Abstract
Background
As management and prevention strategies against COVID-19 evolve, it is still uncertain whether prior exposure to immune checkpoint inhibitors (ICIs) affects COVID-19 severity in patients with cancer.
Methods
In a joint analysis of ICI recipients from OnCovid (NCT04393974) and European Society for Medical Oncology (ESMO) CoCARE registries, we assessed severity and mortality from SARS-CoV-2 in vaccinated and unvaccinated patients with cancer and explored whether prior immune-related adverse events (irAEs) influenced outcome from COVID-19.
Findings
The study population consisted of 240 patients diagnosed with COVID-19 between January 2020 and February 2022 exposed to ICI within 3 months prior to COVID-19 diagnosis, with a 30-day case fatality rate (CFR30) of 23.6% (95% CI 17.8 to 30.7%). Overall, 42 (17.5%) were fully vaccinated prior to COVID-19 and experienced decreased CFR30 (4.8% vs 28.1%, p=0.0009), hospitalization rate (27.5% vs 63.2%, p<0.0001), requirement of oxygen therapy (15.8% vs 41.5%, p=0.0030), COVID-19 complication rate (11.9% vs 34.6%, p=0.0040), with a reduced need for COVID-19-specific therapy (26.3% vs 57.9%, p=0.0004) compared with unvaccinated patients. Inverse probability of treatment weighting (IPTW)-fitted multivariable analysis, following a clustered-robust correction for the data source (OnCovid vs ESMO CoCARE), confirmed that vaccinated patients experienced a decreased risk of death at 30 days (adjusted OR, aOR 0.08, 95% CI 0.01 to 0.69).
Overall, 38 patients (15.8%) experienced at least one irAE of any grade at any time prior to COVID-19, at a median time of 3.2 months (range 0.13–48.7) from COVID-19 diagnosis. IrAEs occurred independently of baseline characteristics except for primary tumor (p=0.0373) and were associated with a significantly decreased CFR30 (10.8% vs 26.0%, p=0.0462) additionally confirmed by the IPTW-fitted multivariable analysis (aOR 0.47, 95% CI 0.33 to 0.67). Patients who experienced irAEs also presented a higher median absolute lymphocyte count at COVID-19 (1.4 vs 0.8 109 cells/L, p=0.0098).
Conclusion
Anti-SARS-CoV-2 vaccination reduces morbidity and mortality from COVID-19 in ICI recipients. History of irAEs might identify patients with pre-existing protection from COVID-19, warranting further investigation of adaptive immune determinants of protection from SARS-CoV-2.
Keywords: COVID-19; Vaccination; Immunogenicity, Vaccine; Cytotoxicity, Immunologic; Immunotherapy
WHAT IS ALREADY KNOWN ON THIS TOPIC
SARS-CoV-2 vaccines significantly improve COVID-19 morbidity and mortality in patients with cancer. Efficacy data from large registry studies in patients receiving immune checkpoint inhibitors (ICIs) are still lacking.
WHAT THIS STUDY ADDS
This joint analysis of patients recently exposed to ICI from OnCovid and European Society for Medical Oncology-CoCARE registries confirms clinical efficacy of SARS-CoV-2 vaccination in reducing COVID-19 morbidity and mortality.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Considering the continuously expanding indication for ICI therapy, these findings are of the utmost importance to ensure effective utilization of this therapy during and beyond the SARS-CoV-2 global pandemic.
Introduction
The efficacy of immune checkpoint inhibitors (ICIs) strongly relies on their capacity of inducing T-cell immune reconstitution.1 T-cell exhaustion is a contributory mechanism underlying the severity of SARS-CoV-2 infection,2 leading on one hand to the investigation of programmed-cell death-1 inhibitors as a therapeutic strategy in severe COVID-19.3 On the other hand, given the pathological immune-mediated mechanisms underlying COVID-19 and the risk of immune-pathology stemming from ICI use, there has been growing concern around the use of ICI in patients with COVID-19 and cancer.4 5
Clinical data in support of a protective, as opposed to detrimental, effect of ICI in the prognosis of COVID-19 in patients with cancer have been inevitably biased by patient selection and underlying clinical characteristics. Initial reports revealed inconsistent results ranging from worse outcomes,6 7 to no difference in COVID-19 severity8 9 in ICI-exposed patients compared with ICI-unexposed patients.
Large metanalyses have suggested no differential impact of ICIs on COVID-19 morbidity and mortality in comparison to other systemic anticancer therapies.10 11
However, COVID-19 outcomes in patients with cancer have substantially evolved over time. Improved management of COVID-19,12 immunization campaigns,13 14 changes in community transmission and the emergence of new SARS-CoV-2 variants15 have considerably changed the clinical impact of SARS-CoV-2 infection on patients with cancer since March 2020.
To date, a significant gap in knowledge remains as to whether the positive effect of SARS-CoV-2 vaccination observed in the general population extends to patients with cancer treated with ICI. Recent evidence suggesting that ICI may precipitate subclinical cytokine release following SARS-CoV-2 vaccination16 strengthens the need to understand the relationship between COVID-19 vaccination and clinical outcomes.
With the aim of providing a contemporary description of COVID-19 morbidity and mortality in patients with cancer who were receiving ICIs at COVID-19 diagnosis and to assess the protective role of SARS-CoV-2 vaccination in this population, we developed this joint analysis of the OnCovid and European Society for Medical Oncology (ESMO) CoCARE registries.
Methods
Study design
OnCovid (NCT04393974) is a European registry study approved by the UK Health Research Authority (20/HRA/1608) collecting data from consecutive patients fulfilling the following inclusion criteria: (1) age ≥18 years; (2) Reverse transcription polymerase chain reaction (RT-PCR) confirmed diagnosis of SARS-CoV-2 infection; (3) history of solid or haematological malignancy either active or in remission at the time of COVID-19 diagnosis.
The ESMO-CoCARE is an observational prospective study, based on a longitudinal multicenter survey of patients with cancer with any solid or hematological malignancy who were diagnosed with COVID-19.
