Abstract
INTRODUCTION:
Chatbots have emerged as a first link to care in recent years. The COVID-19 pandemic, and consequent health system disruptions, expanded their use. Socios En Salud (SES) introduced chatbots in Peru, which experienced one of the highest excess COVID mortalities in the world.
METHODS:
SES and the government identified unmet population health needs, which could be amenable to virtual interventions. Chatbots were developed to screen individuals for these conditions; we describe the period of deployment, number of screenings, and number of people who received services.
RESULTS:
Between April 2020 and May 2021, SES deployed nine ChatBots: four for mental health, two for maternal and child health, and three for chronic diseases: breast cancer, hypertension, diabetes mellitus, and obesity. Mental health services were provided to 42,932 people, 99.99% of those offered services. The other ChatBots reached fewer people. Overall, more than 50% of eligible people accepted chatbot-based services.
DISCUSSION:
ChatBot use was highest for mental health. Chatbots may increase connections between a vulnerable population and health services; this is likely dependent on several factors, including condition, population, and penetration of smart phones. Future research will be critical to understand user experience and preferences and to ensure that chatbots link vulnerable populations to appropriate, high-quality care.
Keywords: SARS-CoV-19, e-health, healthcare utilization, innovation, mental health
Abstract
INTRODUCTION :
Les chatbots se sont imposés comme un premier lien aux soins ces dernières années. La pandémie de COVID-19, et les perturbations du système de santé qui en ont résultées, ont élargi leur champ d’application. Socios En Salud (SES) a introduit les chatbots au Pérou, qui a connu l’une des surmortalités dues au COVID les plus élevées au monde.
MÉTHODES :
SES et le gouvernement ont identifié des besoins non satisfaits en matière de santé de la population, qui pourraient faire l’objet d’interventions virtuelles. Des chatbots ont été développés pour dépister des individus pour ces conditions ; nous décrivons la période de leur déploiement, le nombre de dépistages et le nombre de personnes qui ont reçu ces services.
RÉSULTATS :
Entre avril 2020 et mai 2021, SES a déployé neuf ChatBots : quatre pour la santé mentale, deux pour la santé maternelle et infantile et trois pour les maladies chroniques, comme le cancer du sein, l’hypertension, le diabète et l’obésité. Des services de santé mentale ont été fournis à 42 932 personnes, soit 99,99% des personnes proposées. Les autres ChatBots ont touché moins de personnes. Dans l’ensemble, plus de 50% des personnes éligibles ont accepté les services proposés par les chatbots.
DISCUSSION :
L’utilisation des ChatBots était la plus élevée pour la santé mentale. Les chatbots peuvent augmenter les connexions entre une population vulnérable et les services de santé, mais cela dépende de plusieurs facteurs, dont la condition, la type de population et la pénétration des smartphones. Les recherches futures seront essentielles pour comprendre l’expérience et les préférences des utilisateurs et pour s’assurer que les chatbots relient les populations vulnérables vulnérables aux soins appropriés et de qualité.
Peru has experienced one of the worst COVID-19 outbreaks, and among the highest per capita excess mortality rates in the world.1 By March 16, 2020, the country had closed its borders, suspended nonessential activities, and enacted a mandatory isolation period with restrictions on internal movement and a nightly curfew. Despite these measures, Peru had more than 2.25 million confirmed cases and over 200,000 deaths by December 2021, the majority concentrated in the capital city, Lima, where oxygen and intensive care bed shortages were dire.2 The economy collapsed, with a 30% drop in gross domestic product and 30% rise in unemployment during the second trimester of 2020 compared to the previous year. Health services were simultaneously overwhelmed and shuttered to avoid nosocomial transmission.3,4 Uptake of preventive services plummeted due to resource shortages, travel restrictions, and COVID-19 exposure concerns at medical facilities.5
The psychological burden of social isolation, bereavement, and economic depression exacerbated the already unmet demand for mental health services.6 With an estimated 2.95 psychiatrists and 32.03 mental health workers per 100,000 population,7 the proportion of adults receiving mental health services remains low even among those with a high perceived need for care.8
Digital chatbots and other mobile technologies can bridge this and other health service gaps. Chatbots, also termed “conversational agents,” are digital applications that interact with users through text, voice, or visual graphics. They may be rule-based, with predefined user options and programmed decision trees, or utilize machine learning and natural language processing to interpret and respond to complex user input.9 Chatbots may direct users to relevant information and resources, refer them to human agents, or trigger specific actions like appointment scheduling and medication refills.
