Abstract
Background
During the SARS-CoV-2 global pandemic, one of the longest lockdowns worldwide occurred in Ontario, Canada, during the first wave. For parents and children managing care at home and at risk for COVID-19, the impact on their psychosocial functioning is unknown.
Methods
A total of 122 families of children aged 2–18 years were enrolled as part of the prospective cohort of childhood nephrotic syndrome and completed a survey during the first wave of the pandemic (August 21–December 10), 2020. In a subset, 107 families had data available pre-pandemic to assess change. Validated measures included the McMaster Family Assessment Device (FAD) for parents and children ≥ 12 years for family functioning, the Patient Health Questionnaire for Depression and Anxiety (PHQ-4) for both parent and child, and Pediatric Quality of Life Inventory (PEDSQL™-V4) for children only. Scores were compared using Student’s t-test or the Mann–Whitney U test, as appropriate.
Results
Among the 107 children, 71% were male with a mean age of 9 years old at the time of questionnaire completion, and the mean age of parents was 41 years old. Parents and children reported that family functioning improved during COVID (parent: p < 0.01; child: p = 0.05). Children’s overall HRQOL declined (p = 0.04), specifically increased sleep disruption (p = 0.01). Increasing child age was associated with a greater sleep disruption (β = − 1.6 [IQR: − 2.6, − 0.67]) and a related decrease in QOL (β = − 1.0 [IQR: − 1.7, − 0.2]), adjusted for sex.
Conclusions
Despite the positive effects of family dynamics during the first wave, there were negative effects of sleep disruptions and reduced quality of life in children, especially among older children.
Graphical abstract
A higher resolution version of the Graphical abstract is available as Supplementary information
Supplementary Information
The online version contains supplementary material available at 10.1007/s00467-022-05809-6.
Keywords: Nephrotic syndrome, Chronic disease, Well-being, Quality of life, COVID-19, Family functioning
Introduction
In March 2020, the World Health Organization declared a global pandemic of the novel virus, severe acute respiratory syndrome coronavirus (SARS-CoV-2) [1]. During the first wave of the global pandemic, the province of Ontario, Canada, was under 5 months of lockdown with a slow opening through the recovery phase. This time of crisis led to significant stress for people with months of lockdown, isolation, school closures, and strict social distancing measures in place [2–4].
Children with nephrotic syndrome are more susceptible to infections due to the underlying condition as well as the use of immunosuppressives and are more likely to experience relapse episodes during infection [5]. The susceptibility to infection and relapses increased the fears and uncertainty if exposed to COVID-19 infection. Empirical clinical guidelines and recommendations were available for the pandemic care of children with glomerular diseases [5]. Therefore, we aimed to explore the impact of COVID-19 on parental stress and family functioning in children with nephrotic syndrome [6, 7].
Although several studies have assessed the well-being of children and their caregivers during the pandemic, there are limited data on the mental, physical, and family well-being of both parents and children with a chronic disease, such as nephrotic syndrome, potentially at risk for COVID-19 [3, 6, 7]. Among children with nephrotic syndrome, health-related quality of life (HRQOL) is consistently decreased compared to healthy children or for those on steroids or steroid-sparing agents [8]. Thus, we wanted to assess if children’s mental health status, fatigue, and parental well-being worsened during the pandemic [8]. This study is designed to understand the family functioning and parental and child quality of life during the pandemic compared to pre-pandemic assessment.
Methods
Study design and population
Insight into Nephrotic Syndrome: Investigating Genes, Health, and Therapeutics (INSIGHT) is a prospective cohort study of children with nephrotic syndrome, ages 6 months–18 years, conducted at the Hospital for Sick Children in Toronto, Ontario, approved by the Research Ethics Board (ClinicalTrials.gov Identifier: NCT01605266)[9]. Per protocol, families complete questionnaires at baseline and annual follow-ups using the same validated measures of well-being as used in this study [9]. Among the recruited children in INSIGHT, 122 families completed a survey to assess parental and child well-being during the first wave of the COVID-19 pandemic from August 21 to December 10, 2020. In a subset (n = 107 families), we compared the available pre-pandemic data prior to February 29, 2020, and assessed the changes during the pandemic. Questionnaires were completed by emails, phone calls, or during clinic visits.
