Abstract
Background:
Cardiac rehabilitation (CR) is a multidisciplinary medical program. Most studies have emphasized the effect of exercise-based CR in lowering lipid levels; however, the effect of CR as a comprehensive program on lipid levels remains unclear.
Methods:
Electronic database were searched up to 2022. Randomized controlled trials with lipid profile indicators were included. Standardized mean differences (SMDs) and 95% CIs were used to evaluate the effect size. Begg’s funnel plot and Egger’s linear regression test were used to assess publication bias.
Results:
CR remarkably reduced low-density lipoprotein cholesterol (LDL-C) levels (SMD = –0.23; 95%CI: [–0.38, –0.08]; P < 0.001), triglyceride (TG) levels (SMD = –0.17; 95%CI: [–0.28, –0.06]; P < 0.001), and total cholesterol (TC) levels (SMD = –0.30; 95%CI: [–0.43, –0.16]; P < 0.001) and increased high-density lipoprotein cholesterol (HDL-C) levels (SMD = 0.19; 95%CI: [0.10, 0.29]; P < 0.001).
Conclusions:
CR reduce TC, TG, and LDL-C levels while improving HDL-C levels. CR should be promoted and more trials should be conducted for long-term CR.
Keywords: Coronary disease, coronary disease rehabilitation, lipid profile, randomized controlled trials
Introduction
Coronary heart disease (CHD) is a type of heart disease characterized by progressive coronary atherosclerotic lesions and the accumulation of fatty deposits along the inner layer of the coronary arteries, resulting in narrowing or blockage of coronary arteries and myocardial ischemia. CHD is a major component of cardiovascular disease and the leading cause of morbidity and mortality in the developed world [1,2]. Patients diagnosed with CHD are at increased risk of premature death, myocardial infarction, and readmission to hospital. CHD is an important public health concern and economic burden worldwide [3]. According to clinical guidelines, secondary prevention strategies are crucial after diagnosis because controlling risk factors is the key to recurrence management [4].
Cardiac rehabilitation (CR) is an integration of multiple coordinated, intentional interventions that could offer a comprehensive platform for the administration of secondary prevention measures, such as evidence-based pharmacotherapy, cardiac risk factor management, nutritional counselling, patient education, and physical activity training [5,6].
The proper control of risk factors, such as blood pressure and lipid levels, play an important role in decelerating disease progression and preventing recurrence and complications. Several meta-analyses have shown that exercise-based CR lowers blood lipid levels and blood pressure [7,8]. However, CR is an integrated and comprehensive program; therefore, we have updated and supplemented the data with the aim to measure the effect of multiple modalities of CR on lipids.
Methods
We performed this systematic review and meta-analysis of trials to investigate CR interventions for patients with coronary heart disease (CHD) according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement.
Literature search strategy
Relevant studies were identified through a systematic search of the following electronic databases: MEDLINE, PubMed, EMBASE (Ovid), Web of Science, Scopus, and Cochrane Central Register of Controlled Trials up to 2022. The following Medical Subject Headings (MeSH) terms: ‘cardiac rehabilitation’ or ‘lifestyle change’ or ‘exercise training’ or ‘prevention program’ and ‘CHD’ or ‘CAD’ or ‘AMI’ or ‘ACS’ and ‘lipid profile’ or ‘HDL-C’ or ‘LDL-C’ or ‘TC’ or ‘TG’ were applied in our search strategy. We manually reviewed relevant review articles, reference lists of published trials, and conference abstracts (American Society of Clinical Oncology [ASCO], Annual Meetings, and the European Cancer Conference [ECCO]) for potentially eligible studies.
Inclusion and exclusion criteria for study collection
Studies were included if they met the following criteria: 1) controlled trials of cardiac rehabilitation (life modification, exercise training, etc.) regardless of whether it included allocation concealment or blinding; 2) adult (age ≥ 18 years) patients with coronary artery diseases (CAD) or CHD; 3) intervention group involved patients undergoing cardiac rehabilitation and control group included patients undergoing usual care or medication; and 4) measurement indicators were lipid profiles such as LDL-C, HDL-C, TC, TG. Studies were excluded if they conformed to the following criteria: 1) articles were not in English; 2) studies with a control group of home-based or community-based cardiac rehabilitation; and 3) studies with insufficient information or data. Two investigators independently checked whether each study met the inclusion criteria, and discrepancies were resolved by a third reviewer.
Data extraction
Two researchers independently extracted basic information from the included studies (title, first author, publication year, author information, and document source) and characteristics of study patients (sex, age, country, sample size, and interventions) for both the experimental and control groups and obtained outcome measurements. Any inconsistencies were resolved through consensus.
Quality assessment
Study quality was assessed using the Newcastle-Ottawa Scale (NOS). The total scores ranged from 0 to 9 points; trials considered ‘high quality’ scored higher than six. Two reviewers assessed the quality of the studies separately, and discrepancies were assessed by a third researcher.
Statistical analysis
Statistical analyses were performed using Stata statistical software (version 13.0; Stata Corp., College Station, TX, USA). SMD and 95% CIs were used to evaluate the effect size. The Q test and I2 analysis, with a significance level of <0.1 were employed to assess the heterogeneity between studies. Meta-regression analysis was used to analyze the source of heterogeneity. Begg’s funnel plot and Egger’s linear regression test were used to investigate the possibility of publication bias. Differences were considered statistically significant at P < 0.05.
Results
Literature selection
In total, 3,624 potentially relevant articles were identified through an online search. After careful examination of titles and abstracts, 3,397 were excluded; 1,565 publications were excluded as review articles and other ineligible types of references, 114 were non-English language articles, 227 included experiments on non-human species, 301 articles were duplicates, and 667 had non-targeted endpoints (Figure 1). The remaining 227 articles were retrieved for more detailed assessment. After screening the full text, 162 studies were further excluded because of incomplete data (n = 50), non-target interventions (n = 78), data that could not be extracted directly (n = 33), not including non-CHD patients (n = 6), unsuitable control groups (n = 6), and incomplete data (n = 3). Ultimately, 51 studies were included in the meta-analysis [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59].
Figure 1.

Diagram of including studies selection procedures.
Characteristics of included studies
Fifty-one eligible studies with 10,286 patients were included, all of which were published between 1979 and 2022. The sample sizes ranged from 15 to 903 patients (median = 63). The age of all included patients ranged from 51 to 77.3 years old (median = 58.6); three studies had a three-arm parallel design, while forty-eight studies had a two-arm parallel design (CR and comparison). In Wosornu et al.’s [15] study, participants were assigned to three groups (control group, aerobic group, and strength group), which included people in CR, case-managed, and community-based groups. In a study by Volaklis et al., patients were grouped into land exercise, water exercise, and control. Nine studies were performed in the USA, five in the UK, six in Australia, four in Canada, three in Norway, three in HK, four in Sweden, two in Germany, two in Italy, two in Greece, fifteen studies from other countries. Forty-five studies collected TC measurements. Thirty-seven studies provided information on HDL-C as an endpoint, and forty-three studies used.
