Abstract
Background
Osteonecrosis of the femoral head (ONFH) involves young or middle-aged adults, and its incidence is increasing along with increasing use of steroids in the management of organ transplantation and adjuvant therapy for malignant neoplasms. To date, no pharmacological agent has been proven to prevent or retard the progression of ONFH, and surgical procedures including joint preservation procedures and hip arthroplasties are main treatments for the disease. Although ONFH is the most common or second most common disease for hip arthroplasty in East Asian countries, the trend of surgical procedures in this region remains unknown. Thus, we evaluated trends in surgical treatment of the disease in South Korea.
Methods
We identified patients with ONFH from the Korean Health Insurance Review and Assessment (HIRA) database, a nationwide medical claims database of South Korea, between January 2007 and December 2018 and calculated the proportions of following surgical procedures at each year: total hip arthroplasty (THA), hemiarthroplasty (HA), core decompression/multiple drilling, femoral osteotomy, and vascularized bone grafting.
Results
The total number of procedures increased from 3,824 in 2007 to 6,929 in 2018. Overall, the rate of THA (86%) was far greater than other procedures. From 2007 to 2018, the percentage of THA among the procedures increased from 80% to 91%, while that of joint preservation procedures decreased from 11% to 5%.
Conclusions
The total number of surgical procedures performed for ONFH increased and the percentage of THA increased, while that of joint preservation procedures decreased from 2007 to 2018 in South Korea.
Keywords: Hip, Osteonecrosis, Avascular necrosis, Therapy, Trends
Osteonecrosis of the femoral head (ONFH) is a disease that frequently leads to collapse of the femoral head and subsequent arthritis of the hip. In the United States, the annual incidence of the disease was reported to be 15,000 to 20,000.1,2) In East Asian countries, it is the most common or second most common disease for hip arthroplasty. More than 10,000 patients are affected by the disease yearly in South Korea, and the annual incidence rate is 1.91/100,000 in Japan.3,4) Most ONFH patients in an advanced stage eventually necessitate total hip arthroplasties (THAs). The disease accounts for more than 10% of the overall THAs in the United States5) and around 50% in East Asia and sub-Saharan Africa.6,7,8)
The etiology of ONFH is multifactorial including genetic predispositions, as well as exposure to risk factors. Hereditary thrombophilia/hypofibrinolysis and impaired angiogenesis have been known to be implicated in the pathogenesis of the disease.9) Two of the most common risk factors are the use of steroids and excessive alcohol consumption.10,11) Various medical and surgical treatment options have been implemented based on the pathogenic mechanism. Even though several pharmacological agents such as bisphosphonates, enoxaparin, statins, iloprost, and acetylsalicylic acid have been adopted to alleviate the progression of ONFH,12,13,14,15,16,17) none of them was proven to be effective by high level of evidence.
Operative treatments include (1) joint preservation procedures such as core decompression, multiple drilling, vascularized bone grafting, and proximal femoral osteotomies and (2) hip arthroplasties such as THA and hemiarthroplasty (HA). The joint preservation procedures are tried in early stages of ONFH while patients in an advanced stage are mainly treated with hip arthroplasties. Several studies have reported trends in surgical treatment of ONFH in the United States.18,19) Nevertheless, there is a lack of study reporting the trends in East Asia, where the disease is the leading cause of hip arthroplasties. The purpose of this study was to reveal the trends in surgical treatment of ONFH in South Korea using nationwide medical claims database.
METHODS
The present study was exempted from institutional review board approval because it did not involve human subjects (Seoul National University Bundang Hospital, No. X-1911-579-904). The board approved waiver of informed consent to participate in view of the retrospective nature of the study. The participants consented to the submission of this article to the journal.
Database
The Korean Health Insurance Review and Assessment (HIRA) database was used in this registry study. Ninety-seven percent of Korean citizens are covered by the Korea National Health Insurance Program (KNHIP), while the remaining 3% are supported by the South Korean government through a medical aid program. Medical data from both the KNHIP and the medical aid program are submitted to HIRA for reimbursement. Medical information including patient demographics, diagnoses, procedures, and prescriptions stratified by International Classification of Diseases-10 (ICD-10) codes and Electronic Data Interchange codes is available through the HIRA database.
