logistic analysis, a nomogram of the basic model was constructed using 10 factors (Fig. 1A), and a nomogram of the extended model was constructed using 11 factors (Fig. 1B). Take an example of nomogram usage (a participant was randomly selected from the extended population): 30 years old, no history of GDM, pre-pregnant BMI of 29 kg/m2, HCT of 36%, MPV of 10.1 fL, ALT of 15 U/L, creatinine of 39.9 μmol/L, FBG of 4.4 mmol/L, APTT of 31.5 s, FIB of 4.55 mg/dL, and PAPP-A of 1.250 MoM. Finally, a total score of 1.58 was obtained, and the corresponding incidence probability of GDM was 79.3%.
Fig. 1.
Nomogram for predicting probability of developing GDM of the basic model and extended model. *p value between 0.01 and 0.05; **p value between 0.0009 and 0.009; ***p value < 0.0009. Pre BMI, pre-pregnancy body mass index; GDM, gestational diabetes mellitus; FH, Family history of diabetes mellitus; FPG fasting plasma glucose; WBC, White blood cell count; PLT, Platelet count; MPV, Mean platelet volume; CR, Creatinine; UA, Uric acid; HCT, Hematocrit; ALT, Alanine aminotransferase; APTT, activated partial thromboplastin time; FIB, Fibrinogen; PAPP-A, pregnancy associated plasma protein A
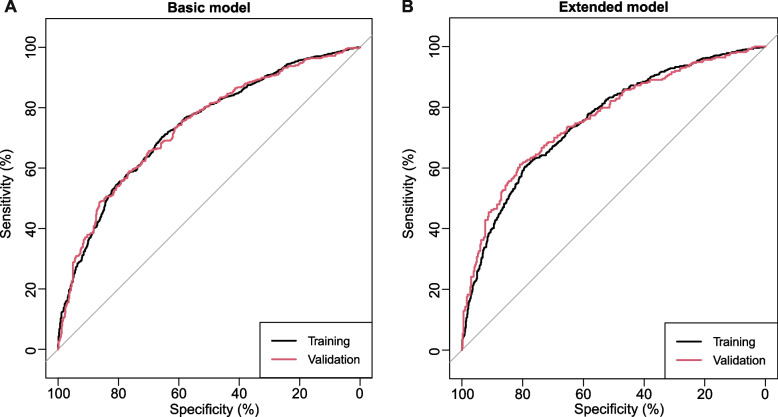
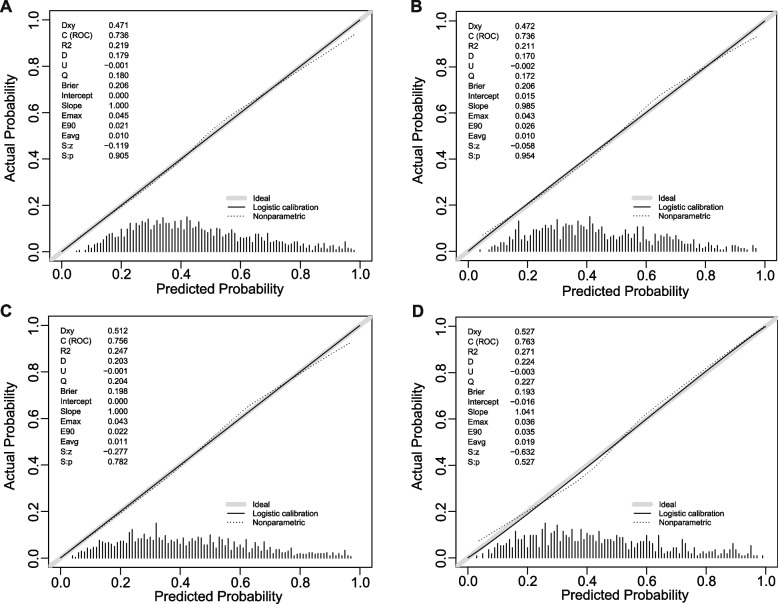
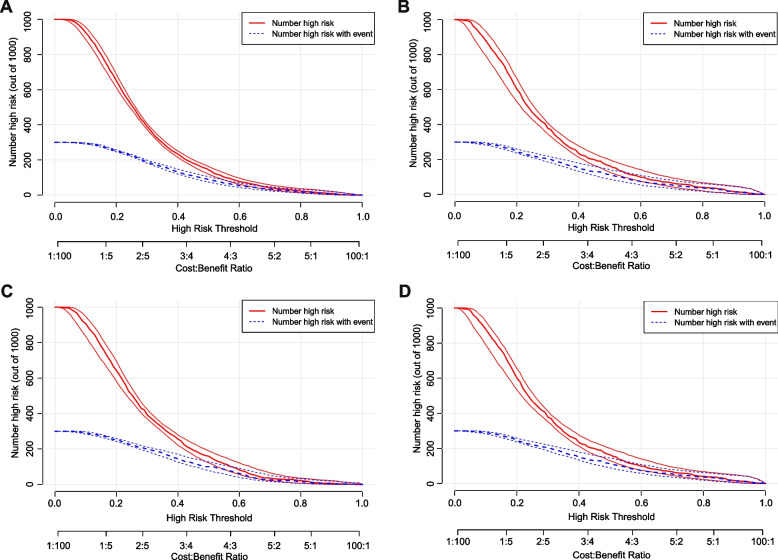
In terms of discrimination, the nomogram of the basic model had an AUC of 0.736 (95%CI: 0.71–0.76) in the training cohort. Applying the exploratory set estimates to the internal validation set yielded an AUC of 0.736 (95%CI: 0.70–0.77) (Fig. 2A). The AUC of the extended model in the training cohort and the internal validation cohort was respectively 0.756 (95%CI: 0.73–0.78) and 0.763 (95%CI: 0.73–0.80) (Fig. 2B), indicating that the two models had good distinguishing abilities. The sensitivity and specificity of the internal validation of the basic model was 0.657 and 0.698, respectively, and those