Abstract
Background
Limited information exists regarding the clinical characteristics, management practices, and outcomes of pediatric patients with liver injury in Japan. The aim of this study is to evaluate the characteristics, management, and outcome of pediatric patients with liver injury in Japan.
Methods
We conducted a multicenter, retrospective cohort study using data from the Japan Trauma Data Bank between 2004 and 2018. Pediatric patients with liver injury were classified into the following management groups: nonoperative management (NOM); NOM with angioembolization (AE); operative management (OM). The primary outcome was in-hospital survival, and the secondary outcomes were dispositions, hospital length of stay (LOS), and rate of discharge to home.
Results
There were 308 pediatric patients with severe liver injury (organ injury scale grades ≥Ⅲ) during the study period; 135 patients had isolated liver injury and 173 patients had non-isolated liver injury. The rates of NOM, NOM with AE, and OM among all patients were 65%, 23%, and 12%, respectively. AE was highly used both in patients with isolated liver injury (27%) and non-isolated liver injury (22%). In-hospital survival of patients with isolated liver injury and those with non-isolated liver injury were 99% and 88%, respectively. Regarding secondary outcomes among patients with isolated liver injury, 82% were admitted to the intensive care unit. LOS was 11 (8–14) days and 82% were discharged to home.
Conclusions
Our retrospective observational study showed that management of pediatric patients with severe liver injury in Japan was characterized by high utilization of AE. The in-hospital survival rate in Japan was comparable with that of other developed countries.
Keywords: pediatrics, surgery, plastic
Key messages.
What is already known about this subject?
Limited information exists regarding the clinical characteristics, management practices, and outcomes of pediatric patients with liver injury in Japan.
Angioembolization has been established as adjunct to nonoperative management among adult patients with liver injury; however, there is limited evidence of utilization of angioembolization for pediatric patients with liver injury.
What are the new findings?
This study showed that management of pediatric patients with severe liver injury in Japan was characterized by high utilization of angioembolization.
How might it impact on clinical practice in the foreseeable future?
Angioembolization for pediatric patients with liver injury may obviate the operative management.
Introduction
Trauma remains as a major cause of death in young people in Japan.1 Abdominal injuries, which occur in 10% to 15% of all pediatric trauma cases, can be a significant source of morbidity.2 Liver injury is one of the most common solid organ injuries in pediatric patients with abdominal injuries.3 4
Management of pediatric patients with liver trauma was drastically changed by the introduction of non-operative management (NOM).5 Previous reports indicate that most pediatric patients with liver injury can be managed with NOM4 6 and only 3% require operative management (OM) to arrest hemorrhage.4 Angioembolization (AE) has been established as adjunct to NOM among adult patients with organ injury7; however, there is limited evidence of utilization of AE for pediatric patients with organ injury, including liver injury,8 and its usefulness was controversial.
The aim of this study was to clarify the characteristics, management patterns, and outcomes of pediatric patients with liver injury in Japan, particularly those who underwent AE.
Methods
Study design
This study was a multicenter, retrospective cohort study using the Japan Trauma Data Bank (JTDB) data from 2004 to 2018. JTDB is a nationwide trauma registry established in 2003 by the Japanese Association for Surgery of Trauma and the Japanese Association for Acute Medicine to improve and ensure the quality of trauma care in Japan. During the study period, 291 hospitals including 95% of tertiary emergency medical centers in Japan participated in the JTDB. The JTDB collects 92 data elements related to patient and hospital information, such as patient demographics, physiology, abbreviated injury scale (AIS) score, injury severity score (ISS), in-hospital procedures, and in-hospital survival.
Patient selection
Pediatric patients aged <16 years and with liver injury [American Association for the Surgery of Trauma Organ Injury Scale (AAST-OIS) grades ≥Ⅲ]. Assignment of liver injury grade was accomplished based on liver AIS scoring.9 Exclusion criteria included cardiopulmonary arrest on arrival, AIS grade=6 for any region, and missing outcome of survival.
Study endpoints
The primary outcome of this study was in-hospital survival, and the secondary outcomes were disposition, hospital length of stay (LOS), and discharged to home.
