Abstract
Objective
To identify the associated factors and assess the inequalities of full vaccination coverage (FVC) among Peruvian infants aged 12–23 months during the COVID-19 pandemic in a nationally representative sample.
Methods
We carried out a population-based cross-sectional study based on a secondary data analysis using the 2021 Peruvian Demographic Health Survey (DHS) in infants aged 12 to 23 months. The sampling design was probabilistic, multistage, stratified, and independent at both departmental and area of residence levels. FVC was defined according to the WHO definition. We performed generalized linear models (GLM) Poisson family log link function to estimate crude (aPR) and adjusted prevalence ratios (aPR). Also, for inequality assessment, we calculated the concentration curve (CC), concentration index (CI), and Erreygers normalized concentration index (ECI).
Results
We included 4,189 infants in our analysis. Nationwide, the prevalence of FVC was 66.19% (95% CI: 64.33–68). Being younger, having a mother with no education or primary education, belonging to a large family, having no access to mass media, having had six or fewer ANC visits, and having a mother whose age was under 20 at first delivery were inversely associated with FVC. Meanwhile, living in the Highlands or on the rest of the coast, and living in rural areas were directly associated with FVC. We found a pro-rich inequality in FVC based on wealth-ranked households (CI: 0.0066; ECI: 0.0175).
Conclusion
FVC has dropped among Peruvian infants aged between 12 and 23 months. There were several factors associated with FVC. It was more concentrated among the better-off infants, although in low magnitude.
Keywords: COVID-19, Vaccination coverage, Healthcare disparities, Peru, Low- and middle-income countries
1. Introduction
Vaccination is one of the most powerful public health interventions worldwide. Vaccines are a highly cost-effective measure, especially in low- and middle-income countries (LMICs) [1], [2]. The positive effects of vaccines encompass the reduction of the incidence, severity, and mortality of different infections called vaccine-preventable diseases (VPD), thereby reducing the disease burden and the healthcare services demand [3], [4]. It is paramount to note that the major effect of vaccines is at the population level through direct and indirect protection, where vaccination coverage is essential [5]. In fact, national vaccination programs are crucial collective health strategies, particularly those aimed at children.
Infants’ vaccination coverage is crucial. Nevertheless, it faces numerous challenges depending on the context, especially considering the current situation due to the COVID-19 pandemic. Globally, vaccination coverage has dropped from 86% in 2019 to 83% in 2020 [6]. Moreover, a relative reduction of 7.7% was estimated for the delivery of the third dose of the diphtheria-tetanus-pertussis vaccine and 7.9% for the first dose of the measles-containing vaccine (MCV1) [7]. This reduction conditions the resurgence of VPD, particularly, in Latin American (LATAM) regions [7]. Prior to the COVID-19 pandemic, infants’ vaccination coverage was jeopardized by various factors such as antivaccine groups, and sociocultural aspects, among others [8]. Worse still, the COVID-19 pandemic had a negative impact on several public health interventions, including immunization programs. Social distancing and isolation were primary measures established by governments to mitigate the COVID-19 pandemic, challenging the delivery of vaccines to the target populations [9]. Nationwide, the temporary closure of primary healthcare centers aggravated the delivery of vaccines [10], [11]. All of this probably contributed to situations like a case of diphtheria reported in Peru after 20 years of epidemiological silence on the disease [12]. According to the above, it is pivotal to evaluate infants’ vaccination coverage during the COVID-19 pandemic.
In the context of the COVID-19 pandemic, it is worthwhile to evaluate the factors associated with vaccination coverage. The World Health Organization (WHO) is concerned about fair access to safe and effective vaccines; thus, its 2030 immunization agenda focuses on improving coverage and reducing inequities worldwide [13]. Before the pandemic, studies conducted on full vaccination coverage (FVC), a WHO-standardized health indicator [14], found that it has increased over the latest decades, but the coverage in the LATAM region remained low with high-income inequality gaps [15]. Several factors such as maternal education, antenatal care (ANC) visits, knowledge, and attitudes about immunization, ethnicity, and mass media access, among others, have shown to be directly associated with FVC [16], [17], [18], [19], whereas home delivery, younger maternal age, urban residence, and no post-natal care visits, among others, were inversely associated with FVC [20], [21]. By implementing policies addressing the factors associated in the Peruvian setting, FVC would broaden. In addition, there are regional differences in FVC, which might be explained by the presence of clusters with different geographic, geopolitical, and demographic characteristics [12], [22]. Therefore, these variations should be studied when it is a priority to identify inequalities in access to vaccines.
The National Vaccination Program is universally administered country-wide in healthcare centers without charge. It was last updated in 2018, and certain vaccines have been added over the years, such as the chickenpox vaccine. It includes seventeen vaccines protecting against at least 26 diseases. Its target population primarily includes infants under five years old, but it also includes pregnant women and the elderly. Its comprehensive character profiles it as one of the most complete vaccination plans in LATAM [23].
Nationwide, regional disparities and high-risk clusters for VPD [12], [22] have been reported, suggesting potential sociodemographic factors and inequalities in FVC. Despite Peru has a very comprehensive and free-of-charge immunization schedule for infants under five years of age [23], it does not ensure broad coverage. To the best of our knowledge, no scientific publications assessed FVC in the pandemic period in LATAM infants. Hence, we aimed to identify the associated factors and assess the inequalities of FVC among Peruvian infants aged 12–23 months during the COVID-19 pandemic in a sample with national representativeness.
2. Materials and methods
2.1. Study design, population, sampling, sample size, and data source
We conducted a cross-sectional study based on the secondary data analysis of the 2021 Peruvian Demographic Health Survey (DHS). This is a national and continuous survey executed yearly by the National Institute of Statistics and Informatics of Peru (INEI, from the Spanish acronym). The sampling design employed was probabilistic, multistage, stratified, and independent at both departmental and area of residence levels. Peruvian DHS has national, departmental, and area of residence representativeness. In urban areas, the sampling unit included conglomerate and private dwellings, while in rural areas, it included rural census regions and private dwellings. Peru is an upper middle-income country, administratively divided into 24 departments and one constitutional province. A table describing the main socioeconomic characteristics of the departments is provided in Supplementary 1. The sample size was 36,760 dwellings: 24,100 from urban areas and 12,660 from rural areas [24]. Specifically, for our analysis, we included infants aged 12 to 23 months. We excluded those subjects without complete data regarding the variables of interest.
