Abstract
Background
Within the last decade, the use of telemedicine within in primary care in the USA has greatly expanded; however, use remains uncommon in surgical specialties. The spread of Coronavirus disease 2019 (COVID-19) prompted healthcare institutions to limit in-person contact, resulting in an increase in telemedicine across all specialties, including pediatric surgery. The aims of this review were to evaluate potential barriers that limited the use of telemedicine in pediatric surgery prior to the COVID-19 period and to define how best to incorporate its use into a pediatric surgical practice going forward.
Methods
A scoping review was performed to identify gaps in the literature pertaining to the use of telemedicine within general pediatric surgery in the USA prior to the outbreak of COVID-19. Next, a focused evaluation of the legislative and organizational policies on telemedicine was performed. Lastly, findings were summarized and recommendations for future research developed in the context of understanding and overcoming barriers that have plagued widespread adoption in the past.
Results
Despite evidence of telemedicine being safe and well received by adult surgical patients, a total of only three studies representing original research on the use of telemedicine within pediatric surgery were identified. Legislative and organizational policies regarding telemedicine have been altered in response to COVID-19, likely resulting in an increase in the use of telemedicine among pediatric surgeons.
Conclusions
Telemedicine offers a safe and effective option for patients seeking an alternative to the in-person clinic appointment. The increased utilization of telemedicine during the COVID-19 pandemic will provide an opportunity to learn how best to leverage the technology to decrease disparities and to overcome previous barriers.
Keywords: COVID-19, qualitative research, pediatrics, patient outcome assessment, technology
Introduction
The potential to remotely evaluate patients dates to the early 1900s when Dutch physiologist Willem Einthoven was able to demonstrate the ability to send and receive cardiac signals over a distance of 1.5 km.1 The term ‘telemedicine’ came into existence in the 1970s, but early attempts to incorporate it into medical practices failed due in large part to inefficiencies and cost. In the 1990s, the internet provided a more reliable means to remotely connect patient and provider, and the use of telemedicine began to gain traction.2 3 However, inconsistencies in reimbursement practices and uncertainty among the public contributed to a lack of support, and widespread adoption in the USA stalled. Throughout the 2000s, a growth in the technology sector coincided with an increase in telemedicine use in the USA. In 2016, a report by the Department of Health and Human Services (HHS) estimated that more than 60% of institutions in the USA had a telemedicine program.4 In 2014, only 8% of telemedicine appointments were completed by specialists, including surgeons, and research on the topic remains rare and is often limited to single-institution pilot studies exploring postdischarge care in adults.5–7 Telemedicine remains underused within surgical fields, with limited application by some programs for postoperative visits.8
On 20 January 2020, the first reported case of infection in the USA by the SARS-CoV-2 virus was reported. The disease that results, Coronavirus disease 2019 (COVID-19), quickly spread throughout the country, necessitating that measures be taken to reduce the rate of transmission, including: suspension of elective procedures, postponement of in-person clinic appointments, and reduction of hospital staffing. These drastic measures forced the expedited adoption of telemedicine across specialties. Policy changes implemented in response increased access to telehealth for patients and lessened institutional barriers by providing clear guidelines for compensation.9 At our institution and others, the use of telemedicine during the COVID-19 period increased; however, its role beyond this period remains undefined. The aims of this review were to evaluate potential barriers that limited the use of telemedicine in pediatric surgery within the USA prior to the COVID-19 period and to define how best to incorporate its use into a pediatric surgical practice going forward.
Methods
Protocol
The protocol for this review was drafted according to the standards established by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews.10 Scoping reviews are appropriate for identifying gaps in the literature and for aiding the planning of future research projects. Given the paucity of studies and the rapidly evolving landscape surrounding telemedicine use in response to COVID-19, a review of legislative and institutional policies was undertaken to help guide a discussion on the potential benefits, barriers, and solutions for adopting telemedicine into a pediatric surgery practice.
Telemedicine in the pre-COVID era
PubMed and Scopus were queried to identify original research articles pertaining to the topic of the use of telemedicine in the pediatric surgery population within the USA prior to the COVID-19 pandemic, defined as the time before 1 December 2019. For this review, the term telemedicine was used to define both phone and video appointments. Two of the authors (GM, JA) independently screened the abstracts identified. Articles were included if they met all of the following criteria: US study population, inclusion of participants less than 21 years of age, and inclusion of surgical patients. Exclusion criteria included studies performed on adults, review articles or opinion papers, non-surgical telemedicine studies, and studies of telesurgery or telementoring.