For both registries, data from consecutive, all-comer patients were collected using electronic case report forms designed with the Research Electronic Data Capture software (Vanderbilt University, Nashville, Tennessee, USA). Study details and procedures, patients’ eligibility, and clinical endpoints for both studies have already been extensively presented.12–14 17–24 A list of participating centers with eligible patients for the present analysis is provided as online supplemental table 1.
jitc-2022-005732supp001.pdf (343KB, pdf)
Objectives and endpoints
The main objective of this analysis was to assess the protective role of SARS-CoV-2 vaccination in patients with cancer treated with a unique immunotherapy strategy, by comparing COVID-19 morbidity and mortality between unvaccinated and vaccinated patients.
In addition, we aimed to describe differences in COVID-19 severity and mortality depending on prior history of immune-related adverse events (irAEs) captured from ICI initiation until COVID-19 diagnosis.
Data of patients who received ICI within 3 months prior to COVID-19 diagnosis were merged from the OnCovid and ESMO CoCARE registries. Patients on chemotherapy-ICI and targeted therapy-ICI combinations were excluded from the analysis.
To reflect the temporal evolution of the pandemic, we first categorized patients according to date of COVID-19 diagnosis into prevaccination (from February 2020 to November 2020), alpha–delta (B.1.1.7–B.1.617.2) variants (from December 2020 to December 14, 2021), and omicron (B.1.1.529) variant (from December 15, 2021 to February 2022) pandemic phases as previously reported,13 and described COVID-19 mortality over time.
All-cause case fatality rate at 30 days (CFR30) was chosen as the main clinical endpoint, to differentiate early COVID-19-related mortality, from late, likely cancer-related deaths. As measures of COVID-19 morbidity, we evaluated the all-cause hospitalization and intensive care unit (ICU) admission rates, the rate of COVID-19 complications (at least one among acute respiratory failure, ARDS, kidney injury, secondary infections, sepsis, septic shock, acute cardiac injury, acute liver injury and others including thrombo-embolic events and other coagulopathies, autoimmune diseases, gastrointestinal reactions), the receipt of at least one COVID-19-oriented therapy (including antivirals, chloroquine-based treatment, antibiotics, corticosteroids, interleukin-6 inhibitors and others) (yes vs no), and supplemental oxygen therapy requirement (yes vs no).
Patients who received two doses of the BNT162b2, mRNA-1273, ChAdOx1-S, and CoronaVac vaccines prior to COVID-19, or in case of infection diagnosed at least 28 days after a single dose of the Ad.26.COV2.S vaccine, were defined as fully vaccinated. Patients who received one vaccination, without meeting the above-mentioned time criteria, were considered partially vaccinated, while patients who received a third dose of either the BNT162b2 or mRNA-1273 vaccine (or a second dose after the Ad.26.COV2.S vaccine) were considered boosted. Considering the limited sample size of vaccinated patients with breakthrough infections in the study population, and that the electronic case report form of the ESMO-CoCARE registry was not designed to collect information on booster doses, patients were grouped as unvaccinated (including partially vaccinated) and fully vaccinated (either double-dosed or boosted patients) for all the comparative analyses, while patients with unknown vaccination status were excluded.
For the irAEs analysis, we evaluated COVID-19 outcomes according to the experience of any grade (National Cancer Institute Common Toxicity Criteria for Adverse Events, V.5.0) treatment-related side effects with a putative immune-mediated mechanisms at any time prior to COVID-19. These were previously evaluated by clinicians at participating sites during routine consultations as clinically indicated, without predefined time points, and collected retrospectively by investigators.
Considering the recognized role of lymphopenia as prognostic biomarker in patients with COVID-19,25 we explored the association between the absolute lymphocyte count at COVID-19 (within 1 week of diagnosis) and the experience of prior irAEs in the subset of patients from the OnCovid registry. A detailed description of statistical analysis is provided as online supplemental methods.
Results
Study population
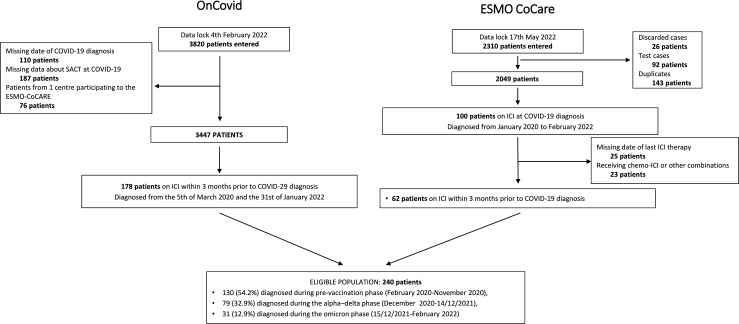
By the respective data lock dates of February 4, 2022 and May 17, 2022, the OnCovid and ESMO CoCARE included 3820 and 2310 patients. After the exclusion of ineligible patients, data from 178 (74.2%—OnCovid) and 62 (25.8%—ESMO CoCARE) patients diagnosed with COVID-19 between January 2020 and February 2022, who were receiving ICIs within 3 months prior to SARS-CoV-2 infection diagnosis, were merged.
Figure 1 reports a detailed study flow diagram. The final study population consisted of 240 patients, of whom 130 (54.2%) were diagnosed with COVID-19 during the prevaccination phase, 79 (32.9%) during the alpha–delta phase, and 31 (12.9%) during the omicron phase, with reducing CFR30 over time: 25.8% (24/93 patients, 95% CI 16.5 to 38.4), 31.5% (17/54 patients, 95% CI 18.3 to 50.4), 3.6% (1/28 patients, 95% CI 0.09 to 19.8).
Figure 1.
Study flow diagram. ESMO, European Society for Medical Oncology; ICI, immune checkpoint inhibitor; SACT, systemic anti-cancer therapies.
The most frequent primary tumor was lung cancer (47.1%), the majority of patients were male (67.5%), aged ≥65 years (62.1%), with at least one comorbidity (77.1%) and presented an active (76.7%), and advanced-stage (80.2%) tumor (table 1).
Table 1.
