Abstract
Background:
The COVID-19 pandemic has had significant impacts on health care access and delivery, with disparate effects across social and racial lines. Federally Qualified Health Centers (FQHCs) provide critical primary care services to the nation’s most underserved populations, including many communities hardest hit by COVID-19.
Methods:
We conducted an ecological analysis that aimed to examine FQHC penetration, COVID-19 mortality, and socio-demographic factors in 4 major United States cities: New York, New York; Chicago, Illinois; Detroit, Michigan; and Seattle, Washington.
Results:
We found the distribution of COVID-19 cases and mortality varied spatially and in magnitude by city. COVID-19 mortality was significantly higher in communities with higher percentages of low-income residents and higher percentages of racial/ethnic minority residents. FQHC penetration was protective against increased COVID-19 mortality, after model adjustment.
Conclusions:
Our study underpins the critical role of safety-net health care and policymakers must ensure investment in long-term sustainability of FQHCs, through strategic deployment of capital, workforce development, and reimbursement reform.
Keywords: COVID-19 mortality, FQHC penetration, community health centers, health disparities
In the United States (US), health care remains inaccessible for millions of Americans in terms of affordability, proximity, and quality, despite significant federal and state efforts to expand access.1 The health disparities resulting from gaps in access to care have been driven in large part by deliberate, long-term disinvestment in communities of color, creating concentrated pockets of poverty and resource gaps across the nation.2 As a result, many of these communities remain fragile both economically and in terms of health. This fragility was laid bare by the COVID-19 pandemic as the virus itself and the subsequent economic impacts disproportionately affected predominately non-white, low-income communities.3
Federally Qualified Health Centers (FQHCs) are community-based health care organizations that provide comprehensive primary care and support services to largely underserved populations regardless of immigration status, insurance coverage, or ability to pay. In recent decades, increased funding for FQHCs has facilitated their transformation into medical homes delivering high-quality, person-centered care and has reduced barriers to care for low-income and racial/ethnic minority populations.4 ,5 Across the US, FQHCs have been strategically placed in high-poverty and medically underserved areas and are often the only source of care in the communities they serve. Studies have shown that patient outcomes at FQHCs are comparable to those at privately owned primary care practices and FQHCs have been vital in ensuring that high-need, under-resourced communities have access to quality care.6-11
The COVID-19 pandemic has illuminated US health care systems challenges, simultaneously underscoring the critical importance and the inadequacy of the safety-net. As the pandemic has disproportionately affected low-income, Black, Latinx, and other marginalized populations, health disparities have been exacerbated for the nation’s most underserved communities.12,13 Emerging research suggests that inequitable access to health care in communities is the primary driver of COVID-19 outcomes, rather than underlying demographic differences in health status.14 While this evidence suggests that lack of access to timely or quality care is driving these prominent racial and socioeconomic COVID-19 disparities, to-date, studies have not examined the role of FQHCs in this equation.3,14 Simultaneously, the COVID-19 pandemic disrupted health care delivery, particularly for the primary care system where chronic disease management and preventive care were delayed or foregone for long periods.
Studies examining disruptions in chronic disease management have shown that even temporary disruptions to care can have long-lasting effects on patients. Throughout the pandemic, FQHC doors remained open and rapid transitions to telehealth occured, ensuring care continuity for the populations they serve. Thus, the contribution of the safety net to COVID-19 outcomes and recovery efforts has emerged as an important area of investigation. Prior to the pandemic, persons living with chronic disease who were regularly engaged in primary care have been shown to have lower rates of Emergency Department visits and reduced complications of severe disease.11,15 It remains to be tested whether utilization of or access to health care plays a similarly protective role with COVID-19 outcomes.
In this study, we aimed to identify and measure community-level associations between FQHC penetration and COVID-19 mortality, and adjust for presence of socio-demographic factors in 4 major US cities. Authors provide recommendations on how to support primary care access and the health care safety-net, and to improve health outcomes for underserved populations during the COVID-19 pandemic recovery and beyond.
Methods
This study is an ecological analysis of COVID-19 epidemiology in 4 major US cities: New York, New York (NYC), Chicago, Illinois, Detroit, Michigan, and Seattle, Washington. Cities were selected based on population size, geographic diversity, and availability of data at the ZIP code level. The 4 cities in this study had both COVID-19 case and mortality data available and extractable at the ZIP code level during analogous periods. All data collected and analyzed as part of this study were publicly available.