2.2. Outcome definition
According to the WHO, crude FVC is defined by those infants aged one year old that have completely received: one dose of Bacille Calmette Guerin (BCG) vaccine; three doses of the combined diphtheria, tetanus, and pertussis vaccine (DTP3); three doses of the polio vaccine (Pol3); and MCV1 [14]. In the Peruvian National Vaccination Schedule, currently ongoing, DTP3 is administered with the pentavalent vaccine, which also includes the Haemophilus b conjugate and hepatitis B (HepB) vaccine. Likewise, MCV1 is administered in combination with the rubella and mumps vaccine (MMR) [23]. (See Supplementary 2) FVC was collected by reviewing infants’ vaccination cards, but in its absence, it was collected from the mothers’ verbal report. This binary variable was coded as 0 for incomplete vaccination coverage and one for FVC.
2.3. Exposure variables
The variables were grouped into four groups: demographic, socioeconomic status (SES), socio-demographic, and delivery. Demographic variables included sex (male, female), age (in years), and region of origin (Metropolitan Lima, the rest of the coast, the Highlands, the jungle). SES included wealth index (poor, middle, rich), and mother’s educational level (no education/primary, secondary, higher). Sociodemographic variables included the area of residence (urban, rural), family size (<4, 4–6, > 6 members), and mass media access (yes, no), which included having a TV, internet, or radio in the household. Finally, delivery-related variables included ANC visits (0–6, > 6 visits), mother’s age at first delivery (<20, 20–34, > 34 years), and place of delivery (home, health facility). (See Fig. 1 ).
Fig. 1.
Scheme of variables.
To assess SES, we employed the wealth index as a proxy measure, which measures households’ assets and holdings such as automobiles, home appliances, access to basic services, and access to healthcare services, among others. It places the individual interviewed on a continuous scale of wealth, which is then divided into five quintiles. It is calculated through a statistical analysis known as principal components analysis [25]. The wealth index has been previously used in other international studies, even in the Peruvian context [26], [27].
2.4. Statistical analysis
2.4.1. Descriptive, bivariate, and multiple regression analysis
All the analyses were performed in STATA version 16.0 (Stata Corporation, College Station, TX, USA) using complex survey design modules (svy). The baseline characteristics of the categorial variables were described through absolute and relative frequencies, whereas age was described through the mean and its standard deviation (SD). For bivariate analysis, the Pearson chi-square test was used to compare the proportion of the outcome variable over each category of the independent variables, while an adjusted Wald test was used for numerical variables. All the variables were adjusted in the multiple regression model, but we also conducted models adjusting by each group of variables. Crude (aPR) and adjusted prevalence ratios (aPR) were estimated through generalized linear models (glm) Poisson family log link function. In addition, we performed a sensitivity analysis according to the source of vaccination data. Confidence intervals were computed to 95% (95% CI), and p values < 0.05 were considered statistically significant.
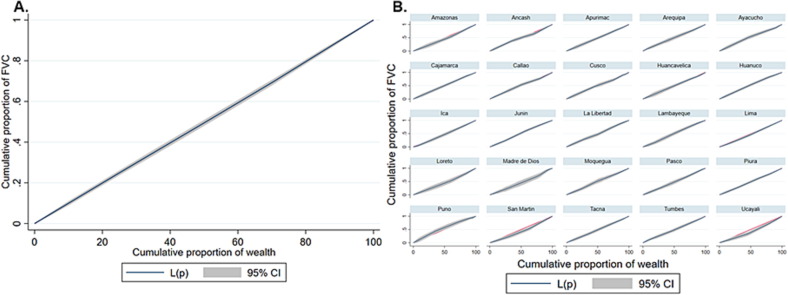
2.4.2. Inequality analysis
We calculated the concentration curve (CC), concentration index (CI), and Erreygers normalized concentration index (ECI) [28], [29]. The CC provides a graphical view of inequality assessing the degree of income-related inequality in the distribution of a health variable. It plots FVC (y-axis) against the wealth index (x-axis). Meanwhile, the ECI is the corrected version of the concentration index (CI), which measures the magnitude of inequality and is defined as twice the area between the CC and the line of equality (45° line). The CI ranges from −1 to + 1. A positive value implies that FVC is concentrated among the richest, while a negative value implies that it is concentrated among the poorest. The correction of CI by Erreygers standardizes the uncorrected index by adjusting the CI to allow for the binary nature of the health variable. The ECI is the CI multiplied by four times the outcome of interest [30]. According to international guidelines, we reported both CI and ECI [31].
2.4.3. Ethical considerations
Peruvian DHS is a database in the public domain [32], and it does not collect personal information that could reveal identities. Thus, it did not require approval by an ethics committee.
3. Results
3.1. Characteristics of participants
A total of 4,334 infants aged 12–23 months were surveyed by the 2021 DHS. Of these, 145 (3.35%) were excluded due to incomplete data for the variables of interest. We included 4,189 infants in our analysis. The mean age of the participants was 17.46 (SD: ± 3.47) months, and 50.83% were male. Most of the population lived in urban areas (73.95%), had a medium family size (62.86%), had access to mass media (90.05%), and was born at health facilities (94%). Likewise, 32.99% and 35.48% had a poor and rich wealth index, respectively. Additionally, 55.2 % of mothers were aged between 20 and 34 years old at first delivery, 72.43% had more than six ANC visits, and 35.48% had a higher educational level. The main source of vaccination data was the direct observation of vaccination cards (90.24%). (See Table 1 ).
Table 1.
