Abstract
Background
Homelessness is an extreme form of social exclusion, with homeless people experiencing considerable social and health inequities. Estimates of morbidity and mortality amongst homeless populations is limited due to the lack of recording of housing status across health datasets. The aim of this study is to: (i) identify a homelessness e-cohort by linking routine health data in Wales, and (ii) explore whether a period of reported past homelessness, places this population at greater risk of morbidity and mortality.
Methods
Homelessness identified through linkage across primary, secondary care and substance misuse datasets in the Secure Anonymised Information Linkage (SAIL) Databank. Mortality was examined through linkage to the Office for National Statistics mortality data.
Results
E-cohort of 15 472 individuals with lived experience of homelessness identified. Of those, 21 individuals died between February and July 2020 involving coronavirus disease of 2019 (COVID-19). Those with lived experience of homelessness had increased mortality from many causes including accidents, liver diseases and suicides.
Conclusion
Linking multiple routine datasets provides a more comprehensive dataset of a marginalized population, including individuals who are not included in government homeless statistics. Application of the cohort demonstrated that individuals with lived experience of homelessness have increased mortality involving COVID-19 and other causes. The underlying reasons, health needs and causes of death warrant further exploration.
Keywords: COVID-19, homelessness, housing, mortality, record linkage
Introduction
Social inequalities are observed in historical pandemics1 and evidence for the coronavirus disease of 2019 (COVID-19; severe acute respiratory syndrome coronavirus 2) pandemic suggests similar disproportionate impact on the already disadvantaged.1,2 Contributing factors include underlying inequalities and higher prevalence of underlying chronic disease.1
Homelessness is a complex and persistent public health challenge3,4 and extreme form of social exclusion,5,6 affecting at least 7% of the Welsh adult population.7 Homelessness can be chronic, episodic or transitional,5,8 and defined as lacking adequate housing or living in housing below a minimum adequacy standard.9 This population experience extreme health inequities,6 have a higher proportion of multiple, complex health needs10–12 and high excess mortality.6,13,14 Data from England and Wales show that mean age of mortality in both sexes is over 30 years younger compared with the general population.14
By June 2020, 16 deaths were reported in the currently homeless population in England where COVID-19 was mentioned on the death certificate (none in Wales).15 Yet a lack of reliable data on homelessness status in routine health and care data means a likely underestimate of homelessness and resulting health impact.4,16 The aim of this study is to generate a population-based retrospective e-cohort of people with lived experience of homelessness using linked routine health data, and to examine mortality including during the COVID-19 pandemic.
Methods
We adopted a broad definition of ‘lived experience of homelessness’ to include street homelessness and precarious/insecure housing,4,8–10,17 thus including ‘hidden homeless’ who are not in government homelessness statistics. All individuals in Wales who accessed National Health Service (NHS) for any activity at any point since 2014 and had a homelessness/precarious housing code in one or more of four datasets held in the Secure Anonymised Information Linkage (SAIL) Databank were flagged as having ‘lived experience of homelessness’ and included in our e-cohort (Fig. 1, Supplementary Material). A unique anonymous linkage field for each individual was used to link across datasets at individual level.18,19 We generated descriptive statistics and compared these with population estimates since 2014.20
Fig. 1 .
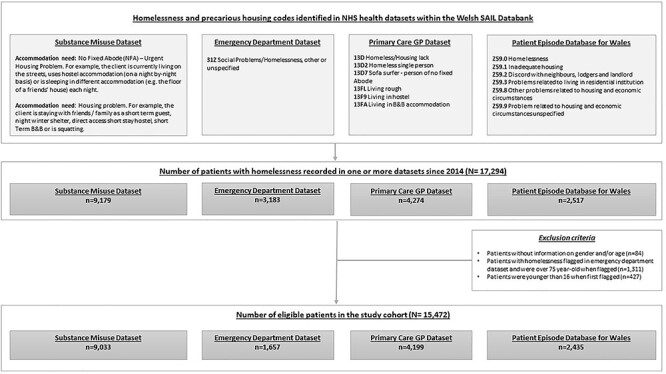
Flow diagram of the construction of our e-cohort of individuals with lived experience of homelessness.
