Abstract
Heart failure (HF) is a long‐term clinical syndrome, with increasing prevalence and considerable healthcare costs that are further expected to increase dramatically. Despite significant advances in therapy and prevention, mortality and morbidity remain high and quality of life poor. Epidemiological data, that is, prevalence, incidence, mortality, and morbidity, show geographical variations across the European countries, depending on differences in aetiology, clinical characteristics, and treatment. However, data on the prevalence of the disease are scarce, as are those on quality of life. For these reasons, the ESC‐HFA has developed a position paper to comprehensively assess our understanding of the burden of HF in Europe, in order to guide future policies for this syndrome. This manuscript will discuss the available epidemiological data on HF prevalence, outcomes, and human costs—in terms of quality of life—in European countries.
Keywords: Heart failure, Impact, Epidemiology, Prognosis, Mortality, Morbidity, Quality of life
Introduction
Heart failure (HF) is a long‐term condition, affecting around 63 million people worldwide, 1 , 2 with increasing prevalence that mirrors the ageing of the population. 3 , 4 HF represents the end stage of various heart diseases, including specific and ill‐defined cardiomyopathies, ischaemic heart disease, and heart valve disease. 5 Importantly, almost all HF patients also have several comorbid conditions [diabetes mellitus (DM), arterial hypertension, chronic kidney disease, chronic obstructive pulmonary disease, iron deficiency, etc.], which further complicate their treatment and negatively impact prognosis.
Worldwide, 5 year mortality rates in patients with chronic advanced HF are >50%. 6 , 7 , 8 Thus, despite improvements in therapy, changes in lifestyle, and better adherence to guidelines, 9 HF mortality and morbidity—especially in high‐risk subgroups—remain high and quality of life (QOL) remains poor. 8 , 10 Consequently, health‐related expenditures are considerable and are expected to increase dramatically in the near future. 11 , 12
Because epidemiological data on HF are not uniform or readily available across European countries, the aim of this position paper of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC) is to provide an impact analysis of HF in terms of prevalence/incidence, outcomes, and QOL. Data on HF healthcare costs will be specifically discussed in an upcoming ESC position paper.
European epidemiological data on heart failure
Prevalence and incidence
Prevalence, incidence, mortality, and morbidity of HF have been reported to vary across the European countries shown in Figure 1 . 8 For the other countries (e.g. France, Austria, Norway, Switzerland, Portugal, Ireland, and Bosnia and Herzegovina), there is a lack of reliable epidemiological data, and this noteworthy gap of knowledge should be filled in upcoming research.
Figure 1.
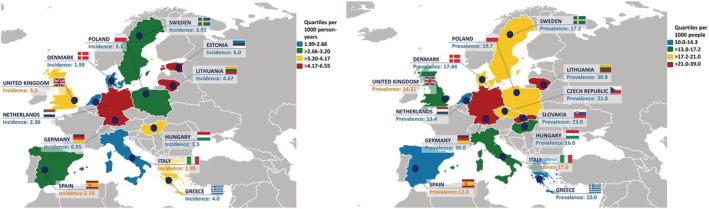
Incidence of heart failure per 1000 person‐years (left) and prevalence of heart failure per 1000 persons (right). Adapted from Seferović et al. 13
Data from the HFA Atlas showed an overall HF prevalence of 17 [inter‐quartile range (IQR), 14–21] cases per 1000 people, ranging from 10 to 14 per 1000 in Spain and the Netherlands, from 14 to 17 in Italy, Hungary, and the UK, from 17 to 21 in Sweden, Denmark, Poland, and Czech Republic, and from 21 to 39 in Slovenia, Lithuania, and Germany. 13 These data highlight considerable heterogeneity across these countries, in line with previous reports, 7 likely representing true differences in prevalence as well as differences in reporting. A recent systematic analysis of the epidemiological burden of HF in 195 countries, from 1990 to 2017, found that most countries in Central Europe had relatively high prevalence rates of HF in 2017 {Hungary: 12 [95% confidence interval (CI) 10–14]; Montenegro: 12 (95% CI 10–14); Slovakia: 12 (95% CI 10–13); Slovenia: 12 (95% CI 10–13); and Czech Republic: 11 (95% CI 10–13) per 1000 people}. 14 On the other hand, the lowest age‐standardized prevalence rate in Europe was observed in an Eastern European country [Latvia: 5 (95% CI 4–6) per 1000 people] in 2017. The countries with greater decreases in age‐adjusted prevalence in HF over time were Portugal [−38% (95% CI −42 to −33)] and Denmark [−37% (95% CI −41 to −33)]. 14 Previous data in Portugal, from the EPidemiologia da Insuficiencia Cardiaca e Aprendizagem (Epidemiology of Heart Failure and Learning—EPICA) study, 15 indicated an increased HF prevalence with ageing, that is, from 1.4% in patients 25–49 years old to 16% in patients >80 years old. In a German study, 16 the prevalence was 1.6% in women and 1.8% in men, with rates increasing with the ageing of the population as well. In a Swedish study, 17 prevalence was stable over the years with similar rates in men and women (2.2%), while a decrease in incidence and mortality was observed. An Italian survey 18 reported a prevalence of 1.4%, with rates increasing with older age. Data from the ESC Atlas of Cardiology, 19 published in 2018, further demonstrated a striking variability across 41 European countries in terms of risk factors, incidence, and mortality for cardiovascular diseases.
Also, whereas an increase in HF prevalence has been consistently observed, HF incidence has been reported to be stable or even decreasing, especially in women. 20 , 21 The decrease in incidence may be explained by factors such as reduced severity and better treatment of acute coronary syndrome (ACS). 8 Additionally, incidence data vary across left ventricular ejection fraction (EF) spectrum. A community‐based study in Spain 22 reported a reduction in the incidence of HF with reduced EF (HFrEF) over time but a parallel increase in the incidence of HF with preserved EF (HFpEF) and HF with mid‐range EF (HFmrEF). Still, the incidence of HFrEF surpassed the one of HFpEF by 0.24 cases per 1000 person‐years. There were 0.32 more HFrEF cases per 1000 people per year in men, whereas for HFpEF, there were 0.17 cases per 1000 people per year more in women. 22 Specifically, when observing the trends over time, in 2007, the rise in the overall incidence of HF plateaued, with HFrEF rates starting to slowly decrease in 2005 while the ones for HFpEF were still increasing. 22 A recent Spanish population‐based study 23 confirmed this trend. From 2017 to 2019, distribution by phenotype of left ventricular EF was as follows: 51.7% HFrEF, 40.2% HFpEF, and 8.1% HFmrEF. In 2019, the prevalence was 1.89% (95% CI 1.70–2.08), with an incidence rate of 2.78 new cases per 1000 persons per year. 23
However, with the expected demographic changes, particularly the marked ageing of the population, a larger number of the population will likely be affected by this syndrome. For instance, in Portugal, the prevalence of HF is expected to increase by 30% by 2035 and by 33% by 2060, compared with 2011. 24 Considering only population ageing over a 22 year horizon from 2014, the deaths and burden of HF in Portugal are expected to increase by 73.0% and 27.9%, respectively. 25
Of note, it should be considered that heart damage arising from COVID‐19 infection is likely to influence the incidence of HF since 2020, leading to a further increase in HF cases. 26 As pointed out by the Heart Failure Policy Network (https://www.hfpolicynetwork.org/), the COVID‐19 pandemic has led to reduced care for HF, 27 and—at the same time—has created a significant rise in demand for HF services, driven by new cases of HF or deterioration in those previously diagnosed, with a considerable burden for healthcare systems in Europe. 28 , 29 Specifically, there is also the risk of under‐diagnoses and under‐treatment in several cardiovascular pathways, 30 , 31 possibly leading to increase the incidence and severity of HF in the future.