The population in this study included residents from the ZIP codes located within each of the 4 cities’ boundaries. Each city boundary encapsulates all the Census Bureau-defined ZIP Code Tabulation Areas (ZCTAs) where the United States Postal Service’s (USPS) postal name for that ZIP code matches the city name. Data obtained at the ZIP code level were spatially attributed to ZCTAs for analysis. As the Census Bureau does not publish an official crosswalk between ZIP codes and ZCTAs, we used the ZIP Code to ZCTA Crosswalk Table developed by John Snow, Inc. (JSI) for use with Health Service Resource Administration’s (HRSA) Uniform Data System’s (UDS) service area data.16
There were a total of 294 ZCTAs included in the study across the 4 US cities. NYC contained 60.2% (n = 177) of the total sample of ZCTAs, followed by Chicago (19.4%), Seattle (11.2%), and Detroit (9.2%).
COVID-19 Outcomes
The primary outcome of interest for the study was the COVID-19 mortality rate per 10 000. All cumulative mortality data were collected as of June 29, 2021. The COVID-19 case rates (per 10 000) as of 6-28-2021 were used as a measure of incidence of COVID-19 infection in an area, as well as a measure of COVID-19 burden/morbidity—and as a measure of risk of death due to COVID-19 (assuming case rates influence mortality rates)—in a community. COVID-19 case rates were included as a control in all models to reduce potential confounding effects of area incidence rates on risk of death due to COVID-19. ZIP code level COVID-19 data were reported by individual city and county health departments as case counts and/or rates.17-20 COVID-19 case and mortality rates per 10 000 residents were calculated for Seattle, Chicago, and Detroit using population and COVID-19 case/death counts reported.
Safety-Net Access—FQHC Penetration
The FQHC penetration rate of the total population refers to the percent of total residents in the ZCTA served by any health center (from FQHCs reporting 11 or more patients residing in that ZCTA). For each ZCTA, the total number of health center patients is divided by the total number of residents. A higher penetration rate is indicative of better access and lower unmet need for care. Conversely, a lower penetration rate is indicative of worse access and higher unmet need. These data were 2015 to 2019 estimates obtained from HRSA’s UDS Mapper.21
Socio-demographic Characteristics
Socio-demographic measures were selected a priori through review of literature to identify salient factors associated with community-level health inequities and those supporting emerging socio-demographic disparities in COVID-19 incidence and mortality. The percentage of uninsured residents, defined as the total civilian, non-institutionalized population for whom income status was known that has no health insurance, and the percentage of racial or ethnic minority residents were 2015 to 2019 estimates obtained from HRSA’s UDS Mapper. Racial and ethnic minorities were defined as the percentage of the total population that self-identified as Non-White. All Hispanic people regardless of race are included in the “Non-White” category. The percent of the total population aged 75 and above and the total percent of people that live below 200% of the Federal Poverty Level (FPL) were obtained from the 2015 to 2019 American Community Survey estimates.22 Variables not found to be statistically significant in initial correlation analyses were not included in final models.
Statistical Analysis
The distributions of all variables in the study were examined by city, including for missingness, and these distributions were compared across the cities. As the missingness of data was uniformly low across the cities, we analyzed the observed data with no imputation. Data exploration was carried out following the protocol described in Zuur et al.23 Univariate statistics and choropleth maps were produced for all variables in the analysis, including separately, for all 4 cities. Bivariate linear regression between all variables was used to establish independent associations and test for collinearity between explanatory factors.
Generalized mixed linear regression analysis was used, nesting ZCTAs within each city, due to the statistical dependence of COVID-19 mortality on the unit of observation (city), and because of the spatial dimension of the epidemiology of COVID-19. First, we assessed between-city variation in COVID-19 mortality rates to determine the variation attributable to neighborhoods (ZCTAs) and cities by building and examining the unconditional model with no predictors. We then used the generated covariance parameter estimates from this first model to compute the Intraclass Correlation Coefficient (ICC) which indicates how much of the variation in COVID-19 mortality is accounted for by the cities and provides support for using a two-level model.