of the extended model was 0.612 and 0.809, respectively. The calibration of the nomogram was evaluated by Hosmer–Lemeshow test, and its calibrations curve had been drawn (Fig. 3A–D). The p value of the calibration curves of the basic model and the extended model in the training group was 0.289 and 0.636, respectively, and those in the internal validation was 0.684 and 0.635, respectively, indicating that the two models had good calibration abilities. To evaluate the clinical effects of the nomogram model more visually, the clinical impact curves were drawn. The “Number high risk” curve was closely to the “Number high risk with event” curve at high-risk threshold from 0.4 to 1.0, which indicated that the nomogram model owns extraordinary predictive power. The clinical impact curves of the basic model and the extended model showed that the predicted probability coincided well with the actual probability in the training cohort, respectively (Fig. 4A, B). Similar results were found in the validation cohort (Fig. 4C, D).
Fig. 2.
ROC curves for train and internal validation group in the basic model and in the extended model. A In the basic model, AUC of the train and internal validation group were 0.736 (95%CI: 0.71–0.76) and 0.736 (95%CI: 0.70–0.77). B In the basic model, AUC of the train and internal validation group were 0.756 (95%CI: 0.73–0.78) and 0.763 (95%CI: 0.73–0.80). ROC, receiver operating characteristic; AUC, area under the receiver operating characteristic
Fig. 3.
Calibration curves. A Basic model in the train cohort. B Basic model in the internal validation cohort. C Extended model in the train cohort. D Extended model in the internal validation cohort. Nomogram-predicted probability of GDM is plotted on the x-axis; actual probability of GDM is plotted on the y-axis. The line adjacent to the ideal line represents the predictive accuracy. GDM, gestational diabetes mellitus
Fig. 4.
