Abstract
Objectives
This study aimed to assess the influences of stigma and HIV status on reproductive intention among heterosexual couples living with HIV in China.
Methods
A cross-sectional study was conducted in Kunming, China among 315 HIV-positive individuals and their spouses (n = 315 couples). An interview questionnaire was used to collect data on intention, desire, HIV Stigma Scale items, and HIV status. Dyadic fertility intention was examined using the actor-partner interdependence mediation model, based on the Traits-Desires-Intentions-Behavior framework.
Results
The husbands’ or wives’ internalized stigma had significant negative effects on their own fertility desire (β = −0.149, p<0.05 and β = −0.238, p<0.01, respectively). HIV-positive status of the husbands was weakly linked to their own fertility intention (β = −0.181, p<0.05). Husbands’ perceived provider stigma was associated with their own and their wives’ fertility intention via the mediating effect of their fertility desire (β = −0.374, p<0.001 and β = −0.203, p<0.01, respectively). The cumulative influence of their reproductive desire mediated the husband’s perceived provider stigma and the wife’s internalized stigma on their fertility intention.
Conclusions
Stigma and HIV status were associated with fertility intention among couples living with HIV, mediated by fertility desire. The high intra-couple correlation suggested that counseling should be conducted when both spouses are present together with extensive discussions on concerns regarding HIV-related stigma, potential discrepancies between each partner’s fertility desire and intention, and the influence of one partner on the other.
Introduction
People living with HIV (PLHIV) in a heterosexual relationship face a unique challenge. Although PLHIV may desire to have children similar to their HIV-negative counterparts [1], conception and childbearing in couples with at least one HIV-positive partner may result in horizontal transmission of HIV between partners, or vertical mother-to-child transmission of HIV. Although the likelihood of such transmissions can be reduced through medical interventions, such as fertility clinics and prevention of mother-to-child transmission (PMTCT) services, HIV-related stigmas create barriers in the use of these interventions [2]. Therefore, it is necessary for relevant stakeholders, particularly those who work in reproductive health and HIV prevention and control, to consider the influence of stigma and HIV-positive status on fertility desire and intention among couples living with HIV.
Despite the importance of these considerations, the majority of previous studies were conducted among PLHIV who were single or without the involvement of their partners if in a partnered relationship. Studies in dyads have the potential to increase our understanding of mutual fertility intention [3]. In that regard, the actor-partner interdependence mediation model (APIMeM) is suitable for investigating mutual intention among couples [4,5]. The APIMeM includes two assessments. The first is the possible correlations between the two types of stigmas (i.e., perceived provider and internalized) or HIV status, which would indicate a compositional effect. The second correlation is the residual nonindependence in the variables related to fertility intention, which indicates nonindependence that the APIMeM itself cannot explain.
On a related note, the Traits-Desires-Intentions-Behavior (TDIB) framework [6,7] denotes how the individual’s perceived stigma and HIV status (traits) interact with the cognitive notions of desire (want) and intention (plan) to have a child [8,9]. However, there has been no empirical data on the influence of one person on his or her spouse’s fertility desire and intention according to this framework. The assessment of mutual fertility intention using the heterosexual couple dyad as the unit of study should greatly improve our understanding of mutual fertility intention.
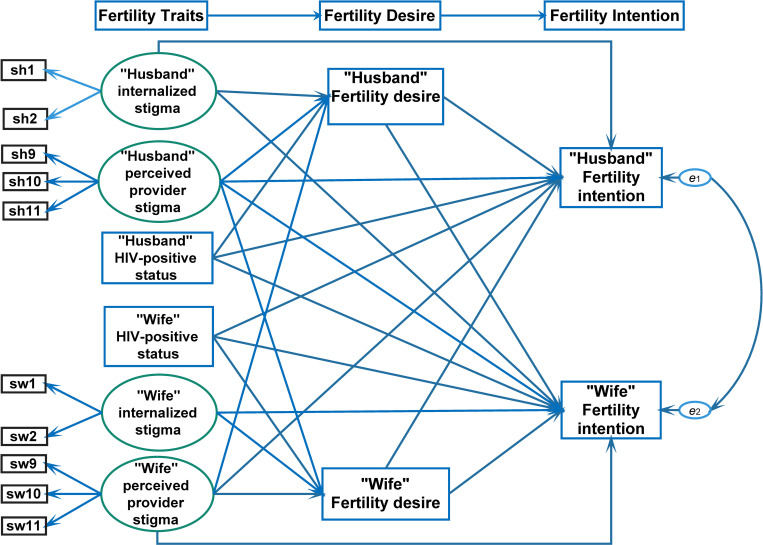
We hereby hypothesize that stigma and HIV-positive status among couples living with HIV are associated with fertility intention, and mediated by fertility desire, based on the APIMeM (Fig 1) [4,5]. The objectives of this study were to assess the direct influence of stigma and HIV-positive status on fertility intention and the extent that the influence of stigma was mediated by fertility desire among heterosexual HIV-positive husband-wife dyads in Kunming, China.