Results
Cohort characteristics
We identified 15 472 individuals with lived experience of homelessness in Wales since 2014, when the Housing (Wales) Act 2014 came into force. Of these, 10 609 (68.6% versus 48.8% in the general population) were male. The first time they appeared in the cohort, 7107 (45.9% versus 29.0%) were between 16 and 34 years old, and 462 (3.0% versus 11.2%) were above 75.
Deaths between January 2014 and July 2020
We linked our e-cohort with the Office for National Statistics mortality data. In total, 1286/15 472 (8.3%) of our e-cohort died between January 2014 and July 2020. Of these, 882/1286 (68.6%) were male and 335/1286 (26.0%) under 45 years old when they died.
We compared underlying causes of deaths21 registered for the following three cohorts (Fig. 2 and Table A1, Supplementary Material).
Fig. 2 .
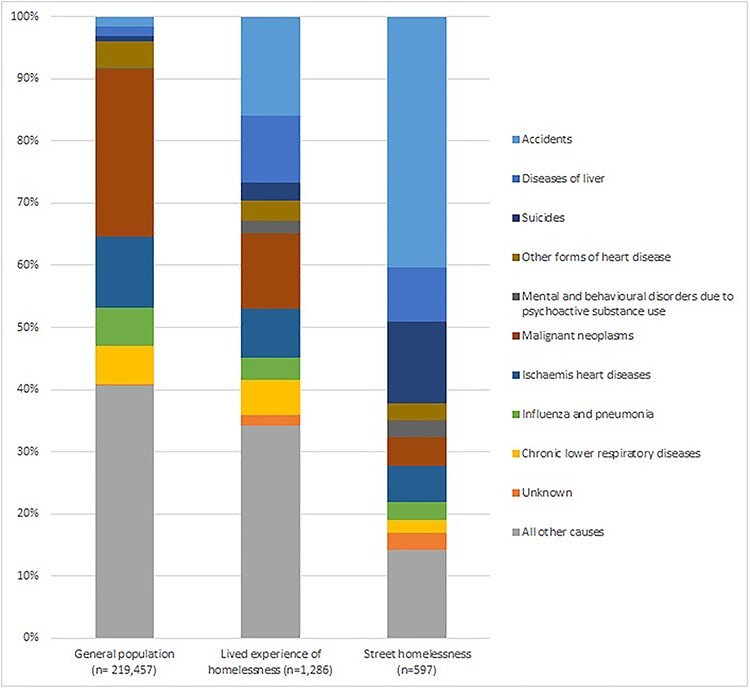
Comparison on underlying causes of death between three cohorts.
General population mortality data (Wales) since 2014 (ONS Deaths);
Our e-cohort ‘lived experience of homelessness’ since 2014 (Wales);
Street homelessness (England and Wales) estimated deaths in England and Wales 201714.
Figure 2 (Supplementary Material) demonstrates how our e-cohort differs to the general population and the street homelessness cohorts. In our e-cohort, deaths from accidents and suicides, and mental and behavioral disorders due to psychoactive substance use, are higher than the general population but lower than the street homelessness cohort.
Deaths during the COVID-19 pandemic
The first confirmed case of COVID-19 in the UK was on 29th January 2020. Between February and July 2020, 141 deaths occurred within our e-cohort. In total, 101/141 (71.6% versus 49.6% in the general population) of the deaths were in males. And, 16/141 (11.3% versus 1.7%) were under 45 years old when they died. Of these, 21/141 (14.9% versus 13.9%) deaths were registered as COVID-19 involved.
Conclusions
Our study created a unique, reproducible e-cohort of individuals across Wales with recorded lived experience of homelessness from multiple NHS datasets that can be used for rapid analysis of health needs and mortality as demonstrated here during COVID-19. A key strength is that we bring together routine data from multiple services, providing a more comprehensive assessment of population health needs. This e-cohort allows for efficient, retrospective privacy-protected follow-up of individuals in healthcare systems, and be used to evaluate future initiatives supporting this vulnerable population.
Compared to similar data linkage studies,22 we used a broader definition of homelessness and did not restrict homelessness as recorded by single healthcare service. This includes those not in government homeless statistics. Our results suggest that this more diverse group have poorer health outcomes than the general population, but not as poor as the street homeless. This is an important consideration for service planning and policy where early identification of precarious housing situations may better inform integrated support.