Mortality and hospitalizations
Patients with HF still have an unfavourable prognosis with an estimated in‐hospital mortality of 2–17%. 32 , 33 In terms of disability‐adjusted lifespan, it is estimated that a patient with HF lives on average 1.1–2.3 years shorter because of premature death or disability. 34 Mortality rises dramatically with ageing, with rates increasing more than four‐fold from age 25–54 to age ≥85, regardless of gender. 35 HF is common in the elderly due to the complex interplay of the cardiovascular ageing process with risk factors, comorbidities, and disease modifiers. 36
Outcomes also differ across HF phenotypes and in acute/chronic HF. In the Swedish Heart Failure Registry (SwedeHF), 37 the adjusted risk of mortality at 3 years was 20% higher in HFrEF vs. HFpEF, whereas HFmrEF and HFpEF had a similar prognosis (Figure 2 ). However, 3 year mortality was higher in HFmrEF than in HFpEF by 11% in the presence of coronary artery disease. The EuroHeart Failure Survey 38 compared prognosis in 3148 patients with HFpEF vs. 3658 with HFrEF and reported higher 90 day mortality in those with HFrEF (12%) compared with HFpEF (10%), but similar readmission rates (21% vs. 22%, respectively). In the EuroHeart Failure Survey II, which enrolled 3580 patients hospitalized for HF, in‐hospital mortality was 6.4%. 39 , 40 In the European Society of Cardiology Heart Failure Long‐Term (ESC‐HF‐LT) registry 41 enrolling 12 440 patients with acute and chronic HF, 1 year all‐cause mortality rates ranged from 22% to 37% for acute HF (AHF) and from 7% to 16% for chronic HF across 21 European and/or Mediterranean countries. The rates for the combined endpoint of mortality or HF hospitalization within 1 year were 36% for AHF and 15% for chronic HF. A subsequent analysis of the ESC‐HF‐LT registry 42 reported that mortality rates at 1 year differed significantly between HFrEF and HFpEF (9% vs. 6%), with HFmrEF patients showing in‐between rates (8%), but overall more similar to HFrEF.
Figure 2.
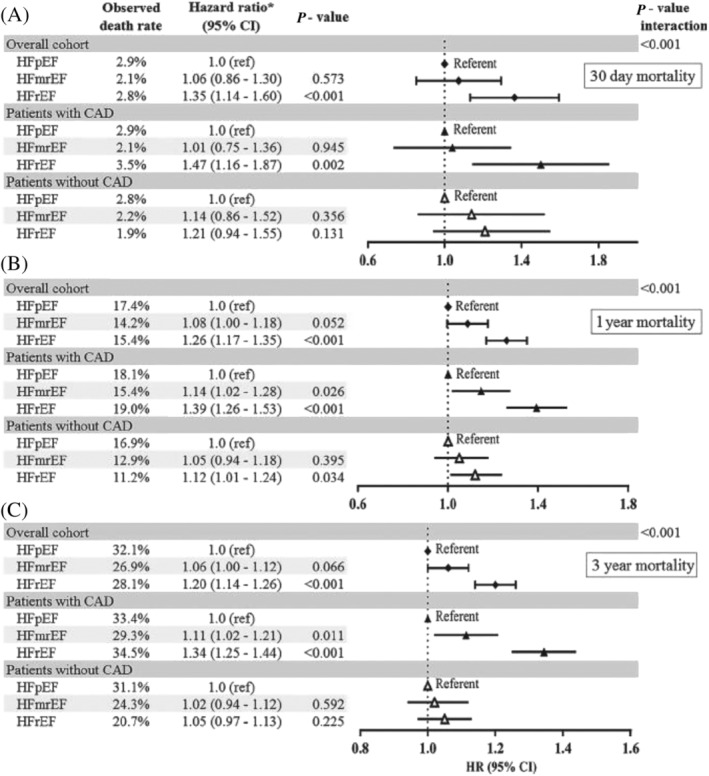
Hazard ratios (HRs) for heart failure with mid‐range ejection fraction (HFmrEF) vs. heart failure with preserved ejection fraction (HFpEF) and heart failure with reduced ejection fraction (HFrEF) vs. HFpEF for all‐cause mortality up to 30 days (A), 1 year (B), and 3 years (C) for the overall cohort and for patients with and without coronary artery disease (CAD) separately. CI, confidence interval. *Adjusted for index year, age, gender, heart rate, estimated glomerular filtration rate, systolic blood pressure, diabetes, CAD, atrial fibrillation, valve disease, lung disease, anaemia, use of angiotensin‐converting enzyme inhibitor or angiotensin receptor blocker, beta‐blocker, diuretic, statin, registration type, living arrangement, and education. From Koh et al. 37
Hospitalizations due to HF represent 1–2% of all admissions, 1 and therefore, costs of HF are mainly driven by hospitalization. 43 After the initial diagnosis, HF patients are hospitalized on average about once a year due to the HF worsening. 44 Of note, HF hospitalization is associated with high 30 day readmission rate, up to 25%. 1 The reasons for readmissions are often related to incomplete decongestion, warranting better implementation of HF care pathways, as well as to other conditions (e.g. DM, chronic obstructive pulmonary disease, and chronic kidney disease), 45 mirroring the high burden of comorbidities in HF. 44
The HFA Atlas showed that the median number of HF hospitalizations in Europe was 2671 (IQR, 1771–4317) per million people annually, ranging from <1000 in Latvia and North Macedonia to >6000 in Romania, Germany, and Norway. 13 The median length of hospital stay for an admission with HF was 8.50 (IQR, 7.38–10) days with considerable variation between European countries (Figure 3 ). Consistently, diagnostic and management resources for HF varied as well, with high‐income ESC member countries having substantially more resources compared with middle‐income countries. These data therefore indicated a great variability in the resources available for HF management and quality of care across ESC member countries. 13
Figure 3.
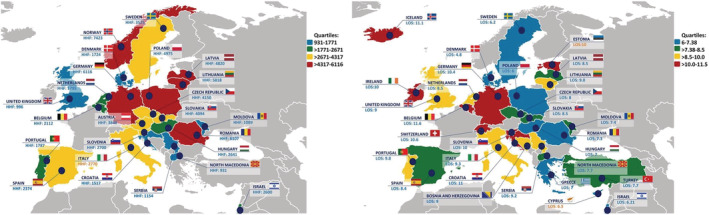
Number of heart failure‐related hospital discharges per million people (left) and average length of stay in hospital primarily due to heart failure (right). Adapted from Seferović et al. 13
Impact of acute heart failure: insights from the European Society of Cardiology Heart Failure Long‐Term registry
Acute HF is a prevalent condition and is the leading cause of hospitalization, especially in individuals aged 65 years or older. 46 , 47 AHF outcome data from the ESC registries are shown in Supporting Information, Figure S1 .
The European Society of Cardiology Heart Failure Long‐Term registry is one of the primary sources of real‐world data on AHF in Europe and baseline characteristics, classifications, management, and outcomes of AHF patients were described by three successive analyses. 41 , 48 , 49 AHF patients enrolled in the ESC‐HF‐LT registry had a mean age of 70 years and were predominantly male (61%), 33% had NYHA IV class, and according to the different classifications used, AHF patients presented most commonly as ‘decompensated HF’ (or ‘wet and warm’) (70%). Clinical phenotypes and classifications of patients hospitalized for AHF are shown in Figure 4 . 48
Figure 4.