Fig 1. Hypothesized framework for fertility intention among monogamous HIV concordant and discordant couples.
Methods
Study design and setting
A cross-sectional study was conducted at a tertiary hospital in Kunming City, China. Structured interviews were carried out from October to December 2020. Kunming City was chosen for the study because it was the site of an on-going HIV epidemic. Furthermore, the hospital’s infectious disease antiretroviral treatment (ART) clinic was one of the pilot sites for a PMTCT program in China, and thus had considerable experience and rapport with the local PLHIV community.
Study participant eligibility criteria and recruitment
The study participants included HIV-infected reproductive-age patients attending an ART clinic at the study hospital. The inclusion criteria included: 1) reproductive age (i.e., 20–40 years for females and 20–50 years for males), 2) stable heterosexual relationship where both partners were aware of the HIV status, 3) no child or 1 child, 4) received ART for at least 12 months with undetectable viral loads, 5) no AIDS-defined illness, and 6) living in Yunnan Province. The exclusion criteria were: 1) unable to communicate, 2) too unwell to participate in the interview, and 3) unable to conceive for any reason (e.g., hysterectomy, oophorectomy, medical illness that contraindicated pregnancy, such as complicated heart disease or active autoimmune disease).
One of the investigators worked at the study hospital and prepared a sampling frame based on the list of current patients at the ART clinic in the ART database. The sampling frame data included the patient’s clinic-specific identification number, gender, and the date of the next appointment. The investigators used a computer program to randomly sample the patients stratified by sex. On the day of the appointment, investigators approached each patient in person, introduced themselves, assessed the patient’s eligibility, provided information about the study, and inquired about the patient’s interest in participation. Each participant was given approximately 10 minutes to decide whether to participate in the study interview. The investigators then asked for verbal informed consent from the patients before starting the study interview. The patients were also asked for permission to contact their partner to provide information and ask for verbal informed consent. In this study, we refer to one pair of the patient and their partner as a couple.
Initially, a total of 325 couples were invited to participate in the study. Ten couples had at least one spouse who did not complete the consent form. Finally, 315 couples (96.9% of all recruited couples) were included in this analysis.
Instrument
The study instrument was a structured interview questionnaire. The questionnaire included a section on socio-demographic characteristics (age, educational level, occupation status, ethnic group, registered residence, religion, and medical insurance), HIV status, HIV-related stigma, fertility desire, and fertility intention.
Measurement of HIV-related stigma
A revised stigma scale was used to measure HIV-related stigma [10–12]. The 5-item scale included two subscales: internalized stigma and stigma from healthcare providers [13,14]. A higher score on the scale indicated a greater level of stigma. The scale is recognized to be valid and reliable by the scientific community. In the current study, the Cronbach’s alpha was 0.50 among the couples living with HIV and 0.99 among the spouses, with subscale reliability values ranging from 0.62 to 0.93 among the spouses.
Divergent validity was used to demonstrate that unrelated constructs were actually unrelated by comparing the squared correlations of all latent variables with their average variance extracted values [15].
Measurement of fertility desire
General desire to have a/another child was assessed using the following question: ‘‘Do you want to have a/another child at the present?” The possible responses were “yes”, “not sure”, or “no” by the couples living with HIV [7].
Measurement of fertility intention
Fertility intention was assessed with a single question: "How likely are you to have a/another child during the next three years?" The responses were on a five-point scale that ranged from definitely disagree to definitely agree [6].
Data collection
The data were obtained by four trained research assistants who worked as part of a team from the hospital’s ART clinic in Kunming City. After providing information about the study and obtaining verbal informed consent, each respondent was interviewed prior to and separately from his or her spouse. Face-to-face interviews with the patient and their spouse, as well as telephone interviews with the spouse (if living far away), took approximately 15–30 minutes. All questionnaires were returned with no missing information.
Data analysis
All statistical analyses were performed using R. The socio-economic characteristics and HIV concordant/discordant status were summarized using descriptive statistics. Pearson correlation coefficients were calculated for the variables measured separately for the wife and husband.