We continued the model-building process by first including each explanatory variable, separately, as fixed effects to identify independent associations, and then including all variables in the model as fixed effects to determine if the influence of the explanatory variables varied among cities. The final model included FQHC penetration as a fixed effect, adjusting for each of the predictors found to be independently associated with COVID-19 mortality. We used the restricted maximum likelihood estimation (REML) and the Kenward-Roger’s degrees of freedom method to estimate the model as both are well-suited for most multilevel models with an unbalanced design and complex covariance structures. REML takes the uncertainty in the fixed parameters into account when estimating the random parameters which leads to less bias/more conservative parameter estimates. Moreover, the Kenward-Rogers degrees of freedom approximation method produces acceptable rates of Type 1 error and is not overly sensitive to small sample size, so it is ideal to use when estimating models with relatively small samples.24,25
All analyses were conducted in SAS 9.2 and ArcGIS. Marginal significance at α < .1 was explored in independent analyses and statistical significance at α < .05 level was established for the final model. We report results for all identified associations and models assessed.
Results
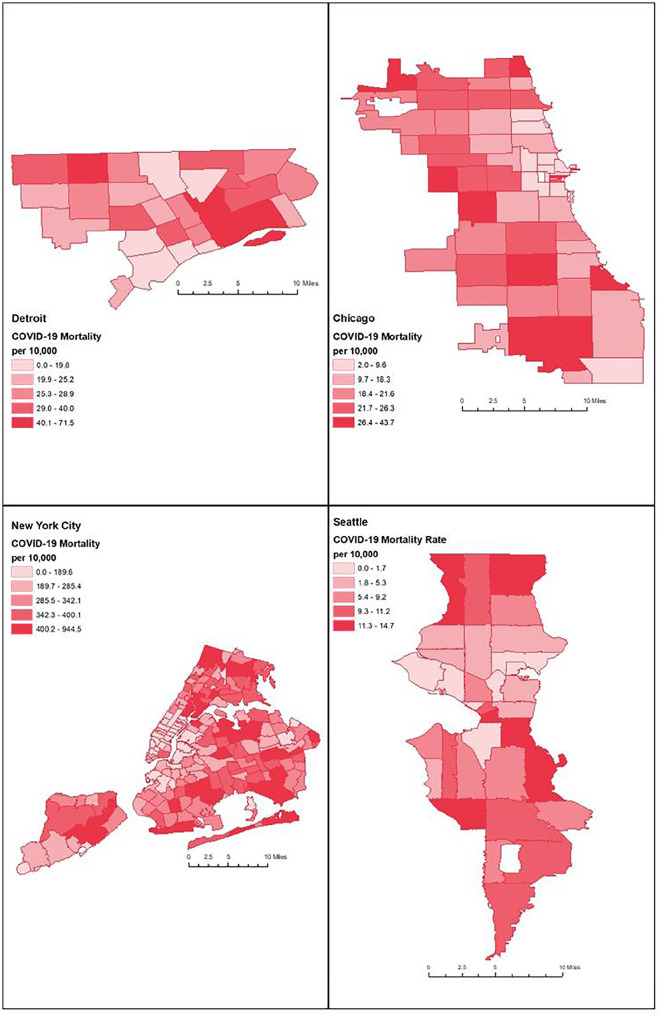
All ZCTAs (n = 294) within the cities of NYC, Detroit, Seattle, and Chicago were included in the analysis. The magnitude of COVID-19 case and mortality rates varied widely across the cities. The highest rates of COVID-19 cases and mortality were concentrated, by far, in New York City, the first epicenter of the pandemic, and were lowest in Seattle (Figure 1, Table 1). Further, unequal distributions of COVID-19 cases and mortality rates were also observed across neighborhoods within cities.
Figure 1.
COVID-19 mortality rates by ZIP code in 4 United States cities, June 28, 2021.
Table 1.
Summary Statistics for Study Variables.