Baseline patient characteristic and COVID-19 outcomes of the study population
| ICI population | |
| N=240 (%) | |
| Country | |
| UK | 47 (19.6) |
| Spain | 77 (32.1) |
| Italy | 90 (37.5) |
| Others | 26 (10.8) |
| Sex | |
| Female | 78 (32.5) |
| Male | 162 (67.5) |
| Age | |
| <65 years | 90 (37.5) |
| ≥65 years | 149 (62.1) |
| Missing | 1 (0.4) |
| Comorbidities | |
| No | 55 (22.9) |
| Yes | 185 (77.1) |
| Primary tumor | |
| Lung | 113 (47.1) |
| Melanoma | 51 (21.2) |
| Others | 76 (31.7) |
| Tumor stage | |
| Non-advanced | 37 (15.6) |
| Advanced | 190 (80.2) |
| Missing | 10 (4.2) |
| Tumor status at COVID-19 diagnosis | |
| Remission/in-response | 52 (21.7) |
| Active malignancy | 184 (76.7) |
| Missing | 4 (1.7) |
| SARS-CoV-2 vaccination status | |
| Unvaccinated | 182 (75.8) |
| Fully vaccinated | 42 (17.5) |
| Partially vaccinated | 3 (1.3) |
| Unkown | 13 (5.4) |
| COVID-19 outcomes | |
| N (rate, 95% CI) | |
| Oxygen therapy Missing |
81 (37.6, 29.9 to 46.8) 25 |
| COVID-19-specific therapy Missing |
114 (51.6, 42.5 to 61.9) 19 |
| Complications from COVID-19 | 73 (30.4, 23.8 to 38.2) |
| Hospitalization Missing |
131 (56.2, 47.0 to 66.7) 7 |
| ICU admission Missing |
22 (9.4, 5.9 to 14.3) 7 |
| 30-days case fatality rate Missing |
55 (23.6, 17.8 to 30.7) 7 |
COVID-19 outcomes' rates are provided in bold.
ICI, immune checkpoint inhibitor; ICU, intensive care unit.
The received ICI-based regimens were: 136 (56.7%) PD-1 inhibitors monotherapy, 54 (22.5%) PD-L1 inhibitors monotherapy, 20 (8.3%) others/experimental ICIs, 19 (7.9%) CTLA-4/PD-1 inhibitors combinations and 11 (4.6%) not specified chemotherapy-free ICI regimens.
Most patients were unvaccinated prior to COVID-19 (75.8%), 17.5% were fully vaccinated, 1.3% partially vaccinated, while vaccination status was unknown for 13 patients (5.4%). Among fully vaccinated patients, 17 from the OnCovid registry received a booster dose. Vaccination details for both the registries are summarized in online supplemental table 2.
The median observation period for the whole cohort was 91 days (IQR: 15.8–319.0) and the CFR30 was 23.6% (95% CI 17.8% to 30.7%). All COVID-19 outcomes for the whole cohort are summarized in table 1
SARS-CoV-2 vaccination is associated with improvement in COVID-19 outcomes in ICI recipients
After the exclusion of 13 patients with unknown vaccination status, 227 patients were included in the SARS-CoV-2 vaccine analysis.
None of the baseline demographics and oncological characteristics were associated with SARS-CoV-2 vaccination status, with the exception of a higher proportion of patients with at least one comorbidity among unvaccinated patients (80.5% vs 64.3%, p=0.0230) (online supplemental table 3).
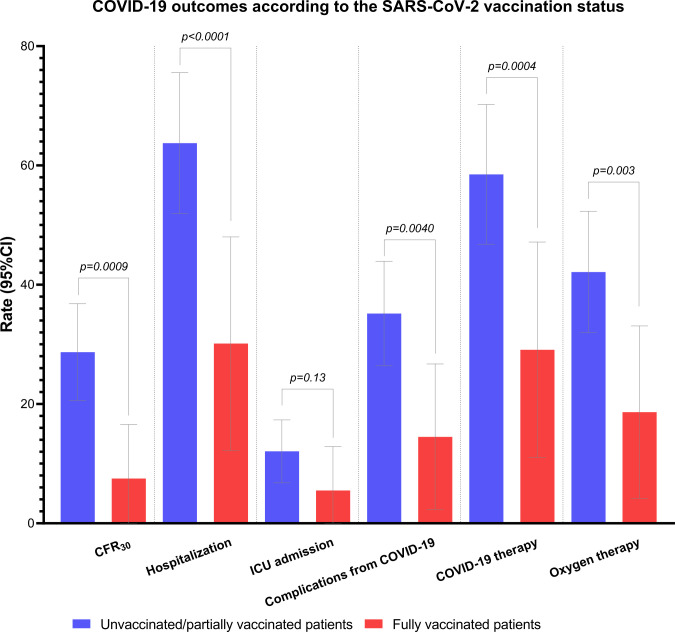
Univariable analysis revealed that fully vaccinated patients experienced decreased rates of death at 30 days (4.8% vs 28.1%, p=0.0009), hospitalization (27.5% vs 63.2%, p<0.0001), COVID-19 complications (11.9% vs 34.6%, p=0.0040), reduced need for COVID-19-specific therapy (26.3% vs 57.9%, p=0.0004) and oxygen therapy (15.8% vs 41.5%, p=0.0030) in comparison to unvaccinated/partially vaccinated patients. We found no significant difference in terms of ICU admission rates, despite arithmetically fewer vaccinated patients being admitted to ICU (4.8% vs 28.1%, p=0.14) (figure 2, online supplemental table 4).
Figure 2.
Histogram plot summarizing all COVID-19 outcomes according to the vaccination status. All rates with 95% CIs are available in online supplemental table 4. CFR30, 30-day case fatality rate; ICU, intensive care unit.