Analysis
Descriptive statistics included frequency and percentage for categorical variables and medians and interquartile range (IQR) for continuous variables. First, pediatric patients with liver injury were classified into isolated liver injury and non-isolated liver injury groups. In addition, the two groups were further subclassified into three management groups (NOM, NOM with AE, and OM). Patients who underwent both AE and OM were included in the OM group. Baseline characteristics and outcomes among pediatric patients with isolated and non-isolated liver injury were compared among the three management groups. Second, we were particularly interested in the use of AE for pediatric patients with liver injury; therefore, we compared baseline characteristics and outcomes among two groups, that is, isolated liver injury and non-isolated liver injury treated with AE. Comparisons of continuous variables between groups were performed using the Kruskal-Wallis test. Categorical variables were expressed as counts and percentages, and comparisons of each categorical variable between groups were performed using the χ2 test. Third, we descriptively analyzed the time to interventions. We defined the time to interventions as the time from hospital arrival to the time of initiation of interventions. For patients who had missing data for the time of hospital arrival, we substituted the time for the time of initiation of physician’s treatment after hospital arrival. Statistical significance was defined as a two-sided p value <0.05 in all statistical analyses. All analyses were performed using IBM SPSS Statistics V.25.0 and R software (V.3.5.2; R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics and primary outcome between patients with isolated liver injury and those with non-isolated liver injury
A total of 361,706 patients were registered in the JTDB from 2004 to 2018. Of the 22,650 pediatric patients, 349 patients had liver injury (liver OIS grades ≥Ⅲ). Among these 349 patients, 41 were excluded based on the aforementioned exclusion criteria (ie, cardiopulmonary arrest on arrival=20, AIS grade=6 for any region=1, and missing outcome of survival; total=20, isolated liver injury=9, and non-isolated liver injury=11). A total of 308 pediatric patients with liver injury were analyzed. Subsequently, the 308 pediatric patients with liver injury were subclassified as isolated liver injury (n=135) and non-isolated liver injury (n=173). Characteristics and primary outcomes of pediatric patients with isolated liver injury and non-isolated liver injury are shown in table 1. The median age was 9 (6–12) years and 67% of the patients were male. Traffic accident was the most frequent cause of injury, accounting for 68% of cases. There was a significant difference in the rate of laparotomy (p=0.028); however, there was no significant difference in the rate of AE between the isolated liver injury group and non-isolated liver injury group (p=0.338). The in-hospital survival rate was 99% in the isolated liver injury group and was 88% in the non-isolated liver injury group. Among patients with isolated liver injury, one died because of intra-abdominal bleeding after laparotomy. Among patients with non-isolated liver injury, 22 were thought to have died from the following causes: traumatic brain injury (head AIS=5) in 5 and multiple blunt force in 17 patients.
Table 1.
Characteristics and in-hospital survival of pediatric patients with liver injury
| Variable | Isolated liver injury (n=135) | Non-isolated liver injury (n=173) | P value |
| At arrival, median (IQR) | |||
| sBP (mmHg) | 116 (104–128) | 118 (96–132) | 0.711 |
| HR (beats per min) | 100 (81–112) | 121 (105–145) | <0.001 |
| RR (breaths per min) | 23 (20–27) | 26 (20–32) | <0.001 |
| GCS value | 15 (15–15) | 14 (9–15) | <0.001 |
| AIS of liver injury, n (%) | 0.008 | ||
| AIS=3 | 105 (78) | 112 (65) | |
| AIS=4 | 27 (20) | 44 (25) | |
| AIS=5 | 3 (2.2) | 17 (10) | |
| Intervention for liver injury, n (%) | |||
| Laparotomy | 10 (7.4) | 27 (16) | 0.028 |
| AE | 35 (26) | 38 (22) | 0.338 |
| ISS, median (IQR) | 9 (9–14) | 27 (22–35) | <0.001 |
| In-hospital survival, n (%) | 134 (99) | 152 (88) | <0.001 |
AE, angioembolization; AIS, abbreviated injury scale; GCS, Glasgow Coma Scale; HR, heart rate; IQR, interquartile range; ISS, injury severity score; RR, respiratory rate; sBP, systolic blood pressure.
