Abstract
Age-related changes in body composition reflect an increased risk for disease as well as disability. Bioimpedance analysis is a safe and inexpensive bed side method to measure body composition, but the calculation of body compartments with BIA is hampered in older adults. Phase angle, a raw parameter derived from bioimpedance analysis, is free from calculation-inherent errors. It declines with age and disease and is highly predictive of a variety of clinical outcomes as well as mortality. This review summarizes the current evidence linking the phase angle to geriatric syndromes such as malnutrition, sarcopenia and frailty and also investigates whether the phase angle reacts to interventions. Since the majority of studies show an association between the phase angle and these geriatric syndromes, a low phase angle is not suitable to exclusively indicate a specific condition. It does not inform on the underlying cause and as such, a low phase angle mainly indicates increased risk. Phase angle decline over time is reflected by deterioration of e.g. frailty status. It reacts to physical training and detraining, but studies investigating whether these induced changes are also associated with improved outcome are missing.
Keywords: Phase angle, Body composition, Aging, Sarcopenia, Frailty, Malnutrition
Introduction
Body composition is known to change with aging hallmarked by a decline in skeletal muscle mass as well as by an increase in total and abdominal fat tissue. As changes in body composition are associated with increased risk for disease and disability, monitoring body composition in the old is of clinical importance.
Sarcopenia has been referred to as a geriatric syndrome [1] as it describes the age-associated loss of muscle mass and function, which is accompanied by a progressive decline in physical performance and is associated with a higher risk for physical disability and need for care. Sarcopenia can be present without apparent weight changes, hence assessing body composition is required in order to detect it. Moreover, older adults are particularly vulnerable to malnutrition [2] which is frequently characterized by involuntary weight loss resulting in further deleterious changes in body composition. The loss of skeletal muscle mass in malnutrition has been shown to be greater in older compared to younger adults [3]. Both malnutrition and sarcopenia are frequent in higher age with considerable overlap between the two entities, as malnutrition can contribute to or accelerate the development of sarcopenia. Importantly, malnutrition and sarcopenia have been linked to the development of the complex frailty syndrome which is a geriatric syndrome associated with lower resilience against stressors and impaired clinical outcome [4]. Both weight loss and low muscle strength or function are principal phenotypic characteristics of the physical frailty syndrome [5].
Bioimpedance analysis (BIA) which is a simple, non-invasive, inexpensive and safe bedside method, has long been considered an attractive alternative to the cumbersome and expensive imaging methods for body composition assessment such as dual X-ray absorptiometry (DXA) or computed tomography (CT). However, deriving body composition in the old using BIA is challenging, as the required conditions for calculating body compartments such as constant hydration of fat free mass or no fluid imbalance, no body shape abnormalities, are frequently not present in the old. They represent a very heterogeneous population with high inter-individual variation of fat free mass hydration and a higher likelihood of disease and multimorbidity which may further affect body composition [6]. Most regression equations for assessing body composition using single frequency BIA developed in healthy populations are not suitable in disease [7] and have even been found inadequate in the old [8, 9]; moreover, only few age-specific equations for single body compartments have been developed so far.
Research on the use of raw bioimpedance parameters such as resistance (R), reactance (Xc) or phase angle without the equation-inherent errors for calculating body composition has increased in the last decade and there is a large body of evidence linking reduced bioimpedance phase angle to a variety of clinical outcomes including mortality in e.g. critically ill, patients with kidney, heart or liver disease, and patients with cancer [10].
Resistance and reactance provide information on hydration of tissues as well as cell membrane mass. R is the pure opposition of the body as a biological conductor to the flow of an alternating electric current; while reactance is the resistive effect produced by the double layer of cell membranes and tissue interfaces. The phase angle as the ratio between Xc and R is therefore interpreted as an indicator of cell membrane integrity and better cell function and health, while lower phase angle values have been associated with impaired cellular structure and greater cell death [11]. While the relationship between phase angle and overall body cell mass (BCM) has been described early, only recently, a study also confirmed an association between phase angle and cell growth and metabolism in healthy older adults. Using a proteomics approach, six protein markers were identified as being strongly associated with the phase angle [12]. When the protein markers were grouped according to their functional characteristics, regulation of the amount and growth of cells emerged as the main biological process which is related to the phase angle [12]. N-terminal pro b-type natriuretic peptide (NT-proBNP) was the key marker of the phase angle. NT-proBNP is an established marker of heart failure which is frequently characterized by overhydration. Studies in patients on hemodialysis show that changes in phase angle over a 6 month period was related to changes in NT-proBNP [13].
Also, age is one of the strongest determinants of phase angle in health, and phase angle prominently declines with higher age. While most studies are cross-sectional consistently showing peak values in young adulthood and lower values in later life [14], a recent study investigated prospective changes in phase angle over time in adults aged over 50 [15]. The authors showed an annual decline in phase angle values which mirrored the decline in muscle quality (hand grip or knee extension strength per kg muscle mass) while overall changes in body composition were not yet detectable. The annual percentage change in this study did not differ between men and women, or between the older (< 65 years) and younger group. However, the precision of the device, which allows evaluation of repeated measurements was not stated in the study.
Phase angle in higher age has also been associated with prominent aging biomarkers such as the higher pro-inflammatory status in higher age (e.g. “inflammaging”) and parameters of oxidative stress [16, 17] which is linked to inflammation and cell damage and therefore also has been implicated in the development of age-related disease [18].
Since phase angle reflects both fluid distribution and BCM, an association with the amount and quality of skeletal muscle mass is expected. Moreover, phase angle has also been linked to muscle strength and functional capacity and therefore several studies have explored the relationship between phase angle values and sarcopenia in older adults.
