Abstract
Recent years have witnessed an increased demand for mobile health (mHealth) platforms owing to the COVID-19 pandemic and preference for doorstep delivery. However, factors impacting user experiences and satisfaction levels across these platforms, using customer reviews, are still largely unexplored in academic research. The empirical framework we proposed in this paper addressed this research gap by analysing unmonitored user comments for some popular mHealth platforms. Using topic-modelling techniques, we identified the impacting factors (predictors) and categorised them into two major dimensions based on strategic adoption and motivational association. Findings from our study suggest that time and money, convenience, responsiveness, and availability emerge as significant predictors for delivering a positive user experience on m-health platforms. Next, we identified substantial moderating effects of review polarity on the predictors related to brand association and hedonic motivation, such as online booking and video consultation. Further, we also identified the top predictors for successful user experience across these platforms. Recommendations from our study will benefit business managers by offering an improved service design leading to higher user satisfaction across these m-health platforms.
Keywords: Mobile health, Service-dominant logic, Machine learning, Text analytics, Proportional-odds logit
1. Introduction and motivation
Mobile-healthcare (mHealth) applications are mobile-based platforms that allow providers (i.e., pharmacies, doctors, healthcare institutions, and clinical laboratories) to reach the consumers (i.e., patients). They offer services for chronic conditions, remote monitoring, patient data, electronic records, and prescriptions, sometimes including fitness and wellness applications. According to a Statista Report1 , the global mHealth market was estimated at USD 23 billion in 2016 and is expected to reach nearly USD 190 billion by 2025. The World Health Organization has also emphasised “patient empowerment” among the significant goals in their Health Policy Framework2 , thereby supporting the increased usage of mHealth applications that allow more patient control. In this manner, mHealth platforms expect to improve the communication between healthcare providers and patients, increase their satisfaction levels, and lead to higher success rates of health-related outcomes (Lamprinos et al., 2016, Tartaglione et al., 2018, Wakefield et al., 2018, Ghose et al., 2021, Yang et al., 2022).
Nevertheless, several challenges still plague mHealth apps, affecting the overall experience the customers (i.e., patients) enjoy during usage. In a recent survey conducted by Accenture3 across 1800 people in the United States, the users reported that they would be more likely to adopt mHealth platforms only if there were adequate customer support (i.e., brand association), recommendations from the health provider (i.e., perceived quality), or if these technologies enabled them to receive better information about their health (i.e., utilitarian motivation). Using Fig. 1 , we explain a few of these constructs built using keywords extracted from the electronic word-of-mouth (eWOM) (i.e., online reviews) submitted for Practo App in India. These reasons motivate mHealth apps users to post reviews and final star ratings as an outcome of their overall “user experience”.Fig. 2. .
Fig. 1.
Online reviews for Practo mobile app demonstrate various sources of motivation for the user.
Fig. 2.
Factors that influence unwillingness to use remote clinical trials (Adapted from PWC Global Top Health Industry Issues 2021)(PwC Global Top Health Industry Issues 2021: https://www.pwc.com/gx/en/industries/healthcare/top-health-industry-issues.html).
Past literature has conclusively identified the impact of hedonic motivation that is observed from a hassle-free consultation and medicine delivery booking (Kim and Hwang, 2012, Dwivedi et al., 2016, Alam et al., 2020a, Biduski et al., 2020, Ashraf et al., 2021, Tran et al., 2021), on a consumer’s choice of mHealth app. The past studies also observed utilitarian motivations such as untethered payment and refund system, time and cost-effectiveness ( Kim and Hwang, 2012, Dwivedi et al., 2016, Ashraf et al., 2021, Tran et al., 2021) are also good motivators for app usage. Social motivation (Tran et al., 2021) and perceived quality are also antecedents of mHealth service quality. Our study reiterates the significance of these motivators (from a user’s perspective) while linking the strategic features (from a firm’s perspective) that an app requires to develop an overall conducive “user experience” (measured by the stars received on a mHealth app). Fig. 1 shows that reviews on certain features have stronger sentiments than others (Chatterjee, Goyal, Prakash, & Sharma, 2021). Also, some features of the mHealth apps were more critical to a given group of consumers than others (Tran et al., 2021). Extant studies have demonstrated that the sentiment polarity of eWOMs and social media platforms is a better measure of the direction of the sentiment as well as its strength rather than using the raw values of positive and negative polarities (Stieglitz and Dang-Xuan, 2013, Salehan and Kim, 2016). Such adjustment in the measurement of sentiment polarity prevents the unbalanced effect of one particular polarity (such as highly positive or highly negative) that can be present in the eWOMs related to the mHealth apps.
Further, according to the self-construal theory, the variations in self-construals can generate different levels of user motivation to use mHealth apps and lead to differential levels of user satisfaction. So, independent users are typically less dependent upon others and rely upon their internal thoughts, feelings, and actions for motivations. For instance, independent users might write the following eWOMs to express their personal experiences, such as “A fantastic doctor I personally want to recommend” or “My refund not sent”. On the contrary, interdependent users value social relationships and emphasise “fitting in” with other users. Therefore, interdependent users express their interconnectedness with a larger group of users for a mHealth app and might write: “Got doctor's consultation within 10 mins when my brother-in-law was in severe pain and needed doctors’ consultation. We could not go to the hospital due to Covid. This app turned out to be very helpful. Thanks, DocsApp! Cheers”. Our study aims to explain these differential ratings across various features and user groups by proposing two predictors - effective polarity (measured by the difference between “positive” and “negative” polarity) and reviewer-type (independent vs self-construal), thereby allowing scholars to measure the impact of each feature on user rating accurately.
1.1. Identification of gaps in the extant literature
A large body of literature has applied the theoretical frameworks of the Technology Acceptance Model (TAM), Unified Theory of Acceptance and Use of Technology (UTAUT and UTAUT2), and Expectation Confirmation Theory (ECT) to examine the adoption and usage continuance of mHealth applications across users (Wu et al., 2011, Lim et al., 2011, Gao et al., 2015, Chang et al., 2016, Cho, 2016, Dwivedi et al., 2016, Hoque and Sorwar, 2017, Kim et al., 2019, Alam et al., 2020a, Alam et al., 2020b, Chiu et al., 2020, Cho et al., 2020, Lim et al., 2021, Nusairat et al., 2021, Prakash et al., 2021, Suroso and Sukmoro, 2021). However, these theoretical frameworks overlooked the growing idea of shared decision-making among the caregivers (e.g., healthcare institutions, doctors) and care receivers (e.g., customers, patients) of mHealth applications.
Recently, a growing body of literature (Tartaglione et al., 2018, Russo et al., 2019, Balta et al., 2021, Dahl et al., 2021, Shirazi et al., 2021) examined mHealth applications and the factors responsible for their successful adoption with the application of service-dominant (SD) logic (Vargo and Lusch, 2004, Barrett et al., 2015). This unique view of looking at mHealth apps also matches the call for more scholarly studies by Stocchi, Pourazad, Michaelidou, Tanusondjaja, and Harrigan (2021) to develop “frameworks of value creation, value fusion, and value co-creation (including SD Logic) for apps and via apps.”.
Therefore, applying SD Logic in this study will enable us to understand the users’ motivation (i.e., hedonic, utilitarian, or social) and observe patients’ reactions by examining eWOMs. Here, the consumers (i.e., patients) transform themselves into central actors through ongoing information acquisition and exchange with their health providers before, during, and after service encounters (McKinley and Wright, 2014, Dahl et al., 2021). Some studies have also identified “poor user experience” as a significant impediment to repeated usage and continuance of mHealth applications among users (Akter et al., 2013b, Kim et al., 2019). Therefore, examining the significant dimensions of “user experience” and improving them will ensure sustainable growth for these apps through increased usage and user base.
This study also addressed a methodological gap in the past literature. Primarily, past researchers mainly relied upon user-based surveys (Azad-Khaneghah, Neubauer, Miguel Cruz, & Liu, 2021) to identify and examine various constructs of user satisfaction, popularity, and adoption of mHealth platforms, such as motivation (Tran et al., 2021), facilitating conditions (Alam et al., 2020a, Alam et al., 2020b), perceived service quality (Akter et al., 2013a, Akter et al., 2013b), service usability (Sadegh, Saadat, Sepehri, & Assadi, 2018), personalisation (Birkmeyer, Wirtz, & Langer, 2021), social networking (Birkmeyer et al., 2021), quality of care (Jannati, Nakhaee, Yazdi-Feyzabadi, & Tjondronegoro, 2021), privacy-protection mechanisms (Rodríguez-Priego, Porcu, & Kitchen, 2022), usage intensity (Veríssimo, 2018), cognitive and social factors (Nusairat et al., 2021, Rahimi and Khoundabi, 2021). However, the excessive reliance of past scholarly studies on surveys as a data collection mechanism poses a methodological challenge by ignoring the vast repository of eWOM data from mHealth apps. Also the use of online reviews from mHealth platforms can serve as an advantage because they are collected from a broad sample pool and therefore diminish the associated instrument bias that could weaken the accuracy of the results (Müller, Junglas, Brocke, & Debortoli, 2016).
