Abstract
Background:
Weightbearing computed tomography (WBCT) measurements allow evaluation of several anatomical points for a correct clinical-radiographic diagnosis of pathologies, such as hallux rigidus (HR). In addition, a new semiautomatic segmentation software obtains automated 3D measurements from WBCT scan data sets, minimizing errors in reading angular measurements. The study’s objective was (1) to evaluate the reliability of WBCT semiautomatic imaging measures in HR, (2) to evaluate correlation and agreement between manual and semiautomatic measures in the setting of HR, and (3) to compare semiautomatic measurements between pathologic (HR) and standard control groups.
Methods:
A retrospective study of HR patients was performed including 20 feet with HR. WBCT manual and semiautomatic 3D measurements were performed using the following parameters: (1) first metatarsal-proximal phalanx angle (1stMPP), (2) hallux valgus angle (HVA), (3) first to second intermetatarsal angle (IMA), (4) hallux interphalangeal angle (IPA), (5) first metatarsal length (1stML), (6) second metatarsal length (2ndML), (7) first metatarsal declination angle (1stMD), (8) second metatarsal declination angles (2ndMD), and (9) metatarsus primus elevatus (MPE). The differences between pathologic and control cases were assessed with a Wilcoxon test.
Results:
Interobserver and intraobserver agreement for manual vs semiautomatic WBCT measurements demonstrated excellent reliability. According to the Pearson coefficient, there was a strong positive linear correlation between both methods for the following parameters evaluated: HVA (ρ = 0.96), IMA (ρ = 0.86), IPA (ρ = 0.89), 1stML (ρ = 0.96), 2ndML (ρ = 0.91), 1stMD (ρ = 0.86), 2ndMD (ρ = 0.95), and MPE (ρ = 0.87). Comparison between the pathologic group with HR and the control (standard) group allowed for the differentiating of the pathologic (HR) from the non-pathologic conditions for MPE (p < 0.05).
Conclusion:
Semiautomatic measurements are reproducible and comparable to measurements performed manually, showing excellent interobserver and intraobserver agreement. The software used differentiated pathologic from nonpathologic conditions when submitted to semiautomatic MPE measurements.
Level of Evidence:
Level III, retrospective comparative study.
Keywords: Hallux rigidus, deformity, WBCT, measurements, three-dimensional, automatic, manual, segmentation, intermetatarsal angles
Introduction
Weightbearing computed tomography (WBCT) measurements represent a reliable tool for the assessment of the first ray, including multiplanar assessment in the axial, sagittal, and coronal planes. This can be important for the study pathologies such as hallux rigidus (HR), which involve several anatomical points to be evaluated for a correct clinical-radiographic diagnosis.5,8,10
Along those same lines, an advanced bone segmentation system that performs actions of semiautomatic bone segmentation allows for more accurate measurements of the forefoot.4 The number of WBCT studies evaluating semiautomatic foot and ankle measurements has grown in the last 2 years. It has revealed that WBCT computer-based semiautomatic imaging measures are repeatable and express good agreement and consistency, showing us that this new technology can be an essential tool in the daily practice of foot and ankle orthopaedic surgery.1,4,5 -7,9
In light of this new knowledge, our study objective is (1) to evaluate the reliability of WBCT computer-based semiautomatic imaging measures in HR, (2) to evaluate correlation and agreement between manual and semiautomatic measures in the setting of HR, and (3) to compare semiautomatic measurements between pathologic (HR) and standard control groups. We hypothesized that semiautomatic measures for HR would be as reliable and precise as measurements executed manually.
Methods
A retrospective study was performed observing the Health Insurance Portability and Accountability Act (HIPAA) requirements.
Between May 2016 and February 2021, patients with a clinical and radiologic diagnosis of HR and who were aged ≥18 years were included in the study.