The impact of COVID-19
The policies pertaining to the use of telemedicine at our institution were reviewed and used to provide context. A search engine was used to identify state and federal legislation related to telemedicine in relation to the COVID-19 pandemic. Additionally, a review of the recent literature on the use of telemedicine in adult surgical patients as well as a review of studies performed outside of the USA was conducted to provide context for understanding the scope of research in children in the USA.
Reviewers met as a group to discuss the full text of all publications and determined the relevancy and quality of these studies by consensus. Data charting was accomplished using Microsoft Excel, and article references were housed in EndNote.
Telemedicine research in pediatric surgery prior to COVID-19
Search results
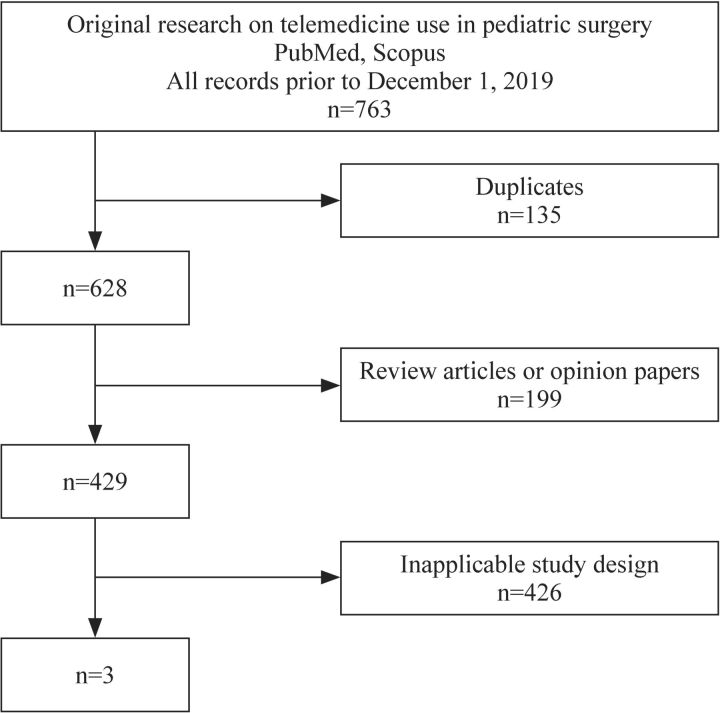
The search yielded a total of 763 articles. There were 199 articles (26.1%) that were review or opinion papers, 28 articles (3.7%) that were based on adult populations, 175 articles (22.9%) that were conducted outside of the USA, 208 studies (27.3%) that did not include surgical patients, and 329 (43.1%) that evaluated communication among providers but not between patient and provider. Only three studies were found to be original studies exploring outcomes related to the use of telemedicine in general pediatric surgery (figure 1).
Figure 1.
Article selection. A comprehensive search of the literature was undertaken to identify original research on the use of telemedicine within pediatric surgery in the USA prior to the onset of COVID-19. In total, three articles met the criteria and were reviewed in their entirety.
Study characteristics
A summary of the studies meeting criteria for inclusion can be found in table 1. The three studies that explored the use of telemedicine in a pediatric surgical population in the USA were prospective cohort studies in the postoperative period. McVay et al 11 studied the use of a phone call as a means for postoperative follow-up after elective surgery. Willard et al 12 studied the use of telemedicine to evaluate patients following discharge from a neonatal intensive care unit, with 76% of their population having undergone a surgery at some point during the admission. DeAntonio et al 13 conducted a pilot study where patients were seen both via an electronic device and in person to determine the feasibility of conducting remote postoperative follow-up appointments.
Table 1.