Outcomes
Validated measures of well-being for parents included the General Functioning Scale of the FAD and PHQ-4 [10, 11]. A validated measure of well-being in children included the age-specific PEDSQL™-V4 [12].
Family functioning
The general functioning subscale of family assessment is a 12-item parent-report scale that measures family functioning. The scale is composed of six positive items that assess healthy family functioning and six items that assess unhealthy functioning [10]. Scoring for each of the items is on a 4-point Likert scale ranging from 1 = strongly agree to 4 = strongly disagree, with the scale for negatively worded items reversed, and the total score is divided by the number of items to provide a score ranging from 1.00 to 4.00, with a cut-off score of < 2.00 indicating better family functioning. Children ≥ 12 years also completed the McMaster Family Assessment Device [10].
Parental anxiety and depression
The PHQ-4 is a 4-item composite screening tool for assessing anxiety and depression in parents [11]. Parents were asked to rate their frequency of 2-item anxiety and 2-item depressive symptoms over the past 2 weeks on a 4-point Likert scale (0–3; 0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day). A cut-off score of ≥ 3 in each anxiety or depression category was used for an indication of mental health conditions [11].
Health-related quality of life in children
The PEDSQL™-V4 is a 41-item parent report or self-report measure that assesses children’s HRQOL and fatigue for the past 1 month [12]. It is composed of a 23-item generic core scale comprising physical functioning (8 items), emotional functioning (5 items), social functioning (5 items), and school functioning (5 items), and an 18-item multidimensional fatigue scale comprising three 6-item domains of general fatigue, sleep/rest fatigue, and cognitive fatigue [12]. Responses were recorded on a 5-point Likert scale (0–4; 0 = not at all a problem; 4 = almost always a problem), and items on each domain are reverse scored and transformed to a scale of 0–100 (0 = 100, 1 = 75, 2 = 50, 3 = 25, and 4 = 0), with higher scores indicating better HRQOL and lower fatigue symptoms [12]. For reference, healthy children have a mean score of 83 ± 15.40 [13]. The school functioning domain is not administered during the summer months as per standard protocol.
Data analyses
Parent and child characteristics were summarized using descriptive statistics, and well-being scores were compared pre- and post-COVID-19 outbreak using the Student’s t-test or the Mann–Whitney U test, as appropriate. We examined the association of demographic characteristics with PEDSQL scores that were found to be statistically different by t-test or Mann–Whitney U test using linear regression.
