Abstract
Background
The present study compared the clinical effect of extracorporeal shock wave therapy (ESWT) with that of ultrasound (US)-guided shoulder steroid injection therapy in patients with supraspinatus tendinitis. We hypothesized that the two treatments would show comparable results.
Methods
The inclusion criteria were age over 20 years and diagnosis of supraspinatus tendinitis using US. Ultimately, 26 patients were assigned using blocked randomization: 13 in the US-guided shoulder injection group and 13 in the ESWT group. Treatment outcomes were evaluated using the pain visual analog scale (pVAS), the American Shoulder and Elbow Society (ASES) score, and the Constant score at baseline and at 1 and 3 months after the procedure.
Results
At 1 month after the intervention, pVAS, ASES, and constant score were significantly higher in the US-guided shoulder injection group than in the ESWT group, but not at 3 months after the intervention. Both groups showed clinically significant treatment effects at 3 months after the intervention compared to baseline. No significance was shown using equivalence testing.
Conclusions
US-guided shoulder injection therapy was not superior to ESWT therapy. Considering the complications and rebound phenomenon of steroid injections, interventions using ESWT may be a good alternative to treat patients with supraspinatus tendinitis.
Keywords: Supraspinatus tendinitis, Extracorporeal shock wave therapy, Injection, Random allocation
A number of literature reviews have revealed that the incidence of rotator cuff disorders is approximately 10% in individuals aged < 20 years and 60% in those aged ≥ 80 years, while the incidence of rotator cuff tendinitis is approximately 5%–6%.1,2) Despite the common occurrence, the exact pathophysiology of rotator cuff tendinitis remains unclear. In most cases, the disease is self-limiting, but chronic tendinitis symptoms can develop in rare cases. The general conservative treatments include rest, nonsteroidal anti-inflammatory drugs, physiotherapy, and steroid injections, although the therapeutic effects of these treatments have not yet been established.3) Various studies have evaluated the efficacy of steroid injections in the shoulder and found that such treatment improves range of motion by reducing pain and inflammation.4,5) However, the long-term effects remain controversial.
As an alternative treatment, extracorporeal shock wave therapy (ESWT) has proven effective in various musculoskeletal disorders.6) In particular, ESWT shows remarkable treatment effects in enthesopathy including epicondylitis, Achilles tendinitis, patella tendinitis, and plantar fasciitis.7,8,9) The precise therapeutic mechanism of ESWT is yet to be elucidated, but the treatment has a positive influence on neovascularization and growth factor release.10) ESWT has proven effective in treating calcific shoulder tendinitis, while the benefits remain controversial in non-calcific shoulder tendinitis.11)
Having reviewed the literature thoroughly, we found that few studies have compared the effects of ESWT with those of steroid injections in the treatment of patients with supraspinatus tendinitis—a subtype of non-calcific shoulder tendinitis. When designing the present study, we hypothesized that the treatment effects of ESWT would have an equivalent outcome to those of steroid injections in patients with supraspinatus tendinitis. The study also compared the clinical results of each patient group after ESWT or an ultrasound (US)-guided shoulder steroid injection to treat supraspinatus tendinitis.
METHODS
Ethical Statement and Study Design
Among patients scheduled for treatment of supraspinatus tendinitis between May 2017 and April 2018, those who conformed to the inclusion/exclusion criteria were recruited to the present study. Prior to participation, the principal investigator (GWL) explained the purpose and methods of the study in detail to the patients, who then signed a consent form to enroll in the study. The research protocol was approved by the Institutional Review Board of Hallym University Kangnam Sacred Heart Hospital (No. 2017-03-015), and the study was carried out in accordance with the Declaration of Helsinki.
To ensure scientific validity and prevent subjective judgment, the participants were assigned in a 1 to 1 ratio to one of the two following intervention groups using a method of random allocation based on probabilistic theory: (1) independent treatment using ESWT and (2) independent treatment using an US-guided shoulder injection. The codes were generated using blocked randomization in a computer program, and the allocation envelope was opened on the first day of the intervention. A three-digit random allocation number (R01 or R02) was assigned to each participant, and each participant received the treatment corresponding to that number.