We used the APIMeM to examine the impact of wives’ and husbands’ reported stigmas on their partner’s fertility intention via mediation of their own and their partner’s fertility desires [16]. The model examines the influences of the husband (direct and indirect) and the wife (direct and indirect). The spouse effect refers to the extent that an individual’s current trait or behavior is influenced by his/her previous trait or behavior and quantifies the trait or behavior’s internal consistency or stability. The wife effect refers to the extent that a certain partner affects a woman’s trait or behavior and quantifies the association in relational data. This model is divided into two sections and includes ten variables: six independent variables, two outcome variables, and two potential mediator variables. The six independent variables were: 1) wife’s internalized stigma, 2) husband’s internalized stigma, 3) wife’s perceived provider stigma, 4) husband’s perceived provider stigma, 5) wife’s HIV-positive status, and 6) husband’s HIV-positive status. The two outcome variables were: wife’s fertility intention and husband’s fertility intention. The two potential mediator variables were: wife’s fertility desire and husband’s fertility desire.
The influences of stigma and HIV status on fertility intention were examined using structural equation modeling. The effects of individual participants on their spouses were estimated and tested using a 5,000 sample size that used the bias-corrected bootstrapping approach with a 95% confidence interval [17].
Ethical considerations
The Human Research Ethics Committee of Prince of Songkla University (REC-63-208-18-1) and the Third People’s Hospital Research Ethics Review Committee authorized this study (2020072001). Pseudonyms were used to protect the participants’ identities in this study. Each patient and spouse volunteered and completed an informed consent form. All data were kept secret and confidential, and only the research team had access to the data.
Results
The socio-economic and HIV status characteristics of the participants are summarized in Table 1. The mean ages and standard deviations of the husbands and wives were 36.82 (5.90) years and 33.81 (5.19) years, respectively. The most common level of educational attainment among the husbands was senior high school, whereas the most common level among the wives was junior high school. Unemployment among the wives was twice as high as among the husbands. Most participants were Han Chinese who lived in rural areas. Most couples (68%) reported the New Rural Cooperative Medical Insurance as their medical insurance provider. The monthly income level varied widely among the study participants. Three-fourths of the couples were sero-discordant with an HIV-positive wife and a HIV-negative husband being slightly more common than vice versa.
Table 1. Socio-demographic and HIV-related characteristics.
| Husband (n = 315) | Wife (n = 315) | Total (N = 630) | |
|---|---|---|---|
| n (%) | n (%) | N (%) | |
| Age category | |||
| 20–30 | 33 (10.5) | 72 (22.9) | 105 (16.7) |
| 31–35 | 93 (29.5) | 103 (32.7) | 196 (31.1) |
| 36–40 | 93 (29.5) | 101 (32.1) | 194 (30.8) |
| 41+ | 96 (30.5) | 39 (12.4) | 135 (21.4) |
| Education level | |||
| Primary school | 34 (10.8) | 42 (13.3) | 76 (12.1) |
| Junior school | 94 (29.8) | 123 (39) | 217 (34.4) |
| Senior school | 103 (32.7) | 93 (29.5) | 196 (31.1) |
| Graduate and above | 84 (26.7) | 57 (18.1) | 141 (22.4) |
| Occupation status | |||
| Government employee | 44 (14) | 18 (5.7) | 62 (9.8) |
| Jobless | 47 (14.9) | 105 (33.3) | 152 (24.1) |
| Manual laborer | 45 (14.3) | 26 (8.3) | 71 (11.3) |
| Private employee | 73 (23.2) | 85 (27) | 158 (25.1) |
| Self-employed | 106 (33.7) | 81 (25.7) | 187 (29.7) |
| Ethnic group | |||
| Han | 283 (89.8) | 263 (83.5) | 546 (86.7) |
| Others | 32 (10.2) | 52 (16.5) | 84 (13.3) |
| Registered residence | |||
| Rural | 194 (61.6) | 203 (64.4) | 397 (63) |
| Urban | 121 (38.4) | 112 (35.6) | 233 (37) |
| Religion | |||
| No | 284 (90.2) | 273 (86.7) | 557 (88.4) |
| Yes | 31 (9.8) | 42 (13.3) | 73 (11.6) |
| Medical insurance status | |||
| NRCMS | 182 (57.8) | 190 (60.3) | 372 (59) |
| UEBMI | 35 (11.1) | 22 (7) | 57 (9) |
| URBMI | 98 (31.1) | 103 (32.7) | 201 (31.9) |
| Couple-level variables | |||
| Household monthly income (CNY) | |||
| 0–5,999 | - | - | 90 (28.6) |
| 6,000–9,999 | - | - | 78 (24.8) |
| 10,000–19,999 | - | - | 79 (25.1) |
| 20,000+ | - | - | 68 (21.6) |
| Couple HIV serostatus | |||
| Both positive | - | - | 84 (26.7) |
| Husband (positive) and wife (negative) | - | - | 103(32.7) |
| Husband (negative) and wife (positive) | - | - | 128 (40.6) |
HIV = human immunodeficiency virus; NRCMS = New Rural Cooperative Medical Insurance Scheme; UEBMI = Urban Employees Basic Medical Insurance; URBMI = Urban Residents Basic Medical Insurance; CNY = Chinese Yuan (Exchange rate: 1 USD = 6.72 CNY).