Chatbots are an appealing adjunct to traditional forms of healthcare because of their scalability; in settings with limited human and financial resources, chatbots can expand existing capacity and promote equity by reducing geographic and economic barriers to care. They also provide an efficient means of triaging patients, assisting in identification of concerns that require in-person attention.9,10 Digital tools permit people to seek help without fear of stigma or discrimination, likely contributing to their popularity for detecting mental illness and cognitive impairments.11,12 Also, chatbots enable users to access services faster and at their convenience.
Socios En Salud (SES), a non-governmental organization based in Lima, Peru, developed a series of Chat-Bots to link Peruvians with health services during the pandemic. SES ChatBots aimed to improve mental health and restore access to preventive care for conditions other than COVID-19. In this paper, we present the SES ChatBot implementation framework, content, evidence uptake, and resulting services.
METHODS
Setting and population
SES ChatBots (Table; Supplementary Data) were developed to serve vulnerable subpopulations in Peru, primarily in Northern Lima, where SES has worked for 25 years. Some SES ChatBots were extended to other parts of metropolitan Lima. For one ChatBot, the target population was Quechua-speaking communities of South-Central Peru. ChatBots were accessible to anyone with a smartphone or computer. Other criteria for use were age (>18 years) for most, women aged 50–69 years for the mammography-referral ChatBot, and caregivers of children aged 6–24 months for the early-childhood-development ChatBot.
TABLE.
Summary description of Socios En Salud ChatBots introduced during the COVID-19 pandemic (see Supplementary Data for more details)
| ChatBot | Objective | Target population | Evaluation | Follow-up and intervention |
|---|---|---|---|---|
| Mental health | ||||
| SAMEbot, Juntos, BienEstar, Kuska | Provide care to Spanish- or Quechua-speaking people with mental health disorders | Mostly adults | Validated depression/anxiety screening instruments | Eligible individuals referred for further evaluation and services |
| Maternal and child health | ||||
| GestAmor | Improve access to prenatal care and reduce pregnancy complications | Group 1: women with suspected pregnancy; Group 2: women with confirmed pregnancy |
Group 1: questionnaire about early signs and symptoms of pregnancy; Group 2: questionnaire about warning signs during the pregnancy and other pregnancy- related concerns |
|
| CASITAbot | Reduce (risk of) developmental delays | Caregivers of children from 6–24 months | Simplified version of the Scale for Evaluation of Psychomotor Development | |
| Care for chronic diseases | ||||
| AlmaBot | Provide free mammography to women at risk for breast cancer | Older, publicly insured women or women with signs or symptoms of breast cancer | Questionnaire | |
| Soy Qhali Kay | Decrease risk for, and improve management of, type 2 diabetes mellitus and hypertension | Adults | Questionnaire derived from multiple sources | |
| NutriBot | Improve diet and physical activity of people at risk for obesity | Adults | Survey about anthropometry, eating habits, and nutritional health |
This report does not constitute human subjects research. As it reports only on the implementation of SES ChatBots and does not contain patient-level information, we did not seek ethics approval.
Identification of community health needs and development of ChatBot concepts
SES collaborated with the Peruvian Ministry of Health (Ministerio de Salud, MINSA), residents, and community health workers in Northern Lima to identify gaps occasioned (or worsened) by COVID-19 and the pandemic response. They selected needs that could be addressed through a ChatBot that entails self-administered screening, follow-up by a health professional to refine risk assessment, and referrals to care.