Previous attempts to understand mortality in the street homeless during COVID-19 found no COVID-related deaths in Wales.14 However, we identified 141 individuals with ‘lived experience of homelessness’ in Wales who died during the pandemic, 21 of whom died with COVID-19. This supports that poorer health combined with complex longer-term health needs7 may amplify prevalence and severity of COVID-19.1,23 We will further explore the differences in causes of death in this group.
Despite drawing on wide expertise to develop a comprehensive code list to identify homelessness and apply this to understand the healthcare needs, this study has a number of limitations. First, it relies on this population seeking health care and disclosing their homeless/housing status, where there are recognized barriers.4,24 Second, there are systematic differences in recording non-health patient information in routine health and care data, for example, in substance misuse data housing status is systematically recorded but in primary care it may be better recorded in settings with a special interest in addressing the health needs of homeless populations. Therefore, these biases contribute to underestimating population size and health needs. Like other studies using routine electronic records, this study also suffers from incomplete control of confounders, i.e. composition for homeless families. These limitations highlight the critical importance of explicit recording good quality homelessness status in health practice.25
Ethics statement
This study is based on anonymized routinely collected electronic health records. All routinely collected anonymized data held in SAIL Databank are exempt from consent due to the anonymized nature of the databank (under section 251, National Research Ethics Committee (NREC)). We have applied and been granted approval by the independent Information Governance Review Panel (IGRP) for permission to conduct this study (project number 0968). The IGRP contains independent members from NREC and British Medical Association (BMA), as well as lay members. The review process has checked that the study is useful, not service evaluation, and will not break anonymization standards.
Supplementary Material
Acknowledgments
We would like to thank the following expert clinicians and stakeholders for their contribution in scoping and reviewing how to capture homelessness in routine data: Dr Simon Braybrook and Dr Kay Saunders (Butetown Medical Practice); Hannah Browne-Gott, Dr Peter Mackie, Dr Naomi Stanton and Dr Ian Thomas (Cardiff University); Asim Butt (Mortality, Office for National Statistics); Rebecca Jackson (Shelter Cymru); Adam Golten and Alex Osmond (The Wallich) and Judith David (Environment, Sustainability and Housing Stats Welsh Government).
We would like to thank Ashley Akbari (Swansea University) for project support in SAIL Databank.
This study makes use of anonymized data held in the Secure Anonymised Information Linkage Databank. We would like to acknowledge all the data providers who make anonymized data available for research.
Jiao Song, Dr, Principal Statistician
Charlotte N.B. Grey, Dr, Public Health Evaluation Lead
Alisha R. Davies, Professor, Consultant in Public Health, Head of Research and Development
Contributor Information
Jiao Song, Research & Evaluation Division, Knowledge Directorate, Public Health Wales, Cardiff, CF10 4BZ, UK.
Charlotte N B Grey, Research & Evaluation Division, Knowledge Directorate, Public Health Wales, Cardiff, CF10 4BZ, UK.
Alisha R Davies, Research & Evaluation Division, Knowledge Directorate, Public Health Wales, Cardiff, CF10 4BZ, UK.
Funding
This research was funded internally through Public Health Wales.
Conflict of interest
The authors declare that there is no conflict of interest.