Descriptive statistics and bivariate correlation in the husband-wife dyads
Pearson’s correlation analysis (Table 2) showed that the husbands’ perceived provider stigma scores were correlated with those of their wives (r = 0.52, p-values <0.05). Significant and positive correlations were found between the husbands and their wives with regards to fertility desire and intention (r = 0.47 and r = 0.73, respectively, all p-values <0.01). In this study, all scales had acceptable levels of Cronbach’s alpha reliability (range = 0.68–0.98) and average variance extracted divergent validity coefficients (0.44–0.96).
Table 2. Pearson correlation coefficients, mean (standard deviation), and Cronbach’s alpha among the study variables (N = 315 couples).
| Mean (SD) | Var 1 | Var 2 | Var 3 | Var 4 | Var 5 | Var 6 | Var 7 | Var 8 | Var 9 | Var 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Var 1 | 2.4 (1.2) | 1 | ||||||||||
| Var 2 | 2.5 (1.2) | −0.17 | 1 | |||||||||
| Var 3 | 3.1 (0.67) | −0.03 | 0.18* | 1 | ||||||||
| Var 4 | 3 (0.72) | 0.04 | 0.52** | -0.1 | 1 | |||||||
| Var 5 | 0.58(0.49) | -0.25** | -0.24** | -0.04 | -0.17* | 1 | ||||||
| Var 6 | 0.62(0.49) | 0.03 | -0.25** | -0.25** | -0.26** | 0.47** | 1 | |||||
| Var 7 | 3.46(1.13) | -0.13 | -0.34** | -0.15* | -0.21** | 0.57** | 0.53** | 1 | ||||
| Var 8 | 3.38(1.23) | -0.02 | -0.28** | -0.18* | -0.26** | 0.51** | 0.65** | 0.73** | 1 | |||
| Var 9 | 0.59(0.49) | 0.50** | -0.14 | 0.23** | -0.09* | -0.17* | -0.16* | -0.16* | -0.1 | 1 | ||
| Var 10 | 0.67(0.47) | -0.34** | 0.16 | -0.45** | 0.21** | 0.06 | 0.08 | 0.08 | 0.04 | -0.58** | 1 | |
| Cronbach’s alpha | - | - | 0.96 | 0.68 | 0.98 | 0.70 | - | - | - | - | - | - |
| Average Variance Extracted | 0.93 | 0.44 | 0.96 | 0.45 | - | - | - | - | - | - |
Note: Var 1 = Internalized stigma (husband); Var 2 = Perceived provider stigma (husband); Var 3 = Internalized stigma (wife); Var 4 = Perceived provider stigma (wife); Var 5 = Positive fertility desire (husband); Var 6 = Positive fertility desire (wife); Var 7 = Fertility intention (husband); Var 8 = Fertility intention (wife); Var 9 = Husband’s HIV-positive status; Var 10 = Wife’s HIV-positive status.
SD = standard deviation
*p<0.05
**p<0.01.
Dyadic data analysis using the APIMeM
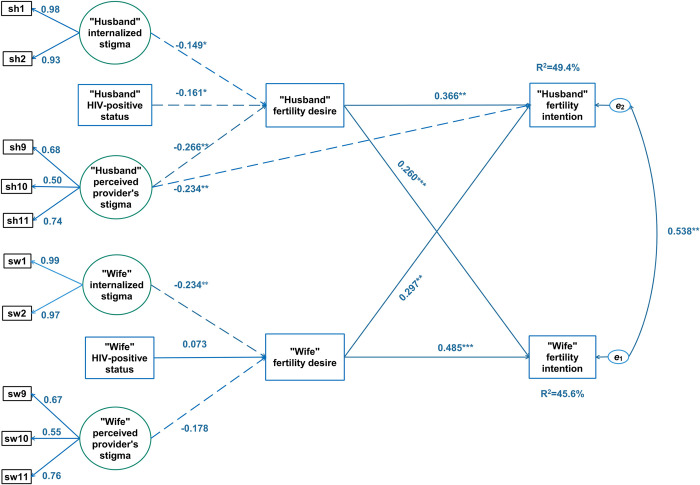
Fig 2 depicts the estimated paths of direct effects with R2 = 0.49 for husbands and R2 = 0.46 for wives. The model fit the data well: x2/df = 2.59; SRMR = 0.047; RMSEA = 0.071; CFI = 0.97; and TLI = 0.95. The covariance of the errors from both sides was statistically significant (β = 0.538, p<0.001), which indicated both husband and wife shared fertility intention. In terms of actor effects, husbands and wives with a high level of fertility desire had a greater intention to have children (β = 0.336, p = 0.000; β = 0.485, p<0.001, respectively). The husband’s desire for children had a statistically significant effect on the wife’s fertility intention (β = 0.260, p<0.001), which was similar to the counterpart effect from the wife to the husband (β = 0.297, p<0.001).