1.2. Role of COVID-19 pandemic as a motivator of mHealth app usage
The global health and financial crisis caused by the COVID-19 pandemic played a pivotal role in facilitating the growth of mHealth apps and reshaping the features that influence overall “user experiences”. For instance, the Zoom app generated revenues of USD 2.65 billion in 2020, followed by a 55 per cent rise to USD 4.10 billion. Subsequently, the lockdown of essential services that led to a rush to adopt e-commerce channels across all significant businesses4 influenced the healthcare business, too (e.g., mHealth and telemedicine services) (Webster, 2020). According to the Global Health Industry Report published by PwC 5 , 51 % of respondents had received virtual medical care (via mobile, email or text) during the quarantine periods, with 91 % willing to do so again in the future. In this manner, COVID-19 created an inflexion point for consumers to adopt and use mHealth applications. Incorporating COVID-19 as a motivator to examine mHealth apps and related eWOM data from the related timeline also allows us to align this study with the recent calls from high-impact journals in business management - “services” theme (Hashemi, Rajabi, & Brashear-Alejandro, 2022); “COVID-19 & digital healthcare” (Verma & Gustafsson, 2020); consumer-centred healthcare (Kraus, Schiavone, Pluzhnikova, & Invernizzi, 2021); “home healthcare services” (Tsiotsou & Boukis, 2022); “scaling virtual contactless services” (Rai, 2020); “information systems value and success in the context of the COVID-19 pandemic” (Ågerfalk, Conboy, & Myers, 2020).
Therefore, in this study, we address the abovementioned research gaps by answering the following three primary research questions:
RQ1: What are the major features that impact the user experience in a mHealth platform during the pandemic?
RQ2a: How does a review’s effective polarity influence the impact of application features on users’ experience?
RQ2b: To what extent does reviewer type (independent/self-construal) influence the impact of hedonic motivation on user experience?
RQ3: What strategies can a mHealth platform adopt to improve its users’ experience based on reviews during the pandemic?
Our study answers the above research questions by performing an in-depth analysis of users’ reviews. We studied the factors influencing user experience based on an extensive literature review. The factors are then used to perform a textual analysis of reviews we collected from multiple mHealth apps. The resultant impact is then revealed by the relationship between the factors, reviews and user ratings. Our study helps in providing guidelines to mobile app developers, technology consultants, and researchers to improve these mHealth platforms by addressing the existing concerns and enhancing the users’ experience.
The remaining part of the paper is structured as follows. Section 2 summarises the background literature on mHealth applications and their theoretical foundations. Section 3 explains the collection of the research data and methodology. Section 4 presents the empirical modelling adopted in our study. Section 5 presents the results, while Section 6 discusses its significant findings. Section 7 discusses the implications of the study while Section 8 concludes the paper and offers the scope for future research. Section 7 concludes the paper and offers the scope for future research.
2. Literature review and theoretical foundation
We examined prior academic works on mHealth before and after the pandemic. Most of the research studies before 2020 have been focused on technology adoption, while most of the research work after 2020 is based on value co-creation and customer rating. These findings clearly show a shift in healthcare IT research after 2020, from adoption-centric to consumer-centric. Kraus et al. (2021) claimed that operational efficiencies and a patient-centric approach could achieve digital transformation in healthcare. Operational efficiency is obtained through resource quality and responsiveness, while the patient-centric approach includes hedonic, social, and utilitarian motivation. Verma and Gustafsson (2020) also highlighted the effect of COVID-19 on digital healthcare (i.e., telemedicine, robust surveillance and wearable devices, and diagnostic and clinical decision-making technologies) that will lead to new operating models to cope with the changing demand pattern by remaining agile and productive. Recent literature reviews are also available that (i) examine mHealth apps for individuals with chronic conditions and diseases (Lorca-Cabrera et al., 2021), (ii) compare measurement scales that were used to evaluate the usability and quality of mHealth apps (Azad-Khaneghah et al., 2021), (iii) mHealth interventions (Yang & Kovarik, 2021) and (iv) identify the factors of acceptance and user behaviour of mHealth users (Wang & Qi, 2021).
2.1. Mobile applications for healthcare
Scholarly research in healthcare information systems has focused on continued usage and behavioural intention to use mHealth apps. The academic research published before 2020 is mostly focused on “actual usage” (Alam et al., 2020a, Azad-Khaneghah et al., 2021, Veríssimo, 2018) and mHealth app evaluations (Nouri et al., 2018, Sadegh et al., 2018), while the focus on value co-creation (Balta et al., 2021, Shirazi et al., 2021) and customer satisfaction (Chatterjee et al., 2021, Jannati et al., 2021) is relatively new. Survey-based research and literature review have shown extensive dominance in terms of methodology, while text-mining and sentiment analysis have been applied only in a few research studies (Chatterjee et al., 2021, Shah et al., 2021). Similarly, owing to the extensive development in application offering based on sharing economy, research on service-dominant logic (S-D logic) has come to the forefront (Peltier et al., 2020, Tran et al., 2021), while the Technology Acceptance Model (TAM) (Lim et al., 2011, Birkmeyer et al., 2021, Nusairat et al., 2021), Unified Theory of Acceptance and Use of Technology (UTAUT) (Dwivedi et al., 2016, Suroso and Sukmoro, 2021, Wu et al., 2022, Zhang et al., 2022), Service Quality theory (SERVQUAL) (Akter et al., 2013a, Akter et al., 2013b, Shah et al., 2021) continue to be a favourable topic for researchers. Some other theories that were discussed on improving mHealth app usage are Expectation–Confirmation model (ECM) (Chiu et al., 2020, Prakash et al., 2021), Resource-Based View (), Theory of Planned Behavior (TPB) (Kim et al., 2019, Stocchi et al., 2021), Protection Motivation Theory (PMT) (McKinley and Wright, 2014, Gao et al., 2015).
We have also analysed existing research to understand the coveted features of users’ expectations from a mHealth application. The most important factor remains the app's overall effectiveness, perceived usefulness and performance (Chang et al., 2016, Veríssimo, 2018, Kim et al., 2019, Biswas et al., 2021, Kraus et al., 2021). However, factors such as (i) trust (Prakash et al., 2021, Wu et al., 2022), (ii) perceived security (Zhao, Ni, & Zhou, 2018), (iii) ease of use (Cho et al., 2020, Biswas et al., 2021), (iv) self-efficacy and control (Dwivedi et al., 2016, Tsiotsou and Boukis, 2022), (v) personalisation (Gimpel, Manner-Romberg, Schmied, & Winkler, 2021), (vi) user satisfaction (Akter et al., 2013a, Akter et al., 2013b, Birkmeyer et al., 2021) and (vii) hedonic and utilitarian motivation (Kim et al., 2019, Tran et al., 2021) have gained importance in the overall evaluation of applications. Customer sentiment is highly important in almost all research (Chatterjee et al., 2021) using eWOMs. User perception about apps’ features that are identified as effective polarity thus influences their motivation to use an application. In Table 1 , we also observe that customer characteristics influence user acceptance of mHealth apps. Further, Tran et al. (2021) explained users with an independent self-construct are more likely to be impacted by hedonic motivations.
Table 1.
Summary of factors from the existing literature on mHealth applications.
Further, we observed that certain factors have specifically gained importance in the post-2020 pandemic period. Factors such as (i) convenience (Balta et al., 2021, Jannati et al., 2021), (ii) responsiveness (Dahl et al., 2021, Gimpel et al., 2021), (iii) sentiment analysis (Chatterjee et al., 2021, Zhang et al., 2022), (iv) customer support (Kraus et al., 2021, Tsiotsou and Boukis, 2022), and (v) competition (Li et al., 2020, Chiu et al., 2020) have obtained considerable significance in the success of mHealth apps post COVID-19 pandemic. The impact of the pandemic, however, has never been taken as a significant contributing factor to the digital transformation of healthcare (Webster, 2020, Verma & Gustafsson, 2020). Further, Stocchi et al. (2021) mentioned a pressing need for “new frameworks outlining and evaluating strategies for apps’ introduction.” Table 1 classifies existing literature into pre-COVID and post-COVID eras and their discussion topics.
Our study has considered these factors while developing a theoretical model that categorises the discussion themes in most reviews. Our work contributes to the text mining-based research in determining mHealth app features. Earlier, Lim et al. (2021) worked on ride-sharing app services where semi-structured interviews, text-mining and topic modelling of app reviews and PLS-SEM on passenger survey responses were used to obtain the essential mHealth app features. Shah et al. (2021) used text-mining, topic modelling and sentiment analysis to create a strategic SWOT framework for healthcare organisations to improve patient satisfaction. Tran et al. (2021) obtained features based on a survey for S-D logic-based research to enhance the brand equity of branded apps. Our study also aims to contribute further using the factor’s coefficient values comparing a mHealth app against its competitors. This objective is achieved by developing a score for the mHealth apps based on “three different sharing economy differentiation strategies” (Frey, Trenz, & Veit, 2019), i.e., technology, partnership and user experience. Thus, our study contributes to mHealth app managers by identifying the essential features that impact user ratings and presenting a strategic view of their position compared to the competitors.
