Abstract
Objectives:
Chronic obstructive pulmonary disease (COPD) is the most common co-morbidity associated with non-small cell lung cancer (NSCLC) patients. Immune checkpoint inhibitors related pneumonitis (CIP) is a common immune-related adverse event that can be life-threatening. The study aims to evaluate the association of COPD with the incidence and outcome of CIP in NSCLC patients receiving immune checkpoint inhibitors (ICIs).
Materials and methods:
We retrospectively collected data from 122 patients diagnosed with NSCLC and treated with ICIs in our department. Baseline pulmonary function was performed in the whole cohort. The incidence, risk factors, treatment and outcome of CIP patients were evaluated. Furthermore, the efficacy of ICIs in patients with COPD was analyzed.
Results:
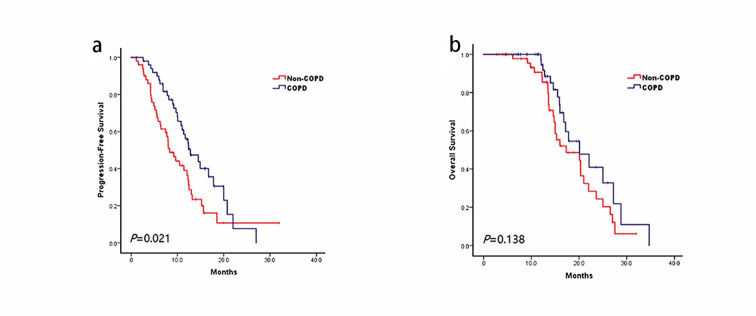
Nineteen patients (15.5%, 19/122) developed CIP during ICIs treatment, most patients with CIP were grade 1–2, and the incidence of CIP was comparable in patients with COPD and those without COPD (18.0% vs. 13.1%, P = 0.618). In addition, an increasing trend in the incidence of CIP among patients with pulmonary fibrosis on baseline chest CT scans (27.3% vs. 13.0%, P = 0.093). There is a longer progression-free survival in COPD patients than the non-COPD patients.
Conclusion:
Coexisting COPD did not predict the higher risk of CIP in NSCLC treated with ICIs therapy. Nevertheless, pre-existing pulmonary fibrosis on CT scan may increase the risk of CIP, close monitoring is advised in these patients during ICIs.
Keywords: Checkpoint inhibitors related pneumonitis, Chronic obstructive pulmonary disease, Immune-related adverse events, Immune checkpoint inhibitors, Lung cancer
Introduction
Lung cancer is the major cause of cancer-related deaths worldwide [1]. The anti-programmed cell death 1 (PD-1)/anti-programmed cell death-ligand 1 (PD-L1) immune checkpoint inhibitors (ICIs) block immune checkpoint pathways, activating a tumor specific T cell immune response [2]. Clinical trials have demonstrated that immunotherapy showed a significant clinical and survival benefit to advanced non-small cell lung cancer (NSCLC) patients [3, 4]. Clinical trials reported a higher quality of life and less treatment-related toxicity with ICIs than standard chemotherapy; however, ICIs have unique side effects in various organs, termed immune-related adverse events (irAEs). The irAE profiles vary from tumor types, and different immune microenvironments may drive histology-specific irAE patterns [5]. A previous study indicated that immune checkpoint inhibitors related pneumonitis (CIP) might occur more often and have a faster onset in NSCLC than in other types of cancer [6]. CIP is a life-threatening irAE that may result in wide-ranging respiratory symptoms with pulmonary parenchymal abnormalities and result in respiratory failure. Although a few research has been done, the risk factors of CIP remain inconclusive [6]. The assessment of the risk factors for CIP and other life-threatening irAEs is a growing clinical need in the effort to personalize and predict the side effects of cancer therapy. Previous studies have suggested that the presence of chronic inflammation prior to immunotherapy, such as rheumatoid arthritis, and lupus, can confer an increased risk of irAEs that involve the target organ of prior injury [7]. Pre-existing pulmonary diseases, including asthma, interstitial lung disease (ILD), pneumothorax and pleural effusion have been reported to be closely associated with the development of CIP in patients with NSCLC [8–11].
Chronic obstructive pulmonary disease (COPD) is a common comorbidity in lung cancer. COPD prevalence in newly-diagnosed lung cancer patients was estimated about 50%, and COPD is considered an independent risk factor of lung cancer [12, 13]. Increasing evidence supports that lung cancer patients with coexistence of COPD might respond better to immunotherapy, which can partially be attributed to the fact that the expression of immune checkpoint proteins PD-1 and PD-L1 is dysregulated in COPD patients [14]. However, the safety of ICIs in lung cancer patients with coexistence of COPD, especially the incidence and outcome of CIP is uncertain. Given the high prevalence of COPD in the lung cancer population and the clinical imperative to determine the comorbidities that might increase a patient’s risk of immune-related pneumonitis, we sought to investigate whether a prior diagnosis of COPD was associated with a higher incidence of CIP. Moreover, we also explored the correlations between clinical risk factors such as pulmonary computed tomography (CT) abnormalities (fibrosis/emphysema) at baseline and the incidence of CIP in lung cancer patients with COPD.