Characteristics of Peruvian infants aged 12–23 months and their FVC.
| Variables | n (%) | FVC % | Non-FVC | p-value | |
|---|---|---|---|---|---|
| Demographic | |||||
| Age (months) | < 0.001a | ||||
| 12–15 | 1,524 (34.07) | 54.55 | 45.45 | ||
| 16–19 | 1,386 (32.35) | 69.4 | 30.6 | ||
| 20–23 | 1,424 (33.58) | 74.93 | 25.07 | ||
| Mean (SD) | 17.46 (±3.47) | 17.91 (±3.37) | 16.57 (±3.51) | < 0.001b | |
| Sex | 0.0551a | ||||
| Male | 2,212 (50.83) | 67.9 | 32.1 | ||
| Female | 2,122 (49.17) | 64.43 | 35.57 | ||
| Region of origin | 0.0017a | ||||
| Lima | 537 (25.29) | 61.65 | 38.35 | ||
| Rest of the coast | 1,308 (28.82) | 67.55 | 32.45 | ||
| Highlands | 1,39 (27.73) | 70.86 | 29.14 | ||
| Jungle | 1,096 (18.15) | 63.25 | 36.75 | ||
| Socioeconomic status | |||||
| Wealth index | 0.5077a | ||||
| Poor | 2,475 (32.99) | 65.44 | 34.56 | ||
| Middle | 834 (31.53) | 65.51 | 34.49 | ||
| Rich | 1,025 (35.48) | 67.94 | 32.06 | ||
| Mother’s education | < 0.001a | ||||
| No education/Primary | 1,484 (32.99) | 60.3 | 39.7 | ||
| Secondary | 1,356 (31.53) | 66.31 | 33.69 | ||
| Higher | 1,494 (35.48) | 71.57 | 28.43 | ||
| Sociodemographic | |||||
| Area of residence | 0.4188a | ||||
| Urban | 2,995 (73.95) | 65.77 | 34.23 | ||
| Rural | 1,339 (26.05) | 67.4 | 32.6 | ||
| Family size | < 0.001a | ||||
| Small (<4 members) | 836 (18.36) | 70.98 | 29.02 | ||
| Medium (4–6 members) | 2,743 (62.86) | 66.92 | 33.08 | ||
| Large (<6 members) | 755 (18.77) | 59.09 | 40.91 | ||
| Mass media access (internet, TV, radio) | 0.0026a | ||||
| Yes | 3,826 (90.05) | 67.01 | 32.99 | ||
| No | 508 (9.95) | 58.78 | 41.22 | ||
| Delivery-related | |||||
| ANC visits | < 0.001a | ||||
| 06 | 1,109 (27.57) | 56.09 | 43.91 | ||
| > 6 | 3,124 (72.43) | 70.16 | 29.84 | ||
| Mother’s age at first delivery | < 0.001a | ||||
| < 20 years | 1,960 (42.4) | 59.79 | 40.21 | ||
| 20–34 years | 2,284 (55.2) | 71.39 | 28.61 | ||
| > 34 years | 90 (2.41) | 59.8 | 40.2 | ||
| Place of delivery | 0.0012a | ||||
| Home | 247 (6) | 54.69 | 45.31 | ||
| Health facility | 4,040 (94) | 66.98 | 33.02 | ||
All proportions were weighted. a Chi square test. b Adjusted Wald test.
3.2. Vaccination coverage
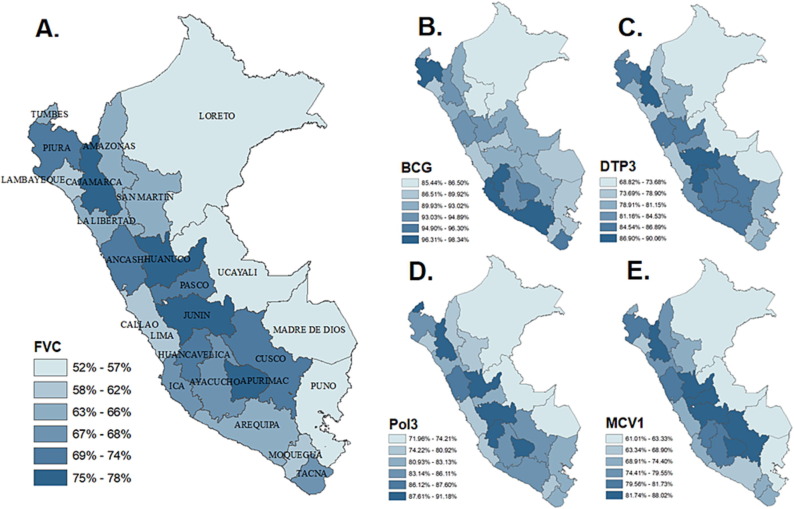
Nationwide, the frequency of FVC was 66.19% (95% CI: 64.33–68) and it ranged from 51.50% to 78.30% among departments. However, when stratifying the analysis according to the source of vaccination data, FVC was 70.62% (95% CI: 68.71–72.46) in those who owned the vaccination card and 25.25 % (95% CI: 20.74–30.35) in those whose mothers self-reported the vaccination data. Concerning the components of FVC, the highest coverage was from BCG (91.89%), followed by Pol3 (82.97%), DTP3 (81.76%), and MCV1 (75.51%). After stratifying by region of origin, the highest coverage of each vaccine was found in the Highlands, whereas the lowest coverage of BCG and DTP3 was found in the Lima Metropolitan area, and of Pol 3 and MCV1 in the Jungle. (See Fig. 2 and Fig. 3 )
Fig. 2.
Proportion of FVC and its components among Peruvian infants aged 12–23 months amid the COVID-19 pandemic, by region of origin. BCG: Bacille Calmette Guerin vaccine. DTP3: three doses of combined diphtheria, tetanus, and pertussis vaccine. Pol3: three doses of polio vaccine. MCV1: measles-containing vaccine.
Fig. 3.
Proportion of FVC and its components among Peruvian infants aged 12–23 months amid the COVID-19 pandemic according to departments. (A) Proportion of FVC according to departments. (B) Coverage of BCG vaccine according to departments. (C) Coverage of DTP3 vaccine according to departments. (D) Coverage of Pol3 vaccine according to departments. (E) Coverage of MCV1 vaccine according to departments.
3.3. FVC according to sociodemographic factors
Most of the evaluated variables showed statistically significant associations (p < 0.05), except for sex, wealth index, and area of residence. FVC showed a higher proportion among mothers whose age at first delivery was 20–34 years old (71.39%), whose mothers had higher education (71.57%), had attended more than six ANC visits (70.16%), had a small family size (70.98%), had mass media access (67.01%), and lived in the Highlands (70.86%). Meanwhile, the lowest FVC was found among those with <6 ANC visits (56.09%) and born at home (54.69%). (See Table 1).