2.2. Theoretical Foundation: Value co-creation in mobile-health platforms
In this study, we apply the theoretical framework of the “Service-Dominant” (S-D) Logic (Vargo and Lusch, 2004, Vargo and Lusch, 2008a, Vargo and Lusch, 2008b) to understand the value co-creation activities that occur when a typical user is consuming the services of mHealth applications by ordering medicines, healthcare services such as telemedicine consultations and diagnostic tests. Vargo and Lusch (2008b) have suggested that S-D logic could provide the foundation for a revised theory of the firm (and other resource-integrating activities), a theory of service systems (Maglio & Spohrer, 2008), and a revised theory of economics and society. We look at how S-D Logic helps us to re-look at these mHealth applications and the related activities that involve multiple actors, including the user(s), the mHealth platform and the caregiver (doctors/consultants).
On the one hand, traditional healthcare services that are designed around the “goods-dominant” (G-D) logic (Vargo and Lusch, 2004, Vargo and Lusch, 2008a, Vargo and Lusch, 2008b), where the patient (or care-receiver) visits the physical premises of the healthcare service provider such as the pharmacy or the hospital to receive medical services such as advice, prescription drugs or treatments. According to the G-D logic, the economic exchange of goods (here medicines and related products) acquire value during their design and manufacturing (Vargo & Lusch, 2004). Ideally, in G-D logic, “this output is tangible, produced away (separate) from the interference of customers, standardisable and capable of being inventoried until sold, all to enable maximum efficiency in operations” (see p. 34, Vargo & Akaka, 2009). On the other hand, are the mHealth applications where the technology (i.e. the mHealth platform) enhances the “value co-creation” of the healthcare services offered to the end-user. The next level of value co-creation takes place when the supplier (or the m-health platform and service provider) and the customer (or the mHealth user) join in a reciprocally symbiotic value-exchange mechanism (Sheth, 2019). Further, the foundational premises of S-D Logic (Vargo & Akaka, 2009), i.e., “FP4: Operant resources are the fundamental source of competitive advantage” and “FP6: The customer is always a co-creator of value”, clearly reflect the theoretical motivation behind our research. Therefore, the mHealth platform is not only meant to offer its resources and collaborate with the users but also to co-create value based on the user's approval.
Now, let us look at the constructs of our study through the theoretical lens of S-D Logic. Each construct we define in our study builds upon this idea of “value co-creation” rather than the process of singular creation and delivery of value to the customer. For instance, the “utilitarian motivation” construct consists of the following variables: “time and money”, “payment”, “convenience”, “refund”, and “lockdown”. Among those variables, “time and money” is measured by how the mHealth App usage helps to save the user’s time and money and, therefore, includes the perception of the cost of service - which directly links to both the user and the firm (or the mHealth platform). Similarly, the construct “perceived quality” consists of the following variables - “responsiveness”, “effectiveness”, and “resource quality.” Now, “responsiveness” is measured by the agility of the responses by the firm’s resources (such as doctors and clinicians) to user’s needs with diligence - which is again a combination of the values co-created by the user and the firm (or the mHealth platform). The proposed conceptual framework for this study depicting all the constructs and their associated variables is presented in Fig. 3 .
Fig. 3.
Conceptual framework to explore the predictors of user experience in mHealth applications.
Finally, recent academic research (Tartaglione et al., 2018, Russo et al., 2019, Balta et al., 2021, Dahl et al., 2021, Pop et al., 2018, Shirazi et al., 2021) suggests that the “user experience” and the related “customer value” are now generated from a collaborative ecosystem, unlike the traditional channels. The S-D logic also recognises mHealth platforms as unique service systems that behave as “dynamic value co-creation configurations of resources (people, technology, organisations, and shared information)” (Maglio & Spohrer, 2008: p. 19). Therefore, these mHealth platforms should be ideally viewed as a concerted and synchronously designed “value-in-use” service system (Maglio and Spohrer, 2008, Osei-Frimpong et al., 2018, Russo et al., 2019) instead of an isolated service-offering mechanism (represented by value-in-exchange).
3. Data collection
We collected users’ reviews and general information of nine mHealth care applications from India, namely, PharmEasy, Tata 1 MG, Apollo 24 X 7, Practo, Netmeds, Medibuddy, MFine, DocsApp and Tata Health, from the Google Play Store for three months starting from 1st June 2021 until 1st September 2021. Table 2 summarises the details (release date, download count, total review count by users, review count in 90 Days, total versions, rank in India, and last version update) for each of these apps till 1st September 2021. While we began our data collection with a total of 41,007 reviews, we removed 156 non-English reviews (such as in regional languages of India), leading to 40,852 reviews for final analysis.
Table 2.
Summary of mHealth applications used in our study.
| App Name | Release Date | Downloads (in 1000 s) | Review Count |
Reviews in last 90 days* |
Total Versions Released* |
Rank in India | Last Version Update | |
|---|---|---|---|---|---|---|---|---|
| PharmEasy | 06/03/2015 | 5000–10000 | 39,700 | 16,835 | 6 | 1 | 12/08/2021 | |
| Tata 1MG | 24/08/2012 | 5000–10000 | 20,400 | 8426 | 3 | 2 | 11/08/2021 | |
| Apollo 24 X 7 | 31/01/2020 | 5000–10000 | 17,100 | 5811 | 7 | 3 | 18/08/2021 | |
| Practo | 15/03/2014 | 5000–10000 | 13,500 | 1963 | 10 | 4 | 03/12/2021 | |
| Netmeds | 08/07/2015 | 5000–10000 | 12,300 | 4120 | 2 | 5 | 11/08/2021 | |
| Medibuddy | 07/07/2014 | 1000–5000 | 21,600 | 1724 | 9 | 9 | 06/12/2021 | |
| MFine | 28/09/2017 | 1000–5000 | 6000 | 187 | 3 | 10 | 03/12/2021 | |
| DocsApp | 14/04/2015 | 5000–10000 | 22,800 | 1601 | 4 | 21 | 10/06/2021 | |
| Tata Health | 13/02/2018 | 100–500 | 550 | 340 | 8 | – | 29/11/2021 | |
| * Data was collected from 1st June 2021 until 1st September 2021 for the analysis | ||||||||
Next, we categorised the independent variables for our study based on a bi-dimensional grid, as shown in Table 3 . This grid explains how each variable can be mapped to two unique dimensions simultaneously – motivational association and strategic adoption. The first dimension links to RQ1, while the second dimension links to RQ2 of our study. While motivational association can be of four types, namely (i) utilitarian motivation, (ii) hedonic motivation, (iii) brand support and loyalty, and (iv) perceived quality; strategic adoption can be of three types, namely (i) technology, (ii) partnership, and (iii) user experience.
Table 3.
Mapping of predictors according to their strategic adoption and motivational associations.
|
Strategic Adoption (Firm) |
||||
|---|---|---|---|---|
| Technology | Partnership | User Experience | ||
|
Motivational Association (User) |
Utilitarian Motivation | Payment |
Time and Money Convenience Refund Lockdown |
|
| Hedonic Motivation | Video Consultation | Online Booking | ||
| Brand Support and Loyalty | Customer Support Availability |
|||
| Perceived Quality | Responsiveness Resource Quality |
Effectiveness | ||
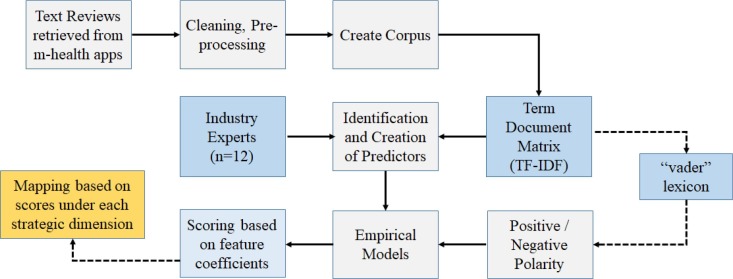
3.1. Using text mining to create new predictors
We applied relevant text-mining techniques to build novel motivational association-based predictors from the reviews received in the mHealth apps. That would help us to generate actionable insights for businesses (Tan, 1999). Text-mining often requires important steps such as cleaning the unstructured text data, pre-processing, and applying the text-mining techniques. In this study, data pre-processing included the following steps - removal of “English” stop-words, removal of punctuation marks (such as /, @, //), and removal of numbers and blank spaces to create the pre-processed corpus. We used the tm package in R to complete the data pre-processing steps and clean the unstructured textual data. For example, the review text “Superb experience in booking appointments always” would read as “superb experi in book appoint always” after pre-processing, text-cleaning, and stemming.
Next, we applied the stemming technique with the corpus generated from the review texts to find significant keywords and then used the TF-IDF scores (Salton and Buckley, 1988, Schütze et al., 2008, Biswas et al., 2021). We used the tm package in R to create the term-document matrix based on the TF-IDF scores. After this step, we consulted 12 experts from healthcare and e-commerce domains with varied profiles ranging from UX designers, operations managers, senior data analysts, and data engineers (presented in Table 4 ), who assisted us in creating the various service attributes that we presented in a novel wordlist (shown in Table 5 ). This lexicon consisted of 12 themes and associated word stems for each theme. These themes were mapped as predictors, which are binary (0 and 1), where “1″ indicates that word stem(s) for that particular category has been discussed in the eWOM and “0” indicates otherwise. Therefore, it is understandable that each review can belong to more than one category. In this manner, we built the predictors through data pre-processing and text-mining the reviews collected from the mHealth apps.