Statistical Analysis
Patients who were admitted due to ONFH from January 2007 to December 2018 were identified via ICD diagnosis codes (M8705, M8715, M8725, M8735, M8785, M8795, M9035, M9045, and M9055). Patients younger than 20 years were excluded because the disease is very rare in this population.1,2) Then, the procedural codes to treat ONFH patients were analyzed. The annual number of each procedure and its crude incidence (the procedural number/year-specific population) were calculated. The annual population data of South Korea were obtained from the Korean Statistical Information Service. Age-adjusted procedural data were obtained from men and women separately. Data analysis was carried out using R software (version 3.5.3; R Foundation, Vienna, Austria). Fisher’s exact test was used to compare proportional differences between various groups. Probability values of 0.05 were considered significant for all analyses.
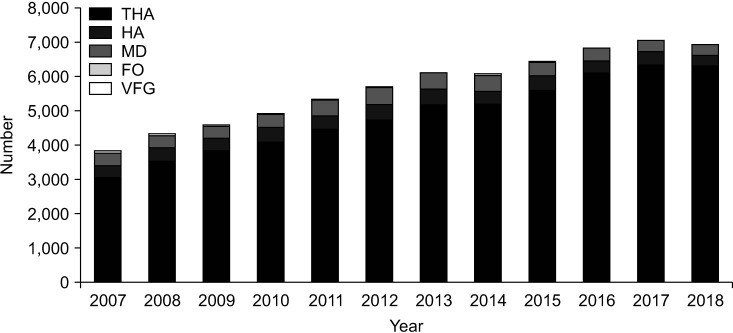
RESULTS
Procedures for ONFH during the study period were THA (N0711, N2070), HA (N0715, N2710), multiple drilling (N0021), femoral osteotomy (N0302, N0305), and vascularized fibular grafting (VFG; N1583, N1584, N1585). The total number of patients who underwent those procedures from 2007 to 2018 was 68,085. The annual number of total procedures increased from 3,824 in 2007 to 6,929 in 2018. The most common procedure was THA (86%), followed by multiple drilling, HA, femoral osteotomy, and VFG. The percentage of THA among all procedures increased from 80% to 91%, while that of joint preservation procedures decreased from 11% to 5% (Table 1, Fig. 1).
Table 1. Number of Procedures Performed on ONFH from 2007 to 2018 in South Korea.
| Procedure | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| THA | 3,058 | 3,516 | 3,829 | 4,094 | 4,473 | 4,736 | 5,198 | 5,194 | 5,612 | 6,106 | 6,354 | 6,305 |
| MD | 361 | 358 | 360 | 369 | 461 | 489 | 474 | 477 | 386 | 359 | 318 | 308 |
| HA | 339 | 400 | 364 | 425 | 378 | 452 | 430 | 369 | 408 | 346 | 374 | 306 |
| FO | 46 | 40 | 19 | 17 | 19 | 15 | 11 | 14 | 9 | 11 | 6 | 10 |
| VFG | 20 | 9 | 7 | 9 | 5 | 5 | 3 | 9 | 4 | 8 | 3 | 0 |
| Total | 3,824 | 4,323 | 4,579 | 4,914 | 5,336 | 5,697 | 6,116 | 6,063 | 6,419 | 6,830 | 7,055 | 6,929 |
ONFH: osteonecrosis of the femoral head, THA: total hip arthroplasty, MD: multiple drilling, HA: hemiarthroplasty, FO: femoral osteotomy, VFG: vascularized fibular graft.
Fig. 1. Annual number of procedures for osteonecrosis of the femoral head from 2007 to 2018 in South Korea. THA: total hip arthroplasty, HA: hemiarthroplasty, MD: multiple drilling, FO: femoral osteotomy, VFG: vascularized fibular graft.