Materials and methods
Patients and study approval
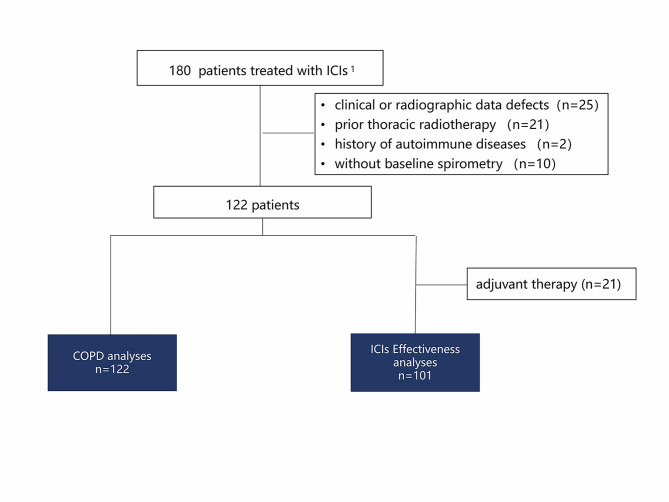
Consecutive patients with histologically confirmed NSCLC who received PD-1 antibodies (nivolumab or pembrolizumab) as routine treatment at the First Affiliated Hospital, College of Medicine, Zhejiang University between December 1, 2018, and May 1, 2021 were reviewed. The last follow-up occurred on December 1, 2021. Patients who received at least 2 cycles of ICIs treatment and underwent chest CT in the 3 months before and after anti-PD-1 therapy were included in this study. Patients with a history of using prior ICIs, thoracic radiotherapy, previous history of autoimmune disease, a previous known history of ILD before diagnosis of lung cancer and required pharmacotherapies to alleviate the symptoms were excluded. The whole cohort was enrolled to analyze the correlation of COPD with the risk of CIP. Among the 122 patients, 21 patients received ICIs as neoadjuvant therapy (stage IIB and IIIA). Hence the overall survival (OS) and progression-free survival (PFS) of ICIs were evaluated in 101 stage IV NSCLC patients. Clinical and treatment information was obtained from our electronic medical records. This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (Registration No. IIT20220383A). Individual consent for this study was waived by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine as the privacy of the patients has not been disclosed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Radiographic and pulmonary function analysis
Baseline chest CT scan findings and pulmonary function testing were recorded, the most recent chest CT scan obtained before the initiation of ICI treatment was recorded as a baseline. A retrospective radiology review of serial chest CT scans of all patients was independently performed by two respiratory physicians. The fibrosis (F) and emphysema (E) scores were evaluated according to the scoring system reported in previous studies [15–17]. The fibrosis score (F score, 0–5) was visually evaluated according to the interlobular septal thickening and discrete honeycombing area, while the emphysema score (E score, 0–4) was determined visually according to the diameter of low attenuation areas (Table 1). Pulmonary function measurements, including spirometry and diffusing capacity of the lung for carbon monoxide (DLco), were performed using respiratory analyzer (Quark PFT, COSMED, Rome, Italy). Diagnoses and classifications of COPD were made in accordance with the Global Initiative for Chronic Obstructive Lung Disease criteria [18], which COPD were defined as those having a forced expiratory volume in 1 s (FEV1) to forced vital capacity ratio (FVC) < 0.7 after bronchodilator use.
Table 1.
Score systems of fibrosis and emphysema
| Fibrosis score(F score) | Emphysema score (E score) | |
|---|---|---|
| 0 | No fibrosis | No low attenuation areas (LAAs) |
| 1 | Interlobular septal thickening; no discrete honeycombing | Sparse, scattered small LAAs up to 5 mm in diameter |
| 2 | Honeycombing (with or without septal thickening) involving < 25% of the lobe | Adjacent LAAs up to 10 mm in diameter |
| 3 | Honeycombing (with or without septal thickening) involving 25–49% of the lobe | LAAs > 10 mm that were adjacent to or indispensable from each other |
| 4 | Honeycombing (with or without septal thickening) involving 50–75% of the lobe | Absence of normal lung parenchyma |
| 5 | Honeycombing (with or without septal thickening) involving > 75% of the lobe | NA |
LAAs, low attenuation areas
Adverse events and response evaluation
Adverse events were graded according to the Common Terminology Criteria for Adverse Events (CTCAE), version 5.0. Management of irAEs based on AE severity following standard protocol guidelines [19]. The treating physician made all treatment strategy decisions. Since CIP is a diagnosis of exclusion, we also used criteria that were reported previously to assess the presence of CIP [20]. The patient was included in the CIP group for analyses only in cases meeting the definite criteria, patients with clinically apparent alternative diagnoses such as pulmonary infection, tumor progression, heart failure, or other etiologies were excluded. The response evaluation of PD-1 inhibitor was based on the immune-related Response Evaluation Criteria in Solid Tumors [21]. PFS was calculated from the first day of immunotherapy to the first radiological evidence of disease progression. OS was defined as the interval from the start of ICIs to the last visit or death. Censored data were defined as data from alive patients and had no evidence of disease progression at the last follow-up visit.
Statistical analysis
Clinical characteristics, including age, gender, smoking history, tumor histology, Eastern Cooperative Oncology Group (ECOG) status, TNM stage, genetic profiles, adverse events and line of treatment were analyzed. Differences between clinic pathological characteristics was performed using the Chi-squared (Fisher’s exact test) for categorical data, and Wilcoxon rank-sum tests for continuous variables. Kaplan-Meier methodology was used to calculate median PFS and OS. All analyses were conducted using SPSS software (ver.22.0). The p values were two-tailed, and p values < 0.05 were considered statistically significant.
Result
Patient characteristics
A total of 122 consecutive lung cancer patients were enrolled in the study (Fig. 1).
Fig. 1.
Patient flow chart of study profile. 1nivolumab or pembrolizumab. Abbreviations: CIP, checkpoint inhibitors related pneumonitis; COPD, chronic obstructive pulmonary disease
, all patients were of Chinese ethnicity. Pulmonary function tests (PFTs) are routinely performed before ICIs, starting as a screen for underlying respiratory abnormalities and baseline lung function measurements. According to the definition of chronic obstructive lung disease criteria, 50% of them (61/122) were identified as COPD.
Baseline characteristics were balanced between the lung cancer patients with and without COPD groups (Table 2). The median age of patients was 66 (range, 45–89) years old. Most patients (95.1%, 116/122) were male and had a smoking history (70.5%, 86/122). Squamous cell carcinoma (54.9%, 67/122) represents the dominant histologic subtypes, while 48 (39.4%) patients were diagnosed with adenocarcinoma lung cancer. Molecular testing, including EGFR/KRAS/NRAS/BRAF/HER-2/MET/PI3KCA mutation and ALK/ROS1/RET fusion, was performed in 41% (59/122) of patients. The expression of PD-L1 was detected by immunohistochemistry (IHC) in thirteen patients (10.7%, 13/122). Among the 13 patients whose PD-L1 expression was detected, ≥ 50% of tumor cells exhibited PD-L1 expression in were observed in 3 patients (23.0%, 3/13), 5 patients (38.5%, 5/13) with PD-L1 expression 1-49%, while 5 patients (38.5%, 5/13) with PD-L1 expression ≤ 1%.
Table 2.