Results
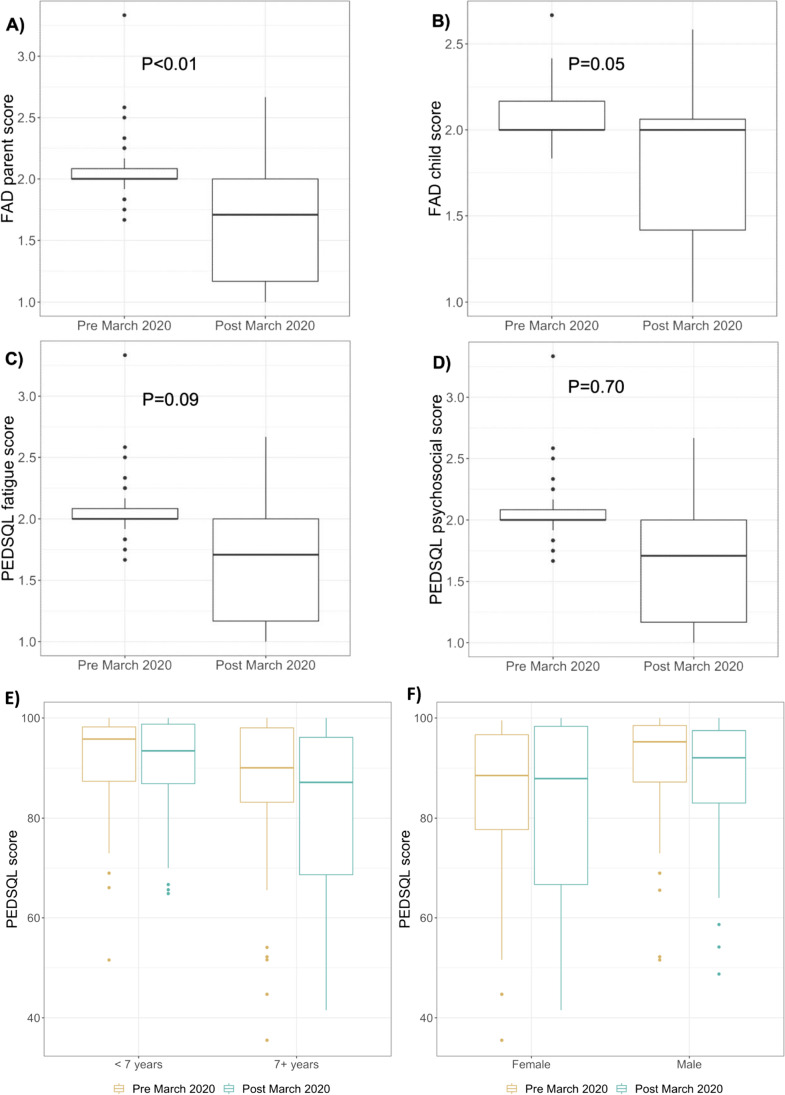
Among the 107 children, 71% were male; the median age at diagnosis was 3.4 years old, and the mean age at survey completion was 9 years old (Supplementary Table S1). Among the parents (n = 107), 77% were employed, and the mean parental age was 41 years old. The median time between the annual questionnaire completed before the pandemic and the COVID-19 survey during the pandemic was 16.9 months. Parents and children reported that family functioning during COVID improved (Fig. 1A and B) compared with pre-COVID (parent 2.03 ± 0.19 vs. 1.65 ± 0.45; p < 0.01; child 2.10 ± 0.21 vs. 1.80 ± 045; p = 0.05). There was no difference in family functioning by age or sex of children. The parent’s depression and anxiety level were affected during COVID but did not show any significant difference.
Fig. 1.
Assessment of family functioning and quality of life before and during wave 1 of the pandemic. Family functioning was assessed by the General Functioning Scale of McMaster Family Assessment Device by parents (A) and children ≥ 12 years (B), with a cut-off score of < 2.00 indicating better family functioning. Quality of life was assessed in children by total PEDSQL fatigue score (C) and PEDSQL psychosocial summary score (D). The total fatigue score is calculated as the mean of all the domains in the multidimensional fatigue scale, and the PEDSQL psychosocial summary is the mean of emotional, social, and school functioning domains. Quality of life assessed in children by total PEDSQL scores by age (E) and by sex (F) of children
Children’s overall HRQOL declined (p = 0.04), specifically increased sleep disruption and decreased energy (p = 0.01) during the pandemic. All other domains were stable across study time points. The total fatigue score (p = 0.09) and psychosocial summary score (p = 0.70) did not show any significant difference (Fig. 1, panels C and D), regardless of medication status (Supplementary Table S2). Further analysis showed that increasing child age was associated with greater sleep disruption (β = − 1.6 [IQR: − 2.6, − 0.67]) and a decrease in overall QOL (β = − 1.0 [IQR: − 1.7, − 0.2]), adjusted for sex.