Blunt isolated and non-isolated liver injury according to management groups
The characteristics and outcomes among patients with blunt isolated and non-isolated liver injury according to management methods are shown in table 2. In the isolated liver injury group, management consisted of NOM in 89 patients (66%), AE in 35 patients (26%), and OM in 10 patients (7%). OM group had significantly lower systolic blood pressure at hospital arrival (p=0.018). There was no statistically significant difference among liver OIS grade between management. In the non-isolated liver injury group, management consisted of NOM in 110 patients (65%), AE in 35 patients (21%), and OM in 24 patients (14%). Systolic blood pressure was lower in OM group (p=0.003), and there were significant differences of rates of liver OIS grades Ⅲ and Ⅴ between management groups.
Table 2.
Characteristics of pediatric patients with blunt isolated and non-isolated liver injury according to management groups
| Group | Isolated liver injury | Non-isolated liver injury | ||||||
| Variable | NOM | NOM with AE | OM | P value | NOM | NOM with AE | OM | P value |
| (n=89) | (n=35) | (n=10) | (n=110) | (n=35) | (n=24) | |||
| Demographics | ||||||||
| Age (y), median (IQR) | 9 (7–11) | 10 (7–12) | 10 (6–12) | 0.476 | 8 (4–11) | 9 (7–14) | 10 (7–12) | 0.075 |
| Gender (male), n (%) | 62 (70) | 28 (80) | 8 (80) | 0.444 | 74 (67) | 17 (49) | 14 (58) | 0.128 |
| Mechanism of injury, n (%) | 0.408 | 0.913 | ||||||
| Traffic accident | 55/89 (62) | 21/34 (62) | 5/10 (50) | 80/105 (76) | 27/35 (77) | 18/24 (75) | ||
| Fall | 22/89 (25) | 6/34 (18) | 1/10 (10) | 20/105 (19) | 7/35 (20) | 4/24 (17) | ||
| Sport | 5/89 (5.6) | 2/34 (5.9) | 1/10 (10) | 0/105 (0) | 0/35 (0) | 0/24 (0) | ||
| Other blunt injury | 7/89 (7.9) | 5/34 (15) | 3/10 (30) | 5/105 (4.8) | 1/35 (2.9) | 2/24 (8.3) | ||
| At arrival, median (IQR) | ||||||||
| sBP (mmHg) | 116 (108–130) | 120 (107–130) | 99 (82–115) | 0.018 | 120 (100–133) | 120 (104–136) | 90 (62–116) | 0.003 |
| HR (beats per min) | 97 (80–112) | 100 (80–110) | 109 (99–138) | 0.163 | 118 (105–142) | 127 (117–147) | 140 (97–150) | 0.161 |
| RR (breaths per min) | 24 (20–28) | 22 (20–24) | 25 (20–29) | 0.253 | 25 (20–32) | 30 (23–33) | 26 (23–32) | 0.282 |
| GCS value | 15 (15–15) | 15 (15–15) | 15 (14–15) | 0.039 | 14 (11–15) | 13 (10–15) | 7 (3–11) | <0.001 |
| Liver OIS grades, n (%) | ||||||||
| Grade Ⅲ | 71 (80) | 27 (77) | 6 (60) | 0.363 | 82 (75) | 18 (51) | 8 (33) | <0.001 |
| Grade Ⅳ | 17 (19) | 7 (20) | 3 (30) | 0.717 | 23 (21) | 14 (40) | 7 (29) | 0.075 |
| Grade Ⅴ | 1 (1.1) | 1 (2.9) | 1 (10) | 0.19 | 5 (4.5) | 3 (8.6) | 9 (38) | <0.001 |
| Blood transfusion, n (%) | 7/89 (8.0) | 7/35 (20) | 7/10 (70) | <0.001 | 30/109 (28) | 27/35 (77) | 21/24 (88) | <0.001 |
| In-hospital survival, n (%) | 89/89 (100) | 35/35 (100) | 9/10 (90) | 0.002 | 101/110 (92) | 34/35 (97) | 14/24 (58) | <0.001 |
AE, angioembolization; GCS, Glasgow Coma Scale; HR, heart rate; IQR, interquartile range; NOM, nonoperative management; OIS, organ injury scale; OM, operative management; RR, respiratory rate; sBP, systolic blood pressure.
