Video
This video details our case as well as our method for successfully eradicating varices immediately prior to esophageal endoscopic submucosal dissection to minimize risks of variceal hemorrhage.
Abbreviations: EIS, endoscopic injection sclerotherapy; ESD, endoscopic submucosal dissection; EVL, endoscopic variceal ligation; RDI, red dichromatic imaging; TIPS, transjugular intrahepatic portosystemic shunt
Introduction
Endoscopic submucosal dissection (ESD) provides an endoscopic treatment option for esophageal cancers limited to the mucosa and submucosa. However, ESD is high-risk in patients with cirrhosis, owing to associated coagulopathy, thrombocytopenia, and portal hypertension, which increases risk for bleeding and life-threatening decompensation. Particularly troublesome in esophageal ESD are esophageal varices.
A case series in 2014 documented successful ESD for esophageal squamous cell carcinoma in 7 patients with cirrhosis and esophageal varices.1 In 2 of the included patients, variceal ligation was completed prior to ESD during the same procedure. This practice was replicated in multiple case reports and case series, though only demonstrated in patients with compensated disease or those classified as having Childs-Pugh A or B cirrhosis.2,3
Case Report
We detail the case of a 55-year-old man with Barrett's esophagus who presented with jaundice, ascites, and hematemesis. He was diagnosed with cirrhosis and acute alcoholic hepatitis with a model for end-stage liver disease - sodium of 27. His labs were notable for hemoglobin of 10.2 g/dL, platelets of 137 × 103/μL, total bilirubin of 32.0 mg/dL, and international normalized ratio of 1.5, and he met criteria for Child-Pugh class C. An upper endoscopy noted F1 varices and an esophageal mass on a background of erosive esophagitis. Bleeding was attributed to his esophagitis.
Once the bleeding resolved, an upper endoscopy with EUS revealed long-segment Barrett esophagus and a 6-mm nodule just proximal. EUS noted intramural esophageal vessels consistent with esophageal varices. No regional lymph nodes were seen. Three variceal bands were placed, and complete eradication was documented. Biopsies of the nodule were concerning for intramucosal carcinoma.
Our patient returned for ESD 2 weeks later (Video 1, available online at www.giejournal.org). Prior to starting the case, he was transfused 2 units of fresh frozen plasma. Unfortunately, 3 columns of now F2 varices were found less than 1 cm distal to the target nodule in the middle and lower portions of the esophagus (Fig. 1). The risk of gastrointestinal hemorrhage was too great to proceed immediately to dissection. Thus, 2 bands were placed 1 cm distal to the nodule on the 2 columns bordering the mass (Fig. 2). These 2 columns were completely eradicated, and we prepared for ESD. We did not feel that marking our target was necessary as the nodule’s borders were very clearly demarcated and the proximity to the varices may have posed additional risk. Fifty milliliters of Hextend with methylene blue were injected with adequate lift of the lesion from the muscularis propria (Fig. 3). A circumferential incision around the lesion into the submucosa was performed with a DualKnife (Olympus America, Center Valley, Pa, USA). Then the lesion was dissected from the underlying deep layers using the DualKnife and ITknife Nano (Olympus America). Multiple sites of transient bleeding were treated with Coagraspers (Olympus America) during the procedure without any significant blood loss. The esophageal lesion was removed en bloc without any adverse events (Figs. 4 and 5). Typically, we use endoscopic suturing to close our large mucosal defects following ESD. However, in this case, we allowed the defect to remain open as we worried that our needle may injure a submucosal varix and cause hemorrhage into the lumen or mediastinum.