3.4. Multiple regression analysis
Factors associated with FVC are shown in Table 2 . In comparison with infants aged 20–23 months, infants aged 12–15 months (aPR = 0.74, 95% CI: 0.69–0.79) and 16–19 months (aPR = 0.94, 95% CI: 0.88–0.99) had less probability of having FVC. Living outside of the Lima Metropolitan area, either in the rest of the Coast (aPR = 1.10, 95% CI: 1.01–1.20) or in the Highlands (aPR = 1.15, 95% CI: 1.05–1.26), was directly associated to FVC. Having had a mother with primary or no education was associated with fewer probabilities of FVC (aPR = 0.87; 95% CI: 0.80–0.95) when compared to mothers with a higher educational level. Additionally, living in a rural setting (aPR = 1.08; 95% CI: 1.00–1.16) was directly associated with FVC, compared to living in an urban area. Other variables inversely associated were not having access to mass media (aPR = 0.89; 95% CI: 0.81–0.98), belonging to a large family (aPR = 0.91; 95% CI: 0.83–0.99), and having had less than six ANC visits (aPR = 0.87; 95% CI: 0.81–0.93).
Table 2.
Factors associated with FVC in Peruvian infants aged 12–23 months.
|
Crude model |
Adjusted model |
||||||
|---|---|---|---|---|---|---|---|
| (c)PRa | 95% CI | p-value | (a)PRb* | 95% CI | p-value | ||
| Demographic | |||||||
| Age (months) | |||||||
| 1215 | 0.72 | 0.68–0.77 | < 0.001 | 0.74 | 0.69–0.79 | < 0.001 | |
| 16–19 | 0.92 | 0.87–0.98 | 0.010 | 0.94 | 0.88–0.99 | 0.042 | |
| 20–23 | Ref | Ref | Ref | Ref | Ref | Ref | |
| Sex | |||||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref | |
| Female | 0.94 | 0.89–1.00 | 0.055 | 0.96 | 0.91–1.01 | 0.148 | |
| Region of origin | |||||||
| Lima Metropolitan | Ref | Ref | Ref | Ref | Ref | Ref | |
| Rest of the coast | 1.09 | 1.00–1.19 | 0.044 | 1.10 | 1.01–1.20 | 0.022 | |
| Highlands | 1.14 | 1.05–1.25 | 0.001 | 1.15 | 1.05–1.26 | 0.001 | |
| Jungle | 1.02 | 0.93–1.12 | 0.598 | 1.08 | 0.98–1.19 | 0.097 | |
| Socioeconomic status | |||||||
| Wealth index | |||||||
| Poor | 0.96 | 0.90–1.02 | 0.259 | 0.99 | 0.91–1.07 | 0.813 | |
| Middle | 0.96 | 0.88–1.05 | 0.402 | 0.97 | 0.90–1.06 | 0.813 | |
| Rich | Ref | Ref | Ref | Ref | Ref | Ref | |
| Mother’s education | |||||||
| No education/Primary | 0.84 | 0.79-0.89 | < 0.001 | 0.87 | 0.80–0.95 | 0.001 | |
| Secondary | 0.92 | 0.87-0.98 | 0.016 | 0.94 | 0.88–1.01 | 0.120 | |
| Higher | Ref | Ref | Ref | Ref | Ref | Ref | |
| Sociodemographic | |||||||
| Area of residence | |||||||
| Urban | Ref | Ref | Ref | Ref | Ref | Ref | |
| Rural | 1.02 | 0.96–1.08 | 0.414 | 1.08 | 1.00–1.16 | 0.035 | |
| Family size | |||||||
| Small (<4 members) | Ref | Ref | Ref | Ref | Ref | Ref | |
| Medium (4–6 members) | 0.94 | 0.88–1-00 | 0.071 | 0.97 | 0.91–1.03 | 0.364 | |
| Large (>6 members) | 0.83 | 0.76–0.75 | < 0.001 | 0.91 | 0.83–0.99 | 0.037 | |
| Mass media access (internet, TV, radio) | |||||||
| Yes | Ref | Ref | Ref | Ref | Ref | Ref | |
| No | 0.87 | 0.79–0.96 | 0.006 | 0.89 | 0.81–0.98 | 0.024 | |
| Delivery-related | |||||||
| ANC visits | |||||||
| 0–6 | 0.79 | 0.74–0.85 | < 0.001 | 0.87 | 0.81–0.93 | < 0.001 | |
| < 6 | Ref | Ref | Ref | Ref | Ref | Ref | |
| Mother’s age at first delivery | |||||||
| < 20 years | 0.83 | 0.79–0.88 | < 0.001 | 0.89 | 0.84-0.95 | 0.001 | |
| 20–34 years | Ref | Ref | Ref | Ref | Ref | Ref | |
| > 34 years | 0.83 | 0.66–1.06 | 0.144 | 0.88 | 0.72–1.09 | 0.269 | |
| Place of delivery | |||||||
| Health facility | Ref | Ref | Ref | Ref | Ref | Ref | |
| Home | 0.81 | 0.70–0.94 | 0.005 | 0.88 | 0.76–1.02 | 0.100 | |
*Multiple regression based on generalized linear model (glm) Poisson family log link function.
(c)PR: crude prevalence ratio; b (a)PR adjusted prevalence ratio.
The multiple regression adjusted by groups of variables is shown in Supplementary 3. Likewise, when stratifying the analysis according to the source of vaccination data, the associations remained similar to those who owned the vaccination card, except for the area of residence, family size, and mass media access, which became not statistically significant. On the other hand, almost all variables were not statistically significant to those whose vaccination data was obtained from the self-report of the mother (See Supplementary 4).
3.5. Inequality analysis
At a national level, there was a pro-rich distribution of FVC among Peruvian infants (CI: 0.0066; ECI: 0.0175) (Fig. 4 A). When stratifying the analysis by departments, the highest values were found in Ucayali (CI: 0.1323; ECI: 0.3001), San Martin (CI: 0.1144; ECI: 0.2999), and Loreto (CI: 0.0755; ECI: 0.1619). Meanwhile, the lowest values were found in Puno (CI: −0.0984; ECI: −0.2153), Huánuco (CI: −0.0429; ECI: −0.1316), and Ayacucho (CI: −0.09287; ECI: −0.0342) (Fig. 4B).