A Summary of original research on telemedicine use in pediatric surgery prior to COVID-19
| Title | Authors | Study type | Patient population | Summary |
| Postoperative follow-up: is a phone call enough? | McVay et al 11 | Retrospective cohort | Pediatric patients undergoing select operative procedures n=563 |
76% of patients were contacted by phone, with 27 patients requiring in-person clinic visits, and a reported 90% satisfaction rate. |
| Complex surgical infants benefit from postdischarge telemedicine visits | Willard et al 12 | Prospective cohort | Complex surgical patients following discharge from the NICU n=93 |
78 postdischarge issues were identified, 50% reported that an additional in-person visit was prevented, resulting in an accumulative 1755 of saved mileage. |
| Utilization of a handheld telemedicine device in postoperative pediatric surgical care | DeAntonio et al 13 | Prospective cohort | Pediatric patients following discharge after undergoing a variety of surgical procedures n=24 |
There were no reported changes in care for telemedicine appointments compared with in-person visits. 92% of caregivers reported being comfortable with a telemedicine-only evaluation. |
NICU, neonatal intensive care unit.
Patient outcomes
DeAntonio et al 13 evaluated patients remotely and then immediately completed an in-person visit. There were no differences observed regarding physical examination findings or treatment recommendations between the virtual meeting and in-person encounter. Willard et al 12 did not include an in-person examination for means of comparison; however, in a cohort of 96 patients there were a total of 78 medical issues identified via telemedicine, with the most common being a surgical site issue (35%).
Caregiver satisfaction
Caregiver satisfaction was high across the three studies. Willard et al 12 reported an average satisfaction and perceived appropriateness score of 3.92 (out of 4) for caregivers. In addition, 92% of caregivers stated that they would have a telemedicine-only visit for postoperative care and 79% reported that they would do the same for preoperative evaluation. Similarly, DeAntonio et al 13 reported that 75% of caregivers preferred a telemedicine follow-up appointment over an in-person visit. McVay et al 11 found that 90% of families were satisfied with postoperative follow-up via telephone.
Health system utilization
Each of the three studies included a measure of postoperative healthcare utilization. Willard et al 12 reported that families were able to avoid 50% of potential emergency department (ED) or primary care visits by using telemedicine and that 12% of telemedicine visits identified an issue that led to a recommendation to be evaluated further via an in-person appointment. DeAntonio et al 13 reported that in their cohort of 12 patients receiving postoperative telemedicine follow-up, none required an ED or clinic visit within 30 days of discharge and that two patients were able to avoid would-be ED visits through evaluation by telemedicine. In the study by McVay et al,11 a cohort of 563 patients received telephone follow-up and 43 ultimately required additional in-person evaluation.
Barriers
The three studies included in this review identified some limitations regarding the use of telemedicine in the evaluation of the pediatric surgery patient. The study designs of DeAntonio and Willard required the use of real-time videoconferencing. Willard et al 12 reported that 5% of telemedicine visits could not be completed due to technical difficulties and that caregivers reported an average satisfaction of 91 (on a scale of 1–100) for ease of use for the required camera. DeAntonio et al 13 reported no issues with connectivity but did have to provide several families with 4G-equipped devices because of a lack of access to Wi-Fi. McVay et al 11 reported that 136 of 563 patients were never reached by phone, representing a 24% rate of failed contact.
Discussion
During the past 15 years, there has been a dramatic increase in the utilization of telemedicine in the USA. Between 2004 and 2005 there were about 7000 telemedicine appointments completed by rural Medicare beneficiaries.14 By 2013, rural Medicare beneficiaries accounted for over 107 000 telemedicine visits, and in 2017 the use of telemedicine among privately insured individuals included more than 200 000 visits per year.14 15 This increased utilization of telemedicine can be attributed to many factors, including the exponential growth in the use of personal technology as well as the mandated use of an electronic health record that coincided with the implementation of the American Recovery and Reinvestment Act in 2009. However, the growth of telemedicine was predominantly in the primary care and behavioral health sectors, with specialists, including surgeons, only accounting for 8% of telemedicine visits in 2017.
Telemedicine offers an opportunity to help address disparities due to the inequity of access to pediatric surgeons based on locale and ability to travel. A recent survey of members of the American Pediatric Surgical Association found that 76% of members reside in the 50 largest metropolitan areas, leading to a relative shortage in rural America.16 In 2013, 55% of surgeries performed in North Carolina on patients less than 18 years of age were performed by a general surgeon.17 Studies have shown that pediatric patients requiring surgery experience fewer complications when their operation is performed by a high-volume pediatric surgeon.18–20 When geographic barriers or resource limitations prevent children from having access to pediatric specialists, the result is more frequent utilization of emergency services and worse long-term health outcomes.21 In the case of an emergency, the need to be seen urgently often outweighs the benefit of traveling to a pediatric facility. However, in the elective setting, telemedicine can offer an opportunity to increase access for patients when distance might otherwise make an in-person appointment impractical.