LDL-C as the endpoint. Thirty-eight studies used TG levels as the endpoint (Table 1).
Table 1.
Characteristics of Including Studies.
|
| ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| AUTHOR | COUNTRY | TYPE OF DISEASE | NO. OF PATIENT | AGE MEAN (SD) | GENDER(M/F) | INTERVENTION | NOS SCALE | |||
|
|
|
|
||||||||
| T | C | T | C | T | C | |||||
|
| ||||||||||
| Kallio 1979 |
Finland | AMI | 183 | 187 | 54.4 | 54.1 | 151/37 | 150/37 | Health education Exercise training |
6 |
|
| ||||||||||
| Ornish 1990 |
USA | CAD | 22 | 19 | 56.1(7.5) | 59.8(9.1) | 21/1 | 15/4 | Lifestyle modification | 8 |
|
| ||||||||||
| Schuler 1992 |
Germany | CAD | 56 | 57 | 52.8(5.8) | 54.2(7.7) | NA | NA | Lifestyle modification Exercise training |
8 |
|
| ||||||||||
| Debusk 1994 |
USA | AMI | 293 | 292 | 57(8) | 57(8) | 230/63 | 231/61 | Lifestyle modification Exercise training |
7 |
|
| ||||||||||
| Fletcher 1994 |
USA | CAD | 16 | 19 | 62(8) | 63(7) | 16/0 | 19/0 | Exercise training | 6 |
|
| ||||||||||
| Haskwell 1994 |
USA | CAD | 119 | 127 | 58.3(9.2) | 56.2(8.2) | 99/20 | 117/10 | Lifestyle modification | 7 |
|
| ||||||||||
| Wosornua 1996 |
UK | CAD | 27 | 27 | 56.5(8.9) | 56.6(7.0) | 27/0 | 27/0 | Aerobic exercise training | 8 |
|
| ||||||||||
| Wosornub 1996 |
UK | CAD | 27 | 27 | 59.2(6.4) | 56.6(7.0) | 27/0 | 27/0 | Strength exercise training |
8 |
|
| ||||||||||
| Gallacher 1997 |
UK | CAD | 198 | 209 | NA | NA | NA | NA | Education (Stress management) |
8 |
|
| ||||||||||
| Niebauer 1997 |
UK | CAD | 56 | 57 | NA | NA | 56/0 | 57/0 | Lifestyle modification Exercise training |
9 |
|
| ||||||||||
| Ornish 1998 |
USA | ACS | 20 | 15 | 57.4(6.4) | 61.8(7.5) | 20/0 | 12/3 | Lifestyle modification | 9 |
|
| ||||||||||
| Carlssona 1998 |
Sweden | CAD | 75 | 67 | 62.2(5.8) | 61.7(6.0) | 58/17 | 51/16 | Lifestyle modification Exercise training |
8 |
|
| ||||||||||
| Carlssonb 1998 |
Sweden | CAD | 31 | 32 | 62.7(4.8) | 59.8(4.8) | 26/5 | 27/5 | Lifestyle modification Exercise training |
8 |
|
| ||||||||||
| Bang 1999 |
Sweden | CAD | 46 | 41 | 53(7) | 53(7) | 37/9 | 36/5 | Lifestyle modification | 8 |
|
| ||||||||||
| Toobert 2000 |
USA | CHD | 14 | 10 | 64(10) | 63(11) | NA | NA | Lifestyle modification | 8 |
|
| ||||||||||
| Belardinelli 2001 |
Italy and USA | CAD | 59 | 59 | 53(11) | 59(10) | 49/10 | 50/9 | Exercise training | 8 |
|
| ||||||||||
| Gordon a 2002 |
USA | CAD | 45 | 52 | 60(9) | 61(10) | 34/11 | 38/14 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Gordon b 2002 |
USA | CAD | 45 | 45 | 60(9) | 60(9) | 34/11 | 35/10 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Vale 2002 |
Australia | CAD | 107 | 112 | 61.5(10.3) | 60.6(9.5) | 80/27 | 84/28 | Education Exercise training |
7 |
|
| ||||||||||
| Yu 2003 |
HK | CHD | 72 | 40 | 62.3(11.2) | 61.2(10.2) | 59/13 | 30/10 | Exercise training | 6 |
|
| ||||||||||
| The Vestfold Heartcare Study Group 2003 | Norway | CHD | 98 | 99 | 54(8) | 55(8) | 79/19 | 83/16 | Lifestyle modification | 8 |
|
| ||||||||||
| Lear 2003 |
Canada | CAD | 151 | 151 | 64.8(8.8) | 63.4(10.2) | 125/26 | 124/27 | Lifestyle modification | 8 |
|
| ||||||||||
| Vale 2003 |
Australia | CHD | 398 | 394 | 58.6(10.6) | 58.3(10.3) | 313/85 | 297/97 | Education Exercise training |
7 |
|
| ||||||||||
| Vona 2004 |
Italy | AMI | 28 | 24 | 56(6) | 57(8) | 21/7 | 19/5 | Exercise training | 7 |
|
| ||||||||||
| Volaklisa 2007 |
Greece | CAD; MI | 12 | 10 | 53(4) | 51(3) | NA | NA | Exercise training | 7 |
|
| ||||||||||
| Volaklisb 2007 |
Greece | CAD; MI | 12 | 10 | 58 (3) | 51(3) | NA | NA | Exercise training | 7 |
|
| ||||||||||
| Zutz 2007 |
Canada | CAD | 8 | 7 | 58(4) | 59(12) | 7/1 | 5/2 | Lifestyle modification | 7 |
|
| ||||||||||
| Naser 2008 |
Iran | CHD | 50 | 50 | 54.8 | 53.2 | 45/5 | 39/11 | Lifestyle modification | 7 |
|
| ||||||||||
| Seki 2008 |
Japan | CHD; ACS; MI | 14 | 10 | 64(10) | 63(11) | NA | NA | Exercise training | 7 |
|
| ||||||||||
| Balen 2008 |
Croatia | AMI | 30 | 30 | 59 (9) | 61 (10) | 21/9 | 23/7 | Exercise training | 7 |
|
| ||||||||||
| Murphy 2009 |
Ireland | MI | 444 | 459 | 68.5(9.3) | 66.5(9.9) | 311/133 | 320/139 | Lifestyle modification Education |
7 |
|
| ||||||||||
| Zetta 2011 |
UK | CAD | 109 | 109 | 65.9(10.0) | 64.8(10) | 71/38 | 78/31 | Lifestyle modification Education |