Table 4.
Details of experts for developing the lexicon.
| No. | Domain | Profile |
Avg. Exp. (in Years) |
|---|---|---|---|
| 2 | Healthcare e-commerce | Product and UX Designer | 3.5 |
| 1 | Business Analytics | Business Analyst | 4 |
| 2 | Product Management | Senior Data Analyst | 3 |
| 2 | Retail E-commerce | Lead Data Engineer | 6.5 |
| 1 | Healthcare Supply-chain | Operations Manager | 5 |
| 4 | Hospital/Medical Center | Senior Manager “Patient Experience” | 5.5 |
Table 5.
Mapping of predictors with associated word stems extracted from reviews.
| Predictor | Word stems |
|---|---|
| Time and Money | time, monei, experi, onlin, appoint, servic, chat, worst, even, wast, refund, paid, take |
| Payment | pay, monei, payment, deduct, paid, experi, ask, servic, chat, custom, need, time, fee, book, use, refund, avail, respond, now, month, talk, fee, free, charg |
| Convenience | conveni, find, help, appoint, good, thank, easi, connect, prescript, download |
| Refund | refund, monei, cancel, deduct, time, experi, appoint, ask, day, wait, onlin, book, paid, chat, bad, repli, amount, membership |
| Lockdown | lockdown, use, covid, pandem, day, thank, great, support, respons, pandem, time, help, situat, realli, helpless, hospit, covid, download |
| Online Booking | onlin, book, appoint, consult, call, servic, good, monei, chat, time, experi, even, cancel, worst, connect, prescript |
| Video Consultation | video, consult, call, appoint, time, onlin, chat, servic, worst, even, book, bad, messag, connect, virtual |
|
Customer Support |
custom, app, care, servic, consult, support, even, onlin, time, experi, appoint, chat, paid, number, call, contact, medicin, ask, cancel, pathet, day, bad, one, wast, feedback |
| Availability | availabl, wait, avail, time, experi, day, onlin, servic, medicin, use, appoint, chat, doc, good, monei, call, connect, download |
| Responsiveness | respons, quick, servic, time, experi, chat, custom, ask, give, take, support, proper, day, help, even, monei, question, prescript, feedback |
| Effectiveness | effectiv, plan, assign, question, wast, refund, paid, take, recommend, feedback, satisfi |
| Resource Quality | resourc, qualiti, avail, consult, nice, app, time, experi, question, medicin, review, fake, fair, wast |
3.2. Using sentiment analysis to create moderating variables
After building the preliminary empirical models, we focussed on creating the moderating variables by applying relevant text-analysis tools and techniques. Each review text can have a significant positive and negative polarity embedded within itself based on its sentence construction which can significantly influence the relationship of the primary predictors towards the user experience (here measured by the ratings received in the mHealth app). We then applied vader 6 lexicon to extract each review text's positive and negative sentiments. Recent studies have confirmed the efficacy of the vader as a powerful analyser of sentiments from online reviews (Kim et al., 2021, Tripathi et al., 2021). Next, we built a measure of effective polarity (“positive polarity” – “negative polarity”) based on extant studies that have demonstrated its superiority compared to using the raw values of positive and negative polarities separately (Stieglitz and Dang-Xuan, 2013, Salehan and Kim, 2016). Such adjustment in the sentiment polarity measurement prevents one particular polarity’s unbalanced effect.
Next, we divided the consumers of the mHealth apps according to self-construal behaviour into independent and interdependent types. The independent users were more concerned about their experience. They often used pronouns such as “I”, “we”, or “you” in sentences to express their personal experiences, such as “A fantastic doctor I personally want to recommend” or “My refund not send”. Reviewers with a more generalised opinion or view of application features are interdependent (i.e. social motivation) (Rahimi and Khoundabi, 2021, Tran et al., 2021), who might write reviews such as “Hello MFine Team, …… due to Covid-19 no doctor was available then I have used your services for my father who was in hometown and symptoms were for stroke but timely help within few minutes from the doctor from Bangalore has helped my family..” We completed the semantic parsing with the LIWC (Linguistic Inquiry and Word Count) tool (Pennebaker, Boyd, Jordan, & Blackburn, 2015). Recent studies have established the validity of LIWC in inferring psychometric properties from text (Biswas et al., 2020, Sengupta et al., 2021). The overall methodology is presented in Fig. 4 . Table 6 and Table 7 present the variables used in this study and their descriptive statistics, respectively.
Fig. 4.
Methodology.
Table 6.
Predictors of “user experience” in this study.
| S. No. | Variable | Brief Description | Literature Source |
|---|---|---|---|
|
Independent Variable Utilitarian Motivation |
|||
| 1 | Time and Money (U) | App usage helps save user’s time and money also includes the perception about cost of service (B) | Tran et al., 2021 |
| 2 | Payment (T) | The payment system is easy to use (B) | Tran et al. (2021) |
| 3 | Convenience (U) | Use of the application is more convenient than the physical experience of service (B) | Developed for this study |
| 4 | Refund (U) | Refund is received conveniently in case of service failure (B) | Developed for this study |
| 5 | Lockdown (U) | Whether review reflects that app has been helpful during lockdown (B) | Developed for this study |
| Hedonic Motivation | |||
| 6 | Online Booking (P) | Booking an appointment using the app can be done seamlessly according to review (B) | Tran et al. (2021) |
| 7 | Video Consultation (T) | Video consultation is done seamlessly according to review (B) | Developed for this study |
| Brand Support and Loyalty | |||
| 8 | Customer Support (P) | Active support from staff is available and effective in solving problems (B) | Tran et al. (2021) |
| 9 | Availability (P) | Whether the services are available or not (B) | Tran et al. (2021) |
| Perceived Quality | |||
| 10 | Responsiveness (P) | Resources such as doctors and clinicians respond to user’s needs with diligence (B) | Tran et al. (2021) |
| 11 | Effectiveness (U) | Service provided by doctors and labs meet users’ requirements (B) | Jannati et al. (2021) |
| 12 | Resource Quality (P) | Perceived quality of solutions/services received is good (B) | Jannati et al. (2021) |
| Moderating Variable | |||
| 13 | Positive Polarity | Positive polarity within user’s comment. Reflects user’s positive experience (N) | Chatterjee et al. (2021) |
| 14 | Negative Polarity | Negative polarity within the user’s comment. Reflects user’s negative experience (N) | Chatterjee et al. (2021) |
| 15 | Reviewer Type | If the user is specific towards their personal experience, more is the score (N) | Developed for this study |
| Dependent Variable | |||
| 16 | User Rating | Review rating assigned by the user after experiencing the app (N) | Chatterjee et al. (2021), Tran et al. (2021) |
| T - Technology; P - Partnership; U - User Experience; B - Binary variable (0 or 1); N-Numeric/Continuous variable | |||
Table 7.
Descriptive statistics for the variables used in this study.
| N | Mean | Std. Dev. | Max | Min | |
|---|---|---|---|---|---|
| Time and Money | 40,852 | 0.562 | 0.496 | 1.000 | 0.000 |
| Payment | 40,852 | 0.681 | 0.466 | 1.000 | 0.000 |
| Convenience | 40,852 | 0.434 | 0.496 | 1.000 | 0.000 |
| Refund | 40,852 | 0.538 | 0.499 | 1.000 | 0.000 |
| Lockdown | 40,852 | 0.595 | 0.491 | 1.000 | 0.000 |
| Online Booking | 40,852 | 0.705 | 0.456 | 1.000 | 0.000 |
| Video Consultation | 40,852 | 0.502 | 0.500 | 1.000 | 0.000 |
| Customer Support | 40,852 | 0.847 | 0.360 | 1.000 | 0.000 |
| Availability | 40,852 | 0.798 | 0.402 | 1.000 | 0.000 |
| Responsiveness | 40,852 | 0.854 | 0.353 | 1.000 | 0.000 |
| Effectiveness | 40,852 | 0.219 | 0.413 | 1.000 | 0.000 |
| Resource Quality | 40,852 | 0.768 | 0.422 | 1.000 | 0.000 |
| Positive Polarity | 40,852 | 0.181 | 0.194 | 0.826 | 0.000 |
| Negative Polarity | 40,852 | −0.089 | 0.123 | 0.000 | −0.835 |
| Reviewer Type | 40,852 | 0.097 | 0.125 | 1.000 | 0.000 |
| User Rating | 40,852 | 2.871 | 1.861 | 5.000 | 1.000 |
We create two separate word clouds from the mHealth reviews - one with positive emotions (Fig. 5a ) and the other with negative emotions (Fig. 5b ). Typically with a word cloud, we understand that the relative size of each keyword is proportional to its frequency of usage in the entire word corpus (Chatterjee et al., 2022, Grover et al., 2021, Malik et al., 2021). Similar to recent literature that has examined social media content by segregation based on emotions, we split the entire corpus of eWOMs based on positive and negative polarities (Chatterjee et al., 2022, Grover et al., 2021, Malik et al., 2021). Therefore, based on Figure 5 (a), we find that users of mHealth apps express their positive emotions with the help of the following keywords - “app”, “good”, “experi”, “help”, “best”, “easi”, “great”, “nice”, “thank” and “excel”. Furthermore, based on Figure 5 (b), we find that users of mHealth apps express their negative emotions with the help of the following keywords - “worst”, “app”, “experi”, “bad”, “waste”, “fake”, “fraud” and “support” (see Fig. 6a. and Fig. 6b. ).