This review focusses on the association of phase angle with parameters of impaired nutritional status, with muscle mass, strength and function as well as sarcopenia and frailty in the old. It moreover explores whether a low phase angle is indicative of incident functional decline and whether it reacts to interventions such as physical training.
Phase angle and its association with impaired nutritional status (malnutrition)
The association between impaired nutritional status and low phase angle is well established [10]. As the calculation of body compartments using BIA in the older adults is not accurate enough, in particular in the presence of disease, the use of raw bioimpedance parameters to indicate impaired nutritional status has gained increasing attention. Malnutrition is characterized by a decrease in BCM and loss of intracellular water with a compensatory increase in extracellular water [10]. Not surprisingly, alterations of electrical tissue properties, reflected by characteristic changes in reactance, occur in malnutrition [19] which is therefore usually accompanied by a decreased phase angle.
The gold standard for the diagnosis of malnutrition has long been under debate, but there are several nutrition screening tools which indicate malnutrition or the risk of developing malnutrition and which have been investigated in relation to phase angle.
We studied phase angle in octogenarians living in a nursing home and found a stepwise reduction in phase angle with increasing degree of malnutrition assessed by the Mini Nutritional Assessment (MNA) [20]. Similarly, in a small sample of old frail hospital patients, the overall phase angle positively correlated with the MNA short-form score [21]. Additionally, malnutrition indicated by the Nutritional Risk Score (NRS-2002) was associated with a significantly lower phase angle in geriatric inpatients [22]. One study in old rehabilitation patients moreover showed that phase angle was predictive of malnutrition assessed with the Geriatric Nutritional Risk Index, with sensitivity and specificity however different between men and women [23].
Although many studies consistently report associations between various nutrition screening tools which indicate malnutrition and the phase angle, one systematic review failed to conclude that phase angle was an accurate predictor of malnutrition assessed by the Subjective Global Assessment (SGA) in different disease settings [24].
Recently, a study in a large clinical cohort of predominantly older patients [25] also showed that the phase angle was an independent and even better predictor of mortality compared to the SGA, indicating that a low phase angle yields additional information which cannot be attributed to nutritional status alone.
Malnutrition is a complex phenomenon, and in disease, of multifactorial origin. Several factors, such as inflammation or disease-specific catabolism, which contribute to malnutrition, also have an adverse impact on phase angle itself [26]. Moreover, both inflammation and malnutrition are frequently accompanied by edema, which per se is known to decrease phase angle. Therefore, while malnutrition and low phase angle are closely linked, the underlying factors will be hard to disentangle. Although malnutrition is most likely accompanied by a reduced phase angle, a low phase angle cannot be interpreted as an exclusive indicator of malnutrition.
Phase angle as an indicator of low muscle strength and sarcopenia
The electric properties of cell membranes are related to both area and integrity of cell membranes and phase angle has been referred to as an index of cell membrane integrity [27] which is one determinant of membrane potential and, together with area, most likely determines muscle cell function [28]. The impedance parameters reactance and resistance normalized for height have both been shown to be independently associated with hand grip strength [29], so an association between phase angle and strength parameters is expected.
In healthy old, phase angle is a predictor of muscle function such as slow gait speed [30] and in healthy older women, moderate associations were obtained between phase angle and muscle quality (strength/kg appendicular lean mass), functional capacity score (composed of various walking and rising tests) [31], gait speed [32] and with 6-meter walking test, forearm flexion and chair stand, dependent on BMI category [33]. In older patients with cancer, low phase angle predicted decreased hand grip strength, knee extension strength and reduced peak expiratory flow, as well as impaired physical function (determined by the European Organization for Research and Treatment of Cancer quality of life questionnaire) [34].
Higher phase angle values suggest higher BCM [35], of which an integral part is skeletal muscle. Not surprisingly, phase angle is increased in athletes reflecting both the higher amount of skeletal muscle mass [36] as well as performance capacity [37] and has been referred to as indicator of muscle quality [38, 39]. Similar to muscle mass, phase angle is affected by age, sex, race, BMI [40] and physical activity [41]. Given these associations, it is likely that sarcopenia, the loss of muscle mass and function in higher age, is accompanied by lower phase angle values.
While the definition of sarcopenia has undergone very few changes in the last decades (from age-related loss of muscle mass to loss of muscle mass and function), the diagnostic criteria have been under debate, which in part is due to the challenges of assessing muscle mass in vivo. Whether phase angle values can be used to indicate sarcopenia has been addressed in several studies in the old or in cancer patients.
A recent systematic review summarized the evidence and analysed the relationship between sarcopenia and phase angle in old adults with and without disease. A correlation between phase angle and muscle mass was seen in six studies, while phase angle correlated with the sarcopenia related muscle parameters hand grip strength and gait speed in six and three studies, respectively. Di Vincenzo and colleagues found significantly lower values of phase angle in sarcopenia in seven out of eight studies and a higher prevalence of sarcopenia in patient groups below cut offs indicating low phase angle in five out of six studies. In two out of four studies, low phase angle significantly predicted sarcopenia. The phase angle cut off values to indicate sarcopenia in the studies, however, ranged considerably from 4° to 5° [42]. It is not clear whether these differences were due to the population studied or due to the BIA device, as the studies included in the systematic review were different and differences between BIA devices from different manufacturers are well known [43].
Similar to malnutrition, when phase angle and sarcopenia were analysed with regard to survival, they were both independent predictors of death in two studies [44, 45] again implying that phase angle provides additional information and is not solely an indicator of sarcopenia.