Clinical impact curves. A Basic model in the training cohort. B Basic model in the internal validation cohort. C Extended model in the training cohort. D Extended model in the internal validation cohort
Comparison and assessment of our model with the previous prediction models
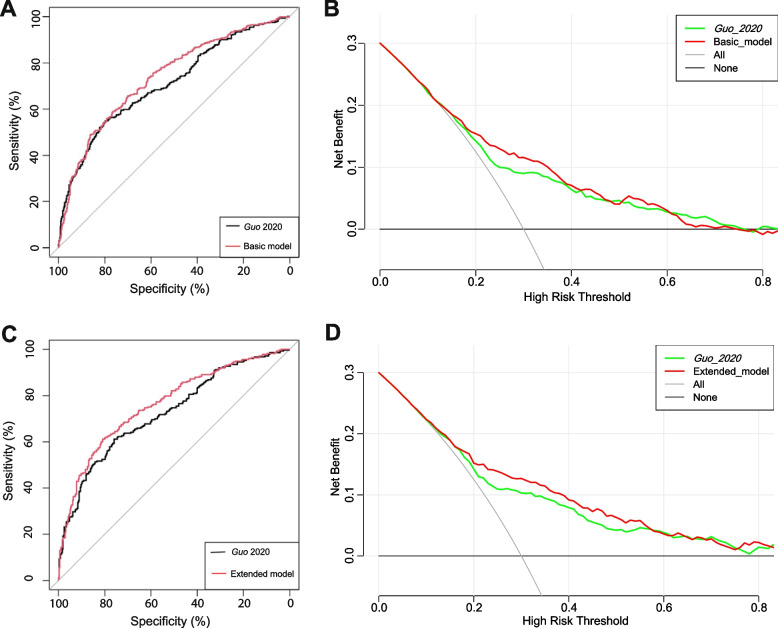
We compared the performance of our prediction models with a previously published early pregnancy prediction model based on the data in the present study, and this model was from Guo 2020 [22] based on age, FBG, family history of diabetes, and history of GDM. The performances of the present nomograms comparing with the Guo 2020 model are shown in Fig. 5A, C. According to the cross-validation, the performance of our basic model with an AUC of 0.736 (95%CI: 0.70–0.77) was greater than the Guo 2020 prediction model with an AUC of 0.707 (95%CI: 0.67–0.74) (p = 0.024) (Fig. 5A). The performance of our extended model with an AUC of 0.763 (95%CI: 0.73–0.80) was also greater than the Guo 2020 prediction model with an AUC of 0.726 (95%CI: 0.69–0.77) (p < 0.001) (Fig. 5C). The predictive abilities were confirmed by the significant AUC difference between our models and the previous published model (p < 0.05) (Table 6).
Fig. 5.
ROC curves and DCA. A Comparison between the basic model and the previous published model. B DCA of the basic model and the previous published model. C Comparison between the extended model and the previous published model. D DCA of the extended model and the previous published model. The horizontal line represented no cases will experience GDM; while the oblique line represents all cases will experience GDM. In the DCA, the area between the “black horizontal line” and “gray slope line” of the model curve meant the clinical validity of the model. The colorful lines represent the clinical net benefits according to the threshold probabilities. ROC, receiver operating characteristic curves; DCA, decision curve analysis; GDM, gestational diabetes mellitus
Table 6.
Calibration and discrimination statistics of our basic model and the previous published model
| Statistics | Basic model | Guo 2020 | Extended model | Guo 2020 |
|---|---|---|---|---|
| Calibration | ||||
| AIC | 1052.298 | 1073.530 | 743.384 | 764.359 |
| BIC | 1104.739 | 1097.367 | 796.827 | 786.627 |
| Discrimination | ||||
| NRI | p < 0.001 | p < 0.001 | ||
| IDI | p < 0.001 | p < 0.001 | ||
| AUC | p = 0.024 | p < 0.001 | ||
Abbreviations: AIC Akaike information criterion, BIC Bayesian information criteria, NRI Net reclassification improvement, IDI integrated discrimination improvement, AUC Area under the receiver operating characteristic curve
The prediction performances of these models were also assessed by means of calibration and discrimination statistics. As showed in Table 6, there was little difference in AIC and BIC between our models and previous published model. In addition, the results for NRI and IDI are similar to those found for the ROC analysis: the risk factors of our basic model improve discrimination compared with the Guo 2020 model (NRI = 0.364, 95%CI: 0.23–0.50, p < 0.001; IDI = 0.036, 95%CI: 0.02–0.05, p < 0.001). As well as the significance of NRI and IDI revealed that our extended model compared with the Guo 2020 model (NRI = 0.386, 95%CI: 0.23–0.54, p < 0.001; IDI = 0.049, 95%CI: 0.03–0.07, p < 0.001), which can differentiate between pregnant women with subsequent GDM and normal pregnant women (Table 6).
The DCA plot indicated good positive net benefits of the predictive nomogram model among majority threshold probabilities (Fig. 5B, D). For example, at a threshold of 30% shown in Fig. 5D, the Guo 2020 model would result in 11 per 100 participants being diagnosed with GDM, while our extended model will result in 13 per 100 participants being diagnosed with GDM without increasing false-positive results. In this analysis, all models showed a better cost effective than “treat all” and “treat none”, and our basic and extended models exhibited good performance.
