Abstract
Uterine carcinosarcomas are aggressive gynaecological cancers comprising less than 5% of uterine malignancies. We present the case of a woman in her 70s with a complicated history of advanced anal carcinoma treated with pelvic radiotherapy and multiple laparotomies, who was referred to gynae-oncology following MRI surveillance imaging showing evidence of endometrial carcinoma and para-aortic lymphadenopathy. Successful surgical excision required multidisciplinary teamwork between gynae-oncology, colorectal and urology surgeons. The patient underwent midline laparotomy, with adhesiolysis, ileum resection and side to side anastomosis, posterior exenteration, left kidney mobilisation and suspension, para-aortic lymph node debulking and left ureteric stent insertion. Significant challenge was posed by the extensive adhesions from previous laparotomies and the debulking of the para-aortic lymph nodes around the renal vessels. This case demonstrates the importance of a multidisciplinary approach in complex pelvic surgery and the vitality of good communication between colleagues in achieving effective patient care.
Keywords: Obstetrics, gynaecology and fertility; Surgical oncology
Background
Uterine carcinosarcoma is a rare malignancy, typically presenting in postmenopausal women between the age of 60–70 years.1 2 Common initial symptoms include abnormal uterine bleeding, abdominal bloating and pelvic pain, with hysteroscopy and biopsy used to diagnose the majority of cases.3 This malignancy is primarily treated by laparoscopic total hysterectomy and bilateral salpingo-oophorectomy with pelvic (and para-aortic) lymphadenectomy.4
We report here a complex case of uterine carcinosarcoma and suspicious para-aortic lymph nodes at the level of the renal vessels, complicated by a history of multiple laparotomies and radiotherapy for anal carcinoma. There is a known link between pelvic radiotherapy and the development of secondary uterine carcinosarcoma.5 6 In this case, the tumour presented 5 years after radiotherapy treatment, making a diagnosis of irradiation-associated uterine carcinosarcoma or de novo occurrence both possible. An extended posterior exenteration was performed, consisting of en block resection of the female reproductive organs and rectosigmoid colon.7 In order to sharply dissect the lymph nodes and the renal vessels, mobilisation of the left kidney was performed, a technique that has been demonstrated in similar complex surgical gynaecological malignancy cases requiring multidisciplinary team (MDT) input.8
Case presentation
We present the case of a woman in her 70s who attended with a change in vaginal discharge and was referred to gynae-oncology following an MRI scan, which showed evidence of an endometrial tumour of potential malignant nature. She has a medical history of insomnia, dyslipidaemia, reflux and a vaginointestinal fistula. In addition, she was diagnosed with advanced anal canal squamous cell carcinoma (SCC) (T4N3M0) in 2017 and has had multiple laparotomies: a total splenectomy for traumatic injury, a transverse colostomy due to a rectosigmoid diverticular stricture obstruction, a lower anterior resection for diverticulitis, with reversal of the colostomy 6 months later, and a subsequent further laparotomy and loop ileostomy. She is postmenopausal and has had two spontaneous vaginal deliveries. Her drug history includes statins, omeprazole and amitriptyline, and she is allergic to cephalexin. She has a body mass index of 20 kg/m2, is an ex-smoker, and has a high performance status.