Each ChatBot aimed to improve uptake and/or retention in the care cascade, i.e., outreach, screening, diagnosis, treatment, and follow-up. Where possible, we used instruments already validated for self-administration (depression, anxiety, developmental delay).13–21 Chronic disease screening integrated several tools into a single survey.22–26 For breast cancer, MINSA screening guidelines were adapted for self-administration.27
Development, testing, and deployment
The SES information technology team developed the ChatBots using a common framework built using ASP. NET and Microsoft SQL Server (MicroSoft, Redmond, WA, USA). Development followed a human-centered, iterative-design approach that included pilot testing by end users. The web interface has multimedia (maps, images, sounds) functionality. It can be accessed on any device with a browser and is served over https. The webpage comprises a questionnaire presented in a format that imitates instant messaging applications. When a user accesses the page, “messages” appear, containing a preamble, followed by questions. Answers are entered at the bottom of the screen in a text-box (Figure 1). Answers are confirmed and used to prompt subsequent questions, based on decision-tree logic. Answers may also be used to compute a numeric score and determine if referral is required. The user is advised of the result and prompted for contact information. An alert is emailed to relevant health professionals at SES who then coordinate care with the user and providers. If the user does not screen positive or declines to provide contact information, they are thanked for their participation and presented with health education messages.
FIGURE 1.
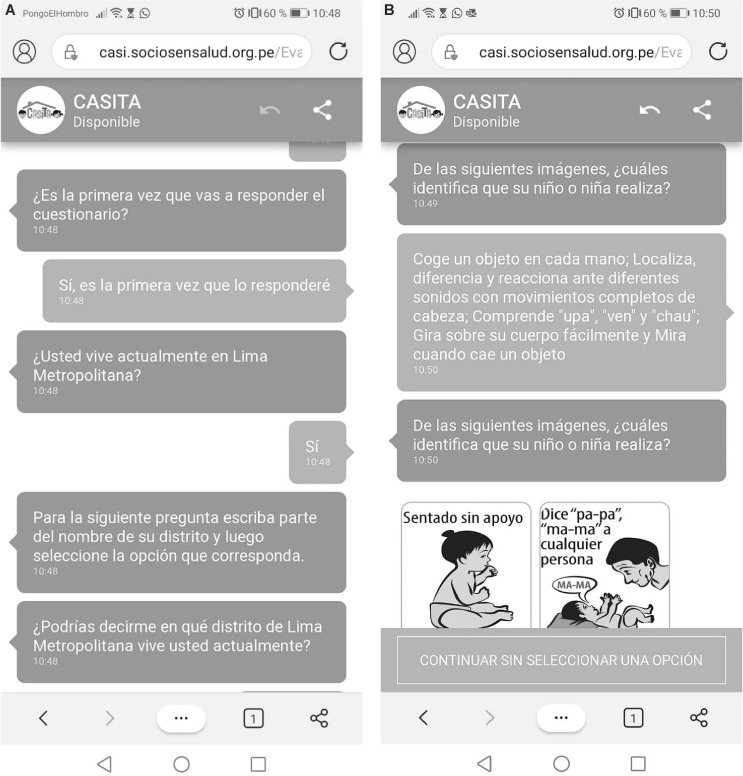
A) Screenshot of CASITA ChatBot establishing residence in the catchment area; B) screenshot of CASITA ChatBot confirming answers, and posing new questions on developmental milestones.
All SES ChatBots use Spanish text interface, with one exception: Kuska, used both text (Quechua) and audio interface to ensure access to Quechua-speaking, low-literacy users.
Dissemination
SES ChatBots were disseminated through social media, community health promoters conducting household visits, and call centers established for health services.28
Analysis
For each application, we calculate the calendar period of deployment, the number of completed screens, and the numbers and proportions who screened positive and who accepted services.
RESULTS
ChatBot purpose and deployment
Between April 1, 2020 and May 11, 2021, SES deployed nine Chat-Bots: four for mental health, two for maternal and child health, and three for chronic diseases (Table; Supplementary Data). Mental health was established as a priority after a noticeable uptick in hotline calls reporting anxiety and depression. SES’s mental health ChatBots screened for depression (using Patient Health Questionnaire 2 [PHQ-2] or PHQ-9) and anxiety (using the Self-Reporting Questionnaire) in Spanish and Quechua. Spanish-language, mental health ChatBots were deployed for Lima from April 2020 to August 2021. Interventions were tailored to the score: users with no symptoms received supportive text messages; those with mild symptoms were offered a single session of psychological first aid, while moderate symptoms were addressed with virtual Problem Management Plus.29 Respondents with severe depression or anxiety or suicidal ideation received accompanied referrals to the public health system. Additional referrals were offered for other services (e.g., domestic violence protection, meal support).