Discussion
We developed two novel models based on clinical characteristics and laboratory biomarkers, providing an estimation of patient-specific risks for GDM at the first antenatal care visit. The present study successfully developed and internally validated the basic and the extended model that could predict the risk of developing GDM among patients with a singleton pregnancy before 16 weeks of gestation. The six predictors determined were age, history of GDM, pre-pregnancy BMI, FBG, creatinine, and MPV, which were all tested in our two models. Notably, the extended model that introduces APTT, FIB, and PAPP-A had a greater AUC of 0.763 compared with the basic model with an AUC of 0.736 for the same internal validation cohort. The nomogram demonstrated a favorable calibration for predicting the probability of GDM. When comparing with Guo 2020 model, our nomograms performed greater in calibration and discrimination. In addition, we performed a DCA to quantify the clinical usefulness of the models and found that our basic and extended models are greater.
We integrated other classical indicators associated with GDM to develop a prediction model in the early pregnancy. Consistent with previous findings [23–25], the present study showed that age, the proportion of history of GDM, the proportion of family history of DM, pre-pregnancy BMI, and FBG level of the women with GDM were significantly higher than those of normal pregnant women. A previous study found that the levels of WBC, PLT, and ALT in the early pregnancy were positively correlated with the risk of developing GDM, but the increased level of creatinine corresponded to a reduced risk [26]. The present results are concordant with several previous findings reporting that the level of MPV of patients with GDM was higher than that of the normal pregnant women [27]. Zhao et al. [28] found that serum uric acid was positively related to insulin resistance and increased in the patients with GDM in the early pregnancy, which is consistent with the present study. The same as the present result, HCT was reported to be significantly higher in the women with GDM in the early pregnancy [29]. Additionally, the present study demonstrated that the level of APTT of women with GDM in the early pregnancy was lower, whereas the level of FIB was higher in GDM group, suggesting that patients with GDM may be hypercoagulable. Those changes of laboratory biomarkers indicated that the pregnant women who subsequently develop GDM may have some abnormal functional changes during the early pregnancy.
Additionally, we found a lower level of PAPP-A in the women with GDM in the early pregnancy, which is consistent with the findings from Tenenbaum-Gavish et al. [18]. PAPP-A MoM refers to circulating PAPP-A concentrations adjusted by diverse maternal factors and medical history, such as age, weight, smoking, race, and diabetes status [30]. The decreased PAPP-A MoM of patients with GDM in the early pregnancy may be associated with impaired adipose tissue remodeling, enhanced pregnancy-induced insulin resistance, and impaired glucose tolerance [31]. Therefore, PAPP-A level in the early pregnancy may be important for GDM prediction. To the best of our knowledge, the introduction of the PAPP-A MoM into the nomogram has not been previously reported.
Although several biomarkers, such as adiponectin, plasma fatty acid-binding protein 4, and sex hormone binding globulin, can also achieve a great AUC [11, 12, 32], and various first-trimester prediction models for GDM have been proposed [33–35], no specific method has been widely used in routine clinical practice. The possible reasons may be that some biomarkers are not routinely tested for every pregnant woman, and some advanced technologies, such as machine learning, are not widely used in routine clinical practice. Therefore, it is necessary to explore more accurate and applicable approaches for predicting GDM in the early pregnancy.
In the present study, the two nomograms are adapted to difference hospital situations, which integrating multiple routine factors during the early pregnancy. The aim of the present study is to detect as many pregnant women with subsequent GDM as possible with high coverage of laboratory parameters and without increasing the psychological and economic burden. Meanwhile, the nomograms showed favorable discrimination and clinical usability for predicting the probability of GDM. However, we need to perform an external validation for the models using a multicenter prospective study in the further.
Conclusions
Early warning and early intervention are of great significance to the prevention, intervention, and prognosis of GDM. The present study established two applicable nomogram models that may accurately predict the risk of developing GDM when the first antenatal visit (generally in the early pregnancy).
Supplementary Information
Acknowledgements
Not applicable.