In addition to increasing access for patients, telemedicine also affords the opportunity to reduce the cost of care for patients, hospitals, and the healthcare system. Each visit with a surgeon requires that caregivers incur the direct cost of the services as well as the indirect expenses associated with travel and missed time from work. One study evaluating the burden associated with traveling to a pediatric surgery clinic found that almost one-third of patients spent more than 4 hours in transit and that for 75% of families at least one adult had to miss work.22 For patients requiring an operation, the traditional model of delivering care requires at least three visits to see a provider—one in the preoperative phase, one for the surgery, and one for postoperative evaluation. For some patients, there is no substitute for the face-to-face interaction that accompanies a traditional clinic visit. For others, telemedicine can offer a safe and effective method for diagnosing many surgical conditions while eliminating the indirect costs of preoperative in-person appointments, without compromising the care that patients receive.23 24 In most situations, the postoperative appointment equates to a cursory view of the operative site and provides limited benefit to the patient despite requiring the same indirect costs and stress associated with travel. Video is an effective method for identifying wound complications, and it can also be used to triage issues that arise prior to the scheduled appointment, preventing unnecessary utilization of emergency services and decreasing the cost for patients.12 25–27 There is benefit associated with the human contact that comes with an in-person appointment that cannot be replicated over video, but telemedicine does offer a chance to decrease the disparities in pediatric surgery by providing affordable and effective care for patients who chose to take advantage of it.
While telemedicine use within pediatric surgery in the USA has been limited, the results have been promising. At Children’s Mercy in Kansas City, a telemedicine initiative in pediatric surgery services was started in 2014. Within the first 2 years, over 170 telemedicine surgery appointments were carried out, with no reported limitations in establishing the correct diagnosis.3 28 In its report from 2016, the HHS postulated that inconsistencies in reimbursement remained one of the major barriers to increasing the prevalence of telemedicine services.4 In 2019, 42 states had telemedicine parity laws, mandating that private insurers compensate providers for remote visits.29 30 However, a report from Lacktman and Levine found that in only 10 states was compensation truly comparable between in-person and remote appointments for most services.31 With uncertain compensation and a lack of studies to show a clear benefit, it is not surprising that the use of telemedicine within pediatric surgery has failed to gain widespread support. In January 2020, a major barrier in compensation equality was removed with implementation of the 2018 Bipartisan Budget Act.7 Under the Act, requirements regarding physical locale of the patient and provider were removed for those covered under government-supported insurance, paving the way for the increased use of telemedicine within surgery and other specialties. Shortly after the Act went into effect, the rapid spread of COVID-19 mandated an acute change in the way that healthcare is delivered and provided an opportunity to study the effects of widespread telemedicine use.
By embracing a telemedicine option for patients, surgical specialties stand to benefit in ways that extend beyond direct patient care. A surgeon’s effectiveness is predicated on the number of patients treated, and when inappropriate or mistimed referrals are made the overall effect is a decrease in efficiency and a potential delay in care for some patients with legitimate surgical needs. Patients, surgeons, and primary care providers all stand to benefit when there is common ground between the surgeon and referring provider. A 2004 study of patients presenting to a pediatric surgeon found that 64.7% of referred cases were not consistent with recommended guidelines for referral.32 The result is a large proportion of patients presenting to clinic and requiring no treatment. Telemedicine promotes more frequent communication and can lead to an increase in satisfaction for both surgeons and referring providers.33 Within a year of implementing a telemedicine consult service, one large hospital system found that the average wait time for patients to be seen by a specialist decreased from 112 to 49 days, and the number of referrals made without a clear question dropped by 75% for surgical patients.34 Telemedicine represents a tool for pediatric surgeons to increase productivity by improving efficiency without demanding an increased workload for the individual surgeon. Similarly, a regional healthcare system can be improved by eliminating the unnecessary transfer of patients between facilities, a goal made feasible with the help of telemedicine. Under most circumstances, the decision to accept a transfer from an outside facility is made without the receiving facility having an opportunity to visualize the patient or access the complete medical record. Up to 20% of transfers result in no difference in care for the patient, but the financial implications can be devastating, as the cost of transfer alone can add more than $11 000 to medical expenses.35 One study of neurosurgical patients found that the use of video evaluation ultimately led to a cancellation of 33 potential transfers, resulting in an estimated savings of over $500 000.36 The addition of video when evaluating trauma, burn, and neurosurgical patients being considered for transfer can save millions of dollars and requires little to no change in workload for providers.37–39 Given the emphasis on decreasing the cost of care across the USA, it is prudent that we consider the potential benefits of including telemedicine evaluations for patients requiring consultation with a pediatric surgeon, including those where transfer to another facility is being considered.