7 |
|
| ||||||||||
| Munk 2011 |
Norway | CAD | 18 | 18 | 59.5(10) | 60.7(9) | 16/2 | 14/4 | Exercise training | 7 |
|
| ||||||||||
| Moholdt 2012 |
Norway | MI | 59 | 30 | 57.5(9.3) | 56.7(10.4) | 49/10 | 25/5 | Exercise training | 7 |
|
| ||||||||||
| Oerkild 2012 |
Denmark | MI | 19 | 21 | 77.3(6.0) | 76.5(7.7) | 12/7 | 11/10 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Vernooij 2012 |
Netherland | CAD | 164 | 166 | 60.7(7.8) | 59.2(8.9) | 128/36 | 118/48 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Luk 2012 |
HK | CAD | 32 | 32 | 67.7(9.0) | 66.6(7.9) | 24/8 | 24/8 | Exercise training | 7 |
|
| ||||||||||
| Lear 2014 |
Canada | CVD | 38 | 40 | 59.2(10.7) | 58.6(9) | 34/4 | 32/8 | Lifestyle modification Exercise training Education by internet |
8 |
|
| ||||||||||
| Raghuram 2014 |
India | CAD | 129 | 121 | 53.3(6.4) | 52.6(6.9) | NA | NA | Yoga training | 8 |
|
| ||||||||||
| Chow 2015 |
Australia | CHD | 352 | 358 | 57.9(9.1) | 57.3(9.3) | 287/65 | 295/63 | Lifestyle modification | 7 |
|
| ||||||||||
| Hassan 2016 |
Egypt | CAD | 30 | 30 | NA | NA | 21/9 | 20/10 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Johnston 2016 |
Sweden | MI | 86 | 80 | 56.8(8.0) | 58.4(8.6) | 71/15 | 63/17 | Lifestyle modification Education |
7 |
|
| ||||||||||
| Tamburús 2016 |
Brazil | CAD | 15 | 17 | NA | NA | NA | NA | Exercise training | 8 |
|
| ||||||||||
| Lin 2017 |
HK | CAD | 144 | 144 | 75.3(7.5) | 74.3(7.5) | 94/50 | 97/47 | Education | 7 |
|
| ||||||||||
| Park 2017 |
South Korea | AMI | 32 | 32 | 57(12) | 55(10) | 29/3 | 27/5 | Education | 7 |
|
| ||||||||||
| Dorje 2019 |
Australia | MI; unstable or stable angina | 156 | 156 | 59.1(9.4) | 61.9(8.7) | 128/28 | 126/30 | Lifestyle modification Education by Wechat |
8 |
|
| ||||||||||
| Maddison 2019 |
Australia; New Zealand | CHD | 82 | 80 | 61(13.2) | 61.5(12.2) | 69/13 | 70/10 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Santo 2019 |
Australia | CHD | 107 | 56 | 58.4(9.0) | 56.8 (8.6) |
93/14 | 50/6 | Education | 7 |
|
| ||||||||||
| Wienbergen 2019 |
Germany | MI | 143 | 138 | 56.5(9.1) | 56.4 (10.3) |
117/36 | 112/26 | Education telephone visits and telemetric risk factor control |
8 |
|
| ||||||||||
| Chaves 2019 |
Canada | MI | 12 | 11 | 60.7(13.3) | 60.6 (8.4) |
12/0 | 4/7 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Zheng 2019 |
China | AMI | 411 | 411 | 56.2(9.3) | 56.6 (9.7) | 353/58 | 353/58 | Lifestyle modification Education by text messages |
8 |
|
| ||||||||||
| Campo 2020 |
Italy | ACS | 118 | 117 | 76(6) | 76.6 (5.2) | 92/26 | 89/28 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Uddin 2020 |
USA | CHD | 71 | 71 | 54(6) | 55(6) | 66/5 | 63/8 | Lifestyle modification Education |
8 |
|
| ||||||||||
| Yudi 2021 |
Australia | ACS | 83 | 85 | 56.8(9.9) | 56.2 (10.2) |
71/12 | 69/16 | Lifestyle modification Education by smartphone |
7 |
|
| ||||||||||
| Dalli Peydro 2022 |
Spain | ACS | 31 | 28 | 57.5(9.0) | 54.7(9.9) | 27/4 | 27/1 | Lifestyle modification Education by smartphone |
7 |
|
| ||||||||||
ACS: acute coronary syndrome; AMI: acute myocardial infarction; CAD: coronary atherosclerotic heart disease; CHD: coronary heart disease; CVD: coronary vascular disease; MI: myocardial infarction; NA: not available; NOS: Newcastle–Ottawa Scale.
Meta-analysis results
TC levels
Forty-four out of 51 studies included in our analysis reported on TC levels after CR. The forest plot showed that ten studies had significantly lower TC serum levels in the intervention group. The results of the studies reported that CR could significantly reduce TC serum levels compared with control groups (SMD = –0.30; 95%CI: [–0.43, –0.16]; P < 0.001, Figure 2).
Figure 2.
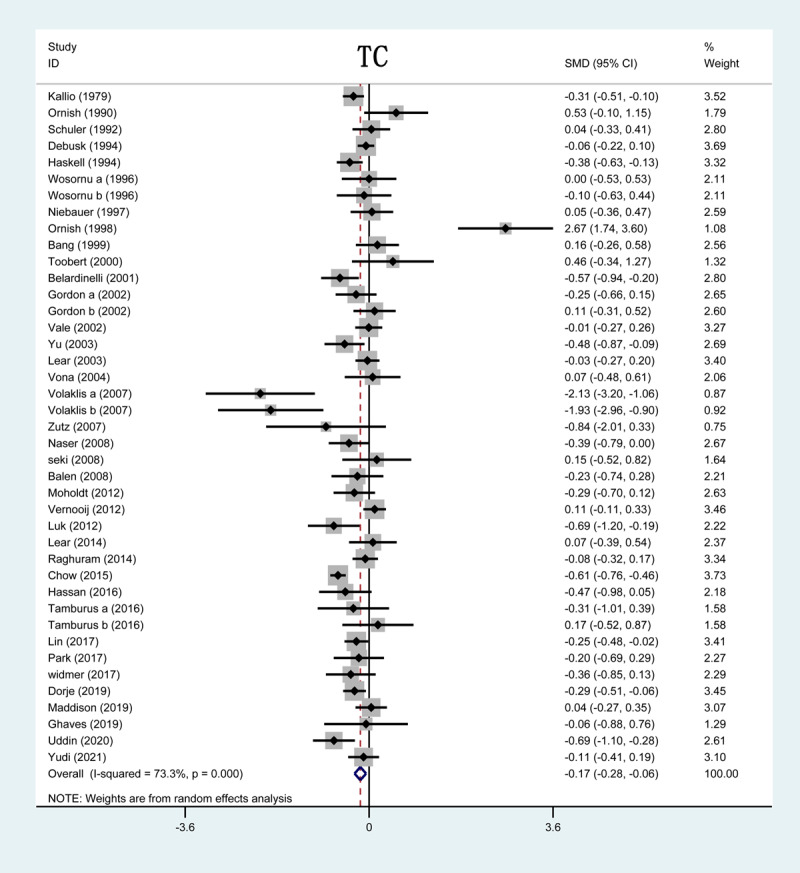
Forrest plot of TC levels after CR treatment. TC: total cholesterol; CR: cardiac rehabilitation; SMD: standardized mean difference.
HDL-C levels
Thirty-seven out of 51 studies included in this analysis reported on HDL-C levels after CR. The forest plot showed that the HDL-C serum levels in three studies were significantly higher in the CR group than in the control group. The results of the overall study revealed HDL-C serum levels were remarkably increased after CR (SMD = 0.19; 95%CI: [0.10, 0.29]; P < 0.001, Figure 3).