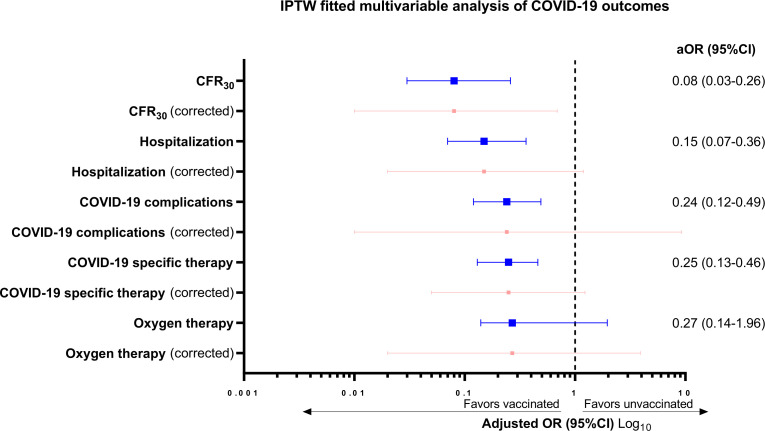
Distribution of baseline patient characteristics prior to and after inverse probability of treatment weighting (IPTW) is reported in online supplemental table 5. Given the suboptimal balancing ability, country, comorbidities, tumor status and tumor stage were included in all IPTW-fitted multivariable logistic regression models for each COVID-19 outcome, which are reported in full as online supplemental table 6 and are summarized in the forest plot graph provided in figure 3. Compared with unvaccinated patients, full vaccination was associated with a decreased risk of death at 30 days (adjusted OR, aOR 0.08, 95% CI 0.03 to 0.26), of hospitalization (aOR 0.15, 95% CI 0.07 to 0.36), of COVID-19 complications (aOR 0.24, 95% CI 0.12 to 0.49) and of need for COVID-19-specific therapy (aOR 0.25, 95% CI 0.13 to 0.46). However, after clustered-robust correction for data source, the upper limit CI crosses one for all COVID-19 outcomes except for CFR30 (aOR 0.08, 95% CI 0.01 to 0.69).
Figure 3.
Summary of the inverse probability of treatment weighing (IPTW) fitted multivariable analyses for each COVID-19 outcomes according to the vaccination status prior to (blue) and after (red) the clustered-robust SE and 95% CI adjustments for the data source. Adjusting covariates for each COVID-19 outcome were country of origin, comorbidities, tumor status, and tumor stage at COVID-19. Full multivariable models are available in online supplemental table 6. aOR, adjusted OR; CFR30, 30-day case fatality rate.
History of irAEs prior to COVID-19 is associated with decreased COVID-19 mortality in patients receiving ICI
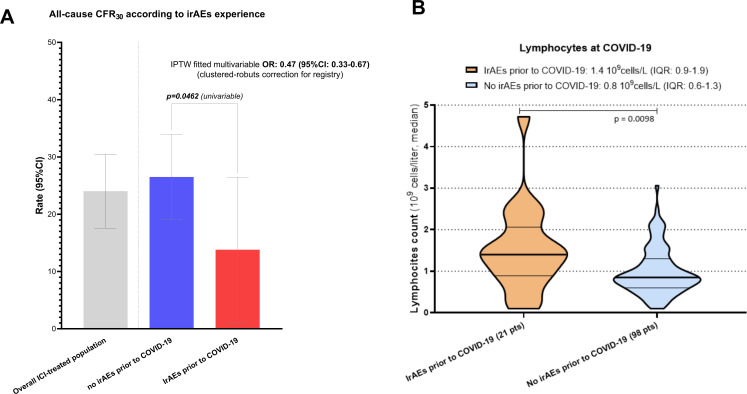
Overall, 38 patients (15.8%) experienced any grade irAEs at any time prior to COVID-19, which are summarized in online supplemental table 7. The median time from occurrence of irAEs and COVID-19 diagnosis was 3.2 months (range 0.13–48.7, computed on data of 27 patients from the OnCovid registry).
The occurrence of irAEs was not associated with any of the baseline demographics and oncological characteristics, including the disease status (active vs remissive/in response) at COVID-19 (p=0.5339), with the exception of the primary tumor (p=0.0373) (online supplemental table 8).
Univariable analysis showed similar rates of hospitalization (51.3% vs 57.1%, p=0.5158), ICU admission (16.2% vs 8.1%, p=0.1252), COVID-19 complications (23.7% vs 31.7%, p=0.3265), COVID-19-specific therapy (45.7% vs 52.6%, p=0.4498) and oxygen requirement (39.3% vs 37.4%, p=0.8251) between patients who experienced and those who did not experience irAEs prior to COVID-19 (online supplemental table 9). However, the occurrence of irAEs was associated with a significantly decreased CFR30 (10.8% vs 26.0%, p=0.0462) (figure 4A).
Figure 4.
(A) Histogram plot summarizing the all-cause 30-day case fatality rate (CFR30) analysis according to the occurrence of any grade immune-related adverse events prior to COVID-19. Inverse probability of treatment weighing (IPTW) fitted adjusted OR for the risk of death at 30 days with clustered robust 95% CI correction for the data source is presented. All rates with 95% CI are available in online supplemental table 9. Adjusting covariates were country of origin, primary tumor, tumor stage at COVID-19 and vaccination status. Full multivariable model is available in online supplemental table 11. (B) Violin plot reporting the median absolute lymphocyte count at COVID-19 (within 1 week of diagnosis) according to the prior occurrence or any grade irAEs. IrAEs, immune-related adverse events.
Distribution of baseline characteristics distribution prior to and after the IPTW is reported in online supplemental table 10. Given the suboptimal balancing ability, country, tumor stage, primary tumor and vaccination status were included in the IPTW-fitted multivariable logistic regression model for COVID-19 mortality, which confirmed that patients who experienced any grade irAEs prior to COVID-19 had a decreased risk of death at 30 days (aOR 0.47, 95% CI 0.23 to 0.99). Clustered-robust correction for data source further strengthened this finding (aOR 0.47, 95% CI 0.33 to 0.67) (online supplemental table 11).
Lastly, in a subset of patients from the OnCovid cohort, we revealed that the median absolute lymphocyte count within 1 week of COVID-19 diagnosis was significantly higher among patients who experienced any grade irAEs prior to COVID-19 than in those who did not experience irAEs (1.4 vs 0.8 109 cells/L, p=0.0098) (figure 4B).