AE use for pediatric patients with liver injury
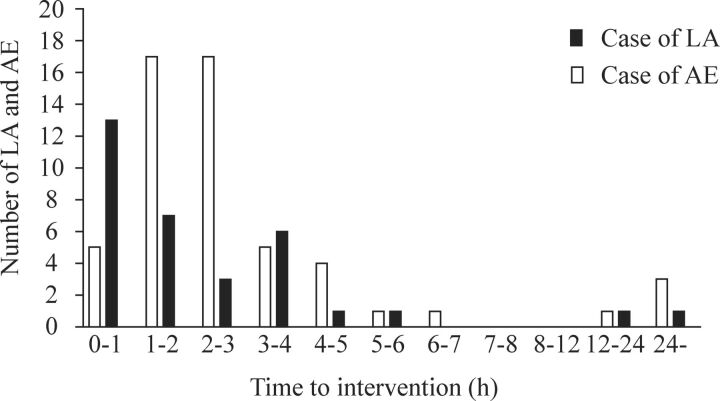
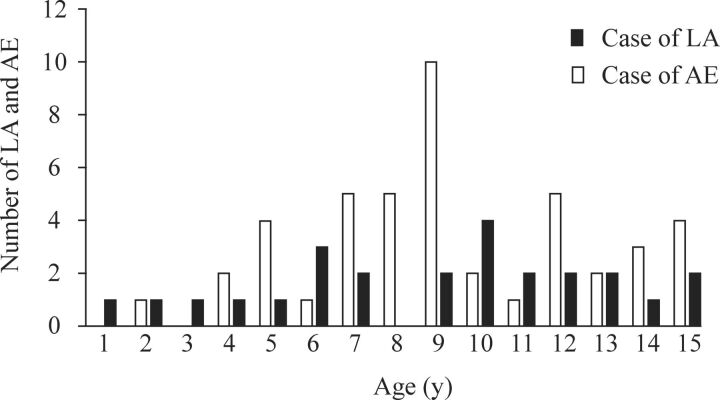
The characteristics and outcomes of pediatric patients with liver injury who underwent AE were classified between isolated and non-isolated liver injury (table 3). The in-hospital survival rate among all pediatric patients with liver injury who underwent AE was 99%, and only one patient who had concomitant severe traumatic brain injury died. The distribution of time to intervention is shown in figure 1. Approximately 70% of laparotomy and 72% of AE procedures were conducted within 3 hours after hospital arrival. The distribution of ages at the time of intervention is shown in figure 2. There were no age differences among AE patients. In the non-isolated liver injury group, eight patients had severe abdominal injury (OIS≥Ⅲ) in addition to severe liver injury, and all patients initially had unstable hemodynamics (online supplemental table 1). Repeated AE was performed for four patients (two patients among isolated liver injury and two patients among non-isolated liver injury).
Table 3.
Characteristics of angioembolization use for pediatric patients with isolated and non-isolated liver injury
| Variable | Isolated liver injury | Non-isolated liver injury | P value |
| (n=35) | (n=35) | ||
| Demographics | |||
| Age (y), median (IQR) | 10 (7–13) | 9 (7–14) | 0.791 |
| Gender (male), n (%) | 28 (80) | 17 (49) | 0.012 |
| Cause of injury, n (%) | 0.126 | ||
| Traffic accident | 21/34 (61) | 27 (77) | |
| Fall | 6/34 (18) | 7 (20) | |
| Sport | 2/34 (5.9) | 0 (0) | |
| Other blunt injury | 5/34 (15) | 1 (2.9) | |
| Prehospital, median (IQR) | |||
| sBP (mmHg) | 117 (103–126) | 111 (100–128) | 0.761 |
| HR (beats per min) | 104 (84–113) | 125 (107–139) | <0.001 |
| RR (breaths per min) | 24 (20–25) | 28 (24–36) | 0.062 |
| At arrival, median (IQR) | |||
| sBP (mmHg) | 120 (106–130) | 120 (104–136) | 0.851 |
| HR (beats per min) | 100 (80–110) | 127 (117–147) | <0.001 |
| RR (breaths per min) | 22 (20–24) | 30 (23–33) | <0.001 |
| GCS value | 15 (15–15) | 13 (10–15) | <0.001 |
| Liver injury AIS, median (IQR) | 3 (3–4) | 4 (3–4) | 0.007 |
| ISS, median (IQR) | 9 (9–14) | 29 (26–34) | <0.001 |
| RTS, median (IQR) | 7.8 (7.8–7.8) | 7.6 (6.6–7.6) | <0.001 |
| TRISS-Ps, median (IQR) | 99 (99–99) | 95 (91–97) | <0.001 |
| Blood transfusion, n (%) | 7 (20) | 27 (77) | <0.001 |
| Time to AE (min), median (IQR) | 144 (101–262) | 138 (85–155) | 0.152 |
| In-hospital survival, n (%) | 35 (100) | 34 (97) | 0.317 |
Missing: cause of injury=1, prehospital sBP=13, prehospital HR=13, prehospital RR=21, at arrival HR=1, at arrival RR=1, at arrival GCS value=2, RTS=3, TRISS-Ps=3, blood transfusion=3, time to angioembolization=16.