Clinical characteristics of patients (N = 122)
| Cohort (N = 122) |
Groups(%) | P | ||
|---|---|---|---|---|
| COPD (N = 61) |
Non-COPD (N = 61) |
|||
| Age | 0.230 | |||
| median | 66 | 67 | 66 | |
| range | 45–89 | 50–83 | 45–89 | |
| Sex | 0.680 | |||
| Male | 116(95.1) | 59(96.7) | 57(93.4) | |
| Female | 6(4.9) | 2(3.3) | 4(6.6) | |
| Smoking history | 0.073 | |||
| Never-smokers | 36(29.5) | 13(21.3) | 23(37.7) | |
| Ever-smokers | 86(70.5) | 48(78.7) | 38(62.3) | |
| Histology | 0.053 | |||
| Adenocarcinoma | 48(39.4) | 19(31.1) | 29(47.5) | |
| Squamous | 67(54.9) | 40(65.6) | 27(44.3) | |
| Others | 7(5.7) | 2(3.3) | 5(8.2) | |
| ECOG performance status | 0.752 | |||
| 0–1 | 120(98.4) | 60(98.4) | 60(98.4) | |
| 2–3 | 2(1.6) | 1(1.6) | 1(1.6) | |
| Genetic profile | 0.037 | |||
| EGFR | 4(3.3) | 1(1.6) | 3(4.9) | |
| KRAS | 7(5.7) | 1(1.6) | 6(9.8) | |
| Others | 3(2.5) | 1(1.6) | 2(3.3) | |
| Negative | 36(29.5) | 14(23.0) | 22(36.1) | |
| NA | 72(59.0) | 44(72.1) | 27(44.3) | |
| Fibrosis score | 0.638 | |||
| 0 | 100(82.0) | 49(80.3) | 51(83.6) | |
| ≥1 | 22(18.0) | 12(19.7) | 10(16.4) | |
| Emphysema score | 0.003 | |||
| 0 | 75(62.0) | 29(47.5) | 46(75.4) | |
| ≥ 1 | 47(38.0) | 32(52.5) | 15(24.6) | |
| Baseline spirometry | 0.642 | |||
| DLco% predicted* | 69.9(16.8) | 65.9(15.2) | 73.5(17.4) | |
| irAE | 0.211 | |||
| No | 90(73.8) | 41(67.2) | 49(80.3) | |
| CIP | 19(15.6) | 11(18.0) | 8(13.1) | |
| Other irAE | 13(10.7) | 9(14.8) | 4(6.6) | |
| Treatment line | 0.847 | |||
| Adjuvant | 21(17.2) | 11(18.0) | 10(16.4) | |
| First-line | 77(63.1) | 38(62.3) | 39(63.9) | |
| Second-line | 16(13.1) | 7(11.5) | 9(14.8) | |
| Subsequent-line | 8(6.6) | 5(8.2) | 3(4.9) | |
CIP, checkpoint inhibitors related pneumonitis; COPD, chronic obstructive pulmonary disease; DLco, diffusing capacity of the lung for carbon monoxide; ECOG, Eastern Cooperative Oncology Group; EGFR: epidermal growth factor receptor; KRAS, Kirsten rat sarcoma viral oncogene homolog; NA, not available; irAE, immune-related adverse events
*Values in the table represent means (standard deviation)
Incidence of CIP in COPD patients
Generally, anti-PD-1 immunotherapy was well tolerated in lung cancer patients with COPD, the side effects are balanced in patients with and without COPD. Among the 122 patients, 19 (15.6%, 19/122) met the criteria and were diagnosed as CIP, 4 cases were grade 1, 11 were grade 2, 3 were grade 3, and 1 was grade 4. There were 11 patients with COPD who developed CIP, corresponding to 18.0% (11/61) of the COPD patients compared to 13.1% (8/61) of the non-COPD patients (P = 0.618). Among the 61 patients with COPD, none have spirometry-defined GOLD stage 4 (Table 3). The incidence of CIP showed no statistical difference among groups across GOLD stages (P = 0.796), 20% (4/20) of patients in GOLD 1 group developed CIP compared with 13.6% (3/22) in GOLD 2 group and 21.1% (4/19) in GOLD 3 group.
Table 3.
The incidence of CIP according to GOLD stage in patients with COPD
| Total N = 61 |
Non-CIP (%) n = 50 |
CIP (%) n = 11 |
P | |
|---|---|---|---|---|
| GOLD | 0.796 | |||
| 1 | 20 | 16 (80.0) | 4 (20.0) | |
| 2 | 22 | 19 (86.4) | 3 (13.6) | |
| 3 | 19 | 15 (78.9) | 4 (21.1) | |
| 4 | 0 | 0 (0) | 0 (0) |
Abbreviations: CIP, checkpoint inhibitors related pneumonitis; COPD, chronic obstructive pulmonary disease; GOLD, chronic obstructive lung disease
Risk factors of CIP
The hypothesized risk factors for CIP were analyzed. In our cohort, 15.5% (19/122) patients with an F score of 1, 2.5% (3/122) patients with an F score of 2, and 82% of patients (100/122) with an F score of 0. The incidence of CIP in patients with an F score 0 was 13% (13/100). CIP occurred in 6 of 22 patients with fibrosis, higher than in patients without fibrosis in baseline CT scan (27.3% vs. 13.0%), but this difference did not reach statistical significance (P = 0.093). In contrast, in F score 1 patient with mild fibrosis and no discrete honeycombing, the incidence of CIP was 31.6% (6/19). However, no CIP occurred in F score 2 patients with honeycombing (0/3). The severity of pulmonary fibrosis score is uncorrelated with CIP (P = 0.102). Among 61 COPD patients, 12 patients with combined pulmonary fibrosis and emphysema (CPFE), the incidence of CIP in these patients was 25.0% (3/12), compared with 16.3% (8/49) in COPD patients (P = 0.676).
Emphysema, defined as an E score ≥ 1, was present in 47 patients (38.5%, 47/122). However, the presence of emphysema in the baseline did not affect the incidence of CIP (14.7% vs. 17.0%, P = 0.727). The incidence of CIP in patients with E score 0 was 14.7% (11/75), in E score 1 patient the incidence was 9.4% (3/32), and 41.7% in E score 2 (5/12). No CIP occurred in E score 3 patients (0/3), and the severity of emphysema score is uncorrelated with CIP (P = 0.051) either. Meanwhile, smoking history, gender, histologic tumor subtype and genetic profile did not significantly affect the risk of CIP developing.