Figure 3.

Forrest plot of HDL-C levels after CR treatment. HDL-C: high-density lipoprotein cholesterol; SMD: standardized mean difference.
LDL-C levels
Out of 51 studies, 42 included in this analysis reported on LDL-C levels after CR. The forest plot showed that the serum LDL-C levels in three studies were significantly lower in the CR group than in the control group. The results of the overall study revealed that compared with control group, LDL-C serum levels were reduced after CR (SMD = –0.23; 95%CI: [–0.38, –0.08]; P < 0.001, Figure 4).
Figure 4.
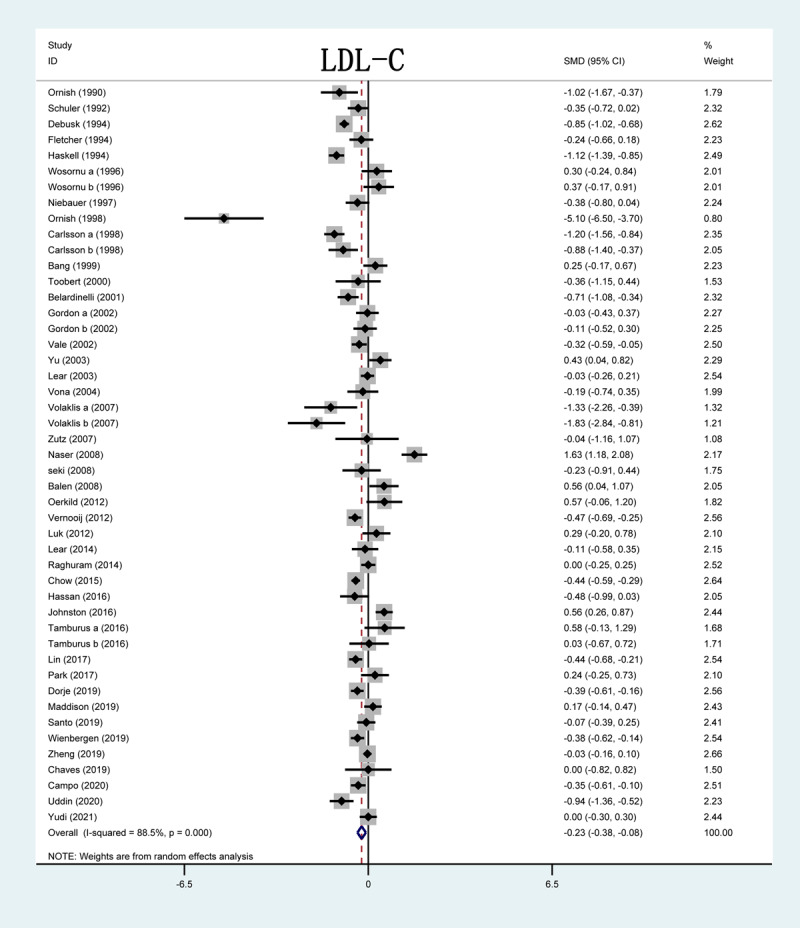
Forrest plot of LDL-C levels after CR treatment. LDL-C: low-density lipoprotein cholesterol; SMD: standardized mean difference.
TG levels
Out of 51 studies, 37 included in this analysis reported on TG levels after CR. The forest plot showed that TG serum levels in 10 studies were significantly lower in the CR group than in the control group. In the results of the overall study, significant decrease in serum TG levels were observed after CR (SMD = –0.17; 95%CI: [–0.28, –0.06]; P < 0.001, Figure 5).
Figure 5.
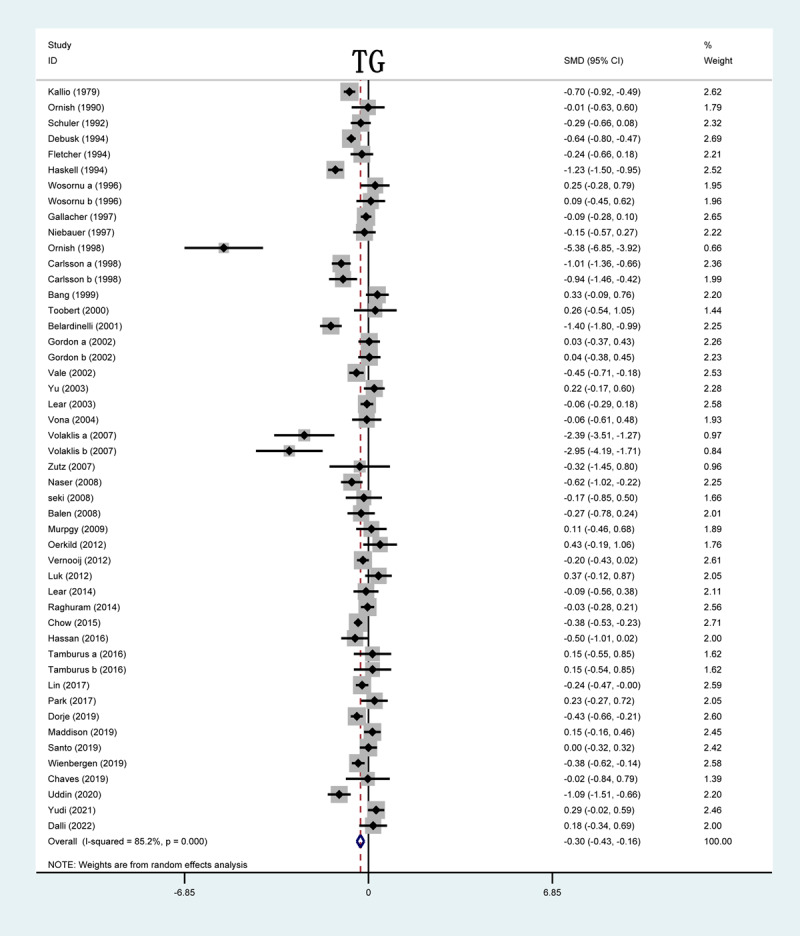
Forrest plot of TG levels after CR treatment. TG: triglyceride; SMD: standardized mean difference.
Apolipoprotein A
Five out of 51 studies included in this analysis and reported on apolipoprotein A (ApoA) levels after CR. The forest plot of ApoA serum levels showed no significant differences between the CR and control groups (SMD = –0.46; 95%CI: [–1.22, 0.30]; P = 0.24, Figure S1).
Apolipoprotein B
Five out of 51 studies included in this analysis and reported on apolipoprotein B (ApoB) levels after CR. The forest plot of ApoB serum levels showed no significant differences between the CR and control groups (SMD = –0.94; 95%CI: [–2.01, 0.13]; P = 0.09, Figure S2).
Subgroup analysis
The subgroup analysis was performed based on the following factors: publication year, sample size (<100 or ≥100), region, number of interventions, and study quality (score <7 or score ≥7).