In summary, there appears to be a consistent association between sarcopenia and low phase angle, however valid phase angle cut off values to reliably indicate sarcopenia are missing. That may in part be due to the lack of gold standard methods used in the studies to assess muscle mass, but also to the multifactoriality of a low phase angle. In the end, a low phase angle cannot be used in a diagnostic way [27] but may be used as a risk factor to indicate low muscle mass or quality.
The relation between phase angle, frailty and the dysmobility syndrome
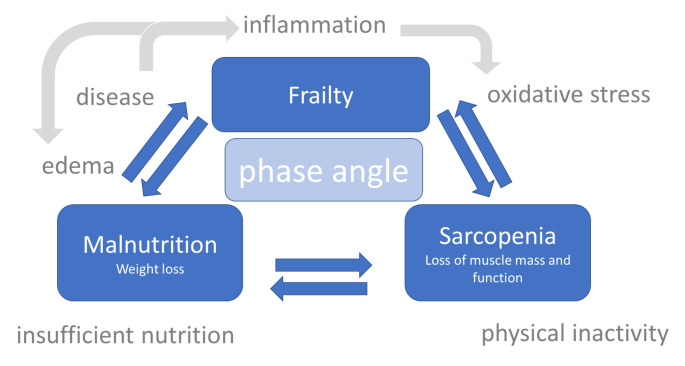
Not surprisingly, there is also a close association between phase angle and frailty, an important geriatric syndrome which is described as a complex multifactorial syndrome with increased vulnerability against stressors [4], of which sarcopenia has often been referred to as the biological substrate [46]. In a nationally representative sample of the NHANES study of 4,667 older adults, men and women with phase angle values below the first quintile had a 3-fold higher risk of being frail [47]. In the FraDySMex cohort study (Frailty, Dynapenia, and Sarcopenia in Mexican Adults), low phase angle was associated with frailty, even after controlling for age, sex, BMI, and comorbidities [48]. Similarly, in a large cohort of community-dwelling old in Japan, a low phase angle was linked to frailty as well to the locomotive syndrome, a condition in which mobility is reduced due impairments of the locomotor system [49] with some sex-specific differences as these associations were more pronounced in men. In a small prospective study in older adults, with every one-degree increment in phase angle over a one-year period, the likelihood of improving from frailty was 4-fold higher [50]. In older patients with rheumatoid arthritis, a low phase angle was also associated with significantly higher odds of being frail. Moreover, the change in phase angle over time was also correlated to the change in frailty status. Deterioration in frailty status was associated with a decline in phase angle, while in non-frail patients who maintained at a stable phase angle either improved or did not change [51]. Figure 1 illustrates the relationship between phase angle, malnutrition, sarcopenia and frailty.
Fig. 1.
Phase angle in the framework of malnutrition, sarcopenia and frailty and age-associated disease, inflammation and oxidative stress
Phase angle has also been linked to the dysmobility syndrome, a recently proposed concept which integrates bone, muscle as well as adipose tissue in order to predict future fracture risk. In a large Korean cohort of community-dwelling old, low phase angle was significantly associated with a more 2-fold risk of having the dysmobility syndrome, independent from significant confounders such as sex, body mass index, and inflammation [52].
Is the phase angle a good predictor of subsequent falls, incident disability and mortality in the old?
Given the observed associations with nutritional status, muscle mass, strength and function as well as frailty in older adults, the question arises whether phase angle is also a useful tool to predict age-relevant clinical outcomes such as falls, disability or mortality.
In a large population of community-dwelling old without disability at baseline, low phase angle was a significant independent predictor of incident disability during a two year follow up period while appendicular lean mass corrected for BMI was not [53]. Also, older community-dwelling adults with low phase angle experienced more falls in a 6-month period [54] and phase angle as well as number of medications were significant predictors of incident fall risk, whereas age, sex, low muscle mass or low muscle function were not. In older patients with rheumatoid arthritis [51], phase angle predicted falls in a two year follow up period, whereas sarcopenia assessed by the Asian Working Group for Sarcopenia 2014 criteria was not a significant risk factor for falls. Similarly, in older patients with cirrhosis, phase angle and the disease severity Model for End-stage liver disease (MELD) score were both independently associated with incident hospitalization and mortality, but phase angle was the only independent predictor of falls [55].
Low phase angle values have also been linked to increased risk of death in many clinical settings [10]. This association of low phase angle and mortality has been observed in community-dwelling older adults as well. In the sub-analysis of the NHANES cohort in older adults described above [47], low phase angle was moreover predictive of long-term mortality independent from sex, age, race or ethnicity and comorbidity. Since these study participants were also more likely frail, this is anticipated, however, even in non-frail individuals with no little or no comorbidity at baseline, lower phase angle was associated with an increased risk of mortality during the follow up period, and the authors therefore suggest that low phase angle can be seen as a global marker of aging [47]. In a large cohort of patients aged over 65 years (n = 1,307), a low phase angle was even associated with mortality in a 10-year period following hospital stay, irrespective of age, sex, comorbidities or BMI category [56]. The presence of acute disease compounds the problem even further. In 1,071 geriatric in-hospital patients, a low phase angle was associated with a 4-fold higher risk of in-hospital mortality [57].