Investigations
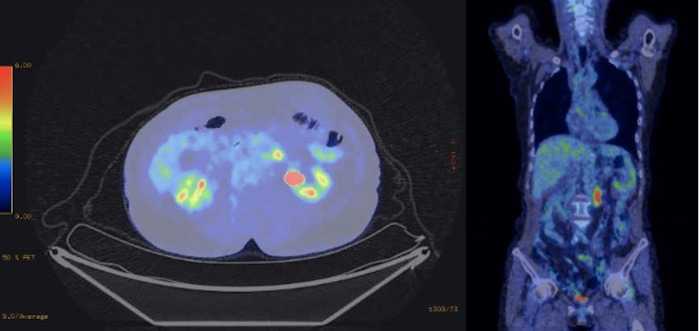
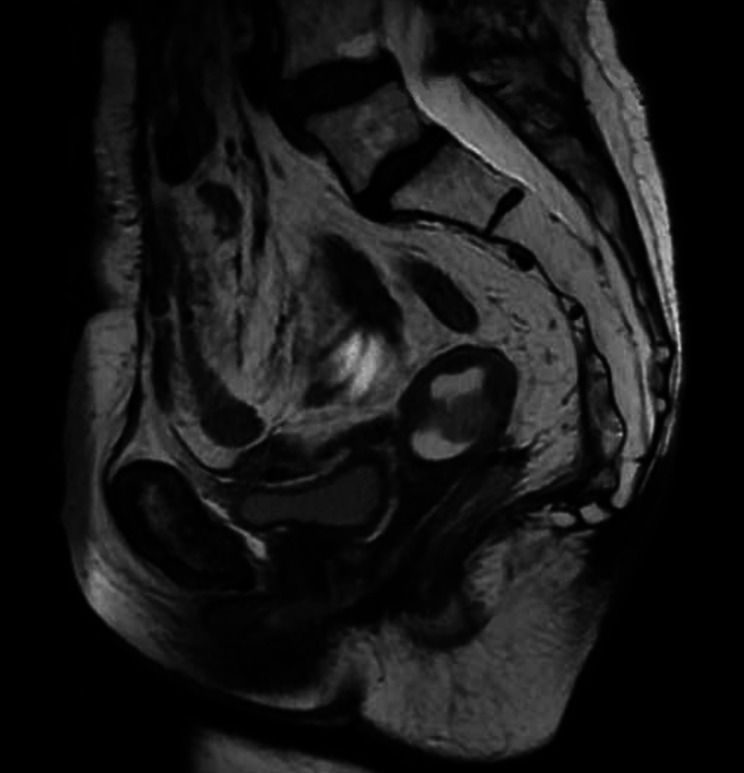
The patient was under the care of the medical oncology team with surveillance imaging, following complete response to pelvic chemoradiotherapy for anal SCC. Positron emission tomography (PET) demonstrated para-aortic lymphadenopathy with evidence of necrosis and PET avidity, in addition to new activity in the uterine fundus (figure 1). A subsequent MRI scan confirmed a multifocal endometrial 45 mm tumour extending into the outer half of the myometrium (figure 2). Proposed differential diagnoses included a primary endometrial cancer or metastatic disease from the anal cancer. Following hysteroscopy and biopsy, histopathology confirmed a high-grade uterine carcinosarcoma, which showed sarcomatous overgrowth and no lymphovascular invasion. Both ovaries were shown to contain benign serous cystadenofibromas, which were adherent to the bowel. CT abdomen, chest and pelvis scan did not reveal any metastasis or pelvic lymphadenopathy. There was also noted to be significant scarring and adhesions.
Figure 1.
PET scan images demonstrating moderate PET avidity of the left para-aortic lymph nodes (standardised uptake value max 8.7) and an focus in the apex of the uterine fundus (SUV max 16.1) warranting further investigation. PET, positron emission tomography.
Figure 2.
MRI pelvis scan sagittal view demonstrating a multifocal endometrial 45 mm tumour that extends into the outer half of the myometrium which is mildly hyperintense on T2-weighted images, demonstrating restricted diffusion and enhancement with gadolinium. There is a hydrometra with an anterior–posterior cavity dimension of approximately 25 mm. There is no extension through the uterine serosa. The cervix appears normal.
Treatment
The patient was discussed at the gynaecological oncology MDT meeting, which recommended that the para-aortic lymphadenopathy was likely metastatic disease secondary to the anal cancer alongside a radiologically stage 1 carcinosarcoma of the uterus. A plan was made for complete macroscopic cytoreduction without pelvic lymphadenectomy in view of normal radiological appearances and previous irradiation.