Fig. 5a.
Word Cloud of mHealth reviews - positive emotions.
Fig. 5b.
Word Cloud of mHealth reviews - negative emotions.
Fig. 6a.
Feature Importance Plot from the Linear Regression Model (combined dataset).
Fig. 6b.
Feature Importance Plot from the Proportional-odds Logit Regression Model (combined dataset).
4. Empirical modelling
4.1. Using multiple linear regression for app-ratings
We applied multiple linear regression to build exploratory models that fit the rating data received from the mobile healthcare apps. We analysed the data as a whole and sub-category-wise according to each app separately. If the rating received in the mobile app by the customer be such that it follows a linear relationship with its predictors as follows:
| (1) |
In Eqn. (1), is the intercept and , , …., are the multiple linear regression coefficients. Therefore, the modified equation for our study is as follows:
| (2) |
4.2. Using proportional odds logit regression for app-ratings
Next, we applied the proportional odds logistic regression models due to possible non-linear relationships between the predictors and the dependent variable “rating”, which is categorical with an order of magnitude (values are 1, 2, 3, 4 and 5) (Agresti, 2003). We applied the proportional-logit odds regression in R using the polr package. We applied the proportional odds logistic regression to analyse the combined data and according to each app separately. Therefore, the generalised equation for the proportional-odds logistic regression in our study is as follows:
| (3) |
where and . Here, is the level of an ordered category with levels, and corresponds to independent variables as follows:
indicates a rating “1″ on the mHealth app;
indicates a rating “2″ on the mHealth app;
….…........... and.
indicates a rating “5″ on the mHealth app.
While the independent variables are denoted as follows:
indicates ;
indicates ;
….….......;
indicates .
4.3. Moderator-based modelling to build exploratory models
Next, we built additional empirical models to examine the moderating effects of “reviewer-type” and the “effective polarity” of the text messages. Therefore, the modified equation with moderator effects for our study is as follows:
| (4) |
## according to Stieglitz and Dang-Xuan (2013).
5. Results
We applied an assortment of empirical models in the R environment to estimate the main effects and moderating effects identified in the proposed framework. The detailed results are reported in Tables A1, A2, A3, A4, A5 and A6, available in the online Appendix.
5.1. Feature importance schemes
Next, we applied feature importance techniques with the help of the varImp() function from the caret package (see Figure 6). This scheme helped us better understand the effect of the predictors on the response variable, i.e., the “ratings” received by the mobile apps. When we applied the varImp() function in conjunction with the linear regression results, the order of precedence of the predictors was similar to their t-statistic values reported in the regression.
6. Discussion of results
We applied various regression techniques to examine the users’ experience measured by the ratings received by the nine mHealth applications. We present the results from the linear regression in Tables A1 and A2 (please see online Appendix) and those from the moderating effects in Tables A3 and A4 (please see online Appendix). Next, we present the results from the proportional-odds logit regression model in Tables A5 and A6 (please see online Appendix).
6.1. Main effects
First, among the different measures of utilitarian motivation of mHealth apps, we found that most apps have received significant positive experiences regarding time and money. However, users of Tata Health, MFine, and MediBuddy faced minor issues. Further, payment-related problems included poor payment portals and issues with the refund when the consultations were cancelled or the medicine deliveries were unsuccessful. Thus, users faced problems related to payment and refunds except for Tata Health and Tata 1MG. On the other hand, most satisfied users were impressed by the convenience created by these mHealth apps, leading to an overall positive effect on the ratings. In similar veins, users of all mHealth applications except the DocsApp platform had an overall positive experience during lockdown-related services.
Second, among the different measures of hedonic motivation of mHealth apps, our results show that video consultation was an ongoing issue for all platforms and a weak motivation for users of Apollo24x7, DocsApp, Mfine and MediBuddy. Next, we found that mHealth users on most apps had a significant negative experience with online booking except for PharmEasy, Tata Health and Tata 1MG, the only mHealth platforms that provided users with a positive and significant user experience during online bookings.
Third, among the different measures of brand support and loyalty for users of mHealth apps, we found that most apps provided significantly poor customer support. However, users of Tata Health and MFine had a relatively better experience with customer support. Next, availability was highly significant and positive for mHealth users across all platforms in our study.
Fourth, among the different measures of perceived quality of mHealth apps, we found that users received significant negative experiences regarding responsiveness except those of Tata 1MG and DocsApp, where users faced relatively minor issues. Next, we found that mHealth users on most apps had a poor experience with effectiveness except for TataHealth, which provided users with a strong and effective user experience. Then, while examining the effect of resource quality of mHealth applications, we found that users were mostly satisfied across all platforms. Thus, our study found a significant and positive impact on ratings.
6.2. Moderating effects of effective polarity and reviewer-type
Next, we examined the moderating effects of effective polarity on all predictors belonging to utilitarian motivation, perceived quality, hedonic motivation, and brand association, which helped us to determine whether the high polarity content of the reviews could amplify the main effects of these variables across mHealth platforms (Tables A3 and A4, online Appendix). First, we examined the predictors belonging to the utilitarian motivation construct. We found that the effective polarity strongly moderated the effects of (i) time and money towards the user experience for all the mHealth applications except for Netmeds; (ii) payment towards the user experience for all the mHealth applications except for TataHealth; (iii) refund towards the user experience for TataHealth; (iv) convenience towards the user experience for all mHealth apps except for DocsApp, Mfine and Netmeds; (v) lockdown towards the user experience for all mHealth apps except for DocsApp and Mfine.
Second, we examined the predictors belonging to the hedonic motivation construct. We found that the effective polarity strongly moderated the effects of (i) online booking towards the user experience for all mHealth applications and, in particular, very strong for TataHealth, Tata 1MG and Apollo24x7; (ii) video consultation towards the user experience for all mHealth applications and, in particular, very strong for TataHealth and PharmEasy.
Third, we examined the predictors belonging to the brand support and loyalty construct. We found that the effective polarity strongly moderated the effects of (i) customer support towards the user experience for all the mHealth applications; (ii) availability towards the user experience for all the mHealth applications except for DocsApp, Mfine and Netmeds.
Fourth, we examined the predictors belonging to the perceived quality construct. We found that the effective polarity strongly moderated the effects of (i) responsiveness towards the user experience for all the mHealth applications except for Practo; (ii) effectiveness towards the user experience for all the mHealth applications except for Medibuddy and PharmEasy; (iii) resource quality towards the user experience for all the mHealth apps and in particular, very strongly for TataHealth, Mfine, Tata 1MG and Apollo24x7.
Fifth, we examined the reviewer type’s moderating effects on the predictors of the hedonic motivation construct. We found that the reviewer type strongly moderated the effects of (i) online booking towards the user experience for all mHealth applications except for Tata 1MG and Netmeds; (ii) video consultation towards the user experience for all mHealth applications and, in particular, very strongly for TataHealth, Mfine, MediBuddy and Tata 1MG .
6.3. Applying the strategy Map: Differentiation strategies for improving user experience on mHealth platforms
Next, we presented the effect of overall experience in a 2-by-2 strategy map (see Fig. 7 ) based on Tables A1, A2, A3, A4, A5 and A6 (see online Appendix) across the three dimensions – user-experience, technology and partnerships. Based on the map, we found that most mHealth applications possessed a solid partnership to ensure a positive user experience. However, they remain stressed on providing an excellent technical experience and subsequent user involvement, especially related to payment processing, refunds, customer support, and effectiveness of responses. In the map in Fig. 7, we observe that for most mHealth applications, user perception of partnership factors, i.e., online booking, availability and resource quality, is optimistic. Tata Health, Tata 1MG, Medibuddy and Apollo 24X7 are significant mentions. Furthermore, Netmeds has the weakest user perception in terms of partnerships.
Fig. 7.
Strategy map showing the nine mHealth apps across the three dimensions.
Almost all the apps, except for Tata Health, have poor user perception regarding technology, i.e., ease of payment completion and video consultation quality. The app with the best perception regarding technology is Tata Health, and the worst is MFine. Apps that have developed a good perception in terms of user experience are, PharmEasy, Netmeds, Apollo 24X7 and MFine, in the order of their performance. User experience includes convenience, refund, lockdown impact, time, value for money and effectiveness. Medibuddy has the worst user experience, while other apps also suffer in user experience, especially regarding refund and efficacy.
The above findings have shown that most mHealth apps need to improve their technology offerings and also ensure a better experience in terms of refund policies and overall offerings and performance. These mHealth app service firms can use this strategic framework to visualise their strategic position and accordingly monitor the impact of their actions on their competitive position. In addition to the strategic map, we also provide a supporting recommendations table (Frey et al., 2019) that can offer actionable agendas to the mHealth platforms and help them overcome their incumbent challenges (see Table 8 ).
Table 8.