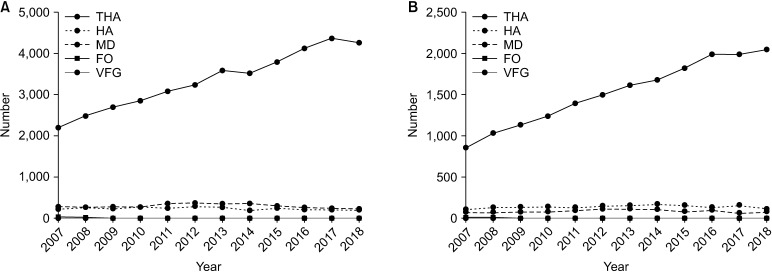
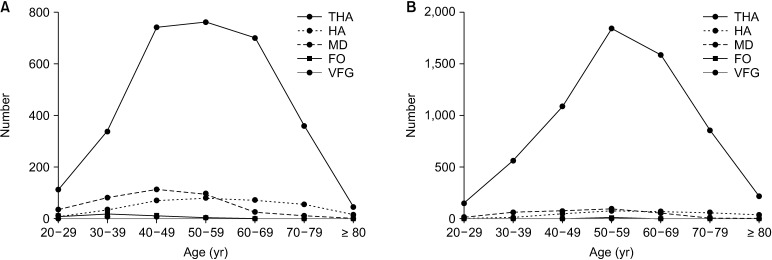
Male preponderance was found in all of the five procedures and the mean age of the patients at the time of procedure was 55.5 ± 14.3 years (range, 20–99 years). Patients undergoing HA or THA were older than those undergoing multiple drilling, femoral osteotomy, or VFG (Table 2). During the study period from 2007 to 2018, the number of THAs nearly doubled, while the numbers of HAs and multiple drillings did not change significantly and the numbers of femoral osteotomies and VFGs decreased (Fig. 2).
Table 2. Sex and Age of Patients Who Underwent Surgery for ONFH between 2007 and 2018.
| Surgery | THA | HA | FO | VFG | MD | |
|---|---|---|---|---|---|---|
| Total number | 58,475 (86) | 4,591 (7) | 217 (0.3) | 82 (0.1) | 4,720 (7) | |
| Sex | ||||||
| Female | 18,263 | 1,707 | 49 | 15 | 1,077 | |
| Male | 40,212 | 2,884 | 168 | 67 | 3,643 | |
| Age (yr) | ||||||
| Mean ± SD | 55.4 ± 13.2 | 59.5 ± 14.3 | 40.8 ± 13.1 | 37.7 ± 8.4 | 47.4 ± 11.9 | |
| Range | 20–98 | 20–95 | 20–83 | 20–61 | 20–92 | |
| Age group (yr) | ||||||
| 20–29 | 1,601 | 65 | 51 | 15 | 322 | |
| 30–39 | 5,839 | 335 | 56 | 33 | 966 | |
| 40–49 | 11,652 | 811 | 51 | 29 | 1,380 | |
| 50–59 | 16,893 | 1,097 | 41 | 4 | 1,342 | |
| 60–69 | 13,060 | 978 | 14 | 1 | 553 | |
| 70–79 | 8,038 | 957 | 3 | 0 | 140 | |
| ≥ 80 | 1,392 | 348 | 1 | 0 | 17 | |
ONFH: osteonecrosis of the femoral head, THA: total hip arthroplasty, HA: hemiarthroplasty, FO: femoral osteotomy, VFG: vascularized fibular graft, MD: multiple drilling, SD: standard deviation.
Fig. 2. Annual number of procedures for osteonecrosis of the femoral head in men (A) and women (B) from 2007 to 2018. THA: total hip arthroplasty, HA: hemiarthroplasty, MD: multiple drilling, FO: femoral osteotomy, VFG: vascularized fibular graft.
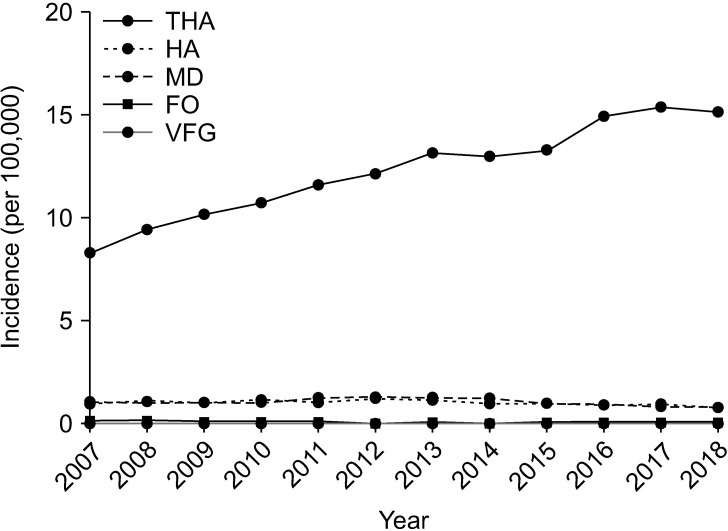
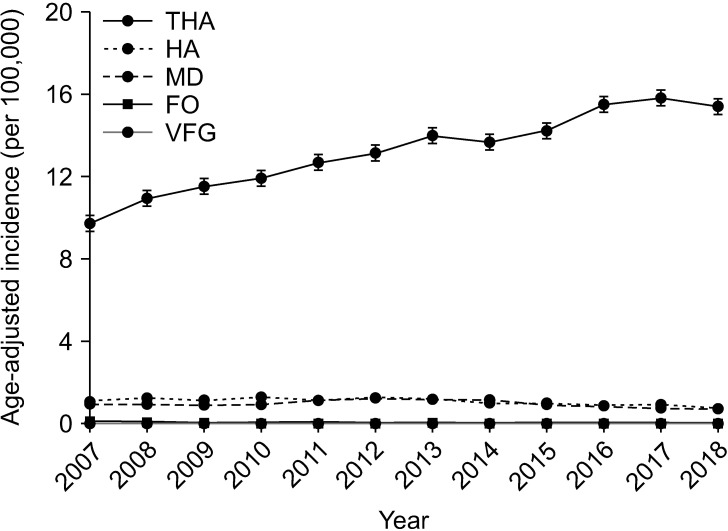
The crude incidence of THA increased (p < 0.001), while that of other procedures decreased during the study period (Fig. 3). This trend did not change even after age adjustment (Fig. 4). The most common age group undergoing THA or HA was 50–59 years, while joint preservation procedures were done in younger patients. VFG was not performed at all in 2018 (Fig. 5).