Telemedicine offers a way for pediatric surgeons to embrace personalized medicine. The term is often poorly defined, but in general personalized medicine refers to the idea that patients benefit most when decisions are made with consideration of as many unique characteristics as possible.40 The needs of the individual patient presenting to a pediatric surgeon will vary, but there are shared characteristics among the population that make this group poised to benefit from the use of telemedicine. For one, there is the matter of comfort in a virtual space. Caregivers for pediatric patients are often younger than the patients presenting to an adult hospital and are more likely to engage with technology. A study by the Pew Research Center in 2015 found that 97% of the US population aged less than 30 years report having access to the internet, compared with 54% of senior citizens.41 Similarly, in a survey of caregivers presenting to a pediatric surgery clinic, 94% of respondents had a smartphone and 92% reported use of some form of mobile health.42 As with any proposed change, it is important to consider any limitations. The suitability of telemedicine appointments can vary widely by subspecialty, as evidenced by the range of usage at our institution. Surgeons who frequently perform office procedures or require specialized equipment for evaluation, such as those in ophthalmology or orthopedics, are less likely to use video appointments for routine care. However, many conditions requiring referral to a pediatric surgeon require a limited physical examination and can be effectively evaluated through video—allowing the patient to remain in the home environment and limiting the stress for the child while reducing the aforementioned cost of travel. Pediatric patients with complex medial conditions benefit from multidisciplinary care that includes consideration of their emotional and physical needs and can affect clinical outcomes and quality of life.43 44 Multidisciplinary treatment plans often require frequent visits to a clinic, which can lead to caregiver strain.45 46 With telemedicine, providers at different locations can interact with a patient during the same appointment, allowing for the patient and caregiver to receive the support needed from multiple specialists without the burden of frequent travel. Lastly, there is the matter of continuity of care for patients who relocate during the follow-up period, such as those pursuing postsecondary education or patients moving out of state for work or family. Telemedicine can be an effective tool for the longitudinal evaluation of postsurgical patients and offers an opportunity for adolescents to obtain access to a familiar provider while away from home or when transitioning to an adult surgeon.47
In the USA, legislative changes have been made in recognition of the need to modify healthcare delivery options in response to COVID-19. On 6 March 2020, an emergency government waiver went into effect that ensured that telemedicine video appointments for patients covered by Medicare would be paid at the same rate as in-person appointments.48 At the same time, the HHS issued an official statement announcing that enforcement of Health Insurance Portability and Accountability Act violations related to software breaches would be relaxed during the COVID-19 pandemic.49 These two measures have combined to provide assurance for providers that telemedicine can be used without loss of compensation or increased exposure to litigation. Across many institutions, the exponential growth in the use of telemedicine among pediatric surgeons during the COVID-19 period has taken place over the course of weeks—changes of this scale are typically carried out over the course of several months. Predictably, the accelerated transition has led to technological, logistical, and procedural challenges that will necessitate further study.
Conclusion
As the USA continues to navigate the challenges associated with COVID-19, the individual states and institutions within their boundaries will be left with the question of how best to move forward with patient care during this unique period in healthcare. Prior to COVID-19, the legislative landscape was evolving to promote increased use of telemedicine. With the ongoing legislative changes and the rapid institutional adoption of telemedicine during COVID-19 across different specialties, there is an opportunity to build a more robust system that offers equal care for patients regardless of locale, insurance status, or income. Further research will be necessary to study the effects that changes in the delivery of healthcare via telemedicine will have on patient outcomes.