Fig. 4.
Concentration curve of FVC among Peruvian infants aged 12–23 months amid the COVID-19 pandemic. (A) Concentration curve of FVC nationwide (B) Concentration curve of FVC according to departments.
4. Discussion
After a high FVC during the 2010–2019 period (albeit stagnant) [22], there was a substantial decline evidenced in 2021 among Peruvian infants. In fact, according to our findings, at least three out of ten Peruvian infants had incomplete vaccination coverage in 2021. Certain factors were inversely associated with FVC, such as being younger, having a mother with no education or primary, belonging to a large family, having no access to mass media, having had six or fewer ANC visits, and having a mother whose age at first delivery was before the age of 20. Meanwhile, living outside Lima, either in the Highlands or on the rest of the coast, and living in rural areas were directly associated with FVC. Furthermore, a pro-rich inequality in FVC was unveiled, albeit low in magnitude. Our results are based on data measured throughout 2021; thus, our population included infants whose first year of age coincided with the first year of the pandemic, depicting the deleterious effect of the pandemic on the childhood vaccination program at a national level. Therefore, our study points to the importance of an in-depth understanding of the factors associated with FVC in the Peruvian setting to implement timely interventions.
4.1. Comparison with previous studies
Nationwide, FVC was 66.19 % among infants aged 12 to 23 months in 2021, which represents a decrease of 7.97 % from 2019 (pre-pandemic era) [22]. Several studies conducted in the post-pandemic era have also revealed a marked decrease in routine vaccination coverage among infants and a slow recovery afterwards [33], [34], [35]. We did not find studies measuring FVC with national data in the post-pandemic period. Our study emerges as one of the first assessing FVC during the pandemic. Unfortunately, FVC in Peru, an upper middle-income country, in 2021 (post-pandemic era) are comparable to coverages reported in certain low-income countries in the pre-pandemic era [18], [36]. Hence, arduous efforts are needed at various levels to prevent vaccination coverage from sinking into suboptimal coverage.
Our results revealed that maternal education and ANC visits were significantly associated with FVC among Peruvian infants. Like other studies [17], [19], we found that having a mother with a higher education level was associated with a higher likelihood of FVC among infants when compared to not having any education or primary. Educational interventions that have been shown to be effective in promoting childhood vaccination would be more beneficial to women with a higher educational level [37]. FVC was also associated with attending at least one ANC visit, and its probability increased when attending more than six visits, as seen in the previous studies [18], [19].
Region of origin would play a key role in having FVC. It was observed that infants living on the rest of the coast or in the Highlands were more likely to be fully immunized in comparison to infants from Metropolitan Lima. The geographic disparities mentioned above agree with studies from other LMICs [17], [20], [38] and others from Peru [12]. Other diseases affecting infants have also shown a regional pattern of inequality countrywide [39]. On the other hand, contrary to several studies [18], [21], [38], our study found that living in rural areas was associated with a higher probability of being fully vaccinated.
We found a pro-rich distribution of FVC on ranked-wealth households, albeit of low magnitude. Likewise, several studies have elucidated a pro-rich and pro-urban inequality concerning vaccination coverage [41]. Moreover, another study revealed inequality in such coverage according to maternal educational status [42].
4.2. Explanation and plausibility of the results
The decrease in FVC could be partially explained by the detrimental effect exerted by the COVID-19 pandemic as it led to lockdowns and restrictions on freedom of movement, temporary disruptions in routine medical care delivery, and avoidance of medical care centers [10], [43]. In addition, there were significant regional differences in FVC, especially as it was higher in regions of origin other than the capital city of Peru (Lima). As foreseen, it may be related to the fragmentation and segmentation of the Peruvian healthcare system [44] and, in turn, centralization. As well, there are wide gaps in health insurance coverage [45] and access to healthcare services [46]. To the best of our knowledge, this is the first study in Peru assessing FVC and its associated factors among infants after the beginning of the pandemic period. This must be highlighted as factors related to vaccination coverage could behave differently since the origin of the pandemic.
As expected, the older the child the more chances they have of being fully vaccinated between 12 and 23 months. This direct association is explained by the fact that each month that passes, the chances of receiving more vaccines and, subsequently, of completing the vaccination schedule increase. Indeed, by the age of 24 months, most vaccines are administered in accordance with the Peruvian immunization schedule [23]. This could mean that vaccination strategies and campaigns (plus promotion and communication actions) are successful over time and greatly reduce the risk associated with under-vaccination in the first months of life.
Both the mother’s education and ANC visits would improve the vaccination status in tandem. Formal education could provide satisfactory knowledge concerning infants’ preventive health, including crucial information about immunization. We believe that highly educated women may have a better understanding during each ANC visit [47]. This finding could be explained by active health promotion through preventive care during each visit since pregnant women receive their respective scheduled immunizations. In fact, the Ministry of Health (MINSA, from the Spanish acronym) sets a minimum of six ANC visits to ensure maternal and child well-being, which, according to our results, is independently associated with FVC [48]. The Peruvian government should guarantee adequate child healthcare indirectly through strategies toward delivery-related factors.
The regional gaps in FVC could be related to multiple geographically distributed factors, as Peru is a multicultural country where various beliefs and customs can influence vaccination intention, but it could also be due to rugged geography where the presence of the health system is burdensome. A recent study reported the presence of high-risk clusters of low vaccination coverage throughout the national territory [12]. Overall, these geographic inequalities should be taken into consideration to target those regions and strengthen the vaccination strategies.