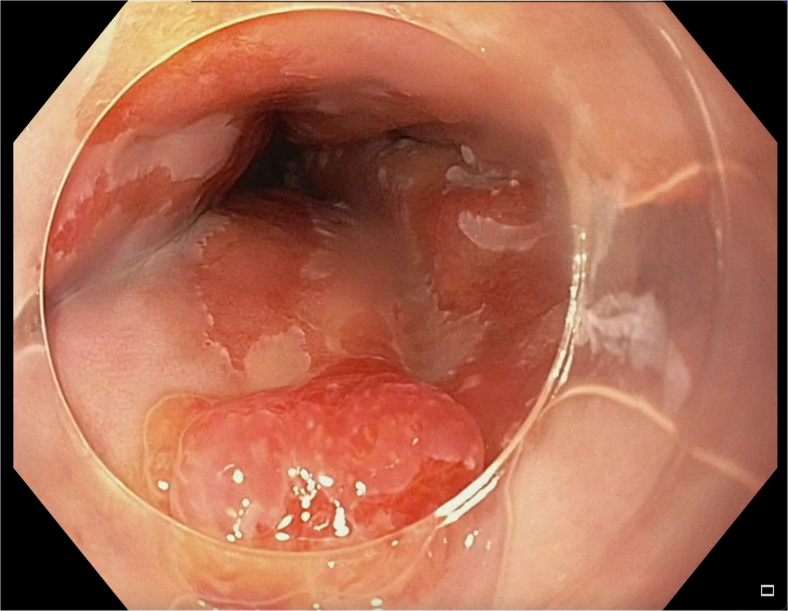
Figure 1.
Endoscopic view of esophageal nodule immediately proximal to multiple columns of F2 esophageal varices.
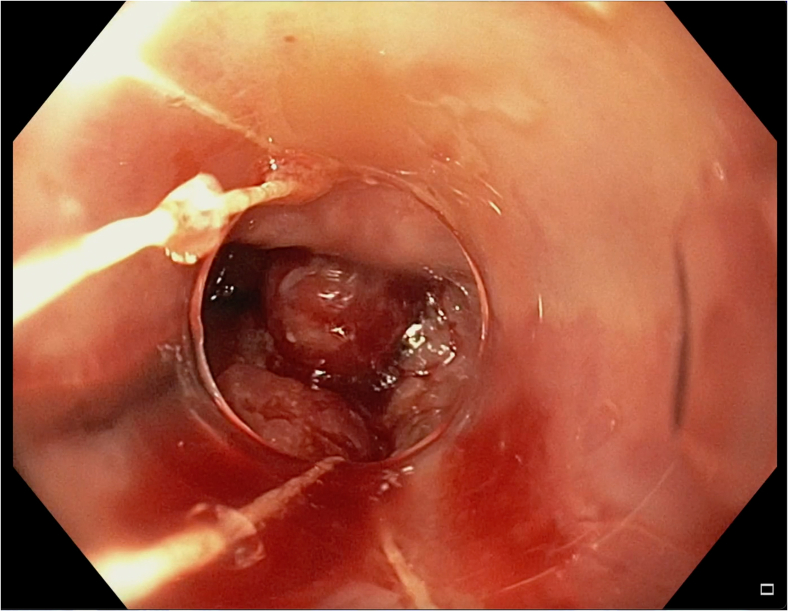
Figure 2.
Multiband ligator with view of esophageal nodule and banded varix.
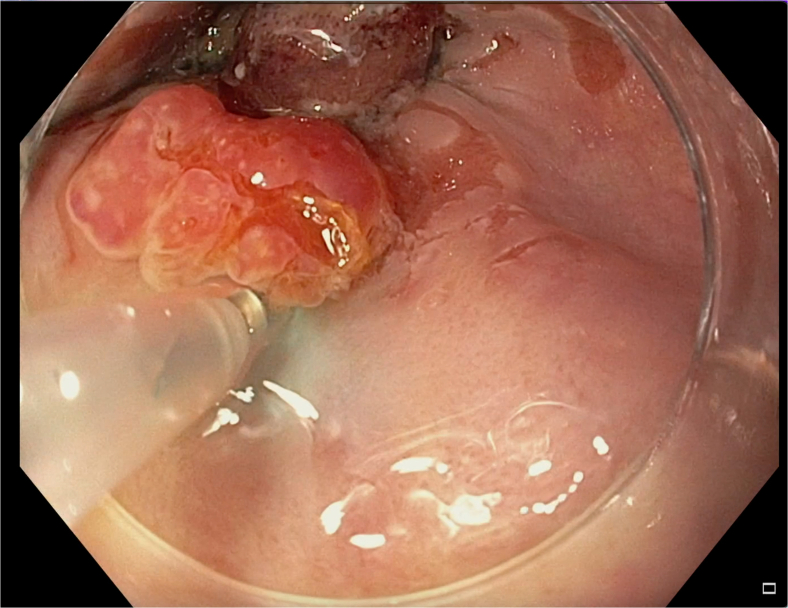
Figure 3.