Strategic recommendations to resolve shortcomings in respective strategic pillars.
| Technology | Partnership | User Experience |
|---|---|---|
| High standardisation | External resources needed | Low standardisation |
| High efficiency | Low budget | |
| High usability | Regional focus | Sharing of expensive or exclusive resources |
| Transactions not planned in advance | Low standardisation | |
| The quality of human–computer interaction defines the experience |
Adapted from Frey et al. (2019).
7. Implications of findings
7.1. Contribution to Theory
Our study offers two significant theoretical contributions, primarily toward the Value Co-Creation Theory and the differentiation strategies in sharing economy. First, our study identifies a “value co-creation mechanism” using S-D Logic where the mHealth platform and the patients (or users) are engaged through the consumption of mHealth services. Contrary to the incumbent healthcare sectors, where the service design aims essentially at G-D logic, the users’ medical facilities, pharmacies, and other primary interactions generate much consumer value. Our study indicates that customer value primarily depends on the service design and depends less on its pre-existing physical attributes. This finding is the primary theoretical contribution to the existing research on mHealth care applications.
Second, our study categorises the identified factors into three differentiation strategies for firms competing in the sharing economy. Mobile health applications depend largely on platform economics to generate successful and enjoyable customer experiences. These firms build partnerships with physicians and clinics that enable patient consultation through mobile platforms. Our study builds a map where it simultaneously draws motivation from the three pillars of strategic adoption and the constructs of motivational association (shown in Table 3). This mapping leads to understanding (i) the current comparative position based on user review and (ii) possible areas of improvement to reach the coveted “aim” where an application meets all the user expectations.
7.2. Contributions to managerial practices
Our study offers interesting recommendations for managers and software developers of mHealth applications. First, it proposes an explanatory framework to measure customer ratings given by the mHealth users. It identifies availability, customer support, responsiveness and seamless payment as significant factors for a successful user experience. Using these findings, managers in mHealth firms can now focus their marketing efforts and monitor the specific product features that will help garner positive consumer reactions in the long run (Nouri et al., 2018). The current scenarios in the mHealth market also coincide, where mobile-health firms are continuously trying to improve the customer experience. Their efforts match the high frequency of new version releases as product manufacturers constantly improvise on existing versions to meet the demand of their customers (Yakubu & Kwong, 2021).
Second, findings from our study will work as a blueprint for app developers working for these mobile-health firms. Often, app developers and back-end programmers remain disconnected from the front-end users, who are essentially consuming the services of the mHealth app. This scenario may lead to challenges, such as incorrect calculations of the app’s overall rating on the Google Play Store or Apple App Store. Finally, the mHealth app’s popularity may diminish among online users, and its usage may reduce, leading to obsolescence. In this aspect, our study presents the detailed specifications and features (see Figure 6) that could also be used to build visualisation tools such as monitoring dashboards. Businesses widely use such dashboards for application performance monitoring7 and feature importance analysis using text-mining user reviews and ratings.
Third, our study identifies a strategy map to help visualise a firm’s relative position and compare its performance with the competitors using the three chosen dimensions – technology, partnership and user experience (see Fig. 7). In this manner, mHealth firms can estimate their relative market positions and plan their business decisions accordingly. In the following sub-section, we explain the map by applying it to the nine mHealth apps in our study and elaborate on their strategy recommendations.
8. Conclusion and future scope of research
This study introduces the application of user reviews in identifying features that impact user star ratings. The study also analyses nine active healthcare apps based on their user review and suggests strategic solutions to improve user satisfaction and rating by a healthcare service provider app. We have divided the reviews into the twelve most relevant factors based on literature review and domain knowledge. We observe that a seamless payment system, transparent refund policy, video consultation, and doctor availability through online booking are factors that need serious attention from the service provider. On the other hand, factors such as lockdown/COVID, time and money, resource quality, convenience and responsiveness have significantly influenced digital transformation in healthcare delivery. This study will provide essential insights on factors that influence a user’s experience of a mHealth app. These findings will allow application and business model developers to understand the basic requirements of developing a user-centric app. It will also help researchers by providing them with a methodological guideline for determining new factors in future as the mHealth industry evolves with time.
Despite these important findings, our study has a few limitations. First, we examined cross-sectional user reviews that we had scraped from mobile health platforms. Future studies can study the longitudinal effects of the predictors across these platforms and incorporate seasonality and economic shocks such as supply-chain disruptions. Second, we worked with mobile health applications based in India. A consequential extension of this study could also examine mobile healthcare apps across various countries and compare their cultural differences. Third, mixed-method studies could be developed by conducting customer interviews and experiments and combining online reviews as a source of customer experience.
CRediT authorship contribution statement
Shounak Pal: Writing – original draft, Software, Methodology, Conceptualization. Baidyanath Biswas: Writing – review & editing, Writing – original draft, Visualization, Supervision, Methodology. Rohit Gupta: Writing – review & editing, Validation, Supervision, Resources, Methodology. Ajay Kumar: Writing – review & editing, Validation, Supervision, Conceptualization. Shivam Gupta: Validation, Supervision, Project administration.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Biographies
Dr. Shounak Pal is working as a Senior Consultant at PricewaterhouseCoopers Private Limited India. He received his PhD (FPM) from IIM Lucknow, India. His research interest includes healthcare information systems, digital twin and data science process modelling.
Dr. Baidyanath Biswas is an Assistant Professor of Digital Business and Information Systems at DCU Business School. He received his PhD (FPM) from IIM Lucknow, India. His research has appeared in Decision Support Systems, Electronic Markets, Computers in Industrial Engineering, and the Journal of Enterprise Information Management. Baidyanath is also associated with top peer-reviewed international conferences, namely, HICSS and ICIS. He has a rich industry-experience of nine years working as a mainframe and DB2 database analyst at Infosys and IBM. Currently, Baidyanath serves on the editorial boards of the Global Business Review and Electronic Markets journal.
Dr. Rohit Gupta is an Assistant Professor of Operations Management Area at Indian Institute of Management Ranchi, Ranchi, India. He received his PhD (FPM) from IIM Lucknow, India.
Dr. Ajay Kumar is an Assistant Professor at EMLYON Business School France. His research and teaching interests are in data and text mining, decision support systems, knowledge management, business intelligence and enterprise modeling. He has been Postdoctoral Fellow at Massachusetts Institute of Technology, USA and Harvard Business School, USA. He has published several research papers in reputed journals, including Journal of Business Research, Decision Support Systems, International Journal of Operations & Production Management, International Journal of Production Economics, Industrial Marketing Management, Technological Forecasting & Social Change, Annals of Operation Research, etc.
Dr. Shivam Gupta is a full Professor at NEOMA Business School, France and expert in Statistics, Cloud Computing, Big Data Analytics, Artificial Intelligence and Sustainability domains. He has published several research papers in reputed journals, including Decision Support Systems, International Journal of Production Economics, Industrial Marketing Management, Journal of Business Research, Annals of Operation Research, etc. He has been the recipient of the International Young Scientist Award by the National Natural Science Foundation of China (NSFC) in 2017 and winner of the 2017 Emerald South Asia LIS award.
Footnotes
Statista Report on Global digital health market by major segment 2015–2025: https://www.statista.com/statistics/387867/value-of-worldwide-digital-health-market-forecast-by-segment/.
Health 2020. A European policy framework and strategy for the 21st Century: https://www.euro.who.int/data/assets/pdf_file/0011/199532/Health2020-Long.pdf.
Accenture Survey on Digital adoption: Reaction or revolution? https://www.accenture.com/us-en/insights/health/digital-adoption-healthcare-reaction-or-revolution.
How COVID-19 triggered the digital and e-commerce turning point:https://unctad.org/news/how-covid-19-triggered-digital-and-e-commerce-turning-point.
PWC Global Top Health Industry Issues 2021:https://www.pwc.com/gx/en/industries/healthcare/top-health-industry-issues.html.
github “vader” https://github.com/cjhutto/vaderSentiment.