A total of 40 patients were registered and then divided into 2 groups. In group 1, 20 HR feet from 20 patients with a median age of 54.3 ± 11.7 years were included based on the following criteria: patients with degenerative arthritis of the first metatarsophalangeal joint, symptoms of pain with joint movement, and soft tissue edema; on physical examination, they showed increased joint size and restricted joint movement and presented as radiographic findings osteophyte formation, presence of loose bodies, subchondral sclerosis, enlargement/flattening of the metatarsal head, and narrowing of the joint space.
In group 2, the control group, 20 feet were selected from 20 patients with a median age of 42.1±17.3 years who underwent WBCT for unilateral foot and ankle conditions, and WBCT of the contralateral foot were used as controls.
Exclusion criteria were having undergone previous foot surgery or significant foot deformity, including progressive collapsing foot deformity or cavus foot (defined as having an altered foot and ankle offset [FAO], with normal values, considered 2.3% ± 2.9%).
CT Imaging and Measurement
All WBCT semiautomatic (using Bonelogic software) and manual (using CubeVue software) 3D measurements were executed by the same 2 fellowship-trained orthopaedic foot and ankle surgeons who independently assessed the following parameters: (1) first metatarsal-proximal phalanx angle (1stMPP) (sagittal plane), (2) hallux valgus angle (HVA), (3) first to second intermetatarsal angle (IMA), (4) hallux interphalangeal angle (IPA), (5) first metatarsal lengths (1stML), (6) second metatarsal length (2ndML), (7) first metatarsal declination angle (1stMD), (8) second metatarsal declination angle (2ndMD), and (9) metatarsus primus elevatus (MPE) (Figures 1 and 2).
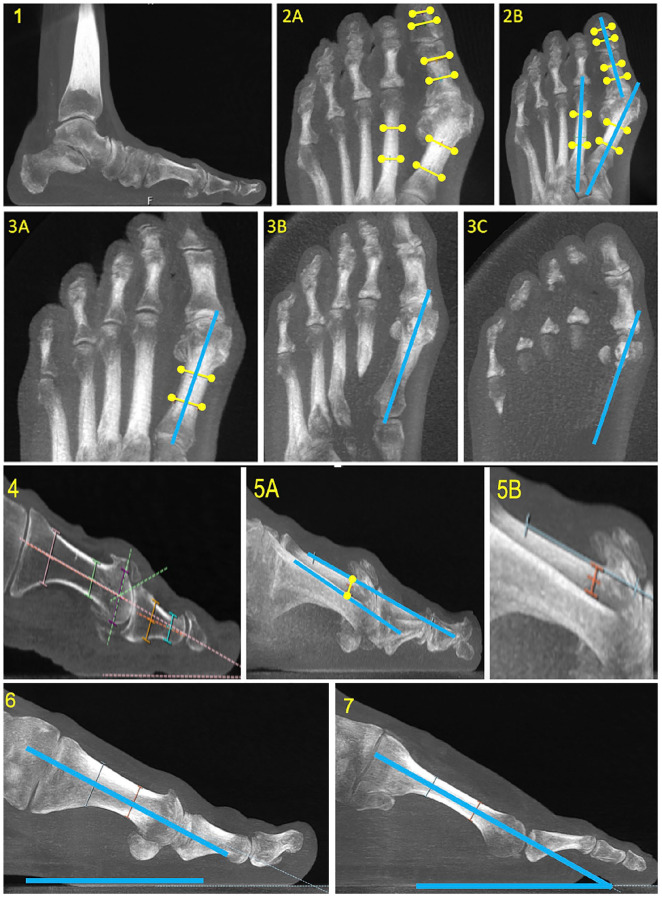
Figure 1.
Sequence of hallux rigidus angle measurements using weightbearing computed tomography (WBCT). Panel 1 demonstrates the increase (approximately 29.5 mm) of the slab (cut thickness) used to find bone axes when the visualization is changed to the axial window. Panel 2 shows measurements of hallux valgus angle (HVA), intermetatarsal angle (IMA), and interphalangeal angle (IPA). The thicker slab is used to find the metatarsal and phalangeal (2A) axes, followed by angular calculations (2B). Hardy and Clapham assessment on WBCT is shown on panel 3, where a thicker slab is used the find the first metatarsal axis (3A), and the exact point where this axis crosses the medial sesamoid is observed by moving inferiorly (3B), portraying the amount of dislocation presented (3C). Panel 4 shows measurements of first metatarsal proximal phalanx angle (1stMPP). Panel 5 shows measurements of metatarsus primus elevatus (MPE) (5A), zoomed in panel 5B. Panel 6 shows measurements of the first metatarsal declination angle (1stMD), and panel 7 shows measurements of the second metatarsal declination angle (2ndMD).