Treatment and outcome of patients who developed CIP
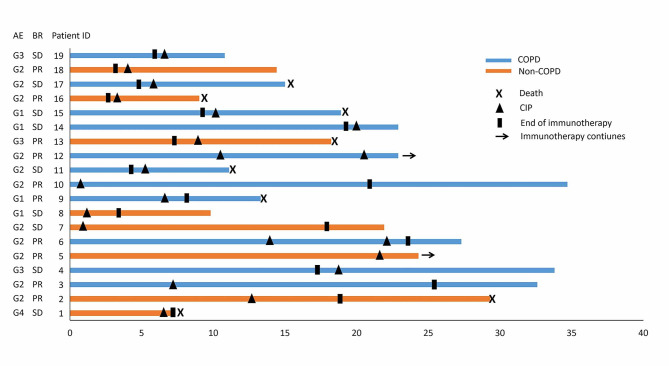
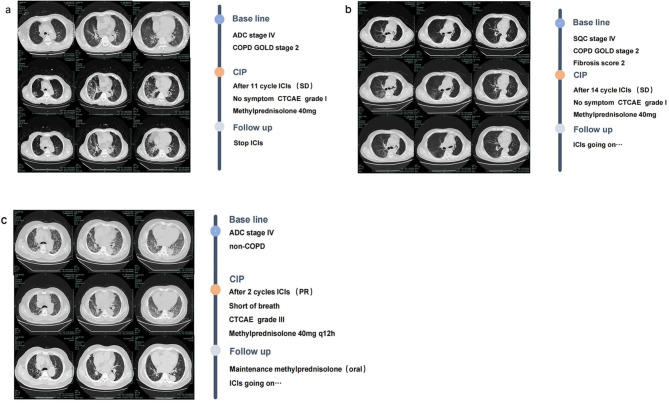
Figure 2 shows the details of the treatment regimens for CIP, CTCAE grade, and clinical courses. Among 19 patients who were observed to develop CIP, the median time to CIP diagnosis from initial ICI treatment was 6.6 months (range 0.6–22.6 months). The predominant respiratory symptoms patients complained of were shortness of breath and cough. In addition, ICIs were withheld and systemic corticosteroid therapy was initiated in 84.2% (16/19) patients as soon as CIP was diagnosed. The remaining 3 patients with CIP demonstrated only radiographic progress, yet without respiratory symptoms, were diagnosed as grade 1 and no one received adjunct treatments to corticosteroids for CIP. Among patients who received systemic corticosteroid for CIP, 93.7% (15/16) patients were improved in both imaging and symptoms after treatment, only one patient (grade 4) died 16 days later of CIP diagnosis. 36.8% of patients (7/19), all with grade 1–2 CIP, were rechallenged with ICIs for treatment of CIP, and two of them (28.6%, 2/7) showed recurrence of CIP (Fig. 2). Fortunately, the two patients with recurrence of CIP recovered on withdrawal of ICIs finally. No clear patterns emerged to differentiate the COPD-CIP from the non-COPD-CIP imaging findings. The CT images of the CIP cases are shown in Fig. 3.
Fig. 2.
Overall survival follow-up of patients with CIP. Abbreviations: AE, adverse events; BR, best response; CIP, checkpoint inhibitors related pneumonitis; COPD, chronic obstructive pulmonary disease; G, grade of toxicity according to common terminology criteria for adverse events; PR, partial response; SD, stable disease
Fig. 3.
Computed tomography scan evolution of three patients developed CIP (a) patient with coexisting lung adenocarcinoma and COPD. (b) patient with pre-existing pulmonary fibrosis who presents with both lung squamous cell carcinoma and COPD. (c) lung adenocarcinoma patient without COPD. Abbreviations: ADC, adenocarcinoma; CIP, checkpoint inhibitors related pneumonitis; COPD, chronic obstructive pulmonary disease; CTCAE, common terminology criteria for adverse events, GOLD, chronic obstructive lung disease; ICI, immune checkpoint inhibitor; PR, partial response; SD, stable disease; SQC, squamous cell carcinoma
Treatment outcomes of ICIs in NSCLC patients with and without COPD
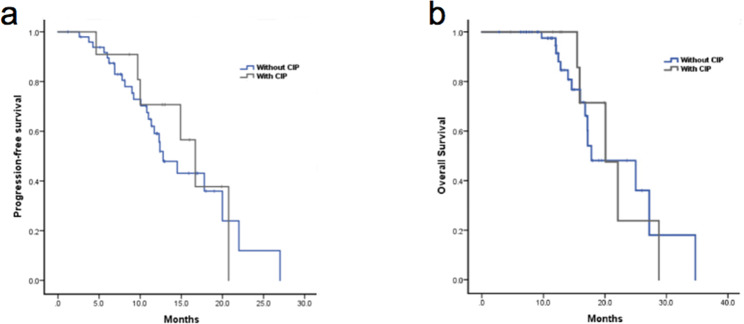
In the cohort, 96.7% of patients (118/122) received pembrolizumab, and the other 4 patients received nivolumab. ICIs were used predominantly in the first-line setting (63.1%, 77/122), 17.2% (21/122) received ICIs as adjuvant therapy, and the remaining 19.7% (24/122) received ICIs as second or later line immunotherapy. 87.7% of patients (107/122) received ICIs combined with chemotherapy, and single-agent anti-PD-1 immunotherapy was given to 12.3% of patients (15/122). Among these patients, 5 patients received single-agent PD-1 inhibitor as first-line therapy for their poor ECOG status or advanced age, 7 patients received single-agent as second-line therapy, and the remaining 3 patients received single-agent as subsequent treatment. Paclitaxel was an especially common agent combined with ICIs, as it was used in 92.5% (62/67) patients with squamous cell lung cancer. Whereas 75% (36/48) of patients diagnosed with adenocarcinoma received pemetrexed combined with ICIs. The survival analysis was performed on 101 patients (90%, 101/122) with metastatic NSCLC. At the time of chart extraction, 68.3% (69/101) of patients experienced disease progression. PFS was 11.4 months (95% CI = 9.2–13.5 months) for the whole cohort. Patients in the COPD group experienced a median PFS of 12.8 months (95% CI = 9.3–12.3 months) compared with only 8.3 months (95% CI = 6.2–10.5 months, P = 0.021) in patients without COPD (Fig. 4a). At the end of the last follow-up time, 45.5% (46/101) patients had died. The median OS was 20.1 months (95% CI = 16.6–23.6) in all study subjects. Median OS after ICI initiation was 20.1 months (95% CI = 14.4–25.8 months) for patients with COPD and 17.3 months (95% CI = 9.7–24.9 months) for patients without COPD (P = 0.138, Fig. 4b). Although no statistical difference was found between groups, there was a trend toward improved OS in the COPD group compared with that in a non-COPD group.
Fig. 4.
Kaplan–Meier curves of (a) progression-free survival and (b) overall survival in advanced lung cancer patients who received ICIs. Abbreviations: COPD, chronic obstructive pulmonary disease; ICI, immune checkpoint inhibitor
Treatment outcomes of ICIs in COPD patients with and without CIP
For patients with spirometry-defined COPD, the Kaplan-Meier curves are shown in Fig. 5. COPD patients who developed CIP were more likely to have longer PFS (16.7 vs. 12.8 months, P = 0.67, Fig. 5a) and OS (20.1 vs. 17.8 months, P = 0.90, Fig. 5b) compared with those without CIP, however the differences did not reach significance.
Fig. 5.
Treatment outcomes of ICIs in spirometry-defined COPD patients with and without CIP. Kaplan-Meier curve of (a) progression-free survival and (b) overall survival. Abbreviations: COPD, chronic obstructive pulmonary disease; ICI, immune checkpoint inhibitor
Discussion
In this retrospective study, we analyzed the potential risk factors and their association with the incidence of CIP. No significant association was observed between COPD and CIP. To the best of our knowledge, this is the largest study to evaluate the impact of spirometry-defined COPD on the incidence and outcome of CIP in patients with NSCLC.