| Study variables (N = 294) | N | Mean (SD) | |
|---|---|---|---|
| COVID-19 outcomesa | |||
| COVID-19 incidence (Cases per 10 000) | All ZCTAs | 294 | 5655.0 (4441.0) |
| New York City | 177 | 8882 (2536) | |
| Chicago | 57 | 1022 (253.9) | |
| Detroit | 27 | 662.4 (127.2) | |
| Seattle | 33 | 431.2 (227.0) | |
| COVID-19 mortality (deaths per 10 000) | All ZCTAs | 292 | 197.2 (184.3) |
| New York City | 177 | 314.4 (145.9) | |
| Chicago | 57 | 18.9 (9.2) | |
| Detroit | 25 | 30.6 (12.6) | |
| Seattle | 33 | 6.7 (4.6) | |
| Safety net accessb | |||
| FQHC penetration (%) | All ZCTAs | 293 | 14.0% (13.0%) |
| New York City | 177 | 12.8% (13.7%) | |
| Chicago | 57 | 17.0% (11.9%) | |
| Detroit | 27 | 11.2% (4.6%) | |
| Seattle | 32 | 17.7% (13.9%) | |
| Socio-demographics | |||
| Racial/Ethnic minority (%) b | All ZCTAs | 294 | 63.0% (26.4%) |
| New York City | 177 | 64.0% (25.9%) | |
| Chicago | 57 | 61.9% (27.6%) | |
| Detroit | 27 | 85.8% (12.9%) | |
| Seattle | 33 | 41.0% (17.2%) | |
| Low-income (%) c | All ZCTAs | 293 | 34.2% (17.5%) |
| New York City | 177 | 31.8% (15.5%) | |
| Chicago | 57 | 35.0% (17.1%) | |
| Detroit | 27 | 61.0% (11.1%) | |
| Seattle | 32 | 23.2% (10.7%) | |
| Aged 75 or above (%) c | All ZCTAs | 294 | 6.1% (2.7%) |
| New York City | 177 | 6.5% (2.9%) | |
| Chicago | 57 | 5.2% (2.3%) | |
| Detroit | 27 | 5.8% (2.2%) | |
| Seattle | 33 | 5.3% (2.2%) | |
| Uninsured (%) b | All ZCTAs | 294 | 7.0% (3.5%) |
| New York City | 177 | 6.4% (3.2%) | |
| Chicago | 57 | 9.1% (4.0%) | |
| Detroit | 27 | 8.4% (1.8%) | |
| Seattle | 33 | 5.0% (2.5%) | |
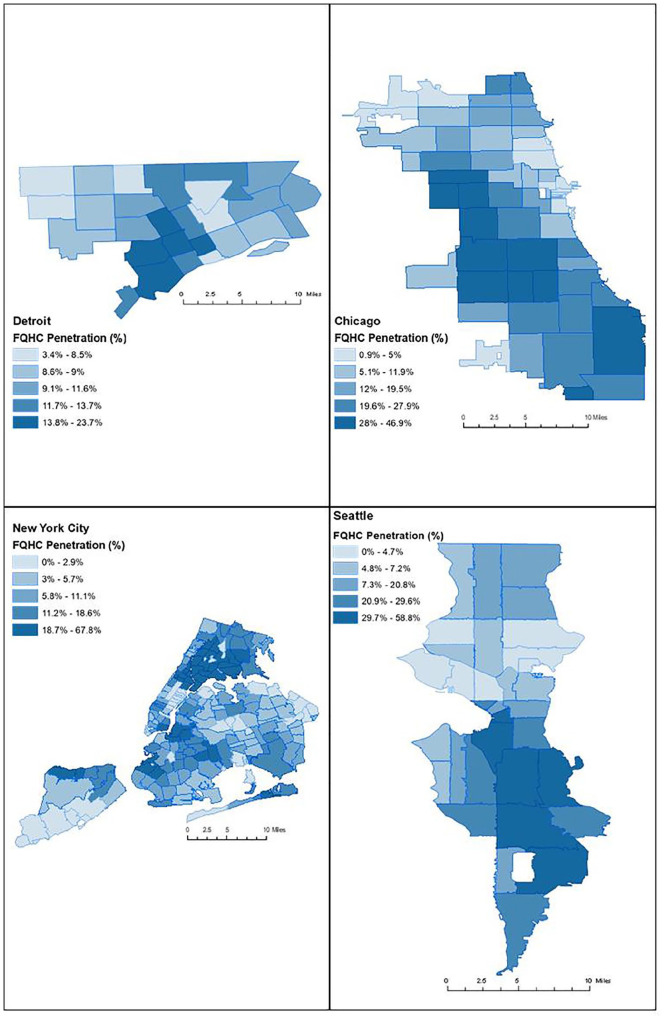
FQHC penetration of the total population (14%) varied greatly across neighborhoods (Figure 2). Detroit neighborhoods had the lowest average FQHC penetration (11.2%) of all the cities, and Seattle had the highest penetration (17.7%). Low-income population rates, by ZCTA, were highest in Detroit neighborhoods (61%), almost twice the average across all cities (34.2%), and lowest in Seattle (23.2%) (Table 1). Similarly, the percentage of racial/ethnic minority residents was highest in Detroit (85.8%) and lowest in Seattle (41%). Within each city, the distribution of both low-income and racial/ethnic minority residents varied greatly across neighborhoods. Uninsured rates did not vary widely across the 4 cities; however, there was unequal distribution of uninsured rates observed within each city. The proportion of the population that was 75 years of age and above was similar across all 4 cities.