In our study, we found that infants living in rural areas were more likely to be fully vaccinated than those in urban areas, which contrasts with several studies from other LMICs [18], [21], [40]. This relationship can be explained by some factors inherent in the Peruvian context. Conditional cash transfer programs, aimed at poor people living mainly in rural areas, provide economic incentives to those families whose children have completed the vaccination schedule [49]. As well, people living in urban areas are more exposed to the media, which is nowadays a source of misinformation on vaccination, thereby generating distrust in the urban population and, consequently, boosting anti-vaccine groups [50]. All in all, this finding is in line with the coverage found in the Highlands, which is significantly higher than in other regions. Many areas of the Highlands are rural and lack mass media access. On the contrary, the Lima Metropolitan area (the capital of Peru), which is mostly urbanized and home to a third of the Peruvian population, had the lowest vaccination coverage.
FVC was more concentrated among the better-off infants in Peru, although of low magnitude. The economic support programs such as JUNTOS could contribute to the absence of major inequalities. This is a conditional cash transfer program founded by the Ministry of Economy. The Ministry of Development and Social Inclusion provides money to mothers who, among other requirements, have their infants vaccinated [49]. Conversely, as MINSA faces shortages, few of the most well-to-do families opt for acquiring vaccines privately, which may generate gaps. Considering this, joint efforts must be continued to maintain this scenario and to continue tackling inequalities.
4.3. Strengths and limitations
Our study must be interpreted considering its limitations. First, due to the cross-sectional design of our study, it was not possible to establish causality. Second, almost 10 % of the FVC information was obtained from the mothers’ reports, from which social desirability bias and recall bias may arise. However, we stratified the analysis by the source of vaccination status data and, as stated by Modi RN et al., to enhance coverage and the effect of vaccines, the mothers’ recall could be used, particularly in LMICs [51]. Third, due to the lack of a direct measurement of SES in the Peruvian DHS (such as income, expenditure, or consumption), we used an asset-based wealth index as a proxy measurement instead, which is suitable for inequality studies in the absence of a direct measure [52]. Fourth, as it was a secondary data analysis, it was not possible to include other variables that would be interesting to analyze. Fifth, our study sought to assess the factors associated to FVC amid the COVID-19 pandemic, instead of comparing vaccination coverages with the pre-pandemic period. On the other hand, our study has several strengths. It was based on a large sample size, and great statistical power was obtained. Also, the database is nationally representative. Even though the FVC definition does not include all the vaccines administered by the National Vaccination Program, such as pneumococcal and rotavirus vaccines [23], FVC is a WHO standardized definition in several studies [14], [53], which confers greater comparability to our study. Indeed, it was the most employed definition according to a scoping review on vaccination assessments with DHS data [53]. Our study is the first to address infants’ vaccination coverage countrywide after the beginning of the pandemic in Peru and could be useful as a basis to redirect health policies.
4.4. Public health implications and recommendations for future studies
It is of the utmost importance that strategies be based on scientific evidence to rationalize the existing health resources. Indeed, our article may serve as a basis to redirect the ongoing national vaccination program. It is necessary to continue providing universal access to vaccination so that it remains equitable between different socioeconomic levels. Multidisciplinary and inter-institutional efforts are needed to tackle the dramatic drop in FVC. By articulating the institutions, social programs may be boosted, and better vaccination strategies could be designed. It is not sufficient to offer a comprehensive vaccination scheme; it is vital to administer it efficiently. Besides, we encourage the implementation of quantitative and qualitative studies that assess the determinants of poor adherence to vaccination in the Peruvian context. Nonetheless, access to electronic records is limited, which hinders research. Thus, it is of paramount importance to improve the collection of primary data, which might be possible through the unification and articulation of the information sources of the MINSA.
5. Conclusion
FVC has dropped to 66,19 % among Peruvian infants aged 12 to 23 months. Infants’ age, their mothers’ education, ANC visits, region of origin, and source of vaccination data have been associated with FVC. A pro-rich inequality in FVC was found, but low in magnitude as vaccines are universal, administered free of charge, and in turn, broadly accessible. Further studies should closely monitor FVC in the upcoming years in Peru. In addition, we encourage the measurement of household incomes rather than assets in future surveys as it provides a better figure for SES.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2022.11.067.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
Data availability
Data will be made available on request.
References
- 1.D’Angiolella L.S., Lafranconi A., Cortesi P.A., Rota S., Cesana G., Mantovani L.G. Costs and effectiveness of influenza vaccination: a systematic review. Ann Ist Super Sanita. 2018;54:49–57. doi: 10.4415/ANN_18_01_10. [DOI] [PubMed] [Google Scholar]
- 2.Haider S., Chaikledkaew U., Thavorncharoensap M., Youngkong S., Islam M.A., Thakkinstian A. Systematic review and meta-analysis of cost-effectiveness of rotavirus vaccine in low-income and lower-middle-income countries. Open Forum Infect Dis. 2019:6. doi: 10.1093/OFID/OFZ117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McGovern M.E., Canning D. Vaccination and all-cause child mortality from 1985 to 2011: global evidence from the demographic and health surveys. Am J Epidemiol. 2015;182:791. doi: 10.1093/AJE/KWV125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Andre F.E., Booy R., Bock H.L., Clemens J., Datta S.K., John T.J., et al. Vaccination greatly reduces disease, disability, death and inequity worldwide. Bull World Health Organ. 2008;86:140. doi: 10.2471/BLT.07.040089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mallory M.L., Lindesmith L.C., Baric R.S. Vaccination-induced herd immunity: Successes and challenges. J Allergy Clin Immunol. 2018;142:64–66. doi: 10.1016/j.jaci.2018.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Immunization coverage 2021. Available from: https://www.who.int/news-room/fact-sheets/detail/immunization-coverage (accessed June 2, 2022).