Lung cancer is the first cause of death in patients with COPD [22]. COPD is a disease associated with chronic inflammation of the airways and lung parenchyma, characterized by persistent lung injury, activates a regulatory mechanism that downgrades the immune response, including PD-L1/PD-1 [23], and thus opening a therapeutic window among patients with COPD who develop lung cancer. Despite the proven longer PFS in lung cancer patients with COPD [24–26], the uncertain safety may limit the use of ICIs. Since it is biologically plausible for immunotherapy to stimulate lymphocytes against healthy lung cancer cells, increasing lung tissue damage and COPD symptoms. Nair et al. reported a series of patients with prolonged and severe COPD exacerbations upon initiating immune checkpoint inhibitor therapy, indicating ICIs may aggravate CODP and irAE [27]. However, given the stringent eligibility criteria applied in clinical trials, healthier patients tend to be enrolled, and thus the real-world frequency of these events in the overall population is unknown. Findings from three recent studies indicated that COPD might associate with CIP [20, 28, 29]. However, these studies have not accounted for some crucial potential confounding factors. Atchley et al. [20] showed that obstructive lung disease was independently associated with CIP (aOR, 2.79; 95% CI, 1.07–7.29). It is noteworthy that the history of COPD is not a statistically significant risk factor for CIP in multivariate logistic regression analysis. Moreover, only 24.1% of these patients had documented baseline spirometry. Additionally, patients with ILD, connective tissue disease (CTD), and prior thoracic radiation history were included in the above research for CIP analysis, while the clinical variables mentioned above have been demonstrated as an independent risk factors for the development of CIP [6, 30, 31]. All the mentioned interfering factors above are difficult to distinguish from the risk conferred by COPD. Another study by Sul et al. [28] recapitulated this finding that CIP occurred more frequently in patients with a history of COPD and asthma than in patients without this history (5.4% vs. 3.1%). Unfortunately, in the study COPD and asthma were grouped together, which could be inappropriate given that the pathophysiology and dominant immunologic mechanisms involved differ [32]. A recent retrospective study reported that the presence of COPD was independently associated with a higher incidence of CIP, 70% of the patients in the CIP group had COPD. Unfortunately, the study investigated this association using physician-diagnosed COPD [29].
Notably, the incidence of CIP was similar in patients regardless of COPD status (18.0% vs. 13.1%, P = 0.618) in our study. The discrepancy might be partly attributed to the confounding factors in the previous study, and therefore, conclusions from these studies to be addressed with caution. Overcoming these limitations, the present study firstly showed that coexisting spirometry-defined COPD was not an independent risk factor for patients with lung cancer who have co-morbid COPD. In our study, the incidence of all CIP was 15.5% (19/122), and the incidence for grade ≥ 3 CIP was 3.3% (4/122), which is consistent with a prior report [6]. With timely and appropriate systemic corticosteroid treatment, the clinical symptoms and imaging changes of CIP can be improved in most patients (93.8%, 15/16). These results support the clinical observation that lung cancer patients can be treated safely with ICI in the context of COPD, and treatment-related irAEs were found to be manageable in COPD patients.
Pre-existing ILD has been reported to exist in approximately 15% of lung cancer patients at the time of initial diagnosis and is associated with a poor prognosis [33, 34]. Since patients with pre-existing pulmonary fibrosis are often excluded in clinical trials of immunotherapy to avoid CIP, the relationship between them needs to be further elucidated. Interstitial lung abnormalities (ILA) are defined as increased lung densities on chest computed tomography images of patients without previous history of ILD [35]. In our retrospective study, analysis according to the F score on baseline CT was analyzed in patients with ILA. The incidence of CIP was similar in two arms, which is inconsistent with previous studies [9, 11, 17]. This may partially attribute to the small sample size of patients with pre-existing pulmonary fibrosis in our study, and thus could not detect the group differences. Additionally, consideration is given to potential harms in the individual patients, physician may be more cautious to prescribe ICIs to patients with severe CT abnormalities (fibrosis/emphysema) in clinical practice. In our study, only 3 patients with F score 2 (presence of honeycomb lungs) received ICIs. According to the result of a phase 2 trial of atezolizumab for pretreated NSCLC with idiopathic interstitial pneumonitis, there is a particularly high risk of CIP in patients with a honeycomb lung on HRCT [11].
We also compared other clinical variables such as smoking history, older age, poor performance status, and underlying medical comorbidities, considered high-risk factors for drug-induced ILD [9, 30, 36]. No significant association was observed between groups according to the variables mentioned above.
Previous study indicated that some patients didn’t meet the spirometric standard of COPD have evidence of structural lung disease (emphysema, gas trapping) on chest imaging, these patients may experience a high risk of lung function decline and have potential to develop COPD in the future [37]. Previous studies reported that pre-existing pulmonary emphysema on baseline chest CT is not a risk factor for CIP [17, 20]. In our study, 24.6% (15/61) of patients in non-COPD group with emphysema in baseline CT scan, we also analyzed the relationship between E score and CIP. Consistent with previous studies, no relation between E score and CIP was revealed in our study.
Several retrospective studies suggest a longer PFS to ICIs in NSCLC patients with COPD compared to those without COPD [24, 26, 38]. However, there was also a limitation in the studies, only a small proportion of patients had documented spirometry in baseline and investigated COPD using physician-diagnosed COPD [24, 26]. In our study, we confirmed the conclusion in spirometry-defined COPD patients with co-morbid lung cancer. Moreover, the findings of previous studies were inconsistent regarding OS. A retrospective study in China was found a prolonged OS in the subgroup of patients with mixed ventilatory defects [26]. Nevertheless, numerous diseases are causing mixed ventilatory pulmonary, and the pathophysiology and underlying molecular mechanisms are different. Therefore, the difference in OS between groups cannot solely be attributed to COPD and the conclusion of the study should be treated with caution. Previous studies demonstrated patients with irAE, especially with lower-grade irAE was associated with better outcomes in patients with ICI treatment for NSCLC [39, 40]. In this study, 78.9% patients (15/19) with grade 1 or 2 CIP. Likewise, we observed that patients with CIP had longer median PFS and OS versus those without CIP in COPD subgroup, but the difference was not statistically significant given the limited sample size.
There are several limitations to this study, which should be addressed. First, the retrospective nature of this study is prone to biases from missing data and reliance on the documentation available for review. Second, the number of patients with CIP might not be sufficient to provide reliable information concerning the significance of the subgroup analysis according to COPD severity. Third, due to the scarcity of lung tissue from patients who received an ICIs, we lacked data regarding the PD-L1 expression and tumor mutational burden (TMB) of patients with COPD, unable to explore the potential interaction between COPD and immune profile. However, our data may be more informative in a real-world clinical setting, as clinical trials have demonstrated that patients achieved clinical benefit from ICI combined chemotherapy irrespective of PD-L1 expression [41], and patients who undergo palliative immunotherapy for NSCLC do not routinely undergo PD-L1 or TMB detection. Further prospective studies are needed to elucidate the complex relationship between the immune profile in tumor and the incidence of CIP in the context of COPD.