Figure 2.
Federally Qualified Health Center penetration by ZIP code in 4 United States cities, 2015 to 2018 estimates.
Independently, all covariates were significantly associated with a positive increase in COVID-19 mortality rates. The percentage of older adult residents had the highest effect estimate (β = 1522.4, P < .01) and COVID-19 case rates (β = .036, P < .01) had the lowest effect estimate. FQHC penetration (β = 159.71, P < .01) was significantly associated with an increase in COVID-19 mortality. The percentage of uninsured (β = 1347.6, P < .01) was significantly associated with an increase in COVID-19 mortality (Table 2).
Table 2.
Mixed Linear Model Results.
| Parameter | Fixed effects | Error variance (Random effects) | Model fit | |||
|---|---|---|---|---|---|---|
| Intercept | Parameter | Intercept | Residual | AIC | BIC | |
| Model 1 | 93.4 (74.60) | 21 952 (18 042.0) | 13 032 (1086.0)* | 3606 | 3604.8 | |
| Model 2 | ||||||
| COVID-19 incidence (cases per 10 000 residents)a | −8.5 (8.6) | 0.04 (0.00)* | 0 | 8148.0 (676.7)* | 3464.7 | 3464.1 |
| FQHC penetration of total population (%)b | 69.9 (76.1) | 159.7 (51.7)* | 22 649 (18 613) | 12 695 (1061.6)* | 3575.5 | 3574.3 |
| Racial/Ethnic minority (%)b | −24.9662 (76.8) | 185.9 (25.2)* | 22 310 (18 282) | 10 988 (917.2)* | 3547.6 | 3546.4 |
| Low-income (%)c | −20.8 (84.6) | 299.2 (41.7)* | 27 338 (22 473) | 11 087 (927.1)* | 3537.7 | 3536.4 |
| Aged 75 or above (%)c | 6.3 (71.6) | 1522.4 (239.7)* | 19 513 (16 040) | 11 479 (958.1)* | 3555.3 | 3554.1 |
| Uninsured (%)b | −4.16 (79.7) | 1347.6 (192.2)* | 24 351 (19 981) | 11 153 (931.0)* | 3548.1 | 3546.9 |
| Model 3 | ||||||
| −201.3 (38.3) | 4467.9 (4128.5) | 5407.6 (455.7)* | 3303 | 3301.8 | ||
| COVID-19 incidence (cases per 10 000 residents)a | 0.03 (0.00)* | |||||
| FQHC penetration of total population (%)b | −185.0 (59.4)* | |||||
| Racial/Ethnic minority (%)b | 109.3 (25.1)* | |||||
| Low-income (%)c | 225.2 (58.6)* | |||||
| Aged 75 or above (%)c | 1561.6 (170.0)* | |||||
Entries show parameter estimates with standard errors in parentheses. Estimation Method = Restricted Maximimum Likelihood Model; Kenward Rogers Approximation.
Source: Authors’ analysis of data from aZIP code level COVID-19 data reported by individual city and county health departments17-20; bHealth Resources and Services Administration. 2021. “UDS Mapper” (Web Application)21; cUnited States Census Bureau via the American Community Survey, 2015 to 2019 Estimates.22
Statistically significant, P < .05; ICC = 0.6275.
All covariates remained significant and positively associated with an increase in COVID-19 mortality rates. The percentage of older adult residents in each neighborhood had the largest effect (β = 1561.9, P < .01) followed by the percentage of low-income residents (β = 225.2, P < .01), and the percentage of racial/ethnic minority residents (β = 109.3, P < .01). COVID-19 case rates had the lowest effect estimate (β = .03, P < .01). In the final model, our explanatory variable of interest, FQHC penetration, remained significant but changed directions. We found that FQHC penetration (β = −185.0, P < .01) was associated with a decrease in neighborhood-level COVID-19 mortality, adjusting for the covariates.