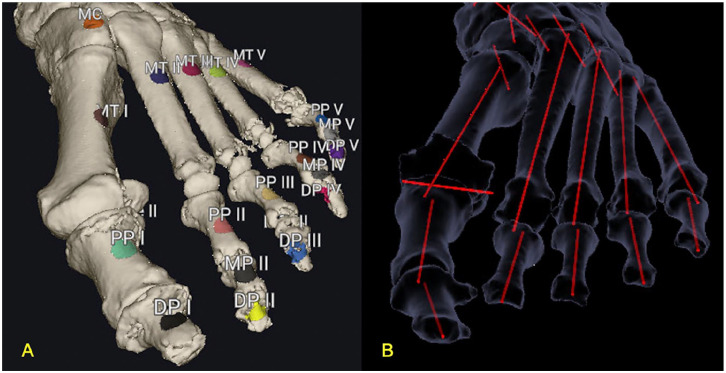
Figure 2.
The semiautomatic 3D measurements were performed using the Disior Bonelogic Ortho Foot and Ankle Software. The user performs bone segmentation by placing at least 1 marker point on each visible bone in the rendered image for analysis (A). The longitudinal axis estimate was generated, and the software automatically registered a mathematical model of the foot and computed the location of measurement landmarks and longitudinal axes of bones, generating the measures of interest (B).
CubeVue software (CurveBeam, LLC, USA) was used to evaluate the images, which were transformed from raw multiplanar nameless data into sagittal, coronal, and axial plane images.4
The HVA, IMA, IPA, 1stML, and 2ndML axes were established in the axial plane. The 1stMPP, 1stMD, and 2ndMD axes were established in the sagittal plane.
The MPE was measured as the distance between the dorsal cortices of the first and second metatarsals.2,8 We used a measurement based on 2 lines. First, a tangent line was drawn along the dorsal cortical bone of the first metatarsal shaft. Second, at the level of the meta-diaphyseal junction, a vertical 90-degree-angle line was drawn from the first line down to the dorsal cortical bone of the second metatarsal shaft. The distance between the 2 intersection points of the 2 dorsal cortical bones along the vertical line determined the MPE.2,8 Angular measurements were performed using the Cobb method (Figure 1).4,8
The semiautomatic 3D measurements were performed using the Disior Bonelogic Foot and Ankle Software (version 2.1; Finland). The user first selects a file in DICOM format for investigation. The software automatically performed a 3D isosurface of the bone tissue. The user executes bone segmentation by placing at least 1 marker point on each visible bone in the performed image for analysis (Figure 2A).
Deformable shape models were used to obtain the patient-specific shape. The longitudinal axis was automatically generated for the metatarsal and phalanx model of each patient, finding the bone center in the proximal to distal orientation and its cross sections at different points.4 After that, the software automatically registered a mathematical model of the foot and ankle on the image and computed the location of measurement landmarks and longitudinal axes of bones of interest (Figure 2B).4
Statistical Analysis
The sample size calculation were performed using G*Power 3.1.9, based on the MPE. Our choice was based on the study by Lee et al8 in which a threshold value of MPE to predict the diagnosis of HR was calculated using a receiver operating characteristic curve and found to be 4.19 mm, with an area under the curve of 0.821 and 77% sensitivity and 77% specificity.
Interrater reliabilities were performed using interclass correlations coefficients (ICCs). Pearson correlation coefficient was used to evaluate the linear relationship between manual and semiautomatic WBCT measurements. Agreement between semiautomatic (SA) and manual (M) methods was verified using Bland-Altman plots.