Conclusion
The finding of our study identifying coexisting COPD did not predict the higher risk of CIP, and supports the clinical observation that lung cancer patients can be treated safely with ICIs in the context of COPD. Although there is no statistic difference, an increasing trend in the incidence of CIP among patients with pulmonary fibrosis on baseline chest CT scans. Moreover, we confirmed that COPD was associated with a longer PFS to ICI treatment, by using an objective measure for COPD diagnosis in NSCLC patients. This study fills an essential gap in the literature and supplements the limited number of published reports on CIP in the context of COPD. Further clinical studies are warranted to validate these findings.
Acknowledgements
The authors would like to thank all study participants and their families.
Author contributions
Zhu Zeng, Yuehong Wang and Jianying Zhou contributed to the study conception and design. Material preparation, data collection and analysis were performed by Zhu Zeng, Jingjing Qu, Yake Yao, Fei Xu, Shan Lu, Pei Zhang, Yinan Yao and Ning Li. The first draft of the manuscript was written by Zhu Zeng and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This research was supported by National Natural Science Foundation of China under Grant Number 82002411; Natural Science Foundation of Zhejiang Province under Grant Number LQ19H160042; the key projects of Natural Science Foundation of Zhejiang Province under Grant Number LZ22H160011.
Availability of data and materials
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine (Registration No. IIT20220383A). Individual consent for this study was waived by the Ethics Committee of the First Affiliated Hospital, Zhejiang University School of Medicine as the privacy of the patients has not been disclosed. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Consent to publish
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jianying Zhou, Email: zjyhz@zju.edu.cn.
Yuehong Wang, Email: yuehongw@zju.edu.cn.
References
- 1.Siegel RL, Miller KD, Jemal A. Cancer statistics. 2020. CA Cancer J Clin. 2020;70(1):7–30. Epub 2020/01/09. 10.3322/caac.21590. [DOI] [PubMed]
- 2.Akinleye A, Rasool Z. Immune checkpoint inhibitors of PD-L1 as cancer therapeutics. J Hematol Oncol. 2019;12(1):92. doi: 10.1186/s13045-019-0779-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reck M, Rodriguez-Abreu D, Robinson AG, Hui R, Csoszi T, Fulop A, Gottfried M, Peled N, Tafreshi A, Cuffe S, O’Brien M, Rao S, Hotta K, Leiby MA, Lubiniecki GM, Shentu Y, Rangwala R, Brahmer JR, Investigators K. Pembrolizumab versus Chemotherapy for PD-L1-Positive Non-Small-Cell Lung Cancer. N Engl J Med. 2016;375(19):1823–33. doi: 10.1056/NEJMoa1606774. [DOI] [PubMed] [Google Scholar]
- 4.Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, Molina J, Kim JH, Arvis CD, Ahn MJ, Majem M, Fidler MJ, de Castro G, Jr, Garrido M, Lubiniecki GM, Shentu Y, Im E, Dolled-Filhart M, Garon EB. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387(10027):1540–50. doi: 10.1016/S0140-6736(15)01281-7. [DOI] [PubMed] [Google Scholar]
- 5.Khoja L, Day D, Wei-Wu Chen T, Siu LL, Hansen AR. Tumour- and class-specific patterns of immune-related adverse events of immune checkpoint inhibitors: a systematic review. Ann Oncol. 2017;28(10):2377–85. doi: 10.1093/annonc/mdx286. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Q, Tang L, Zhou Y, He W, Li W. Immune Checkpoint Inhibitor-Associated Pneumonitis in Non-Small Cell Lung Cancer: Current Understanding in Characteristics, Diagnosis, and Management. Front Immunol. 2021;12:663986. doi: 10.3389/fimmu.2021.663986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Menzies AM, Johnson DB, Ramanujam S, Atkinson VG, Wong ANM, Park JJ, McQuade JL, Shoushtari AN, Tsai KK, Eroglu Z, Klein O, Hassel JC, Sosman JA, Guminski A, Sullivan RJ, Ribas A, Carlino MS, Davies MA, Sandhu SK, Long GV. Anti-PD-1 therapy in patients with advanced melanoma and preexisting autoimmune disorders or major toxicity with ipilimumab. Ann Oncol. 2017;28(2):368–76. doi: 10.1093/annonc/mdw443. [DOI] [PubMed] [Google Scholar]
- 8.Galant-Swafford J, Troesch A, Tran L, Weaver A, Doherty TA, Patel SP. Landscape of Immune-Related Pneumonitis in Cancer Patients with Asthma Being Treated with Immune Checkpoint Blockade. Oncology. 2020;98(2):123–30. doi: 10.1159/000503566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shibaki R, Murakami S, Matsumoto Y, Yoshida T, Goto Y, Kanda S, Horinouchi H, Fujiwara Y, Yamamoto N, Kusumoto M, Yamamoto N, Ohe Y. Association of immune-related pneumonitis with the presence of preexisting interstitial lung disease in patients with non-small lung cancer receiving anti-programmed cell death 1 antibody. Cancer Immunol Immunother. 2020;69(1):15–22. doi: 10.1007/s00262-019-02431-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nishino M, Giobbie-Hurder A, Hatabu H, Ramaiya NH, Hodi FS. Incidence of Programmed Cell Death 1 Inhibitor-Related Pneumonitis in Patients With Advanced Cancer: A Systematic Review and Meta-analysis. JAMA Oncol. 2016;2(12):1607–16. doi: 10.1001/jamaoncol.2016.2453. [DOI] [PubMed] [Google Scholar]
- 11.Ikeda S, Kato T, Kenmotsu H, Ogura T, Iwasawa S, Sato Y, Harada T, Kubota K, Tokito T, Okamoto I, Furuya N, Yokoyama T, Hosokawa S, Iwasawa T, Yamanaka T, Okamoto H. A Phase 2 Study of Atezolizumab for Pretreated NSCLC With Idiopathic Interstitial Pneumonitis. J Thorac Oncol. 2020;15(12):1935–42. doi: 10.1016/j.jtho.2020.08.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brenner DR, McLaughlin JR, Hung RJ. Previous lung diseases and lung cancer risk: a systematic review and meta-analysis. PLoS One. 2011;6(3):e17479. Epub 2011/04/13. 10.1371/journal.pone.0017479. Accession Number|; PMCPMC3069026. [DOI] [PMC free article] [PubMed]