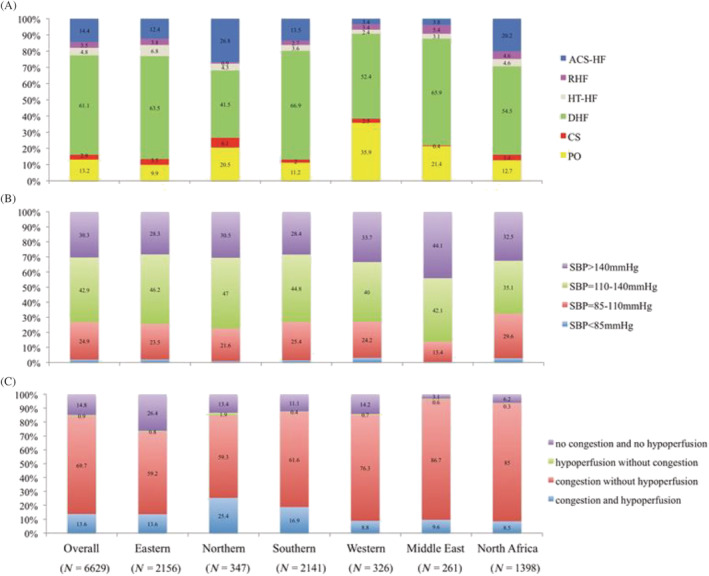
Classification of acute heart failure patients by geographical area (ESC‐HF‐LT registry). (A) Clinical profile classification by geographical area. (B) Systolic blood pressure (SBP) classification by geographical area. (C) Congestion/hypoperfusion classification by geographical area. ACS‐HF, acute heart failure and associated acute coronary syndrome; CS, cardiogenic shock; DHF, decompensated heart failure; HT‐HF, hypertensive heart failure; PO, pulmonary oedema; RHF, right heart failure. Eastern Europe = Bulgaria, Czech Republic, Hungary, Poland, Romania, Russian Federation, Slovakia, and Republics of Belarus, Moldova, and Ukraine. Northern Europe = UK, Sweden, Denmark, Finland, Norway, Ireland, Lithuania, Latvia, Estonia, Iceland, Channel Islands, Isle of Man, and Faeroe Islands. Southern Europe = Italy, Spain, Greece, Portugal, Serbia, Croatia, Bosnia and Herzegovina, Albania, North Macedonia, Slovenia, Montenegro, Malta, Andorra, Gibraltar, San Marino, and Holy See. Western Europe = Germany, France, the Netherlands, Belgium, Austria, Switzerland, Luxembourg, Monaco, and Liechtenstein. From Chioncel et al. 48
Cardiac and non‐cardiac comorbidities are extremely prevalent among chronic and acute patients globally. In AHF, the ESC‐HF‐LT registry showed that more than one‐half of all patients (56%) had known ischaemic heart disease, which was complicated by myocardial infarction in 20–30% of cases. In addition, approximately 70% and 40% of AHF patients, respectively, had a history of hypertension and atrial fibrillation. Non‐cardiac comorbidities including DM (39%), chronic kidney disease (26%), and chronic obstructive pulmonary disease (21%) were also very common. 48 , 49 These conditions not only impact the pathophysiological progression of HF but also limit the initiation and titration of evidence‐based drug and diuretic therapy, leading to increased risk of hospitalization and a large impact on healthcare systems expenditures. 50 In particular, iron deficiency is one of the most common comorbidities in patients with HF, occurring in around 35–55% of patients with chronic HF and reaching up to 70–80% in those with AHF. 51 , 52 The expert of the board chose to focus on the most widely recommended disease‐modifying treatment for AHF, ferric carboxymaltose (FCM). In the AFFIRM‐AHF trial, intravenous therapy with FCM as compared with placebo reduced the risk of recurrent hospitalizations for HF 53 and improved QOL 54 in iron‐deficient patients with left ventricular EF < 50%, stabilized after an episode of AHF. In the pharmacoeconomic analysis, FCM was compared with placebo using data from the AFFIRM‐AHF trial from the Italian, UK, US, and Swiss payer perspectives. 55 Treatment with FCM was dominant (cost saving with additional health gains) in the UK, USA, and Switzerland and highly cost‐effective in Italy. Results were driven by reduced costs for HHF events combined with quality‐adjusted life year gains attributable to increased time in higher Kansas City Cardiomyopathy Questionnaire (KCCQ) states (representing better functional outcomes). 55
The type and proportions of vasoactive medications were similar to those reported by other contemporary registries, except for use of intravenous inotropes, which was lower. 56 , 57 It is also noteworthy that the vast majority of AHF patients did not receive any procedural interventions during their hospital stay. 41 , 49 , 58 Although ischaemic heart disease is by far the most common aetiology of AHF and many patients present with ACS, coronary angiography and PCI and CABG were performed only in 21% and 10%, respectively, of AHF patients. 41 , 49 , 57 Furthermore, even in patients classified as ACS‐HF, coronary angiography and PCI or CABG were performed in 46% and 34%, respectively, 48 suggesting large variations in available facilities, as well as variations in guideline adherence across the participating centres. 47 , 58
Despite predefined inclusion/exclusion criteria, there were major regional differences in the severity and particularly the outcomes of AHF patients enrolled in ESC‐HF‐LT registry. Overall, in‐hospital mortality was 5.5%, 41 , 49 , 58 and substantial variations were found when patients were stratified by clinical profile 48 or the congestion/hypoperfusion classification scheme 49 at admission. Patients with cardiogenic shock reported the highest in‐hospital mortality rate with 50% of the deaths occurred in the first day of admission, 48 suggesting that the early identification of hypoperfusion signs, as well as appropriateness of initial therapies, is critical in this setting. 59 Early recognition of hypoperfusion signs (‘pre‐shock’), even in the absence of hypotension, may help to identify in an appropriate therapeutic window the ‘high‐risk’ patients who will develop cardiac shock and require mechanical circulatory assistance or specific organ function support. 59
In terms of 1 year outcomes, 27% of AHF patients died within 1 year, 26% were readmitted because of HF, and 44% of patients died or were readmitted within 1 year following discharge. 41 , 48 , 49 Notably, the incidence of 1 year all‐cause hospitalization was very high (45%) and did not change at 4 years. 41 , 48 , 49 Substantial between‐region differences in 1 year outcome rates were reported in the registries, with a large North to South gradient, which may be partially explained by the significant differences in HF management organization across ESC countries, different criteria for AHF admission, and differences in cultural perceptions of severity among participating countries. 47
Update on diabetes and heart failure in registry‐based analyses in Sweden and other Nordic countries
The experts of the board chose to focus on DM as it is a main comorbidity of HF, affecting up to 40% of HF population, with prevalence markedly increasing. HF registries can report on the unmet need in HF according to the different EF categories, that is, HFrEF, HFmrEF, and HFpEF. They are keys to collecting important prognostic data and to phenotyping HF. Registries can also more specifically address implementation of HF therapy. As an indication of the present document, we suggest that implementation can be assessed as follows: (i) describe use of HF interventions; (ii) assess indications for HF interventions; (iii) investigate independent reasons for non‐use of evidence‐based HF interventions; and (iv) conduct registry‐based randomized controlled clinical trials (RCTs) on a registry platform to assess efficacy in the real‐world setting and thus have a platform for rapid implementation of the trial findings in daily clinical practice.
The SwedeHF 37 is one of the largest and most representative HF registries with approximately 120 000 patients, 23% with HFpEF, 21% with HFmrEF, and 56% with HFrEF. The prevalence of type 2 DM (T2DM) in SwedeHF ranged from 24% to 25% based on the inclusion criteria of the analyses, which was similar across the EF spectrum. 60 , 61 T2DM was associated with higher mortality regardless of EF, but the magnitude of the association was higher in HFrEF and HFmrEF vs. HFpEF, which might highlight the importance of preventing myocardial damage in diabetes patients. Diabetes‐associated risk of HF hospitalization was instead similar across the EF spectrum. 61 The most common risk factors in diabetic patients were ischaemic heart disease and hypertension, which can be the target of preventive strategies. Ischaemic heart disease was present in >60% of all diabetic patients, and only 10% had none of the reported comorbidities.
Based on other contemporary national registries from Sweden, the incidence of HF is two‐fold higher in patients with vs. without diabetes. 62 An analysis of the Swedish national quality diabetes registry showed that if HbA1c, blood pressure, LDL cholesterol, microalbuminuria, and smoking were well controlled, the risk of myocardial infarction and mortality was similar in patients with vs. without diabetes, but the risk of HF was still increased in the first vs. the latter. 63 These data, together with evidence from a subsequent analysis of the SWEDEHEART registry 64 that showed that HF represents the most severe and common complication after myocardial infarction in diabetic patients, highlight the still unmet need for strategies to prevent HF and increase its awareness. 65
Primary preventive strategies in patients with diabetes are currently tested in Sweden by a registry‐based RCT, the SMARTEST trial (NCT03982381), where patients with diabetes but no cardiovascular disease are randomized within the Swedish national quality diabetes registry to metformin vs. the sodium–glucose cotransporter‐2 inhibitor (SGLT2i) dapagliflozin and the endpoints are collected in the national patient registry and the causes of death registry.