Discussion
Higher FQHC penetration was associated with reduced COVID-19 mortality rates across 4 major US cities, highlighting the importance of the high-quality health care delivered by FQHCs and its important role regarding COVID-19 in cities’ most vulnerable communities. The associations were observed both across all and within cities, suggesting that FQHCs play this supportive role both in aggregate and at the local-level. The COVID-19 mortality rates were also associated with income and race/ethnic minority groups, the primary populations served by FQHCs, highlighting the disproportionate disease burden in these communities. Our results support the emerging research showing that poor health care access is driving disparities in COVID-19 rates and outcomes to a greater degree than poor health status.11
More broadly, the findings from our analyses bolster the evidence base on the importance of investing in the safety-net to increase access to primary care. Primary care improves individual and community health, and is central to health equity.26-29 Prior to and during the COVID-19 pandemic, primary care has kept people healthy and protected against severe disease outcomes, and has had an essential role in public health emergency response as well.26,29,30 Often the only source of primary care in the most vulnerable communities, FQHCs consistently are shown to provide high-quality care that supports improvements in disease outcomes.5-10,15 Our findings demonstrate how FQHCs contribution to community health have supported better disease outcomes at the population level. Ensuring the long-term sustainability of community health centers—a critical pillar of the safety-net—to deliver necessary services is essential to prevent widening racial and health disparities due to the COVID-19 pandemic.
Based on the results presented in this paper, we suggest 2 primary areas for municipal, state, and federal entities to focus on. First, community health centers must have sufficient funding and/or access to low-cost capital so that they can expand existing facilities, build, and establish new delivery sites, and enhance care delivery. While there are several federal funding programs for community health centers, many of these programs are temporary or lack long-term, guaranteed funding to meaningful sustain these organizations.31 Second, it is imperative to build and invest in a well-trained, diverse, and culturally competent workforce for community health centers and the safety net in communities with shortages of primary care providers. A range of programs have been developed at the federal and state levels to attract and maintain staff in underserved areas; however, experts have found that “funding for the preparation of the primary care workforce is inconsistent and insufficient.”32-35
In neighborhoods that lack sufficient access to primary care, even with the above recommendations, it will take time to invest in new infrastructure and workforce development. In the short term, policymakers can direct funding and other support to community-based organizations and other social services providers that play a critical role in connecting community members with health care resources outside of their immediate neighborhoods.36 Enabling FQHCs and community providers to be responsive to the shifting public health needs of their communities will further promote responsive, culturally-targeted primary care during the later phases of the COVID-19 pandemic response.
Future Research
In order to learn from this pandemic and plan more effectively for the next pandemic or other emergency, more research is needed to document primary care providers’ experiences in this pandemic, including not just community health centers but also independent primary care practices and hospital-associated primary and ambulatory care facilities. Research may also examine access and care delivery differences in FQHCs compared to private practices in higher-income communities to establish whether parity has remained during the pandemic.6-9 Such research could focus on the guidance primary care givers were provided with, if any, as well as access to PPE, emergency funds, testing materials, and vaccines. Lastly, we urge local and state health departments to routinely make available data on chronic and communicable diseases to aid researchers in monitoring trends, both geographically and temporally, in population health outcomes.
Limitations
The analysis is subject to several limitations resulting from the ecological analysis design, including the ecological fallacy whereby the ZCTA-level associations identified in the analysis may not translate to individual-level associations. Additionally, the modifiable area unit problem may result from the ZCTA level data, and the associations may not exist when examined at other geographic units. Additional limitations resulted from the availability, or lack thereof, of COVID-19 data for many states and localities across the country. To best align the COVID-19 data, authors ensured data were available at the same geographic level and for the same dates, which limited the metropolitan areas available for inclusion in the analysis. The dynamic and ongoing nature of the COVID-19 pandemic also means that at a given point in time (here June 2021) each metropolitan area was experiencing a somewhat different COVID-19 epidemiology in terms of outbreak timing and local control and vaccination efforts. We believe the study period selected reflects a full year’s period from when COVID-19 had reached most, if not all, US cities. Lastly, given the availability of COVID-19 data in the 4 cities included in the study, it is likely that these cities have COVID-19 surveillance and response efforts unique from localities that do not make data public, which may have an impact on the overall public health and outcomes.