Due to the complicated nature of this case, a surgical MDT approach was used, involving the colorectal surgeons, gynae-oncology surgeons and urologists (renal transplant specialists). Once in the modified Lloyd Davies position and following midline laparotomy, challenging adhesiolysis revealed inadvertent small bowel enterotomy formation, requiring resection of the ileum and end to end anastomosis using the Barcelona technique.8 Following full colonic mobilisation, the uterus was noted to be adherent to the neorectum and was therefore mobilised to the level of the pelvic floor. The fallopian tubes and ovaries were frozen in adhesions and scarring. A posterior exenteration (radical hysterectomy, bilateral salpingoophrectomy, en block extended anterior resection of the mid transverse colon to the low rectum below the previous anastomosis with further stump mobilisation and stapling at the level of the anorectal junction) and supracolic and infracolic omentectomy was then performed.9 10 This was completed following bilateral ureterolysis, ligation and division of the internal iliac arteries, round ligaments and infundibulopelvic ligaments. The bladder was reflected with subsequent colpotomy and rectovaginal septum dissection. The retroperitoneal structures were approached through Mattox and Cattel-Braash manoeuvres, with full exposure of the aorta and inferior vena cava, and the (inferior mesenteric artery) was sacrificed. Following this, the left renal artery and vein were skeletonised with ureteric dissection to the level of the kidney, and the left kidney mobilised. The adrenal gland was visualised and preserved. The enlarged 4 cm para-aortic nodal mass was excised with complete macroscopic debulking around the renal vessels (figure 3). The left kidney was then suspended to the abdominal side wall. Finally, cystoscopy and left JJ ureteric stenting (under radiological guidance and pyelogram) were performed. Two Robinson’s drains were left in situ in the prepancreal and pelvic regions. There was no palpable pelvic lymphadenopathy and no extrauterine (or indeed serosal) macroscopic disease visualised at the time of surgery. In total, the operation took 10 hours with an estimated blood loss of 500 mL, for which the patient received 1 unit of red blood cells. The patient was admitted to high dependency unit postoperatively.
Figure 3.
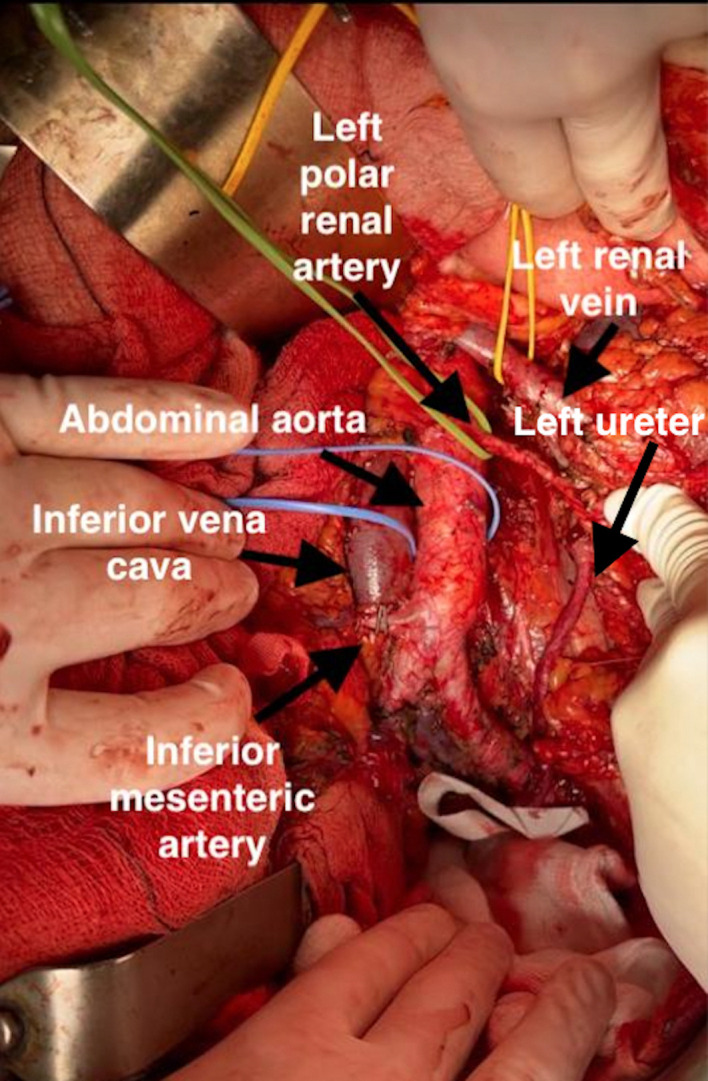
Intraoperative image following dissection of the left-sided para-aortic lymph nodes.
The patient showed slow recovery with development of bilateral segmental pulmonary emboli on day 7, requiring treatment dose low-molecular-weight heparin. Due to several episodes of acute confusion and hallucinations she under went CT head and abdomen pelvis (CTAP), showing pyelonephritis, which was treated with antibiotics, and her amitriptyline was withheld. The left renal artery was noted to have been ligated. She was discharged on day 17 with anticoagulation, urology and gynae-oncology follow-up arrangements.