Discussion
Our results highlight that family functioning improved in families with childhood nephrotic syndrome during the first wave in Ontario, in contrast to pre-pandemic assessment, with no significant change in parental anxiety and depression level. The pandemic, however, did impact the overall quality of life in children, with significant sleep disruption, especially among older children.
Improved family dynamics and cohesion, as reported by families and older children, could perhaps be attributed to families spending more time at home together, engaging in family activities, and better communication [14]. These results presented are supported by comments made in the survey by participating families, such as “It is been summer holidays for us, so our family has had a very positive time this last 2 months.” Although parental mental health status has been negatively impacted during the pandemic, as reported in several studies, our study does not show any significant levels of parental stress and anxiety [6].
Overall HRQOL had significantly declined in children, although no physical or psychosocial domains other than sleep fatigue were significantly impacted over the pandemic with lockdown measures in place. This adds to the existing evidence of already reduced scores in HRQOL in children with nephrotic syndrome receiving steroid and steroid-sparing treatments [8]. We demonstrated that children experience greater sleep disruption, related to difficulty maintaining sleep, daytime tiredness, spending more time in bed, and decreased energy, possibly in the context of loss of routines, reduced outdoor activities, virtual schooling, more screen time, and fear of COVID-19 infection [15]. We specifically found that decreased HRQOL and sleep disruption are seen more among older children, which could be related to stress, change in routine, and increased screen time [15].
Single parent–reported responses, a small sample size of a selected group of participants, limited online survey completion, and reporting bias are some limitations of this study. Nonetheless, the study results give a unique opportunity to highlight the importance of studying both the potential positive impact on family functioning as well as negative impacts on the overall quality of life and sleep disruption during the pandemic.
Our results highlight the need to develop effective strategies to improve the overall mental health and well-being of both children with nephrotic syndrome and their parents.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the participants and their families for their time and effort, as well as the nurses and staff from the Nephrology Clinic at The Hospital for Sick Children.
Author contribution
Nowrin F. Aman conceptualized and designed the study, collected data, drafted the initial manuscript, interpreted the data, and critically reviewed and revised the manuscript. Jessica Fitzpatrick-Collins carried out the data analyses and critically reviewed and revised the manuscript. Isabel de Verteuil conceptualized and designed the study, designed the data collection instruments, collected data, carried out the initial analyses, and critically reviewed and revised the manuscript. Jovanka Vasilevska-Ristovska conceptualized and designed the study, designed the data collection instruments, interpreted the data, and critically reviewed and revised the manuscript. Tonny Hue Minh Banh designed the data collection instruments, analyzed the data, interpreted the data, and critically reviewed and revised the manuscript. Daphne J Korczak conceptualized and designed the study, coordinated and supervised data collection, interpreted the data, and critically reviewed the manuscript for important intellectual content. Rulan S. Parekh conceptualized and designed the study, coordinated and supervised data collection, interpreted the data, and critically reviewed and revised the manuscript for important intellectual content. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics approval
The questionnaire and methodology for this study were approved by the Research Ethics Board of the Hospital for Sick Children, in Toronto, Ontario (ethics approval number: 1000021384).
Consent to participate
Informed consent was obtained from all parents/legal guardians of individual participants included in the study.