AE, angioembolization; AIS, abbreviated injury scale; GCS, Glasgow Coma Scale; HR, heart rate; IQR, interquartile range; ISS, injury severity score; RR, respiratory rate; RTS, revised trauma score; sBP, systolic blood pressure; TRISS-Ps, trauma and injury severity score–probability of survival.
Figure 1.
Distribution of time to intervention. AE, angioembolization; LA, laparotomy.
Figure 2.
Distribution of ages between laparotomy and angioembolization. LA, laparotomy;AE, angioembolization.
wjps-2021-000270supp001.pdf (34.3KB, pdf)
Secondary outcomes among patients with isolated liver injury according to management groups
Secondary outcomes among patients with isolated liver injury according to the method of management are shown in table 4. The rate of admission to the intensive care unit (ICU) was significantly lower in the NOM group, whereas there were no significant differences among LOS and discharged to home between management groups.
Table 4.
Secondary outcomes of pediatric patients with isolated liver injury according to management groups
| Outcome | NOM | NOM with AE | OM | P value |
| (n=90) | (n=35) | (n=10) | ||
| Disposition, n (%) | 0.016 | |||
| Intensive care unit | 68 (76) | 34 (97) | 9 (90) | |
| Ward | 19 (21) | 1 (2.9) | 0 (0) | |
| Other | 2 (2.2) | 0 (0) | 1 (10) | |
| LOS (d), median (IQR) | 10 (8–14) | 13 (10–15) | 16 (12–46) | 0.097 |
| Discharge place, n (%) | 0.916 | |||
| Home | 74 (82) | 30 (86) | 7 (78) | |
| Another hospital | 14 (16) | 4 (11) | 2 (22) | |
| Other places | 2 (2.2) | 1 (2.9) | 0 (0) | |
Missing: LOS=2, ward=1, discharge place=1.
AE, angioembolization; IQR, interquartile range; LOS, hospital length of stay; NOM, nonoperative management; OM, operative management.
Discussion
The in-hospital survival rates among the isolated liver injury and non-isolated liver injury groups were 99% and 88%, respectively, and the rates of AE utilization were 27% and 22%, respectively.
To facilitate comparison with the present study, the design and results of previous studies are summarized in online supplemental table 2. In our study, the population was limited to severe liver injury (liver OIS grades ≥Ⅲ), which was thought to affect the management and outcomes. Among patients with isolated liver injury, approximately 26% underwent AE, and this rate was higher than in previous studies of cases with high-grade injury (grade Ⅲ or higher, 4.8%).10 A recent systematic review of pediatric organ injury indicated that the use of AE was limited to patients with hemodynamic compromise from ongoing bleeding.8 11 In our study the isolated liver injury patients requiring AE whose age-adjusted shock index12 were approximately 40% (27/68) positive, and this rate was higher than the rate (25%) of Swendiman’s study.10 With respect to hemodynamic status, AE for isolated liver injury was used for appropriate hemodynamically unstable cases. Among patients with isolated liver injury who underwent AE, only 20% needed blood transfusion. We were unable to find any published studies regarding the incidence rate of blood transfusion among patients with isolated liver injury requiring AE; thus, there was no frame of reference for comparison with our results. Kiankhooy and colleagues reported that pediatric patients with solid organ injury did not require blood transfusion after AE.13 In the present study, the median time to AE was 144 (101–262) minutes, which was shorter than in previous reports10 13 [216 (120–420) minutes]; therefore, a shorter time to AE may contribute to lower blood transfusion rates.