Fig. 3. Annual crude incidence of procedures (per 100,000 persons) for osteonecrosis of the femoral head in South Korea. THA: total hip arthroplasty, HA: hemiarthroplasty, MD: multiple drilling, FO: femoral osteotomy, VFG: vascularized fibular graft.
Fig. 4. Annual age-adjusted rate of procedures (per 100,000 persons) for osteonecrosis of the femoral head in South Korea. THA: total hip arthroplasty, HA: hemiarthroplasty, MD: multiple drilling, FO: femoral osteotomy, VFG: vascularized fibular graft.
Fig. 5. The number of procedures for osteonecrosis of the femoral head by age group in 2007 (A) and 2018 (B). THA: total hip arthroplasty, HA: hemiarthroplasty, MD: multiple drilling, FO: femoral osteotomy, VFG: vascularized fibular graft.
DISCUSSION
Our study showed that the total number of procedures performed for ONFH nearly doubled from 3,824 to 6,929, and the proportion of THA increased from 80% (3,058/3,824) to 91% (6,305/6,929), while that of joint preservation procedures decreased from 11% to 5% during the period from 2007 to 2018 in South Korea. Similar trends were found in the United States. In a registry study using Nationwide Inpatient Sample data between 1992 and 2008, Johnson et al.18) reported that the number of total procedures for ONFH increased twice and the percentage of THA increased from 76% to 88%, while that of joint preservation procedures decreased from 25% to 12%. A Japanese multicenter study showed a twofold increase in the number of THA and approximately 45% decrease in that of osteotomy between 2003 and 2017.20)
The growing proportion of THA in the treatment of the disease is due to excellent outcome and survivorship of THAs using durable bearing surfaces of contemporary ceramic composites or highly cross-linked polyethylene.21,22,23,24) Mid- to long-term studies of THAs using these bearings showed over 95% survival rates and excellent functional outcomes.21,22,25,26,27) In our study, the proportion of joint preservation procedures decreased by more than 50% during the study period.
The criteria for choosing surgical procedures are mainly based on the size, location, and collapse of the ONFH lesion. Core decompression and multiple drilling have been used in early-stage (pre-collapse) ONFH with the assumption that it prevents or reverses the disease progression. Recently, injection of bone marrow aspirate concentration is used to improve results.28) However, the results of these procedures were not consistent, and the effectiveness was questioned.29) Femoral osteotomies and vascularized bone grafts are criticized due to the technical difficulties and unfavorable outcomes.30)
Our study was based on HIRA data, which has inherent limitations due to de-identification and lack of detailed information. Erroneous coding might have compromised the accuracy of the database study. However, the strength of this study is that it covers nearly 100% of all procedures for ONFH in South Korea. Furthermore, as the counted event in the analysis was the surgery rather than the patient, there were duplications such as bilateral operations or multiple operations such as prior multiple drilling and subsequent THA.
In conclusion, the number of surgical procedures for ONFH markedly increased from 2007 to 2018 in South Korea. THA accounted for 86% and nearly doubled in number, while the percentage of joint preservation procedures decreased from 11% to 5% during the period.