Subgroup analysis according to publication year
We executed a subgroup analysis based on publication year, and included studies were divided into three subgroups: before 2000, 2000–2010 and after 2010. CR could obviously increase HDL-C level in all three subgroups. However, CR significantly decreased LDL-C level in subgroups of before 2000 (SMD: –0.75; 95%CI: –1.12, –0.38) and after 2010 (SMD: –0.13; 95%CI: –0.38, –0.08). Remarkably reduced TC level in subgroups of before 2000 (SMD: –0.52; 95%CI: –0.81, –0.22) and 2000–2010 (SMD: –0.40; 95%CI: –0.70, –0.10) and lower TG level in subgroups of 2000–2010 (SMD: –0.29; 95%CI: –0.51, –0.06) and after 2010 (SMD: –0.23; 95%CI: –0.39, –0.08) were observed when compared with control group (Table S3–S6).
Subgroup analysis according to sample size
Stratified group analysis was conducted based on the sample size and the studies were divided into two subgroups: those with number of patients less than 100 (<100) and greater than or equal to 100 (≥100). Results showed that in subgroup of sample size <100, LDL-C level was significantly decreased after CR (SMD: –0.32; 95%CI: –0.59, –0.04). In subgroup of sample size ≥100, TC (SMD: –0.39; 95%CI: –0.55, –0.24) and TG (SMD: –0.22; 95%CI: –0.34, –0.10) levels were considerably reduced after CR (Table S4–S6).
Subgroup analysis according to the number of interventions
We also carried out the subgroup analysis in terms of number of interventions. Studies were divided into three subgroups: those with one type, two types and three types interventions. We found that HDL-C level was significantly improved in subgroup of one type intervention (SMD: 0.25; 95%CI: 0.11, 0.39) and two types interventions (SMD: 0.10; 95%CI: 0.02, 0.18) subgroup. LDL-C level was decreased in subgroup of two types interventions (SMD: –0.30; 95%CI: –0.49, –0.12). TC level was reduced in subgroup of one type (SMD: –0.32; 95%CI: –0.54, –0.11) and two types interventions (SMD: –0.30; 95%CI: –0.48, –0.13). TG levels were reduced in subgroup of one type (SMD: –0.20; 95%CI: –0.38, –0.02) and two types interventions (SMD: –0.12; 95%CI: –0.23, –0.01) (Table S3–S6).
Subgroup analysis according to different regions
Subgroup analysis was performed in accordance with studies conducted in different regions. Based on the region, the studies were divided into six subgroups including US and Canada, Europe, Asia-Pacific, country combination, Africa, and South America subgroups. Based on the pooled results, we found that in US and Canada subgroup, LDL-C (SMD: –0.60; 95%CI: –0.95, –0.26) and TC (SMD: –0.49; 95%CI: –0.85, –0.14) levels were significantly reduced. In Europe subgroup, HDL-C (SMD: 0.17; 95%CI: 0.06, 0.28) was significantly improved, TC (SMD: –0.49; 95%CI: –0.85, –0.14) was reduced. In Asia-Pacific subgroup, HDL-C was increased (SMD: 0.24; 95%CI: 0.02, 0.45) and, TG level was reduced (SMD: –0.25; 95%CI: –0.41, –0.09). In combination subgroup, HDL-C was enhanced (SMD: 0.39; 95%CI: 0.03, 0.76) and, LDL-C (SMD: –0.71; 95%CI: –1.08, –0.34), TC (SMD: –1.4; 95%CI: –1.8, –0.99) and TG (SMD: –0.57; 95%CI: –0.94, –0.20) levels were all reduced. In Africa and South America subgroup, CR had insignificant effect on outcomes (Table S3–S6). As for ApoA and ApoB, we found insignificant differences between CR group and control group. We also did not find any potential sources of heterogeneity in this analysis (Table S1–S6).
Publication bias
According to the results of Egger’s test and Begg’s funnel plots, there was no publication bias seen among TG, TC, HDL-C, LDL-C, ApoA, and ApoB. The details are presented in Table S7 and Figure S3.
Discussion
This study highlights the effect of CR on lipid levels in patients with CHD. According to our results, CR can significantly reduce serum LDL-C, TC, and TG levels and increase serum HDL-C levels. The ApoA and ApoB levels did not change significantly.
The conclusion of our study is not in accordance with that of previous studies. In Chen’s study, LDL-C and HDL-C levels were improved after aerobic exercise, but TG and TC serum levels did not substantially change [8]. They collected four articles to conduct their analysis, though we have assembled 51 studies in our systematic review. The reason for the varied results may be the small number of articles on lipid analysis included in their studies. Similarly inconsistent with our conclusion, a meta-analysis by Javaherian et al. indicated that CR considerably reduced serum LDL-C, TC, and TG levels; however, no marked change was observed in HDL-C serum levels. They evaluated exercise-based CR and focused on all types of CR, including exercise, education, lifestyle modification, and so on. First, their CR range was more comprehensive. Second, our number of included articles was higher than that in their study. Third, they selected patients with cardiovascular disease (CVD) for analysis, while we restricted our review to patients with CHD. Few studies have focused on ApoA and ApoB; thus, the data were not sufficient.
In the subgroup analysis, we found that in one type and two types interventions subgroup, HDL-C levels were enhanced; LDL-C and TC levels were reduced. However, all endpoints found no significant differences in three types interventions subgroup; this might be due to inclusion of inadequate number of studies, (For each endpoint, only one study was included in three types interventions group). In subgroup of before 2000, LDL-C and TC levels were decreased. In subgroup of after 2010, LDL-C and TG levels were reduced. HDL-C was increased in all three subgroups according to the publication years. TC and TG levels were reduced in subgroup of sample size ≥100; LDL-C level was decreased after CR in studies with sample size<100. HDL-C, LDL-C, TG, and TC levels in group with study quality score higher than seven were obviously affected in positive way after CR. In terms of region, there were no magnificent differences observed in studies conducted in Africa and South America region after CR. Nevertheless, in other three regions, CR had remarkable effects on HDL-C, LDL-C, TC and TG. This difference might have been caused firstly by the inclusion of inadequate number of studies in Africa and South America region. Secondly, medical skills, types of insurance for commercially insured patients with different socioeconomic status and medication adherence were in different regions (Table S1-S6).
This study focused on comprehensively investigating the effects of CR on lipid profiles. In this study, CR was widely defined and not limited to specific types, such as exercise training. Moreover, all the trials included in this study were randomized controlled trials. Another strength of our study is the number of trials we were able to include in this review. Fifty-one articles provide a sufficient amount of trials for review. Consequently, our conclusions are hypothesized to be more reliable because of the larger number and higher quality of studies that we were able to incorporate in our systematic review.
Limitations
Our analysis has some limitations. First, although the subgroup analysis was performed using a fixed model, the source of heterogeneity was still not observed. Second, in over 50 studies, most patients were male, and due to a lack of data assessing CR effect by sex, a subgroup analysis of sex was not performed. Third, we included articles only in English, and all other non-English and written literatures were excluded. Considering these limitations, the results should be interpreted with caution.