Acknowledgments
We thank Libbey Hoang and Laura McLaughlin for providing our institutional data, and we acknowledge the entire NCH Telehealth Team for their important contributions to the quick launch of our program.
Footnotes
Contributors: MG contributed to conceptualization, data curation, formal analysis, investigation, validation, visualization, writing–original draft, writing–review and editing.JK engaged in conceptualization, data curation, writing–review and editing. AJ cotributed to data curation, formal analysis, writing–review and editing. DKJ contributed to conceptualization, methodology, writing–review and editing. MPC contributed to conceptualization, methodology, supervision, writing–original draft. HI contributed to conceptualization, methodology, project administration, supervision, visualization, writing–original draft, writing–revision and editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Not required for this review article.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data included in this manuscript are available in public, open access repositories.
References
- 1. Strehle EM, Shabde N. One hundred years of telemedicine: does this new technology have a place in paediatrics? Arch Dis Child 2006;91:956–9. 10.1136/adc.2006.099622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Mun SK, Turner JW. Telemedicine: emerging E-medicine. Annu Rev Biomed Eng 1999;1:589–610. 10.1146/annurev.bioeng.1.1.589 [DOI] [PubMed] [Google Scholar]
- 3. Waller M, Stotler C. Telemedicine: a primer. Curr Allergy Asthma Rep 2018;18:54. 10.1007/s11882-018-0808-4 [DOI] [PubMed] [Google Scholar]
- 4. Report to Congress: e-health and telemedicine. In: services USDoHaH; 2016.
- 5. Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: a systematic review. J Am Coll Surg 2016;222:915–27. 10.1016/j.jamcollsurg.2016.01.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Asiri A, AlBishi S, AlMadani W, et al. The use of telemedicine in surgical care: a systematic review. Acta Inform Med 2018;26:201–6. 10.5455/aim.2018.26.201-206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. HHS . Medicare and Medicaid programs; policy and technical changes to the Medicare advantage, Medicare prescription drug benefit, programs of All-Inclusive care for the elderly (PACE), Medicaid fee-for-service, and Medicaid managed care programs for years 2020 and 2021. Fed Regist 2019;84:15680–844 [Google Scholar]
- 8. Nikolian VC, Williams AM, Jacobs BN, et al. Pilot study to evaluate the safety, feasibility, and financial implications of a postoperative telemedicine program. Ann Surg 2018;268:700–7. 10.1097/SLA.0000000000002931 [DOI] [PubMed] [Google Scholar]
- 9. HHS . Medicare and Medicaid programs; policy and regulatory revisions in response to the COVID–19 public health emergency. Fed Regist 2020;85:19230–290 [Google Scholar]
- 10. Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 11. McVay MR, Kelley KR, Mathews DL, et al. Postoperative follow-up: is a phone call enough? J Pediatr Surg 2008;43:83–6. 10.1016/j.jpedsurg.2007.09.025 [DOI] [PubMed] [Google Scholar]
- 12. Willard A, Brown E, Masten M, et al. Complex surgical infants benefit from Postdischarge telemedicine visits. Adv Neonatal Care 2018;18:22–30. 10.1097/ANC.0000000000000460 [DOI] [PubMed] [Google Scholar]
- 13. DeAntonio JH, Kang HS, Cockrell HC, et al. Utilization of a handheld telemedicine device in postoperative pediatric surgical care. J Pediatr Surg 2019;54:1005–8. 10.1016/j.jpedsurg.2019.01.032 [DOI] [PubMed] [Google Scholar]