Abbreviations
- ALT
Alanine aminotransferase
- APTT
Activated partial thromboplastin time
- AST
Aspartate aminotransferase
- AUC
Area under the receiver operating characteristic curve
- BMI
Body mass index
- DCA
Decision-curve analysis
- DM
Diabetes mellitus
- FBG
Fasting blood glucose
- FIB
Fibrinogen
- GDM
Gestational diabetes mellitus
- HCT
Hematocrit
- HGB
Hemoglobin
- IDI
Integrated discrimination improvement
- MPV
Mean platelet volume
- NEUT
Neutrophil percentage
- NRI
Net reclassification improvement
- OGTT
Oral glucose tolerance test
- PAPP-A
Pregnancy associated plasma protein A
- PCOS
Polycystic ovary syndrome
- PLT
Platelet count
- PT
Prothrombin time
- RBC
Red blood cell count
- ROC
Receiver operating characteristic
- WBC
White blood cell count
Authors’ contributions
(I) Conception and design: R Li, Y Wei, A He; (II) Provision of study materials and collection of clinical information: Y Wei, H Liu, L Li, F Shen, J Li; (III) Data analysis and interpretation: C Tang, X Yang, X Wang, J Liu; (IV) Manuscript writing: Y Wei, A He; (V) Final approval of manuscript: All authors.
Funding
This work was supported by a grant from the China’s National Key R&D Programmes (Grant No. 2019YFC0121904) and a grant from the Natural Science Foundation of Guangdong Province, China (Grant No. 2022A1515012139).
Availability of data and materials
All data generated or analyzed during this study are included in the supplementary information files.
Declarations
Ethics approval and consent to participate
This work had been approved by the Scientific and Ethics Review Committees of the First Affiliated Hospital of Jinan University and Jiangmen Maternity and Child Health Care Hospital. Scientific and Ethics Review Committees of the First Affiliated Hospital of Jinan University and Jiangmen Maternity and Child Health Care Hospital had waived informed consent for the study as the nature of the present study is retrospective. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors have no conflicts of interest to declare.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yiling Wei and Andong He contributed equally to this work.
References
- 1.Zhu Y, Zhang C. Prevalence of gestational diabetes and risk of progression to type 2 diabetes: a global perspective. Curr Diab Rep. 2016;16(1):7. doi: 10.1007/s11892-015-0699-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American Diabetes A: 14 Management of diabetes in pregnancy: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S165–S172. doi: 10.2337/dc19-S014. [DOI] [PubMed] [Google Scholar]
- 3.Group HSCR. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, Hadden DR, McCance DR, Hod M, et al. Hyperglycemia and adverse pregnancy outcomes. N Engl J Med. 2008;358(19):1991–2002. doi: 10.1056/NEJMoa0707943. [DOI] [PubMed] [Google Scholar]
- 4.LaC B. Juan-Pablo and Hingorani, Aroon D and Williams, David: Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet (London, England) 2009;373:1773–1779. doi: 10.1016/S0140-6736(09)60731-5. [DOI] [PubMed] [Google Scholar]
- 5.Gabbe SG. Gestational diabetes mellitus. N Engl J Med. 1986;315(16):1025–1026. doi: 10.1056/NEJM198610163151609. [DOI] [PubMed] [Google Scholar]
- 6.Yessoufou A, Moutairou K. Maternal diabetes in pregnancy: early and long-term outcomes on the offspring and the concept of "metabolic memory". Exp Diabetes Res. 2011;2011:218598. doi: 10.1155/2011/218598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.American Diabetes A: 2 Classification and diagnosis of diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S14–S31. doi: 10.2337/dc20-S002. [DOI] [PubMed] [Google Scholar]
- 8.Sletner L, Jenum AK, Yajnik CS, Morkrid K, Nakstad B, Rognerud-Jensen OH, Birkeland KI, Vangen S. Fetal growth trajectories in pregnancies of European and South Asian mothers with and without gestational diabetes, a population-based cohort study. PLoS One. 2017;12(3):e0172946. doi: 10.1371/journal.pone.0172946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Naylor CD, Sermer M, Chen E, Farine D. Selective screening for gestational diabetes mellitus. Toronto Trihospital gestational diabetes project investigators. N Engl J Med. 1997;337(22):1591–1596. doi: 10.1056/NEJM199711273372204. [DOI] [PubMed] [Google Scholar]