Fig 2. Associations of wives and husbands’ childbearing internalized and provider stigma and fertility intention through fertility desire based on actor-partner interdependence mediation (APIMeM) model.
Significant (p < .05) positive effect, significant (p < .05) negative effect, ***: p < .01, **: p < .05; R2: Squared multiple correlation, e1 and e2: Residual error.
The pattern of cross-over effects was lacking at the trait level. Traits only directly influenced fertility desire and intention of the same individual and not his or her spouse, which is not shown in Fig 1.
Husbands’ or wives’ internalized stigma had significant negative effects on their own fertility desire (β = −0.149, p < 0.05 and β = −0.238, p < 0.01, respectively). However, only husbands had a significant negative effect of perceived provider stigma on their own fertility desire (β = −0.226, p < 0.01) and fertility intention (β = −0.234, p < 0.01).
Total effects of stigma and HIV status on fertility intention consists of direct effects and indirect effects. The direct effects were not significant and are not shown in Fig 1. The indirect effects are listed in sections a.1 and a.3 and the total effects are in sections a.2 and b.2 of Table 3.
Table 3. Coefficients of indirect and total significant effects in the APIMeM.
| Path | β | SE | p-value | CI |
|---|---|---|---|---|
|
a. Husband’s stigma and HIV positive status→ Fertility desire (husband and wife) →
Fertility intention (husband and wife) | ||||
| a.1 Indirect effects | ||||
| Provider stigma (Husband) → Fertility intention (husband) | −0.14 | 0.106 | 0.018 | (−0.508, −0.073) |
| Provider stigma (Husband) → Fertility intention (wife) | −0.139 | 0.132 | 0.041 | (−0.568, −0.022) |
| HIV-positive status (husband) → Fertility intention (husband) | −0.096 | 0.103 | 0.03 | (−0.45, −0.032) |
| HIV-positive Status (husband) → Fertility intention (wife) |
−0.102 | 0.117 | 0.028 | (−0.52, −0.05) |
| a.2 Total effects | ||||
| Provider stigma (husband) → Fertility intention (husband) |
−0.374 | 0.178 | 0.00 | (−1.073, −0.298) |
| Provider stigma (husband) → Fertility intention (wife) | −0.203 | 0.171 | 0.021 | (−0.786, −0.144) |
| HIV-positive status (husband) → Fertility intention (husband) | −0.181 | 0.168 | 0.013 | (−0.732, −0.082) |
|
b. Wife’s stigma and HIV-positive status→ Fertility desire (husband and wife) →
Fertility intention (Husband and Wife) | ||||
| b.1 Indirect effects | ||||
| Internalized stigma (wife) → Fertility intention (wife) |
−0.117 | 0.042 | 0.007 | (−0.197, −0.028) |
| b.2 Total effects | ||||
| Internalized stigma (wife) → Fertility intention (wife) |
−0.164 | 0.058 | 0.006 | (−0.27, −0.029) |
| Internalized stigma (wife) → Fertility intention (husband) |
−0.135 | 0.054 | 0.024 | (−0.229, −0.001) |
Note: β = standardized estimate.
SE = standard error; CI = confidence interval; APIMeM = actor-partner interdependence mediation model.
Husbands’ perceived provider stigma was associated with their own and their wives’ fertility intention via the mediating total effect of their fertility desire (β = −0.374, p < 0.001 and β = −0.203, p < 0.01, respectively). HIV-positive status of the husbands was weakly linked to their own fertility intention (β = −0.181, p < 0.05). Through the whole mediating effect of their fertility desire, the wives’ internalized stigma was linked with their own and their husbands’ fertility intention (β = −0.164, p < 0.05 and β = −0.135, p < 0.05, respectively). Both husbands and wives reported that HIV-related reproductive stigma reduced their fertility intention by decreasing their desire to have a/another child, while their fertility intention was related to an increased fertility desire.