Discussion
Our study is the largest analysis on patients with cancer on ICIs diagnosed with COVID-19 to date. With the inclusion of patients diagnosed up until February 2022, it provides a more contemporary picture of COVID-19 outcomes in this specific population. Although merely descriptive due to the limited sample size of subgroups, the reducing CFR30 across the pandemic phases suggests a time-dependent improvement of COVID-19 mortality, especially during the more recent Omicron outbreak, as already reported for the OnCovid population.13
Even considering the time requirements for the delivery of immunization campaigns since the first SARS-CoV-2 vaccine approval,26 and that most of the included patients were diagnosed during the prevaccination phase, we consider 17.5% of full vaccination a relatively low rate, and a possible impact of vaccine hesitancy, as initially reported in early 2021,27 28 cannot be excluded.
Although preliminary evidence from clinical trials supports the safety and immunogenicity of SARS-CoV-2 vaccines in patients with cancer on active ICI-based treatments,16 29 30 this study demonstrates the efficacy of anti-COVID-19 vaccination in patients receiving ICI in routine clinical practice. The ~83% reduction in the CFR30 in fully vaccinated patients along with COVID-19-related morbidity is confirmed after adjustment for major prognostic confounders in IPTW-fitted models, a process made necessary by the inherent differences existing in study procedures and data collection modalities between the two registries.
The convergence of COVID-19 and ICI-toxicity in eliciting unopposed T-cell activation and downstream cytokine excess has been highlighted suggested as a hypothetical source of clinical risk to patients with cancer ever since the beginning of the pandemic.5 31 Contrary to initial concerns, we document an association between the occurrence of irAEs and reduced CFR30: a novel finding of potential interest in the development of COVID-19-specific therapeutics.
In our study, the protective role of irAEs of all grades on COVID-19-related mortality was independent of common clinicopathological features relating to cancer and COVID-19 prognosis, including SARS-CoV-2 vaccination status. It has been established that patients experiencing irAEs are those capable of mounting a more vigorous anticancer immune reconstitution, resulting in longer survival.32 Because T-cell exhaustion is not solely a hallmark of cancer progression but a mechanism of COVID-19 severity,25 31 we speculate whether history of prior irAE might be a surrogate of more functional T-cell immunity, leading to improved mortality from COVID-19 irrespective of vaccine status.
In keeping with this view, we found that the absolute lymphocyte count at COVID-19, was significantly higher among patients who experienced prior irAEs. It is well known that patients with severe COVID-19 show reduced counts of peripheral CD4+and CD8+ T cells31, and that reduced CD4+/CD8+T cells, B cells, NK cells, and absolute lymphocyte cell count levels are significantly associated with COVID-19 mortality in the general population.25 At the same time, the known mechanisms leading to irAEs involve expansion of intratumoral and peripheral T-cell receptor repertoires along with a mobilization of large numbers of T cells33 34 and, to a lesser extent, activation and exhaustion of CD21low B cells.35 On the other hand, a decrease in the absolute lymphocyte count has been reported with severe ICI-associated myocarditis.36
While OnCovid and ESMO CoCARE registries lack information on T-cell phenotype at COVID-19 diagnosis, our findings are provocative in suggesting that prior irAE might represent a hallmark of protection from COVID-19 mortality through invigorated T-cell immunity. These findings deserve further mechanistic studies to fully elucidate the immunological links between irAEs and COVID-19 outcomes in patients with cancer.
Our study acknowledges several limitations, including lack of data regarding the smoking status and more detailed information regarding irAEs duration and management. Of note, previous irAEs and their putative immune-mediated mechanism were assessed at participating site in routine practice, without predefined time points. This might have impacted the quality of data with risks of underreporting, as the 16.7% and 3.1% rates of all grade and ≥G3 irAEs, respectively, are lower than those reported in interventional clinical trials with ICI-based regimens,37 but comparable to reports from clinical practice.38
In addition, inherent differences between the two registries significantly impacted the accuracy of the estimates from the vaccination analysis: information about booster doses only recently started to be collected for patients entered in the ESMO CoCARE registry and was not available for our analysis. Furthermore, for ~24% of vaccinated patients, the specific type of vaccine could not be reconstructed. While constituting an important limitation, this is unlikely to have affected our results, given recent evidence suggesting largely comparable efficacy of commonly available SARS-CoV-2 vaccines.39
Lastly, despite the inclusion of a significant proportion of more recently diagnosed patients, the lack of availability of viral genomic sequences across the pandemic phases did not allow us to make conclusive considerations about new SARS-CoV-2 variants, while the limited sample size of the ‘alpha–delta’ and ‘omicron’ phases subgroups prevented us from running adequately powered time-adjusted analyses.
Despite the mentioned limitations, our results collectively support the notion that ICI recipients are not especially vulnerable to COVID-19, with mortality rates that are in keeping with the general population with COVID-19 and cancer. In these patients, SARS-CoV-2 vaccination leads to significantly improved outcome from COVID-19, comparably with other oncological patient populations.13 14 40 Considering the continuously expanding indication for ICI therapy,41 our findings are of utmost importance to ensure effective utilization of this therapy during and beyond the SARS-CoV-2 global epidemic.
Footnotes
Twitter: @DettorreGino, @matteolambe, @prat_aleix, @RamonSalazarS
ER and DJP contributed equally.
Contributors: All authors contributed to the publication according to the ICMJE guidelines for the authorship. All authors had access to all the data reported in the study. All authors read and approved the submitted version of the manuscript (and any substantially modified version that involves the author’s contribution to the study). Each author has agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. The corresponding author (AC) had full access to all of the data and and acts as guarantor of the overall content of the study. AC accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish. AC, DJP, SP, ZT, and UD have accessed and verified the study data. Study concept and design: AC, ER, and DJP. Acquisition of data: AC, GMD, UD, JA-C, LC-B, ML, SG, VA, AS-L, JR, PP, DV, AP, MR, RB, TA-G, SG, GD, PQ, SP, AB, MB, DA, RS, MT, KJH, FM, UM, ZT, OM, FP, JB, BV, AP, FB, MK, JT, GP, AG, SP, ER, and DJP. Analysis and interpretation of data: AC, ER, DJP. Drafting of the manuscript: AC, ER, DJP. Statistical analysis: AC, ZT, and UD. Manuscript review and approval: AC, GMD, UD, JA-C, LC-B, ML, SG, VA, AS-L, JR, PP, DV, AP, MR, RB, TA-G, SG, GD, PQ, SP, AB, MB, DA, RS, MT, KJH, FM, UM, ZT, OM, FP, JB, BV, AP, FB, MK, JT, GP, AG, SP, ER, and DJP. Obtained funding: DJP and ER. Study supervision: ER and DJP.