Conclusions
Our study demonstrates the important role FQHCs had in supporting reduced COVID-19 mortality in multiple US cities. We recommend that policymakers strengthen the FQHC safety net through key investments and strategically deployed capital. Additionally, FQHCs and community primary care providers must be enabled to provide high-quality, culturally competent care through investments in the health care workforce, which can be supported through shifting reimbursement models toward prospective payments and value-based payments. In summary, we conclude that strategic investment in community health, particularly that delivered through FQHCs, is essential to improving population health and making meaningful strides toward closing health inequities across racial and social lines.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Mary M. Ford  https://orcid.org/0000-0003-3256-4276
https://orcid.org/0000-0003-3256-4276
Angela Allard  https://orcid.org/0000-0001-5756-0250
https://orcid.org/0000-0001-5756-0250
References
- 1. Starfield B, Shi L, Macinko J. Contribution of primary care to health systems and health. Milbank Q. 2005;83(3):457-502. doi: 10.1111/j.1468-0009.2005.00409.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Friedman S, Insaf T, Lee J-W, Adeyeye T. COVID-19 mortality in New York City across neighborhoods by race, ethnicity, and nativity status. Understanding and eliminating minority health disparities in a 21st-century pandemic: A white paper collection. University at Albany, Suny, Scholars Archive; 2021. Accessed September 8, 2021. https://scholarsarchive.library.albany.edu/covid_mhd_nys_white_papers/8 [Google Scholar]
- 3. Ogedegbe G, Ravenell J, Adhikari S, et al. Assessment of racial/ethnic disparities in hospitalization and mortality in patients with COVID-19 in New York City. JAMA Network Open. 2020;3(12):e2026881. doi: 10.1001/jamanetworkopen.2020.26881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Seymour JW, Polsky DE, Brown EJ, Barbu CM, Grande D. The role of community health centers in reducing racial disparities in spatial access to primary care. J Prim Care Community Health. 2017;8(3):147-152. doi: 10.1177/2150131917699029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN. At federally funded health centers, medicaid expansion was associated with improved quality of care. Health Affairs. 2017;36(1):40-48. doi:10.1377/hlthaff.2016.0804 [DOI] [PubMed] [Google Scholar]
- 6. Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43(2):142-149. doi: 10.1016/j.amepre.2012.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ku L, Jones E, Shin P, Byrne FR, Long SK. Safety-net providers after health care reform: lessons from Massachusetts. Arch Intern Med. 2011;171(15):1379-1384. doi: 10.1001/archinternmed.2011.317 [DOI] [PubMed] [Google Scholar]
- 8. Mehta PP, Santiago-Torres JE, Wisely CE, et al. Primary care continuity improves diabetic health outcomes: from free clinics to federally qualified health centers. J Am Board Fam Med. 2016;29(3):318-324. doi: 10.3122/jabfm.2016.03.150256 [DOI] [PubMed] [Google Scholar]
- 9. Weiss E, Haslanger K, Cantor JC. Accessibility of primary care services in safety net clinics in New York City. Am J Public Health. 2001;91(8):1240-1245. doi: 10.2105/AJPH.91.8.1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lewis VA, Spivack S, Murray GF, Rodriguez HP. FQHC designation and safety net patient revenue associated with primary care practice capabilities for access and quality. J Gen Intern Med. 2021;36(10):2922-2928. doi: 10.1007/s11606-021-06746-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Nath JB, Costigan S, Lin F, Vittinghoff E, Hsia RY. Access to federally qualified health centers and emergency department use among uninsured and medicaid-insured adults: California, 2005 to 2013. Acad Emerg Med. 2019. ;26(2):129-139. doi: 10.1111/acem.13494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Office of Behavioral Health Equity. Substance Abuse and Mental Health Services Administration. Double jeopardy: COVID-19 and behavioral health disparities for black and latino communities in the U.S. (Submitted by OBHE). 2020. [Google Scholar]
- 13. Maciosek MV, Coffield AB, Flottemesch TJ, Edwards NM, Solberg LI. Greater use of preventive services in U.S. Health Care could save lives at little or no cost. Health Affairs. 2010;29(9): 1656-60. doi: 10.1377/hlthaff.2008.0701 [DOI] [PubMed] [Google Scholar]
- 14. Azar KMJ, Shen Z, Romanelli RJ, et al. Disparities in outcomes among COVID-19 patients in a large health care system in California. Health Aff. 2020;39(7):1253-1262. doi: 10.1377/hlthaff.2020.00598 [DOI] [PubMed] [Google Scholar]
- 15. Cole MB, Kim J, Levengood TW, Trivedi AN. Association of medicaid expansion with 5-year changes in hypertension and diabetes outcomes at federally qualified health centers. JAMA Health Forum. 2021;2(9):e212375. doi:10.1001/jamahealthforum.2021.2375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Health Resources and Services Administration. “UDS Mapper” (Web Application). ZIP code to ZCTA crosswalk. 2020. Accessed June 19, 2021. https://udsmapper.org/zip-code-to-zcta-crosswalk
- 17. NYC. Coronavirus disease 2019 (COVID-19) data: Totals. New York City Department of Health & Mental Hygiene. 2021. Accessed June 27, 2021. https://www1.nyc.gov/site/doh/covid/covid-19-data-totals.page
- 18. Seattle & King County Government. 2021. Daily COVID-19 outbreak summary dashboard. Accessed June 28, 2021. https://kingcounty.gov/depts/health/covid-19/data/daily-summary.aspx
- 19. Cook County Government. Medical examiner case archive - COVID-19 related deaths. Accessed June 27, 2021. https://datacatalog.cookcountyil.gov/Public-Safety/Medical-Examiner-Case-Archive-COVID-19-Related-Dea/3trz-enys
- 20. Detroit Department of Health. 2021. COVID-19 dashboard. Accessed June 27, 2021. https://codtableau.detroitmi.gov/t/DHD/views/CityofDetroit-PublicCOVIDDashboard/ZIPCodeDeathRatesDashboard?%3AisGuestRedirectFromVizportal=y&%3Aembed=y
- 21. Human Resources and Services Administration (HRSA). UDS mapper. 2021. Accessed June 28, 2021. http://www.udsmapper.org
- 22. U.S. Census Bureau. 2020. American community survey, 2015-2019 estimates.