GestAmor was developed in response to constrained prenatal and delivery services. GestAmor sought to identify pregnant women, particularly those at high-risk for poor outcomes. Still in operation, it facilitates access to pregnancy tests, prenatal care, (virtual) consultation with obstetricians, registration for public insurance, referrals for delivery, or family planning services.
CASITAbot screened for developmental delays using an adapted, validated version of the Scale for Evaluation of Psycho-motor Development.19 Those confirmed by subsequent in-person evaluation to be experiencing developmental delays received an early-childhood development intervention to promote health and stimulation. These services had previously been delivered in-person in one district in Northern Lima.30–32 The virtual platform, launched in August 2020, provided video content to a larger population. Caregivers also received virtual accompaniment by community health workers, telemedicine consultations, socioeconomic support, and referrals for other services as needed.
AlmaBot replaced a (planned) in-person intervention using a virtual referral system. It responded to low rates of mammography screening, late-stage diagnoses, and poor outcomes among women diagnosed with breast cancer. AlmaBot targeted women in northern Lima aged 50–69 years, eligible for Peruvian public health insurance (Segura Integral de Salud, SIS), who had not had a mammogram in the previous 2 years; other women with signs or symptoms of breast cancer were also eligible. Launched in August 2020, AlmaBot provided participants with accompanied referrals to local hospitals for clinical consultations, mammograms, and further diagnostic testing.
Introduced in August 2020, Soy Qhali Kay responded to reports of patients with diabetes mellitus and hypertension not receiving follow-up care, and screened for risk of hypertension and/or diabetes. Those screening positive were referred to a community health program for chronic illnesses. They were eligible for diagnostic tests, nutritional evaluation, and group sessions on eating habits and physical activity. Soy Qhali Kay also restored connection with health services for those with pre-pandemic diagnoses of diabetes and/or hypertension, including laboratory testing and prescription refills.
NutriBot was developed in response to emerging data revealing a higher COVID-19 mortality risk for people with obesity and over-weight. From August 2020 to mid-April 2021, screening instruments assessed diet, physical activity, risk behaviors, and anthropometry. Those with a combined score indicating risk of being overweight/obesity were referred to a local health facility for further evaluation. Those classified as obese (body mass index ⩾30 kg/m2) were invited to participate in the intervention, which combined virtual and in-person activities that included consultation with a nutritionist, exercise, group discussions, and follow-up anthropometry.22
Numbers screened, referred, and served
Figure 2 shows the cascade of acceptance of screening and care for ChatBots. Across four mental health ChatBots, nearly 150,000 screenings occurred for depression and/or anxiety. More than 50% (n = 75,440) screened positive. Services were provided to nearly all users of mental health ChatBots who accepted to be contacted (42,932/42,933, 99.9%).
FIGURE 2.
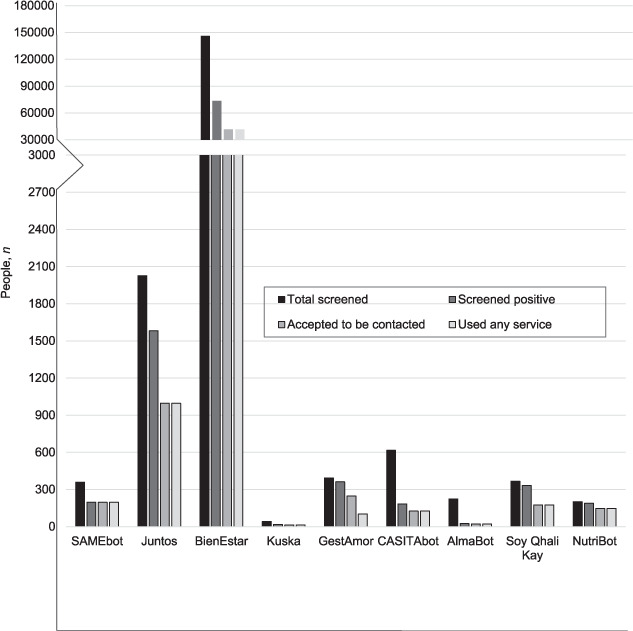
Cascade of care (numbers screened, those with positive screen, those who agreed to be contacted, and those who used any service) for each SES ChatBots implemented during the COVID-19 pandemic. SES = Socios en Salud.