- 7.Causey K., Fullman N., Sorensen R.J.D., Galles N.C., Zheng P., Aravkin A., et al. Estimating global and regional disruptions to routine childhood vaccine coverage during the COVID-19 pandemic in 2020: a modelling study. Lancet. 2021;398:522–534. doi: 10.1016/S0140-6736(21)01337-4/ATTACHMENT/E2A80C09-5727-4E6E-864E-1D8F7F0DDD15/MMC1.PDF. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacDonald N.E., Eskola J., Liang X., Chaudhuri M., Dube E., Gellin B., et al. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–4164. doi: 10.1016/J.VACCINE.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 9.Hungerford D., Cunliffe N.A. Coronavirus disease (COVID-19) – impact on vaccine preventable diseases. Eurosurveillance. 2020;25:2000756. doi: 10.2807/1560-7917.ES.2020.25.18.2000756/CITE/PLAINTEXT. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atamari-Anahui N., Conto-Palomino N.M., Pereira-Victorio C.J., Atamari-Anahui N., Conto-Palomino N.M., Pereira-Victorio C.J. Actividades de inmunización en el contexto de la pandemia por la COVID-19 en Latinoamérica. Rev Peru Med Exp Salud Publica. 2020;37:773–775. doi: 10.17843/rpmesp.2020.374.5758. [DOI] [PubMed] [Google Scholar]
- 11.Herrera-Añazco P., Uyen-Cateriano A., Mezones-Holguin E., Taype-Rondan A., Mayta-Tristan P., Malaga G., et al. Some lessons that Peru did not learn before the second wave of COVID-19. Int J Health Plann Manage. 2021;36:995–998. doi: 10.1002/hpm.3135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mezones-Holguin E., Al-kassab-Córdova A., Maguiña J.L., Rodriguez-Morales A.J. Vaccination coverage and preventable diseases in Peru: Reflections on the first diphtheria case in two decades during the midst of COVID-19 pandemic. Travel Med Infect Dis. 2021;40 doi: 10.1016/J.TMAID.2020.101956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.World Health Organization. Immunization Agenda 2030: A Global Strategy To Leave No One Behind. 2020. [DOI] [PubMed]
- 14.World Health Organization. Full immunization coverage among one-year-olds (%) (Health Equity Monitor) n.d. Available from: https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3317 (accessed June 2, 2022).
- 15.Colomé-Hidalgo M, Campos JD, de Miguel ÁG. Monitoring inequality changes in full immunization coverage in infants in Latin America and the Caribbean. Rev Panam Salud Pública 2020;44. doi: 10.26633/RPSP.2020.56. [DOI] [PMC free article] [PubMed]
- 16.Kawakatsu Y., Honda S. Individual-, family- and community-level determinants of full vaccination coverage among children aged 12–23 months in western Kenya. Vaccine. 2012;30:7588–7593. doi: 10.1016/J.VACCINE.2012.10.037. [DOI] [PubMed] [Google Scholar]
- 17.Kibreab F, Lewycka S, Tewelde A. Impact of mother’s education on full immunization of children aged 12-23 months in Eritrea: population and health survey 2010 data analysis. BMC Public Health 2020;20. doi: 10.1186/S12889-020-8281-0. [DOI] [PMC free article] [PubMed]
- 18.Biset G., Woday A., Mihret S., Tsihay M. Full immunization coverage and associated factors among children age 12–23 months in Ethiopia: systematic review and meta-analysis of observational studies. Hum Vaccin Immunother. 2021;17:2326–2335. doi: 10.1080/21645515.2020.1870392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Afolabi R.F., Salawu M.M., Gbadebo B.M., Salawu A.T., Fagbamigbe A.F., Adebowale A.S. Ethnicity as a cultural factor influencing complete vaccination among children aged 12–23 months in Nigeria. Hum Vaccin Immunother. 2021;17:2008–2017. doi: 10.1080/21645515.2020.1870394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moran E.B., Wagner A.L., Asiedu-Bekoe F., Abdul-Karim A., Schroeder L.F., Boulton M.L. Socioeconomic characteristics associated with the introduction of new vaccines and full childhood vaccination in Ghana, 2014. Vaccine. 2020;38:2937–2942. doi: 10.1016/J.VACCINE.2020.02.065. [DOI] [PubMed] [Google Scholar]
- 21.Budu E., Seidu A.A., Agbaglo E., Armah-Ansah E.K., Dickson K.S., Hormenu T., et al. Maternal healthcare utilization and full immunization coverage among 12–23 months children in Benin: a cross sectional study using population-based data. Arch Public Health. 2021:79. doi: 10.1186/S13690-021-00554-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Al-kassab-Córdova A., Silva-Perez C., Maguiña J.L. Spatial distribution, determinants and trends of full vaccination coverage in children aged 12–59 months in Peru: a subanalysis of the Peruvian Demographic and Health Survey. BMJ Open. 2022;12(11):e05211. doi: 10.1136/bmjopen-2021-050211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ministerio de Salud. Norma técnica que establece el Esquema Nacional de Vacunación. Lima: 2018.
- 24.INEI. Informe Principal de la Encuesta Demográfica y de Salud Familiar - ENDES 2021. Lima: 2022.
- 25.Rutstein SO, Johnson K. The DHS wealth index . DHS Comparative Reports. No. 6. Calverton: 2004.
- 26.Guerrero-Díaz D.V., Hernández-Vásquez A., Montoya-Rivera W.C., Rojas-Roque C., Chacón Díaz M.A., Bendezu-Quispe G. Undiagnosed hypertension in Peru: analysis of associated factors and socioeconomic inequalities, 2019. Heliyon. 2021;7:e07516. doi: 10.1016/j.heliyon.2021.e07516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shifti D.M., Chojenta C., Holliday E.G., Loxton D. Socioeconomic inequality in short birth interval in Ethiopia: a decomposition analysis. BMC Public Health. 2020;20:1504. doi: 10.1186/s12889-020-09537-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jann B. Estimating Lorenz and concentration curves. Stata J. 2016;16:837–866. doi: 10.1177/1536867X1601600403. [DOI] [Google Scholar]
- 29.O’Donnell O., O’Neill S., Van Ourti T., Walsh B. conindex: Estimation of concentration indices. Stata J. 2016;16:112–138. doi: 10.1177/1536867X1601600112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Erreygers G. Correcting the concentration index. J Health Econ. 2009;28:504–515. doi: 10.1016/J.JHEALECO.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 31.Erreygers G., Van Ourti T. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: A recipe for good practice. J Health Econ. 2011;30:685–694. doi: 10.1016/J.JHEALECO.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.INEI. ENCUESTA DEMOGRÁFICA Y DE SALUD FAMILIAR - ENDES 2021. Microdatos 2021. Available from: http://iinei.inei.gob.pe/microdatos/.