In a cohort of old patients with cancer, a low phase angle was an independent predictor of one-year mortality next to cancer severity, whereas grip strength was not [34]. Also, in older patients undergoing major cardiac surgery, phase angle was associated with frailty and higher risk for overall morbidity and longer hospital stay as well as higher short term and one-year mortality [58]. Moreover, in older patients with COVID-19 [59], low phase angle was an independent predictor of short-term mortality risk irrespective of age, sex, BMI, and comorbidities. In a small study in critically ill older patients, phase angle improved after five days in survivors while it decreased further in non-survivors [60]. Overall, a low phase angle is a strong independent predictor of mortality in various diseases and is also associated with a higher incidence of disability as well as falls in older adults who were healthy at baseline.
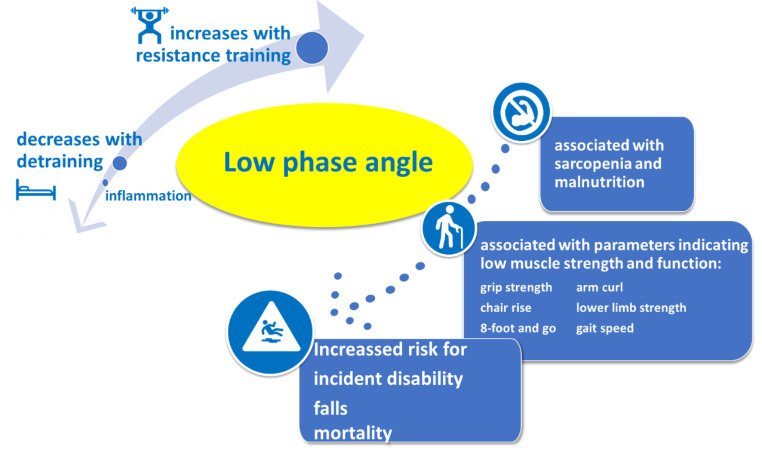
Phase angle changes with training and detraining
Aside from the biological determinants age and sex, phase angle is impacted by various parameters in disease, such as inflammation and catabolism; while physical activity is believed to be the strongest modifiable determinant of phase angle in health. Whether phase angle also reflects acute changes achieved by exercise or by phases of detraining has been studied in older adults. One systematic review summarizing seven studies showed in their meta-analysis that resistance training induced increases in phase angle, which result from an increase in reactance with a concomitant reduction in resistance [61].
The improvements of phase angle after a 12-week resistance training in women aged over 60 were mirrored by increases in muscle quality as assessed by the muscle quality index (MQI) which is calculated as total strength 1 repetition maximum / total body lean mass (by DXA) [62]. Interestingly, the improvement of the phase angle following a 12-week resistance training was also correlated with decreases in the pro-inflammatory cytokines TNF-α and CRP and with a decrease in advanced oxidation protein products [63]. Conversely, a systematic detraining phase of only two weeks was reflected by an acute decline in phase angle values in older trained adults. These changes were due to decreases in reactance with minimal changes in resistance (R) which were observed while they were still no measurable changes in e.g. knee extension strength [64].
While data consistently show an association between phase angle and conditions which are reflected by low BCM such as malnutrition, sarcopenia and impaired functionality, low phase angle itself is not a diagnostic or an exclusive parameter. It can be seen as an indicator of general at-risk conditions which are associated with worsened outcome. While phase angle reacts to training exercises and detraining phases as well as to changes in inflammation over time [65, 66], it has not yet been shown that these improvements are also associated with improved outcome.
Conclusion
In the old, phase angle is impacted by disease, inflammation and oxidative stress. Current literature shows that a low phase angle is linked to various age relevant conditions such as malnutrition, sarcopenia and frailty and predicts disability and mortality in older adults (Fig. 2). This indicates that the phase angle, while highly predictive of mortality, is not a good indicator of a single entity, as it does not inform on its etiology. A low phase angle in individuals only indicates increased risk, but the underlying cause is unknown and needs to be investigated. This also explains the wide range of proposed cut off values which differ with regard to e.g. disease and the outcome or the condition it was related to. At present, no universal phase angle cut off value exists and caution is also necessary due to the lacking comparability of BIA devices. In healthy older adults, the phase angle increases after training and decreases after detraining, however whether these induced changes also indicate a change in prognosis has not yet been investigated. It however stands to reason, as phase angle increases over time have e.g. been shown to reflect improvement from the frailty syndrome.
Fig. 2.