Funding: OnCovid is sponsored by Imperial College London and received direct project funding and infrastructural support by the NIHR Imperial Biomedical Research Centre (BRC).
Disclaimer: The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care. Neither sponsor nor the funders of the study had any role in study design, data collection, data analysis, data interpretation, or writing of the report. ESMO CoCARE is supported by a grant from the European Society of Medical Oncology.
Competing interests: KJH declares research funding from AstraZeneca, Boehringer-Ingelheim, MSD, Replimune and advisory board fees/honoraria from Arch Oncology, AstraZeneca, BMS, Boehringer-Ingelheim, Codiak Biosciences, Inzen Therapeutics, Merck-Serono, MSD, Pfizer, Replimune. DA reports consultation/advisory role for AstraZeneca, Bristol Myers Squibb, Merck Sharp reports speaker’s engagement from AstraZeneca, Bristol Myers Squibb, Merck Sharp reports serving as local PI for Bristol Myers Squibb, Pierre Fabre Pharma and coordinating PI for OncoLytics; reports grant funding from AbbVie; reports being/been DSMB chair of Sanofi (Genzyme); reports being/been a steering committee member of Roche. Olivier Michielin reports personal fees from Bristol-Myers Squibb, MSD, Novartis, Roche, Amgen, NeraCare, outside the submitted work. JR received speaker or advisory fees from Roche, Astra Zeneca, Merck, Ferrer, Persan Farma, Teva Pharma, Leo Pharma, Fresenius kabi, MSD, BMS. Travel expenses support from BMS, MSD, RocheUrania Dafni reports honorarium as Member of the Tumor Agnostic Evidence Generation Working Group of Roche, outside the submitted work. GP reports grants from Amgen, Lilly; grants, personal fees and nonfinancial support from Merck; grants and non-financial support from AstraZeneca; grants and personal fees from Roche, Bristol Myers Squibb, MSD, Novartis, outside the submitted work. Solange Peters reports consultation/advisory role for AbbVie, Amgen, AstraZeneca, Bayer, BeiGene, Biocartis, Bio Invent, Blueprint Medicines, Boehringer Ingelheim, Bristol- Myers Squibb, Clovis, Daiichi Sankyo, Debiopharm, Eli Lilly, Elsevier, F Hoffmann-La Roche/Genentech, Foundation Medicine, Illumina, Incyte, IQVIA, Janssen, Medscape, Merck Sharp and Dohme, Merck Serono, Merrimack, Mirati, Novartis, Pharma Mar, Phosplatin Therapeutics, Pfizer, Regeneron, Sanofi, Seattle Genetics, Takeda, Vaccibody; talk in a company’s organized public event for AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, e-cancer, Eli Lilly, F. Hoffmann-La Roche/Genentech, Illumina, Medscape, Merck Sharp and Dohme, Novartis, PER, Pfizer, Prime, RTP, Sanofi, Takeda; receipt of grants/research supports from being a (sub)investigator in trials (institutional financial support for clinical trials) sponsored by Amgen, AstraZeneca, Biodesix, Boehringer Ingelheim, Bristol-Myers Squibb, Clovis, F Hoffmann-La Roche/Genentech, GSK, Illumina, Lilly, Merck Sharp and Dohme, Merck Serono, Mirati, Novartis, and Pfizer, Phosplatin Therapeutics. Emanuela Rromano reports investigator-initiated trial (funds paid to the institution) supported by Astra-Zeneca, BMS; serves on the consultancy/advisory board for Astra-Zeneca, Merck, Roche, Pierre Fabre. ML acted as consultant for Roche, Novartis, Lilly, AstraZeneca, Exact Sciences, MSD, Pfizer, Seagen and received speaker honoraria from Roche, Novartis, Lilly, Pfizer, Takeda, Ipsen and Sandoz outside the submitted work.Alessandra Gennari has declared consulting/advisory role for Roche, MSD, Eli Lilly, Pierre Fabre, EISAI, and Daichii Sankyo; speakers bureau for Eisai, Novartis, Eli Lilly, Roche, Teva, Gentili, Pfizer, Astra Zeneca, Celgene, and Daichii Sankyo; research funds: EISAI, Eli Lilly, and Roche. CMV has received travel grants and other honoraria from BMS, MSD, Novartis and Roche. Joan Brunet has declared consulting/advisory role for MSD and Astra Zeneca. Aleix Prat has declared personal honoraria from Pfizer, Roche, MSD Oncology, Eli Lilly, and Daiichi Sankyo; travel, accommodations, and expenses paid by Daiichi Sankyo; research funding from Roche and Novartis; and consulting/advisory role for NanoString Technologies, Amgen, Roche, Novartis, Pfizer and Bristol-Myers Squibb. Mark Bower received speakers’ fee from EISAI pharma, Gilead Sciences, Merck and ViiV. JT reports consulting fees from Array Biopharma, AstraZeneca, Avvinity, Bayer, Boehringer Ingelheim, Chugai, Daiichi Sankyo, F Hoffmann-La Roche, Genentech, HalioDX SAS, Hutchison MediPharma International, Ikena Oncology, Inspirna, IQVIA, Lilly, Menarini, Merck Serono, Merus, MSD, Mirati, Neophore, Novartis, Ona Therapeutics, Orion Biotechnology, Peptomyc, Pfizer, Pierre Fabre, Samsung Bioepis, Sanofi, Seattle Genetics, Scandion Oncology, Servier, Sotio Biotech, Taiho, Tessa Therapeutics, and TheraMyc; speaker’s fees from Imedex, Medscape Education, MJH Life Sciences, PeerView Institute for Medical Education, and Physicians Education Resource; and institutional research support from Amgen, Array Biopharma, AstraZeneca Pharmaceuticals, BeiGene, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Debiopharm International, F Hoffmann-La Roche, Genentech, HalioDX, Hutchison MediPharma International, Janssen-Cilag, MedImmune, Menarini, Merck Health, Merck Sharp and has had leadership roles in the European AIDS Clinical Society, UNAIDS, WHO, and The European Hematology Association/ European Society of Medical Oncology. DJP received lecture fees from ViiV Healthcare, Bayer Healthcare, BMS, Roche, EISAI, Falk Foundation, travel expenses from BMS and Bayer Healthcare; consulting fees for Mina Therapeutics, EISAI, Roche, DaVolterra and Astra Zeneca; research funding (to institution) from MSD and BMS. AC received consulting fees from MSD, BMS, AstraZeneca, Roche; speakers’ fee from AstraZeneca, MSD, Novartis and Eisai. All remaining authors have declared no conflicts of interest.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. Individual, deidentified participant data and data dictionary may be made available at the request of investigators whose proposed use of the data has been approved by the OnCovid consortium and ESMO CoCARE steering committees following review of a methodologically sound research proposal.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Bagchi S, Yuan R, Engleman EG. Immune checkpoint inhibitors for the treatment of cancer: clinical impact and mechanisms of response and resistance. Annu Rev Pathol 2021;16:223–49. 10.1146/annurev-pathol-042020-042741 [DOI] [PubMed] [Google Scholar]