wjps-2021-000270supp002.pdf (34KB, pdf)
AE was often used among patients with non-isolated liver injury in the present study. Notably, liver trauma patients who had additional severe abdominal injury and underwent AE (online supplemental table 1) were initially hemodynamically unstable, and all patients required blood transfusion. Half of the patients had both liver injury and splenic injury. It has been reported that combined liver and splenic injury is a risk factor for NOM failure4 and that NOM failure for bleeding occurs within 162 (102–240) minutes from injury.4 14 In our study, AE was deployed within 180 minutes as well as laparotomy (figure 1). Especially in patients with combined liver and additional abdominal injury, the median time to AE was 84 (67–128) minutes, and this shorter time could obviate the need for laparotomy.
The decision to use AE and laparotomy depends on various factors, including hospital-related factors, such as the utilization of angiography. A previous report showed that adult trauma centers conducted angiography for isolated splenic trauma at nine times the frequency of pediatric trauma centers.10 In Japan, there are few pediatric trauma centers, and pediatric trauma patients are generally managed at adult trauma centers, which could account for the country’s high frequency of AE use. Guidelines of interventional radiology for liver injury in Japan suggest the practice of interventional radiology for pediatric patients with liver injury could be selected based on CT findings (the existence of arterial extravasation) and should be selected more carefully than adult patients.15 On the other hand, all the 70 patients underwent AE in this study and there was no report that demonstrated such a large pediatric case underwent AE, and this was one of the strengths of this study.
The in-hospital survival rate among patient with isolated liver injury was 99% and was similar to previous reports.4 6 10 Regardless of the grades of liver injury, pediatric patients with isolated liver injury could be expected to survive. The in-hospital survival rate among patients with non-isolated liver injury was 12%, which was higher than the 7.5% rate reported by Dervan et al (online supplemental table 2). The higher rate was likely attributable to disease severity (OIS≥Ⅲ) in the patients selected, and the causes of death were thought to be multisystem trauma including traumatic brain injury.4 Regarding secondary outcomes among patients with isolated liver injury, almost all the cases that underwent NOM with AE and approximately 76% of the NOM cases were admitted to the ICU. Stylianos showed that approximately 76% of patients with isolated spleen or liver injury with a CT grade greater than 3 were admitted to the ICU, and this rate was similar to that in our study.11 Recent guidelines suggest ICU admission for patients with a CT grade greater than 4.8 11 In addition, LOS in our study was longer than that of recent systematic review recommendations.8 This result may be attributed to characteristics of the healthcare system in Japan.16 The self-pay burden of patients is low in Japan because Japan has a universal healthcare system and the High-Cost Medical Expense Financial Plan extends to almost all citizens. Therefore, the LOS was longer compared with that of other countries.
There were several limitations of this study. First, because this was an observational study, we could not obtain precise indication for AE, such as arterial extravasation on enhanced CT or information on embolized arteries. Second, we could not gain information of who was initially managing pediatric patients with liver injury.10 Therefore, additional prospective study is needed to verify the usefulness of AE for pediatric patients with liver injury.
In conclusion, this study showed that in-hospital survival among pediatric patients with liver injury in Japan was comparable with that of other developed countries, while the management approach was characterized by high rates of AE utilization (27% and 22% among patients with isolated liver injury and non-isolated liver injury, respectively). A shorter time to AE may have reduced NOM failure among patients with non-isolated liver injury.
Acknowledgments
We thank the JTDB and all personnel at the participating institutions who facilitated the study.
Footnotes
Contributors: AM contributed to writing—original draft, data curation, investigation, methodology and visualization. AT contributed to methodology and writing—review and editing. HS contributed to writing—review and editing. SD contributed to writing—review and editing. OK contributed to writing—review and editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study was approved by the medical ethics committee of the Gunma University Hospital. Because of the anonymous and retrospective nature of the study, the need for informed consent was waived.