GestAmor was completed 362 times; 248 (68.5%) respondents were pregnant, the remainder were referred for family planning counseling. Among pregnant women, all but six (98%) accepted ChatBot services: two refused and the other four could access care through private insurance.
CASITAbot was used 616 times to evaluate children for developmental delays: 184 (29.9%) children screened positive. Of these, 126 (68.5%) participated in a 12-week virtual intervention.
For chronic-disease-oriented ChatBots, 25/223 (11.2%) AlmaBot users met initial eligibility criteria for referral for mammography. Of these, 22 (88.0%) were referred and all accepted services. Soy Qhali Kay ChatBot was used 367 times; 332 (90.5%) screened positive. After further evaluation, 176 (53.0%) were eligible for services and all accepted. Finally, Chatea con Nutri Chat-Bot was completed 201 times; 189 (94.0%) users screened positive. Of these, 147 (77.8%) were recommended for further services; all accepted.
DISCUSSION
This report describes the rapid deployment and dissemination of nine SES ChatBots early in the COVID-19 pandemic in Lima, Peru. The ChatBots connected a large population with a range of services for mental health, maternal and child health, and chronic diseases. These ChatBots provided an important link to care when services were profoundly diminished by the pandemic.
Overall response to the ChatBots, and services to which they afforded entry, was encouraging. The reach of each ChatBot is likely, in part, a function of the size of the population targeted and penetration of smartphones and computers in that population. To note, the mental health applications, which were used almost 150,000 times, were initially deployed in the largely urban districts of northern Lima with an estimated 2020 population of just over 2 million adults.33 As of 2019, 74.5% of the Lima population aged ⩾6 years report accessing internet services, 45.7% of households own at least one computer, and almost 80% had smartphones.34–36 In contrast to BienEstar, AlmaBot was intended to reach older, low-income women, likely a group with less access to technology. It was used only 223 times in an estimated population of 48,000 women aged 50–69 years who use SIS insurance in targeted districts.33,37
More than 50% of Spanish language screens were positive using mental health, diabetes/hypertension, and nutrition/weight loss applications. The frequency of positive screens across some applications was higher than the estimated prevalence of the conditions in the general population; for example, prevalence of depression was estimated at 25% prior to the pandemic.38 This difference is likely multifactorial: first, dissemination of applications was targeted to individuals and communities with known high risk for the conditions. Second, users may have completed Chat-Bots more than once; those with known or perceived risk for chronic diseases and/or mental illness may be more likely to screen repeatedly.39 Third, in the context of the pandemic, new mental health issues and worsening chronic conditions emerged.6,40–43 The fact that positive screens as a percentage of all uses was lower for breast cancer and early childhood development cannot be interpreted as lower prevalence of these conditions. Rather, these apps may not have reached the targeted population. Users of the Quechua language mental health ChatBot were more likely to live in rural areas than their Spanish language counterparts; rural residence may protect against some mental health consequences of the pandemic and response, a phenomenon observed elsewhere.44–46
Acceptance of services was above 50% for all SES ChatBots. This may suggest alignment between services provided and needs of the population as identified by SES, MINSA, community residents, and health promoters. The need may have been most pronounced for mental health because of increased stress and fear about direct (sickness, death) and indirect effects (isolation, poverty) of the virus. Furthermore, the high acceptance of referral for mental health services may be because the screening instruments are validated for self-administration in local languages and uniquely correspond to feelings experienced by users, including affective disorders.47 Other factors that may influence acceptance include type of referral, timing relative to pandemic and response conditions, and perceived engagement of those who offered services. Regarding type of referral, possible factors include whether it was for single intervention vs. continuous service, whether the service was provided virtually or in-person, convenience of the service, and the individual’s prior experience with the health system. These all represent areas ripe for future qualitative or mixed-methods research.