- 2.Kusnadi A, Ramírez-Suástegui C, Fajardo V, et al. Severely ill COVID-19 patients display impaired exhaustion features in SARS-CoV-2-reactive CD8+ T cells. Sci Immunol 2021;6:eabe4782. 10.1126/sciimmunol.abe4782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Awadasseid A, Yin Q, Wu Y, et al. Potential protective role of the anti-PD-1 blockade against SARS-CoV-2 infection. Biomed Pharmacother 2021;142:111957. 10.1016/j.biopha.2021.111957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garassino MC, Ribas A. At the crossroads: COVID-19 and Immune-Checkpoint blockade for cancer. Cancer Immunol Res 2021;9:261–4. 10.1158/2326-6066.CIR-21-0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bersanelli M. Controversies about COVID-19 and anticancer treatment with immune checkpoint inhibitors. Immunotherapy 2020;12:269–73. 10.2217/imt-2020-0067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bersanelli M, Giannarelli D, De Giorgi U, et al. Symptomatic COVID-19 in advanced-cancer patients treated with immune-checkpoint inhibitors: prospective analysis from a multicentre observational trial by FICOG. Ther Adv Med Oncol 2020;12:1758835920968463. 10.1177/1758835920968463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Robilotti EV, Babady NE, Mead PA, et al. Determinants of COVID-19 disease severity in patients with cancer. Nat Med 2020;26:1218–23. 10.1038/s41591-020-0979-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luo J, Rizvi H, Egger JV, et al. Impact of PD-1 blockade on severity of COVID-19 in patients with lung cancers. Cancer Discov 2020;10:1121–8. 10.1158/2159-8290.CD-20-0596 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rogiers A, Pires da Silva I, Tentori C, et al. Clinical impact of COVID-19 on patients with cancer treated with immune checkpoint inhibition. J Immunother Cancer 2021;9:e001931. 10.1136/jitc-2020-001931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Y, Liu S, Qin Y, et al. Does prior exposure to immune checkpoint inhibitors treatment affect incidence and mortality of COVID-19 among the cancer patients: the systematic review and meta-analysis. Int Immunopharmacol 2021;101:108242. 10.1016/j.intimp.2021.108242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lazarus G, Budiman RA, Rinaldi I. Does immune checkpoint inhibitor increase the risks of poor outcomes in COVID-19-infected cancer patients? A systematic review and meta-analysis. Cancer Immunol Immunother 2022;71:373–86. 10.1007/s00262-021-02990-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12., Pinato DJ, Patel M, et al. , OnCovid Study Group . Time-Dependent COVID-19 mortality in patients with cancer: an updated analysis of the OnCovid registry. JAMA Oncol 2022;8:114–22. 10.1001/jamaoncol.2021.6199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pinato DJ, Aguilar-Company J, Ferrante D. Outcomes of the SARS-CoV-2 omicron (B.1.1.529) variant outbreak among vaccinated and unvaccinated patients with cancer in Europe: results from the retrospective, multicentre, OnCovid registry study. Lancet Oncol 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pinato DJ, Ferrante D, Aguilar-Company J, et al. Vaccination against SARS-CoV-2 protects from morbidity, mortality and sequelae from COVID19 in patients with cancer. Eur J Cancer 2022;171:64–74. 10.1016/j.ejca.2022.04.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Callaway E. Beyond omicron: what's next for COVID's viral evolution. Nature 2021;600:204–7. 10.1038/d41586-021-03619-8 [DOI] [PubMed] [Google Scholar]
- 16.Walle T, Bajaj S, Kraske JA, et al. Cytokine release syndrome-like serum responses after COVID-19 vaccination are frequent and clinically inapparent under cancer immunotherapy. Nat Cancer 2022;3:1039–51. 10.1038/s43018-022-00398-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pinato DJ, Lee AJX, Biello F, et al. Presenting features and early mortality from SARS-CoV-2 infection in cancer patients during the initial stage of the COVID-19 pandemic in Europe. Cancers 2020;12. doi: 10.3390/cancers12071841. [Epub ahead of print: 08 07 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pinato DJ, Scotti L, Gennari A, et al. Determinants of enhanced vulnerability to coronavirus disease 2019 in UK patients with cancer: a European study. Eur J Cancer 2021;150:190–202. 10.1016/j.ejca.2021.03.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pinato DJ, Tabernero J, Bower M, et al. Prevalence and impact of COVID-19 sequelae on treatment and survival of patients with cancer who recovered from SARS-CoV-2 infection: evidence from the OnCovid retrospective, multicentre registry study. Lancet Oncol 2021;22:1669–80. 10.1016/S1470-2045(21)00573-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pinato DJ, Zambelli A, Aguilar-Company J, et al. Clinical portrait of the SARS-CoV-2 epidemic in European cancer patients. Cancer Discov 2020. doi: 10.1158/2159-8290.CD-20-0773. [Epub ahead of print: 31 Jul 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cortellini A, Salazar R, Gennari A, et al. Persistence of long-term COVID-19 sequelae in patients with cancer: an analysis from the OnCovid registry. Eur J Cancer 2022;170:10–16. 10.1016/j.ejca.2022.03.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cortellini A, Gennari A, Pommeret F, et al. COVID-19 sequelae and the host proinflammatory response: an analysis from the OnCovid registry. J Natl Cancer Inst 2022;114:979–87. 10.1093/jnci/djac057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.ESMO-COCARE registry. Available: https://www.esmo.org/covid-19-and-cancer/registries-studies-and-surveys/esmo-cocare-registry [Accessed 26 Jun 2022].