References
- 1. Aoki M, Abe T, Saitoh D, et al. Epidemiology, patterns of treatment, and mortality of pediatric trauma patients in Japan. Sci Rep 2019;9:917. 10.1038/s41598-018-37579-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gaines BA. Intra-abdominal solid organ injury in children: diagnosis and treatment. J Trauma 2009;67:S135–9. 10.1097/TA.0b013e3181adc17a [DOI] [PubMed] [Google Scholar]
- 3. Tataria M, Nance ML, Holmes JH, et al. Pediatric blunt abdominal injury: age is irrelevant and delayed operation is not detrimental. J Trauma 2007;63:608–14. 10.1097/TA.0b013e318142d2c2 [DOI] [PubMed] [Google Scholar]
- 4. Linnaus ME, Langlais CS, Garcia NM, et al. Failure of nonoperative management of pediatric blunt liver and spleen injuries: a prospective Arizona-Texas-Oklahoma-Memphis-Arkansas Consortium study. J Trauma Acute Care Surg 2017;82:672–9. 10.1097/TA.0000000000001375 [DOI] [PubMed] [Google Scholar]
- 5. Douglas GJ, Simpson JS. The conservative management of splenic trauma. J Pediatr Surg 1971;6:565–70. 10.1016/0022-3468(71)90380-0 [DOI] [PubMed] [Google Scholar]
- 6. Dervan LA, King MA, Cuschieri J, et al. Pediatric solid organ injury operative interventions and outcomes at Harborview Medical Center, before and after introduction of a solid organ injury pathway for pediatrics. J Trauma Acute Care Surg 2015;79:215–20. 10.1097/TA.0000000000000726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Coccolini F, Coimbra R, Ordonez C. WSES expert panel. liver trauma: WSES 2020 guidelines. World J Emerg Surg 2020;15:24. 10.1186/s13017-020-00302-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gates RL, Price M, Cameron DB, et al. Non-operative management of solid organ injuries in children: an American Pediatric Surgical Association Outcomes and Evidence Based Practice Committee systematic review. J Pediatr Surg 2019;54:1519–26. 10.1016/j.jpedsurg.2019.01.012 [DOI] [PubMed] [Google Scholar]
- 9. Tinkoff G, Esposito TJ, Reed J, et al. American Association for the Surgery of Trauma Organ Injury Scale I: spleen, liver, and kidney, validation based on the National Trauma Data Bank. J Am Coll Surg 2008;207:646–55. 10.1016/j.jamcollsurg.2008.06.342 [DOI] [PubMed] [Google Scholar]
- 10. Swendiman RA, Goldshore MA, Fenton SJ, et al. Defining the role of angioembolization in pediatric isolated blunt solid organ injury. J Pediatr Surg 2020;55:688–92. 10.1016/j.jpedsurg.2019.04.036 [DOI] [PubMed] [Google Scholar]
- 11. Stylianos S. Evidence-based guidelines for resource utilization in children with isolated spleen or liver injury. The APSA trauma committee. J Pediatr Surg 2000;35:164–9. 10.1016/S0022-3468(00)90003-4 [DOI] [PubMed] [Google Scholar]
- 12. Acker SN, Ross JT, Partrick DA, et al. Pediatric specific shock index accurately identifies severely injured children. J Pediatr Surg 2015;50:331–4. 10.1016/j.jpedsurg.2014.08.009 [DOI] [PubMed] [Google Scholar]
- 13. Kiankhooy A, Sartorelli KH, Vane DW, et al. Angiographic embolization is safe and effective therapy for blunt abdominal solid organ injury in children. J Trauma 2010;68:526–31. 10.1097/TA.0b013e3181d3e5b7 [DOI] [PubMed] [Google Scholar]
- 14. Holmes JH, Wiebe DJ, Tataria M, et al. The failure of nonoperative management in pediatric solid organ injury: a multi-institutional experience. J Trauma 2005;59:1309–13. 10.1097/01.ta.0000197366.38404.79 [DOI] [PubMed] [Google Scholar]
- 15. Guideline of interventional radiology for liver trauma, 2016. Available: http://www.jsir.or.jp/about/guide_line/kangaisyo/ [Accessed July 1, 2020].
- 16. Matsumoto S, Jung K, Smith A, et al. Comparison of trauma outcomes between Japan and the USA using national trauma registries. Trauma Surg Acute Care Open 2018;3:e000247. 10.1136/tsaco-2018-000247 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
wjps-2021-000270supp001.pdf (34.3KB, pdf)
wjps-2021-000270supp002.pdf (34KB, pdf)
Data Availability Statement
Data are available on reasonable request.