Esophageal nodule lifted from muscularis propria via injection. Banded varix seen at top of image.
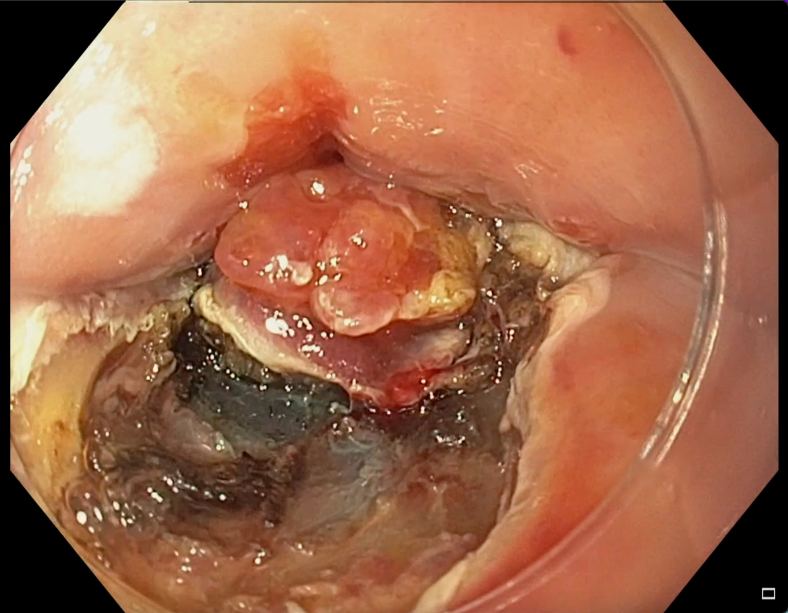
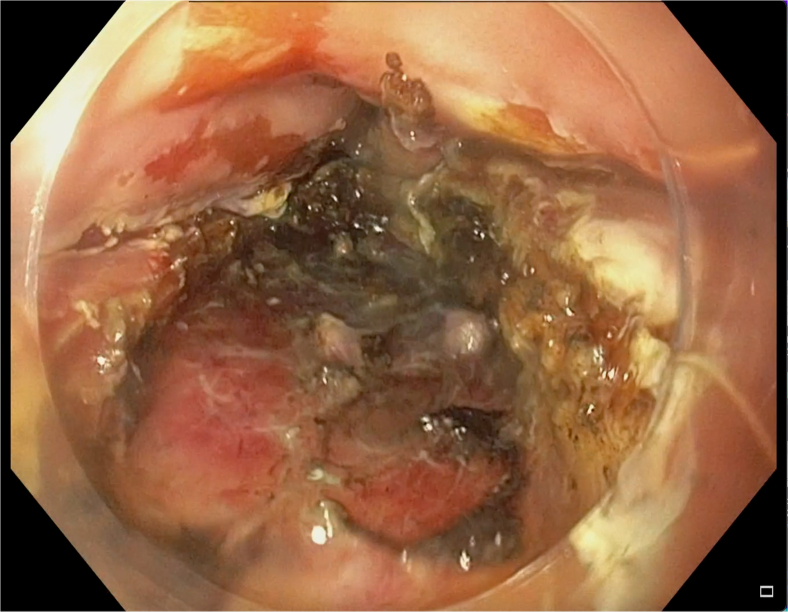
Figure 4.
Nodule removed en bloc via endoscopic submucosal dissection. Pathology revealed adenocarcinoma with clear margins.
Figure 5.
Esophagus following variceal banding and endoscopic submucosal dissection.
Pathology determined that the nodule was adenocarcinoma in situ arising from high-grade dysplasia (Fig. 6). There was no evidence of invasive carcinoma, and our deep and peripheral margins were negative of adenocarcinoma. Our patient has recovered and undergone additional variceal ligation as well as radiofrequency ablation of his Barrett's esophagus (Fig. 7).