Changes in phase angle and its association with outcome in older adults
Abbreviations
- BCM
Body cell mass
- BIA
Bioelectrical impedance analysis
- BMI
Body mass index
- CT
Computed tomography
- DXA
Dual X-ray absorptiometry
- FraDySMex
Frailty, Dynapenia, and Sarcopenia in Mexican Adults
- MNA
Mini Nutritional Assessment
- NRS
Nutritional Risk Score
- MELD
Model for End-stage liver disease
- MQI
Muscle quality index
- R
Resistance
- SGA
Subjective Global Assessment
- Xc
Reactance
Statements and declarations
The authors have no financial or proprietary interests in any material discussed in this article.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cruz-Jentoft AJ, Landi F, Topinkova E, Michel JP. Understanding sarcopenia as a geriatric syndrome. Curr Opin Clin Nutr Metab Care. 2010;13:1–7. doi: 10.1097/MCO.0b013e328333c1c1. [DOI] [PubMed] [Google Scholar]
- 2.Norman K, Hass U, Pirlich M. Malnutrition in older adults-recent advances and remaining Challenges. Nutrients. 2021;13. DOI:10.3390/nu13082764. [DOI] [PMC free article] [PubMed]
- 3.Hebuterne X, Bermon S, Schneider SM. Ageing and muscle: the effects of malnutrition, re-nutrition, and physical exercise. Curr Opin Clin Nutr Metab Care. 2001;4:295–300. doi: 10.1097/00075197-200107000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Morley JE, Vellas B, van Kan GA, Anker SD, Bauer JM, Bernabei R, Cesari M, Chumlea WC, Doehner W, Evans J, Fried LP, Guralnik JM, Katz PR, Malmstrom TK, McCarter RJ, Gutierrez Robledo LM, Rockwood K, von Haehling S, Vandewoude MF, Walston J. Frailty consensus: a call to action. J Am Med Dir Assoc. 2013;14:392–7. doi: 10.1016/j.jamda.2013.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA, Cardiovascular Health Study Collaborative Research G Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146-56. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 6.Graf CE, Herrmann FR, Genton L. Relation of disease with standardized Phase Angle among older patients. J Nutr Health Aging. 2018;22:601–7. doi: 10.1007/s12603-018-1034-4. [DOI] [PubMed] [Google Scholar]
- 7.Haverkort EB, Reijven PL, Binnekade JM, de van der Schueren MA, Earthman CP, Gouma DJ, de Haan RJ. Bioelectrical impedance analysis to estimate body composition in surgical and oncological patients: a systematic review. Eur J Clin Nutr. 2015;69:3–13. doi: 10.1038/ejcn.2014.203. [DOI] [PubMed] [Google Scholar]
- 8.Bussolotto M, Ceccon A, Sergi G, Giantin V, Beninca P, Enzi G. Assessment of body composition in elderly: accuracy of bioelectrical impedance analysis. Gerontology. 1999;45:39–43. doi: 10.1159/000022053. [DOI] [PubMed] [Google Scholar]
- 9.Lupoli L, Sergi G, Coin A, Perissinotto E, Volpato S, Busetto L, Inelmen EM, Enzi G. Body composition in underweight elderly subjects: reliability of bioelectrical impedance analysis. Clin Nutr. 2004;23:1371–80. doi: 10.1016/j.clnu.2004.05.005. [DOI] [PubMed] [Google Scholar]
- 10.Norman K, Stobaus N, Pirlich M, Bosy-Westphal A. Bioelectrical phase angle and impedance vector analysis–clinical relevance and applicability of impedance parameters. Clin Nutr. 2012;31:854–61. doi: 10.1016/j.clnu.2012.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Baumgartner RN, Chumlea WC, Roche AF. Bioelectric impedance phase angle and body composition. Am J Clin Nutr. 1988;48:16–23. doi: 10.1093/ajcn/48.1.16. [DOI] [PubMed] [Google Scholar]
- 12.Huemer MT, Petrera A, Hauck SM, Drey M, Peters A, Thorand B. Proteomics of the phase angle: results from the population-based KORA S4 study. Clin Nutr. 2022;41:1818–26. doi: 10.1016/j.clnu.2022.06.038. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs LH, van de Kerkhof JJ, Mingels AM, Passos VL, Kleijnen VW, Mazairac AH, van der Sande FM, Wodzig WK, Konings CJ, Leunissen KM, van Dieijen-Visser MP, Kooman JP. Inflammation, overhydration and cardiac biomarkers in haemodialysis patients: a longitudinal study. Nephrol Dial Transplant. 2010;25:243–8. doi: 10.1093/ndt/gfp417. [DOI] [PubMed] [Google Scholar]
- 14.Mattiello R, Amaral MA, Mundstock E, Ziegelmann PK. Reference values for the phase angle of the electrical bioimpedance: systematic review and meta-analysis involving more than 250,000 subjects. Clin Nutr. 2020;39:1411–7. doi: 10.1016/j.clnu.2019.07.004. [DOI] [PubMed] [Google Scholar]
- 15.Kolodziej M, Ignasiak Z, Ignasiak T. Annual changes in appendicular skeletal muscle mass and quality in adults over 50 y of age, assessed using bioelectrical impedance analysis. Nutrition. 2021;90:111342. doi: 10.1016/j.nut.2021.111342. [DOI] [PubMed] [Google Scholar]
- 16.da Silva BR, Gonzalez MC, Cereda E, Prado CM. Exploring the potential role of phase angle as a marker of oxidative stress: a narrative review. Nutrition. 2022;93:111493. doi: 10.1016/j.nut.2021.111493. [DOI] [PubMed] [Google Scholar]