Impact of heart failure on quality of life in European countries
It is well recognized that patients with HF have impaired QOL, which declines as the disease becomes more severe. Indeed, patients with advanced HF have a symptom burden and QOL that is worse than many chronic conditions including cancer or chronic pulmonary disease. 10
The multicentre CHARM trial (Candesartan in Heart Failure: Assessment of Reduction in Mortality and Morbidity) 66 found that QOL was impaired, regardless of whether the patient had reduced or preserved EF. This was confirmed by other European studies. 67 , 68 A number of factors are associated with poor QOL, such as comorbidities, female sex, and increased body mass index, which have more recently been associated with HFpEF. 39 , 69 Further evidence from a UK study 70 on 179 patients found that those with poor QOL were younger and had a higher NYHA class and lower socio‐economic status including a lack of social support in the form of informal carers. More starkly, these patients also had an increased risk of hospital admissions and death. Furthermore, depression, higher comorbidity level, and low social support are found to be related to poor QOL in patients with HF. 71
These data highlight the urgent need for optimal multidisciplinary HF management, including optimal medication and device treatment, patient education, and self‐care support, 72 to improve QOL in this vulnerable population. 9 , 73 , 74 , 75 Relatively new therapies, such as sacubitril/valsartan, and the SGLT2i drugs dapagliflozin and empagliflozin have demonstrated notable improvements in patients' QOL 58 , 76 , 77 as have implanted device therapies (e.g. cardiac resynchronization therapy and ventricular assist devices). 78 , 79
However, QOL is often not routinely assessed within daily practice in cardiovascular patients. 80 We live in an ageing society, where the majority of patients with HF live with at least one other comorbidity such as kidney disease, physical deconditioning, chronic obstructive pulmonary disease, or DM, which also significantly impacts QOL. 81 As such, the contribution of HF to QOL is not always easy to assess. 81 Tools to measure QOL such as the KCCQ, European QoL‐5 Dimensions, or Minnesota Living with Heart Failure Questionnaire should be common place within all HF trials and integrated more readily to inform clinical practice. It has recently been shown that changes in patient assessed QOL by, for example, the KCCQ score better predicts future risk than does physician assessed NYHA classification of HF severity. 82 As an indication from the present document, as also suggested by the US Food and Drug Administration, the KCCQ is recommended as a performance measure for quantifying QOL in HF patients, being strongly associated with clinical events over time.
Finally, there is evidence that medication adherence interventions improve QOL, HF mortality, and readmission rates. 83 For all these reasons, several outcome measure initiatives have been implemented, such as Get With The Guidelines 84 and International Consortium for Health Outcomes Measurement. 85 Their value is to facilitate international comparison in HF care, using standardized parameters and meaningful patient‐centred outcomes for research and quality of care assessments.
Data from randomized controlled clinical trials vs. real‐world data
Country‐based differences in HF epidemiology across Europe might be explained by different HF aetiologies, phenotypes, patients' characteristics, and data sources considered for calculations. Another methodological explanation relates to the scientific literature on HF, which generally reports epidemiological data from patients recruited into RCTs, or included in specialty registries conducted by dedicated cardiologists. Less frequently, information is derived from administrative data or electronic health records (EHRs) (i.e. real‐world data), which potentially involves the totality of the population of patients with HF but lacks important granularity, such as EF and other characteristics. 86 In general, patients included in RCTs have less severe HF and especially less comorbidity compared with those enrolled in observational studies, because of specific eligibility criteria for the trial that reduce competing risks and the fact that the patients are attending highly selected and hence non‐representative cardiology centres. On the other hand, HFrEF patients included in the latest RCT have remarkably implantation rates of ICD, although they have been recommended by guidelines. Patients followed by cardiologists are generally younger, more frequently of the male sex, with fewer extra‐cardiac comorbidities. 58 A systematic review, 87 pooling data on 105 studies in general practice (a total of 196 105 HF patients), revealed that the most common phenotype of patients followed by general practitioners are older women with hypertension. On the contrary, the evaluation of the HF patient clinical profiles derived from EHRs includes all type of patients, without exclusion criteria and followed by all types of health professionals dealing with this clinical condition. 86 As a consequence, the mean age of these patients is higher, extra‐cardiac comorbidities are more frequent, and the outcome is generally more severe than that described in RCTs or specialty registries. 85 Although this topic is not specific for HF but can regard every disease, RCTs and specialty registries provide a larger number of clinical variables and with better quality than data from EHRs, which may not define appropriately the severity of the disease. Our indication from the present document is that real‐world data from EHRs should be preferred as the most realistic source of information regarding the total burden of HF.
Conclusions
The present document presents data on prevalence/incidence, outcomes, and QOL in many European countries. Indications are shown in Table 1 . The term ‘Europe’ used throughout the manuscript is for illustrative purposes only. Our conclusions cannot be generalized beyond the precise countries we have summarized.
Table 1.
Indications from the experts of the board
| Epidemiological studies in France, Austria, Norway, Switzerland, Portugal, Ireland, and Bosnia and Herzegovina are warranted because of paucity of data. |
| There is the need to develop common strategies to assess the burden of HF in Europe, to overcome differences in data collection and analysis. |
| Real‐world data from EHRs should be preferred as the most realistic source of information regarding the total burden of HF. |
| Assessment of quality of life is pivotal in HF patients, and the KCCQ is the recommended instrument to this aim. |
| It is advisable to conduct registry‐based RCTs on a registry platform to assess efficacy of HF therapy in the real‐world setting. |
| Upcoming HFA‐ESC projects (e.g. second edition on HFA Atlas) are to be developed to improve HF management and outcomes. |
EHRs, electronic health records; ESC, European Society of Cardiology; HF, heart failure; HFA, Heart Failure Association; KCCQ, Kansas City Cardiomyopathy Questionnaire; RCTs, randomized controlled clinical trials.
Heart failure represents a major global health problem in Europe and worldwide, leading to heavy economic costs, frequent hospitalizations, and high mortality. 88 There is the need to conduct epidemiological studies in France, Austria, Norway, Switzerland, Portugal, Ireland, and Bosnia and Herzegovina. Epidemiological data suggest that HF prevalence is going to rise further, which will lead to an additional increase in hospitalization rates and, consequently, in healthcare costs. The prognosis for HF patients has remained alarmingly poor over the last two decades despite the advances in medical and device therapies in particular for HFrEF. Differences in data collection and analysis might contribute to explain some of the geographical variations in epidemiological data, which highlights the need to develop common strategies to assess the burden of HF in Europe. For all these reasons, this document calls to action on flagship projects of the HFA of the ESC, such as second edition on HFA Atlas, registries, and others.
Conflict of interest
None declared.
Supporting information
Figure S1. Supporting Information.
Rosano, G. M. C. , Seferovic, P. , Savarese, G. , Spoletini, I. , Lopatin, Y. , Gustafsson, F. , Bayes‐Genis, A. , Jaarsma, T. , Abdelhamid, M. , Miqueo, A. G. , Piepoli, M. , Tocchetti, C. G. , Ristić, A. D. , Jankowska, E. , Moura, B. , Hill, L. , Filippatos, G. , Metra, M. , Milicic, D. , Thum, T. , Chioncel, O. , Ben Gal, T. , Lund, L. H. , Farmakis, D. , Mullens, W. , Adamopoulos, S. , Bohm, M. , Norhammar, A. , Bollmann, A. , Banerjee, A. , Maggioni, A. P. , Voors, A. , Solal, A. C. , and Coats, A. J. S. (2022) Impact analysis of heart failure across European countries: an ESC‐HFA position paper. ESC Heart Failure, 9: 2767–2778. 10.1002/ehf2.14076.