Patient Enrollment
In the G-Power 3.1.5 software, the sample size was estimated based on an effect size of 0.45, a significance level of 0.05, and a power of 0.80, yielding a sample size of 12 subjects per group—24 subjects in total. Taking into account a ≥ 10% dropout rate, a total of 26 patients (13 in each group) were recruited.12) The study participants were outpatients visiting the hospital. When the predetermined number of subjects assigned to a group reached 100%, enrollment in this group was ended, while enrollment in the other group continued.
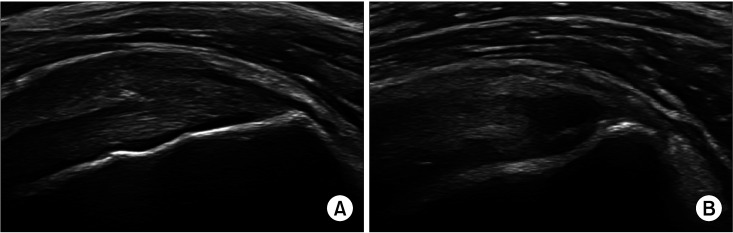
The inclusion criteria were as follows: (1) age ≥ 20 years, (2) diagnosis of supraspinatus tendinitis by US, and (3) written consent to participate in the study. US examinations were performed and read according to standardized procedures by a musculoskeletal radiologist with over 20 years of experience (IY). This result was confirmed secondary by a senior clinician (KCN). If a local hypoechoic lesion was seen or fibrillar disruption was less than 25% of the tendon height, it was classified as tendinitis, and if it was more than 25%, it was classified as partial thickness and excluded from the study (Fig. 1).
Fig. 1. Ultrasound images of a patient with tendinitis (A) and a patient with a partial thickness rotator cuff tear (B).
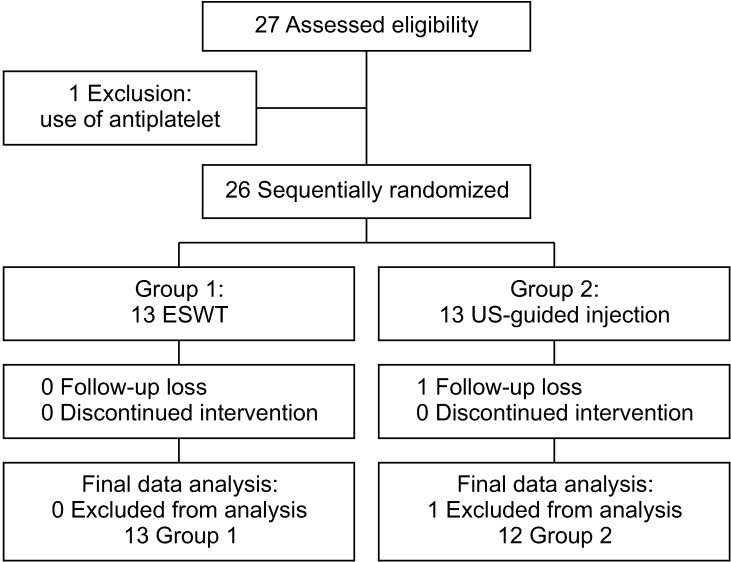
The exclusion criteria were as follows: (1) rotator cuff surgery on the corresponding side, (2) superior labral reconstruction on the corresponding side, (3) rupture in the supraspinatus or complete rupture in other rotator cuff tendons, (4) any steroid intervention (oral or injected) within the previous 3 months, (5) history of allergy to lidocaine or US gel, (6) inflammatory or autoimmune disease, (7) fever or infectious disease within the previous 2 weeks, (8) diabetes mellitus, (9) blood disorders such as platelet dysfunction syndrome that prevented treatment using an injection, (10) increased hemorrhagic risk caused by an antiplatelet drug, (11) pregnancy or lactation, (12) individuals who failed to satisfy the requirements of the clinical study, as determined by the principal investigator (GWL) (Fig. 2).
Fig. 2. Flowchart of patient selection in the study. ESWT: extracorporeal shock wave therapy, US: ultrasound.
Outcome Measures
To ensure that the study was valid, all participants underwent a clinical evaluation (pain visual analog scale [pVAS], American Shoulder and Elbow Society [ASES] score, and Constant score) prior to the intervention and at 1 month and 3 months after the intervention. Pain was measured using the pVAS, which visualizes the level of subjective pain on a scale of 0–100: 0 indicated no pain and 100 the worst imaginable pain. The ASES score assesses shoulder joint functions based on the patient’s subjective pain and most frequently performed daily activities. The Constant score allows both subjective and objective functional assessments as it includes scores for range of motion (40 points) and muscular strength (25 points), measured using physical tests performed by an investigator, as well as scores for the level of subjective pain (15 point) and the level of patient satisfaction regarding sleep, work, exercise, and leisure (20 points).