- 23. Zuur AF, Ieno EN, Elphick CS. A protocol for data exploration to avoid common statistical problems. Methods Ecol Evol. 2010;1(1):3-14. doi: 10.1111/j.2041-210X.2009.00001.x [DOI] [Google Scholar]
- 24. Luke SG. Evaluating significance in linear mixed-effects models in R. Behav Res Methods. 2017;49(4):1494-1502. doi: 10.3758/s13428-016-0809-y [DOI] [PubMed] [Google Scholar]
- 25. Kerkhoff D, Nussbeck FW. The influence of sample size on parameter estimates in three-level random-effects models. Front Psychol. 2019;10:1067. doi: 10.3389/fpsyg.2019.01067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Starfield B. Primary care and equity in health: the importance to effectiveness and equity of responsiveness to peoples’ needs. Humanity & Society. 2009;33:56-73. https://www.jhsph.edu/research/centers-and-institutes/johns-hopkins-primary-care-policy-center/Publications_PDFs/A243.pdf [Google Scholar]
- 27. Macinko J, Starfield B, Shi L. Quantifying the health benefits of primary care physician supply in the United States. Int J Health Serv. 2007;37:111-126. https://www.researchgate.net/publication/6391542_ [DOI] [PubMed] [Google Scholar]
- 28. Leiyu S, et al. Primary care, self-rated health, and reductions in social disparities in health. Health Serv. Res. 2002;37:529. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1434650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Blewett LA, Johnson PJ, Lee B, Scal PB. When a usual source of care and usual provider matter: adult prevention and screening services. J Gen Intern Med. 2008;23(9):1354-1360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Williams MD, Jean MC, Chen B, Molinari NAM, LeBlanc TT. Primary care emergency preparedness network, New York City, 2015: comparison of member and nonmember sites. Am J Public Health. 2017;107:S193-S198. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5594394/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. US Department of Treasury. New market tax credit program. 2020. Accessed October 3, 2021. https://www.cdfifund.gov/programs-training/programs/new-markets-tax-credit.
- 32. State of Illinois. Governor Quinn signs law to expand health and wellness services in communities across Illinois. 2014. Accessed October 3, 2021. https://www.illinois.gov/news/press-release.12466.html
- 33. Zimmerschied C. How med student loan burdens can deepen health disparities. American Medical Association; 2017. Accessed October 3, 2021. https://www.ama-assn.org/education/medical-school-diversity/how-med-student-loan-burdens-can-deepen-health-disparities.
- 34. Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians' role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174(2):289-291. doi: 10.1001/jamainternmed.2013.12756 [DOI] [PubMed] [Google Scholar]
- 35. McCauley L, Phillips RL, Meisnere M, Robinson SK. eds. Implementing High-Quality Primary Care. National Academies Press; 2021. [PubMed] [Google Scholar]
- 36. Nguyen KH, Fields JD, Cemballi AG, et al. The role of community-based organizations in improving chronic care for safety-net populations. J Am Board Fam Med. 2021;34(4):698-708. doi: 10.3122/jabfm.2021.04.200591 [DOI] [PMC free article] [PubMed] [Google Scholar]