- 13.Young RP, Hopkins RJ, Christmas T, Black PN, Metcalf P, Gamble GD. COPD prevalence is increased in lung cancer, independent of age, sex and smoking history. Eur Respir J. 2009;34(2):380–6. doi: 10.1183/09031936.00144208. [DOI] [PubMed] [Google Scholar]
- 14.Narayanapillai SC, Han YH, Song JM, Kebede ME, Upadhyaya P, Kassie F. Modulation of the PD-1/PD-L1 immune checkpoint axis during inflammation-associated lung tumorigenesis. Carcinogenesis. 2020;41(11):1518–28. doi: 10.1093/carcin/bgaa059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kazerooni EA, Martinez FJ, Flint A, Jamadar DA, Gross BH, Spizarny DL, Cascade PN, Whyte RI, Lynch JP, Toews G. Thin-section CT obtained at 10-mm increments versus limited three-level thin-section CT for idiopathic pulmonary fibrosis: correlation with pathologic scoring. AJR Am J Roentgenol. 1997;169(4):977–83. doi: 10.2214/ajr.169.4.9308447. [DOI] [PubMed] [Google Scholar]
- 16.Satoh K, Kobayashi T, Misao T, Hitani Y, Yamamoto Y, Nishiyama Y, Ohkawa M. CT assessment of subtypes of pulmonary emphysema in smokers. Chest. 2001;120(3):725–9. doi: 10.1378/chest.120.3.725. [DOI] [PubMed] [Google Scholar]
- 17.Yamaguchi T, Shimizu J, Hasegawa T, Horio Y, Inaba Y, Yatabe Y, Hida T. Pre-existing pulmonary fibrosis is a risk factor for anti-PD-1-related pneumonitis in patients with non-small cell lung cancer: A retrospective analysis. Lung Cancer. 2018;125:212–7. doi: 10.1016/j.lungcan.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 18.Vogelmeier CF, Criner GJ, Martinez FJ, Anzueto A, Barnes PJ, Bourbeau J, Celli BR, Chen R, Decramer M, Fabbri LM, Frith P, Halpin DM, Lopez Varela MV, Nishimura M, Roche N, Rodriguez-Roisin R, Sin DD, Singh D, Stockley R, Vestbo J, Wedzicha JA, Agusti A. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Lung Disease 2017 Report. GOLD Executive Summary. Am J Respir Crit Care Med. 2017;195(5):557–82. doi: 10.1164/rccm.201701-0218PP. [DOI] [PubMed] [Google Scholar]
- 19.Postow MA, Sidlow R, Hellmann MD. Immune-Related Adverse Events Associated with Immune Checkpoint Blockade. N Engl J Med. 2018;378(2):158–68. doi: 10.1056/NEJMra1703481. [DOI] [PubMed] [Google Scholar]
- 20.Atchley WT, Alvarez C, Saxena-Beem S, Schwartz TA, Ishizawar RC, Patel KP, Rivera MP. Immune Checkpoint Inhibitor-Related Pneumonitis in Lung Cancer: Real-World Incidence, Risk Factors, and Management Practices Across Six Health Care Centers in North Carolina. Chest. 2021;160(2):731–42. doi: 10.1016/j.chest.2021.02.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Seymour L, Bogaerts J, Perrone A, Ford R, Schwartz LH, Mandrekar S, Lin NU, Litiere S, Dancey J, Chen A, Hodi FS, Therasse P, Hoekstra OS, Shankar LK, Wolchok JD, Ballinger M, Caramella C, de Vries EGE, group Rw iRECIST: guidelines for response criteria for use in trials testing immunotherapeutics. Lancet Oncol. 2017;18(3):e143-e52. doi: 10.1016/S1470-2045(17)30074-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mirza S, Clay RD, Koslow MA, Scanlon PD. COPD Guidelines: A Review of the 2018 GOLD Report. Mayo Clin Proc. 2018;93(10):1488 – 502. Epub 2018/10/06. 10.1016/j.mayocp.2018.05.026. [DOI] [PubMed]
- 23.Francisco LM, Salinas VH, Brown KE, Vanguri VK, Freeman GJ, Kuchroo VK, Sharpe AH. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med. 2009;206(13):3015–29. doi: 10.1084/jem.20090847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mark NM, Kargl J, Busch SE, Yang GHY, Metz HE, Zhang H, Hubbard JJ, Pipavath SNJ, Madtes DK, Houghton AM. Chronic Obstructive Pulmonary Disease Alters Immune Cell Composition and Immune Checkpoint Inhibitor Efficacy in Non-Small Cell Lung Cancer. Am J Respir Crit Care Med. 2018;197(3):325–36. doi: 10.1164/rccm.201704-0795OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Biton J, Ouakrim H, Dechartres A, Alifano M, Mansuet-Lupo A, Si H, Halpin R, Creasy T, Bantsimba-Malanda C, Arrondeau J, Goldwasser F, Boudou-Rouquette P, Fournel L, Roche N, Burgel PR, Goc J, Devi-Marulkar P, Germain C, Dieu-Nosjean MC, Cremer I, Herbst R, Damotte D. Impaired Tumor-Infiltrating T Cells in Patients with Chronic Obstructive Pulmonary Disease Impact Lung Cancer Response to PD-1 Blockade. Am J Respir Crit Care Med. 2018;198(7):928–40. doi: 10.1164/rccm.201706-1110OC. [DOI] [PubMed] [Google Scholar]
- 26.Zhou J, Chao Y, Yao D, Ding N, Li J, Gao L, Zhang Y, Xu X, Zhou J, Halmos B, Tsoukalas N, Kataoka Y, de Mello RA, Song Y, Hu J. Impact of chronic obstructive pulmonary disease on immune checkpoint inhibitor efficacy in advanced lung cancer and the potential prognostic factors. Transl Lung Cancer Res. 2021;10(5):2148–62. doi: 10.21037/tlcr-21-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nair VS, Eaton K, McGarry Houghton A. A case series of morbid COPD exacerbations during immune checkpoint inhibitor therapy in cancer patients. Respir Med Case Rep. 2021;34:101541. doi: 10.1016/j.rmcr.2021.101541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sul J, Blumenthal GM, Jiang X, He K, Keegan P, Pazdur R. FDA Approval Summary: Pembrolizumab for the Treatment of Patients With Metastatic Non-Small Cell Lung Cancer Whose Tumors Express Programmed Death-Ligand 1. Oncologist. 2016;21(5):643–50. doi: 10.1634/theoncologist.2015-0498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chao Y, Zhou J, Hsu S, Ding N, Li J, Zhang Y, Xu X, Tang X, Wei T, Zhu Z, Chu Q, Neal JW, Wu JT, Song Y, Hu J. Risk factors for immune checkpoint inhibitor-related pneumonitis in non-small cell lung cancer. Transl Lung Cancer Res. 2022;11(2):295–306. doi: 10.21037/tlcr-22-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shibata Y, Murakami S, Kato T. Overview of checkpoint inhibitor pneumonitis: incidence and associated risk factors. Expert Opin Drug Saf. 2021;20(5):537–47. doi: 10.1080/14740338.2021.1898584. [DOI] [PubMed] [Google Scholar]