Interventions
US-guided shoulder injection
To accurately detect the lesion area, the injection was performed under US guidance. A posterior approach was used because it allowed the marker to be easily identified and because the space between the humeral head and the acromion was usually larger in that region. Firstly, the posterolateral edge of the acromion was sensed with the thumb and forefinger. After wiping the skin with an alcohol swab, the patient’s upper arm was placed on the thigh to relax the deltoid. As the anterior acromion was sensed with one finger, a 25-G injection needle was pointed in the direction of the finger. When resistance was felt during the injection, the needle was determined to be in the tendon; the needle was then slowly pulled back until the resistance faded, and 2 mL of 2% lidocaine was rapidly injected. For 2 minutes, the clinicians monitored whether the anesthetic was working. The syringe containing the anesthetic was then replaced with a syringe containing a steroid (triamcinolone acetonide; 40 mg/m/V) in the same position. All injection treatments were administered once.
ESWT
Prior to the intervention, the patients were given detailed explanations of the possible side effects and intervention time. They were also told that the treatment effects of ESWT could fail if they moved. Next, the shock wave frequency and energy were selected (mode: linear focused, counter: 2000, energy level setting 5 = positive Energy Flux Density of 0.142 mJ/mm2), and the head of the ESWT device (PiezoWave2 MULTIUSE60; WOLF) was covered evenly with US gel.13) ESWT was then applied once to the lesion area.
Statistical Analysis
To analyze the mean and frequency, the demographic data and the results of the questionnaire were evaluated. For categorical data, Pearson’s chi-square and Fisher’s exact tests were used. For continuous data from the pVAS, ASES, and constant score, the Student’s t-test and Wilcoxon rank-sum test were used. For comparative analysis of time-dependent data (baseline, 1 month, and 3 months) from the two intervention groups, repeated-measures analysis of variance and the linear mixed model were used. A post hoc Bonferroni test was used to compare the means of baseline scores between the groups. To determine equivalence between the groups, equivalence testing was carried out. In all statistical analyses, IBM SPSS ver. 24.0 (IBM Inc., Armonk, NY, USA) was used, while statistical significance was set at a p-value of < 0.05.
RESULTS
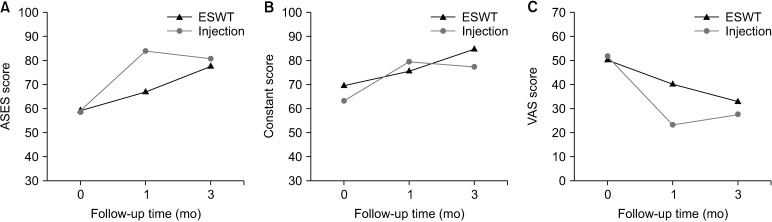
The present study was conducted in a total of 26 patients: 13 in each group. In the US-guided shoulder injection group, 1 patient was lost to follow-up, while no one dropped out of the ESWT intervention group. The two groups showed no significant difference in sex, age, or involved site (Table 1). Regarding the clinical treatment effects in each intervention group, the US-guided shoulder injection group showed treatment effects in the pVAS, ASES score, and Constant score at both 1 and 3 months after the intervention compared to baseline. However, the effects at 3 months after the intervention were significantly lower than those at 1 month after the intervention. The ESWT group showed significant treatment effects in the pVAS, ASES score, and Constant score at 3 months after the intervention compared to baseline, but not at 1 month after the intervention (Fig. 3).
Table 1. Demographic Data of ESWT and US-Guided Injection Groups at Baseline.
| Variable | Group 1: ESWT (n = 13) | Group 2: US-guided Injection (n = 12) | p-value | |
|---|---|---|---|---|
| Sex | 0.673 | |||
| Male | 5 (38.46) | 3 (25.00) | ||
| Female | 8 (61.54) | 9 (75.00) | ||
| Age (yr) | 52.31 ± 7.25 | 53.00 ± 9.52 | 0.921 | |
| Involved site | 1.000 | |||
| Right | 7 | 6 | ||
| Left | 6 | 6 | ||
Values are presented as number (%) or mean ± standard deviation.