- 17.Tomeleri CM, Cavaglieri CR, de Souza MF, Cavalcante EF, Antunes M, Nabbuco HCG, Venturini D, Barbosa DS, Silva AM, Cyrino ES. Phase angle is related with inflammatory and oxidative stress biomarkers in older women. Exp Gerontol. 2018;102:12–8. doi: 10.1016/j.exger.2017.11.019. [DOI] [PubMed] [Google Scholar]
- 18.Luo J, Mills K, le Cessie S, Noordam R, van Heemst D. Ageing, age-related diseases and oxidative stress: what to do next? Ageing Res Rev. 2020;57:100982. doi: 10.1016/j.arr.2019.100982. [DOI] [PubMed] [Google Scholar]
- 19.Norman K, Smoliner C, Kilbert A, Valentini L, Lochs H, Pirlich M. Disease-related malnutrition but not underweight by BMI is reflected by disturbed electric tissue properties in the bioelectrical impedance vector analysis. Br J Nutr. 2008;100:590–5. doi: 10.1017/S0007114508911545. [DOI] [PubMed] [Google Scholar]
- 20.Norman K, Smoliner C, Valentini L, Lochs H, Pirlich M. Is bioelectrical impedance vector analysis of value in the elderly with malnutrition and impaired functionality? Nutrition. 2007;23:564–9. doi: 10.1016/j.nut.2007.05.007. [DOI] [PubMed] [Google Scholar]
- 21.Slee A, Birc D, Stokoe D. Bioelectrical impedance vector analysis, phase-angle assessment and relationship with malnutrition risk in a cohort of frail older hospital patients in the United Kingdom. Nutrition. 2015;31:132–7. doi: 10.1016/j.nut.2014.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Varan HD, Bolayir B, Kara O, Arik G, Kizilarslanoglu MC, Kilic MK, Sumer F, Kuyumcu ME, Yesil Y, Yavuz BB, Halil M, Cankurtaran M. Phase angle assessment by bioelectrical impedance analysis and its predictive value for malnutrition risk in hospitalized geriatric patients. Aging Clin Exp Res. 2016;28:1121–6. doi: 10.1007/s40520-015-0528-8. [DOI] [PubMed] [Google Scholar]
- 23.Kubo Y, Noritake K, Nakashima D, Fujii K, Yamada K. Relationship between nutritional status and phase angle as a noninvasive method to predict malnutrition by sex in older inpatients. Nagoya J Med Sci. 2021;83:31–40. doi: 10.18999/nagjms.83.1.31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rinaldi S, Gilliland J, O’Connor C, Chesworth B, Madill J. Is phase angle an appropriate indicator of malnutrition in different disease states? A systematic review. Clin Nutr ESPEN. 2019;29:1–14. doi: 10.1016/j.clnesp.2018.10.010. [DOI] [PubMed] [Google Scholar]
- 25.Plauth M, Sulz I, Viertel M, Hofer V, Witt M, Raddatz F, Reich M, Hiesmayr M, Bauer P. Phase Angle is a stronger predictor of Hospital Outcome than Subjective Global Assessment-Results from the prospective Dessau Hospital Malnutrition Study. Nutrients. 2022;14. DOI:10.3390/nu14091780. [DOI] [PMC free article] [PubMed]
- 26.Stobaus N, Pirlich M, Valentini L, Schulzke JD, Norman K. Determinants of bioelectrical phase angle in disease. Br J Nutr. 2012;107:1217–20. doi: 10.1017/S0007114511004028. [DOI] [PubMed] [Google Scholar]
- 27.Lukaski HC, Kyle UG, Kondrup J. Assessment of adult malnutrition and prognosis with bioelectrical impedance analysis: phase angle and impedance ratio. Curr Opin Clin Nutr Metab Care. 2017;20:330–9. doi: 10.1097/MCO.0000000000000387. [DOI] [PubMed] [Google Scholar]
- 28.Stark G. Functional consequences of oxidative membrane damage. J Membr Biol. 2005;205:1–16. doi: 10.1007/s00232-005-0753-8. [DOI] [PubMed] [Google Scholar]
- 29.Norman K, Pirlich M, Sorensen J, Christensen P, Kemps M, Schutz T, Lochs H, Kondrup J. Bioimpedance vector analysis as a measure of muscle function. Clin Nutr. 2009;28:78–82. doi: 10.1016/j.clnu.2008.11.001. [DOI] [PubMed] [Google Scholar]
- 30.Hirano Y, Yamada Y, Matsui Y, Ota S, Arai H. Lower limb muscle quality and phase angle contribute to the reduced walking speed among older adults. Geriatr Gerontol Int. 2022;22:603–9. doi: 10.1111/ggi.14423. [DOI] [PubMed] [Google Scholar]
- 31.Tomeleri CM, Cavalcante EF, Antunes M, Nabuco HCG, de Souza MF, Teixeira DC, Gobbo LA, Silva AM, Cyrino ES. Phase Angle is moderately Associated with muscle quality and functional capacity, Independent of Age and Body Composition in Older Women. J Geriatr Phys Ther. 2019;42:281–6. doi: 10.1519/JPT.0000000000000161. [DOI] [PubMed] [Google Scholar]
- 32.Bittencourt DCD, Schieferdecker MEM, Macedo DS, Biesek S, Silveira Gomes AR, Rabito EI. Phase Angle reflects loss of functionality in Older Women. J Nutr Health Aging. 2020;24:251–4. doi: 10.1007/s12603-020-1324-5. [DOI] [PubMed] [Google Scholar]
- 33.Oliveira R, Leao C, Silva AF, Clemente FM, Santamarinha CT, Nobari H, Brito JP. Comparisons between Bioelectrical Impedance variables, functional tests and blood markers based on BMI in older women and their Association with Phase Angle. Int J Environ Res Public Health. 2022;19. DOI:10.3390/ijerph19116851. [DOI] [PMC free article] [PubMed]
- 34.Norman K, Wirth R, Neubauer M, Eckardt R, Stobaus N. The bioimpedance phase angle predicts low muscle strength, impaired quality of life, and increased mortality in old patients with cancer. J Am Med Dir Assoc. 2015;16:173 e17–22. doi: 10.1016/j.jamda.2014.10.024. [DOI] [PubMed] [Google Scholar]