Additional future research would be valuable to track methods of chatbot dissemination, evaluate their relative success, and measure “response rate.” Qualitative methods would give voice to client experiences and reasons for accepting (or not) services. SES plans to expand the scope of its ChatBots. In the future, the Chat-Bots will route patients directly to relevant specialists, rather than requiring an intermediary. SES is developing a component called YoPromotor, which will allow community health workers to view patient data collected through ChatBots and exchange messages with patients (and providers). Other initiatives could explore ethics and feasibility of increased, longitudinal data collection with ChatBots and integration of machine learning to inform care.
Limitations of this study include the inability to estimate prevalence of conditions in the population or document changes over the course of the pandemic and to assess response among exposed people. Other noted limitations have been recommended for future research.
In conclusion, our results suggest that in certain digitally oriented populations, person-centered chatbots may be helpful in times of crises that preclude full access to health systems and, possibly, routinely. Chatbots may be good for initial screening-prioritized connection to other services. They could be particularly helpful when they rely on tools that are well-validated for self-administration. It is important to establish the scope of services that can be successfully delivered through this digital interface so it can facilitate access and promote equity. There is a real, documented risk that, in vulnerable populations with poor health-service access, such applications will replace quality, individualized, professional care.48 Maximum benefit of these digital tools will be achieved if they serve as link—not as an alternative—to equitable and resilient health systems.
ACKNOWLEDGEMENTS
The authors thank the populations of the Peruvian provinces of Lima and Trujillo who provided us with the facilities and support to carry out activities within their communities during the COVID-19 pandemic; and the Ministries of Health and Social Security of Peru, especially the local representatives in Northern Lima, for their administrative, logistical, and operational support.
Funding Statement
Public health response activities were financed by Peruvian Ministry of Health, Partners In Health (Lima, Peru) and the United States Agency for International Development (grant number 72052720FA00003).
Footnotes
Conflicts of interest: none declared.
References
- 1.Taylor L. Covid-19: Why Peru suffers from one of the highest excess death rates in the world. BMJ. 2021;372:n611. doi: 10.1136/bmj.n611. [DOI] [PubMed] [Google Scholar]
- 2.Dong E, Du H, Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect Dis. 2020;20(5):533–534. doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Institute for Statistics and Information of Peru Producto bruto interno trimestral por tipo de gasto 2007–2020-IV (valores a precios constantes de 2007) Lima, Peru: NISI; 2020. [Google Scholar]
- 4.National Institute for Statistics and Information of Peru Informe de empleo. Lima, Peru: NISI; 2020. https://www.inei.gob.pe/biblioteca-virtual/boletines/informe-de-empleo/2020/1/ [Google Scholar]
- 5.Anderson KE, et al. Reports of forgone medical care among US adults during the initial phase of the COVID-19 pandemic. JAMA Netw Open. 2021;4(1):e2034882. doi: 10.1001/jamanetworkopen.2020.34882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ruiz-Frutos C, et al. Effects of the COVID-19 pandemic on mental health in Peru: psychological distress. Healthcare. 2021;9(6):691. doi: 10.3390/healthcare9060691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.World Health Organization Mental Health Atlas, 2017. Member State Profile. Peru. Geneva, Switzerland: WHO; 2017. [Google Scholar]
- 8.Saavedra JE, Galea JT. Access of mental health services by the adult population in Metropolitan Lima, Peru: characteristics, perceptions and need for care. Community Ment Health J. 2021;57(2):228–237. doi: 10.1007/s10597-020-00639-y. [DOI] [PubMed] [Google Scholar]