Conclusion
In conclusion, this study illustrates that CR can reduce the levels of TC, TG, and LDL-C and improve levels of HDL-C. However, ApoA and ApoB levels did not change significantly after CR. Considering the efficacy of CR on improving blood lipid levels, which plays an important role in delaying disease progression and preventing recurrence and complications, CR should be widely promoted, and more clinical trials should be conducted regarding the long-term effects of CR.
Data Accessibility Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Additional Files
The additional files for this article can be found as follows:
Figures S1 to S3.
Tables S1 to S7.
Acknowledgements
We would like to thank Editage (www.editage.cn) for English language editing.
Funding Statement
This research was supported by Research Program of Health Commission of Anhui Province. Grant Number: AHWJ2021b095.
Funding information
This research was supported by Research Program of Health Commission of Anhui.
Province. Grant Number: AHWJ2021b095.
Competing Interests
The authors have no competing interests to declare.
Authors contributions
ZS contributed to conception and design of the research. GW contributed to data collection, and data analysis. YH contributed to data analysis. KD contributed to manuscript writing. XL and JL contributed to revising the manuscript critically for important intellectual content. All authors have read and approved the manuscript.
References
- 1.Roth GA, Huffman MD, Moran AE, et al. Global and regional patterns in cardiovascular mortality from 1990 to 2013. Circulation. 2015; 132(17): 1667–78. DOI: 10.1161/CIRCULATIONAHA.114.008720 [DOI] [PubMed] [Google Scholar]
- 2.Sekikawa A, Doyle MF, Kuller LH. Recent findings of long-chain n-3 polyunsaturated fatty acids (LCn-3 PUFAs) on atherosclerosis and coronary heart disease (CHD) contrasting studies in Western countries to Japan. Trends in Cardiovascular Medicine. 2015; 25(8): 717–23. DOI: 10.1016/j.tcm.2015.03.001 [DOI] [PubMed] [Google Scholar]
- 3.Smith SC, Jr., Benjamin EJ, Bonow RO, et al. AHA/ACCF Secondary Prevention and Risk Reduction Therapy for Patients with Coronary and other Atherosclerotic Vascular Disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124(22): 2458–73. DOI: 10.1161/CIR.0b013e318235eb4d [DOI] [PubMed] [Google Scholar]
- 4.Zhao M, Graham I, Cooney MT, et al. Determinants of coronary artery disease risk factor management across three world regions. Heart Asia. 2019; 11(1): e011112. DOI: 10.1136/heartasia-2018-011112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Li J, Li Y, Gong F, et al. Effect of cardiac rehabilitation training on patients with coronary heart disease: a systematic review and meta-analysis. Annals of Palliative Medicine. 2021; 10(11): 11901–9. DOI: 10.21037/apm-21-3136 [DOI] [PubMed] [Google Scholar]
- 6.Buckley JP, Furze G, Doherty P, et al. BACPR scientific statement: British standards and core components for cardiovascular disease prevention and rehabilitation. Heart (British Cardiac Society). 2013; 99(15): 1069–71. DOI: 10.1136/heartjnl-2012-303460 [DOI] [PubMed] [Google Scholar]
- 7.Javaherian M, Dabbaghipour N, Mohammadpour Z, Attarbashi Moghadam B. The role of the characteristics of exercise-based cardiac rehabilitation program in the improvement of lipid profile level: A systematic review and meta-analysis. ARYA Atherosclerosis. 2020; 16(4): 192–207. DOI: 10.22122/arya.v16i4.2123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen YC, Tsai JC, Liou YM, Chan P. Effectiveness of endurance exercise training in patients with coronary artery disease: A meta-analysis of randomised controlled trials. European journal of cardiovascular nursing: journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology. 2017; 16(5): 397–408. DOI: 10.1177/1474515116684407 [DOI] [PubMed] [Google Scholar]
- 9.Kallio V, Hämäläinen H, Hakkila J, Luurila OJ. Reduction in sudden deaths by a multifactorial intervention programme after acute myocardial infarction. Lancet (London, England). 1979; 2(8152): 1091–4. DOI: 10.1016/S0140-6736(79)92502-9 [DOI] [PubMed] [Google Scholar]
- 10.Ornish D, Brown SE, Scherwitz LW, et al. Can lifestyle changes reverse coronary heart disease? The Lifestyle Heart Trial. Lancet (London, England). 1990; 336(8708): 129–33. DOI: 10.1016/0140-6736(90)91656-U [DOI] [PubMed] [Google Scholar]
- 11.Schuler G, Hambrecht R, Schlierf G, et al. Regular physical exercise and low-fat diet. Effects on progression of coronary artery disease. Circulation. 1992; 86(1): 1–11. DOI: 10.1161/01.CIR.86.1.1 [DOI] [PubMed] [Google Scholar]
- 12.DeBusk RF, Miller NH, Superko HR, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Annals of Internal Medicine. 1994; 120(9): 721–9. DOI: 10.7326/0003-4819-120-9-199405010-00001 [DOI] [PubMed] [Google Scholar]
- 13.Fletcher BJ, Dunbar SB, Felner JM, et al. Exercise testing and training in physically disabled men with clinical evidence of coronary artery disease. The American Journal of Cardiology. 1994; 73(2): 170–4. DOI: 10.1016/0002-9149(94)90209-7 [DOI] [PubMed] [Google Scholar]
- 14.Haskell WL, Alderman EL, Fair JM, et al. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease. The Stanford Coronary Risk Intervention Project (SCRIP). Circulation. 1994; 89(3): 975–90. DOI: 10.1161/01.CIR.89.3.975 [DOI] [PubMed] [Google Scholar]
- 15.Wosornu D, Bedford D, Ballantyne D. A comparison of the effects of strength and aerobic exercise training on exercise capacity and lipids after coronary artery bypass surgery. European Heart Journal. 1996; 17(6): 854–63. DOI: 10.1093/oxfordjournals.eurheartj.a014966 [DOI] [PubMed] [Google Scholar]
- 16.Gallacher JEJ, Hopkinson CA, Bennett P, Burr ML, Elwood PC. Effect of stress management on angina. Psychology & Health. 1997; 12(4): 523–32. DOI: 10.1080/08870449708406728 [DOI] [Google Scholar]
- 17.Niebauer J, Hambrecht R, Velich T, et al. Attenuated progression of coronary artery disease after 6 years of multifactorial risk intervention: role of physical exercise. Circulation. 1997; 96(8): 2534–41. DOI: 10.1161/01.CIR.96.8.2534 [DOI] [PubMed] [Google Scholar]
- 18.Carlsson R. Serum cholesterol, lifestyle, working capacity and quality of life in patients with coronary artery disease. Experiences from a hospital-based secondary prevention programme. Scandinavian Cardiovascular Journal Supplement. 1998; 50: 1–20. DOI: 10.1080/140174398427956-1 [DOI] [PubMed] [Google Scholar]