- 35.Selberg O, Selberg D. Norms and correlates of bioimpedance phase angle in healthy human subjects, hospitalized patients, and patients with liver cirrhosis. Eur J Appl Physiol. 2002;86:509–16. doi: 10.1007/s00421-001-0570-4. [DOI] [PubMed] [Google Scholar]
- 36.Di Vincenzo O, Marra M, Scalfi L. Bioelectrical impedance phase angle in sport: a systematic review. J Int Soc Sports Nutr. 2019;16:49. doi: 10.1186/s12970-019-0319-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Genton L, Mareschal J, Norman K, Karsegard VL, Delsoglio M, Pichard C, Graf C, Herrmann FR. Association of phase angle and running performance. Clin Nutr ESPEN. 2020;37:65–8. doi: 10.1016/j.clnesp.2020.03.020. [DOI] [PubMed] [Google Scholar]
- 38.Akamatsu Y, Kusakabe T, Arai H, Yamamoto Y, Nakao K, Ikeue K, Ishihara Y, Tagami T, Yasoda A, Ishii K, Satoh-Asahara N. Phase angle from bioelectrical impedance analysis is a useful indicator of muscle quality. J Cachexia Sarcopenia Muscle. 2022;13:180–9. doi: 10.1002/jcsm.12860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyere O, Cederholm T, Cooper C, Landi F, Rolland Y, Sayer AA, Schneider SM, Sieber CC, Topinkova E, Vandewoude M, Visser M, Zamboni M. Writing Group for the european Working Group on Sarcopenia in older P, the Extended Group for E. Sarcopenia: revised european consensus on definition and diagnosis. Age Ageing. 2019;48:16–31. doi: 10.1093/ageing/afy169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gonzalez MC, Barbosa-Silva TG, Bielemann RM, Gallagher D, Heymsfield SB. Phase angle and its determinants in healthy subjects: influence of body composition. Am J Clin Nutr. 2016;103:712–6. doi: 10.3945/ajcn.115.116772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Mundstock E, Amaral MA, Baptista RR, Sarria EE, Dos Santos RRG, Filho AD, Rodrigues CAS, Forte GC, Castro L, Padoin AV, Stein R, Perez LM, Ziegelmann PK, Mattiello R. Association between phase angle from bioelectrical impedance analysis and level of physical activity: systematic review and meta-analysis. Clin Nutr. 2019;38:1504–10. doi: 10.1016/j.clnu.2018.08.031. [DOI] [PubMed] [Google Scholar]
- 42.Di Vincenzo O, Marra M, Di Gregorio A, Pasanisi F, Scalfi L. Bioelectrical impedance analysis (BIA) -derived phase angle in sarcopenia: a systematic review. Clin Nutr. 2021;40:3052–61. doi: 10.1016/j.clnu.2020.10.048. [DOI] [PubMed] [Google Scholar]
- 43.Walowski CO, Braun W, Maisch MJ, Jensen B, Peine S, Norman K, Muller MJ, Bosy-Westphal A. Reference values for skeletal muscle Mass - Current Concepts and Methodological Considerations. Nutrients. 2020;12. DOI:10.3390/nu12030755. [DOI] [PMC free article] [PubMed]
- 44.Perez Camargo DA, Allende Perez SR, Verastegui Aviles E, Rivera Franco MM, Meneses Garcia A, Herrera Gomez A, Urbalejo Ceniceros VI. Assessment and Impact of Phase Angle and Sarcopenia in Palliative Cancer Patients. Nutr Cancer. 2017;69:1227–33. doi: 10.1080/01635581.2017.1367939. [DOI] [PubMed] [Google Scholar]
- 45.Sipers W, de Blois W, Schols J, van Loon LJC, Verdijk LB. Sarcopenia is related to Mortality in the acutely hospitalized geriatric patient. J Nutr Health Aging. 2019;23:128–37. doi: 10.1007/s12603-018-1134-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landi F, Calvani R, Cesari M, Tosato M, Martone AM, Bernabei R, Onder G, Marzetti E. Sarcopenia as the Biological substrate of physical Frailty. Clin Geriatr Med. 2015;31:367–74. doi: 10.1016/j.cger.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 47.Wilhelm-Leen ER, Hall YN, Horwitz RI, Chertow GM. Phase angle, frailty and mortality in older adults. J Gen Intern Med. 2014;29:147–54. doi: 10.1007/s11606-013-2585-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rosas-Carrasco O, Ruiz-Valenzuela RE, Lopez-Teros MT. Phase Angle cut-off points and their Association with Sarcopenia and Frailty in adults of 50–64 years old and older adults in Mexico City. Front Med (Lausanne) 2021;8:617126. doi: 10.3389/fmed.2021.617126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tanaka S, Ando K, Kobayashi K, Seki T, Hamada T, Machino M, Ota K, Morozumi M, Kanbara S, Ito S, Ishiguro N, Hasegawa Y, Imagama S. Low Bioelectrical Impedance Phase Angle is a significant risk factor for Frailty. Biomed Res Int. 2019;2019:6283153. doi: 10.1155/2019/6283153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zanforlini BM, Trevisan C, Bertocco A, Piovesan F, Dianin M, Mazzochin M, Alessi A, Zoccarato F, Manzato E, Sergi G. Phase angle and metabolic equivalents as predictors of frailty transitions in advanced age. Exp Gerontol. 2019;122:47–52. doi: 10.1016/j.exger.2019.04.016. [DOI] [PubMed] [Google Scholar]
- 51.Matsumoto Y, Tada M, Yamada Y, Mandai K, Hidaka N, Koike T. The bioimpedance phase angle is more useful than sarcopenia as a predictor of falls in patients with rheumatoid arthritis: results from a 2-y prospective cohort study. Nutrition. 2022;102:111729. doi: 10.1016/j.nut.2022.111729. [DOI] [PubMed] [Google Scholar]