ESWT: extracorporeal shock wave therapy, US: ultrasound.
Fig. 3. Changes in the American Shoulder and Elbow Society (ASES) score (A), Constant score (B), and visual analog scale (VAS) score (C) over time. ESWT: extracorporeal shock wave therapy.
When the two groups were compared, the pVAS, ASES score, and Constant score measured before intervention showed no significant difference between the US-guided shoulder injection group and the ESWT group. At 1 month after the intervention, the pVAS, ASES score, and Constant score indicated that the treatment effects were significantly better in the US-guided shoulder injection group than in the ESWT group. However, at 3 months after the intervention, the 3 measures showed no significant intergroup difference in treatment effects (Table 2). Based on these findings, equivalence testing was carried out to verify the equivalence of post-intervention clinical outcome between the US-guided shoulder injection group and ESWT group, but the results showed no statistical significance (Table 3).
Table 2. Comparison of Clinical Score Difference between ESWT and Injection Groups.
| Variable | ESWT group | Injection group | p-value | |
|---|---|---|---|---|
| ASES score | ||||
| ΔASES1 month | 6.42 ± 9.31 | 25.08 ± 17.45 | 0.005* | |
| ΔASES3 months | 15.68 ± 13.03 | 22.22 ± 19.33 | 0.375 | |
| Constant score | ||||
| ΔConstant1 month | 6.17 ± 4.76 | 16.25 ± 14.98 | 0.044* | |
| ΔConstant3 months | 12.30 ± 8.69 | 14.42 ± 17.80 | 0.870 | |
| VAS score | ||||
| ΔVAS1 month | –8.42 ± 15.93 | –28.50 ± 20.93 | 0.015* | |
| ΔVAS3 months | –18.00 ± 18.15 | –24.17 ± 20.97 | 0.474 | |
Values are presented as mean ± standard deviation.
ESWT: extracorporeal shock wave therapy, ASES: American Shoulder and Elbow Society, ΔASESmonths: ASESmonths – ASESbaseline, ΔConstantmonths: Constantmonths – Constantbaseline, VAS: visual analog scale, ΔVASmonths: VASmonths – VASbaseline.
*Indicates statistical significance (p < 0.05).
Table 3. Equivalence Testing of Clinical Score between ESWT and Injection Groups at 3 Months.
| Variable | ESWT group | Injection group | p-value |
|---|---|---|---|
| ASES score | 77.82 ± 12.25 | 80.66 ± 17.76 | 0.299 |
| Constant score | 85.10 ± 12.13 | 77.42 ± 10.65 | 0.129 |
| VAS score | 33.00 ± 15.85 | 27.50 ± 24.63 | 0.688 |
Values are presented as mean ± standard deviation.
ESWT: extracorporeal shock wave therapy, ASES: American Shoulder and Elbow Society, VAS: visual analog scale.
DISCUSSION
By comparing clinical outcome in the US-guided shoulder injection and ESWT groups, the present study showed that the latter can be considered an adequate alternative treatment for supraspinatus tendinitis. Although the ESWT group showed no significant treatment effects 1 month after the intervention, significant treatment effects were obtained in 3 months. The clinical treatment effects 1 month after intervention were significantly higher in the US-guided shoulder injection group. However, 3 months after intervention, the treatment effects showed no significant intergroup difference. While the effects of independent ESWT treatment consistently increased over time, those of the US-guided shoulder steroid injection did not, presumably because the rebound phenomenon diminished the effects of the steroid treatment. In the present study, equivalence testing was carried out to verify equivalence in the treatment effects between the groups, but the results could not confirm any equivalence, probably because the patient groups were too small for the statistical analyses.
Most previous studies on patients with shoulder complaints have compared ESWT with a placebo,14,15) determined the independent effects of ESWT,16) or compared ESWT with physical therapy,17) kinesio taping,18) or acromion type.19) The short-term and long-term effects of ESWT to treat non-calcific tendinopathy of the rotator cuff remain controversial. Previous studies comparing the treatment effect between placebo or control groups and an ESWT group have reported that the pain and constant scores indicated a significant treatment effect in the short term, but that the long-term effects were not different from those of a placebo.14,15,20) The present study showed that independent ESWT treatment had marked effects compared to the steroid injection during the 3-month follow-up period. These results are of great significance because they showed that ESWT has positive treatment effects on supraspinatus tendinitis in a prospective comparison of clinical results between independent ESWT treatment and the US-guided shoulder injection.