- 14. Mehrotra A, Jena AB, Busch AB, et al. Utilization of telemedicine among rural Medicare beneficiaries. JAMA 2016;315:2015–6. 10.1001/jama.2016.2186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barnett ML, Ray KN, Souza J, et al. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA 2018;320:2147–9. 10.1001/jama.2018.12354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Nakayama DK, Burd RS, Newman KD. Pediatric surgery workforce: supply and demand. J Pediatr Surg 2009;44:1677–82. 10.1016/j.jpedsurg.2009.03.036 [DOI] [PubMed] [Google Scholar]
- 17. Ricketts TC, Adamson WT, Fraher EP, et al. Future supply of pediatric surgeons: analytical study of the current and projected supply of pediatric surgeons in the context of a rapidly changing process for specialty and subspecialty training. Ann Surg 2017;265:609–15. 10.1097/SLA.0000000000001810 [DOI] [PubMed] [Google Scholar]
- 18. Kalfa D, Chai P, Bacha E. Surgical volume-to-outcome relationship and monitoring of technical performance in pediatric cardiac surgery. Pediatr Cardiol 2014;35:899–905. 10.1007/s00246-014-0938-y [DOI] [PubMed] [Google Scholar]
- 19. Drews JD, Cooper JN, Onwuka EA, et al. The relationships of surgeon volume and specialty with outcomes following pediatric thyroidectomy. J Pediatr Surg 2019;54:1226–32. 10.1016/j.jpedsurg.2019.02.033 [DOI] [PubMed] [Google Scholar]
- 20. Morche J, Mathes T, Jacobs A, et al. Relationship between volume and outcome for congenital diaphragmatic hernia: a systematic review protocol. Syst Rev 2018;7:185. 10.1186/s13643-018-0872-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res 2016;79:169–76. 10.1038/pr.2015.192 [DOI] [PubMed] [Google Scholar]
- 22. Bator EX, Gleason JM, Lorenzo AJ, et al. The burden of attending a pediatric surgical clinic and family preferences toward telemedicine. J Pediatr Surg 2015;50:1776–82. 10.1016/j.jpedsurg.2015.06.005 [DOI] [PubMed] [Google Scholar]
- 23. Tam A, Leung A, O'Callaghan C, et al. Role of telehealth in perioperative medicine for regional and rural patients in Queensland. Intern Med J 2017;47:933–7. 10.1111/imj.13484 [DOI] [PubMed] [Google Scholar]
- 24. Shivji S, Metcalfe P, Khan A, et al. Pediatric surgery telehealth: patient and clinician satisfaction. Pediatr Surg Int 2011;27:523–6. 10.1007/s00383-010-2823-y [DOI] [PubMed] [Google Scholar]
- 25. Philips R, Seim N, Matrka L, et al. Cost savings associated with an outpatient otolaryngology telemedicine clinic. Laryngoscope Investig Otolaryngol 2019;4:234–40. 10.1002/lio2.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Goedeke J, Ertl A, Zöller D, et al. Telemedicine for pediatric surgical outpatient follow-up: a prospective, randomized single-center trial. J Pediatr Surg 2019;54:200–7. 10.1016/j.jpedsurg.2018.10.014 [DOI] [PubMed] [Google Scholar]
- 27. Kummerow Broman K, Oyefule OO, Phillips SE, et al. Postoperative Care Using a Secure Online Patient Portal: Changing the (Inter)Face of General Surgery. J Am Coll Surg 2015;221:1057–66. 10.1016/j.jamcollsurg.2015.08.429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lesher AP, Shah SR. Telemedicine in the perioperative experience. Semin Pediatr Surg 2018;27:102–6. 10.1053/j.sempedsurg.2018.02.007 [DOI] [PubMed] [Google Scholar]
- 29. Brown NA. State Medicaid and private payer reimbursement for telemedicine: an overview. J Telemed Telecare 2006;12(Suppl 2):S32–9. 10.1258/135763306778393108 [DOI] [PubMed] [Google Scholar]
- 30. State telehealth laws and reimbursement policies. in: policy TCfCH, editor 2020. Available: https://www.cchpca.org/telehealth-policy/state-telehealth-laws-and-reimbursement-policies-report
- 31. Lacktman NA, J Levine S. 50-State survey of telehealth commercial payer statutes 2019.