The difference between the pathologic (HR) and control cases using semiautomatic measurements was evaluated with the Wilcoxon test. P values ≤.05 were considered significant.
Results
Interobserver and intraobserver agreement and consistency using ICC were >0.90 for WBCT semiautomatic readings (Table 1).
Table 1.
Intraobserver and Interobserver Agreement and Consistency of Semiautomatic (SA) Measurements Assessed by ICC.
| Interobserver (SA) | Intraobserver (SA) | |||||
|---|---|---|---|---|---|---|
| Agreement (95% CI) |
Consistency (95% CI) |
P Valuea | Agreement (95% CI) |
Consistency (95% CI) |
P Valuea | |
| HVA | 1 (0.999, 1.000) | 1 (0.999, 1.000) | <.001* | 1 (0.999, 1.000) | 1 (0.999, 1.000) | <.001* |
| IMA | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* | 1 (0.999, 1.000) | 1 (0.999, 1.000) | <.001* |
| IPA | 0.973 (0.932, 0.989) | 0.972 (0.930, 0.989) | <.001* | 0.998 (0.996, 0.999) | 0.998 (0.996, 0.999) | <.001* |
| 1stMPP | 1 (0.999, 1.000) | 1 (0.999, 1.000) | <.001* | 1 (0.999, 1.000) | 1 (0.999, 1.000) | <.001* |
| 1stML | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* |
| 2ndML | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* |
| 1stMD | 0.999 (0.998, 1.000) | 0.999 (0.998, 1.000) | <.001* | 1 (0.999, 1.000) | 1 (1.000, 1.000) | <.001* |
| 2ndMD | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* | 1 (1.000, 1.000) | 1 (1.000, 1.000) | <.001* |
| MPE | 0.999 (0.997, 1.000) | 0.999 (0.997, 1.000) | <.001* | 0.998 (0.996, 0.999) | 0.998 (0.995, 0.999) | <.001* |
Abbreviations:1stMD, first metatarsal declination angle; 1stML, first metatarsal length; 1stMPP, first metatarsal-proximal phalanx angle; 2ndMD, second metatarsal declination angle; 2ndML, second metatarsal length; HVA, hallux valgus angle; IMA, intermetatarsal angle; IPA, interphalangeal angle; MPE, metatarsus primus elevatus; SA, semiautomatic measurement.
P values are based on F tests inherent in function icc/R package irr.
Statistical significance, P < .05.
Semiautomatic and manual mean measurements were executed in individuals with HR (Table 2) and according to Pearson coefficient, there was a strong significant (P’s < .001) positive linear correlation between manual and semiautomatic measurements for the following assessed parameters: HVA, r = 0.96; IMA, r = 0.86; IPA, r = 0.89; 1stML, r = 0.96; 2ndML, r = 0.91; 1stMD, r = 0.86; 2ndMD, r = 0.95, and MPE, r = 0.87.
Table 2.
Measurements Performed on Individuals With Hallux Rigidus.
| Manual Measurement | Semiautomatic Measurement | ||||
|---|---|---|---|---|---|
| Mean | 95% Prediction Limits | Mean | 95% Prediction Limits | P Valuea | |
| HVA | 17.04 | (14.17-19.90) | 14.41 | (11.36-17.45) | <.001* |
| IMA | 11.77 | (10.51-13.02) | 12.37 | (11.01-13.73) | <.001* |
| IPA | 13.47 | (11.68-15.25) | 13.53 | (11.44-15.62) | <.001* |
| 1stMPP | 11.11 | (8.66-13.55) | 11.69 | (9.50-13.88) | .004* |
| 1stML | 60.56 | (58.78-62.33) | 62.68 | (60.73-64.62) | <.001* |
| 2ndML | 69.16 | (67.43-70.89) | 76.23 | (74.09-78.41) | <.001* |
| 1stMD | 21.43 | (19.81-23.03) | 19.96 | (18.38-21.54) | <.001* |
| 2ndMD | 25.02 | (23.40-26.62) | 24.15 | (22.51-25.78) | <.001* |
| MPE | 5.54 | (4.77-6.30) | 7.45 | (6.56-8.33) | <.001* |
Abbreviations: 1stMPP, first metatarsal-proximal phalanx angle; 1stML, first metatarsal length; 2ndML, second metatarsal length; 1stMD, first metatarsal declination angle; 2ndMD, second metatarsal declination angle; HVA, hallux valgus angle; IMA, intermetatarsal angle; IPA, interphalangeal angle; MPE, metatarsus primus elevatus.