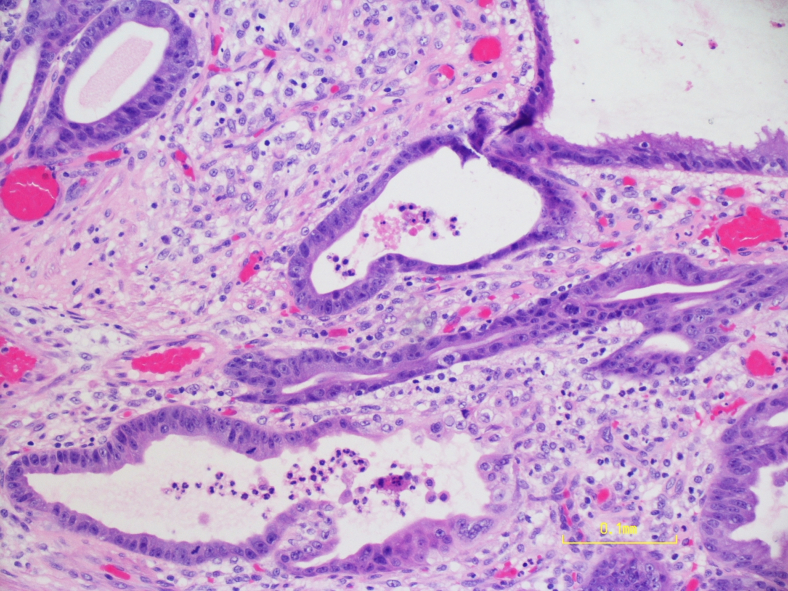
Figure 6.
Resected tissue under high-power magnification demonstrating dilated mucinous glands with enlarged nuclei, loss of polarity, and brisk mitosis consistent with adenocarcinoma in situ arising from Barrett's mucosa (H&E, orig. mag. ×100).
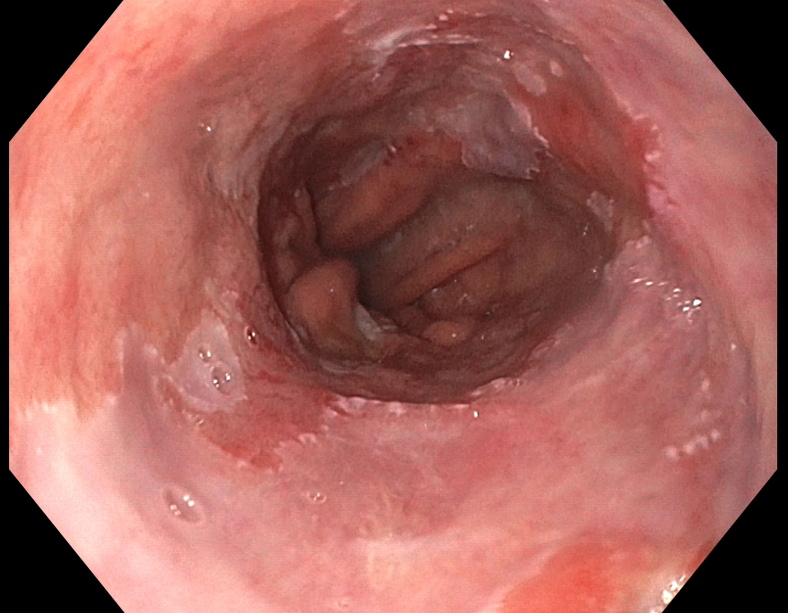
Figure 7.
Follow-up exam revealing well-healed esophagus and successfully eradicated varices. Barrett's esophagus is present and requires additional radiofrequency ablation.
Discussion
Our patient was not a surgical candidate for esophagectomy. The presence of his esophageal cancer precluded him from transplant consideration until sufficiently treated. Fortunately, this ESD not only treated his esophageal cancer but has allowed him to pursue this lifesaving treatment.