- 31.Cui P, Liu Z, Wang G, Ma J, Qian Y, Zhang F, Han C, Long Y, Li Y, Zheng X, Sun D, Zhang J, Cai S, Jiao S, Hu Y. Risk factors for pneumonitis in patients treated with anti-programmed death-1 therapy: A case-control study. Cancer Med. 2018;7(8):4115–20. doi: 10.1002/cam4.1579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barnes PJ. Immunology of asthma and chronic obstructive pulmonary disease. Nat Rev Immunol. 2008;8(3):183–92. doi: 10.1038/nri2254. [DOI] [PubMed] [Google Scholar]
- 33.Fujimoto D, Kato R, Morimoto T, Shimizu R, Sato Y, Kogo M, Ito J, Teraoka S, Nagata K, Nakagawa A, Otsuka K, Tomii K. Characteristics and Prognostic Impact of Pneumonitis during Systemic Anti-Cancer Therapy in Patients with Advanced Non-Small-Cell Lung Cancer. PLoS ONE. 2016;11(12):e0168465. doi: 10.1371/journal.pone.0168465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Omori T, Tajiri M, Baba T, Ogura T, Iwasawa T, Okudela K, Takemura T, Oba MS, Maehara T, Nakayama H, Tsuboi M, Masuda M. Pulmonary Resection for Lung Cancer in Patients With Idiopathic Interstitial Pneumonia. Ann Thorac Surg. 2015;100(3):954–60. doi: 10.1016/j.athoracsur.2015.03.094. [DOI] [PubMed] [Google Scholar]
- 35.Washko GR, Hunninghake GM, Fernandez IE, Nishino M, Okajima Y, Yamashiro T, Ross JC, Estepar RS, Lynch DA, Brehm JM, Andriole KP, Diaz AA, Khorasani R, D’Aco K, Sciurba FC, Silverman EK, Hatabu H, Rosas IO, Investigators CO. Lung volumes and emphysema in smokers with interstitial lung abnormalities. N Engl J Med. 2011;364(10):897–906. doi: 10.1056/NEJMoa1007285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sears CR, Peikert T, Possick JD, Naidoo J, Nishino M, Patel SP, Camus P, Gaga M, Garon EB, Gould MK, Limper AH, Montgrain PR, Travis WD, Rivera MP. Knowledge Gaps and Research Priorities in Immune Checkpoint Inhibitor-related Pneumonitis. An Official American Thoracic Society Research Statement. Am J Respir Crit Care Med. 2019;200(6):e31–43. doi: 10.1164/rccm.201906-1202ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lowe KE, Regan EA, Anzueto A, Austin E, Austin JHM, Beaty TH, Benos PV, Benway CJ, Bhatt SP, Bleecker ER, Bodduluri S, Bon J, Boriek AM, Boueiz AR, Bowler RP, Budoff M, Casaburi R, Castaldi PJ, Charbonnier JP, Cho MH, Comellas A, Conrad D, Costa Davis C, Criner GJ, Curran-Everett D, Curtis JL, DeMeo DL, Diaz AA, Dransfield MT, Dy JG, Fawzy A, Fleming M, Flenaugh EL, Foreman MG, Fortis S, Gebrekristos H, Grant S, Grenier PA, Gu T, Gupta A, Han MK, Hanania NA, Hansel NN, Hayden LP, Hersh CP, Hobbs BD, Hoffman EA, Hogg JC, Hokanson JE, Hoth KF, Hsiao A, Humphries S, Jacobs K, Jacobson FL, Kazerooni EA, Kim V, Kim WJ, Kinney GL, Koegler H, Lutz SM, Lynch DA, MacIntye NR, Jr, Make BJ, Marchetti N, Martinez FJ, Maselli DJ, Mathews AM, McCormack MC, McDonald MN, McEvoy CE, Moll M, Molye SS, Murray S, Nath H, Newell JD, Jr, Occhipinti M, Paoletti M, Parekh T, Pistolesi M, Pratte KA, Putcha N, Ragland M, Reinhardt JM, Rennard SI, Rosiello RA, Ross JC, Rossiter HB, Ruczinski I, Estepar R, Sciurba FC, Sieren JC, Singh H, Soler X, Steiner RM, Strand MJ, Stringer WW, Tal-Singer R, Thomashow B, Vegas Sanchez-Ferrero G, Walsh JW, Wan ES, Washko GR, Michael Wells J, Wendt CH, Westney G, Wilson A, Wise RA, Yen A, Young K, Yun J, Silverman EK, Crapo JD. COPDGene((R)) 2019: Redefining the Diagnosis of Chronic Obstructive Pulmonary Disease. Chronic Obstr Pulm Dis. 2019;6(5):384–99. doi: 10.15326/jcopdf.6.5.2019.0149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shin SH, Park HY, Im Y, Jung HA, Sun JM, Ahn JS, Ahn MJ, Park K, Lee HY, Lee SH. Improved treatment outcome of pembrolizumab in patients with nonsmall cell lung cancer and chronic obstructive pulmonary disease. Int J Cancer. 2019;145(9):2433–9. doi: 10.1002/ijc.32235. [DOI] [PubMed] [Google Scholar]
- 39.Grangeon M, Tomasini P, Chaleat S, Jeanson A, Souquet-Bressand M, Khobta N, Bermudez J, Trigui Y, Greillier L, Blanchon M, Boucekine M, Mascaux C, Barlesi F. Association Between Immune-related Adverse Events and Efficacy of Immune Checkpoint Inhibitors in Non-small-cell Lung Cancer. Clin Lung Cancer. 2019;20(3):201–7. doi: 10.1016/j.cllc.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 40.Wang W, Gu X, Wang L, Pu X, Feng H, Xu C, Lou G, Shao L, Xu Y, Wang Q, Wang S, Gao W, Zhang Y, Song Z. The prognostic impact of mild and severe immune-related adverse events in non-small cell lung cancer treated with immune checkpoint inhibitors: a multicenter retrospective study. Cancer Immunol Immunother. 2022;71(7):1693–703. doi: 10.1007/s00262-021-03115-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gandhi L, Rodriguez-Abreu D, Gadgeel S, Esteban E, Felip E, De Angelis F, Domine M, Clingan P, Hochmair MJ, Powell SF, Cheng SY, Bischoff HG, Peled N, Grossi F, Jennens RR, Reck M, Hui R, Garon EB, Boyer M, Rubio-Viqueira B, Novello S, Kurata T, Gray JE, Vida J, Wei Z, Yang J, Raftopoulos H, Pietanza MC, Garassino MC. Investigators K-. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med. 2018;378(22):2078–92. doi: 10.1056/NEJMoa1801005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.