Discussion
We assessed the extent that fertility desire mediated the association between HIV-related stigma and fertility intention among couples living with HIV, as well as the mediation on the association between HIV status and fertility intention. The findings indicated a strong reciprocal relationship within each couple on fertility intentions. Intra-spouse residual correlation of fertility intention was strong. The husbands’ fertility intention considerably predicted the wives’ fertility intention. Fertility intention of the wives or husbands was strongly influenced by their own fertility intention, their spouses’ fertility intention, and their spouses’ fertility desire. On the other hand, fertility traits related to HIV status and stigma influenced only one’s own fertility desire without significant effects on the spouse. Total effects of trait variables on fertility intention mainly acted through fertility desire. The husbands’ perceived provider stigma directly predicted their own fertility intention. Other direct effects were not statistically significant. The novelty of using this analysis for fertility behavior of couples living with HIV would be useful for future studies and health services.
The findings suggested that fertility intention in couples living with HIV occurred as dyads (i.e., there was significant interconnectedness in each couple with regard to fertility intention). The findings were consistent with a previous study, which found that the strongest predictor for a person’s intention to have children was having a partner who intended to have children [18]. Other studies also showed that HIV patients reported that their spouse desired to have children but such data were not collected directly from the patient’s partners [19–21]. This current study contributed to the body of literature by collecting data from both partners and analyzing the data as dyads, which enabled direct reflection of the couple dyad psyche.
Participants’ fertility desire was found to be strongly associated with their own fertility intention, which was similar to the findings of a previous study [6]. Furthermore, there was mutual influence of the participants’ own fertility desire on the fertility intention of their spouses. A plausible explanation for these results was that among HIV-positive individuals a couple’s relationship status was a significant predictor of the partner’s fertility desire [14]. The support and encouragement of a spouse with a positive desire for children may be a significant factor in fertility intentions [7,22]. Furthermore, fertility desire is the most important mediating factor for fertility intention among HIV patients, and it is a key variation that has an important impact on the active response to fertility behavior [7].
No significant association was observed between demographic-socio-economic characteristics and fertility intention. Previous studies, on the other hand, showed a close link between gender and perceived stigma from healthcare providers [8,23,24]. These disparities by gender also could have accounted for the stronger association among the husbands compared to the wives.
Wives’ internalized stigma was more strongly associated with the husbands’ fertility intention via fertility desire than vice versa. It was possible that HIV-positive women were more sensitive to internalized stigma than their husbands. Some of the discrepancies between this study’s findings and those of earlier studies might be explained by the cultural context of this study. In Chinese society and culture, wives are primarily reliant on their husbands for fertility [25–27]. Furthermore, it seems that the wives’ fertility intention was more influenced by the efforts of their husbands to address stigma, fertility desire, and fertility intention [24,28] than from other factors.
Only minor differences were found in fertility intention between HIV-positive versus HIV-negative husbands. However, the differences were more noticeable among HIV-positive versus HIV-negative wives. Consistent with previous research in Mozambique [29], no association was found between a woman’s HIV status and fertility desire. HIV-positive women were found to be less likely to have children than HIV-negative women [30]. These contradictory findings could be attributed in part to the widespread belief that childbirth was incompatible with HIV. However, PMTCT programs have been available in the study area for more than 20 years, which might have reduced the fear of HIV vertical transmission, particularly among the women [31].
Strengths and limitations
Our study had a fairly high participation rate from the recruited couples, which potentially reduced the possibility of selection bias. However, a number of limitations should be considered in the interpretation of our study findings. First, the causal pathway in this article was based on an existing theory with a relatively straightforward pathway and a focus on the couple dyad. Findings from a more inductive or inferential approach could have yielded different results. Second, the level of stigma experienced by each participant might have varied over time but our cross-sectional study design precluded the measurement of these variations and reflected mainly the self-reported stigma at the time of the interview. Findings from a longitudinal study may yield different results. Third, this study was conducted in Yunnan Province, which is an area in China with high ethnic diversity and a relatively high level of poverty. The findings of this study may have limited generalizability to couples living with HIV in other settings.
Conclusions
We assessed the extent that fertility desire mediated the association between HIV-related stigma and fertility intention among couples living with HIV, as well as the mediation on the association between HIV status and fertility intention. The outcomes of this study show the importance of stigma in intra-couple fertility intention. The study findings have implications for family planning counseling in couples living with HIV. The high intra-couple correlation between fertility desire and intention suggests that couples should receive counseling on fertility together, with extensive discussions on concerns regarding HIV-related stigma, potential discrepancies between each partner’s fertility desire and intention, and the influence of one partner on the other.