We chose ESD as opposed to EMR because EMR is associated with a greater risk of positive margins. Additionally, EMR may have made hemostasis difficult as all underlying vessels would have been severed simultaneously. ESD allowed us to treat each vessel individually. Previous case reports and case series have shown that a combination of variceal banding prior to ESD is a useful technique to mitigate bleeding.4 However, the above case further highlights its use by demonstrating this method’s safety even in a decompensated, Child-Pugh C patient.
There is now growing literature to suggest that esophageal ESD can be completed safely in patients with sequela of cirrhosis, whether esophageal varices are evident on initial luminal examination or not. Below we review various techniques used to safely complete these cases.
-
1.
Endoscopic variceal ligation (EVL) prior to ESD. As mentioned before, multiple reports document successful variceal ligation prior to initiation of ESD to eradicate the esophageal varices and decrease risk of hemorrhage.1, 2, 3, 4 Cases show that this is a safe technique when completed on an earlier date or even on the same day as ESD. Unfortunately, esophageal varices often require multiple sessions for complete eradication, which can significantly delay ESD.
-
2.
Endoscopic injection sclerotherapy (EIS) prior to ESD. There are no reported cases of sclerotherapy of esophageal varices in anticipation of ESD. Nevertheless, it has been done prior to esophageal EMR. This is not ideal as EIS causes submucosal fibrosis and scarring and may subsequently prevent the lesion from lifting with injection.5 Additionally, the variceal response to EIS is slower than with EVL.1
-
3.
Procoagulation of varices. This method has been used in multiple cases to treat submucosal varices encountered during dissection when variceal ligation is no longer an option.6,7 No reports have documented adverse events.
-
4.
Red dichromatic imaging (RDI). This is a new image-enhancing endoscopic technology that uses 3 long wavelengths of irradiating light to enhance the visualization of blood vessels. RDI has been used to identify submucosal esophageal varices during ESD to better avoid them during injection.8 This helps minimize risk of hemorrhage or hematoma formation; however, it does not abolish varices should their location in relation to the lesion be too close for complete avoidance.8, 9
-
5.
Water-pocket ESD. Seen in one case report of a patient with esophageal adenocarcinoma and esophageal varices, this ESD technique incorporates tunneling dissection through a water pool created in the submucosa under the target lesion. This method prevents coagulation smoke from impeding visualization and magnifies the tissue to identify blood vessels more readily. In the setting of submucosal varices, this enables pre-emptive coagulation of large vessels.
-
6.
Transjugular intrahepatic portosystemic shunt (TIPS). One study compared TIPS against EVL as pretreatment of esophageal varices prior to planned ESD.5 With TIPS, they found less frequent and less severe intraprocedural bleeding. TIPS was also felt to cause fewer submucosal adhesions and scarring, which impedes successful ESD. However, this comparison was made with only 2 patients in each group.5 Additionally, TIPS has many associated risks such as acute liver failure, encephalopathy, and damage to surrounding organs. With such a limited study, it is too early to consider this a truly superior method, particularly while we have reviewed many case series of successful ESD following variceal ligation.
-
7.
Thrombopoietin receptor agonist. In one case, avatrombopag was administered to a patient with decompensated cirrhosis 5 days before ESD.7 Platelet transfusions are often administered before invasive procedures in those with chronic liver disease and thrombocytopenia as a means to decrease periprocedural bleeding. Unfortunately, the benefit of platelet transfusion is fleeting, and thrombopoietin receptor agonists such as avatrombopag or lusutrombopag have been able to produce greater increases in platelet count for longer durations.10 Following ESD, this sustained rise in platelet count may have added benefit while the defect heals.
-
8.
Avoiding varices. Variceal treatment may not always be necessary. There have been multiple case reports of endoscopists successfully completing esophageal ESD in patients with esophageal varices without ligation or any form of variceal eradication when there was sufficient distance between the lesion of interest and the varices.1,5,11
Conclusion
Despite multiple reported modalities to treat esophageal varices prior to esophageal ESD, there are very sparce data to guide patient care, and most of the data at this point is anecdotal. Variceal ligation in anticipation of or immediately prior to ESD is the most widely documented method and has repeatedly shown the ability to minimize risk of hemorrhage in these cases. Providers need to recognize that all these techniques exist and should individualize their plan to fit the clinical situation of their patients as this is a very sick, heterogeneous population.