- 24.Castelo-Branco L, Tsourti Z, Gennatas S, et al. COVID-19 in patients with cancer: first report of the ESMO international, registry-based, cohort study (ESMO-CoCARE). ESMO Open 2022;7:100499. 10.1016/j.esmoop.2022.100499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Huang W, Berube J, McNamara M, et al. Lymphocyte subset counts in COVID-19 patients: a meta-analysis. Cytometry A 2020;97:772–6. 10.1002/cyto.a.24172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Covid-19 vaccine: first person receives pfizer Jab in UK. Available: https://www.bbc.com/news/uk-55227325 [Accessed 23 Aug 2022].
- 27.Ingram SA, Caston NE, Andrews CJ, et al. Hesitancy and malignancy: vaccine hesitancy among individuals with cancer. Journal of Clinical Oncology 2021;39:148. 10.1200/JCO.2020.39.28_suppl.148 [DOI] [Google Scholar]
- 28.Villarreal-Garza C, Vaca-Cartagena BF, Becerril-Gaitan A, et al. Attitudes and factors associated with COVID-19 vaccine Hesitancy among patients with breast cancer. JAMA Oncol 2021;7:1242–4. 10.1001/jamaoncol.2021.1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Waissengrin B, Agbarya A, Safadi E, et al. Short-term safety of the BNT162b2 mRNA COVID-19 vaccine in patients with cancer treated with immune checkpoint inhibitors. Lancet Oncol 2021;22:581–3. 10.1016/S1470-2045(21)00155-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hibino M, Uryu K, Takeda T, et al. Safety and immunogenicity of mRNA vaccines against severe acute respiratory syndrome coronavirus 2 in patients with lung cancer receiving immune checkpoint inhibitors: a multicenter observational study in Japan. J Thorac Oncol 2022;17:1002–13. 10.1016/j.jtho.2022.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Xu Z, Shi L, Wang Y, et al. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir Med 2020;8:420–2. 10.1016/S2213-2600(20)30076-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cortellini A, Buti S, Agostinelli V, et al. A systematic review on the emerging association between the occurrence of immune-related adverse events and clinical outcomes with checkpoint inhibitors in advanced cancer patients. Semin Oncol 2019;46:362–71. 10.1053/j.seminoncol.2019.10.003 [DOI] [PubMed] [Google Scholar]
- 33.Weinmann SC, Pisetsky DS. Mechanisms of immune-related adverse events during the treatment of cancer with immune checkpoint inhibitors. Rheumatology 2019;58:vii59–67. 10.1093/rheumatology/kez308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lozano AX, Chaudhuri AA, Nene A, et al. T cell characteristics associated with toxicity to immune checkpoint blockade in patients with melanoma. Nat Med 2022;28:353–62. 10.1038/s41591-021-01623-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Das R, Bar N, Ferreira M, et al. Early B cell changes predict autoimmunity following combination immune checkpoint blockade. J Clin Invest 2018;128:715–20. 10.1172/JCI96798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Drobni ZD, Zafar A, Zubiri L, et al. Decreased absolute lymphocyte count and increased neutrophil/lymphocyte ratio with immune checkpoint inhibitor-associated myocarditis. J Am Heart Assoc 2020;9:e018306. 10.1161/JAHA.120.018306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Arnaud-Coffin P, Maillet D, Gan HK, et al. A systematic review of adverse events in randomized trials assessing immune checkpoint inhibitors. Int J Cancer 2019;145:639–48. 10.1002/ijc.32132 [DOI] [PubMed] [Google Scholar]
- 38.Raschi E, Gatti M, Gelsomino F, et al. Lessons to be learnt from real-world studies on immune-related adverse events with checkpoint inhibitors: a clinical perspective from pharmacovigilance. Target Oncol 2020;15:449–66. 10.1007/s11523-020-00738-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Munro APS, Janani L, Cornelius V, et al. Safety and immunogenicity of seven COVID-19 vaccines as a third dose (booster) following two doses of ChAdOx1 nCov-19 or BNT162b2 in the UK (COV-BOOST): a blinded, multicentre, randomised, controlled, phase 2 trial. Lancet 2021;398:2258–76. 10.1016/S0140-6736(21)02717-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bestvina CM, Whisenant JG, Torri V, et al. Coronavirus disease 2019 outcomes, patient vaccination status, and cancer-related delays during the omicron wave: a brief report from the TERAVOLT analysis. JTO Clin Res Rep 2022;3:100335. 10.1016/j.jtocrr.2022.100335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Twomey JD, Zhang B. Cancer immunotherapy update: FDA-approved checkpoint inhibitors and companion diagnostics. Aaps J 2021;23:39. 10.1208/s12248-021-00574-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
jitc-2022-005732supp001.pdf (343KB, pdf)
Data Availability Statement
Data are available on reasonable request. Individual, deidentified participant data and data dictionary may be made available at the request of investigators whose proposed use of the data has been approved by the OnCovid consortium and ESMO CoCARE steering committees following review of a methodologically sound research proposal.