What are Application Performance Monitoring Tools? https://www.gartner.com/reviews/market/application-performance-monitoring.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jbusres.2022.113484.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- Ågerfalk P.J., Conboy K., Myers M.D. Information systems in the age of pandemics: COVID-19 and beyond. European Journal of Information Systems. 2020;29(3):203–207. [Google Scholar]
- Akter S., D’Ambra J., Ray P. Development and validation of an instrument to measure user perceived service quality of mHealth. Information & Management. 2013;50(4):181–195. [Google Scholar]
- Akter S., Ray P., D’Ambra J. Continuance of mHealth services at the bottom of the pyramid: The roles of service quality and trust. Electronic Markets. 2013;23(1):29–47. [Google Scholar]
- Alam M.Z., Hu W., Kaium M.A., Hoque M.R., Alam M.M.D. Understanding the determinants of mHealth apps adoption in Bangladesh: A SEM-Neural network approach. Technology in Society. 2020;61 [Google Scholar]
- Alam M.Z., Hoque M.R., Hu W., Barua Z. Factors influencing the adoption of mHealth services in a developing country: A patient-centric study. International Journal of Information Management. 2020;50:128–143. [Google Scholar]
- Agresti A. Vol. 482. John Wiley & Sons; 2003. (Categorical data analysis). [Google Scholar]
- Ashraf A.R., Tek N.T., Anwar A., Lapa L., Venkatesh V. Perceived values and motivations influencing m-commerce use: A nine-country comparative study. International Journal of Information Management. 2021;59 [Google Scholar]
- Azad-Khaneghah P., Neubauer N., Miguel Cruz A., Liu L. Mobile health app usability and quality rating scales: A systematic review. Disability and Rehabilitation: Assistive Technology. 2021;16(7):712–721. doi: 10.1080/17483107.2019.1701103. [DOI] [PubMed] [Google Scholar]
- Balta M., Valsecchi R., Papadopoulos T., Bourne D.J. Digitalization and co-creation of healthcare value: A case study in Occupational Health. Technological Forecasting and Social Change. 2021;168 [Google Scholar]
- Barrett M., Davidson E., Prabhu J., Vargo S.L. Service innovation in the digital age. MIS Quarterly. 2015;39(1):135–154. [Google Scholar]
- Biduski D., Bellei E.A., Rodriguez J.P.M., Zaina L.A.M., De Marchi A.C.B. Assessing long-term user experience on a mobile health application through an in-app embedded conversation-based questionnaire. Computers in Human Behavior. 2020;104 [Google Scholar]
- Birkmeyer S., Wirtz B.W., Langer P.F. Determinants of mHealth success: An empirical investigation of the user perspective. International Journal of Information Management. 2021;59 doi: 10.1016/j.ijinfomgt.2021.102351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biswas B., Sengupta P., Chatterjee D. Examining the determinants of the count of customer reviews in peer-to-peer home-sharing platforms using clustering and count regression techniques. Decision Support Systems. 2020;135 [Google Scholar]
- Biswas M., Tania M.H., Kaiser M.S., Kabir R., Mahmud M., Kemal A.A. ACCU3RATE: A mobile health application rating scale based on user reviews. PloS one. 2021;16(12):e0258050. doi: 10.1371/journal.pone.0258050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chatterjee S., Goyal D., Prakash A., Sharma J. Exploring healthcare/health-product ecommerce satisfaction: A text mining and machine learning application. Journal of Business Research. 2021;131:815–825. [Google Scholar]
- Chatterjee S., Ghatak A., Nikte R., Gupta S., Kumar A. Measuring SERVQUAL dimensions and their importance for customer-satisfaction using online reviews: A text mining approach. Journal of Enterprise Information Management. 2022 [Google Scholar]
- Chiu W., Cho H., Chi C.G. Consumers' continuance intention to use fitness and health apps: An integration of the expectation–confirmation model and investment model. Information Technology & People. 2020 [Google Scholar]
- Cho J. The impact of post-adoption beliefs on the continued use of health apps. International Journal of Medical Informatics. 2016;87:75–83. doi: 10.1016/j.ijmedinf.2015.12.016. [DOI] [PubMed] [Google Scholar]
- Cho H., Chi C., Chiu W. Understanding sustained usage of health and fitness apps: Incorporating the technology acceptance model with the investment model. Technology in Society. 2020;63 [Google Scholar]
- Chang I.C., Chou P.C., Yeh R.K.J., Tseng H.T. Factors influencing Chinese tourists’ intentions to use the Taiwan Medical Travel App. Telematics and Informatics. 2016;33(2):401–409. [Google Scholar]
- Dahl A.J., Milne G.R., Peltier J.W. Digital health information seeking in an omni-channel environment: A shared decision-making and service-dominant logic perspective. Journal of Business Research. 2021;125:840–850. [Google Scholar]
- Dwivedi Y.K., Shareef M.A., Simintiras A.C., Lal B., Weerakkody V. A generalised adoption model for services: A cross-country comparison of mobile health (m-health) Government Information Quarterly. 2016;33(1):174–187. [Google Scholar]
- Frey A., Trenz M., Veit D. Three Differentiation Strategies for Competing in the Sharing Economy. MIS Quarterly Executive. 2019;18(2) [Google Scholar]
- Gao Y., Li H., Luo Y. An empirical study of wearable technology acceptance in healthcare. Industrial Management & Data Systems. 2015 [Google Scholar]
- Ghose A., Guo X., Li B., Dang Y. Empowering patients using smart mobile health platforms: Evidence from a randomized field experiment. MIS Quarterly. 2021 [Google Scholar]
- Gimpel H., Manner-Romberg T., Schmied F., Winkler T.J. Understanding the evaluation of mHealth app features based on a cross-country Kano analysis. Electronic Markets. 2021:1–30. doi: 10.1007/s12525-020-00455-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grover P., Kar A.K., Gupta S., Modgil S. Influence of political leaders on sustainable development goals–insights from twitter. Journal of Enterprise Information Management. 2021;34(6):1893–1916. [Google Scholar]
- Hashemi H., Rajabi R., Brashear-Alejandro T.G. COVID-19 Research in Management: An Updated Bibliometric Analysis. Journal of Business Research. 2022 doi: 10.1016/j.jbusres.2022.05.082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoque R., Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. International Journal of Medical Informatics. 2017;101:75–84. doi: 10.1016/j.ijmedinf.2017.02.002. [DOI] [PubMed] [Google Scholar]
- Jannati N., Nakhaee N., Yazdi-Feyzabadi V., Tjondronegoro D. A cross-sectional online survey on patients’ satisfaction using store-and-forward voice and text messaging teleconsultation service during the COVID-19 pandemic. International Journal of Medical Informatics. 2021;151 doi: 10.1016/j.ijmedinf.2021.104474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D.J., Hwang Y. A study of mobile internet user’s service quality perceptions from a user’s utilitarian and hedonic value tendency perspectives. Information Systems Frontiers. 2012;14(2):409–421. [Google Scholar]
- Kim K.H., Kim K.J., Lee D.H., Kim M.G. Identification of critical quality dimensions for continuance intention in mHealth services: Case study of onecare service. International Journal of Information Management. 2019;46:187–197. [Google Scholar]
- Kim M., Lee S.M., Choi S., Kim S.Y. Impact of visual information on online consumer review behavior: Evidence from a hotel booking website. Journal of Retailing and Consumer Services. 2021;60 [Google Scholar]
- Kraus S., Schiavone F., Pluzhnikova A., Invernizzi A.C. Digital transformation in healthcare: Analyzing the current state-of-research. Journal of Business Research. 2021;123:557–567. [Google Scholar]
- Lamprinos I., Demski H., Mantwill S., Kabak Y., Hildebrand C., Ploessnig M. Modular ICT-based patient empowerment framework for self-management of diabetes: Design perspectives and validation results. International Journal of Medical Informatics. 2016;91:31–43. doi: 10.1016/j.ijmedinf.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Li J., Zhang C., Li X., Zhang C. Patients’ emotional bonding with MHealth apps: An attachment perspective on patients’ use of MHealth applications. International Journal of Information Management. 2020;51 [Google Scholar]
- Lim S., Xue L., Yen C.C., Chang L., Chan H.C., Tai B.C.…Choolani M. A study on Singaporean women's acceptance of using mobile phones to seek health information. International Journal of Medical Informatics. 2011;80(12):e189–e202. doi: 10.1016/j.ijmedinf.2011.08.007. [DOI] [PubMed] [Google Scholar]
- Lim W.M., Gupta G., Biswas B., Gupta R. Collaborative consumption continuance: A mixed-methods analysis of the service quality-loyalty relationship in ride-sharing services. Electronic Markets. 2021:1–22. [Google Scholar]
- Lorca-Cabrera J., Marti-Arques R., Albacar-Rioboo N., Raigal-Aran L., Roldan-Merino J., Ferre-Grau C. Mobile applications for caregivers of individuals with chronic conditions and/or diseases: Quantitative content analysis. International Journal of Medical Informatics. 2021;145 doi: 10.1016/j.ijmedinf.2020.104310. [DOI] [PubMed] [Google Scholar]
- Malik N., Tripathi S.N., Kar A.K., Gupta S. Impact of artificial intelligence on employees working in industry 4.0 led organizations. International Journal of Manpower. 2021;43(2):334–354. [Google Scholar]
- Maglio P.P., Spohrer J. Fundamentals of service science. Journal of the Academy of Marketing Science. 2008;36(1):18–20. [Google Scholar]
- McKinley C.J., Wright P.J. Informational social support and online health information seeking: Examining the association between factors contributing to healthy eating behavior. Computers in Human Behavior. 2014;37:107–116. [Google Scholar]