P values are based on Shapiro-Wilk test.
Statistical significance, P < .05.
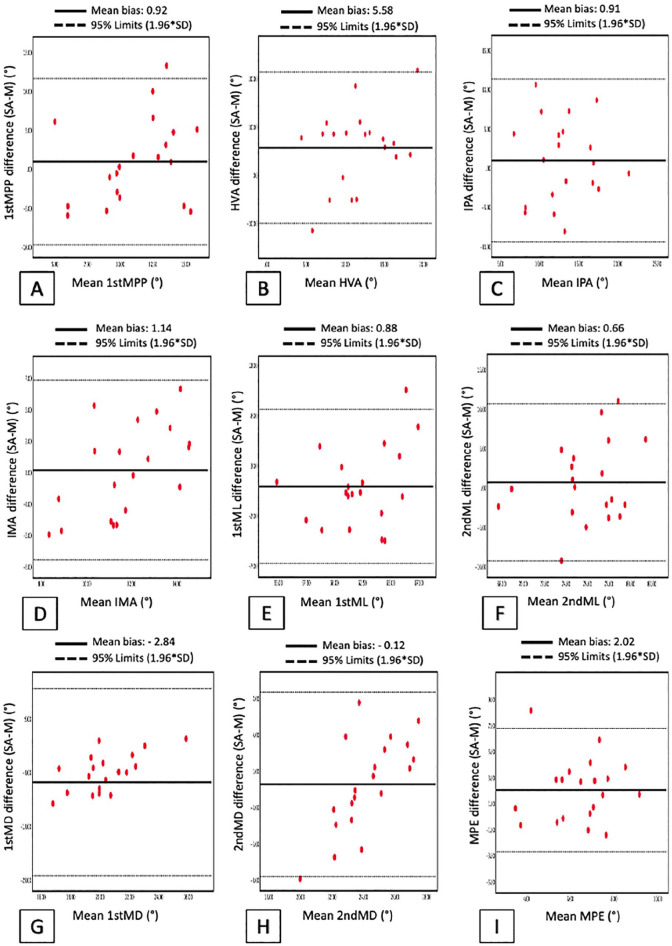
Agreement between semiautomatic (SA) and manual (M) methods was tested for 1stMPP, HVA, IMA, IPA, 1stML, 2ndML, 1stMD, 2ndMD, and MPE using the Bland-Altman plots (Figure 3). This method stated excellent agreement between semiautomatic and manual segmentation, and the results denoted a high correlation between the parameters calculated from the semiautomatic and manual measurements, and a strong agreement between the software and the readers.
Figure 3.
Bland-Altman plots for (A) first metatarsal-proximal phalanx angle (1stMPP) (sagittal plane), (B) hallux valgus angle (HVA), (C) hallux interphalangeal angle (IPA), (D) first to second intermetatarsal angle (IMA), (E) first metatarsal length (1stML), (F) second metatarsal length (2ndML), (G) first metatarsal declination angle (1stMD), (H) second metatarsal declination angle (2ndMD), and (I) metatarsus primus elevatus (MPE). The mean for each pair of semiautomatic (SA) and manual (M) measurement is shown on the x axis. The corresponding difference (bias) between this SA and M measurement (SA minus M) is shown on the y axis. Mean difference (solid line). Dashed black lines represent 95% limits of agreement (mean difference ± 1.96 SD of the difference).
Comparison between pathologic group with HR and control group using semiautomatic measurements could differentiate nonpathologic from pathologic (HR) conditions for the HVA and MPE (P < .05) (Table 3).
Table 3.