Supporting information
(TIF)
(CSV)
Acknowledgments
This study is a part of the first author’s thesis in partial fulfillment of the requirements for a Ph.D. degree in Epidemiology at Prince of Songkla University, Songkhla, Thailand. We greatly appreciate the assistance from the staff members of the HIV treatment center who supported our study at the Third People’s Hospital in Kunming, China.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
Funding was received from the Higher Education Research Promotion and Thailand’s Education Hub for the Southern Region of ASEAN Countries Project Office of the Higher Education Commission (TEH-AC:016/2018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Jose H, Madi D, Chowta N, Ramapuram J, Bhaskaran U, Achappa B, et al. Fertility Desires and Intentions among People Living with HIV/AIDS (PLWHA) in Southern India. J Clin Diagn Res JCDR. 2016;10: OC19–OC22. doi: 10.7860/JCDR/2016/20282.7968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turan JM, Nyblade L. HIV-related Stigma as a Barrier to Achievement of Global PMTCT and Maternal Health Goals: A Review of the Evidence. AIDS Behav. 2013;17: 2528–2539. doi: 10.1007/s10461-013-0446-8 [DOI] [PubMed] [Google Scholar]
- 3.Reed RG, Butler EA. Dyadic Models for the Study of Health. Soc Personal Psychol Compass. 2013;7: 228–245. doi: 10.1111/spc3.12022 [DOI] [Google Scholar]
- 4.Cook WL, Kenny DA. The Actor–Partner Interdependence Model: A model of bidirectional effects in developmental studies. Int J Behav Dev. 2005;29: 101–109. doi: 10.1080/01650250444000405 [DOI] [Google Scholar]
- 5.Chen Z, Hou L. An Actor-Partner Interdependence Model of Work Challenge Stressors and Work-Family Outcomes: the Moderating Roles of Dual-Career Couples’ Stress Mindsets. J Bus Psychol. 2021;36: 1109–1123. doi: 10.1007/s10869-020-09724-1 [DOI] [Google Scholar]
- 6.Miller WB, Severy LJ, Pasta DJ. A framework for modelling fertility motivation in couples. Popul Stud. 2004;58: 193–205. doi: 10.1080/0032472042000213712 [DOI] [PubMed] [Google Scholar]
- 7.Wagner AC, Ivanova EL, Hart TA, Loutfy MR. Examining the Traits-Desires-Intentions-Behavior (TDIB) Model for Fertility Planning in Women Living with HIV in Ontario, Canada. AIDS Patient Care STDs. 2014;28: 594–601. doi: 10.1089/apc.2014.0075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nöstlinger C, Desjardins F, Dec J, Platteau T, Hasker E, Eurosupport V Study Group. Child desire in women and men living with HIV attending HIV outpatient clinics: evidence from a European multicentre study. Eur J Contracept Reprod Health Care Off J Eur Soc Contracept. 2013;18: 251–263. doi: 10.3109/13625187.2013.801072 [DOI] [PubMed] [Google Scholar]
- 9.Withers M, Dworkin S, Harrington E, Kwena Z, Onono M, Bukusi E, et al. Fertility intentions among HIV-infected, sero-concordant Kenyan couples in Nyanza Province, Kenya. Cult Health Sex. 2013;15. doi: 10.1080/13691058.2013.811289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tavakoli F, Karamouzian M, Rafiei-Rad AA, Iranpour A, Farrokhnia M, Noroozi M, et al. HIV-Related Stigma Among Healthcare Providers in Different Healthcare Settings: A Cross-Sectional Study in Kerman, Iran. Int J Health Policy Manag. 2020;9: 163–169. doi: 10.15171/ijhpm.2019.92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tran BX, Phan HT. Understanding Global HIV Stigma and Discrimination: Are Contextual Factors Sufficiently Studied? (GAPRESEARCH). Int J Environ Res Public Health. 2019;16. doi: 10.3390/ijerph16111899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz IT, Ryu AE, Onuegbu AG, Psaros C, Weiser SD, Bangsberg DR, et al. Impact of HIV-related stigma on treatment adherence: systematic review and meta-synthesis. J Int AIDS Soc. 2013;16: 18640. doi: 10.7448/IAS.16.3.18640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Earnshaw VA, Smith LR, Chaudoir SR, Amico KR, Copenhaver MM. HIV Stigma Mechanisms and Well-Being Among PLWH: A Test of the HIV Stigma Framework. AIDS Behav. 2013;17: 1785–1795. doi: 10.1007/s10461-013-0437-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gutin SA, Harper GW, Moshashane N, Ramontshonyana K, Stephenson R, Shade SB, et al. Relationship, partner factors and stigma are associated with safer conception information, motivation, and behavioral skills among women living with HIV in Botswana. BMC Public Health. 2021;21: 2231. doi: 10.1186/s12889-021-12268-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Assessment of Vehicular Pollution in China: Journal of the Air & Waste Management Association: Vol 51, No 5. [cited 19 Oct 2022]. Available: https://www.tandfonline.com/doi/abs/10.1080/10473289.2001.10464300. [DOI] [PubMed]