References
- 1. Groenewegen A, Rutten FH, Mosterd A, Hoes AW. Epidemiology of heart failure. Eur J Heart Fail. 2020; 22: 1342–1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. GBD 2017 Disease and Injury Incidence and Prevalence Collaborators . Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392: 1789–1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bui AL, Horwich TB, Fonarow GC. Epidemiology and risk profile of heart failure. Nat Rev Cardiol. 2011; 8: 30–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, Ikonomidis JS, Khavjou O, Konstam MA, Maddox TM, Nichol G, Pham M, Piña IL, Trogdon JG, American Heart Association Advocacy Coordinating Committee , Council on Arteriosclerosis, Thrombosis and Vascular Biology , Council on Cardiovascular Radiology and Intervention , Council on Clinical Cardiology , Council on Epidemiology and Prevention , Stroke Council . Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail. 2013; 6: 606–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez‐Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A, ESC Committee for Practice Guidelines . ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012; 33: 1787–1847. [DOI] [PubMed] [Google Scholar]
- 6. AlHabib KF, Elasfar AA, Alfaleh H, Kashour T, Hersi A, AlBackr H, Alshaer F, AlNemer K, Hussein GA, Mimish L, Almasood A, AlHabeeb W, AlGhamdi S, Alsharari M, Chakra E, Malik A, Soomro R, Ghabashi A, Al‐Murayeh M, Abuosa A. Clinical features, management, and short‐ and long‐term outcomes of patients with acute decompensated heart failure: phase I results of the HEARTS database. Eur J Heart Fail. 2014; 16: 461–469. [DOI] [PubMed] [Google Scholar]
- 7. Ponikowski P, Anker SD, AlHabib KF, Cowie MR, Force TL, Hu S, Jaarsma T, Krum H, Rastogi V, Rohde LE, Samal UC, Shimokawa H, Budi Siswanto B, Sliwa K, Filippatos G. Heart failure: preventing disease and death worldwide. ESC Heart Fail. 2014; 1: 4–25. [DOI] [PubMed] [Google Scholar]
- 8. Savarese G, Lund LH. Global public health burden of heart failure. Card Fail Rev. 2017; 3: 7–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Authors/Task Force Members , Document Reviewers . 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18: 891–975. [DOI] [PubMed] [Google Scholar]
- 10. Hobbs FD, Kenkre JE, Roalfe AK, Davis RC, Hare R, Davies MK. Impact of heart failure and left ventricular systolic dysfunction on quality of life: a cross‐sectional study comparing common chronic cardiac and medical disorders and a representative adult population. Eur Heart J. 2002; 23: 1867–1876. [DOI] [PubMed] [Google Scholar]
- 11. Shafie AA, Tan YP, Ng CH. Systematic review of economic burden of heart failure. Heart Fail Rev. 2018; 23: 131–145. [DOI] [PubMed] [Google Scholar]
- 12. Braunschweig F, Cowie MR, Auricchio A. What are the costs of heart failure? Europace. 2011; 13: ii13–ii17. [DOI] [PubMed] [Google Scholar]
- 13. Seferović PM, Vardas P, Jankowska EA, Maggioni AP, Timmis A, Milinković I, Polovina M, Gale CP, Lund LH, Lopatin Y, Lainscak M, Savarese G, Huculeci R, Kazakiewicz D, Coats AJS, National Heart Failure Societies of the ESC member countries . The Heart Failure Association Atlas: heart failure epidemiology and management statistics 2019. Eur J Heart Fail. 2021; 26. [DOI] [PubMed] [Google Scholar]
- 14. Bragazzi NL, Zhong W, Shu J, Abu Much A, Lotan D, Grupper A, Younis A, Dai H. Burden of heart failure and underlying causes in 195 countries and territories from 1990 to 2017. Eur J Prev Cardiol. 2021: zwaa147. [DOI] [PubMed] [Google Scholar]
- 15. Ceia F, Fonseca C, Mota T, Morais H, Matias F, de Sousa A, Oliveira A, EPICA Investigators . Prevalence of chronic heart failure in Southwestern Europe: the EPICA study. Eur J Heart Fail. 2002; 4: 531–539. [DOI] [PubMed] [Google Scholar]
- 16. Ohlmeier C, Mikolajczyk R, Frick J, Prütz F, Haverkamp W, Garbe E. Incidence, prevalence and 1‐year all‐cause mortality of heart failure in Germany: a study based on electronic healthcare data of more than six million persons. Clin Res Cardiol. 2015; 104: 688–696. [DOI] [PubMed] [Google Scholar]
- 17. Zarrinkoub R, Wettermark B, Wändell P, Mejhert M, Szulkin R, Ljunggren G, Kahan T. The epidemiology of heart failure, based on data for 2.1 million inhabitants in Sweden. Eur J Heart Fail. 2013; 15: 995–1002. [DOI] [PubMed] [Google Scholar]
- 18. Buja A, Solinas G, Visca M, Federico B, Gini R, Baldo V, Francesconi P, Sartor G, Bellentani M, Damiani G. Prevalence of heart failure and adherence to process indicators: which socio‐demographic determinants are involved? Int J Environ Res Public Health. 2016; 13: 238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Timmis A, Townsend N, Gale C, Grobbee R, Maniadakis N, Flather M, Wilkins E, Wright L, Vos R, Bax J, Blum M, Pinto F, Vardas P, ESC Scientific Document Group . European Society of Cardiology: cardiovascular disease statistics 2017. Eur Heart J. 2018; 39: 508–579. [DOI] [PubMed] [Google Scholar]
- 20. Levy D, Kenchaiah S, Larson MG, Benjamin EJ, Kupka MJ, Ho KK, Murabito JM, Vasan RS. Long‐term trends in the incidence of and survival with heart failure. Engl J Med. 2002; 347: 1397–1402. [DOI] [PubMed] [Google Scholar]
- 21. Najafi F, Jamrozik K, Dobson AJ. Understanding the ‘epidemic of heart failure’: a systematic review of trends in determinants of heart failure. Eur J Heart Fail. 2009; 11: 472–479. [DOI] [PubMed] [Google Scholar]
- 22. Gomez‐Soto FM, Andrey JL, Garcia‐Egido AA, Escobar MA, Romero SP, Garcia‐Arjona R, Gutierrez J, Gomez F. Incidence and mortality of heart failure: a community‐based study. Int J Cardiol. 2011; 151: 40–45. [DOI] [PubMed] [Google Scholar]
- 23. Sicras‐Mainar A, Sicras‐Navarro A, Palacios B, Varela L, Delgado JF. Epidemiology and treatment of heart failure in Spain: the HF‐PATHWAYS study. Rev Esp Cardiol (Engl Ed). 2022; 75: 31–38. [DOI] [PubMed] [Google Scholar]
- 24. Fonseca C, Brás D, Araújo I, Ceia F. Heart failure in numbers: estimates for the 21st century in Portugal. Rev Port Cardiol (Engl Ed). 2018; 37: 97–104. [DOI] [PubMed] [Google Scholar]
- 25. Gouveia M, Ascenção R, Fiorentino F, Costa J, Caldeira D, Broeiro‐Gonçalves P, Fonseca C, Borges M. The current and future burden of heart failure in Portugal. ESC Heart Fail. 2019; 6: 254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dweck MR, Bularga A, Hahn RT, Bing R, Lee KK, Chapman AR, White A, Salvo GD, Sade LE, Pearce K, Newby DE, Popescu BA, Donal E, Cosyns B, Edvardsen T, Mills NL, Haugaa K. Global evaluation of echocardiography in patients with COVID‐19. Eur Heart J Cardiovasc Imaging. 2020; 21: 949–958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sokolski M, Gajewski P, Zymliński R, Biegus J, Berg JMT, Bor W, Braunschweig F, Caldeira D, Cuculi F, D'Elia E, Edes IF, Garus M, Greenwood JP, Halfwerk FR, Hindricks G, Knuuti J, Kristensen SD, Landmesser U, Lund LH, Lyon A, Mebazaa A, Merkely B, Nawrocka‐Millward S, Pinto FJ, Ruschitzka F, Semedo E, Senni M, Sepehri Shamloo A, Sorensen J, Stengaard C, Thiele H, Toggweiler S, Tukiendorf A, Verhorst PM, Wright DJ, Zamorano P, Zuber M, Narula J, Bax JJ, Ponikowski P. Impact of coronavirus disease 2019 (COVID‐19) outbreak on acute admissions at the emergency and cardiology departments across Europe. Am J Med. 2021; 134: 482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Farmakis D, Mehra MR, Parissis J, Filippatos G. Heart failure in the course of a pandemic. Eur J Heart Fail. 2020; 2020: 1755–1758. [DOI] [PubMed] [Google Scholar]