- 9.Tudor Car L et al. Conversational agents in health care: scoping review and conceptual analysis. J Med Internet Res. 2020;22(8):e17158. doi: 10.2196/17158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Espinoza J, Crown K, Kulkarni O. A guide to chatbots for COVID-19 screening at pediatric health care facilities. JMIR Public Health Surveill. 2020;6(2):e18808. doi: 10.2196/18808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Abd-Alrazaq AA, et al. An overview of the features of chatbots in mental health: a scoping review. Int J Med Inform. 2019;132:103978. doi: 10.1016/j.ijmedinf.2019.103978. [DOI] [PubMed] [Google Scholar]
- 12.Pacheco-Lorenzo MR, et al. Smart conversational agents for the detection of neuropsychiatric disorders: a systematic review. J Biomed Inform. 2021;113:103632. doi: 10.1016/j.jbi.2020.103632. [DOI] [PubMed] [Google Scholar]
- 13.Calderon M, et al. [Validation of the Peruvian version of the PHQ-9 for diagnosing depression] Rev Peru Med Exp Salud Publica. 2012;29(4):578–579. doi: 10.1590/s1726-46342012000400027. [Spanish] [DOI] [PubMed] [Google Scholar]
- 14.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ali GC, Ryan G, De Silva MJ. Validated screening tools for common mental disorders in low- and middle-income countries: a systematic review. PLoS One. 2016;11(6):e0156939. doi: 10.1371/journal.pone.0156939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Netsereab TB, et al. Validation of the WHO self-reporting questionnaire-20 (SRQ-20) item in primary health care settings in Eritrea. Int J Ment Health Syst. 2018;12:61. doi: 10.1186/s13033-018-0242-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Harpham T, et al. Measuring mental health in a cost-effective manner. Health Policy Plan. 2003;18(3):344–349. doi: 10.1093/heapol/czg041. [DOI] [PubMed] [Google Scholar]
- 18.Sartorius N, Janca A. Psychiatric assessment instruments developed by the World Health Organization. Soc Psychiatry Psychiatr Epidemiol. 1996;31(2):55–69. doi: 10.1007/BF00801901. [DOI] [PubMed] [Google Scholar]
- 19.Ministerio de Salud Dirección General de Intervenciones Estratégicas en Salud Pública. Norma técnica de salud para el control del crecimiento y desarrollo de la niña y el niño menor de cinco años Lima. Lima, Peru: MINSA; 2017. [Spanish] [Google Scholar]
- 20.Rodriguez S, Arancibia V, Undurraga C. Escala de evaluación del desarrollo psicomotor de 0–24 meses. Santiago, Chile: Editorial Galdoc; 1996. [Spanish] [Google Scholar]
- 21.Scholte WF, et al. Psychometric properties and longitudinal validation of the self-reporting questionnaire (SRQ-20) in a Rwandan community setting: a validation study. BMC Med Res Methodol. 2011;11:116. doi: 10.1186/1471-2288-11-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Aguilar Esenarro L Guía técnica para la valoración nutricional antropométrica de la persona adulta mayor. Lima, Peru: Ministerio de Salud, Instituto Nacional de Salud; 2013. [Google Scholar]
- 23.Centers for Disease Control and Prevention Atlanta, GA, USA: CDC; Prediabetes risk test. [Google Scholar]
- 24.American Diabetes Association Risk test. Arlington, VA, USA: AMA, Bernabe-Ortiz A, et al. Diagnostic accuracy of the Finnish Diabetes Risk Score (FINDRISC) for undiagnosed T2DM in Peruvian population. Prim Care Diabetes. 2018;12(6):517–525. doi: 10.1016/j.pcd.2018.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ministerio de Salud, Dirección General de Salud de las Personas, Estrategia Sanitaria Nacional de Prevención y Control de Daños No Transmisibles. Guía de práctica clínica para la prevención y control de la enfermedad hipertensiva en el primer nivel de atención R. M. N 491-2009/MINSA. Lima, Peru: MINSA; 2011. [Spanish] [Google Scholar]
- 26.Ministerio de Salud, Dirección General de Intervenciones Estratégicas en Salud Pública, Dirección de Prevención y Control de Cáncer. Plan nacional para la prevención y control de cáncer de mama en el Perú 2017–2021. R.M. N 442-2017/MINSA. Lima, Peru: MINSA; 2017. [Google Scholar]
- 27.Socios En Salud. Lima, Peru: SES; 2020. Chatbot GESTAMOR. [Google Scholar]