Comparison Between Pathologic vs. Control Group Using Semiautomatic Measurement.
| Pathologic Group | Control Group | |||
|---|---|---|---|---|
| Mean | Mean | Mean Difference | P Valuea | |
| HVA | 14.41 | 8.83 | 5.58 | .006* |
| IMA | 12.37 | 11.2 | 1.17 | .097 |
| IPA | 13.53 | 12.53 | 1 | .448 |
| 1stMPP | 11.69 | 10.71 | 0.98 | .459 |
| 1stML | 62.68 | 61.79 | 0.89 | .324 |
| 2ndML | 76.23 | 75.56 | 0.67 | .568 |
| 1stMD | 19.96 | 22.81 | –2.85 | .114 |
| 2ndMD | 24.15 | 24.28 | –0.13 | >.99 |
| MPE | 7.45 | 5.43 | 2.02 | .001* |
Abbreviations: 1stMD, first metatarsal declination angle; 1stML, first metatarsal length; 1stMPP, first metatarsal-proximal phalanx angle; 2ndML, second metatarsal length; 2ndMD, second metatarsal declination angle; HVA, hallux valgus angle; IMA, intermetatarsal angle; IPA, interphalangeal angle; MPE, metatarsus primus elevatus.
P values are based on the Wilcoxon test.
Statistical significance, P < .05.
Discussion
This study confirmed our hypotheses that the semiautomatic measurements used in the WBCT would show excellent Inter and intraobserver reliability to assess the 1stMPP, HVA, IMA, IPA, 1stML, 2ndML, 1stMD, 2ndMD, and MPE in the presence of Hallux Rigidus. Furthermore, it confirmed that semiautomatic WBCT measurements are as accurate as manual WBCT measurements.
However, as we expected, only the MPE measure was capable of differentiating pathologic (HR) from nonpathologic conditions (Table 3). Our expectation was based on previous studies that state that patients with HR have increased MPE.2,3,8
Cheung et al3 were the first to study the relationship between HR and WBCT measurements. In their study that evaluated foot alignment and MPE in patients with hallux rigidus, they found that patients with HR significantly decreased declination ratios from the first to the second metatarsal, indicating the presence of MPE. Furthermore, they state that with excellent intraobserver and interobserver reliability, WBCT has proven to be a reliable method of assessing foot alignment in patients with HR.
Along the same line, in a recent case-control study, Lee et al8 asked whether MPE really exists in hallux rigidus and evaluated if MPE could affect the forefoot spatial relationship in the HR group compared with controls. Using WBCT, they concluded that the group with HR had increased MPE. In this study, a threshold value was calculated to evaluate the diagnostic value of WBCT MPE for hallux rigidus using a receiver operating characteristic curve. The threshold value was found to be 4.19 mm with 77% sensitivity and 77% specificity in their cohort. In our study, we found a mean MPE value in the HR group of 7.45 mm (Table 3).
Nevertheless, our study has some limitations. First, we eliminated patients who had intraosseous metallic artifacts. We still do not have an answer about the effects of this new technology in the presence of these objects. Second, this study has a small cohort. Finally, this is a developing technology restricted to a few research centers.
Conclusion
Semiautomatic measurements reliably expressed excellent inter- and intraobserver agreement and are reproducible and comparable to measurements executed manually in the setting of HR. The comparison between the control group without HR and the pathologic group with HR through semiautomatic measurements was capable to differentiate pathologic conditions (HR) from nonpathologic conditions for the MPE measurement. The improvement of advanced semiautomatic segmentation software with minimal user intervention allows the establishment of big data, which is an essential step toward the use of Artificial Intelligence that should guide diagnostic and therapeutic approaches in the future to facilitate decision making.
Footnotes
Ethical Approval: Ethics Committee approved this research under the Institutional Review Boards (IRB) number 202012422 and 201904825 in accordance with the Declaration of Helsinki. The study complies with the Health Insurance Portability and Accountability Act (HIPAA).