- 16.Kenny DA, Ledermann T. Detecting, measuring, and testing dyadic patterns in the actor–partner interdependence model. J Fam Psychol. 2010;24: 359–366. doi: 10.1037/a0019651 [DOI] [PubMed] [Google Scholar]
- 17.Stas L, Kenny DA, Mayer A, Loeys T. Giving dyadic data analysis away: A user-friendly app for actor–partner interdependence models. Pers Relatsh. 2018;25: 103–119. doi: 10.1111/pere.12230 [DOI] [Google Scholar]
- 18.Cook R, Hayden R, Weiss SM, Jones DL. Desire for fertility among HIV-seroconcordant and -discordant couples in Lusaka, Zambia. Cult Health Sex. 2014;16: 741–751. doi: 10.1080/13691058.2014.902103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finger JL, Clum GA, Trent ME, Ellen JM. Desire for pregnancy and risk behavior in young HIV-positive women. AIDS Patient Care STDs. 2012;26: 173–180. doi: 10.1089/apc.2011.0225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hashemzadeh M, Shariati M, Mohammad Nazari A, Keramat A. Childbearing intention and its associated factors: A systematic review. Nurs Open. 2021;8: 2354–2368. doi: 10.1002/nop2.849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Breitnauer BT, Mmeje O, Njoroge B, Darbes LA, Leddy A, Brown J. Community perceptions of childbearing and use of safer conception strategies among HIV-discordant couples in Kisumu, Kenya. J Int Aids Soc. 2015;18: 19972. doi: 10.7448/IAS.18.1.19972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Joseph Davey DL, Wall KM, Kilembe W, Khu NH, Brill I, Vwalika B, et al. Difficult decisions: Evaluating individual and couple-level fertility intentions and HIV acquisition among HIV serodiscordant couples in Zambia. PLoS ONE. 2018;13. doi: 10.1371/journal.pone.0189869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Joseph Davey D, West S, Umutoni V, Taleghani S. A Systematic Review of the Current Status of Safer Conception Strategies for HIV Affected Heterosexual Couples in Sub-Saharan Africa. AIDS Behav. 2018;22: 2916–2946. doi: 10.1007/s10461-018-2170-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Skerritt L, Kaida A, O’Brien N, Burchell AN, Bartlett G, Savoie E, et al. Patterns of changing pregnancy intentions among women living with HIV in Canada. Bmc Womens Health. 2021;21: 350. doi: 10.1186/s12905-021-01492-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tang Z., Confucianism Chinese culture, and reproductive behavior. undefined. 1995. [cited 14 May 2021]. Available: /paper/Has-the-Chinese-family-planning-policy-been-in-Merli-Smith/f2e4a530664c40f925162d322669927137b67193. [Google Scholar]
- 26.Sallam H, Sallam N. Religious aspects of assisted reproduction. Facts Views Vis ObGyn. 2016;8: 33–48. [PMC free article] [PubMed] [Google Scholar]
- 27.Miller W, Pasta D. Behavioral Intentions: Which Ones Predict Fertility Behavior in Married Couples?1. J Appl Soc Psychol. 2006;25: 530–555. doi: 10.1111/j.1559-1816.1995.tb01766.x [DOI] [Google Scholar]
- 28.Li L, Wu Z, Wu S, Jia M, Lieber E, Lu Y. Impacts of HIV/AIDS Stigma on Family Identity and Interactions in China. Fam Syst Health J Collab Fam Healthc. 2008;26: 431–442. doi: 10.1037/1091-7527.26.4.431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Agadjanian V, Hayford SR. HIV status, fertility intentions, and contraception in the era of expanded access to antiretroviral therapy: A case study of rural Mozambique. Glob Public Health. 2018;13: 582–596. doi: 10.1080/17441692.2016.1268188 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kaida A, Laher F, Strathdee SA, Janssen PA, Money D, Hogg RS, et al. Childbearing Intentions of HIV-Positive Women of Reproductive Age in Soweto, South Africa: The Influence of Expanding Access to HAART in an HIV Hyperendemic Setting. Am J Public Health. 2011;101: 350–358. doi: 10.2105/AJPH.2009.177469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aliyu MH, Sam-Agudu NA, Shenoi S, Goga AE, Ramraj T, Vermund SH, et al. Increasing male engagement in the prevention of vertical transmission of HIV: what works in sub-Saharan Africa? BMJ. 2019;365: l1965. doi: 10.1136/bmj.l1965 [DOI] [PMC free article] [PubMed] [Google Scholar]