Unfortunately, 3 weeks after the surgery, the patient both contracted COVID-19 and presented with generalised abdominal pain and vomiting faecal material despite normal stoma function. CTAP revealed an 8 cm presacral pelvic collection. Seventy per cent infarct in the left kidney was also noted, which was not for further treatment following urology consultation. She was managed conservatively with antibiotics following MDT discussion including interventional radiology consideration. Input was sought regarding COVID-19 status with a plan made for intravenous remdesivir in view of active solid metastatic cancer and risk of severe COVID-19 (with the addition of dexamethasone should the patient develop an oxygen requirement).
Outcome and follow-up
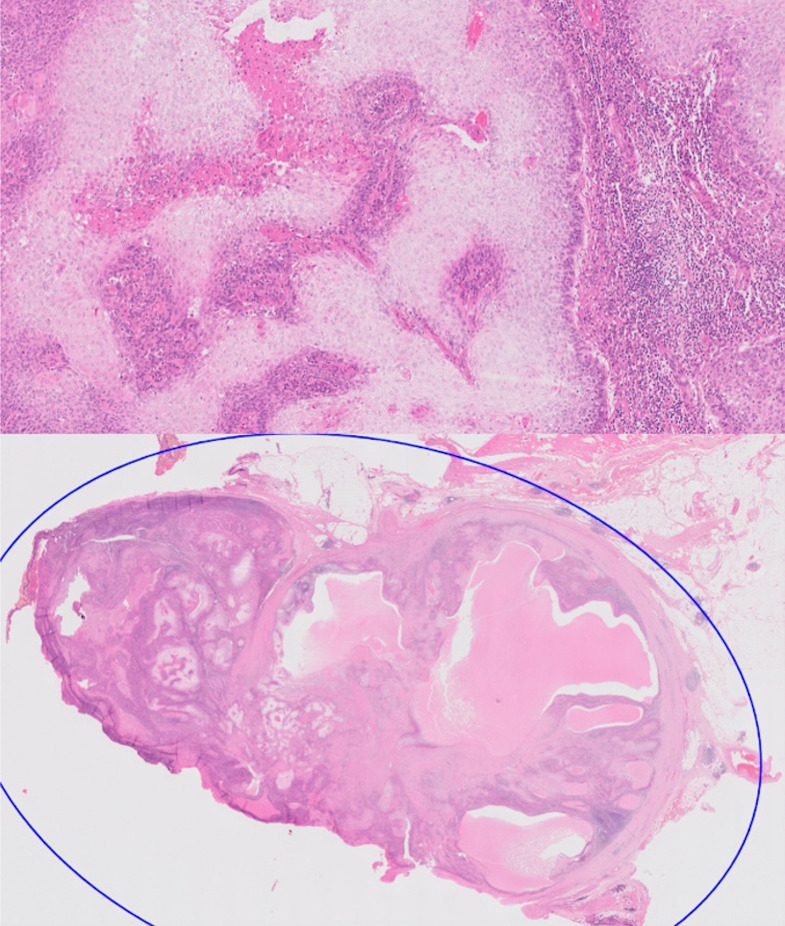
The patient was reviewed in the gynae-oncology clinic following review of histology results at the MDT. This confirmed stage 1b uterine carcinosarcoma with para-aortic lymph nodes showing metastatic anal SCC of stage T4 N3 M1 (figure 4). Further gynae-oncology treatment was not recommended due to previous pelvic radiotherapy, however, the patient has also been referred to the colorectal MDT for consideration of stereotactic radiotherapy to the para-aortic lymph node region for the relapsed anal SCC.
Figure 4.
Microscopic histopathology images demonstrating evidence of metastatic squamous cell carcinoma of the left para-aortic lymph nodes.
Discussion
Uterine carcinosarcoma is a rare gynaecological malignancy characterised by poor prognosis, with one-fourth of patients presenting with metastases.11 These tumours typically occur in postmenopausal women with a peak incidence at the ages of 60–70 years.11 The typical presentation of the disease is with abnormal uterine bleeding, rapid uterine enlargement, abdominal bloating and pelvic pain, as well as features of distant haematological and lymphatic spread.12 This case was unusual, in that the patient’s cancer was identified by regular imaging surveillance for her known enlarged para-aortic lymph nodes after treatment for anal carcinoma. The patient reported a change in vaginal discharge but was otherwise asymptomatic.