- 19.Ornish D, Scherwitz LW, Billings JH, et al. Intensive lifestyle changes for reversal of coronary heart disease. Jama. 1998; 280(23): 2001–7. DOI: 10.1001/jama.280.23.2001 [DOI] [PubMed] [Google Scholar]
- 20.Hofman-Bang C, Lisspers J, Nordlander R, et al. Two-year results of a controlled study of residential rehabilitation for patients treated with percutaneous transluminal coronary angioplasty. A randomized study of a multifactorial programme. European Heart Journal. 1999; 20(20): 1465–74. DOI: 10.1053/euhj.1999.1544 [DOI] [PubMed] [Google Scholar]
- 21.Toobert DJ, Glasgow RE, Radcliffe JL. Physiologic and related behavioral outcomes from the Women’s Lifestyle Heart Trial. Annals of behavioral medicine: a publication of the Society of Behavioral Medicine. 2000; 22(1): 1–9. DOI: 10.1007/BF02895162 [DOI] [PubMed] [Google Scholar]
- 22.Belardinelli R, Paolini I, Cianci G, et al. Exercise training intervention after coronary angioplasty: the ETICA trial. Journal of the American College of Cardiology. 2001; 37(7): 1891–900. DOI: 10.1016/S0735-1097(01)01236-0 [DOI] [PubMed] [Google Scholar]
- 23.Gordon NF, English CD, Contractor AS, et al. Effectiveness of three models for comprehensive cardiovascular disease risk reduction. The American Journal of Cardiology. 2002; 89(11): 1263–8. DOI: 10.1016/S0002-9149(02)02323-8 [DOI] [PubMed] [Google Scholar]
- 24.Vale MJ, Jelinek MV, Best JD, Santamaria JD. Coaching patients with coronary heart disease to achieve the target cholesterol: a method to bridge the gap between evidence-based medicine and the ‘real world’--randomized controlled trial. Journal of Clinical Epidemiology. 2002; 55(3): 245–52. DOI: 10.1016/S0895-4356(01)00460-7 [DOI] [PubMed] [Google Scholar]
- 25.The Vestfold Heartcare Study Group. Influence on lifestyle measures and five-year coronary risk by a comprehensive lifestyle intervention programme in patients with coronary heart disease. European Journal of Cardiovascular Prevention and Rehabilitation: Official Journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2003; 10(6): 429–37. DOI: 10.1097/01.hjr.0000107024.38316.6a [DOI] [PubMed] [Google Scholar]
- 26.Lear SA, Ignaszewski A, Linden W, et al. The Extensive Lifestyle Management Intervention (ELMI) following cardiac rehabilitation trial. European Heart Journal. 2003; 24(21): 1920–7. DOI: 10.1016/j.ehj.2003.08.015 [DOI] [PubMed] [Google Scholar]
- 27.Vale MJ, Jelinek MV, Best JD, et al. Coaching patients On Achieving Cardiovascular Health (COACH): a multicenter randomized trial in patients with coronary heart disease. Archives of Internal Medicine. 2003; 163(22): 2775–83. DOI: 10.1001/archinte.163.22.2775 [DOI] [PubMed] [Google Scholar]
- 28.Yu CM, Li LS, Ho HH, Lau CP. Long-term changes in exercise capacity, quality of life, body anthropometry, and lipid profiles after a cardiac rehabilitation program in obese patients with coronary heart disease. The American Journal of Cardiology. 2003; 91(3): 321–5. DOI: 10.1016/S0002-9149(02)03159-4 [DOI] [PubMed] [Google Scholar]
- 29.Vona M, Rossi A, Capodaglio P, et al. Impact of physical training and detraining on endothelium-dependent vasodilation in patients with recent acute myocardial infarction. American Heart Journal. 2004; 147(6): 1039–46. DOI: 10.1016/j.ahj.2003.12.023 [DOI] [PubMed] [Google Scholar]
- 30.Volaklis KA, Spassis AT, Tokmakidis SP. Land versus water exercise in patients with coronary artery disease: effects on body composition, blood lipids, and physical fitness. American Heart Journal. 2007; 154(3): 560.e1–6. DOI: 10.1016/j.ahj.2007.06.029 [DOI] [PubMed] [Google Scholar]
- 31.Zutz A, Ignaszewski A, Bates J, Lear SA. Utilization of the internet to deliver cardiac rehabilitation at a distance: a pilot study. Telemedicine Journal and E-health: the Official Journal of the American Telemedicine Association. 2007; 13(3): 323–30. DOI: 10.1089/tmj.2006.0051 [DOI] [PubMed] [Google Scholar]
- 32.Balen S, Vukelić-Damijani N, Persić V, et al. Anti-inflammatory effects of exercise training in the early period after myocardial infarction. Collegium Antropologicum. 2008; 32(1): 285–91. [PubMed] [Google Scholar]
- 33.Naser A, Jafar S, Kumar GV, et al. Cardiac risk factor changes through an intensive multifactorial life style modification program in CHD patients: results from a two year follow up. Aust J Biol Sci. 2008; 8(2): 248–57. DOI: 10.3923/jbs.2008.248.257 [DOI] [Google Scholar]
- 34.Seki E, Watanabe Y, Shimada K, et al. Effects of a phase III cardiac rehabilitation program on physical status and lipid profiles in elderly patients with coronary artery disease: Juntendo Cardiac Rehabilitation Program (J-CARP). Circulation Journal: Official Journal of the Japanese Circulation Society. 2008; 72(8): 1230–4. DOI: 10.1253/circj.72.1230 [DOI] [PubMed] [Google Scholar]
- 35.Murphy AW, Cupples ME, Smith SM, et al. Effect of tailored practice and patient care plans on secondary prevention of heart disease in general practice: cluster randomised controlled trial. BMJ (Clinical research ed). 2009; 339: b4220. DOI: 10.1136/bmj.b4220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Munk PS, Breland UM, Aukrust P, et al. High intensity interval training reduces systemic inflammation in post-PCI patients. European Journal of Cardiovascular Prevention and Rehabilitation: Official Journal of the European Society of Cardiology, Working Groups on Epidemiology & Prevention and Cardiac Rehabilitation and Exercise Physiology. 2011; 18(6): 850–7. DOI: 10.1177/1741826710397600 [DOI] [PubMed] [Google Scholar]
- 37.Zetta S, Smith K, Jones M, Allcoat P, Sullivan F. Evaluating the angina plan in patients admitted to hospital with angina: a randomized controlled trial. Cardiovascular Therapeutics. 2011; 29(2): 112–24. DOI: 10.1111/j.1755-5922.2009.00109.x [DOI] [PubMed] [Google Scholar]
- 38.Luk TH, Dai YL, Siu CW, et al. Effect of exercise training on vascular endothelial function in patients with stable coronary artery disease: a randomized controlled trial. European Journal of Preventive Cardiology. 2012; 19(4): 830–9. DOI: 10.1177/1741826711415679 [DOI] [PubMed] [Google Scholar]
- 39.Moholdt T, Aamot IL, Granøien I, et al. Aerobic interval training increases peak oxygen uptake more than usual care exercise training in myocardial infarction patients: a randomized controlled study. Clinical Rehabilitation. 2012; 26(1): 33–44. DOI: 10.1177/0269215511405229 [DOI] [PubMed] [Google Scholar]