- 52.Jung YW, Hong N, Kim CO, Kim HC, Youm Y, Choi J, Rhee Y. The diagnostic value of phase angle, an integrative bioelectrical marker, for identifying individuals with dysmobility syndrome: the korean Urban-Rural Elderly study. Osteoporos Int. 2021;32:939–49. doi: 10.1007/s00198-020-05708-2. [DOI] [PubMed] [Google Scholar]
- 53.Uemura K, Doi T, Tsutsumimoto K, Nakakubo S, Kim MJ, Kurita S, Ishii H, Shimada H. Predictivity of bioimpedance phase angle for incident disability in older adults. J Cachexia Sarcopenia Muscle. 2020;11:46–54. doi: 10.1002/jcsm.12492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Uemura K, Yamada M, Okamoto H. Association of bioimpedance phase angle and prospective falls in older adults. Geriatr Gerontol Int. 2019;19:503–7. doi: 10.1111/ggi.13651. [DOI] [PubMed] [Google Scholar]
- 55.Roman E, Poca M, Amoros-Figueras G, Rosell-Ferrer J, Gely C, Nieto JC, Vidal S, Urgell E, Ferrero-Gregori A, Alvarado-Tapias E, Cuyas B, Hernandez E, Santesmases R, Guarner C, Escorsell A, Soriano G. Phase angle by electrical bioimpedance is a predictive factor of hospitalisation, falls and mortality in patients with cirrhosis. Sci Rep. 2021;11:20415. doi: 10.1038/s41598-021-99199-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Genton L, Norman K, Spoerri A, Pichard C, Karsegard VL, Herrmann FR, Graf CE. Bioimpedance-Derived Phase Angle and Mortality among older people. Rejuvenation Res. 2017;20:118–24. doi: 10.1089/rej.2016.1879. [DOI] [PubMed] [Google Scholar]
- 57.Wirth R, Volkert D, Rosler A, Sieber CC, Bauer JM. Bioelectric impedance phase angle is associated with hospital mortality of geriatric patients. Arch Gerontol Geriatr. 2010;51:290–4. doi: 10.1016/j.archger.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 58.Mullie L, Obrand A, Bendayan M, Trnkus A, Ouimet MC, Moss E, Chen-Tournoux A, Rudski LG, Afilalo J. Phase Angle as a biomarker for Frailty and Postoperative Mortality: the BICS Study. J Am Heart Assoc. 2018;7:e008721. doi: 10.1161/JAHA.118.008721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Cornejo-Pareja I, Vegas-Aguilar IM, Garcia-Almeida JM, Bellido-Guerrero D, Talluri A, Lukaski H, Tinahones FJ. Phase angle and standardized phase angle from bioelectrical impedance measurements as a prognostic factor for mortality at 90 days in patients with COVID-19: a longitudinal cohort study. Clin Nutr. 2021 doi: 10.1016/j.clnu.2021.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ellegard LH, Petersen P, Ohrn L, Bosaeus I. Longitudinal changes in phase angle by bioimpedance in intensive care patients differ between survivors and non-survivors. Clin Nutr ESPEN. 2018;24:170–2. doi: 10.1016/j.clnesp.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 61.Campa F, Colognesi LA, Moro T, Paoli A, Casolo A, Santos L, Correia RR, Lemes IR, Milanez VF, Christofaro DD, Cyrino ES, Gobbo LA. Effect of resistance training on bioelectrical phase angle in older adults: a systematic review with Meta-analysis of randomized controlled trials. Rev Endocr Metab Disord. 2022 doi: 10.1007/s11154-022-09747-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nunes JP, Ribeiro AS, Silva AM, Schoenfeld BJ, Dos Santos L, Cunha PM, Nascimento MA, Tomeleri CM, Nabuco HCG, Antunes M, Cyrino LT, Cyrino ES. Improvements in Phase Angle are related with muscle Quality Index after Resistance Training in Older Women. J Aging Phys Act. 2019;27:515–20. doi: 10.1123/japa.2018-0259. [DOI] [PubMed] [Google Scholar]
- 63.Tomeleri CM, Ribeiro AS, Cavaglieri CR, Deminice R, Schoenfeld BJ, Schiavoni D, Dos Santos L, de Souza MF, Antunes M, Venturini D, Barbosa DS, Sardinha LB, Cyrino ES. Correlations between resistance training-induced changes on phase angle and biochemical markers in older women. Scand J Med Sci Sports. 2018;28:2173–82. doi: 10.1111/sms.13232. [DOI] [PubMed] [Google Scholar]
- 64.Freitas SP, Judice PB, Hetherington-Rauth M, Magalhaes JP, Correia IR, Lopes JM, Strong C, Matos D, Sardinha LB. The impact of 2 weeks of detraining on phase angle, BIVA patterns, and muscle strength in trained older adults. Exp Gerontol. 2021;144:111175. doi: 10.1016/j.exger.2020.111175. [DOI] [PubMed] [Google Scholar]
- 65.Barrea L, Muscogiuri G, Aprano S, Vetrani C, de Alteriis G, Varcamonti L, Verde L, Colao A, Savastano S. Phase angle as an easy diagnostic tool for the nutritionist in the evaluation of inflammatory changes during the active stage of a very low-calorie ketogenic diet. Int J Obes (Lond) 2022;46:1591–7. doi: 10.1038/s41366-022-01152-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Beberashvili I, Azar A, Sinuani I, Kadoshi H, Shapiro G, Feldman L, Sandbank J, Averbukh Z. Longitudinal changes in bioimpedance phase angle reflect inverse changes in serum IL-6 levels in maintenance hemodialysis patients. Nutrition. 2014;30:297–304. doi: 10.1016/j.nut.2013.08.017. [DOI] [PubMed] [Google Scholar]