Numerous studies and case reports have reported the development of secondary uterine carcinosarcoma following therapeutic pelvic irradiation.5 6 The interval between the time of irradiation and the diagnosis of uterine carcinosarcoma varies between 3 and 30 years, with the total radiation doses ranging from 2400 to 8000 cGy.6 In this case, the tumour presented 5 years after the patients’ previous pelvic radiotherapy, making a diagnosis of irradiation-associated uterine carcinosarcoma a possibility. However, it cannot be completely ruled out that this was not a de novo occurrence.
The standard management of high-grade uterine carcinosarcoma is a total hysterectomy and bilateral salpingo-oophorectomy, as well as dissection of pelvic (and para-aortic) lymph nodes, carried out through a laparoscopic approach.4 In this case, a posterior exenteration was performed—a more radical procedure chosen due to the patient’s history of anal carcinoma, the presence of bulky necrotic para-aortic lymph nodes and her previous pelvic radiotherapy preventing any future adjuvant treatment.7 In addition, a midline laparotomy approach was used because of her complex history of multiple laparotomies, and the need for adequate nodal debulking around the renal vessels.
Para-aortic lymphadenectomy up to the level of the left renal vein is recommended in the treatment of uterine carcinosarcoma due to improved overall survival of patients.13 One of the greatest challenges of this case was presented by the critical relation of the bulky necrotic para-aortic lymph nodes to the renal vessels and hence the uncertainty of whether the left kidney could be preserved. The main nodal mass was identified behind the left renal vein alongside the aorta. In some cases, para-aortic lymph nodes in the region of the left renal vein can be removed by exposing and moving the left renal vein and artery with mobilisation. However, as was the case here, if the metastatic lymph nodes behind the left renal vein are grossly enlarged, the mobilisation of the kidney allows a sharp dissection between the lymph nodes and the renal vessels under direct vision.14
A further complication to this patient’s clinical course is that future adjuvant treatment of her uterine cancer is made difficult by previous adjuvant pelvic radiotherapy for the anal SCC. Adjuvant radiotherapy for uterine carcinosarcoma has not been thoroughly evaluated, but one study has demonstrated the advantage of radiotherapy for local control in advanced disease.15 However, considering the possibility of significant adverse side effects, pelvic radiotherapy was not deemed appropriate here, due to her previous exposure.
Although certain challenges arise from involving multiple specialities in a patient’s care; such as confirming and sharing opinions on management strategies, and coordinating operating lists and rotas, multidisciplinary cancer care has been recommended by cancer organisations and healthcare organisations as best practice since 1995.16 Multiple studies have shown that multidisciplinary care for surgical procedures is associated with reduced length of hospital stay, postoperative complications and mortality.17 18 Overall, this case demonstrates the importance of a multidisciplinary approach in complex pelvic surgeries for uterine carcinosarcoma. The patients’ medical history of multiple laparotomies with extensive adhesions, and anal carcinoma, as well as the presence of enlarged para-aortic lymph nodes in close proximity to the renal vessels, led to the involvement of gynae-oncology, colorectal and urology surgeons. With histological confirmation that the enlarged para-aortic lymph nodes removed during the surgery were indeed caused by metastasis of the previous anal carcinoma rather than the uterine carcinosarcoma, there will be continued liaison between multiple specialities to decide on future treatment. The vitality of teamwork between colleagues from multiple specialities has hence been highlighted here, as well as the centrality of the MDT to achieve the best outcome in such complex cases.
Learning points.
This is a complex case of a rare gynaecological malignancy, complicated by previous multiple laparotomies anal carcinoma, previous pelvic radiotherapy and enlarged para-aortic lymph nodes at the level of the renal vessels.
A multidisciplinary approach between gynae-oncology, urology and colorectal surgeons was required to manage a difficult pelvic surgery for uterine carcinosarcoma. This case required careful planning and a full complement of specialist expertise.
Effective teamwork between colleagues in the multidisciplinary team is essential to achieving optimal patient care.