- 33.Silveira M.M., Conrad N.L., Leivas Leite F.P. Effect of COVID-19 on vaccination coverage in Brazil. J Med Microbiol. 2021;70 doi: 10.1099/JMM.0.001466/CITE/REFWORKS. [DOI] [PubMed] [Google Scholar]
- 34.Ji C., Piché-Renaud P.P., Apajee J., Stephenson E., Forte M., Friedman J.N., et al. Impact of the COVID-19 pandemic on routine immunization coverage in children under 2 years old in Ontario, Canada: a retrospective cohort study. Vaccine. 2022;40:1790–1798. doi: 10.1016/J.VACCINE.2022.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.SeyedAlinaghi SA, Karimi A, Mojdeganlou H, Alilou S, Mirghaderi SP, Noori T, et al. Impact of COVID‐19 pandemic on routine vaccination coverage of children and adolescents: A systematic review. Heal Sci Rep 2022;5. doi: 10.1002/HSR2.516. [DOI] [PMC free article] [PubMed] [Retracted]
- 36.Tesema G.A., Tessema Z.T., Tamirat K.S., Teshale A.B. Complete basic childhood vaccination and associated factors among children aged 12–23 months in East Africa: a multilevel analysis of recent demographic and health surveys. BMC Public Health. 2020;20:1837. doi: 10.1186/s12889-020-09965-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saeterdal I., Lewin S., Austvoll-Dahlgren A., Glenton C., Munabi-Babigumira S. Interventions aimed at communities to inform and/or educate about early childhood vaccination. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD010232.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Clouston S., Kidman R., Palermo T. Social inequalities in vaccination uptake among children aged 0–59 months living in Madagascar: an analysis of Demographic and Health Survey data from 2008 to 2009. Vaccine. 2014;32:3533–3539. doi: 10.1016/J.VACCINE.2014.04.030. [DOI] [PubMed] [Google Scholar]
- 39.Al-Kassab-Córdova A., Mendez-Guerra C., Quevedo-Ramirez A., Espinoza R., Enriquez-Vera D., Robles-Valcarcel P. Rural and urban disparities in anemia among Peruvian children aged 6–59 months: a multivariate decomposition and spatial analysis. Rural Remote Health. 2022;22(6936) doi: 10.22605/RRH6936. [DOI] [PubMed] [Google Scholar]
- 40.Debie A., Lakew A.M., Tamirat K.S., Amare G., Tesema G.A. Complete vaccination service utilization inequalities among children aged 12–23 months in Ethiopia: a multivariate decomposition analyses. Int J Equity Health. 2020;19:65. doi: 10.1186/s12939-020-01166-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Restrepo-Méndez M.C., Barros A.J.D., Wong K.L.M., Johnson H.L., Pariyo G., França G.V.A., et al. Inequalities in full immunization coverage: trends in low-and middle-income countries. Bull World Health Organ. 2016;94:794–805A. doi: 10.2471/BLT.15.162172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Acharya K., Paudel Y.R., Dharel D. The trend of full vaccination coverage in infants and inequalities by wealth quintile and maternal education: analysis from four recent demographic and health surveys in Nepal. BMC Public Health. 2019;19:1673. doi: 10.1186/s12889-019-7995-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, Thierry JM, et al. Delay or Avoidance of Medical Care Because of COVID-19–Related Concerns — United States, June 2020. MMWR Morb Mortal Wkly Rep 2022;69:1250–7. doi: 10.15585/MMWR.MM6936A4. [DOI] [PMC free article] [PubMed]
- 44.Sanchez-Moreno F. The national health system in Peru. Rev Peru Med Exp Salud Publica. 2014;31:747–753. doi: 10.17843/rpmesp.2014.314.129. [DOI] [PubMed] [Google Scholar]
- 45.Mezones-Holguín E., Amaya E., Bellido-Boza L., Mougenot B., Murillo J.P., Villegas-Ortega J., et al. Health insurance coverage: the peruvian case since the universal insurance act. Rev Peru Med Exp Salud Publica. 2019;36:196–206. doi: 10.17843/rpmesp.2019.362.3998. [DOI] [PubMed] [Google Scholar]
- 46.Mezones-Holguín E., Solis-Cóndor R., Benites-Zapata V.A., Garnica-Pinazo G., Marquez-Bobadilla E., Tantaleán-Del-Águila M., et al. Institutional differences in the ineffective access to prescription medication in health care centers in Peru: analysis of the National Survey on User Satisfaction of Health Services (ENSUSALUD 2014) Rev Peru Med Exp Salud Publica. 2016;33:205–214. doi: 10.17843/rpmesp.2016.332.2197. [DOI] [PubMed] [Google Scholar]
- 47.Miller L.C., Joshi N., Lohani M., Rogers B., Mahato S., Ghosh S., et al. Women’s education level amplifies the effects of a livelihoods-based intervention on household wealth, child diet, and child growth in rural Nepal. Int J Equity Health. 2017;16:183. doi: 10.1186/s12939-017-0681-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ministerio de Salud Norma técnica de salud para la atención integral de salud materna. Lima. 2013 [Google Scholar]
- 49.Ministerio de Desarrollo e Inclusión Social. Programa Nacional de Apoyo Directo a los más Pobres - JUNTOS 2022. Available from: https://www.gob.pe/juntos.
- 50.Germani F., Biller-Andorno N. The anti-vaccination infodemic on social media: a behavioral analysis. PLoS One. 2021;16:e0247642. doi: 10.1371/journal.pone.0247642. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 51.Modi R.N., King C., Bar-Zeev N., Colbourn T. Caregiver recall in childhood vaccination surveys: systematic review of recall quality and use in low- and middle-income settings. Vaccine. 2018;36:4161–4170. doi: 10.1016/j.vaccine.2018.05.089. [DOI] [PubMed] [Google Scholar]
- 52.McKenzie D.J. Measuring inequality with asset indicators. J Popul Econ. 2005;18:229–260. doi: 10.1007/S00148-005-0224-7. [DOI] [Google Scholar]
- 53.Shenton L.M., Wagner A.L., Ji M., Carlson B.F., Boulton M.L. Vaccination assessments using the Demographic and Health Survey, 2005–2018: a scoping review. BMJ Open. 2020;10:e039693. doi: 10.1136/bmjopen-2020-039693. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data will be made available on request.