The therapeutic mechanism of ESWT in tendinitis has not been precisely defined, although there are various theories. In the case of non-calcific shoulder tendinitis, the neovascularization and blood supply effects of ESWT exert an influence on pain and functional improvement, while a decompressive effect occurs in patients with calcific tendinitis.10,21) ESWT is also thought to inhibit persistent inflammatory reactions in soft tissues by inducing the repair of inflamed tissues and stimulating nitric oxide synthase.22) In this study, we used an energy level of about 0.15 mJ/mm2. Although the consensus on the criteria for dividing energy level is not clear, it can be classified as low or medium. Similar to this study, there was a study showing that ESWT of medium energy (0.11 mJ/mm2) was effective in the treatment of calcific tendinitis.23) Although opinions are divided on non-calcifying rotator cuff tendinitis, effective results of low-energy ESWT have been reported, which are consistent with the good results of this study.15,24)
In some studies, steroid injection has been more effective and cost-efficient than ESWT.25) In vitro studies have shown that in addition to anti-inflammatory effects, corticosteroids provide a therapeutic effect by inhibiting the production of collagen, extracellular matrix molecules, and granulation tissue.26) In addition, it is reported that corticosteroid injections are effective in pain relief and functional improvement in a short period of time (3 to 6 weeks).27,28) However, there are potential complications of steroid injections, including subcutaneous atrophy, transient hyperglycemia, infection, skin pigmentation, ruptured tendon, and risk of allergic reaction to local anesthetics. Topical administration of glucocorticoids has been reported to have significant negative effects on tendon cells in vitro through reduced cell survival, cell proliferation, and collagen synthesis.29) It was also reported that the mid-term and long-term effects after corticosteroid injections were not significant, and the results were similar to those of our study.30) Considering these disadvantages of corticosteroid injections, ESWT could be recommended as an alternative treatment because it can induce neovascularization and tissue regeneration.
The present study has several limitations. Firstly, the sample size was small. Although the G-power was used to compute the number of patients, a larger sample size would have led to more significant results in the equivalence testing. In the future, by designing a study with a larger sample size, we could compare and analyze a placebo group, a simultaneous injection group, and ESWT group, which was not possible in the present study. Secondly, the follow-up period was relatively short. While previous studies have also relied on an 8-week or 3-month follow-up, a year or more of long-term follow-up would have led to more reliable results. However, this would increase the possibility of increased patient dropout due to the rebound phenomenon of steroid injections. Lastly, the ESWT intervention was given only once. Had sequential intervention been carried out, superior results may have been obtained.
In conclusion, ESWT can be a safe and effective treatment for shoulder tendinitis. Furthermore, US-guided shoulder injections did not produce superior effects than independent ESWT treatment. Considering the complications and rebound phenomenon of steroid injections, ESWT treatment may be a good alternative in patients with supraspinatus tendinitis.
ACKNOWLEDGEMENTS
The authors would like to express gratitude to Ms. Su-Jin Jung (Kyung Hee University Medical Center, Seoul, Korea) for her technical assistance and contributions to the statistical analysis and Ik Yang, MD, PhD (Department of Radiology, Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea) for ultrasound examination and evaluation.
This research was supported by Hallym University Research Fund 2017 (HURF-2017-15).