Consent for publication
The authors affirm that human research participants provided informed consent for the publication of the data.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.World Health Organization (WHO) (2020) Coronavirus disease (COVID-2019) situation reports. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports. Accessed July 14, 2020
- 2.Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, Rubin GJ. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fegert JM, Vitiello B, Plener PL, Clemens V. Challenges and burden of the Coronavirus 2019 (COVID-19) pandemic for child and adolescent mental health: a narrative review to highlight clinical and research needs in the acute phase and the long return to normality. Child Adolesc Psychiatry Ment Health. 2020;14:20. doi: 10.1186/s13034-020-00329-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Viner R, Russell S, Saulle R, Croker H, Stansfield C, Packer J, Nicholls D, Goddings AL, Bonell C, Hudson L, Hope S, Ward J, Schwalbe N, Morgan A, Minozzi S. School closures during social lockdown and mental health, health behaviors, and well-being among children and adolescents during the first COVID-19 wave: a systematic review. JAMA Pediatr. 2022;176:400–409. doi: 10.1001/jamapediatrics.2021.5840. [DOI] [PubMed] [Google Scholar]
- 5.Robinson C, Ruhl M, Kirpalani A, Alabbas A, Noone D, Teoh CW, Langlois V, Phan V, Lemaire M, Chanchlani R, authors of the CCRRT recommendations for adults with glomerulonephritis Management of Canadian pediatric patients with glomerular diseases during the COVID-19 pandemic: recommendations from the Canadian Association of Pediatric Nephrologists COVID-19 rapid response team. Can J Kidney Health Dis. 2020;7:2054358120970713. doi: 10.1177/2054358120970713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ademhan Tural D, Emiralioglu N, Tural Hesapcioglu S, Karahan S, Ozsezen B, Sunman B, Nayir Buyuksahin H, Yalcin E, Dogru D, Ozcelik U, Kiper N. Psychiatric and general health effects of COVID-19 pandemic on children with chronic lung disease and parents’ coping styles. Pediatr Pulmonol. 2020;55:3579–3586. doi: 10.1002/ppul.250827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Serlachius A, Badawy SM, Thabrew H. Psychosocial challenges and opportunities for youth with chronic health conditions during the COVID-19 pandemic. JMIR Pediatr Parent. 2020;3:e23057. doi: 10.2196/23057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khullar S, Banh T, Vasilevska-Ristovska J, Chanchlani R, Brooke J, Licht CPB, Reddon M, Radhakrishnan S, Piekut M, Langlois V, Aitken-Menezes K, Pearl RJ, Hebert D, Noone D, Parekh RS. Impact of steroids and steroid-sparing agents on quality of life in children with nephrotic syndrome. Pediatr Nephrol. 2021;36:93–102. doi: 10.1007/s00467-020-04684-3. [DOI] [PubMed] [Google Scholar]
- 9.Hussain N, Zello JA, Vasilevska-Ristovska J, Banh TM, Patel VP, Patel P, Battiston CD, Hebert D, Licht CP, Piscione TD, Parekh RS. The rationale and design of insight into nephrotic syndrome: investigating genes, health and therapeutics (INSIGHT): a prospective cohort study of childhood nephrotic syndrome. BMC Nephrol. 2013;14:25. doi: 10.1186/1471-2369-14-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Byles J, Byrne C, Boyle MH, Offord DR. Ontario Child Health Study: reliability and validity of the general functioning subscale of the McMaster Family Assessment Device. Fam Process. 1988;27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- 11.Kroenke K, Spitzer RL, Williams JB, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.61312. [DOI] [PubMed] [Google Scholar]
- 12.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–812. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Varni JW, Limbers CA, Burwinkle TM. Impaired health-related quality of life in children and adolescents with chronic conditions: a comparative analysis of 10 disease clusters and 33 disease categories/severities utilizing the PedsQL 4.0 generic core scales. Health Qual Life Outcomes. 2007;5:43. doi: 10.1186/1477-7525-5-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tam W, Poon SN, Mahendran R, Kua EH, Wu XV. Impacts of COVID-19 and partial lockdown on family functioning, intergenerational communication and associated psychosocial factors among young adults in Singapore. BMC Psychiatry. 2021;21:595. doi: 10.1186/s12888-021-03599-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dondi A, Fetta A, Lenzi J, Morigi F, Candela E, Rocca A, Cordelli DM, Lanari M. Sleep disorders reveal distress among children and adolescents during the COVID-19 first wave: results of a large web-based Italian survey. Ital J Pediatr. 2021;47:130. doi: 10.1186/s13052-021-01083-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author upon reasonable request.