- 10.Li-Zhen L, Yun X, Xiao-Dong Z, Shu-Bin H, Zi-Lian W, Adrian Sandra D, Bin L. Evaluation of guidelines on the screening and diagnosis of gestational diabetes mellitus: systematic review. BMJ Open. 2019;9(5):e023014. doi: 10.1136/bmjopen-2018-023014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ning H, Tao H, Weng Z, Zhao X. Plasma fatty acid-binding protein 4 (FABP4) as a novel biomarker to predict gestational diabetes mellitus. Acta Diabetol. 2016;53(6):891–898. doi: 10.1007/s00592-016-0867-8. [DOI] [PubMed] [Google Scholar]
- 12.Tawfeek MA, Alfadhli EM, Alayoubi AM, El-Beshbishy HA, Habib FA. Sex hormone binding globulin as a valuable biochemical marker in predicting gestational diabetes mellitus. BMC Womens Health. 2017;17(1):18. doi: 10.1186/s12905-017-0373-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gillet V, Ouellet A, Stepanov Y, Rodosthenous RS, Croft EK, Brennan K, Abdelouahab N, Baccarelli A, Takser L. miRNA profiles in extracellular vesicles from serum early in pregnancies complicated by gestational diabetes mellitus. J Clin Endocrinol Metab. 2019;104(11):5157–5169. doi: 10.1210/jc.2018-02693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Salomon C, Scholz-Romero K, Sarker S, Sweeney E, Kobayashi M, Correa P, Longo S, Duncombe G, Mitchell MD, Rice GE, et al. Gestational diabetes mellitus is associated with changes in the concentration and bioactivity of placenta-derived exosomes in maternal circulation across gestation. Diabetes. 2016;65(3):598–609. doi: 10.2337/db15-0966. [DOI] [PubMed] [Google Scholar]
- 15.Rawal S, Hinkle SN, Bao W, Zhu Y, Grewal J, Albert PS, Weir NL, Tsai MY, Zhang C. A longitudinal study of iron status during pregnancy and the risk of gestational diabetes: findings from a prospective, multiracial cohort. Diabetologia. 2017;60(2):249–257. doi: 10.1007/s00125-016-4149-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hughes RC, Moore MP, Gullam JE, Mohamed K, Rowan J. An early pregnancy HbA1c >/=5.9% (41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care. 2014;37(11):2953–2959. doi: 10.2337/dc14-1312. [DOI] [PubMed] [Google Scholar]
- 17.Zhu H, He D, Liang N, Lai A, Zeng J, Yu H. High serum triglyceride levels in the early first trimester of pregnancy are associated with gestational diabetes mellitus: a prospective cohort study. J Diabetes Investig. 2020;11(6):1635–1642. doi: 10.1111/jdi.13273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tenenbaum-Gavish K, Sharabi-Nov A, Binyamin D, Moller HJ, Danon D, Rothman L, Hadar E, Idelson A, Vogel I, Koren O, et al. First trimester biomarkers for prediction of gestational diabetes mellitus. Placenta. 2020;101:80–89. doi: 10.1016/j.placenta.2020.08.020. [DOI] [PubMed] [Google Scholar]
- 19.Artzi NS, Shilo S, Hadar E, Rossman H, Barbash-Hazan S, Ben-Haroush A, Balicer RD, Feldman B, Wiznitzer A, Segal E. Prediction of gestational diabetes based on nationwide electronic health records. Nat Med. 2020;26(1):71–76. doi: 10.1038/s41591-019-0724-8. [DOI] [PubMed] [Google Scholar]
- 20.Xiong Y, Lin L, Chen Y, Salerno S, Li Y, Zeng X, Li H: Prediction of gestational diabetes mellitus in the first 19 weeks of pregnancy using machine learning techniques. J Matern Fetal Neonatal Med. 2020:1–7. [DOI] [PubMed]