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Littlewood C, May S, Walters S. Epidemiology of rotator cuff tendinopathy: a systematic review. Shoulder Elb. 2013;5(4):256–265. [Google Scholar]
- 2.Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014;23(12):1913–1921. doi: 10.1016/j.jse.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Karthikeyan S, Kwong HT, Upadhyay PK, Parsons N, Drew SJ, Griffin D. A double-blind randomised controlled study comparing subacromial injection of tenoxicam or methylprednisolone in patients with subacromial impingement. J Bone Joint Surg Br. 2010;92(1):77–82. doi: 10.1302/0301-620X.92B1.22137. [DOI] [PubMed] [Google Scholar]
- 4.Akbari N, Ozen S, Senlikci HB, Haberal M, Cetin N. Ultrasound-guided versus blind subacromial corticosteroid and local anesthetic injection in the treatment of subacromial impingement syndrome: a randomized study of efficacy. Jt Dis Relat Surg. 2020;31(1):115–122. doi: 10.5606/ehc.2020.71056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Roddy E, Zwierska I, Hay EM, et al. Subacromial impingement syndrome and pain: protocol for a randomised controlled trial of exercise and corticosteroid injection (the SUPPORT trial) BMC Musculoskelet Disord. 2014;15:81. doi: 10.1186/1471-2474-15-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rompe JD, Zoellner J, Nafe B. Shock wave therapy versus conventional surgery in the treatment of calcifying tendinitis of the shoulder. Clin Orthop Relat Res. 2001;(387):72–82. doi: 10.1097/00003086-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Aqil A, Siddiqui MR, Solan M, Redfern DJ, Gulati V, Cobb JP. Extracorporeal shock wave therapy is effective in treating chronic plantar fasciitis: a meta-analysis of RCTs. Clin Orthop Relat Res. 2013;471(11):3645–3652. doi: 10.1007/s11999-013-3132-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang CJ, Ko JY, Chan YS, Weng LH, Hsu SL. Extracorporeal shockwave for chronic patellar tendinopathy. Am J Sports Med. 2007;35(6):972–978. doi: 10.1177/0363546506298109. [DOI] [PubMed] [Google Scholar]
- 9.Gerdesmeyer L, Mittermayr R, Fuerst M, et al. Current evidence of extracorporeal shock wave therapy in chronic Achilles tendinopathy. Int J Surg. 2015;24(Pt B):154–159. doi: 10.1016/j.ijsu.2015.07.718. [DOI] [PubMed] [Google Scholar]
- 10.Wang CJ, Wang FS, Yang KD, et al. Shock wave therapy induces neovascularization at the tendon-bone junction: a study in rabbits. J Orthop Res. 2003;21(6):984–989. doi: 10.1016/S0736-0266(03)00104-9. [DOI] [PubMed] [Google Scholar]
- 11.Moya D, Ramon S, Schaden W, Wang CJ, Guiloff L, Cheng JH. The role of extracorporeal shockwave treatment in musculoskeletal disorders. J Bone Joint Surg Am. 2018;100(3):251–263. doi: 10.2106/JBJS.17.00661. [DOI] [PubMed] [Google Scholar]
- 12.Chen TW, Huei Su J, Lin TY, Lin CW, Chou PS, Huang MH. Effects of eccentric exercise and extracorporeal shock wave therapy on rehabilitation of patients with noncalcific rotator cuff tendinopathy. Clin Res Foot Ankle. 2017;5:222 [Google Scholar]
- 13.Mouzopoulos G, Stamatakos M, Mouzopoulos D, Tzurbakis M. Extracorporeal shock wave treatment for shoulder calcific tendonitis: a systematic review. Skeletal Radiol. 2007;36(9):803–811. doi: 10.1007/s00256-007-0297-3. [DOI] [PubMed] [Google Scholar]
- 14.Li W, Zhang SX, Yang Q, Li BL, Meng QG, Guo ZG. Effect of extracorporeal shock-wave therapy for treating patients with chronic rotator cuff tendonitis. Medicine (Baltimore) 2017;96(35):e7940. doi: 10.1097/MD.0000000000007940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Galasso O, Amelio E, Riccelli DA, Gasparini G. Short-term outcomes of extracorporeal shock wave therapy for the treatment of chronic non-calcific tendinopathy of the supraspinatus: a double-blind, randomized, placebo-controlled trial. BMC Musculoskelet Disord. 2012;13:86. doi: 10.1186/1471-2474-13-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu KT, Chou WY, Wang CJ, et al. Efficacy of extracorporeal shockwave therapy on calcified and noncalcified shoulder tendinosis: a propensity score matched analysis. Biomed Res Int. 2019;2019:2958251. doi: 10.1155/2019/2958251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Santamato A, Panza F, Notarnicola A, et al. Is extracorporeal shockwave therapy combined with isokinetic exercise more effective than extracorporeal shockwave therapy alone for subacromial impingement syndrome?: a randomized clinical trial. J Orthop Sports Phys Ther. 2016;46(9):714–725. doi: 10.2519/jospt.2016.4629. [DOI] [PubMed] [Google Scholar]