Disclosure
Dr Kantsevoy has the following disclosures; however, none have been deemed conflicts of interest based on the nature of this article and the associated video: cofounder of, equity in, and consultant for Endocages; investor of EndoSound; consultant for Olympus and Medtronic; equity in and consultant for Vizballoons; advisory board member of and consultant for LumenDi; and equity in and consultant for Slater Endoscopy. All other authors disclosed no financial relationships. Verbal patient consent was obtained for publication of the case details on September 28, 2021.
Supplementary data
This video details our case as well as our method for successfully eradicating varices immediately prior to esophageal endoscopic submucosal dissection to minimize risks of variceal hemorrhage.
References
- 1.Sawaguchi M., Jin M., Matsuhashi T., et al. The feasibility of endoscopic submucosal dissection for superficial esophageal cancer in patients with cirrhosis (with video) Gastrointest Endosc. 2014;79:681–685. doi: 10.1016/j.gie.2013.11.004. [DOI] [PubMed] [Google Scholar]
- 2.Jovani M., Anderloni A., Carrara S., et al. Circumferential endoscopic submucosal dissection of a squamous cell carcinoma in a cirrhotic patient with esophageal varices. Gastrointest Endosc. 2015;82:963–964. doi: 10.1016/j.gie.2015.05.023. [DOI] [PubMed] [Google Scholar]
- 3.Tsou Y.K., Liu C.Y., Fu K.I., et al. Endoscopic submucosal dissection of superficial esophageal neoplasms is feasible and not riskier for patients with liver cirrhosis. Dig Dis Sci. 2016;61:3565–3571. doi: 10.1007/s10620-016-4342-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiratori Y., Ikeya T., Nakamura K. Early esophageal squamous cell carcinoma on varix treated with endoscopic submucosal dissection after variceal banding. ACG Case Rep J. 2019;6 doi: 10.14309/crj.0000000000000185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu Z.G., Zhao Y.B., Yu J., et al. Novel endoscopic treatment strategy for early esophageal cancer in cirrhotic patients with esophageal varices. Oncol Lett. 2019;18:2560–2567. doi: 10.3892/ol.2019.10532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kolb J.M., Wani S., Soetikno R., et al. Endoscopic submucosal dissection for early esophageal and gastric neoplasia in decompensated cirrhosis with varices. Endoscopy. 2021;53:E128–E129. doi: 10.1055/a-1216-0148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohapatra S., Montgomery E., Kohli R., et al. Endoscopic submucosal dissection for Barrett's-associated adenocarcinoma in a patient with decompensated cirrhosis and esophageal varices. VideoGIE. 2020;5:190–192. doi: 10.1016/j.vgie.2020.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miyazaki K., Kato M., Matsuura N., et al. Esophageal endoscopic submucosal dissection on postendoscopic variceal ligation scars with injection under red dichromatic imaging. VideoGIE. 2021;6:536–539. doi: 10.1016/j.vgie.2021.08.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dhaliwal L., Codipilly D.C., Rowan D.J., et al. Water-pocket endoscopic submucosal dissection of an early esophageal adenocarcinoma in a patient with portal hypertension and varices. VideoGIE. 2020;5:646–648. doi: 10.1016/j.vgie.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Furuichi Y., Takeuchi H., Yoshimasu Y., et al. Thrombopoietin receptor agonist is more effective than platelet transfusion for chronic liver disease with thrombocytopenia, shown by propensity score matching. Hepatol Res. 2020;50:1062–1070. doi: 10.1111/hepr.13530. [DOI] [PubMed] [Google Scholar]
- 11.Wang A.Y., Smith E.Z., Sauer B.G., et al. A pilot experience of endoscopic submucosal dissection of Barrett's dysplasia despite esophageal varices and decompensated cirrhosis. Hepatology. 2019;70:2225–2227. doi: 10.1002/hep.30850. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This video details our case as well as our method for successfully eradicating varices immediately prior to esophageal endoscopic submucosal dissection to minimize risks of variceal hemorrhage.
This video details our case as well as our method for successfully eradicating varices immediately prior to esophageal endoscopic submucosal dissection to minimize risks of variceal hemorrhage.