References
- 1. Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Tsai J, Wilson M. COVID-19: a potential public health problem for homeless populations. Lancet Public Heal. 2020;(April):e186–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mabhala MA, Yohannes A, Griffith M. Social conditions of becoming homelessness: Qualitative analysis of life stories of homeless peoples. Int J Equity Health. 2017;16(1):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dorney-smith S, Schneller K, Aboim S. Meeting the healthcare needs of people experiencing homelessness. Nursing Standard, 2018. doi: 10.7748/ns.2018.e11155 [DOI] [PubMed]
- 5. Benjaminsen L, Knutagård M. Homeless research and policy development: examples from the Nordic Countries. Eur J Homelessness. 2016;10(3):45–66. [Google Scholar]
- 6. Aldridge RW, Story A, Hwang SWet al. Morbidity and mortality in homeless individuals, prisoners, sex workers, and individuals with substance use disorders in high-income countries: a systematic review and meta-analysis. Lancet [Internet] 2017;391(10117):241–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Grey CNB, Woodfine L. Voices of Those with Lived Experiences of Homelessness and Adversity in Wales: Informing Prevention and Response. Public Health Wales NHS Trust. Cardiff, 2019. [Google Scholar]
- 8. Casey S. Snakes and ladders: women’s pathways into and out of homelessness. Compet Visef Proc Natl Soc Policy Conf 1995;2001(2002):75–90. [Google Scholar]
- 9. Amore K, Baker M, Howden-Chapman P. The ETHOS definition and classification of homelessness: an analysis. Eur J Homelessness [Internet]. 2011;5(2):19–37. [Google Scholar]
- 10. Adebowale V. There is no excuse for homelessness in Britain in 2018—homelessness is a neon sign that something is fundamentally wrong. BMJ. 2018;360:1–2. [DOI] [PubMed] [Google Scholar]
- 11. McDonagh T. Tackling Homelessness and Exclusion: Understanding Complex Lives. Joseph Rowntree Foundation: York, 2011. [Google Scholar]
- 12. Shelton K, Taylor P, Bonner A, Bree M. Risk factors for homelessness: evidence from a population-based study. Psychiatr Serv. 2009;60(4):465–72. [DOI] [PubMed] [Google Scholar]
- 13. The Faculty for Homeless and Inclusion Health . Homeless and Inclusion Health Standards for Commissioners and Service Providers, Pathway - healthcare for homeless people, London, 2018.
- 14. Georgeson B. Statistical Bulletin. Deaths of Homeless people in England and Wales: 2013 to 2017 [Internet]. 2018. Available from: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsofhomelesspeopleinenglandandwales/2013to2017 (25 November 2020, date last accessed).
- 15. Georgeson B, Martin J. Coronavirus and Deaths of Homeless People, England and Wales: Deaths Registered up to 26 June 2020 [Internet]. 2020. Available from:https://www.ons.gov.uk/releases/deathsofhomelesspeopleinvolvingcovid19englandandwalesdeathsregisteredupto26june2020 (25 November 2020, date last accessed).
- 16. Edgar B, Doherty J. Homelessness Research in Europe, FEANTSA, Brussels, 2010.
- 17. Mccoy S, Hug B. Danger Zones and Stepping Stones: Young People’s Experiences of Hidden Homelessness, British Association of Social Workers, Birmingham, 2016.
- 18. Ford DV, Jones KH, Verplancke JPet al. The SAIL Databank: building a national architecture for e-health research and evaluation. BMC Health Serv Res. 2009;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Lyons RA, Jones KH, John Get al. The SAIL databank: linking multiple health and social care datasets. BMC Med Inform Decis Mak. 2009;9(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Welsh Government . National Level Population Estimates by Year, Age and UK Country [Internet]. StatsWales. 2021. Available from: https://statswales.gov.wales/Catalogue/Population-and-Migration/Population/Estimates/nationallevelpopulationestimates-by-year-age-ukcountry (8 March 2021, date last accessed).
- 21. Aldridge RW. Causes of death among homeless people: a population-based cross-sectional study of linked hospitalisation and mortality data in England. In: [Dataset]: Extended Data File 3: ICD-10 Codes Used to Classify Underlying Causes of Death Groups in Figure 2, 2019. [DOI] [PMC free article] [PubMed]
- 22. Aldridge RW, Menezes D, Lewer Det al. Causes of death among homeless people : a population-based cross-sectional study of linked hospitalisation and mortality data in England. Wellcome OPen Res 2019;(May):1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Perri M, Dosani N, Hwang SW. COVID-19 and people experiencing homelessness: challenges and mitigation strategies. CMAJ. 2020;192(26):E716–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Public Health England . Homelessness Applying All Our Health [Internet]. Public Health England, London, 2016. Available from: https://www.gov.uk/government/publications/homelessness-applying-all-our-health/homelessness-applying-all-our-health (10 March 2021, date last accessed).
- 25. Whiteford M, Simpson G. “There is still a perception that homelessness is a housing problem”: devolution, homelessness and health in the UK. Housing, Care Support. 2016;19(2):33–44. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