- 32. Reeder BM, Lyne ED, Patel DR, et al. Referral patterns to a pediatric orthopedic clinic: implications for education and practice. Pediatrics 2004;113:e163–7. 10.1542/peds.113.3.e163 [DOI] [PubMed] [Google Scholar]
- 33. Davis A, Gilchrist V, Grumbach K, et al. Advancing the PRIMARY/SPECIALTY care interface through ECONSULTS and enhanced referrals. Ann Fam Med 2015;13:387–8. 10.1370/afm.1829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Chen AH, Murphy EJ, Yee HF. eReferral--a new model for integrated care. N Engl J Med 2013;368:2450–3. 10.1056/NEJMp1215594 [DOI] [PubMed] [Google Scholar]
- 35. Kuhn EN, Warmus BA, Davis MC, et al. Identification and cost of potentially avoidable transfers to a tertiary care neurosurgery service: a pilot study. Neurosurgery 2016;79:541–8. 10.1227/NEU.0000000000001378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bailes JE, Poole CC, Hutchison W, et al. Utilization and cost savings of a wide-area computer network for neurosurgical consultation. Telemed J 1997;3:135–9. 10.1089/tmj.1.1997.3.135 [DOI] [PubMed] [Google Scholar]
- 37. Hoseini F, Ayatollahi H, Salehi SH. Systematized review of telemedicine applications in treating burn patients. Med J Islam Repub Iran 2016;30:459. [PMC free article] [PubMed] [Google Scholar]
- 38. Kim PT, Falcone RA. The use of telemedicine in the care of the pediatric trauma patient. Semin Pediatr Surg 2017;26:47–53. 10.1053/j.sempedsurg.2017.01.008 [DOI] [PubMed] [Google Scholar]
- 39. Lapointe L, Lavallee-Bourget MH, Pichard-Jolicoeur A, et al. Impact of telemedicine on diagnosis, clinical management and outcomes in rural trauma patients: a rapid review. Can J Rural Med 2020;25:31–40. 10.4103/CJRM.CJRM_8_19 [DOI] [PubMed] [Google Scholar]
- 40. Di Sanzo M, Cipolloni L, Borro M, et al. Clinical applications of personalized medicine: a new paradigm and challenge. Curr Pharm Biotechnol 2017;18:194–203. 10.2174/1389201018666170224105600 [DOI] [PubMed] [Google Scholar]
- 41. Perrin AD M. Americans' Internet access: 2000-2015, 2015. The Pew research center. Available: https://www.pewresearch.org/internet/2015/06/26/americans-internet-access-2000-2015/ [Accessed 1 Dec 2020].
- 42. Hamilton EC, Saiyed F, Miller CC, et al. The digital divide in adoption and use of mobile health technology among caregivers of pediatric surgery patients. J Pediatr Surg 2018;53:1478–93. 10.1016/j.jpedsurg.2017.08.023 [DOI] [PubMed] [Google Scholar]
- 43. Morrow AM, Quine S, Loughlin EVO, et al. Different priorities: a comparison of parents' and health professionals' perceptions of quality of life in quadriplegic cerebral palsy. Arch Dis Child 2008;93:119–25. 10.1136/adc.2006.115055 [DOI] [PubMed] [Google Scholar]
- 44. John V, Chacko J, Mathai J, et al. Psychosocial aspects of follow-up of children operated for intermediate anorectal malformations. Pediatr Surg Int 2010;26:989–94. 10.1007/s00383-010-2647-9 [DOI] [PubMed] [Google Scholar]
- 45. Pilapil M, Coletti DJ, Rabey C, et al. Caring for the caregiver: supporting families of youth with special health care needs. Curr Probl Pediatr Adolesc Health Care 2017;47:190–9. 10.1016/j.cppeds.2017.07.003 [DOI] [PubMed] [Google Scholar]
- 46. Lim J, Davis A, Tang AR, et al. Caregiver stress in children with craniosynostosis: a systematic literature review. Childs Nerv Syst 2019;35:217–25. 10.1007/s00381-018-3959-7 [DOI] [PubMed] [Google Scholar]
- 47. Gerlach UA, Vrakas G, Holdaway L, et al. Skype clinics after intestinal transplantation - follow-up beyond post codes. Clin Transplant 2016;30:760–6. 10.1111/ctr.12745 [DOI] [PubMed] [Google Scholar]
- 48. Oum SW, A; Kates J. The U.S. response to coronavirus: summary of the coronavirus preparedness and response supplemental Appropriations act, 2020, 2020. Available: https://www.kff.org/coronavirus-covid-19/issue-brief/the-u-s-response-to-coronavirus-summary-of-the-coronavirus-preparedness-and-response-supplemental-appropriations-act-2020/ [Accessed 1 Dec 2020].
- 49. HHS . Notification of enforcement discretion for telehealth remote communications during the COVID-19 nationwide public health emergency, 2020. Available: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html [Accessed 1 Dec 2020].