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Cesar de Cesar Netto is a paid consultant to Curvebeam and has stock options with Curvebeam. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Kepler Alencar Mendes de Carvalho, MD,  https://orcid.org/0000-0003-1082-6490
https://orcid.org/0000-0003-1082-6490
Vineel Mallavarapu, BS,  https://orcid.org/0000-0002-8612-5941
https://orcid.org/0000-0002-8612-5941
Kevin Dibbern, PhD,  https://orcid.org/0000-0002-8061-4453
https://orcid.org/0000-0002-8061-4453
Nacime Salomao Barbachan Mansur, MD, PhD,  https://orcid.org/0000-0003-1067-727X
https://orcid.org/0000-0003-1067-727X
Cesar de Cesar Netto, MD, PhD,  https://orcid.org/0000-0001-6037-0685
https://orcid.org/0000-0001-6037-0685
References
- 1. Bernasconi A, Cooper L, Lyle S, et al. Intraobserver and interobserver reliability of cone beam weightbearing semi-automatic three-dimensional measurements in symptomatic pes cavovarus. Foot Ankle Surg. 2020;26(5):564-572. doi: 10.1016/j.fas.2019.07.005 [DOI] [PubMed] [Google Scholar]
- 2. Bouaicha S, Ehrmann C, Moor BK, Maquieira GJ, Espinosa N. Radiographic analysis of metatarsus primus elevatus and hallux rigidus. Foot Ankle Int. 2010;31(9):807-814. [DOI] [PubMed] [Google Scholar]
- 3. Cheung ZB, Myerson MS, Tracey J, Vulcano E. Weightbearing CT scan assessment of foot alignment in patients with hallux rigidus. Foot Ankle Int. 2018;39(1):67-74. doi: 10.1177/1071100717732549 [DOI] [PubMed] [Google Scholar]
- 4. De Carvalho KAM, Walt JS, Ehret A, et al. Comparison between weightbearing-CT semiautomatic and manual measurements in hallux valgus. Foot Ankle Surg. 2022;28(4):518-525. doi: 10.1016/j.fas.2022.02.014 [DOI] [PubMed] [Google Scholar]
- 5. De Cesar Netto C, Richter M. Use of advanced weightbearing imaging in evaluation of hallux valgus. Foot Ankle Clin. 2020;25(1):31-45. [DOI] [PubMed] [Google Scholar]
- 6. Krähenbühl N, Kvarda P, Susdorf R, Burssens A, Ruiz R, Barg A, Hintermann B. Assessment of progressive collapsing foot deformity using semiautomated 3D measurements derived from weightbearing CT scans. Foot Ankle Int. 2022;43(3):363-370. doi: 10.1177/10711007211049754 [DOI] [PubMed] [Google Scholar]
- 7. Kvarda P, Krähenbühl N, Susdorf R, Burssens A, Ruiz R, Barg A, Hintermann B. High reliability for semiautomated 3D measurements based on weightbearing CT scans. Foot Ankle Int. 2022;43(1):91-95. doi: 10.1177/10711007211034522 [DOI] [PubMed] [Google Scholar]
- 8. Lee HY, Mansur NS, Lalevee M, et al. Does metatarsus primus elevatus really exist in hallux rigidus? A weightbearing CT case-control study. Arch Orthop Trauma Surg. Published online September 9, 2021. doi: 10.1007/s00402-021-04168-5 [DOI] [PubMed] [Google Scholar]
- 9. Richter M, Schilke R, Duerr F, Zech S, Andreas Meissner S, Naef I. Automatic software-based 3D-angular measurement for Weight-Bearing CT (WBCT) provides different angles than measurement by hand. Foot Ankle Surg. 2022;28(7):863-871. doi: 10.1016/j.fas.2021.11.010 [DOI] [PubMed] [Google Scholar]
- 10. Scheele CB, Christel ST, Fröhlich I, et al. A cone beam CT based 3D-assessment of bony forefoot geometry after modified Lapidus arthrodesis. Foot Ankle Surg. 2020;26(8):883-889. doi: 10.1016/j.fas.2019.11.006 [DOI] [PubMed] [Google Scholar]