- Miró J., Llorens-Vernet P. Assessing the Quality of Mobile Health-Related Apps: Interrater Reliability Study of Two Guides. JMIR mHealth and uHealth. 2021;9(4):e26471. doi: 10.2196/26471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Müller O., Junglas I., Brocke J.V., Debortoli S. Utilising big data analytics for information systems research: Challenges, promises and guidelines. European Journal of Information Systems. 2016;25(4):289–302. [Google Scholar]
- Nouri, R., R Niakan Kalhori, S., Ghazisaeedi, M., Marchand, G., & Yasini, M. (2018). Criteria for assessing the quality of mHealth apps: a systematic review. Journal of the American Medical Informatics Association, 25(8), 1089-1098. [DOI] [PMC free article] [PubMed]
- Nusairat N., Abdellatif H., Al-Gasawneh J., Akhorshaideh A., Aloqool A., Rabah S., Ahmad A. Determinants of behavioral intentions to use mobile healthcare applications in Jordan. International Journal of Data and Network Science. 2021;5(4):547–556. [Google Scholar]
- Osei-Frimpong K., Wilson A., Lemke F. Patient co-creation activities in healthcare service delivery at the micro level: The influence of online access to healthcare information. Technological Forecasting and Social Change. 2018;126:14–27. [Google Scholar]
- Pal S., Mukhopadhyay A., Shukla G.K. Proceedings of the 2018 ACM SIGMIS Conference on Computers and People Research. 2018. Can IT Improve Cardiac Treatment Quality? A Quantitative Study of Interaction between Technology and External Factors; pp. 18–25. [DOI] [Google Scholar]
- Paramita N., Noviarisanti S. Service Quality Analysis of Mhealth Services Using Text Mining Method: Alodokter and Halodoc. International Journal of Management, Finance and Accounting. 2021;2(2):1–21. [Google Scholar]
- Peltier J.W., Dahl A.J., Swan E.L. Digital information flows across a B2C/C2C continuum and technological innovations in service ecosystems: A service-dominant logic perspective. Journal of Business Research. 2020;121:724–734. [Google Scholar]
- Pennebaker J.W., Boyd R.L., Jordan K., Blackburn K. Pennebaker Conglomerates; Austin, TX: 2015. The development and psychometric properties of LIWC2015. [Google Scholar]
- Pop O.M., Leroi-Werelds S., Roijakkers N., Andreassen T.W. Institutional types and institutional change in healthcare ecosystems. Journal of Service Management. 2018 [Google Scholar]
- Prakash A.V., Das S., Pillai K.R. Understanding digital contact tracing app continuance: Insights from India. Health Policy and Technology. 2021;10(4) [Google Scholar]
- Rahimi R., Khoundabi B. Investigating the effective factors of using mHealth apps for monitoring COVID-19 symptoms and contact tracing: A survey among Iranian citizens. International Journal of Medical Informatics. 2021;155 doi: 10.1016/j.ijmedinf.2021.104571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Priego N., Porcu L., Kitchen P.J. Sharing but caring: Location based mobile applications (LBMA) and privacy protection motivation. Journal of Business Research. 2022;140:546–555. [Google Scholar]
- Russo G., Moretta Tartaglione A., Cavacece Y. Empowering patients to co-create a sustainable healthcare value. Sustainability. 2019;11(5):1315. [Google Scholar]
- Sadegh S.S., Saadat P.K., Sepehri M.M., Assadi V. A framework for mHealth service development and success evaluation. International Journal of Medical Informatics. 2018;112:123–130. doi: 10.1016/j.ijmedinf.2018.01.003. [DOI] [PubMed] [Google Scholar]
- Salehan M., Kim D.J. Predicting the performance of online consumer reviews: A sentiment mining approach to big data analytics. Decision Support Systems. 2016;81:30–40. [Google Scholar]
- Salton G., Buckley C. Term-weighting approaches in automatic text retrieval. Information Processing & Management. 1988;24(5):513–523. [Google Scholar]
- Schütze H., Manning C.D., Raghavan P. Introduction to information retrieval. 2008;Vol. 39:234–265. [Google Scholar]
- Sengupta P., Biswas B., Kumar A., Shankar R., Gupta S. Examining the predictors of successful Airbnb bookings with Hurdle models: Evidence from Europe, Australia, USA and Asia-Pacific cities. Journal of Business Research. 2021;137:538–554. [Google Scholar]
- Shah A.M., Yan X., Tariq S., Khan S. Listening to the patient voice: Using a semantic computing model to evaluate physicians’ healthcare service quality for strategic planning in hospitals. Quality & Quantity. 2021;55:173–201. [Google Scholar]
- Sheth J.N. Customer value propositions: Value co-creation. Industrial Marketing Management. 2019;87:312–315. [Google Scholar]
- Shirazi F., Wu Y., Hajli A., Zadeh A.H., Hajli N., Lin X. Value co-creation in online healthcare communities. Technological Forecasting and Social Change. 2021;167 [Google Scholar]
- Stieglitz S., Dang-Xuan L. Emotions and information diffusion in social media—sentiment of microblogs and sharing behavior. Journal of Management Information Systems. 2013;29(4):217–248. [Google Scholar]
- Stocchi L., Pourazad N., Michaelidou N., Tanusondjaja A., Harrigan P. Marketing research on Mobile apps: Past, present and future. Journal of the Academy of Marketing Science. 2021:1–31. doi: 10.1007/s11747-021-00815-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suroso J.S., Sukmoro T.C. Factors affecting behavior of the use of healthcare mobile application technology in Indonesian society. Journal of Theoretical and Applied Information Technology. 2021;99(15):3923–3934. [Google Scholar]
- Tan, A. H. (1999). Text mining: The state of the art and the challenges. In Proceedings of the PAKDD 1999 Workshop on Knowledge Discovery from Advanced Databases (Vol. 8, pp. 65-70).
- Tan H., Yan M. Physician-user interaction and users' perceived service quality: Evidence from Chinese mobile healthcare consultation. Information Technology & People. 2020 [Google Scholar]
- Tartaglione A.M., Cavacece Y., Cassia F., Russo G. The excellence of patient-centered healthcare: Investigating the links between empowerment, co-creation and satisfaction. The TQM Journal. 2018 [Google Scholar]
- Tran T.P., Mai E.S., Taylor E.C. Enhancing brand equity of branded mobile apps via motivations: A service-dominant logic perspective. Journal of Business Research. 2021;125:239–251. [Google Scholar]
- Tripathi S., Deokar A.V., Ajjan H. Understanding the Order Effect of Online Reviews: A Text Mining Perspective. Information Systems Frontiers. 2021:1–18. [Google Scholar]
- Tsiotsou R.H., Boukis A. In-home service consumption: A systematic review, integrative framework and future research agenda. Journal of Business Research. 2022;145:49–64. [Google Scholar]
- Vargo S.L., Lusch R.F. Evolving to a new dominant logic for marketing. Journal of Marketing. 2004;68(1):1–17. [Google Scholar]
- Vargo S.L., Lusch R.F. Service-dominant logic: Continuing the evolution. Journal of the Academy of Marketing Science. 2008;36(1):1–10. [Google Scholar]
- Vargo S.L., Lusch R.F. From goods to service (s): Divergences and convergences of logics. Industrial Marketing Management. 2008;37(3):254–259. [Google Scholar]
- Vargo S.L., Akaka M.A. Service-dominant logic as a foundation for service science: Clarifications. Service Science. 2009;1(1):32–41. [Google Scholar]
- Veríssimo J.M.C. Usage intensity of mobile medical apps: A tale of two methods. Journal of Business Research. 2018;89:442–447. [Google Scholar]
- Verma S., Gustafsson A. Investigating the emerging COVID-19 research trends in the field of business and management: A bibliometric analysis approach. Journal of Business Research. 2020;118:253–261. doi: 10.1016/j.jbusres.2020.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang, C., & Qi, H. (2021, March). Influencing factors of acceptance and use behavior of mobile health application users: systematic review. In Healthcare (Vol. 9, No. 3, p. 357). MDPI. [DOI] [PMC free article] [PubMed]
- Wakefield D., Bayly J., Selman L.E., Firth A.M., Higginson I.J., Murtagh F.E. Patient empowerment, what does it mean for adults in the advanced stages of a life-limiting illness: A systematic review using critical interpretive synthesis. Palliative Medicine. 2018;32(8):1288–1304. doi: 10.1177/0269216318783919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webster P. Virtual health care in the era of COVID-19. The Lancet. 2020;395(10231):1180–1181. doi: 10.1016/S0140-6736(20)30818-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L., Li J.Y., Fu C.Y. The adoption of mobile healthcare by hospital's professionals: An integrative perspective. Decision Support Systems. 2011;51(3):587–596. [Google Scholar]
- Wu P., Zhang R., Luan J., Zhu M. Factors affecting physicians using mobile health applications: An empirical study. BMC Health Services Research. 2022;22(1):1–14. doi: 10.1186/s12913-021-07339-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yakubu H., Kwong C.K. Forecasting the importance of product attributes using online customer reviews and Google Trends. Technological Forecasting and Social Change. 2021;171 doi: 10.1016/j.techfore.2021.120983. [DOI] [Google Scholar]
- Yang H., Guo X., Peng Z., Lai K.H. Patient empowerment in an online health platform: Exploring the quadratic effects of patients’ conscious-competence on perceived health status. Computers in Human Behavior. 2022;107346 [Google Scholar]
- Yang X., Kovarik C.L. A systematic review of mobile health interventions in China: Identifying gaps in care. Journal of Telemedicine and Telecare. 2021;27(1):3–22. doi: 10.1177/1357633X19856746. [DOI] [PubMed] [Google Scholar]
- Zhang M., Zhang C., Shi Q., Zeng S., Balezentis T. Operationalising the telemedicine platforms through the social network knowledge: An MCDM model based on the CIPFOHW operator. Technological Forecasting and Social Change. 2022;174 [Google Scholar]
- Zhao Y., Ni Q., Zhou R. What factors influence the mobile health service adoption? A meta-analysis and the moderating role of age. International Journal of Information Management. 2018;43:342–350. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.