- 40.Oerkild B, Frederiksen M, Hansen JF, Prescott E. Home-based cardiac rehabilitation is an attractive alternative to no cardiac rehabilitation for elderly patients with coronary heart disease: results from a randomised clinical trial. BMJ Open. 2012; 2(6). DOI: 10.1136/bmjopen-2012-001820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Vernooij JW, Kaasjager HA, van der Graaf Y, et al. Internet based vascular risk factor management for patients with clinically manifest vascular disease: randomised controlled trial. BMJ (Clinical research ed). 2012; 344: e3750. DOI: 10.1136/bmj.e3750 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lear SA, Singer J, Banner-Lukaris D, et al. Randomized trial of a virtual cardiac rehabilitation program delivered at a distance via the Internet. Circulation Cardiovascular Quality and Outcomes. 2014; 7(6): 952–9. DOI: 10.1161/CIRCOUTCOMES.114.001230 [DOI] [PubMed] [Google Scholar]
- 43.Raghuram N, Parachuri VR, Swarnagowri MV, et al. Yoga based cardiac rehabilitation after coronary artery bypass surgery: One-year results on LVEF, lipid profile and psychological states – A randomized controlled study. Indian Heart Journal. 2014; 66(5): 490–502. DOI: 10.1016/j.ihj.2014.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chow CK, Redfern J, Hillis GS, et al. Effect of Lifestyle-Focused Text Messaging on Risk Factor Modification in Patients with Coronary Heart Disease: A Randomized Clinical Trial. Jama. 2015; 314(12): 1255–63. DOI: 10.1001/jama.2015.10945 [DOI] [PubMed] [Google Scholar]
- 45.Hassan AM ENN. Efficacy of cardiac rehabilitation after percutaneous coronary intervention. Int J PharmTech Res. 2016; 9: 134–41. [Google Scholar]
- 46.Johnston N, Bodegard J, Jerström S, et al. Effects of interactive patient smartphone support app on drug adherence and lifestyle changes in myocardial infarction patients: A randomized study. American Heart Journal. 2016; 178: 85–94. DOI: 10.1016/j.ahj.2016.05.005 [DOI] [PubMed] [Google Scholar]
- 47.Tamburús NY, Kunz VC, Salviati MR, et al. Interval training based on ventilatory anaerobic threshold improves aerobic functional capacity and metabolic profile: a randomized controlled trial in coronary artery disease patients. European Journal of Physical and Rehabilitation Medicine. 2016; 52(1): 1–11. PMID:26086326 [PubMed] [Google Scholar]
- 48.Lin CY, Yaseri M, Pakpour AH, et al. Can a Multifaceted Intervention Including Motivational Interviewing Improve Medication Adherence, Quality of Life, and Mortality Rates in Older Patients Undergoing Coronary Artery Bypass Surgery? A Multicenter, Randomized Controlled Trial with 18-Month Follow-Up. Drugs & Aging. 2017; 34(2): 143–56. DOI: 10.1007/s40266-016-0429-3 [DOI] [PubMed] [Google Scholar]
- 49.Park M, Song R, Jeong JO. Effect of goal attainment theory based education program on cardiovascular risks, behavioral modification, and quality of life among patients with first episode of acute myocardial infarction: Randomized study. International Journal of Nursing Studies. 2017; 71: 8–16. DOI: 10.1016/j.ijnurstu.2017.02.019 [DOI] [PubMed] [Google Scholar]
- 50.Chaves GSS, Lima de Melo Ghisi G, Britto RR, Grace SL. Maintenance of Gains, Morbidity, and Mortality at 1 Year Following Cardiac Rehabilitation in a Middle-Income Country: A Wait-List Control Crossover Trial. Journal of the American Heart Association. 2019; 8(4): e011228–e. DOI: 10.1161/JAHA.118.011228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Dorje T, Zhao G, Tso K, et al. Smartphone and social media-based cardiac rehabilitation and secondary prevention in China (SMART-CR/SP): a parallel-group, single-blind, randomised controlled trial. The Lancet Digital Health. 2019; 1(7): e363–e74. DOI: 10.1016/S2589-7500(19)30151-7 [DOI] [PubMed] [Google Scholar]
- 52.Maddison R, Rawstorn JC, Stewart RAH, et al. Effects and costs of real-time cardiac telerehabilitation: randomised controlled non-inferiority trial. Heart (British Cardiac Society). 2019; 105(2): 122–9. DOI: 10.1136/heartjnl-2018-313189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Santo K, Singleton A, Rogers K, et al. Medication reminder applications to improve adherence in coronary heart disease: a randomised clinical trial. Heart (British Cardiac Society). 2019; 105(4): 323–9. DOI: 10.1136/heartjnl-2018-313479 [DOI] [PubMed] [Google Scholar]
- 54.Wienbergen H, Fach A, Meyer S, et al. Effects of an intensive long-term prevention programme after myocardial infarction – a randomized trial. European Journal of Preventive Cardiology. 2019; 26(5): 522–30. DOI: 10.1177/2047487318781109 [DOI] [PubMed] [Google Scholar]
- 55.Zheng X, Spatz ES, Bai X, et al. Effect of Text Messaging on Risk Factor Management in Patients with Coronary Heart Disease: The CHAT Randomized Clinical Trial. Circulation Cardiovascular Quality and Outcomes. 2019; 12(4): e005616. DOI: 10.1161/CIRCOUTCOMES.119.005616 [DOI] [PubMed] [Google Scholar]
- 56.Campo G, Tonet E, Chiaranda G, et al. Exercise intervention improves quality of life in older adults after myocardial infarction: randomised clinical trial. Heart (British Cardiac Society). 2020; 106(21): 1658–64. DOI: 10.1136/heartjnl-2019-316349 [DOI] [PubMed] [Google Scholar]
- 57.Uddin J, Joshi VL, Moniruzzaman M, et al. Effect of Home-Based Cardiac Rehabilitation in a Lower-Middle Income Country: RESULTS FROM A CONTROLLED TRIAL. Journal of Cardiopulmonary Rehabilitation and Prevention. 2020; 40(1): 29–34. DOI: 10.1097/HCR.0000000000000471 [DOI] [PubMed] [Google Scholar]
- 58.Yudi MB, Clark DJ, Tsang D, et al. SMARTphone-based, early cardiac REHABilitation in patients with acute coronary syndromes: a randomized controlled trial. Coronary Artery Disease. 2021; 32(5): 432–40. DOI: 10.1097/MCA.0000000000000938 [DOI] [PubMed] [Google Scholar]
- 59.Dalli Peydró E, Sanz Sevilla N, Tuzón Segarra MT, et al. A randomized controlled clinical trial of cardiac telerehabilitation with a prolonged mobile care monitoring strategy after an acute coronary syndrome. Clinical Cardiology. 2022; 45(1): 31–41. DOI: 10.1002/clc.23757 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figures S1 to S3.
Tables S1 to S7.
Data Availability Statement
All data generated or analyzed during this study are included in this published article and its supplementary information files.