ACKNOWLEDGEMENTS
This research was supported by a grant (No. 02-2021-0025) from the Seoul National University Bundang Hospital Research Fund.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am. 1995;77(3):459–474. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 2.Moya-Angeler J, Gianakos AL, Villa JC, Ni A, Lane JM. Current concepts on osteonecrosis of the femoral head. World J Orthop. 2015;6(8):590–601. doi: 10.5312/wjo.v6.i8.590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ikeuchi K, Hasegawa Y, Seki T, Takegami Y, Amano T, Ishiguro N. Epidemiology of nontraumatic osteonecrosis of the femoral head in Japan. Mod Rheumatol. 2015;25(2):278–281. doi: 10.3109/14397595.2014.932038. [DOI] [PubMed] [Google Scholar]
- 4.Kang JS, Park S, Song JH, Jung YY, Cho MR, Rhyu KH. Prevalence of osteonecrosis of the femoral head: a nationwide epidemiologic analysis in Korea. J Arthroplast. 2009;24(8):1178–1183. doi: 10.1016/j.arth.2009.05.022. [DOI] [PubMed] [Google Scholar]
- 5.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis) N Engl J Med. 1992;326(22):1473–1479. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 6.Chan VW, Chan PK, Chiu KY, Yan CH, Ng FY. Why do Hong Kong patients need total hip arthroplasty?: an analysis of 512 hips from 1998 to 2010. Hong Kong Med J. 2016;22(1):11–15. doi: 10.12809/hkmj144483. [DOI] [PubMed] [Google Scholar]
- 7.Lai YS, Wei HW, Cheng CK. Incidence of hip replacement among national health insurance enrollees in Taiwan. J Orthop Surg Res. 2008;3:42. doi: 10.1186/1749-799X-3-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lubega N, Mkandawire NC, Sibande GC, Norrish AR, Harrison WJ. Joint replacement in Malawi: establishment of a National Joint Registry. J Bone Joint Surg Br. 2009;91(3):341–343. doi: 10.1302/0301-620X.91B3.21706. [DOI] [PubMed] [Google Scholar]
- 9.Glueck CJ, Freiberg R, Tracy T, Stroop D, Wang P. Thrombophilia and hypofibrinolysis: pathophysiologies of osteonecrosis. Clin Orthop Relat Res. 1997;(334):43–56. [PubMed] [Google Scholar]
- 10.Yoon BH, Jones LC, Chen CH, et al. Etiologic classification criteria of ARCO on femoral head osteonecrosis part 2: alcohol-associated osteonecrosis. J Arthroplasty. 2019;34(1):169–174. doi: 10.1016/j.arth.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 11.Yoon BH, Jones LC, Chen CH, et al. Etiologic classification criteria of ARCO on femoral head osteonecrosis part 1: glucocorticoid-associated osteonecrosis. J Arthroplasty. 2019;34(1):163–168. doi: 10.1016/j.arth.2018.09.005. [DOI] [PubMed] [Google Scholar]
- 12.Ajmal M, Matas AJ, Kuskowski M, Cheng EY. Does statin usage reduce the risk of corticosteroid-related osteonecrosis in renal transplant population? Orthop Clin North Am. 2009;40(2):235–239. doi: 10.1016/j.ocl.2009.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Albers A, Carli A, Routy B, Harvey EJ, Seguin C. Treatment with acetylsalicylic acid prevents short to mid-term radiographic progression of nontraumatic osteonecrosis of the femoral head: a pilot study. Can J Surg. 2015;58(3):198–205. doi: 10.1503/cjs.016814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen CH, Chang JK, Lai KA, Hou SM, Chang CH, Wang GJ. Alendronate in the prevention of collapse of the femoral head in nontraumatic osteonecrosis: a two-year multicenter, prospective, randomized, double-blind, placebo-controlled study. Arthritis Rheum. 2012;64(5):1572–1578. doi: 10.1002/art.33498. [DOI] [PubMed] [Google Scholar]
- 15.Classen T, Becker A, Landgraeber S, et al. Long-term clinical results after iloprost treatment for bone marrow edema and avascular necrosis. Orthop Rev (Pavia) 2016;8(1):6150. doi: 10.4081/or.2016.6150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Glueck CJ, Freiberg RA, Sieve L, Wang P. Enoxaparin prevents progression of stages I and II osteonecrosis of the hip. Clin Orthop Relat Res. 2005;(435):164–170. doi: 10.1097/01.blo.0000157539.67567.03. [DOI] [PubMed] [Google Scholar]