- 29. Charman SJ, Velicki L, Okwose NC, Harwood A, McGregor G, Ristic A, Banerjee P, Seferovic PM, MacGowan GA, Jakovljevic DG. Insights into heart failure hospitalizations, management, and services during and beyond COVID‐19. ESC Heart Fail. 2021; 8: 175–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. König S, Ueberham L, Pellissier V, Hohenstein S, Meier‐Hellmann A, Thiele H, Ahmadli V, Borger MA, Kuhlen R, Hindricks G, Bollmann A. Hospitalization deficit of in‐ and outpatient cases with cardiovascular diseases and utilization of cardiological interventions during the COVID‐19 pandemic: insights from the German‐wide helios hospital network. Clin Cardiol. 2021; 44: 392–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. König S, Hohenstein S, Meier‐Hellmann A, Kuhlen R, Hindricks G, Bollmann A. In‐hospital care in acute heart failure during the COVID‐19 pandemic: insights from the German‐wide Helios hospital network. Eur J Heart Fail. 2020; 22: 2190–2201. [DOI] [PubMed] [Google Scholar]
- 32. Taylor CJ, Roalfe AK, Iles R, Hobbs FD. Ten‐year prognosis of heart failure in the community: follow‐up data from the Echocardiographic Heart of England Screening (ECHOES) study. Eur J Heart Fail. 2012; 14: 176–184. [DOI] [PubMed] [Google Scholar]
- 33. Barasa A, Schaufelberger M, Lappas G, Swedberg K, Dellborg M, Rosengren A. Heart failure in young adults: 20‐year trends in hospitalization, aetiology, and case fatality in Sweden. Eur Heart J. 2014; 35: 25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Salem K, El Khateeb O. Gender‐adjusted and age‐adjusted economic inpatient burden of congestive heart failure: cost and disability adjusted life‐year analysis. ESC Heart Fail. 2017; 4: 259–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Buddeke J, Valstar GB, van Dis I, Visseren FLJ, Rutten FH, den Ruijter HM, Vaartjes I, Bots ML, Queen of Hearts and RECONNECT investigators . Mortality after hospital admission for heart failure: improvement over time, equally strong in women as in men. BMC Public Health. 2020; 20: 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Triposkiadis F, Xanthopoulos A, Butler J. Cardiovascular aging and heart failure: JACC review topic of the week. J Am Coll Cardiol. 2019; 74: 804–813. [DOI] [PubMed] [Google Scholar]
- 37. Koh AS, Tay WT, Teng THK, Vedin O, Benson L, Dahlstrom U, Savarese G, Lam CSP, Lund LH. A comprehensive population‐based characterization of heart failure with mid‐range ejection fraction. Eur J Heart Fail. 2017; 19: 1624–1634. [DOI] [PubMed] [Google Scholar]
- 38. Lenzen MJ, Scholte op Reimer WJ, Boersma E, Vantrimpont PJ, Follath F, Swedberg K, Cleland J, Komajda M. Differences between patients with a preserved and a depressed left ventricular function: a report from the EuroHeart Failure Survey. Eur Heart J. 2004; 25: 1214–1220. [DOI] [PubMed] [Google Scholar]
- 39. Lund LH, Donal E, Oger E, Hage C, Persson H, Haugen‐Löfman I, Ennezat PV, Sportouch‐Dukhan C, Drouet E, Daubert JC, Linde C, KaRen Investigators . Association between cardiovascular vs. non‐cardiovascular co‐morbidities and outcomes in heart failure with preserved ejection fraction. Eur J Heart Fail. 2014; 16: 992–1001. [DOI] [PubMed] [Google Scholar]
- 40. Nieminen MS, Brutsaert D, Dickstein K, Drexler H, Follath F, Harjola V, Hochadel M, Komajda M, Lassus J, Lopez‐Sendon JL, Ponikowski P, Tavazzi L, EuroHeart Survey Investigators , Heart Failure Association, European Society of Cardiology , EuroHeart Survey Investigators , Heart Failure Association , European Society of Cardiology . EuroHeart Failure Survey II (EHFS II): a survey on hospitalized acute heart failure patients: description of population. Eur Heart J. 2006; 27: 2725–2736. [DOI] [PubMed] [Google Scholar]
- 41. Crespo‐Leiro MG, Anker SD, Maggioni AP, Coats AJ, Filippatos G, Ruschitzka F, Ferrari R, Piepoli MF, Delgado Jimenez JF, Metra M, Fonseca C, Hradec J, Amir O, Logeart D, Dahlström U, Merkely B, Drozdz J, Goncalvesova E, Hassanein M, Chioncel O, Lainscak M, Seferovic PM, Tousoulis D, Kavoliuniene A, Fruhwald F, Fazlibegovic E, Temizhan A, Gatzov P, Erglis A, Laroche C, Mebazaa A, Heart Failure Association (HFA) of the European Society of Cardiology (ESC) . European Society of Cardiology Heart Failure Long‐Term Registry (ESC‐HF‐LT): 1‐year follow‐up outcomes and differences across regions. Eur J Heart Fail. 2016; 18: 613–625. [DOI] [PubMed] [Google Scholar]
- 42. Chioncel O, Lainscak M, Seferovic PM, Anker SD, Crespo‐Leiro MG, Harjola VP, Parissis J, Laroche C, Piepoli MF, Fonseca C, Mebazaa A, Lund L, Ambrosio GA, Coats AJ, Ferrari R, Ruschitzka F, Maggioni AP, Filippatos G. Epidemiology and one‐year outcomes in patients with chronic heart failure and preserved, mid‐range and reduced ejection fraction: an analysis of the ESC Heart Failure Long‐Term Registry. Eur J Heart Fail. 2017; 19: 1574–1585. [DOI] [PubMed] [Google Scholar]
- 43. Boman K, Lindmark K, Stålhammar J, Olofsson M, Costa‐Scharplatz M, Fonseca AF, Johansson S, Heller V, Törnblom M, Wikström G. Healthcare resource utilisation and costs associated with a heart failure diagnosis: a retrospective, population‐based cohort study in Sweden. BMJ Open. 2021; 11: e053806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Kamiya K, Sato Y, Takahashi T, Tsuchihashi‐Makaya M, Kotooka N, Ikegame T, Takura T, Yamamoto T, Nagayama M, Goto Y, Makita S, Isobe M. Multidisciplinary cardiac rehabilitation and long‐term prognosis in patients with heart failure. Circ Heart Fail. 2020; 13: e006798. [DOI] [PubMed] [Google Scholar]
- 45. Moita B, Marques AP, Camacho AM, Leão Neves P, Santana R. One‐year rehospitalisations for congestive heart failure in Portuguese NHS hospitals: a multilevel approach on patterns of use and contributing factors. 2019; 9: e031346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kurmani S, Squire I. Acute heart failure: definition, classification and epidemiology. Curr Heart Fail Rep. 2017; 14: 385–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CSP, Sato N, Shah AN, Gheorghiade M. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014; 63: 1123–1133. [DOI] [PubMed] [Google Scholar]
- 48. Chioncel O, Mebazaa A, Harjola VP, Coats AJ, Piepoli MF, Crespo‐Leiro MG, Laroche C, Seferovic PM, Anker SD, Ferrari R, Ruschitzka F, Lopez‐Fernandez S, Miani D, Filippatos G, Maggioni AP, ESC Heart Failure Long‐Term Registry Investigators . Clinical phenotypes and outcome of patients hospitalized for acute heart failure: the ESC Heart Failure Long‐Term Registry. Eur J Heart Fail. 2017; 19: 1242–1254. [DOI] [PubMed] [Google Scholar]