- 21.Weinert LS. International Association of Diabetes and Pregnancy Study Groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy: comment to the International Association of Diabetes and Pregnancy Study Groups Consensus Panel. Diabetes Care. 2010;33(7):e97. doi: 10.2337/dc10-0544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo F, Yang S, Zhang Y, Yang X, Zhang C, Fan J. Nomogram for prediction of gestational diabetes mellitus in urban, Chinese, pregnant women. BMC Pregnancy Childbirth. 2020;20(1):43. doi: 10.1186/s12884-019-2703-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gao C, Sun X, Lu L, Liu F, Yuan J. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis. J Diabetes Investig. 2019;10(1):154–162. doi: 10.1111/jdi.12854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chong YS, Cai S, Lin H, Soh SE, Lee YS, Leow MK, Chan YH, Chen L, Holbrook JD, Tan KH, et al. Ethnic differences translate to inadequacy of high-risk screening for gestational diabetes mellitus in an Asian population: a cohort study. BMC Pregnancy Childbirth. 2014;14:345. doi: 10.1186/1471-2393-14-345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Immanuel J, Simmons D. Screening and treatment for early-onset gestational diabetes mellitus: a systematic review and meta-analysis. Curr Diab Rep. 2017;17(11):115. doi: 10.1007/s11892-017-0943-7. [DOI] [PubMed] [Google Scholar]
- 26.Zhao M, Yang S, Hung TC, Zheng W, Su X. Association of pre- and early-pregnancy factors with the risk for gestational diabetes mellitus in a large Chinese population. Sci Rep. 2021;11(1):7335. doi: 10.1038/s41598-021-86818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhou Z, Chen H, Sun M, Ju H. Mean platelet volume and gestational diabetes mellitus: a systematic review and meta-analysis. J Diabetes Res. 2018;2018:1985026. doi: 10.1155/2018/1985026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao Y, Zhao Y, Fan K, Jin L. Serum uric acid in early pregnancy and risk of gestational diabetes mellitus: a cohort study of 85,609 pregnant women. Diabetes Metab. 2021;48(3):101293. doi: 10.1016/j.diabet.2021.101293. [DOI] [PubMed] [Google Scholar]
- 29.Shaarbaf Eidgahi E, Nasiri M, Kariman N, Safavi Ardebili N, Salehi M, Kazemi M, Zayeri F. Diagnostic accuracy of first and early second trimester multiple biomarkers for prediction of gestational diabetes mellitus: a multivariate longitudinal approach. BMC Pregnancy Childbirth. 2022;22(1):13. doi: 10.1186/s12884-021-04348-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wright D, Silva M, Papadopoulos S, Wright A, Nicolaides KH. Serum pregnancy-associated plasma protein-A in the three trimesters of pregnancy: effects of maternal characteristics and medical history. Ultrasound Obstet Gynecol. 2015;46(1):42–50. doi: 10.1002/uog.14870. [DOI] [PubMed] [Google Scholar]
- 31.Rojas-Rodriguez R, Ziegler R, DeSouza T, Majid S, Madore AS, Amir N, Pace VA, Nachreiner D, Alfego D, Mathew J, et al. PAPPA-mediated adipose tissue remodeling mitigates insulin resistance and protects against gestational diabetes in mice and humans. Sci Transl Med. 2020;12(571):eaay4145. doi: 10.1126/scitranslmed.aay4145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abell SK, Shorakae S, Boyle JA, De Courten B, Stepto NK, Teede HJ, Harrison CL. Role of serum biomarkers to optimise a validated clinical risk prediction tool for gestational diabetes. Aust N Z J Obstet Gynaecol. 2019;59(2):251–257. doi: 10.1111/ajo.12833. [DOI] [PubMed] [Google Scholar]
- 33.Zhang X, Zhao X, Huo L, Yuan N, Sun J, Du J, Nan M, Ji L. Risk prediction model of gestational diabetes mellitus based on nomogram in a Chinese population cohort study. Sci Rep. 2020;10(1):21223. doi: 10.1038/s41598-020-78164-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wu Y, Ma S, Wang Y, Chen F, Zhu F, Sun W, Shen W, Zhang J, Chen H. A risk prediction model of gestational diabetes mellitus before 16 gestational weeks in Chinese pregnant women. Diabetes Res Clin Pract. 2021;179:109001. doi: 10.1016/j.diabres.2021.109001. [DOI] [PubMed] [Google Scholar]
- 35.Kang M, Zhang H, Zhang J, Huang K, Zhao J, Hu J, Lu C, Shao J, Weng J, Yang Y, et al. A novel nomogram for predicting gestational diabetes mellitus during early pregnancy. Front Endocrinol (Lausanne) 2021;12:779210. doi: 10.3389/fendo.2021.779210. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in the supplementary information files.