- 18.Frassanito P, Cavalieri C, Maestri R, Felicetti G. Effectiveness of extracorporeal shock wave therapy and kinesio taping in calcific tendinopathy of the shoulder: a randomized controlled trial. Eur J Phys Rehabil Med. 2018;54(3):333–340. doi: 10.23736/S1973-9087.17.04749-9. [DOI] [PubMed] [Google Scholar]
- 19.Circi E, Okur SC, Aksu O, Mumcuoglu E, Tuzuner T, Caglar N. The effectiveness of extracorporeal shockwave treatment in subacromial impingement syndrome and its relation with acromion morphology. Acta Orthop Traumatol Turc. 2018;52(1):17–21. doi: 10.1016/j.aott.2017.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kolk A, Yang KG, Tamminga R, van der Hoeven H. Radial extracorporeal shock-wave therapy in patients with chronic rotator cuff tendinitis: a prospective randomised double-blind placebo-controlled multicentre trial. Bone Joint J. 2013;95(11):1521–1526. doi: 10.1302/0301-620X.95B11.31879. [DOI] [PubMed] [Google Scholar]
- 21.Orhan Z, Ozturan K, Guven A, Cam K. The effect of extracorporeal shock waves on a rat model of injury to tendo Achillis: a histological and biomechanical study. J Bone Joint Surg Br. 2004;86(4):613–618. [PubMed] [Google Scholar]
- 22.Ciampa AR, de Prati AC, Amelio E, et al. Nitric oxide mediates anti-inflammatory action of extracorporeal shock waves. FEBS Lett. 2005;579(30):6839–6845. doi: 10.1016/j.febslet.2005.11.023. [DOI] [PubMed] [Google Scholar]
- 23.Moretti B, Garofalo R, Genco S, Patella V, Mouhsine E. Medium-energy shock wave therapy in the treatment of rotator cuff calcifying tendinitis. Knee Surg Sports Traumatol Arthrosc. 2005;13(5):405–410. doi: 10.1007/s00167-005-0619-8. [DOI] [PubMed] [Google Scholar]
- 24.Frizziero A, Vittadini F, Barazzuol M, et al. Extracorporeal shockwaves therapy versus hyaluronic acid injection for the treatment of painful non-calcific rotator cuff tendinopathies: preliminary results. J Sports Med Phys Fitness. 2017;57(9):1162–1168. doi: 10.23736/S0022-4707.16.06408-2. [DOI] [PubMed] [Google Scholar]
- 25.Crowther MA, Bannister GC, Huma H, Rooker GD. A prospective, randomized study to compare extracorporeal shock-wave therapy and injection of steroid for the treatment of tennis elbow. J Bone Joint Surg Br. 2002;84(5):678–679. doi: 10.1302/0301-620x.84b5.12741. [DOI] [PubMed] [Google Scholar]
- 26.Paavola M, Kannus P, Jarvinen TA, Jarvinen TL, Jozsa L, Jarvinen M. Treatment of tendon disorders: is there a role for corticosteroid injection? Foot Ankle Clin. 2002;7(3):501–513. doi: 10.1016/s1083-7515(02)00056-6. [DOI] [PubMed] [Google Scholar]
- 27.Coombes BK, Bisset L, Vicenzino B. Efficacy and safety of corticosteroid injections and other injections for management of tendinopathy: a systematic review of randomised controlled trials. Lancet. 2010;376(9754):1751–1767. doi: 10.1016/S0140-6736(10)61160-9. [DOI] [PubMed] [Google Scholar]
- 28.Mohamadi A, Chan JJ, Claessen FM, Ring D, Chen NC. Corticosteroid injections give small and transient pain relief in rotator cuff tendinosis: a meta-analysis. Clin Orthop Relat Res. 2017;475(1):232–243. doi: 10.1007/s11999-016-5002-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dean BJ, Lostis E, Oakley T, Rombach I, Morrey ME, Carr AJ. The risks and benefits of glucocorticoid treatment for tendinopathy: a systematic review of the effects of local glucocorticoid on tendon. Semin Arthritis Rheum. 2014;43(4):570–576. doi: 10.1016/j.semarthrit.2013.08.006. [DOI] [PubMed] [Google Scholar]
- 30.Lin MT, Chiang CF, Wu CH, Huang YT, Tu YK, Wang TG. Comparative effectiveness of injection therapies in rotator cuff tendinopathy: a systematic review, pairwise and network meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2019;100(2):336–349. doi: 10.1016/j.apmr.2018.06.028. [DOI] [PubMed] [Google Scholar]