- 49. Chioncel O, Mebazaa A, Maggioni AP, Harjola VP, Rosano G, Laroche C, Piepoli MF, Crespo‐Leiro MG, Lainscak M, Ponikowski P, Filippatos G, Ruschitzka F, Seferovic P, Coats AJS, Lund LH. Acute heart failure congestion and perfusion status—impact of the clinical classification on in‐hospital and long‐term outcomes; insights from the ESC‐EORP HFA Heart Failure Long‐Term Registry. Eur J Heart Fail. 2019; 21: 1338–1352. [DOI] [PubMed] [Google Scholar]
- 50. Hollingworth W, Biswas M, Maishman RL, Dayer MJ, McDonagh T, Purdy S, Reeves BC, Rogers CA, Williams R, Pufulete M. The healthcare costs of heart failure during the last five years of life: a retrospective cohort study. Int J Cardiol. 2016; 224: 132–138. [DOI] [PubMed] [Google Scholar]
- 51. Jankowska EA, von Haehling S, Anker SD, Macdougall IC, Ponikowski P. Iron deficiency and heart failure: diagnostic dilemmas and therapeutic perspectives. Eur Heart J. 2013; 34: 816–829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Rocha BML, Cunha GJL, Menezes Falcão LF. The burden of iron deficiency in heart failure: therapeutic approach. J Am Coll Cardiol. 2018; 71: 782–793. [DOI] [PubMed] [Google Scholar]
- 53. Ponikowski P, Kirwan BA, Anker SD, McDonagh T, Dorobantu M, Drozdz J, Fabien V, Filippatos G, Göhring UM, Keren A, Khintibidze I, Kragten H, Martinez FA, Metra M, Milicic D, Nicolau JC, Ohlsson M, Parkhomenko A, Pascual‐Figal DA, Ruschitzka F, Sim D, Skouri H, van der Meer P, Lewis BS, Comin‐Colet J, von Haehling S, Cohen‐Solal A, Danchin N, Doehner W, Dargie HJ, Motro M, Butler J, Friede T, Jensen KH, Pocock S, Jankowska EA, AFFIRM‐AHF investigators . Ferric carboxymaltose for iron deficiency at discharge after acute heart failure: a multicentre, double‐blind, randomised, controlled trial. Lancet. 2020; 396: 1895–1904. [DOI] [PubMed] [Google Scholar]
- 54. Jankowska EA, Kirwan BA, Kosiborod M, Butler J, Anker SD, McDonagh T, Dorobantu M, Drozdz J, Filippatos G, Keren A, Khintibidze I, Kragten H, Martinez FA, Metra M, Milicic D, Nicolau JC, Ohlsson M, Parkhomenko A, Pascual‐Figal DA, Ruschitzka F, Sim D, Skouri H, van der Meer P, Lewis BS, Comin‐Colet J, von Haehling S, Cohen‐Solal A, Danchin N, Doehner W, Dargie HJ, Motro M, Friede T, Fabien V, Dorigotti F, Pocock S, Ponikowski P. The effect of intravenous ferric carboxymaltose on health‐related quality of life in iron‐deficient patients with acute heart failure: the results of the AFFIRM‐AHF study. Eur Heart J. 2021: ehab234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. McEwan P, Ponikowski P, Davis JA, Rosano G, Coats AJS, Dorigotti F, O'Sullivan D, Ramirez de Arellano A, Jankowska EA. Ferric carboxymaltose for the treatment of iron deficiency in heart failure: a multinational cost‐effectiveness analysis utilising AFFIRM‐AHF. Eur J Heart Fail. 2021; 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Logeart D, Isnard R, Resche‐Rigon M, Seronde MF, de Groote P, Jondeau G, Galinier M, Mulak G, Donal E, Delahaye F, Juilliere Y, Damy T, Jourdain P, Bauer F, Eicher JC, Neuder Y, Trochu JN, Heart Failure of the French Society of Cardiology . Current aspects of the spectrum of acute heart failure syndromes in a real‐life setting: the OFICA study. Eur J Heart Fail. 2013; 15: 465–476. [DOI] [PubMed] [Google Scholar]
- 57. Miró Ò, García Sarasola A, Fuenzalida C, Calderón S, Jacob J, Aguirre A, Wu DM, Rizzi MA, Malchair P, Haro A, Herrera S, Gil V, Martín‐Sánchez FJ, Llorens P, Herrero Puente P, Bueno H, Domínguez Rodríguez A, Müller CE, Mebazaa A, Chioncel O, Alquézar‐Arbé A, ICA‐SEMES Research Group . Departments involved during the first episode of acute heart failure and subsequent emergency department revisits and rehospitalisations: an outlook through the NOVICA cohort. Eur J Heart Fail. 2019; 21: 1231–1244. [DOI] [PubMed] [Google Scholar]
- 58. McMurray JJV, Solomon SD, Inzucchi SE, Køber L, Kosiborod MN, Martinez FA, Ponikowski P, Sabatine MS, Anand IS, Bělohlávek J, Böhm M, Chiang CE, Chopra VK, de Boer RA, Desai AS, Diez M, Drozdz J, Dukát A, Ge J, Howlett JG, Katova T, Kitakaze M, Ljungman CEA, Merkely B, Nicolau JC, O'Meara E, Petrie MC, Vinh PN, Schou M, Tereshchenko S, Verma S, Held C, DeMets DL, Docherty KF, Jhund PS, Bengtsson O, Sjöstrand M, Langkilde AM, DAPA‐HF Trial Committees and Investigators . Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019; 381: 1995–2008. [DOI] [PubMed] [Google Scholar]
- 59. Chioncel O, Parissis J, Mebazaa A, Thiele H, Desch S, Bauersachs J, Harjola VP, Antohi EL, Arrigo M, Gal TB, Celutkiene J, Collins SP, DeBacker D, Iliescu VA, Jankowska E, Jaarsma T, Keramida K, Lainscak M, Lund LH, Lyon AR, Masip J, Metra M, Miro O, Mortara A, Mueller C, Mullens W, Nikolaou M, Piepoli M, Price S, Rosano G, Vieillard‐Baron A, Weinstein JM, Anker SD, Filippatos G, Ruschitzka F, Coats AJS, Seferovic P. Epidemiology, pathophysiology and contemporary management of cardiogenic shock—a position statement from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2020; 22: 1315–1341. [DOI] [PubMed] [Google Scholar]
- 60. Johansson I, Dahlstrom U, Edner M, Nasman P, Ryden L, Norhammar A. Type 2 diabetes and heart failure: characteristics and prognosis in preserved, mid‐range and reduced ventricular function. Diab Vasc Dis Res. 2018; 15: 494–503. [DOI] [PubMed] [Google Scholar]
- 61. Savarese G, Settergren C, Schrage B, Thorvaldsen T, Löfman I, Sartipy U, Mellbin L, Meyers A, Farsani SF, Brueckmann M, Brodovicz KG, Vedin O, Asselbergs FW, Dahlström U, Cosentino F, Lund LH. Comorbidities and cause‐specific outcomes in heart failure across the ejection fraction spectrum: a blueprint for clinical trial design. Int J Cardiol. 2020; 313: 76–82. [DOI] [PubMed] [Google Scholar]
- 62. Norhammar A, Bodegård J, Nyström T, Eriksson JW, Thuresson M, Nathanson D. Incidence, prevalence and mortality of type 2 diabetes requiring glucose‐lowering treatment, and associated risks of cardiovascular complications: a nationwide study in Sweden, 2006–2013. Diabetologia. 2016; 59: 1692–1701. [DOI] [PubMed] [Google Scholar]
- 63. Rawshani A, Rawshani A, Franzén S, Sattar N, Eliasson B, Svensson AM, Zethelius B, Miftaraj M, McGuire DK, Rosengren A, Gudbjörnsdottir S. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018; 379: 633–644. [DOI] [PubMed] [Google Scholar]
- 64. Ritsinger V, Nystrom T, Saleh N, Lagerqvist B, Norhammar A. Heart failure is a common complication after acute myocardial infarction in patients with diabetes: a nationwide study in the SWEDEHEART registry. Eur J Prev Cardiol. 2020; 27: 1890–1901. [DOI] [PubMed] [Google Scholar]
- 65. Birkeland K, Bodegard J, Eriksson JW, Norhammar A, Haller H, Linssen GCM, Banerjee A, Marcus Thuresson M, Okami S, Garal‐Pantaler E, Overbeek J, Mamza JB, Zhang R, Yajima T, Komuro I, Kadowaki T. Heart failure and chronic kidney disease manifestation and mortality risk associations in type 2 diabetes: a large multinational cohort study. Diabetes Obes Metab. 2020; 22: 1607–1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Lewis EF, Lamas GA, O'Meara E, Granger CB, Dunlap ME, McKelvie RS, Probstfield JL, Young JB, Michelson EL, Halling K, Carlsson J, Olofsson B, McMurray JJV, Yusuf S, Swedberg K, Pfeffer MA, CHARM Investigators . Characterization of health‐related quality of life in heart failure patients with preserved versus low ejection fraction in CHARM. Eur J Heart Fail. 2007; 9: 83–91. [DOI] [PubMed] [Google Scholar]