- 28.Dawson KS, et al. Problem Management Plus (PM+): a WHO transdiagnostic psychological intervention for common mental health problems. World Psychiatry. 2015;14(3):354–357. doi: 10.1002/wps.20255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Miller AC, et al. Success at scale: outcomes of community-based neurodevelopment intervention (CASITA) for children 6–20 months with risk of delay in Lima, Peru. Child Dev. 2021;92(6):e1275–e1289. doi: 10.1111/cdev.13602. [DOI] [PubMed] [Google Scholar]
- 30.Ndayizigiye M, et al. BMJ Open. 2021. Improving child development and parenting skills by integrating an early child development intervention into primary health care in rural Lesotho. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nelson AK, et al. CASITA: a controlled pilot study of community-based family coaching to stimulate early child development in Lima, Peru. BMJ Paediatr Open. 2018;2(1):e000268. doi: 10.1136/bmjpo-2018-000268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ministerio de Salud. Población estimada de la DIRIS Lima Norte por edades simples, grupos de edad, según distrito y establecimientos, año 2019. Lima, Peru: MINSA; 2019. [Google Scholar]
- 33.National Institute for Statistics and Information of Peru Población de 6 y más años de edad que hace uso del servicio de internet, según ámbitos geográficos. Lima, Peru: NISI; 2019. [Google Scholar]
- 34.National Institute for Statistics and Information of Peru Hogares con al menos una computadora, por años, según ámbitos geográficos. Lima, Peru: NISI; 2019. [Google Scholar]
- 35.Statistica Smartphone user penetration rate in Lima, Peru between 2012 and 2019. Lima, Peru: Statistica; 2021. [Google Scholar]
- 36.National Institute for Statistics and Information of Peru Población afiliada a algún seguro de salud. Lima, Peru: NISI; 2018. [Google Scholar]
- 37.Vilchez-Cornejo J, et al. Depression and Abuse During Medical Internships in Peruvian Hospitals. Rev Colomb Psiquiatr. 2020;49(2):76–83. doi: 10.1016/j.rcp.2018.08.001. [DOI] [PubMed] [Google Scholar]
- 38.BinDhim NF, et al. Depression screening via a smartphone app: cross-country user characteristics and feasibility. J Am Med Inform Assoc. 2015;22(1):29–34. doi: 10.1136/amiajnl-2014-002840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Antiporta DA, et al. Depressive symptoms among Peruvian adult residents amidst a national lockdown during the COVID-19 pandemic. BMC Psychiatry. 2021;21(1):111. doi: 10.1186/s12888-021-03107-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hossain MM, et al. Epidemiology of mental health problems in COVID-19: a review. F1000Res. 2020;9:636. doi: 10.12688/f1000research.24457.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chudasama YV, et al. Impact of COVID-19 on routine care for chronic diseases: a global survey of views from healthcare professionals. Diabetes Metab Syndr. 2020;14(5):965–967. doi: 10.1016/j.dsx.2020.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fekadu G, et al. Impact of COVID-19 pandemic on chronic diseases care follow-up and current perspectives in low resource settings: a narrative review. Int J Physiol Pathophysiol Pharmacol. 2021;13(3):86–93. [PMC free article] [PubMed] [Google Scholar]
- 43.National Institute for Statistics and Information of Peru Perú resultados definitivos de los censos nacionales, 2017. Lima, Peru: NISI; 2018. [Google Scholar]
- 44.Zhang J, et al. Rural-urban disparities in knowledge, behaviors, and mental health during COVID-19 pandemic: a community-based cross-sectional survey. Medicine. 2021;100(13):e25207. doi: 10.1097/MD.0000000000025207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xiong J, et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Malpass A, et al. Concordance between PHQ-9 scores and patients’ experiences of depression: a mixed methods study. Br J Gen Pract. 2010;60(575):e231–238. doi: 10.3399/bjgp10X502119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Brown J, Halpern J. AI chatbots cannot replace human interactions in the pursuit of more inclusive mental healthcare. SSM Mental Health. 2021;1:100017. [Google Scholar]