- 17.Lee YK, Ha YC, Cho YJ, et al. Does zoledronate prevent femoral head collapse from osteonecrosis?: a prospective, randomized, open-label, multicenter study. J Bone Joint Surg Am. 2015;97(14):1142–1148. doi: 10.2106/JBJS.N.01157. [DOI] [PubMed] [Google Scholar]
- 18.Johnson AJ, Mont MA, Tsao AK, Jones LC. Treatment of femoral head osteonecrosis in the United States: 16-year analysis of the Nationwide Inpatient Sample. Clin Orthop Relat Res. 2014;472(2):617–623. doi: 10.1007/s11999-013-3220-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sodhi N, Acuna A, Etcheson J, et al. Management of osteonecrosis of the femoral head. Bone Joint J. 2020;102-B(7_Supple_B):122–128. doi: 10.1302/0301-620X.102B7.BJJ-2019-1611.R1. [DOI] [PubMed] [Google Scholar]
- 20.Kaneko S, Takegami Y, Seki T, et al. Surgery trends for osteonecrosis of the femoral head: a fifteen-year multi-centre study in Japan. Int Orthop. 2020;44(4):761–769. doi: 10.1007/s00264-020-04480-6. [DOI] [PubMed] [Google Scholar]
- 21.Carli AV, Patel AR, Cross MB, et al. Long-term performance of oxidized zirconium on conventional and highly cross-linked polyethylene in total hip arthroplasty. SICOT J. 2020;6:10. doi: 10.1051/sicotj/2020010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hart A, Janz V, Trousdale RT, Sierra RJ, Berry DJ, Abdel MP. Long-term survivorship of total hip arthroplasty with highly cross-linked polyethylene for osteonecrosis. J Bone Joint Surg Am. 2019;101(17):1563–1568. doi: 10.2106/JBJS.18.01218. [DOI] [PubMed] [Google Scholar]
- 23.Lee YK, Ha YC, Yoo JI, Jo WL, Kim KC, Koo KH. Mid-term results of the BIOLOX delta ceramic-on-ceramic total hip arthroplasty. Bone Joint J. 2017;99(6):741–748. doi: 10.1302/0301-620X.99B6.BJJ-2016-0486.R3. [DOI] [PubMed] [Google Scholar]
- 24.Solarino G, Zagra L, Piazzolla A, Morizio A, Vicenti G, Moretti B. Results of 200 consecutive ceramic-on-ceramic cementless hip arthroplasties in patients up to 50 years of age: a 5-24 years of follow-up study. J Arthroplasty. 2019;34(7S):S232–S237. doi: 10.1016/j.arth.2019.01.057. [DOI] [PubMed] [Google Scholar]
- 25.Bergvinsson H, Zampelis V, Sundberg M, Flivik G. Highly cross-linked polyethylene still outperforms conventional polyethylene in THA: 10-year RSA results. Acta Orthop. 2021;92(5):568–574. doi: 10.1080/17453674.2021.1932140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.D’Antonio JA, Capello WN, Naughton M. High survivorship with a titanium-encased alumina ceramic bearing for total hip arthroplasty. Clin Orthop Relat Res. 2014;472(2):611–616. doi: 10.1007/s11999-013-2943-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yoo JI, Ha YC, Kim DH, Lee YK, Koo KH. Total hip arthroplasty using hybrid ceramic bearing: a minimum 10-year followup study. Indian J Orthop. 2019;53(5):637–640. doi: 10.4103/ortho.IJOrtho_416_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernigou P, Dubory A, Homma Y, et al. Cell therapy versus simultaneous contralateral decompression in symptomatic corticosteroid osteonecrosis: a thirty year follow-up prospective randomized study of one hundred and twenty five adult patients. Int Orthop. 2018;42(7):1639–1649. doi: 10.1007/s00264-018-3941-8. [DOI] [PubMed] [Google Scholar]
- 29.Yoon BH, Lee YK, Kim KC, Ha YC, Koo KH. No differences in the efficacy among various core decompression modalities and non-operative treatment: a network meta-analysis. Int Orthop. 2018;42(12):2737–2743. doi: 10.1007/s00264-018-3977-9. [DOI] [PubMed] [Google Scholar]
- 30.Hines JT, Jo WL, Cui Q, et al. Osteonecrosis of the femoral head: an updated review of ARCO on pathogenesis, staging and treatment. J Korean Med Sci. 2021;36(24):e177. doi: 10.3346/jkms.2021.36.e177. [DOI] [PMC free article] [PubMed] [Google Scholar]