- 67. Jaarsma T, Johansson P, Agren S, Strömberg A. Quality of life and symptoms of depression in advanced heart failure patients and their partners. Curr Opin Support Palliat Care. 2010; 4: 233–237. [DOI] [PubMed] [Google Scholar]
- 68. Hoekstra T, Lesman‐Leegte I, van Veldhuisen DJ, Sanderman R, Jaarsma T. Quality of life is impaired similarly in heart failure patients with preserved and reduced ejection fraction. Eur J Heart Fail. 2011; 13: 1013–1018. [DOI] [PubMed] [Google Scholar]
- 69. Pieske B, Tschöpe C, de Boer RA, Fraser AG, Anker SD, Donal E, Edelmann F, Fu M, Guazzi M, Lam CSP, Lancellotti P, Melenovsky V, Morris DA, Nagel E, Pieske‐Kraigher E, Ponikowski P, Solomon SD, Vasan RS, Rutten FH, Voors AA, Ruschitzka F, Paulus WJ, Seferovic P, Filippatos G. How to diagnose heart failure with preserved ejection fraction: the HFA‐PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail. 2020; 22: 391–412. [DOI] [PubMed] [Google Scholar]
- 70. Iqbal J, Francis L, Reid J, Murray S, Denvir M. Quality of life in patients with chronic heart failure and their carers: a 3‐year follow‐up study assessing hospitalization and mortality. Eur J Heart Fail. 2010; 12: 1002–1008. [DOI] [PubMed] [Google Scholar]
- 71. Rasmussen AA, Johnsen SP, Berg SK, Rasmussen TB, Borregaard B, Thrysoee L, Thorup CB, Mols RE, Wiggers H, Larsen SH. Predictors of patient‐reported outcomes at discharge in patients with heart failure. Eur J Cardiovasc Nurs. 2020; 19: 748–756. [DOI] [PubMed] [Google Scholar]
- 72. Jaarsma T, Hill L, Bayes‐Genis A, La Rocca HB, Castiello T, Čelutkienė J, Marques‐Sule E, Plymen CM, Piper SE, Riegel B, Rutten FH, Ben Gal T, Bauersachs J, Coats AJS, Chioncel O, Lopatin Y, Lund LH, Lainscak M, Moura B, Mullens W, Piepoli MF, Rosano G, Seferovic P, Strömberg A. Self‐care of heart failure patients: practical management recommendations from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2021; 23: 157–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Komajda M, Cowie MR, Tavazzi L, Ponikowski P, Anker SD, Filippatos GS. Physicians' guideline adherence is associated with better prognosis in outpatients with heart failure with reduced ejection fraction: the QUALIFY international registry. Eur J Heart Fail. 2017; 19: 1414–1423. [DOI] [PubMed] [Google Scholar]
- 74. Van Spall HGC, Rahman T, Mytton O, Ramasundarahettige C, Ibrahim Q, Kabali C, Coppens M, Brian Haynes R, Connolly S. Comparative effectiveness of transitional care services in patients discharged from the hospital with heart failure: a systematic review and network meta‐analysis. Eur J Heart Fail. 2017; 19: 1427–1443. [DOI] [PubMed] [Google Scholar]
- 75. Vitale C, Spoletini I, Rosano GM. Frailty in heart failure: implications for management. Card Fail Rev. 2018; 4: 104–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Butler J, Anker SD, Filippatos G, Khan MS, Ferreira JP, Pocock SJ, Giannetti N, Januzzi JL, Piña IL, Lam CSP, Ponikowski P, Sattar N, Verma S, Brueckmann M, Jamal W, Vedin O, Peil B, Zeller C, Zannad F, Packer M, EMPEROR‐Reduced Trial Committees and Investigators . Empagliflozin and health‐related quality of life outcomes in patients with heart failure with reduced ejection fraction: the EMPEROR‐Reduced trial. Eur Heart J. 2021; 42: 1203–1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. McMurray J, Parker M, Desai AS, Gong J, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, PARADIGM‐HF Investigators and Committees . Angiotensin–neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014; 371: 993–1004. [DOI] [PubMed] [Google Scholar]
- 78. Nagy KV, Merkely B, Rosero S, Geller L, Kosztin A, McNitt S, Polonsky B, Goldenberg I, Zareba W, Kutyifa V. Quality of life predicting long‐term outcomes in cardiac resynchronization therapy patients. Europace. 2019; 21: 1865–1875. [DOI] [PubMed] [Google Scholar]
- 79. Crespo‐Leiro MG, Metra M, Lund LH, Milicic D, Costanzo MR, Filippatos G, Gustafsson F, Tsui S, Barge‐Caballero E, De Jonge N, Frigerio M, Hamdan R, Hasin T, Hülsmann M, Nalbantgil S, Potena L, Bauersachs J, Gkouziouta A, Ruhparwar A, Ristic AD, Straburzynska‐Migaj E, McDonagh T, Seferovic P, Ruschitzka F. Advanced heart failure: a position statement of the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2018; 20: 1505–1535. [DOI] [PubMed] [Google Scholar]
- 80. Spoletini I, Ferrari R, Rosano GMC. Living with stable angina: patients' pathway and needs in angina. J Cardiovasc Med (Hagerstown). 2020; 21: 377–382. [DOI] [PubMed] [Google Scholar]
- 81. Van Deursen VM, Urso R, Laroche C, Damman K, Dahlstom U, Tavazzi L, Maggioni AP, Voors AA. Comorbidities in patients with heart failure: an analysis of the European Heart Failure Pilot Survey. Eur J Heart Fail. 2014; 16: 103–111. [DOI] [PubMed] [Google Scholar]
- 82. Greene SJ, Butler J, Spertus JA, Hellkamp AS, Vaduganathan M, DeVore AD, Albert NM, Duffy CI, Patterson JH, Thomas L, Williams FB, Hernandez AF, Fonarow GC. Comparison of New York Heart Association class and patient‐reported outcomes for heart failure with reduced ejection fraction. JAMA Cardiol. 2021; 6: 522–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Ruppar TM, Cooper PS, Mehr DR, Delgado JM, Dunbar‐Jacob JM. Medication adherence interventions improve heart failure mortality and readmission rates: systematic review and meta‐analysis of controlled trials. J Am Heart Assoc. 2016; 5: e002606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Heidenreich PA, Hernandez AF, Yancy CW, Liang L, Peterson ED, Fonarow GC. Get With The Guidelines program participation, process of care, and outcome for Medicare patients hospitalized with heart failure. Circ Cardiovasc Qual Outcomes. 2012; 5: 37–43. [DOI] [PubMed] [Google Scholar]
- 85. Burns DJP, Arora J, Okunade O, Beltrame JF, Bernardez‐Pereira S, Crespo‐Leiro MG, Filippatos GS, Hardman S, Hoes AW, Hutchison S, Jessup M, Kinsella T, Knapton M, Lam CSP, Masoudi FA, McIntyre H, Mindham R, Morgan L, Otterspoor L, Parker V, Persson HE, Pinnock C, Reid CM, Riley J, Stevenson LW, McDonagh TA. International Consortium for Health Outcomes Measurement (ICHOM): standardized patient‐centered outcomes measurement set for heart failure patients. JACC Heart Fail. 2020; 8: 212–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Lund LH, Carrero JJ, Farahmand B, Henriksson KM, Jonsson Å, Jernberg T, Dahlström U. Association between enrolment in a heart failure quality registry and subsequent mortality—a nationwide cohort study. Eur J Heart Fail. 2017; 19: 1107–1116. [DOI] [PubMed] [Google Scholar]
- 87. Smeets M, Henrard S, Aertgeerts B, Cools F, Janssens S, Vaes B. Methods to identify heart failure patients in general practice and their impact on patient characteristics: a systematic review. Int J Cardiol. 2018; 257: 199–206. [DOI] [PubMed] [Google Scholar]
- 88. Guha K, McDonagh T. Heart failure epidemiology: European perspective. Curr Cardiol Rev. 2013; 9: 123–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Supporting Information.