Footnotes
Contributors: IC is the primary manuscript author. SS gave draft guidance and performed senior review of the case report. SE performed senior review of the case report and was involved in the clinical care of the patient. HSM conceptualised the manuscript, performed senior review of the case report and was involved in the clinical care of the patient.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.D'Angelo E, Prat J. Uterine sarcomas: a review. Gynecol Oncol 2010;116:131–9. 10.1016/j.ygyno.2009.09.023 [DOI] [PubMed] [Google Scholar]
- 2.Pappa C, Smyth SL, Soleymani Majd H. Late presentation during the COVID-19 pandemic of severe procidentia: a high-grade poorly differentiated sarcoma of unknown origin. BMJ Case Rep 2022;15:e246710. 10.1136/bcr-2021-246710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pezzicoli G, Moscaritolo F, Silvestris E, et al. Uterine carcinosarcoma: an overview. Crit Rev Oncol Hematol 2021;163:103369. 10.1016/j.critrevonc.2021.103369 [DOI] [PubMed] [Google Scholar]
- 4.Morrison J, Balega J, Buckley L, et al. British gynaecological cancer Society (BGCS) uterine cancer guidelines: recommendations for practice. Eur J Obstet Gynecol Reprod Biol 2022;270:50–89. 10.1016/j.ejogrb.2021.11.423 [DOI] [PubMed] [Google Scholar]
- 5.Kahraman K, Ortac F, Kankaya D, et al. Uterine carcinosarcoma associated with pelvic radiotherapy for sacral chordoma: a case report. Taiwan J Obstet Gynecol 2012;51:89–92. 10.1016/j.tjog.2012.01.018 [DOI] [PubMed] [Google Scholar]
- 6.Murray EM, Werner D, Greeff EA, et al. Postradiation sarcomas: 20 cases and a literature review. Int J Radiat Oncol Biol Phys 1999;45:951–61. 10.1016/S0360-3016(99)00279-5 [DOI] [PubMed] [Google Scholar]
- 7.Benn T, Brooks RA, Zhang Q, et al. Pelvic exenteration in gynecologic oncology: a single institution study over 20 years. Gynecol Oncol 2011;122:14–18. 10.1016/j.ygyno.2011.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Addley S, McMullan JC, Scott S, et al. ‘Well‐leg’ compartment syndrome associated with gynaecological surgery: a perioperative risk‐reduction protocol and checklist. BJOG 2021;128:1517–25. 10.1111/1471-0528.16749 [DOI] [PubMed] [Google Scholar]
- 9.Sadeghi N, Addley S, Alazzam M, et al. Intravascular leiomyomatosis; mimicking low grade endometrial sarcoma. J Obstet Gynaecol 2022;42:1564–8. 10.1080/01443615.2021.1963220 [DOI] [PubMed] [Google Scholar]
- 10.Cowie P, Eastwood B, Smyth S, et al. Atypical presentation of intravascular leiomyomatosis mimicking advanced uterine sarcoma: modified laterally extended endopelvic resection with preservation of pelvic neural structures. BMJ Case Rep 2021;14:e244774. 10.1136/bcr-2021-244774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nama N, Cason FD, Misra S, et al. Carcinosarcoma of the uterus: a study from the surveillance epidemiology and end result (SEER) database. Cureus 2020;12:e10283. 10.7759/cureus.10283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ravishankar P, Smith DA, Avril S, et al. Uterine carcinosarcoma: a primer for radiologists. Abdom Radiol 2019;44:2874–85. 10.1007/s00261-019-02038-8 [DOI] [PubMed] [Google Scholar]
- 13.Hoellen F, Waldmann A, Benthin S, et al. The role of lymphadenectomy in uterine sarcoma: a clinical practical approach based on retrospective analysis. Anticancer Res 2014;34:985-93. [PubMed] [Google Scholar]
- 14.Kato K, Omatsu K, Takeshima N. Secondary debulking surgery in ovarian cancer patients with isolated nodal recurrence located in the region above and behind the renal vein. Gynecol Oncol 2013;130:226–8. 10.1016/j.ygyno.2013.03.025 [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez Bosquet J, Terstriep SA, Cliby WA, et al. The impact of multi-modal therapy on survival for uterine carcinosarcomas. Gynecol Oncol 2010;116:419–23. 10.1016/j.ygyno.2009.10.053 [DOI] [PubMed] [Google Scholar]
- 16.Selby P, Gillis C, Haward R. Benefits from specialised cancer care. Lancet 1996;348:313–8. 10.1016/S0140-6736(96)02482-8 [DOI] [PubMed] [Google Scholar]
- 17.Grigoryan KV, Javedan H, Rudolph JL. Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 2014;28:e49-55. 10.1097/BOT.0b013e3182a5a045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Publishing Asia B, Stephens MR, Lewis WG, et al. Multidisciplinary team management is associated with improved outcomes after surgery for esophageal cancer [Internet]. Vol. 19, Diseases of the Esophagus, 2006. Available: https://academic.oup.com/dote/article/19/3/164/2194890 [DOI] [PubMed]